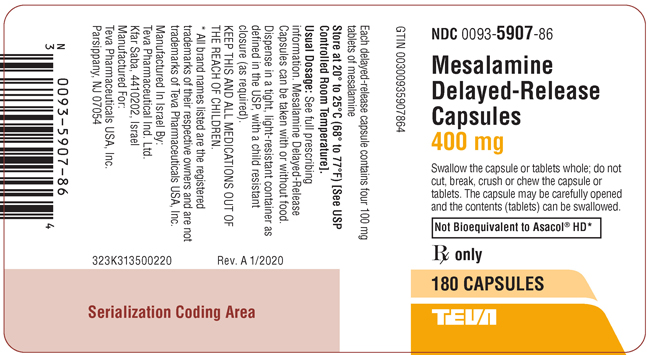
Label: MESALAMINE capsule, delayed release
- NDC Code(s): 0093-5907-86
- Packager: Teva Pharmaceuticals USA, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated May 31, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MESALAMINE DELAYED-RELEASE CAPSULES safely and effectively. See full prescribing information for MESALAMINE DELAYED-RELEASE CAPSULES.
MESALAMINE delayed-release capsules, for oral use
Initial U.S. Approval: 1987INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
Important Administration Instructions:
- Do not substitute two mesalamine delayed-release 400 mg capsules with one mesalamine delayed-release 800 mg tablet. (2.1)
- Evaluate renal function prior to initiation of mesalamine delayed-release capsules. (2.1, 5.1)
- Take with or without food. (2.1)
- Swallow the capsules whole; do not cut, break, crush or chew. (2.1)
- For patients who are unable to swallow the capsules, the capsules can be opened and the inner tablets swallowed. (2.1)
- Drink an adequate amount of fluids. (2.1, 5.7)
Treatment of Mildly to Moderately Active Ulcerative Colitis:
- Adults: 800 mg (two 400 mg capsules) three times daily for 6 weeks.
- Pediatric Patients 5 years or older: See weight-based dosing table in the full prescribing information; twice daily dosing for 6 weeks. (2.2)
Maintenance of Remission of Ulcerative Colitis:
- Adults: 1.6 grams (four 400 mg capsules) daily, in two to four divided doses. (2.3)
DOSAGE FORMS AND STRENGTHS
Delayed-release capsules (containing four 100 mg tablets): 400 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Renal Impairment: Assess renal function at the beginning of treatment and periodically during treatment. Evaluate the risks and benefits of using mesalamine delayed-release capsules in patients with known renal impairment or taking nephrotoxic drugs; monitor renal function. Discontinue mesalamine delayed-release capsules if renal function deteriorates. (5.1, 7.1, 8.6, 13.2)
- Mesalamine-induced Acute Intolerance Syndrome: Symptoms may be difficult to distinguish from an ulcerative colitis exacerbation; monitor for worsening symptoms while on treatment; discontinue treatment, if acute intolerance syndrome is suspected. (5.2)
- Hypersensitivity Reactions, including myocarditis and pericarditis: Evaluate patients immediately and discontinue mesalamine delayed-release capsules, if a hypersensitivity reaction is suspected. (5.3)
- Hepatic Failure: Evaluate the risks and benefits of using mesalamine delayed-release capsules in patients with known liver impairment. (5.4)
- Severe Cutaneous Adverse Reactions: Discontinue at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation. (5.5)
-
Photosensitivity: Advise patients with pre-existing skin conditions to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors. (5.6)
- Nephrolithiasis: Mesalamine-containing stones undetectable by standard radiography or computed tomography (CT). Ensure adequate fluid intake during treatment. (5.7)
- Iron Content of Mesalamine Delayed-Release Capsules: Consider the iron content of mesalamine delayed-release capsules in patients taking iron supplementation and those at risk of iron overload. (5.8)
- Interference with Laboratory Tests: Use of mesalamine may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection. (5.9)
ADVERSE REACTIONS
The most common adverse reactions (≥5%) are:
- Adults: eructation, abdominal pain, constipation, dizziness, rhinitis, back pain, and rash. (6.1)
- Pediatrics: nasopharyngitis, headache, abdominal pain, dizziness, sinusitis, rash, cough and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Teva at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
Geriatric Patients: Increased risk of blood dyscrasias; monitor complete blood cell counts and platelet counts. (8.5)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Treatment of Mildly to Moderately Active Ulcerative Colitis
1.2 Maintenance of Remission of Ulcerative Colitis
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosage for Treatment of Mildly to Moderately Active Ulcerative Colitis
2.3 Dosage for Maintenance of Remission of Ulcerative Colitis
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Renal Impairment
5.2 Mesalamine-Induced Acute Intolerance Syndrome
5.3 Hypersensitivity Reactions
5.4 Hepatic Failure
5.5 Severe Cutaneous Adverse Reactions
5.6 Photosensitivity
5.7 Nephrolithiasis
5.8 Iron Content of Mesalamine Delayed-Release Capsules
5.9 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Nephrotoxic Agents, Including Non-Steroidal Anti-Inflammatory Drugs
7.2 Azathioprine or 6-Mercaptopurine
7.3 Interference With Urinary Normetanephrine Measurements
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Treatment of Mildly to Moderately Active Ulcerative Colitis
14.2 Maintenance of Remission of Ulcerative Colitis
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
- Do not substitute two mesalamine delayed-release 400 mg capsules with one mesalamine delayed-release 800 mg tablet.
- Evaluate renal function prior to initiation of mesalamine delayed-release capsules.
- Take mesalamine delayed-release capsules with or without food.
- Swallow the capsules whole; do not cut, break, crush or chew the capsules.
- For patients who are unable to swallow the capsules whole, carefully open the capsule(s) and swallow the contents (four 100 mg tablets).
- Open the number of capsules required to make up a complete dose [see Dosage and Administration (2.2, 2.3)].
- There are 4 tablets per capsule. Ensure all tablets per capsule are swallowed and no tablets are retained in the mouth.
- Swallow the tablets whole; do not cut, break, crush or chew the tablets.
- Drink an adequate amount of fluids [see Warnings and Precautions (5.7)].
- Intact, partially intact, and/or tablet shells have been reported in the stool; Instruct patients to contact their healthcare provider if this occurs repeatedly. Protect mesalamine delayed-release capsules from moisture. Close the container tightly and leave any desiccant pouches present in the bottle along with the capsules.
2.2 Dosage for Treatment of Mildly to Moderately Active Ulcerative Colitis
Adults
For adults, the recommended dosage of mesalamine delayed-release capsules is 800 mg (two 400 mg capsules) three times daily (total daily dosage of 2.4 grams) for a duration of 6 weeks [see Clinical Studies (14.1)].
Pediatrics
For pediatric patients 5 years of age and older, the recommended total daily dosage of mesalamine delayed-release capsules is weight-based (up to maximum of 2.4 grams per day) divided into two daily doses for a duration of 6 weeks (see Table 1).
Table 1. Pediatric Dosage by Weight Weight Group (kg)
Daily Dosage (mg/kg/day)
Maximum Daily Dosage
(grams per day)Morning Dosage
Afternoon Dosage
17 to 32
36 to 71
1.2
two 400 mg capsules
one 400 mg capsules
33 to 53
37 to 61
2
three 400 mg capsules
two 400 mg capsules
54 to 90
27 to 44
2.4
three 400 mg capsules
three 400 mg capsules
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Renal Impairment
Renal impairment, including minimal change disease, acute and chronic interstitial nephritis, and renal failure, has been reported in patients taking products such as mesalamine delayed-release capsules that contain mesalamine or are converted to mesalamine. In animal studies, the kidney was the principal organ of mesalamine toxicity [see Adverse Reactions (6.2), Nonclinical Toxicology (13.2)].
Evaluate renal function prior to initiation of mesalamine delayed-release capsules and periodically while on therapy. Discontinue mesalamine delayed-release capsules if renal function deteriorates while on therapy.
Evaluate the risks and benefits of using mesalamine delayed-release capsules in patients with known renal impairment or history of renal disease or taking concomitant nephrotoxic drugs [see Drug Interactions (7.1), Use in Specific Populations (8.6)].
5.2 Mesalamine-Induced Acute Intolerance Syndrome
Mesalamine has been associated with an acute intolerance syndrome that may be difficult to distinguish from an exacerbation of ulcerative colitis. Although the exact frequency of occurrence has not been determined, it has occurred in 3% of controlled clinical trials of mesalamine or sulfasalazine. Symptoms include cramping, abdominal pain, bloody diarrhea, and sometimes fever, headache, malaise, pruritus, conjunctivitis and rash. Monitor patients closely for worsening of these symptoms while on treatment. If acute intolerance syndrome is suspected, promptly discontinue treatment with mesalamine delayed-release capsules.
5.3 Hypersensitivity Reactions
Hypersensitivity reactions have been reported in patients taking sulfasalazine. Some patients may have a similar reaction to mesalamine or to other compounds that contain or are converted to mesalamine.
As with sulfasalazine, mesalamine-induced hypersensitivity reactions may present as internal organ involvement, including myocarditis, pericarditis, nephritis, hepatitis, pneumonitis, and hematologic abnormalities. Evaluate patients immediately if signs or symptoms of a hypersensitivity reaction are present. Discontinue mesalamine delayed-release capsules if an alternative etiology for the signs or symptoms cannot be established.
5.4 Hepatic Failure
There have been reports of hepatic failure in patients with pre-existing liver disease who have been administered mesalamine. Evaluate the risk and benefits of using mesalamine delayed-release capsules in patients with known liver impairment.
5.5 Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported with the use of mesalamine [see Adverse Reactions (6.2)]. Discontinue mesalamine delayed-release capsules at the first appearance of signs or symptoms of severe cutaneous adverse reactions, or other signs of hypersensitivity and consider further evaluation.
5.6 Photosensitivity
Patients treated with mesalamine or sulfasalazine who have pre-existing skin conditions such as atopic dermatitis and atopic eczema have reported more severe photosensitivity reactions. Advise patients to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors.
5.7 Nephrolithiasis
Cases of nephrolithiasis have been reported with the use of mesalamine, including stones of 100% mesalamine content. Mesalamine-containing stones are radiotransparent and undetectable by standard radiography or computed tomography (CT). Ensure adequate fluid intake during treatment with mesalamine delayed-release capsules.
5.8 Iron Content of Mesalamine Delayed-Release Capsules
Mesalamine delayed-release capsules contains iron oxide as a colorant in the coating of the delayed-release capsules. Each 400 mg delayed-release capsule contains 0.589 mg of iron. The total content of iron is 3.54 mg at the maximum recommended daily dosage in adults [see Dosage and Administration (2.2)]. Before prescribing mesalamine delayed-release capsules to patients receiving iron supplementation or those at risk of developing iron overload, consider the combined daily amount of iron from all sources, including mesalamine delayed-release capsules.
5.9 Interference with Laboratory Tests
Use of mesalamine delayed-release capsules may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection because of the similarity in the chromatograms of normetanephrine and the main metabolite of mesalamine, N-acetyl-5-aminosalicylic acid (N-Ac-5-ASA). Consider an alternative, selective assay for normetanephrine.
-
6 ADVERSE REACTIONS
The most serious adverse reactions seen in mesalamine clinical trials or with other products that contain or are metabolized to mesalamine are:
- Renal Impairment [see Warnings and Precautions (5.1)]
- Mesalamine-Induced Acute Intolerance Syndrome [see Warnings and Precautions (5.2)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Hepatic Failure [see Warnings and Precautions (5.4)]
- Severe Cutaneous Adverse Reactions [see Warnings and Precautions (5.5)]
- Photosensitivity [see Warnings and Precautions (5.6)]
- Nephrolithiasis [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of mesalamine has been established based on adequate and well-controlled studies of mesalamine delayed-release tablets. In total, mesalamine delayed-release 400 mg tablets have been evaluated in 2690 patients with ulcerative colitis in controlled and open-label trials. Below is a description of the adverse reactions of mesalamine delayed-release tablets in these adequate and well-controlled studies.
Clinical studies supporting mesalamine delayed-release tablets use for the treatment of mildly to moderately active ulcerative colitis included two 6-week, placebo-controlled, randomized, double-blind studies in adults with mildly to moderately active ulcerative colitis (Studies 1 and 2), and one 6-week, randomized, double-blind, study of 2 dosage levels in children with mildly to moderately active ulcerative colitis (Study 3). Clinical studies supporting the use of mesalamine delayed-release tablets in the maintenance of remission of ulcerative colitis included a 6-month, randomized, double-blind, placebo-controlled, multi-center study (Study 4) and four active-controlled maintenance trials comparing mesalamine delayed-release with sulfasalazine. Mesalamine delayed-release tablets have been evaluated in 427 adults and 107 children with ulcerative colitis in these controlled studies.
Treatment of Mildly to Moderately Active Ulcerative Colitis
Adults
In a 6-week placebo-controlled clinical study (Study 1) involving 105 patients, 53 of whom were randomized to mesalamine delayed-release tablets 2.4 grams per day [see Clinical Studies (14.1)], 4% of the mesalamine delayed release tablets-treated patients in 2.4 grams per day group discontinued therapy because of adverse reactions as compared to 0% of the placebo-treated patients. The average age of patients was 41 years and 49% of patients were male. Adverse reactions leading to withdrawal from mesalamine delayed-release tablets included (each in one patient): diarrhea and colitis flare; dizziness, nausea, joint pain, and headache.
The most common adverse reactions in patients treated with mesalamine delayed release tablets 2.4 grams per day in Study 1 are listed in Table 2 below.
Table 2. Most Common Adverse Reactions Reported in Study 1 for the Treatment of Mild to Moderate Ulcerative Colitis in Adults* Adverse Reaction
% of Patients with Adverse Reactions
Mesalamine Delayed-Release
2.4 grams per dayPlacebo
(n = 53)
(n = 52)
Eructation
26
19
Abdominal pain
21
12
Constipation
11
0
Dizziness
9
8
Rhinitis
8
6
Back pain
6
4
Rash
6
4
Dyspepsia
4
0
Flu syndrome
4
2
* At Least 2% of Patients in the Mesalamine Delayed-Release Tablets Group and at a Rate Greater than Placebo Pediatric Patients 5 to 17 Years Old
A randomized, double-blind, 6-week study of 2 dosage levels of mesalamine delayed-release 400 mg tablets (Study 3) was conducted in 82 pediatric patients 5 to 17 years of age with mildly to moderately active ulcerative colitis. All patients were divided by body weight category (17 to less than 33 kg, 33 to less than 54 kg, and 54 to 90 kg) and randomly assigned to receive a low dosage (1.2, 2, and 2.4 grams per day for the respective body weight category) or a high dosage (2.0, 3.6, and 4.8 grams per day).
The high dosage regimen is not recommended because it was not found to be more effective than the recommended low dosage regimen [see Dosage and Administration (2.2), Clinical Studies (14.1)].
Duration of exposure to mesalamine among the 82 patients in the study ranged from 12 to 50 days (mean of 40 days in each dosage group). The majority (88%) of patients in each group were treated for more than 5 weeks. Table 3 provides a summary of the specific reported adverse reactions.
Table 3. Adverse Reactions ≥ 5% Reported in Study 3 for the Treatment of Mild to Moderate Ulcerative Colitis in Pediatric Patients* Adverse Reaction
% of Patients with Adverse Reactions
Low Dosage
High Dosage
(n=41)
(n=41)
Nasopharyngitis
15
12
Headache
10
5
Abdominal pain
10
2
Dizziness
7
2
Sinusitis
7
0
Rash
5
5
Cough
5
0
Diarrhea
5
0
Fatigue
2
10
Pyrexia
0
7
Increased Lipase
0
5
Low Dosage = mesalamine 400 mg delayed-release tablet 1.2 to 2.4 grams/day; High Dosage = mesalamine 400 mg delayed-release tablet 2.0 to 4.8 grams/day. Dosage was dependent on body weight.
Adverse Reactions reported at the 1-week telephone follow-up visit are included.* At Least 5% of Patients in the low dosage or high dosage group Twelve percent of the patients in the low dosage group (5 patients) and 2% of the patients in the high dosage group (1 patient) had serious adverse reactions. The serious adverse reactions consisted of sinusitis, adenovirus infection, and pancreatitis in one patient each in the low dosage group. Abdominal pain and decreased body mass index occurred in one patient and bloody diarrhea and sclerosing cholangitis also occurred in one patient in the low dosage group. Anemia and syncope occurred in one patient in the high dosage group.
Five patients were withdrawn from the study due to adverse reactions: 3 (7%) in the low dosage group (1 patient each with adenovirus infection, sclerosing cholangitis, and pancreatitis) and 2 patients (5%) in the high dosage group (1 patient with increased amylase and increased lipase, and 1 patient with upper abdominal pain).
In general, the nature and severity of reactions in the pediatric population was similar to those reported in adult populations of patients with ulcerative colitis.
Maintenance of Remission of Ulcerative Colitis
Clinical studies supporting the use of mesalamine delayed release tablets in the maintenance of remission of ulcerative colitis in adults included a randomized, double-blind, multi-center, placebo-controlled clinical trial of 6 months’ duration in 264 patients (Study 4) [see Clinical Studies (14.2)].
In Study 4, a randomized, double-blind, multi-center, placebo-controlled clinical trial of 6 months’ duration, 87 patients were randomized to receive mesalamine delayed release tablets 1.6 grams per /day compared to 87 patients randomized to placebo. The average age of patients in Study 4 was 42 years and 55% of patients were male. Adverse reactions leading to study withdrawal in patients using mesalamine delayed release tablets included (each in one patient): anxiety, stomatitis and asthenia.
In addition to the adverse reactions listed in Table 2, the following occurred at a frequency of 2% or greater in patients who received mesalamine delayed-release tablets in Study 4: abdominal enlargement, gastroenteritis, gastrointestinal hemorrhage, infection, joint disorder, nervousness, paresthesia, hemorrhoids, tenesmus, urinary frequency and vision abnormalities.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of mesalamine delayed-release capsules or other mesalamine-containing products. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole: Neck pain, facial edema, edema, lupus-like syndrome, drug fever.
Cardiovascular: Pericarditis, myocarditis [see Warnings and Precautions (5.3)].
Endocrine: Nephrogenic diabetes insipidus.
Gastrointestinal: Anorexia, pancreatitis, gastritis, increased appetite, cholecystitis, dry mouth, oral ulcers, perforated peptic ulcer, bloody diarrhea.
Hematologic: Agranulocytosis, aplastic anemia, thrombocytopenia, eosinophilia, leukopenia, anemia, lymphadenopathy.
Musculoskeletal: Gout.
Nervous: Depression, somnolence, emotional lability, hyperesthesia, vertigo, confusion, tremor, peripheral neuropathy, transverse myelitis, Guillain-Barré syndrome, intracranial hypertension.
Renal: Renal failure, interstitial nephritis, minimal change disease, nephrolithiasis [see Warnings and Precautions (5.1, 5.7)].
Respiratory/Pulmonary: Eosinophilic pneumonia, interstitial pneumonitis, asthma exacerbation, pleurisy/pleuritis.
Skin: Alopecia, psoriasis, pyoderma gangrenosum, dry skin, erythema nodosum, urticaria, SJS/TEN, DRESS, and AGEP [see Warnings and Precautions (5.5)].
Special Senses: Eye pain, taste perversion, blurred vision, tinnitus.
Urogenital: Dysuria, urinary urgency, hematuria, epididymitis, menorrhagia, reversible oligospermia.
- Urine discoloration occurring ex-vivo caused by contact of mesalamine, including inactive metabolite, with surfaces or water treated with hypochlorite containing bleach.
Laboratory Abnormalities: Elevated AST (SGOT) or ALT (SGPT), elevated alkaline phosphatase, elevated GGT, elevated LDH, elevated bilirubin, elevated serum creatinine and BUN.
-
7 DRUG INTERACTIONS
7.1 Nephrotoxic Agents, Including Non-Steroidal Anti-Inflammatory Drugs
The concurrent use of mesalamine with known nephrotoxic agents, including non-steroidal anti-inflammatory drugs (NSAIDs) may increase the risk of nephrotoxicity. Monitor patients taking nephrotoxic drugs for changes in renal function and mesalamine-related adverse reactions [see Warnings and Precautions (5.1)].
7.2 Azathioprine or 6-Mercaptopurine
The concurrent use of mesalamine with azathioprine or 6-mercaptopurine and/or other drugs known to cause myelotoxicity may increase the risk for blood disorders, bone marrow failure, and associated complications. If concomitant use of mesalamine delayed-release capsules and azathioprine or 6-mercaptopurine cannot be avoided, monitor blood tests, including complete blood cell counts and platelet counts.
7.3 Interference With Urinary Normetanephrine Measurements
Use of mesalamine delayed-release capsules may lead to spuriously elevated test results when measuring urinary normetanephrine by liquid chromatography with electrochemical detection [see Warnings and Precautions (5.9)]. Consider an alternative, selective assay for normetanephrine.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate and well controlled studies of mesalamine use in pregnant women. Limited published human data on mesalamine show no increase in the overall rate of congenital malformations. Some data show an increased rate of preterm birth, stillbirth, and low birth weight; however, these adverse pregnancy outcomes are also associated with active inflammatory bowel disease. Furthermore, all pregnancies, regardless of drug exposure, have a background rate of 2% to 4% for major malformations, and 15% to 20% for pregnancy loss. No evidence of fetal harm was observed in animal reproduction studies of mesalamine in rats and rabbits at oral doses approximately 1.9 times (rat) and 3.9 times (rabbit) the recommended human dose. Mesalamine should be used during pregnancy only if clearly needed.
Human Data
Mesalamine crosses the placenta. In prospective and retrospective studies of over 600 women exposed to mesalamine during pregnancy, the observed rate of congenital malformations was not increased above the background rate in the general population. Some data show an increased rate of preterm birth, stillbirth, and low birth weight, but it is unclear whether this was due to underlying maternal disease, drug exposure, or both, as active inflammatory bowel disease is also associated with adverse pregnancy outcomes.
Animal data
Reproduction studies with mesalamine were performed during organogenesis in rats and rabbits at oral doses up to 480 mg/kg/day. There was no evidence of impaired fertility or harm to the fetus. These mesalamine doses were about 1.9 times (rat) and 3.9 times (rabbit) the recommended human dose, based on body surface area.
8.2 Lactation
Mesalamine and its N-acetyl metabolite are present in human milk. In published lactation studies, maternal mesalamine doses from various oral and rectal formulations and products ranged from 500 mg to 3 g daily. The concentration of mesalamine in milk ranged from non-detectable to 0.11 mg/L. The concentration of the N-acetyl-5-aminosalicylic acid metabolite ranged from 5 mg/L to 18.1 mg/L. Based on these concentrations, estimated infant daily doses for an exclusively breastfed infant are 0 mg/kg/day to 0.017 mg/kg/day of mesalamine and 0.75 mg/kg/day to 2.72 mg/kg/day of N-acetyl-5-aminosalicylic acid. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for mesalamine and any potential adverse effects on the breastfed child from the drug or from the underlying maternal condition. Caution should be exercised when mesalamine delayed-release capsules are administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of mesalamine delayed-release capsules for the treatment of mildly to moderately active ulcerative colitis in pediatric patients 5 to 17 years of age has been established based on adequate and well-controlled studies using mesalamine delayed-release 400 mg tablets. Use of mesalamine delayed-release capsules in these pediatric age groups is supported by evidence from adequate and well controlled studies of mesalamine delayed-release 400 mg tablets in adults and a single 6-week study in 82 pediatric patients 5 to 17 years of age [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), Clinical Studies (14.1)].
The safety and effectiveness of mesalamine delayed-release capsules for the treatment of mildly to moderately active ulcerative colitis in pediatric patients below the age of 5 years have not been established. The safety and effectiveness of mesalamine delayed-release capsules in the maintenance of remission of ulcerative colitis in pediatric patients have not been established.
8.5 Geriatric Use
Clinical studies of mesalamine delayed-release tablets did not include sufficient numbers of patients aged 65 years and over to determine whether they respond differently than younger patients. Reports from uncontrolled clinical studies and postmarketing experience suggest a higher incidence of blood dyscrasias (agranulocytosis, neutropenia, pancytopenia) in subjects receiving mesalamine delayed-release tablets who are 65 years or older compared to younger patients taking mesalamine-containing products such as mesalamine delayed-release capsules. Monitor complete blood cell counts and platelet counts in elderly patients during treatment with mesalamine delayed-release capsules.
In general, consider the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy in elderly patients when prescribing mesalamine delayed-release capsules [see Use in Specific Populations (8.6)].
8.6 Renal Impairment
Mesalamine is known to be substantially excreted by the kidney, and the risk of toxic reactions may be greater in patients with impaired renal function. Evaluate renal function in all patients prior to initiation and periodically while on mesalamine delayed-release capsules therapy. Monitor patients with known renal impairment or history of renal disease or taking nephrotoxic drugs for decreased renal function and mesalamine-related adverse reactions. Discontinue mesalamine delayed-release capsules if renal function deteriorates while on therapy [see Warnings and Precautions (5.1), Adverse Reactions (6.2), Drug Interactions (7.1)].
-
10 OVERDOSAGE
Mesalamine delayed-release capsules is an aminosalicylate, and symptoms of salicylate toxicity include nausea, vomiting and abdominal pain, tachypnea, hyperpnea, tinnitus, and neurologic symptoms (headache, dizziness, confusion, seizures). Severe salicylate intoxication may lead to electrolyte and blood pH imbalance and potentially to other organ (e.g., renal and liver) involvement. There is no specific antidote for mesalamine overdose; however, conventional therapy for salicylate toxicity may be beneficial in the event of acute overdosage and may include gastrointestinal tract decontamination to prevent of further absorption. Correct fluid and electrolyte imbalance by the administration of appropriate intravenous therapy and maintain adequate renal function.
Mesalamine delayed-release capsules is a pH dependent delayed-release product and this factor should be considered when treating a suspected overdose.
-
11 DESCRIPTION
Each Mesalamine delayed-release capsule for oral administration contains four 100 mg tablets of mesalamine, an aminosalicylate. Mesalamine delayed-release capsules contain acrylic based resin, methacrylic acid copolymer (Eudragit S), which dissolves at pH 7 or greater and releases mesalamine in the terminal ileum and beyond for topical anti-inflammatory action in the colon. Mesalamine, USP (also referred to as 5-aminosalicylic acid or 5-ASA) has the chemical name 5-amino-2-hydroxybenzoic acid. Its structural formula is:
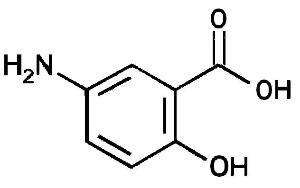
C7H7NO3 M.W. 153.14
Inactive Ingredients: Each capsule contains colloidal silicon dioxide, dibutyl sebacate, hypromellose, iron oxide black, iron oxide red, lactose monohydrate, magnesium stearate, methacrylic acid copolymer, polyethylene glycol, potassium hydroxide, povidone, propylene glycol, shellac, sodium starch glycolate (potato), and talc.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of mesalamine is not fully understood, but appears to be a topical anti-inflammatory effect on colonic epithelial cells. Mucosal production of arachidonic acid metabolites, both through the cyclooxygenase pathways, that is, prostanoids, and through the lipoxygenase pathways, that is, leukotrienes and hydroxyeicosatetraenoic acids, is increased in patients with ulcerative colitis, and it is possible that mesalamine diminishes inflammation by blocking cyclooxygenase and inhibiting prostaglandin production in the colon.
12.3 Pharmacokinetics
Absorption
Approximately 28% of mesalamine in mesalamine delayed-release formulation is absorbed after oral ingestion. Following replicate single dose oral administration of mesalamine delayed-release 400 mg capsules containing four 100 mg tablets in healthy subjects (N = 146) under fasted conditions, the mean Cmax, AUC8-48 and AUCtldc values were 150 ± 235 ng/mL, 640 ± 521 ng.h/mL, and 909 ± 777 ng.h/mL, respectively. The median [range] Tmax for mesalamine following mesalamine delayed-release 400 mg capsules containing four 100 mg tablets was approximately 10 hours [5.5 to 48 hours], reflecting the delayed-release characteristics of the formulation.
A high fat meal increased systemic exposure of mesalamine (geometric mean Cmax: ↑ 32%; AUC8-48 h: ↑ 46%; AUC: ↑ 29%) and delayed the median tmax by approximately 4 hours compared to results in the fasted state. The observed differences in mesalamine exposure due to concomitant food intake are not considered to be clinically relevant at the total daily dosage of 2.4 grams per day.
Elimination
Metabolism
The absorbed mesalamine is rapidly acetylated in the gut mucosal wall and by the liver to N-acetyl-5-aminosalicylic acid.
Excretion
Absorbed mesalamine is excreted mainly by the kidney as N-acetyl-5-aminosalicylic acid. Unabsorbed mesalamine is excreted in feces.
After intravenous administration, the elimination half-life of mesalamine is reported to be approximately 40 minutes. After oral dosing, the median terminal t1/2 values for mesalamine are usually about 25 hours, but are variable, ranging from 1.5 to 296 hours. There is a large inter-subject and intra-subject variability in the plasma concentrations of mesalamine and N-acetyl-5-aminosalicylic acid and in their terminal half-lives following administration of mesalamine.
Specific Populations
Pediatric Patients
In a dose-ranging pharmacokinetic study evaluating 30 mg/kg, 60 mg/kg and 90 mg/kg per day doses of mesalamine delayed-release 400 mg tablets administered twice daily for four weeks, the mean Cavg values of mesalamine in pediatric ulcerative colitis patients ranged from approximately 400 ng/mL to 2100 ng/mL based on data from all dose levels.
In a study evaluating mesalamine delayed-release tablets in pediatric ulcerative colitis patients (Study 3), mean plasma concentrations of mesalamine (based on sparse sampling) were 820 to 988 ng/mL at the low dose level (that is, 1.2, 2 or 2.4 grams/day based on body weight strata of 17 to less than 33 kg, 33 to less than 54 kg, and 54 to 90 kg, respectively).
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Mesalamine was not carcinogenic at dietary doses of up to 480 mg/kg/day in rats and 2000 mg/kg/day in mice, which are about 2.9 and 6.1 times the maximum recommended maintenance dose of mesalamine of 1.6 grams per day or 26.7 mg/kg/day, based on 60 kg body weight, respectively, based on body surface area.
Mutagenesis
Mesalamine was negative in the Ames assay for mutagenesis, negative for induction of sister chromatid exchanges (SCE) and chromosomal aberrations in Chinese hamster ovary cells in vitro, and negative for induction of micronuclei (MN) in mouse bone marrow polychromatic erythrocytes.
Impairment of Fertility
Mesalamine, at oral doses up to 480 mg/kg/day (about 1.9 times the recommended human treatment dose on a body surface area basis), was found to have no effect on fertility or reproductive performance of male and female rats.
13.2 Animal Toxicology and/or Pharmacology
In animal studies (rats, mice, dogs), the kidney was the principal organ for toxicity. (In the following, comparisons of animal dosing to recommended human dosing are based on body surface area and a 2.4 grams per day dose for a 60 kg person.)
Mesalamine causes renal papillary necrosis in rats at single doses of approximately 750 mg/kg to 1000 mg/kg (approximately 3 to 4 times the recommended human dose based on body surface area). Doses of 170 and 360 mg/kg/day (about 0.7 and 1.5 times the recommended human dose based on body surface area) given to rats for six months produced papillary necrosis, papillary edema, tubular degeneration, tubular mineralization, and urothelial hyperplasia.
In mice, oral doses of 4000 mg/kg/day mesalamine (approximately 8 times the recommended human dose based on body surface area) for three months produced tubular nephrosis, multifocal/diffuse tubulo-interstitial inflammation, and multifocal/diffuse papillary necrosis.
In dogs, single doses of 6000 mg (approximately 8 times the recommended human dose based on body surface area) of delayed-release mesalamine tablets resulted in renal papillary necrosis but were not fatal. Renal changes have occurred in dogs given chronic administration of mesalamine at doses of 80 mg/kg/day (1.1 times the recommended human dose based on body surface area).
-
14 CLINICAL STUDIES
The safety and efficacy of mesalamine has been established based on adequate and well-controlled studies of mesalamine delayed-release tablets. Below is a description of the results of the adequate and well-controlled studies of mesalamine delayed-release tablets for the treatment of mildly to moderately active ulcerative colitis in adults and pediatric patients 5 to 17 years of age and the maintenance of remission of ulcerative colitis in adults.
14.1 Treatment of Mildly to Moderately Active Ulcerative Colitis
Adults
Two placebo-controlled studies (Studies 1 and 2) have demonstrated the efficacy of mesalamine delayed-release tablets in patients with mildly to moderately active ulcerative colitis.
In one randomized, double-blind, multi-center, placebo-controlled clinical trial of 6 weeks’ duration in 158 patients (Study 1), patients received mesalamine delayed release dosages of 1.6 grams per day (800 mg twice a day; n=53) and 2.4 grams per day (800 mg three times a day; n=53), compared to placebo (n=52). The scoring system for determination of treatment efficacy included assessment of stool frequency, rectal bleeding, sigmoidoscopic findings, patient’s functional assessment, and physician global assessment. At the dosage of 2.4 grams per day, 21 of 43 (49%) patients using mesalamine delayed release tablets showed an improvement in sigmoidoscopic appearance of the bowel compared to 12 of 44 (27%) patients using placebo (p = 0.048). In addition, significantly more patients in the mesalamine delayed release tablets 2.4 grams per day group showed improvement in rectal bleeding and stool frequency. The 1.6 grams per day dosage regimen is not recommended because it did not produce consistent evidence of effectiveness [see Dosage and Administration (2.2)].
In a second randomized, double-blind, placebo-controlled clinical trial of 6 weeks’ duration in 87 patients (Study 2), patients received mesalamine delayed release tablets of 1.6 grams per day (400 mg four times a day; n=11) and 4.8 grams per day (1.2 grams four times a day; n=38), compared to placebo four times a day (n=38). Mesalamine delayed release tablets 4.8 grams per day for 6 weeks resulted in sigmoidoscopic improvement in 28 of 38 (74%) patients compared to 10 of 38 (26%) placebo patients (p less than 0.001). Also, more patients in the mesalamine delayed release tablets 4.8 grams per day group than the placebo group showed improvement in overall symptoms. The 4.8 grams per day dosage regimen is not recommended because greater efficacy was not demonstrated with this dosage compared to the 2.4 grams per day dosage [see Dosage and Administration (2.2)].
Pediatrics
The safety and effectiveness of mesalamine delayed release in pediatric patients 5 to 17 years of age for treatment of mildly to moderately active ulcerative colitis are supported by evidence from adequate and well controlled studies of mesalamine delayed release in adults and a single study in pediatric patients.
A randomized, double-blind, 6-week study of two dosage levels of mesalamine delayed release tablets (Study 3) was conducted in 82 pediatric patients 5 to 17 years of age with mildly or moderately active ulcerative colitis defined as a score of 10 to 55 on the Pediatric Ulcerative Colitis Activity Index (PUCAI) (which includes assessment of abdominal pain, rectal bleeding, stool consistency, number of stools per 24 hours, presence of nocturnal bowel movement and activity level, and has a total maximum score of 85; each of the subscales are scored from 0 to 10 except rectal bleeding which is scored from 0 to 30, and number of stools per 24 hours which is scored from 0 to 15) and rectal bleeding and stool frequency Mayo subscale scores of ≥1 (each of these subscales are scored from zero (normal) to three (most severe).
All patients were divided by weight category (17 to less than 33 kg, 33 to less than 54 kg, and 54 to 90 kg) and randomly assigned to receive a low dosage (1.2, 2, and 2.4 grams per day for the respective weight category) or a high dosage (2, 3.6, and 4.8 grams per day). Doses were administered every 12 hours.
The proportion of patients who achieved success based on the Truncated Mayo Score (TM-Mayo) (based on the stool frequency and rectal bleeding subscores of the Mayo Score) and based on the PUCAI was measured after 6 weeks of treatment. Success based on TM-Mayo was defined as either partial response (improvement from baseline in stool frequency or rectal bleeding subscores with no worsening in the other) or complete response (both stool frequency and rectal bleeding subscores equal 0). Success based on PUCAI was defined as either partial response (PUCAI reduction of greater than or equal to 20 points from Baseline to Week 6 with Week 6 score greater than or equal to 10) or complete response (PUCAI less than 10 at Week 6).
There were 41 patients in the low dosage group and 41 patients in the high dosage group who received at least one dose of mesalamine delayed-release 400 mg tablets; 36 patients in each dosage group completed the study. Patients were considered treatment failures if they did not achieve success or dropped out due to adverse reaction or lack of efficacy.
At Week 6, 73% of the patients in the low dosage group, and 70% of the patients in the high dosage group achieved success based on the TM-Mayo; 34% of the patients in the low dosage group and 43% of the patients in the high dosage group achieved complete response. At Week 6, 56% of the patients in the low dosage group, and 55% of the patients in the high dosage group achieved success based on the PUCAI; 46% of the patients in the low dosage group and 43% of the patients in the high dosage group achieved complete response.
The high dosage regimen is not recommended because it was not more effective than the low dosage regimen [see Dosage and Administration (2.2)].
14.2 Maintenance of Remission of Ulcerative Colitis
Adults
In a randomized, double-blind, multi-center, placebo-controlled clinical trial of 6 months’ duration in 264 patients (Study 4), patients received mesalamine delayed-release tablets of 0.8 grams per day (400 mg twice a day; n = 90) and 1.6 grams per day (400 mg four times a day; n = 87), compared to placebo four times a day (n = 87). The proportion of patients treated with 0.8 grams per day who maintained endoscopic remission was not statistically significant compared to placebo; the 0.8 grams per day dosage regimen is not recommended [see Dosage and Administration (2.3)]. The number of patients using mesalamine delayed-release tablets 1.6 grams per day who maintained endoscopic remission of ulcerative colitis was 61 of 87 (70%) compared with 42 of 87 (48%) of placebo patients (p = 0.005).
A pooled efficacy analysis of 4 maintenance trials compared mesalamine delayed release tablets at dosages of 0.8 to 2.8 grams per day, in divided doses ranging from twice daily to four times per day, with sulfasalazine, at dosages of 2 to 4 grams per day. Treatment success was seen in 59 of 98 (59%) patients using mesalamine delayed release tablets and 70 of 102 (69%) patients using sulfasalazine, a non-significant difference.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Mesalamine delayed-release capsules are available as clear capsules imprinted with “TEVA” and “5907” on both the cap and the body in black ink. Each capsule contains four reddish-brown, film-coated round 100 mg mesalamine tablets.
NDC 0093-5907-86 Bottle of 180 capsules
Store at 20º to 25ºC (68º to 77ºF) [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Administration
- Inform patients that if they are switching from a previous oral mesalamine therapy to mesalamine delayed-release capsules to discontinue their previous oral mesalamine therapy and follow the dosing instructions for mesalamine delayed-release capsules. Inform patients that two mesalamine delayed-release 400 mg capsules cannot be substituted for one mesalamine delayed-release 800 mg tablet.
- Inform patients that mesalamine delayed-release capsules can be taken with or without food.
- Instruct patients to swallow the mesalamine delayed-release capsules whole. Do not cut, break, crush or chew the capsules.
- For patients who are unable to swallow the capsules whole, carefully open the capsules and swallow the contents (four 100 mg tablets).
- Open the number of capsules required to make up a complete dose.
- There are 4 tablets per capsule. Ensure all tablets per capsule are swallowed and no tablets are retained in the mouth.
- Swallow the tablets whole; do not cut, break, crush or chew the tablets.
- Drink an adequate amount of fluids.
- Inform patients that intact, partially intact, and/or tablet shells have been reported in the stool. Instruct patients to contact their healthcare provider if this occurs repeatedly.
- Inform patients that urine may become discolored reddish-brown while taking mesalamine delayed-release capsules when it comes in contact with surfaces or water treated with hypochlorite-containing bleach. If discolored urine is observed, advise patients to observe their urine flow. Report to the healthcare provider only if urine is discolored on leaving the body, before contact with any surface or water (e.g., in the toilet).
- Instruct patients to protect mesalamine delayed-release capsules from moisture. Instruct patients to close the container tightly and to leave any desiccant pouches present in the bottle along with the capsules.
Renal Impairment
- Inform patients that mesalamine delayed-release capsules may decrease their renal function, especially if they have known renal impairment or are taking nephrotoxic drugs, including NSAIDs, and periodic monitoring of renal function will be performed while they are on therapy. Advise patients to complete all blood tests ordered by their healthcare provider [see Warnings and Precautions (5.1), Drug Interactions (7.1)].
Mesalamine-Induced Acute Intolerance Syndrome and Other Hypersensitivity Reactions
- Inform patients of the signs and symptoms of hypersensitivity reactions. Instruct patients to stop taking mesalamine delayed-release capsules and report to their healthcare provider if they experience new or worsening symptoms of Acute Intolerance Syndrome (cramping, abdominal pain, bloody diarrhea, fever, headache, malaise, conjunctivitis and rash) or other symptoms suggestive of mesalamine-induced hypersensitivity [see Warnings and Precautions (5.2, 5.3)].
Hepatic Failure
- Inform patients with known liver disease of the signs and symptoms of worsening liver function and advise them to report to their healthcare provider if they experience such signs or symptoms [see Warnings and Precautions (5.4)].
Severe Cutaneous Adverse Reactions
- Inform patients of the signs and symptoms of severe cutaneous adverse reactions. Instruct patients to stop taking mesalamine delayed-release capsules and report to their healthcare provider at first appearance of a severe cutaneous adverse reaction or other sign of hypersensitivity [see Warnings and Precautions (5.5)].
Photosensitivity
- Advise patients with pre-existing skin conditions to avoid sun exposure, wear protective clothing, and use a broad-spectrum sunscreen when outdoors [see Warnings and Precautions (5.6)].
Nephrolithiasis
- Instruct patients to maintain an adequate fluid intake during treatment in order to minimize the risk of kidney stone formation and to contact their healthcare provider if they experience signs or symptoms of a kidney stone (e.g., severe side or back pain, blood in the urine) [see Warnings and Precautions (5.7)].
Iron Content of Mesalamine Delayed-Release Capsules
- Advise patients to inform their healthcare provider if they take iron-containing supplements [see Warnings and Precaution (5.8)].
Blood Disorders
- Inform elderly patients and those taking azathioprine or 6-mercaptopurine of the risk for blood disorders and the need for periodic monitoring of complete blood cell counts and platelet counts while on therapy. Advise patients to complete all blood tests ordered by their healthcare provider [see Drug Interactions (7.2), Use in Specific Populations (8.5)].
Manufactured In Israel By:
Teva Pharmaceutical Ind. Ltd.
Kfar Saba, 4410202, IsraelManufactured For:
Teva Pharmaceuticals USA, Inc.
Parsippany, NJ 07054Rev. G 4/2024
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
MESALAMINE
mesalamine capsule, delayed releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0093-5907 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MESALAMINE (UNII: 4Q81I59GXC) (MESALAMINE - UNII:4Q81I59GXC) MESALAMINE 400 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) DIBUTYL SEBACATE (UNII: 4W5IH7FLNY) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) FERROSOFERRIC OXIDE (UNII: XM0M87F357) FERRIC OXIDE RED (UNII: 1K09F3G675) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - METHYL METHACRYLATE COPOLYMER (1:2) (UNII: 5KY68S2577) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) POVIDONE K30 (UNII: U725QWY32X) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TALC (UNII: 7SEV7J4R1U) Product Characteristics Color white (clear) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code TEVA;5907 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0093-5907-86 180 in 1 BOTTLE; Type 0: Not a Combination Product 05/09/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207873 05/09/2019 Labeler - Teva Pharmaceuticals USA, Inc. (001627975)