Label: KRINTAFEL- tafenoquine succinate tablet, film coated
- NDC Code(s): 0173-0889-39
- Packager: GlaxoSmithKline LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated August 2, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use KRINTAFEL safely and effectively. See full prescribing information for KRINTAFEL.
KRINTAFEL (tafenoquine) tablets, for oral use
Initial U.S. Approval: 2018INDICATIONS AND USAGE
KRINTAFEL is an antimalarial indicated for the radical cure (prevention of relapse) of Plasmodium vivax malaria in patients aged 16 years and older who are receiving chloroquine therapy for acute P. vivax infection. (1)
Limitations of Use
DOSAGE AND ADMINISTRATION
- •
- All patients must be tested for glucose-6-phosphate dehydrogenase (G6PD) deficiency prior to prescribing KRINTAFEL. (2.1)
- •
- Pregnancy testing is recommended for females of reproductive potential prior to initiating treatment with KRINTAFEL. (2.1)
- •
- The recommended dose of KRINTAFEL in patients aged 16 years and older is a single dose of 300 mg administered as two 150-mg KRINTAFEL tablets taken together. (2.2)
- •
- Coadminister KRINTAFEL on the first or second day of chloroquine therapy for the acute P. vivax malaria. (2.2)
- •
- Administer KRINTAFEL with food. (2.2)
DOSAGE FORMS AND STRENGTHS
Tablets: 150 mg of tafenoquine (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- •
- Hemolytic Anemia: G6PD testing must be performed before prescribing KRINTAFEL due to the risk of hemolytic anemia. Monitor patients for clinical signs or symptoms of hemolysis. (5.1)
- •
- G6PD Deficiency in Pregnancy or Lactation: KRINTAFEL may cause hemolytic anemia when administered to a pregnant woman with a G6PD-deficient fetus. KRINTAFEL is not recommended during pregnancy. A G6PD-deficient infant may be at risk for hemolytic anemia from exposure to KRINTAFEL through breast milk. Check infant’s G6PD status before breastfeeding begins. (5.2, 8.1, 8.2)
- •
- Methemoglobinemia: Asymptomatic elevations in blood methemoglobin have been observed. Initiate appropriate therapy if signs or symptoms of methemoglobinemia occur. (5.3)
- •
- Psychiatric Effects: Serious psychiatric adverse reactions have been observed in patients with a previous history of psychiatric conditions at doses higher than the approved dose. The benefit of treatment with KRINTAFEL must be weighed against the potential risk for psychiatric adverse reactions in patients with a history of psychiatric illness. (5.4)
- •
- Hypersensitivity Reactions: Serious hypersensitivity reactions (e.g., angioedema) have been observed with administration of KRINTAFEL. If hypersensitivity reactions occur, institute appropriate therapy. (5.5)
- •
- Due to the long half-life of KRINTAFEL (15 days), psychiatric effects and hypersensitivity reactions may be delayed in onset and/or duration. (5.4, 5.5, 12.3)
- •
- Risk of P. vivax Malaria Recurrence: Lack of efficacy in reducing P. vivax malaria recurrence in patients treated with KRINTAFEL combined with dihydroartemisinin/piperaquine (not approved artemisinin-containing antimalarial) was seen in a clinical trial. Use with antimalarials other than chloroquine is not recommended. (1, 5.6)
ADVERSE REACTIONS
Common adverse reactions (≥5%) were dizziness, nausea, vomiting, headache, and decreased hemoglobin. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Avoid coadministration with drugs that are substrates of organic cation transporter-2 (OCT2) or multidrug and toxin extrusion (MATE) transporters. (7.1)
USE IN SPECIFIC POPULATIONS
Lactation: Advise women not to breastfeed a G6PD-deficient infant or infant with unknown G6PD status for 3 months after the dose of KRINTAFEL. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Tests to be Performed Prior to Treatment with KRINTAFEL
2.2 Recommended Dosage and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hemolytic Anemia
5.2 G6PD Deficiency in Pregnancy or Lactation
5.3 Methemoglobinemia
5.4 Psychiatric Effects
5.5 Hypersensitivity Reactions
5.6 Risk of P. vivax Malaria Recurrence
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Effect of KRINTAFEL on Organic Cation Transporter-2 (OCT2) and Multidrug and Toxin Extrusion (MATE) Substrates
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
KRINTAFEL is indicated for the radical cure (prevention of relapse) of Plasmodium vivax malaria in patients aged 16 years and older who are receiving chloroquine therapy for acute P. vivax infection [see Dosage and Administration (2.2)].
Limitations of Use
- •
- KRINTAFEL is NOT indicated for the treatment of acute P. vivax malaria.
- •
- Concomitant use of KRINTAFEL with antimalarials other than chloroquine is not recommended because of the risk of recurrence of P. vivax malaria [see Warnings and Precautions (5.6)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Tests to be Performed Prior to Treatment with KRINTAFEL
All patients must be tested for glucose-6-phosphate dehydrogenase (G6PD) deficiency prior to prescribing KRINTAFEL [see Contraindications (4), Warnings and Precautions (5.1)].
Pregnancy testing is recommended for females of reproductive potential prior to initiating treatment with KRINTAFEL [see Use in Specific Populations (8.1, 8.3)].
2.2 Recommended Dosage and Administration
The recommended dose of KRINTAFEL in patients aged 16 years and older is a single dose of 300 mg administered as two 150-mg tablets taken together. Coadminister KRINTAFEL on the first or second day of chloroquine therapy for acute P. vivax malaria [see Clinical Studies (14)].
Administer KRINTAFEL with food to increase systemic absorption [see Clinical Pharmacology (12.3)].
Swallow tablets whole. Do not break, crush, or chew the tablets.
In the event of vomiting within 1 hour after dosing, a repeat dose should be given. Re-dosing should not be attempted more than once.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
KRINTAFEL is contraindicated in:
- •
- Patients with G6PD deficiency or unknown G6PD status due to the risk of hemolytic anemia [see Warnings and Precautions (5.1)].
- •
- Breastfeeding by a lactating woman when the infant is found to be G6PD deficient or if the G6PD status of the infant is unknown [see Use in Specific Populations (8.2)].
- •
- Patients with known hypersensitivity to tafenoquine, other 8-aminoquinolines, or any component of KRINTAFEL [see Warnings and Precautions (5.5)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hemolytic Anemia
Due to the risk of hemolytic anemia in patients with G6PD deficiency, G6PD testing must be performed before prescribing KRINTAFEL [see Dosage and Administration (2.1)]. Due to the limitations of G6PD tests, physicians need to be aware of residual risk of hemolysis and adequate medical support and follow-up to manage hemolytic risk should be available. Treatment with KRINTAFEL is contraindicated in patients with G6PD deficiency or unknown G6PD status [see Contraindications (4)]. Patients were excluded from clinical trials of KRINTAFEL if they had a G6PD enzyme activity level <70% of the site median value for G6PD normal activity [see Clinical Studies (14)]. In clinical trials, declines in hemoglobin levels were reported in some G6PD-normal patients [see Adverse Reactions (6.1)]. Monitor patients for clinical signs or symptoms of hemolysis. Advise patients to seek medical attention if signs of hemolysis occur.
5.2 G6PD Deficiency in Pregnancy or Lactation
Potential Harm to the Fetus
The use of KRINTAFEL during pregnancy may cause hemolytic anemia in a G6PD-deficient fetus. Even if a pregnant woman has normal levels of G6PD, the fetus could be G6PD deficient. Advise females of reproductive potential that treatment with KRINTAFEL during pregnancy is not recommended and to avoid pregnancy or use effective contraception for 3 months after the dose of KRINTAFEL [see Use in Specific Populations (8.1, 8.3)].
Potential Harm to the Breastfeeding Infant
A G6PD-deficient infant may be at risk for hemolytic anemia from exposure to KRINTAFEL through breast milk. Infant G6PD status should be checked before breastfeeding begins. KRINTAFEL is contraindicated in breastfeeding women when the infant is found to be G6PD deficient or the G6PD status of the infant is unknown [see Contraindications (4)]. Advise the woman with a G6PD-deficient infant or if the G6PD status of the infant is unknown not to breastfeed for 3 months after the dose of KRINTAFEL [see Use in Specific Populations (8.2)].
5.3 Methemoglobinemia
Asymptomatic elevations in methemoglobin have been observed in the clinical trials of KRINTAFEL [see Adverse Reactions (6.1)]. Institute appropriate therapy if signs or symptoms of methemoglobinemia occur. Carefully monitor individuals with nicotinamide adenine dinucleotide (NADH)-dependent methemoglobin reductase deficiency. Advise patients to seek medical attention if signs of methemoglobinemia occur.
5.4 Psychiatric Effects
Psychiatric adverse reactions including anxiety (<1%), abnormal dreams (<1%), and insomnia (3%) have been reported in clinical trials of KRINTAFEL [see Adverse Reactions (6.1)]. Two cases of depression and 2 cases of psychosis have occurred primarily in patients with a history of psychiatric disorders following receipt of single doses of tafenoquine that were higher than the approved 300-mg dose (350 mg to 600 mg). Safety and effectiveness of KRINTAFEL have not been established at doses or regimens other than the approved regimen; use of KRINTAFEL at doses or regimens other than a 300-mg single dose is not approved by FDA.
The benefit of treatment with KRINTAFEL must be weighed against the potential risk for psychiatric adverse reactions in patients with a history of psychiatric illness. Due to the long half-life of KRINTAFEL (approximately 15 days), signs or symptoms of psychiatric adverse reactions that may occur could be delayed in onset and/or duration [see Clinical Pharmacology (12.3)].
5.5 Hypersensitivity Reactions
Serious hypersensitivity reactions (e.g., angioedema, urticaria) have been observed with administration of KRINTAFEL [see Adverse Reactions (6.1)]. Institute appropriate therapy if hypersensitivity reactions occur. Do not re-administer KRINTAFEL. KRINTAFEL is contraindicated in patients who develop hypersensitivity to tafenoquine or any component of KRINTAFEL or other 8-aminoquinolines [see Contraindications (4)].
Due to the long half-life of KRINTAFEL (approximately 15 days), signs or symptoms of hypersensitivity adverse reactions that may occur could be delayed in onset and/or duration [see Clinical Pharmacology (12.3)]. Advise patients to seek medical attention if signs of hypersensitivity occur.
5.6 Risk of P. vivax Malaria Recurrence
Lack of efficacy in reducing P. vivax malaria recurrence in patients treated with KRINTAFEL combined with an artemisinin-containing antimalarial was seen in a clinical trial (NCT02802501). In this double-blind, randomized, placebo-controlled trial in which all patients with P. vivax malaria were treated with dihydroartemisinin/piperaquine (not approved artemisinin-containing antimalarial) and were coadministered KRINTAFEL, primaquine, or placebo, lack of efficacy (recurrence rates at 6 months following treatment) was seen in patients treated with KRINTAFEL.
Concomitant administration of KRINTAFEL with antimalarials other than chloroquine is not recommended.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions have been observed with KRINTAFEL and are discussed in detail in the Warnings and Precautions section:
- •
- Hemolytic anemia [see Warnings and Precautions (5.1)]
- •
- Methemoglobinemia [see Warnings and Precautions (5.3)]
- •
- Psychiatric effects [see Warnings and Precautions (5.4)]
- •
- Hypersensitivity reactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described below reflect exposure to 4,129 subjects, of whom 810 received a 300-mg single dose of KRINTAFEL. KRINTAFEL was evaluated in patients with P. vivax malaria (n = 483) in 3 randomized, double-blind trials including a placebo-controlled trial comparing KRINTAFEL plus chloroquine (n = 260) with chloroquine alone (Trial 1), a placebo-controlled dose-ranging trial (Trial 2) (n = 57) [see Clinical Studies (14)], and a hematologic safety trial (Trial 3, NCT02216123) (n = 166).
In Trial 1, in patients with P. vivax malaria, the most common adverse reactions reported in ≥5% of patients treated with KRINTAFEL are listed in Table 1. Patients included in the trial had a mean age of 35 (range: 16 to 79 years), were 75% male and from the following regions: 70% Latin America (Brazil and Peru), 19% Southeast (SE) Asia (Thailand, Cambodia, and the Philippines), and 11% Africa (Ethiopia).
Table 1. Selected Adverse Reactionsa Reported in ≥5% of Patients with P. vivax Malaria Receiving KRINTAFEL in a Randomized, Active-Controlled Trial (Trial 1) a Adverse reactions reported prior to Day 29 as subsequent adverse reactions can be confounded by recurrence of malaria or retreatment with another agent from the quinoline class. Adverse Reaction
Chloroquine
KRINTAFEL
+ Chloroquine
(n = 133)
(n = 260)
%
%
Dizziness
3
8
Nausea
7
6
Vomiting
5
6
Decreased Hemoglobin
2
5
Headache
7
5
Other Adverse Reactions Reported with KRINTAFEL
Clinically significant adverse reactions with KRINTAFEL 300-mg single dose in clinical trials (n = 810) in ≤3% of subjects are listed below:
Psychiatric Disorders: Anxiety, insomnia, abnormal dreams.
Nervous System Disorders: Somnolence.
Laboratory Investigations: Increased blood creatinine, increased blood methemoglobin, increased alanine aminotransferase.
Immune System Disorders: Hypersensitivity reactions (e.g., angioedema, urticaria) [see Contraindications (4), Warnings and Precautions (5.5)].
Eye Disorders: Vortex keratopathy, photophobia.
-
7 DRUG INTERACTIONS
7.1 Effect of KRINTAFEL on Organic Cation Transporter-2 (OCT2) and Multidrug and Toxin Extrusion (MATE) Substrates
The effect of coadministration of tafenoquine on the pharmacokinetics of OCT2 and MATE substrates in humans is unknown. However, in vitro observations suggest the potential for increased concentrations of these substrates [see Clinical Pharmacology (12.3)] which may increase the risk of toxicity of these drugs.
Avoid coadministration of KRINTAFEL with OCT2 and MATE substrates (e.g., dofetilide, metformin). If coadministration cannot be avoided, monitor for drug-related toxicities and consider dosage reduction if needed based on approved product labeling of the coadministered drug.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The use of KRINTAFEL during pregnancy may cause hemolytic anemia in a fetus who is G6PD deficient. Treatment with KRINTAFEL during pregnancy is not recommended [see Warnings and Precautions (5.2)]. Available data with use of KRINTAFEL in pregnant women are insufficient to establish a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. In animal studies, there were increased abortions, with and without maternal toxicity, when KRINTAFEL was given orally to pregnant rabbits at and above doses equivalent to about 0.4 times the clinical exposure based on body surface area comparisons. No fetotoxicity was observed at doses equivalent to the clinical exposure (based on body surface area comparisons) in a similar study in rats.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk: Malaria during pregnancy increases the risk for adverse pregnancy outcomes, including maternal anemia, prematurity, spontaneous abortion, and stillbirth.
Data
Animal Data: Tafenoquine resulted in dose-related abortions when given orally to pregnant rabbits during organogenesis (Gestation Days 6 to 18) at doses of 7 mg/kg (about 0.4 times the clinical exposure based on body surface area comparisons) and above. Doses higher than 7 mg/kg were also associated with maternal toxicity (mortality and reduced body weight gain). In a similar study in rats, doses of 3, 10, or 30 mg/kg/day resulted in maternal toxicity (enlarged spleen, reduced body weight, and reduced food intake) but no fetotoxicity at the high dose (equivalent to the clinical exposure based on body surface area comparisons). There was no evidence of malformations in either species. In a pre- and postnatal development study in rats, tafenoquine administered throughout pregnancy and lactation produced maternal toxicity and a reversible decrease in offspring body weight gain and decrease in motor activity at 18 mg/kg/day, which is equivalent to about 0.6 times the clinical dose based on body surface area comparisons.
8.2 Lactation
Risk Summary
A breastfed infant with G6PD deficiency is at risk for hemolytic anemia from exposure to KRINTAFEL. Infant G6PD status should be checked before breastfeeding begins. KRINTAFEL is contraindicated in breastfeeding women when the infant is found to be G6PD deficient or the G6PD status of the infant is unknown [see Contraindications (4), Clinical Considerations].
There is no information regarding the presence of KRINTAFEL in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. In a breastfed infant with normal G6PD, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for KRINTAFEL and any potential effects on the breastfed infant from KRINTAFEL or from the underlying maternal condition.
Clinical Considerations
Check the infant’s G6PD status before maternal breastfeeding commences. If an infant is G6PD deficient, exposure to KRINTAFEL during breastfeeding may result in hemolytic anemia in the infant; therefore, advise the woman with an infant who has G6PD deficiency or whose G6PD status is unknown not to breastfeed for 3 months after the dose of KRINTAFEL.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status in females of reproductive potential prior to initiating treatment with KRINTAFEL [see Warnings and Precautions (5.2), Use in Specific Populations (8.1)].
Contraception
KRINTAFEL may cause hemolytic anemia in a G6PD-deficient fetus [see Warnings and Precautions (5.2), Use in Specific Populations (8.1)]. Advise females of reproductive potential that treatment with KRINTAFEL during pregnancy is not recommended and to avoid pregnancy or use effective contraception for 3 months after the dose of KRINTAFEL.
8.4 Pediatric Use
The safety and effectiveness of KRINTAFEL have been established in pediatric patients aged 16 years and older. Use of KRINTAFEL in these pediatric patients is supported by evidence from adequate and well-controlled studies of KRINTAFEL [see Clinical Studies (14)].
Safety and effectiveness of KRINTAFEL in pediatric patients younger than 16 years have not been established.
8.5 Geriatric Use
Clinical trials of KRINTAFEL did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
KRINTAFEL contains tafenoquine succinate, an antimalarial agent for oral administration. The chemical name of tafenoquine succinate is (±) 8-[(4-amino-1-methylbutyl)amino]-2,6-dimethoxy-4‑methyl-5-[3-(trifluoromethyl)phenoxy]quinoline succinate. The molecular formula of tafenoquine succinate is C24H28F3N3O3•C4H6O4, and its molecular mass is 581.6 as the succinate salt (463.5 as free base). The structural formula is shown below.
Each KRINTAFEL tablet contains 150 mg of tafenoquine (equivalent to 188.2 mg tafenoquine succinate). Inactive ingredients include magnesium stearate, mannitol, and microcrystalline cellulose. The tablet film-coating inactive ingredients include hydroxypropylmethylcellulose, polyethylene glycol, red iron oxide, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tafenoquine is an 8-aminoquinoline antimalarial drug [see Microbiology (12.4)].
12.2 Pharmacodynamics
Cardiac Electrophysiology
The effect of tafenoquine on the QTc interval was evaluated in a Phase 1 randomized, single-blind, placebo- and positive-controlled, parallel-group thorough QTc study in 260 healthy adult subjects. At a cumulative dose of 1,200 mg (400 mg/day for 3 days; 4 times the maximum recommended dose), tafenoquine did not prolong the QTc interval to any clinically relevant extent.
Exposure-Response Relationships
A saturable relationship between tafenoquine exposure (AUC) and clinical response (recurrence-free rate at 6 months) was identified. Tafenoquine exposures achieved with doses of 300 mg and higher are on the plateau of the exposure-response curve. Use of KRINTAFEL at doses or regimens other than a 300-mg single dose is not approved by the FDA.
12.3 Pharmacokinetics
Absorption
Maximum plasma concentrations were generally observed 12 to 15 hours following oral administration.
Food Effect: Plasma tafenoquine AUC increased by 41% and Cmax increased by 31% when administered as an investigational capsule formulation with a high-calorie, high-fat meal (approximately 1,000 calories with 15% protein, 25% carbohydrate, and 60% fat) compared with the fasted state.
Distribution
Protein binding of tafenoquine is >99.5%. The apparent oral volume of distribution is ~1,600 L. Following single- and multiple-oral-dose administration, tafenoquine whole blood concentrations were on average 67% higher than corresponding plasma values.
Elimination
The apparent oral clearance of tafenoquine is approximately 3 L/h. The average terminal half-life is approximately 15 days.
Metabolism: Tafenoquine undergoes slow metabolism. Unchanged tafenoquine represented the only notable drug-related component in human plasma after a single oral dose of tafenoquine.
Excretion: The full excretion profile of tafenoquine in humans is unknown. Over a 6-day collection period, renal elimination of unchanged tafenoquine was low.
Specific Populations
Pharmacokinetics of tafenoquine were not significantly impacted by age, sex, ethnicity, and body weight. The effect of renal or hepatic impairment on tafenoquine pharmacokinetics is unknown.
Drug Interaction Studies
Clinical Studies: No clinically significant effects on tafenoquine pharmacokinetics were observed following coadministration with chloroquine, dihydroartemisinin-piperaquine, or artemether-lumefantrine in healthy subjects.
No clinically significant effects on the pharmacokinetics of dihydroartemisinin, piperaquine, artemether, lumefantrine, or substrates of cytochrome P450 isoenzymes (CYP)1A2 (caffeine), CYP2D6 (desipramine), CYP2C8 (chloroquine), CYP2C9 (flurbiprofen), or CYP3A4 (midazolam, chloroquine) were observed following coadministration of tafenoquine in healthy subjects.
In Vitro Studies Where Drug Interaction Potential Was Not Further Evaluated Clinically: Tafenoquine inhibited metformin transport via human OCT2, MATE-1, and MATE2-K transporters. Clinical drug interaction studies with tafenoquine and OCT2 and MATE substrates have not been conducted [see Drug Interactions (7)].
The effect of tafenoquine on substrates of P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and organic anion transporting polypeptides 1B1/1B3 (OATP1B1/OATP1B3) is unknown.
12.4 Microbiology
Mechanism of Action
Tafenoquine, an 8-aminoquinoline antimalarial, is active against the liver stages including the hypnozoite (dormant stage) of P. vivax. In addition to its effect on the parasite, tafenoquine causes red blood cell shrinkage in vitro. The molecular target of tafenoquine is not known.
Antimicrobial Activity
Tafenoquine is active against pre-erythrocytic (liver) and erythrocytic (asexual) forms as well as gametocytes of P. vivax. The activity of tafenoquine against the pre-erythrocytic liver stages of the parasite prevents the development of the erythrocytic forms of the parasite, which are responsible for relapses in P. vivax malaria [see Clinical Studies (14)].
Resistance
A potential for development of resistance of Plasmodium species to tafenoquine was not evaluated.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year oral carcinogenicity studies were conducted in rats and mice. Renal cell adenomas and carcinomas were increased in male rats at doses of 1 mg/kg/day and above (3 times the clinical exposure based on AUC comparisons). Tafenoquine was not carcinogenic in mice. Given the single-dose administration of KRINTAFEL, these findings may not represent a carcinogenicity risk to humans.
Mutagenesis
Tafenoquine did not cause mutations or chromosomal damage in 2 definitive in vitro tests (bacterial mutation assay and mouse lymphoma L5178Y cell assay) or in an in vivo oral rat micronucleus test.
Impairment of Fertility
In a rat fertility study, tafenoquine was given orally at 1.5, 5, and 15 mg/kg/day (up to about 0.5 times the human dose based on body surface area comparisons) to males for at least 67 days, including 29 days prior to mating, and to females from 15 days prior to mating through early pregnancy. Tafenoquine resulted in reduced number of viable fetuses, implantation sites, and corpora lutea at 15 mg/kg in the presence of maternal toxicity (mortality, piloerection, rough coat, and reduced body weight).
-
14 CLINICAL STUDIES
Trial 1 (NCT01376167) was a double-blind, controlled clinical trial of 522 adults positive for P. vivax across 3 regions (Asia, Africa, and Latin America). All patients received chloroquine phosphate (600-mg free base on Days 1 and 2 with 300-mg free base on Day 3) to treat the acute infection in addition to either a one-time dose of KRINTAFEL (two 150-mg tablets) on Day 1 or Day 2 (n = 260), an active control (n = 129), or placebo (n = 133) in a 2:1:1 fashion. Patients included in the trial had a mean age of 35 (range: 16 to 79 years), were 75% male and from the following regions: 70% Latin America (Brazil and Peru), 19% SE Asia (Thailand, Cambodia, and the Philippines), and 11% Africa (Ethiopia).
Patients were considered recurrence-free at 6 months if they demonstrated initial parasite clearance, took no antimalarial medications, and were confirmed parasite-free at the 6-month final assessment (i.e., absence of relapse or new infection).
Due to the risk of hemolytic anemia, patients were excluded from the trial if they had a G6PD enzyme activity level <70% of the site median value for G6PD normals (8.2 IU/gHb). In this trial, the minimum G6PD enzyme level of any subject was 5.4 IU/gHb. Patients with severe malaria were excluded from the trial.
The recurrence-free efficacy rates at 6 months among the groups receiving KRINTAFEL and placebo are presented in Table 2. The risk of recurrence for KRINTAFEL plus chloroquine was reduced by 76% compared with placebo plus chloroquine.
Table 2. Recurrence-Free Efficacy Rates of KRINTAFEL in Patients with P. vivax at 6 Months – Trial 1a a All randomized patients were treated and had a positive parasite smear for P. vivax at baseline.
b Odds ratio of the risk of recurrence of KRINTAFEL plus chloroquine versus placebo plus chloroquine using logistic regression model with treatment and region as covariates. Subjects who did not demonstrate initial clearance, took a concomitant medication with antimalarial activity, or who had a missing Day 180 assessment were considered ‘missing/indeterminate’ and were counted as recurrences in the analysis.KRINTAFEL/
Placebo/
Chloroquine
Chloroquine
(n = 260)
(n = 133)
Recurrence-free efficacy
155 (60%)
35 (26%)
Recurrence
85 (33%)
88 (66%)
Missing/indeterminate outcome
20 (8%)
10 (8%)
ORb (95% CI)
0.24 (0.15, 0.38)
P value
<0.001
In Trial 2 (NCT01376167), a dose-ranging trial with a study design similar to Trial 1, 57 and 54 subjects were randomized to KRINTAFEL 300-mg single dose plus chloroquine (same dose as in Trial 1) and placebo plus chloroquine groups, respectively. KRINTAFEL plus chloroquine demonstrated a statistically significantly higher rate of recurrence-free efficacy at 6 months compared with the placebo plus chloroquine control group (84% versus 39%, with a difference of 45% and 95% CI [29%, 61%]).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
KRINTAFEL tablets contain 150 mg of tafenoquine (equivalent to 188.2 mg tafenoquine succinate) and are pink, film‑coated, capsule-shaped, and debossed with ‘GS J11’ on one side. KRINTAFEL is supplied as follows:
- •
- Unit Dose Pack of 2 tablets in a bottle with child-resistant closure (NDC 0173-0889-39). Bottles contain a desiccant.
Storage
Store at 20°C to 25°C (68°F to 77°F). Temperature excursions are permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Store in the original package to protect from moisture. Keep the bottle tightly closed and do not remove the desiccant.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
G6PD Testing and Hemolytic Anemia
Inform patients of the need for testing for G6PD deficiency before starting KRINTAFEL. Advise patients of the symptoms of hemolytic anemia and instruct them to seek medical advice promptly if such symptoms occur. Patients should contact their healthcare provider if they develop dark lips or urine as these may be signs of hemolysis or methemoglobinemia [see Warnings and Precautions (5.1)].
Important Administration Instructions
Advise patients to take KRINTAFEL with food to increase absorption [see Dosage and Administration (2)].
Advise patients to swallow the tablet whole and not to break, crush, or chew it.
Potential Harm to the Fetus
Advise females of reproductive potential of the potential risk of KRINTAFEL to a fetus and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.2), Use in Specific Populations 8.1)].
Advise females of reproductive potential to avoid pregnancy or use effective contraception for 3 months after the dose of KRINTAFEL [see Use in Specific Populations (8.3)].
Lactation
Advise women with a G6PD-deficient infant, or if they do not know the G6PD status of their infant, not to breastfeed for 3 months after the dose of KRINTAFEL [see Contraindications (4), Warnings and Precautions (5.2), Use in Specific Populations (8.2)].
Methemoglobinemia
Inform patients that methemoglobinemia has occurred with KRINTAFEL. Advise patients of the symptoms of methemoglobinemia and instruct them to seek medical advice promptly if such symptoms occur [see Warnings and Precautions (5.3)].
Psychiatric Symptoms
Advise patients with a history of psychiatric illness regarding the potential for new or worsening psychiatric symptoms with KRINTAFEL and instruct them to seek medical advice promptly if such symptoms occur [see Warnings and Precautions (5.4)].
Hypersensitivity Reactions
Inform patients that hypersensitivity reactions have occurred with KRINTAFEL. Advise patients of the symptoms of hypersensitivity reactions and instruct them to seek medical advice promptly if such symptoms occur [see Warnings and Precautions (5.5)].
Trademarks are owned by or licensed to the GSK group of companies.
GlaxoSmithKline
Durham, NC 27701
©2023 GSK group of companies or its licensor.
KFL:4PI
-
PATIENT PACKAGE INSERT
- _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
PHARMACIST—DETACH HERE AND GIVE PATIENT INFORMATION TO PATIENT
- _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
PATIENT INFORMATION
KRINTAFEL (KRIN-TAH-FELL)
(tafenoquine)
tablets, for oral useWhat is KRINTAFEL?
- •
- KRINTAFEL is a prescription medicine used to treat malaria caused by a parasite called Plasmodium vivax in patients aged 16 years and older who are also receiving chloroquine to treat acute Plasmodium vivax malaria.
- •
- Malaria is a serious disease of the blood that is spread by infected mosquitos. KRINTAFEL does not work for all types of malaria.
- •
- It is not known if KRINTAFEL is safe and effective in children younger than 16 years.
Do not use KRINTAFEL if you:
- •
- have a blood problem called glucose-6-phosphate dehydrogenase (G6PD) deficiency (sometimes known as favism) or you have not been tested for G6PD deficiency. KRINTAFEL can cause a breakdown of red blood cells (hemolysis) in people with G6PD deficiency. Your healthcare provider will test you for G6PD deficiency before you start taking KRINTAFEL.
- •
- are breastfeeding a child known to have G6PD deficiency or breastfeeding a child that has not been tested for G6PD deficiency.
- •
- are allergic to tafenoquine or any of the ingredients in KRINTAFEL or if you have had an allergic reaction to similar medicines containing 8-aminoquinolines. See the end of this Patient Information leaflet for a complete list of ingredients in KRINTAFEL.
Before taking KRINTAFEL, tell your healthcare provider about all of your medical conditions, including if you:
- •
- have or have had mental health problems.
- •
- are pregnant or plan to become pregnant. KRINTAFEL can harm an unborn baby who has G6PD deficiency.
- •
- are breastfeeding or plan to breastfeed. It is not known if KRINTAFEL passes into breast milk.
- •
- See “Do not use KRINTAFEL if you:”
- •
- Your healthcare provider should check your child for G6PD deficiency before you start breastfeeding.
- •
- If you know your child has G6PD deficiency, do not breastfeed while taking KRINTAFEL and for 3 months after your last dose of KRINTAFEL.
- •
- Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. KRINTAFEL and other medicines may affect each other causing side effects.
How should I take KRINTAFEL?
- •
- Your healthcare provider will test you for G6PD deficiency before you start taking KRINTAFEL.
- •
- KRINTAFEL is given as 2 tablets that you take together as a single dose.
- •
- You will take KRINTAFEL on the first or second day of your treatment with chloroquine.
- •
- Take KRINTAFEL with food to make sure the right amount of medicine is absorbed into your body.
- •
- Swallow KRINTAFEL tablets whole. Do not break, crush, or chew the tablets.
- •
- If you vomit within 1 hour of taking KRINTAFEL, call your healthcare provider as you may need to take a second dose of KRINTAFEL.
What are the possible side effects of KRINTAFEL?
KRINTAFEL can cause serious side effects, including:
- •
- Breakdown of red blood cells (hemolytic anemia). Contact your healthcare provider if you develop signs of hemolytic anemia, which include darkening of the lips or urine, dizziness, confusion, feeling tired, light-headedness, or shortness of breath.
- •
- Hemolytic anemia in an unborn baby who has G6PD deficiency.
- •
- Females who are able to become pregnant should avoid pregnancy or use effective birth control (contraception) for 3 months after the dose of KRINTAFEL. Talk with your healthcare provider about birth control methods that might be right for you.
- •
- Your healthcare provider will do a pregnancy test before you start taking KRINTAFEL. Tell your healthcare provider right away if you become pregnant or think you might be pregnant during treatment with KRINTAFEL.
- •
- Decrease of oxygen in your blood caused by a certain type of abnormal red blood cell (methemoglobinemia). Get medical help right away if you have darkening of the urine, nail beds, lips, or the inside of your mouth.
- •
- Allergic (hypersensitivity) reactions. Serious allergic reactions can happen after you take KRINTAFEL. Allergic reactions can sometimes happen hours or days after you take a dose of KRINTAFEL. Tell your healthcare provider or get emergency help right away if you have any signs or symptoms of an allergic reaction including:
- •
- swelling of your face, lips, tongue, or throat
- •
- itching
- •
- trouble breathing
- •
- fainting, dizziness, feeling lightheaded
- •
- rash
- •
- hives
Other side effects of KRINTAFEL include mental health (psychiatric) symptoms. KRINTAFEL can cause new psychiatric symptoms including anxiety, abnormal dreams, and trouble sleeping (insomnia), or make the symptoms you already have worse. Contact your healthcare provider right away if you have new or worsening psychiatric symptoms.
The most common side effects of KRINTAFEL include: dizziness, nausea, vomiting, headache, and changes in laboratory tests for hemoglobin.
These are not all the possible side effects of KRINTAFEL.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Keep KRINTAFEL and all medicines out of the reach of children.
General information about the safe and effective use of KRINTAFEL.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet.
Do not use KRINTAFEL for a condition for which it was not prescribed. Do not give KRINTAFEL to other people even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about KRINTAFEL that is written for health professionals.
What are the ingredients in KRINTAFEL?
Active Ingredient: tafenoquine succinate.
Inactive Ingredients: magnesium stearate, mannitol, and microcrystalline cellulose.
GlaxoSmithKline, Durham, NC 27701
Trademarks are owned by or licensed to the GSK group of companies.
©2023 GSK group of companies or its licensor.
KFL:3PIL
For more information, call GlaxoSmithKline (GSK) at 1-888-825-5249.
This Patient Information has been approved by the U.S. Food and Drug Administration. Approved: August 2023
-
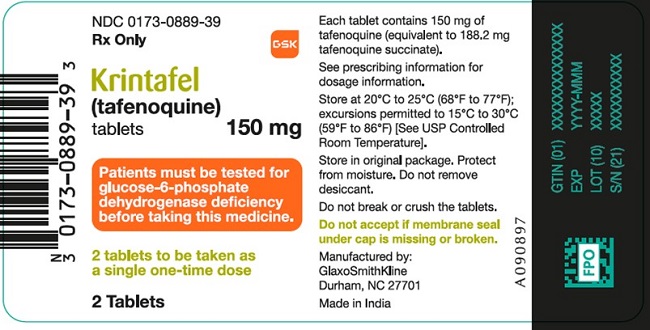
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC 0173-0889-39
Krintafel
(tafenoquine)
tablets
150 mg
Rx Only
Patients must be tested for glucose-6-phosphate dehydrogenase deficiency before taking this medicine.
2 tablets to be taken as a single one-time dose
2 Tablets
GSK
Each tablet contains 150 mg of tafenoquine (equivalent to 188.2 mg tafenoquine succinate).
See prescribing information for dosage information.
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [See USP controlled Room Temperature].
Store in original package. Protect from moisture. Do not remove desiccant.
Do not break or crush the tablets.
Do not accept if membrane seal under cap is missing or broken.
Manufactured by:
GlaxoSmithKline
Durham, NC 27701
Made in India
62000000090897
-
INGREDIENTS AND APPEARANCE
KRINTAFEL
tafenoquine succinate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0173-0889 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TAFENOQUINE SUCCINATE (UNII: DL5J0B8VSS) (TAFENOQUINE - UNII:262P8GS9L9) TAFENOQUINE 150 mg Inactive Ingredients Ingredient Name Strength MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color PINK Score no score Shape CAPSULE Size 17mm Flavor Imprint Code GS;J11 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0173-0889-39 2 in 1 BOTTLE; Type 0: Not a Combination Product 01/22/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA210795 01/22/2019 Labeler - GlaxoSmithKline LLC (167380711)