14.1 Chronic Idiopathic Constipation in Adults
- Two double-blinded, placebo-controlled studies of identical design were conducted in patients with CIC. CIC was defined as, on average, less than ...
14.1 Chronic Idiopathic Constipation in Adults
Two double-blinded, placebo-controlled studies of identical design were conducted in patients with CIC. CIC was defined as, on average, less than 3 SBMs per week (a SBM is a bowel movement occurring in the absence of laxative use) along with one or more of the following symptoms of constipation for at least 6 months prior to randomization: 1) very hard stools for at least a quarter of all bowel movements; 2) sensation of incomplete evacuation following at least a quarter of all bowel movements; and 3) straining with defecation at least a quarter of the time.
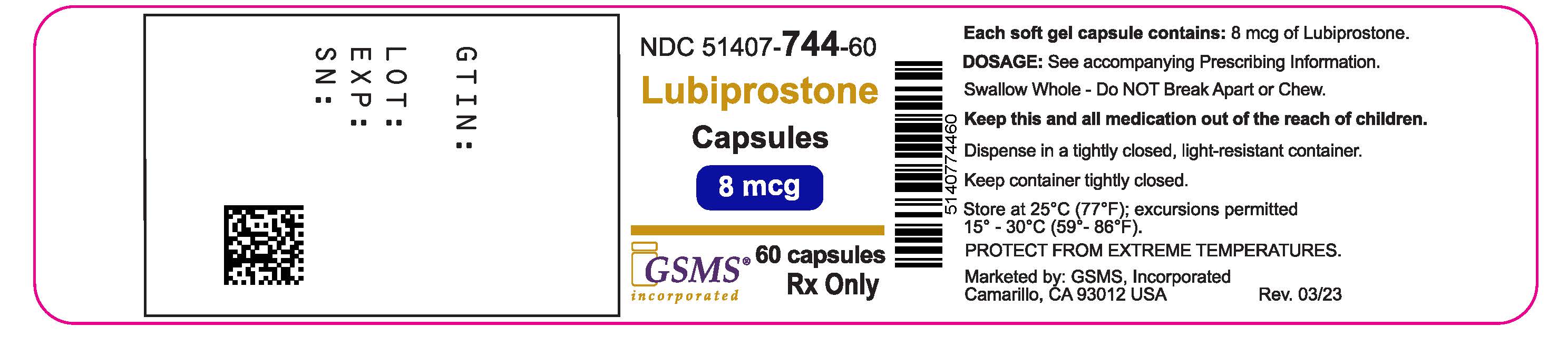
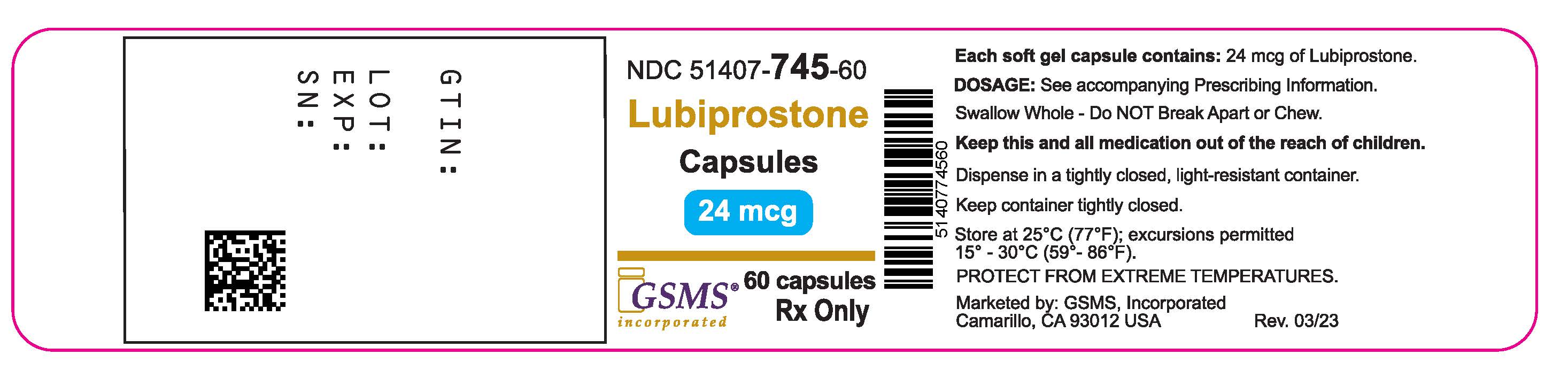
Following a 2-week baseline/washout period, a total of 479 patients (mean age 47 [range 20 to 81] years; 89% female; 81% Caucasian, 10% African American, 7% Hispanic, 2% Asian, 11% at least 65 years of age) were randomized and received lubiprostone 24 mcg twice daily or placebo twice daily for 4 weeks. The primary endpoint of the studies was SBM frequency. The studies demonstrated that patients treated with lubiprostone had a higher frequency of SBMs during Week 1 than the placebo patients. In both studies, results similar to those in Week 1 were also observed in Weeks 2, 3, and 4 of therapy (Table 6).
In both studies, lubiprostone demonstrated increases in the percentage of patients who experienced SBMs within the first 24 hours after administration when compared to placebo (57% vs. 37% in Study 1 and 63% vs. 32% in Study 2, respectively). Similarly, the time to first SBM was shorter for patients receiving lubiprostone than for those receiving placebo.
Signs and symptoms related to constipation, including abdominal bloating, abdominal discomfort, stool consistency, and straining, as well as constipation severity ratings, were also improved with lubiprostone versus placebo. The results were consistent in subpopulation analyses for gender, race, and elderly patients at least 65 years of age.
During a 7-week randomized withdrawal study, patients who received lubiprostone during a 4-week treatment period were then randomized to receive either placebo or to continue treatment with lubiprostone. Inlubiprostone-treated patients randomized to placebo, SBM frequency rates returned toward baseline within 1 week and did not result in worsening compared to baseline. Patients who continued on lubiprostone maintained their response to therapy over the additional 3 weeks of treatment.
14.2 Opioid-Induced Constipation in Adults with Chronic Non-Cancer Pain
The efficacy of lubiprostone in the treatment of OIC in patients receiving opioid therapy for chronic, non-cancer-related pain was assessed in three randomized, double-blinded, placebo-controlled studies. In Study 1, the median age was 52 years (range 20 to 82) and 63% were female. In Study 2, the median age was 50 years (range 21 to 77) and 64% were female. In Study 3, the median age was 50 years (range 21 to 89) and 60% were female. Patients had been receiving stable opioid therapy for at least 30 days prior to screening, which was to continue throughout the 12-week treatment period. At baseline, mean oral morphine equivalent daily doses (MEDDs) were 99 mg and 130 mg for placebo-treated and lubiprostone-treated patients, respectively, in Study 1. Baseline mean MEDDs were 237 mg and 265 mg for placebo-treated and lubiprostone-treated patients, respectively, in Study 2. In Study 3, baseline mean MEDDs were 330 mg and 373 mg for placebo-treated and lubiprostone-treated patients, respectively. The Brief Pain Inventory-Short Form (BPI-SF) questionnaire was administered to patients at baseline and monthly during the treatment period to assess pain control. Patients had documented opioid-induced constipation at baseline, defined as having less than 3 spontaneous bowel movements (SBMs) per week, with at least 25% of SBMs associated with one or more of the following conditions: (1) hard to very hard stool consistency; (2) moderate to very severe straining; and/or (3) having a sensation of incomplete evacuation. Laxative use was discontinued at the beginning of the screening period and throughout the study. With the exception of the 48-hour period prior to first dose and for at least 72 hours (Study 1) or 1 week (Study 2 and Study 3) following first dose, use of rescue medication was allowed in cases where no bowel movement had occurred in a 3-day period. Median weekly SBM frequencies at baseline were 1.5 for placebo patients and 1.0 for lubiprostone patients in Study 1 and, for both Study 2 and Study 3, median weekly SBM frequencies at baseline were 1.5 for both treatment groups.
In Study 1, patients receiving non-diphenylheptane (e.g., non-methadone) opioids (n = 431) were randomized to receive placebo (n = 217) or lubiprostone 24 mcg twice daily (n = 214) for 12 weeks. The primary efficacy analysis was a comparison of the proportion of "overall responders" in each treatment arm. A patient was considered an "overall responder" if ≥1 SBM improvement over baseline were reported for all treatment weeks for which data were available
and≥3 SBMs/week were reported for at least 9 of 12 treatment weeks. The proportion of patients in Study 1 qualifying as an "overall responder" was 27.1% in the group receiving lubiprostone 24 mcg twice daily compared to 18.9% of patients receiving placebo twice daily (treatment difference = 8.2%; p-value = 0.03). Examination of gender and race subgroups did not identify differences in response to lubiprostone among these subgroups. There were too few elderly patients (≥ 65 years of age) to adequately assess differences in effects in that population.
In Study 2, patients receiving opioids (N = 418) were randomized to receive placebo (n = 208) or lubiprostone 24 mcg twice daily (n = 210) for 12 weeks. Study 2 did not exclude patients receiving diphenylheptane opioids (e.g., methadone). The primary efficacy endpoint was the mean change from baseline in SBM frequency at Week 8; 3.3 vs. 2.4 for lubiprostone and placebo-treated patients, respectively; treatment difference = 0.9; p-value = 0.004. The proportion of patients in Study 2 qualifying as an "overall responder," as prespecified in Study 1, was 24% in the group receiving lubiprostone compared to 15% of patients receiving placebo. In the subgroup of patients in Study 2 taking diphenylheptane opioids (baseline mean [median] MEDDs of 691 [403] mg and 672 [450] mg for placebo and lubiprostone patients, respectively), the proportion of patients qualifying as an "overall responder" was 20.5% (8/39) in the group receiving lubiprostone compared to 6.3% (2/32) of patients receiving placebo. Examination of gender and race subgroups did not identify differences in response to lubiprostone among these subgroups. There were too few elderly patients (≥ 65 years of age) to adequately assess differences in effects in that population.
In Study 3, patients receiving opioids (N = 451) were randomized to placebo (n = 216) or lubiprostone 24 mcg twice daily (n = 235) for 12 weeks. Study 3 did not exclude patients receiving diphenylheptane opioids (e.g., methadone). The primary efficacy endpoint was the change from baseline in SBM frequency at Week 8. The study did not demonstrate a statistically significant improvement in SBM frequency rates at Week 8 (mean change from baseline of 2.7 vs. 2.5 for lubiprostone and placebo-treated patients, respectively; treatment difference = 0.2; p-value = 0.76). The proportion of patients in Study 3 qualifying as an "overall responder," as prespecified in Study 1, was 15% in the patients receiving lubiprostone compared to 13% of patients receiving placebo. In the subgroup of patients in Study 3 taking diphenylheptane opioids (baseline mean [median] MEDDs of 730 [518] mg and 992 [480] mg for placebo and lubiprostone patients, respectively), the proportion of patients qualifying as an "overall responder" was 2% (1/47) in the group receiving lubiprostone compared to 12% (5/41) of patients receiving placebo.
14.3 Irritable Bowel Syndrome with Constipation
Two double-blinded, placebo-controlled studies of similar design were conducted in adult patients with IBS-C. IBS was defined as abdominal pain or discomfort occurring over at least 6 months with two or more of the following: 1) relieved with defecation; 2) onset associated with a change in stool frequency; and 3) onset associated with a change in stool form. Patients were sub-typed as having IBS-C if they also experienced two of three of the following: 1) <3 spontaneous bowel movements (SBMs) per week, 2) >25% hard stools, and 3) >25% SBMs associated with straining.
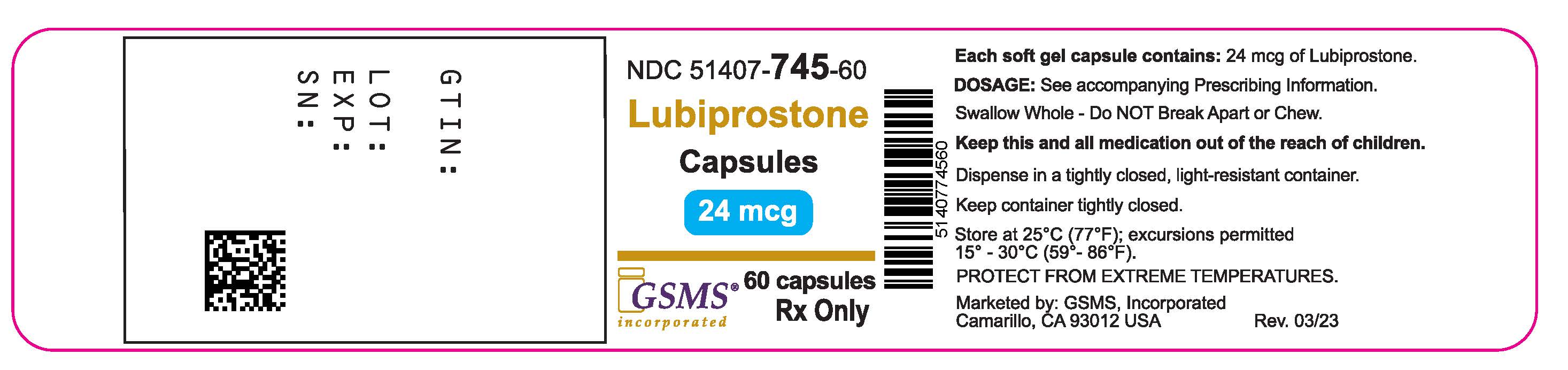
Following a 4-week baseline/washout period, a total of 1154 patients (mean age 47 [range 18 to 85] years; 92% female; 77% Caucasian, 13% African American, 9% Hispanic, 0.4% Asian; 8% at least 65 years of age) were randomized and received lubiprostone 8 mcg twice daily (16 mcg/day) or placebo twice daily for 12 weeks. The primary efficacy endpoint was assessed weekly utilizing the patient's response to a global symptom relief question based on a 7-point, balanced scale ("significantly worse" to "significantly relieved"): "How would you rate your relief of IBS symptoms (abdominal discomfort/pain, bowel habits, and other IBS symptoms) over the past week compared to how you felt before you entered the study?"
The primary efficacy analysis was a comparison of the proportion of "overall responders" in each arm. A patient was considered an "overall responder" if the criteria for being designated a "monthly responder" were met in at least 2 of the 3 months on study. A "monthly responder" was defined as a patient who had reported "significantly relieved" for at least 2 weeks of the month or at least "moderately relieved" in all 4 weeks of that month. During each monthly evaluation period, patients reporting "moderately worse" or "significantly worse" relief, an increase in rescue medication use, or those who discontinued due to lack of efficacy, were deemed non-responders.
The percentage of patients in Study 1 qualifying as an "overall responder" was 14% in the group receiving lubiprostone 8 mcg twice daily compared to 8% of patients receiving placebo twice daily. In Study 2, 12% of patients in the lubiprostone 8 mcg group were "overall responders" versus 6% of patients in the placebo group. In both studies, the treatment differences between the placebo and lubiprostone groups were statistically significant.
Results in men:The two randomized, placebo-controlled, double-blinded studies comprised 97 (8%) male patients, which is insufficient to determine whether men with IBS-C respond differently to lubiprostone from women.
During a 4-week randomized withdrawal period following Study 1, patients who received lubiprostone during the 12-week treatment period were re-randomized to receive either placebo or to continue treatment with lubiprostone. In lubiprostone-treated patients who were "overall responders" during Study 1 and who were re-randomized to placebo, SBM frequency rates did not result in worsening compared to baseline.
Close