6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
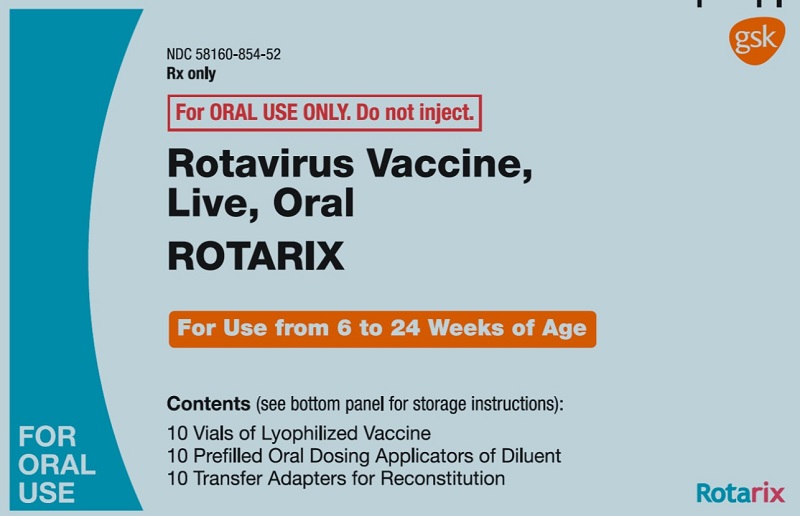
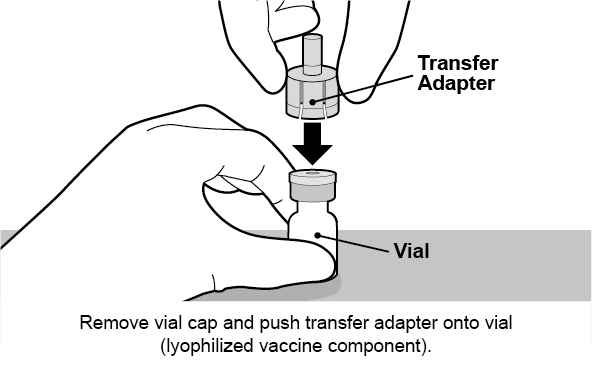
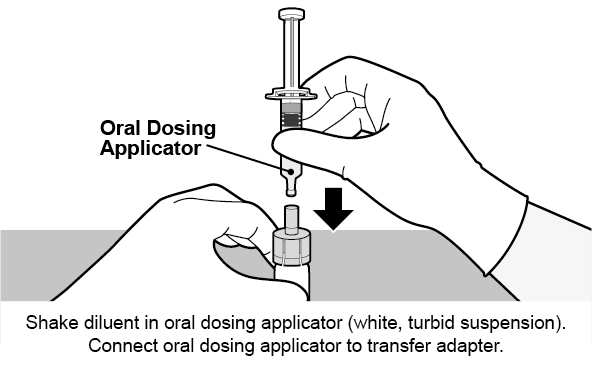
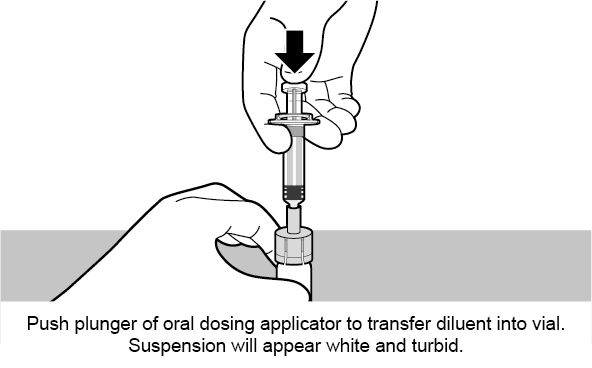
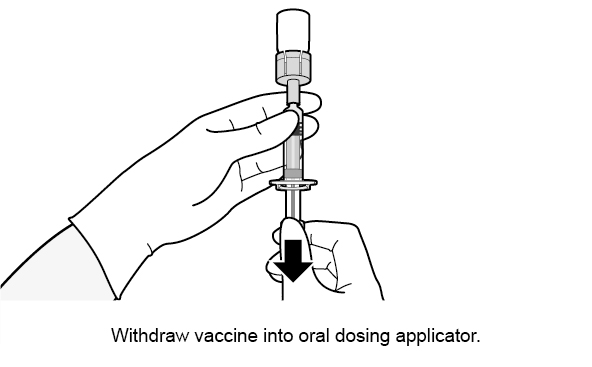
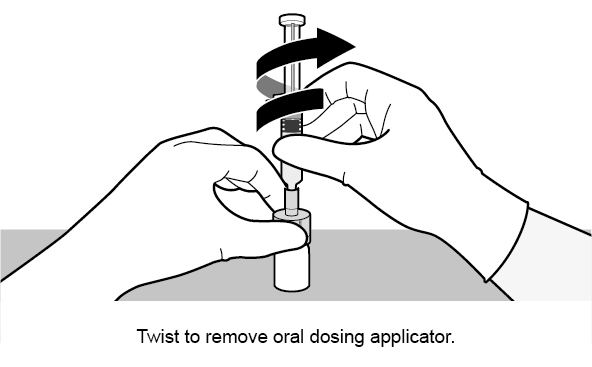
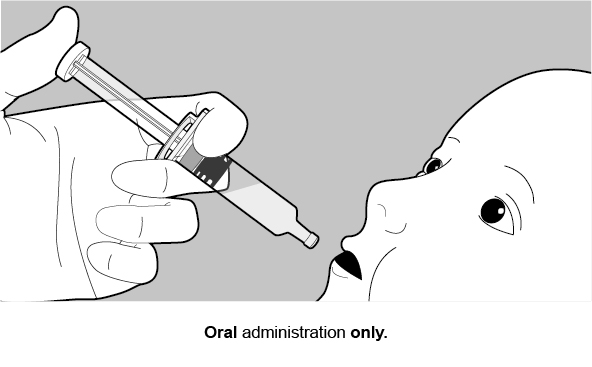
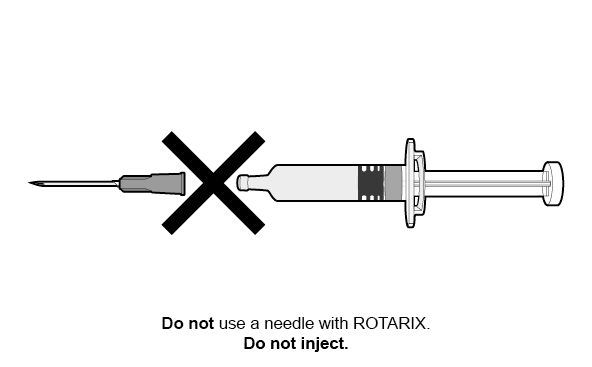
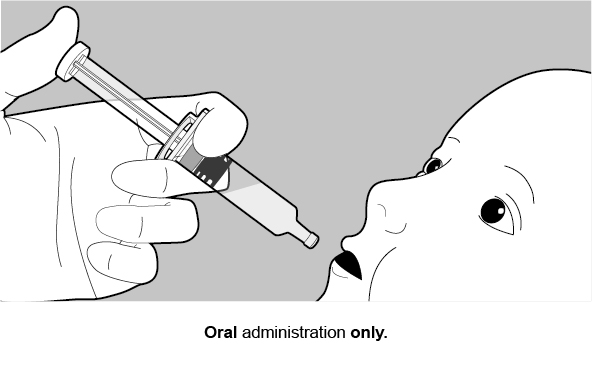
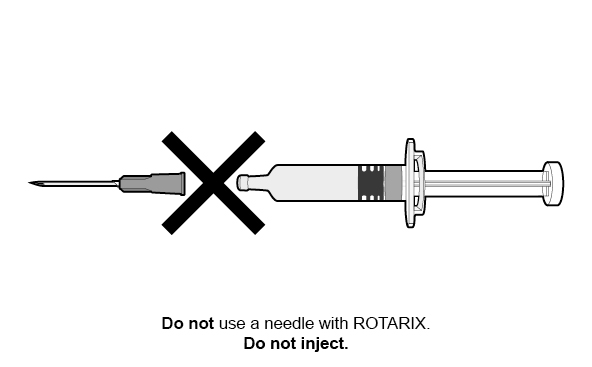
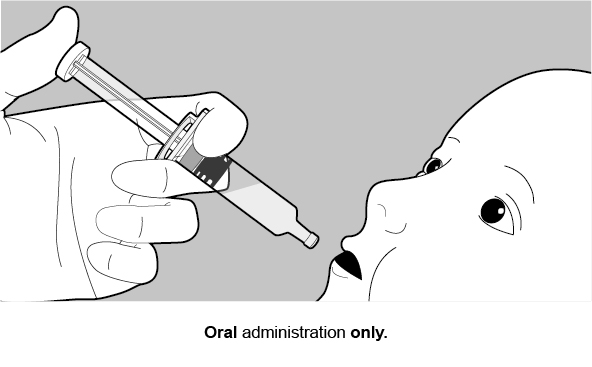
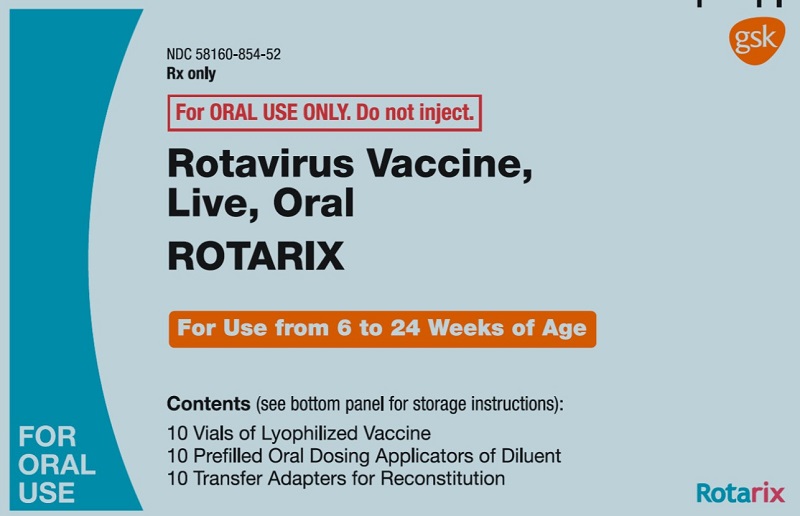
There are two formulations of ROTARIX: a reconstituted lyophilized formulation (supplied in a vial and oral dosing applicator presentation) and a liquid formulation (supplied in an oral dosing applicator only presentation) [see Description (11)]. Safety data accrued with each formulation is relevant to the other because each contains the same live, attenuated rotavirus strain and is manufactured using a similar process.
Common (≥5%) solicited adverse reactions included fussiness/irritability, cough/runny nose, fever, loss of appetite, and vomiting.
Solicited adverse reactions, unsolicited adverse events, serious adverse events (SAEs), and cases of intussusception were collected in 7 clinical studies (Studies 1 to 7; NCT00729001, NCT00385320, NCT00429481, NCT00757770, NCT00140686, NCT00169455, NCT00137930). Cases of intussusception and SAEs were collected in an additional large safety study (Study 8; NCT00140673) that compared ROTARIX (reconstituted lyophilized formulation) to placebo. Solicited adverse reactions, unsolicited adverse events, and SAEs were collected in 3 clinical studies (Studies 9 to 11; NCT02914184, NCT03207750, NCT03954743) that compared the two ROTARIX formulations.
Clinical Trials Experience with ROTARIX (Reconstituted Lyophilized Formulation)
Studies 1 to 8 evaluated a total of 71,209 infants who received ROTARIX (n = 36,755) or placebo (n = 34,454). The racial distribution for these studies was as follows: Hispanic 73.4%, White 16.2%, Black 1.0%, and other 9.4%; 51% were male.
Solicited Adverse Reactions: In 7 clinical studies (Studies 1 to 7), detailed safety information was collected by parents/guardians for 8 consecutive days following vaccination with ROTARIX (i.e., day of vaccination and the next 7 days). A diary card was completed to record fussiness/irritability, cough/runny nose, the infant’s temperature, loss of appetite, vomiting, or diarrhea on a daily basis during the first week following each dose of ROTARIX or placebo. Adverse reactions among recipients of ROTARIX and placebo occurred at similar rates (Table 1).
Unsolicited Adverse Reactions: Infants were monitored for unsolicited serious and non-SAEs that occurred in the 31-day period following vaccination in 7 clinical studies (Studies 1 to 7). The following adverse reactions occurred at a statistically higher incidence (95% Confidence Interval [CI] of Relative Risk [RR] excluding 1) among recipients of ROTARIX (n = 5,082) as compared with placebo recipients (n = 2,902): irritability (ROTARIX 11.4%, placebo 8.7%) and flatulence (ROTARIX 2.2%, placebo 1.3%).
Serious Adverse Reactions: Infants were monitored for SAEs that occurred in the 31-day period following vaccination in 8 clinical studies (Studies 1 to 8). Serious adverse reactions occurred in 1.7% of recipients of ROTARIX (n = 36,755) as compared with 1.9% of placebo recipients (n = 34,454). Among placebo recipients, diarrhea (placebo 0.07%, ROTARIX 0.02%), dehydration (placebo 0.06%, ROTARIX 0.02%), and gastroenteritis (placebo 0.3%, ROTARIX 0.2%) occurred at a statistically higher incidence (95% CI of RR excluding 1) as compared with recipients of ROTARIX.
Deaths: During the entire course of 8 clinical studies (Studies 1 to 8), there were 68 (0.19%) deaths following administration of ROTARIX (n = 36,755) and 50 (0.15%) deaths following placebo administration (n = 34,454). The most commonly reported cause of death following vaccination was pneumonia, which was observed in 19 (0.05%) recipients of ROTARIX and 10 (0.03%) placebo recipients (RR: 1.74, 95% CI: 0.76, 4.23).
Intussusception: In a controlled safety study (Study 8) conducted in Latin America and Finland, the risk of intussusception was evaluated in 63,225 infants (31,673 received ROTARIX and 31,552 received placebo). Infants were monitored by active surveillance including independent, complementary methods (prospective hospital surveillance and parent reporting at scheduled study visits) to identify potential cases of intussusception within 31 days after vaccination and, in a subset of 20,169 infants (10,159 received ROTARIX and 10,010 received placebo), up to one year after the first dose.
No increased risk of intussusception following administration of ROTARIX was observed within a 31-day period following any dose, and rates were comparable to the placebo group after a median of 100 days (Table 2). In a subset of 20,169 infants (10,159 received ROTARIX and 10,010 received placebo) followed up to one year after Dose 1, there were 4 cases of intussusception with ROTARIX compared with 14 cases of intussusception with placebo (RR: 0.28 [95% CI: 0.10, 0.81]). All of the infants who developed intussusception recovered without sequelae.
Among vaccine recipients, there were no confirmed cases of intussusception within the 0- to 14-day period after the first dose (Table 3), which was the period of highest risk for the previously licensed oral live rhesus rotavirus-based vaccine.1
Kawasaki Disease − Results from Controlled and Uncontrolled Clinical Studies: Kawasaki disease has been reported in 18 (0.035%) recipients of ROTARIX and 9 (0.021%) placebo recipients from 16 completed or ongoing clinical trials (Studies 1 to 8; Studies 12 to 14, NCT00425737, NCT00346892, NCT00139347; Studies 15 to 17, NCT00197210 for the 3 studies; Studies 18 and 19, NCT00334607, NCT00382772). Of the 27 cases, 5 occurred following ROTARIX in clinical trials that were either not placebo-controlled or 1:1 randomized. In placebo-controlled trials, Kawasaki disease was reported in 17 recipients of ROTARIX and 9 placebo recipients (RR: 1.71 [95% CI: 0.71, 4.38]). Three of the 27 cases were reported within 30 days post-vaccination: 2 cases (ROTARIX = 1, placebo = 1) were from placebo-controlled trials (RR: 1.00 [95% CI: 0.01, 78.35]) and one case following ROTARIX was from a non–placebo-controlled trial. Among recipients of ROTARIX, the time of onset after study dose ranged 3 days to 19 months.
Clinical Trials Comparing the Two ROTARIX Formulations
The safety of the ROTARIX liquid formulation was evaluated in 3 randomized clinical studies (Studies 9 to 11). A total of 4,223 infants received ROTARIX (liquid formulation, n = 2,507; reconstituted lyophilized formulation, n = 1,716). The racial distribution for these 3 studies was as follows: Asian 24.4%, White 63.2%, Black or African American 5.1%, and other 7.3%; 49.7% were male.
In Study 10, a concomitant vaccine administration study conducted in United States, 1,272 infants received ROTARIX (liquid formulation, n = 632; reconstituted lyophilized formulation, n = 640). The racial distribution for this study was as follows: Asian 3.3%, White 73.8%, Black or African American 11.9%, and other 10.9%; 51.5% were male.
In Studies 9 to 11, solicited general adverse reactions (cough/runny nose, diarrhea, fever, irritability/fussiness, loss of appetite and vomiting) were recorded by the parent on diary cards during the 8 days after each vaccination (day of vaccination and 7 following days). Unsolicited adverse events were assessed within 31 days following each vaccination (day of vaccination and 30 following days). SAEs were assessed through 6 months after the last dose.
Solicited Adverse Reactions: In Study 10, solicited adverse reactions among recipients of the two ROTARIX formulations are presented in the Table 4:
Unsolicited Adverse Events: Infants were monitored for unsolicited serious and non-SAEs that occurred in the 31-day period following vaccination in Studies 9 to 11. There were no notable differences in the occurrence and frequency of unsolicited adverse events between the groups.
Serious Adverse Events: During the entire course of Studies 9 to 11, SAEs occurred in 4.7% of recipients of ROTARIX liquid formulation (n = 2,507) as compared with 4.4% of ROTARIX reconstituted lyophilized formulation recipients (n = 1,716).
During the entire course of Studies 9 to 11, there was 1 fatal SAE (with diagnosis of sudden infant death syndrome) following administration of ROTARIX liquid formulation (Study 10). The SAE was assessed as not causally related to the vaccination.
Among participants in Studies 9 to 11, 2 intussusception cases were reported. One subject from Study 10 experienced intussusception 8 days after receiving the second dose of ROTARIX (reconstituted lyophilized formulation). The event was considered possibly related to ROTARIX. One subject from Study 9 experienced intussusception 133 days after receiving the second dose of ROTARIX (liquid formulation); the event was not considered related to ROTARIX. Both subjects were hospitalized, and the outcome of intussusception was reported as resolved.
6.2 Postmarketing Experience
The temporal association between vaccination with ROTARIX and intussusception was evaluated in a hospital-based active surveillance study that identified infants with intussusception at participating hospitals in Mexico. Using a self-controlled case series method,4 the incidence of intussusception during the first 7 days after receipt of ROTARIX and during the 31-day period after receipt of ROTARIX was compared with a control period. The control period was from birth to one year, excluding the pre-defined risk period (first 7 days or first 31 days post-vaccination, respectively).
Over a 2-year period, the participating hospitals provided health services to approximately 1 million infants under 1 year of age. Among 750 infants with intussusception, the relative incidence of intussusception in the 31‑day period after the first dose of ROTARIX compared with the control period was 1.96 (95.5% CI: 1.46, 2.63)]; the relative incidence of intussusception in the first 7 days after the first dose of ROTARIX compared with the control period was 6.07 (95.5% CI: 4.20, 8.63).
The Mexico study did not take into account all medical conditions that may predispose infants to intussusception. The results may not be generalizable to U.S. infants who have a lower background rate of intussusception than Mexican infants. However, if a temporal increase in the risk for intussusception following ROTARIX similar in magnitude to that observed in the Mexico study does exist in U.S. infants, it is estimated that approximately 1 to 3 additional cases of intussusception hospitalizations would occur per 100,000 vaccinated infants in the U.S. within 7 days following the first dose of ROTARIX. In the first year of life, the background rate of intussusception hospitalizations in the U.S. has been estimated to be approximately 34 per 100,000 infants.5
Other postmarketing observational studies conducted in Brazil and Australia also suggest an increased risk of intussusception within the first 7 days following the second dose of ROTARIX.2,3
Worldwide passive postmarketing surveillance data suggest that most cases of intussusception reported following ROTARIX occur in the 7-day period after the first dose.
The following adverse reactions have been identified during postapproval use of ROTARIX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccination.
Gastrointestinal Disorders
Intussusception (including death), recurrent intussusception (including death), hematochezia, gastroenteritis with vaccine viral shedding in infants with SCID.
Blood and Lymphatic System Disorders
Idiopathic thrombocytopenic purpura.
Vascular Disorders
Kawasaki disease.
General Disorders and Administration Site Conditions
Maladministration.