Label: VALPROIC ACID solution
- NDC Code(s): 17856-0792-1, 17856-0792-2, 17856-0792-5, 17856-0792-6
- Packager: ATLANTIC BIOLOGICALS CORP.
- This is a repackaged label.
- Source NDC Code(s): 50383-792
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated May 16, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
HEPATOTOXICITY
HEPATIC FAILURE RESULTING IN FATALITIES HAS OCCURRED IN PATIENTS RECEIVING VALPROIC ACID. EXPERIENCE HAS INDICATED THAT CHILDREN UNDER THE AGE OF TWO YEARS ARE AT A CONSIDERABLY INCREASED RISK OF DEVELOPING FATAL HEPATOTOXICITY, ESPECIALLY THOSE ON MULTIPLE ANTICONVULSANTS, THOSE WITH CONGENITAL METABOLIC DISORDERS, THOSE WITH SEVERE SEIZURE DISORDERS ACCOMPANIED BY MENTAL RETARDATION, AND THOSE WITH ORGANIC BRAIN DISEASE. WHEN VALPROIC ACID PRODUCTS ARE USED IN THIS PATIENT GROUP, THEY SHOULD BE USED WITH EXTREME CAUTION AND AS A SOLE AGENT. THE BENEFITS OF THERAPY SHOULD BE WEIGHED AGAINST THE RISKS. ABOVE THIS AGE GROUP, EXPERIENCE IN EPILEPSY HAS INCIDENCE THAT THE INCIDENT OF FATAL HEPATOTOXICITY DECREASES CONSIDERABLY IN PROGRESSIVELY OLDER PATIENT GROUPS.
THESE INCIDENTS USUALLY HAVE OCCURRED DURING THE FIRST SIX MONTHS OF TREATMENT. SERIOUS OR FATAL HEPATOTOXICITY MAY BE PRECEDED BY NON-SPECIFIC SYMPTOMS SUCH AS MALAISE, WEAKNESS, LETHARGY, FACIAL EDEMA, ANOREXIA AND VOMITING. IN PATIENTS WITH EPILEPSY, A LOSS OF SEIZURE CONTROL MAY ALSO OCCUR. PATIENTS SHOULD BE MONITORED CLOSELY FOR APPEARANCE OF THESE SYMPTOMS. LIVER FUNCTION TESTS SHOULD BE PERFORMED PRIOR TO THERAPY AND AT FREQUENT INTERVALS THEREAFTER, ESPECIALLY DURING THE FIRST SIX MONTHS.
TERATOGENICITY
VALPROATE CAN PRODUCE TERATOGENIC EFFECTS SUCH AS NEURAL TUBE DEFECTS (E.G., SPINA BIFIDA). ACCORDINGLY, THE USE OF VALPROATE PRODUCTS IN WOMEN OF CHILDBEARING POTENTIAL REQUIRES THAT THE BENEFITS OF ITS USE BE WEIGHED AGAINST THE RISK OF INJURY TO THE FETUS.
THIS IS ESPECIALLY IMPORTANT WHEN THE TREATMENT OF A SPONTANEOUSLY REVERSIBLE CONDITION NOT ORDINARILY ASSOCIATED WITH PERMANENT INJURY OR RISK OF DEATH (E.G., MIGRAINE) IS CONTEMPLATED. SEE WARNINGS, INFORMATION FOR PATIENTS.
A PATIENT INFORMATION LEAFLET DESCRIBING THE TERATOGENIC POTENTIAL OF VALPROATE IS AVAILABLE FOR PATIENTS.
PANCREATITIS
CASES OF LIFE-THREATENING PANCREATITIS HAVE BEEN REPORTED IN BOTH CHILDREN AND ADULTS RECEIVING VALPROATE. SOME OF THE CASES HAVE BEEN DESCRIBED AS HEMORRHAGIC WITH A RAPID PROGRESSION FROM INITIAL SYMPTOMS TO DEATH. CASES HAVE BEEN REPORTED SHORTLY AFTER INITIAL USE AS WELL AS AFTER SEVERAL YEARS OF USE. PATIENTS AND GUARDIANS SHOULD BE WARNED THAT ABDOMINAL PAIN, NAUSEA, VOMITING, AND/OR ANOREXIA CAN BE SYMPTOMS OF PANCREATITIS THAT REQUIRE PROMPT MEDICAL EVALUATION. IF PANCREATITIS IS DIAGNOSED, VALPROATE SHOULD ORDINARILY BE DISCONTINUED. ALTERNATIVE TREATMENT FOR THE UNDERLYING MEDICAL CONDITION SHOULD BE INITIATED AS CLINICALLY INDICATED. (See and .) WARNINGSPRECAUTIONS
-
DESCRIPTION
Valproic acid is a carboxylic acid designated as 2-propylpentanoic acid. It is also known as dipropylacetic acid. Valproic acid has the following structure:
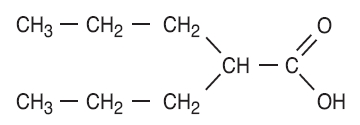
Valproic acid (pKa 4.8) has a molecular weight of 144 and occurs as a colorless liquid with a characteristic odor. It is slightly soluble in water (1.3 mg/mL) and very soluble in organic solvents.
Valproic acid oral solution, USP is an antiepileptic for oral administration. The oral solution contains the equivalent of 250 mg valproic acid per 5 mL as the sodium salt.
FD&C Red No. 40, methylparaben, natural and artificial raspberry flavor, propylparaben, purified water, sodium hydroxide, sorbitol, and sucrose. Inactive Ingredients:
-
CLINICAL PHARMACOLOGY
Pharmacodynamics
Valproic acid dissociates to the valproate ion in the gastrointestinal tract. The mechanisms by which valproate exerts its antiepileptic effects have not been established. It has been suggested that its activity in epilepsy is related to increased brain concentrations of gamma-aminobutyric acid (GABA).
Pharmacokinetics
Absorption/Bioavailability
Equivalent oral doses of divalproex sodium products and valproic acid capsules deliver equivalent quantities of valproate ion systemically. Although the rate of valproate ion absorption may vary with the formulation administered (liquid, solid, or sprinkle), conditions of use (e.g., fasting or postprandial) and the method of administration (e.g., whether the contents of the capsule are sprinkled on food or the capsule is taken intact), these differences should be of minor clinical importance under the steady state conditions achieved in chronic use in the treatment of epilepsy.
However, it is possible that differences among the various valproate products in Tmax and Cmax could be important upon initiation of treatment. For example, in single dose studies, the effect of feeding had a greater influence on the rate of absorption of the divalproex sodium tablet (increase in Tmax from 4 to 8 hours) than on the absorption of the divalproex sodium sprinkle capsules (increase in Tmax from 3.3 to 4.8 hours).
While the absorption rate from the G.I. tract and fluctuation in valproate plasma concentrations vary with dosing regimen and formulation, the efficacy of valproate as an anticonvulsant in chronic use is unlikely to be affected. Experience employing dosing regimens from once-a-day to four-times-a-day, as well as studies in primate epilepsy models involving constant rate infusion, indicate that total daily systemic bioavailability (extent of absorption) is the primary determinant of seizure control and that differences in the ratios of plasma peak to trough concentrations between valproate formulations are inconsequential from a practical clinical standpoint.
Co-administration of oral valproate products with food and substitution among the various divalproex sodium and valproic acid formulations should cause no clinical problems in the management of patients with epilepsy (see ). Nonetheless, any changes in dosage administration, or the addition or discontinuance of concomitant drugs should ordinarily be accompanied by close monitoring of clinical status and valproate plasma concentrations. DOSAGE AND ADMINISTRATION
Distribution:
Protein Binding:
The plasma protein binding of valproate is concentration dependent and the free fraction increases from approximately 10% at 40 μg/mL to 18.5% at 130 μg/mL. Protein binding of valproate is reduced in the elderly, in patients with chronic hepatic diseases, in patients with renal impairment, and in the presence of other drugs (e.g., aspirin). Conversely, valproate may displace certain protein-bound drugs (e.g., phenytoin, carbamazepine, warfarin, and tolbutamide). (See for more detailed information on the pharmacokinetic interactions of valproate with other drugs.) PRECAUTIONS, Drug Interactions
CNS Distribution
Valproate concentrations in cerebrospinal fluid (CSF) approximate unbound concentrations in plasma (about 10% of total concentration).
Metabolism
Valproate is metabolized almost entirely by the liver. In adult patients on monotherapy, 30-50% of an administered dose appears in urine as a glucuronide conjugate. Mitochondrial ß-oxidation is the other major metabolic pathway, typically accounting for over 40% of the dose. Usually, less than 15-20% of the dose is eliminated by other oxidative mechanisms. Less than 3% of an administered dose is excreted unchanged in urine.
The relationship between dose and total valproate concentration is nonlinear; concentration does not increase proportionally with the dose, but rather, increases to a lesser extent due to saturable plasma protein binding. The kinetics of unbound drug are linear.
Elimination
Mean plasma clearance and volume of distribution for total valproate are 0.56 L/hr/1.73 m and 11 L/1.73 m , respectively. Mean plasma clearance and volume of distribution for free valproate are 4.6 L/hr/1.73 m and 92 L/1.73 m . Mean terminal half-life for valproate monotherapy ranged from 9 to 16 hours following oral dosing regimens of 250 to 1000 mg. 2222
The estimates cited apply primarily to patients who are not taking drugs that affect hepatic metabolizing enzyme systems. For example, patients taking enzyme-inducing antiepileptic drugs (carbamazepine, phenytoin, and phenobarbital) will clear valproate more rapidly. Because of these changes in valproate clearance, monitoring of antiepileptic concentrations should be intensified whenever concomitant antiepileptics are introduced or withdrawn.
Special Populations
Effect of Age:
Neonates
Children within the first two months of life have a markedly decreased ability to eliminate valproate compared to older children and adults. This is a result of reduced clearance (perhaps due to delay in development of glucuronosyltransferase and other enzyme systems involved in valproate elimination) as well as increased volume of distribution (in part due to decreased plasma protein binding). For example, in one study, the half-life in children under 10 days ranged from 10 to 67 hours compared to a range of 7 to 13 hours in children greater than 2 months.
Children
Pediatric patients (i.e., between 3 months and 10 years) have 50% higher clearances expressed on weight (i.e., mL/min/kg) than do adults. Over the age of 10 years, children have pharmacokinetic parameters that approximate those of adults.
Elderly
The capacity of elderly patients (age range: 68 to 89 years) to eliminate valproate has been shown to be reduced compared to younger adults (age range: 22 to 26). Intrinsic clearance is reduced by 39%; the free fraction is increased by 44%. Accordingly, the initial dosage should be reduced in the elderly. (See ). DOSAGE AND ADMINISTRATION
Effect of Gender
There are no differences in the body surface area adjusted unbound clearance between males and females (4.8 ± 0.17 and 4.7 ± 0.07 L/hr per 1.73 m , respectively). 2
Effect of Disease
Liver Disease
(See and ). Liver disease impairs the capacity to eliminate valproate. In one study, the clearance of free valproate was decreased by 50% in 7 patients with cirrhosis and by 16% in 4 patients with acute hepatitis, compared with 6 healthy subjects. In that study, the half-life of valproate was increased from 12 to 18 hours. Liver disease is also associated with decreased albumin concentrations and larger unbound fractions (2 to 2.6 fold increase) of valproate. Accordingly, monitoring of total concentrations may be misleading since free concentrations may be substantially elevated in patients with hepatic disease whereas total concentrations may appear to be normal. , , BOXED WARNINGCONTRAINDICATIONSWARNINGS
Renal Disease
A slight reduction (27%) in the unbound clearance of valproate has been reported in patients with renal failure (creatinine clearance < 10 mL/minute); however, hemodialysis typically reduces valproate concentrations by about 20%. Therefore, no dosage adjustment appears to be necessary in patients with renal failure. Protein binding in these patients is substantially reduced; thus, monitoring total concentrations may be misleading.
Plasma Levels and Clinical Effect
The relationship between plasma concentration and clinical response is not well documented. One contributing factor is the nonlinear, concentration dependent protein binding of valproate which affects the clearance of the drug. Thus, monitoring of total serum valproate cannot provide a reliable index of the bioactive valproate species.
For example, because the plasma protein binding of valproate is concentration dependent, the free fraction increases from approximately 10% at 40 μg/mL to 18.5% at 130 μg/mL. Higher than expected free fractions occur in the elderly, in hyperlipidemic patients, and in patients with hepatic and renal diseases.
Clinical Trials
The studies described in the following section were conducted using divalproex sodium tablets.
Epilepsy
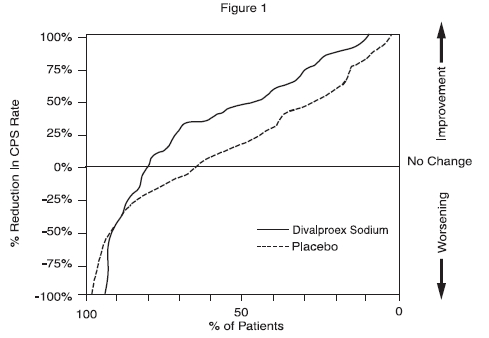
The efficacy of divalproex sodium in reducing the incidence of complex partial seizures (CPS) that occur in isolation or in association with other seizure types was established in two controlled trials.
In one, multiclinic, placebo controlled study employing an add-on design (adjunctive therapy), 144 patients who continued to suffer eight or more CPS per 8 weeks during an 8 week period of monotherapy with doses of either carbamazepine or phenytoin sufficient to assure plasma concentrations within the "therapeutic range" were randomized to receive, in addition to their original antiepilepsy drug (AED), either divalproex sodium or placebo. Randomized patients were to be followed for a total of 16 weeks. The following table presents the findings.
- *
- *Reduction from baseline statistically significantly greater for divalproex sodium than placebo at p ≤ 0.05 level.
Adjunctive Therapy Study
Median Incidence of CPS per 8 WeeksAdd-on
TreatmentNumber of
PatientsBaseline
IncidenceExperimental
IncidenceDivalproex Sodium 75 16.0 8.9* * Placebo 69 14.5 11.5 Figure 1 presents the proportion of patients (X axis) whose percentage reduction from baseline in complex partial seizure rates was at least as great as that indicated on the Y axis in the adjunctive therapy study. A positive percent reduction indicates an improvement (i.e., a decrease in seizure frequency), while a negative percent reduction indicates worsening. Thus, in a display of this type, the curve for an effective treatment is shifted to the left of the curve for placebo. This figure shows that the proportion of patients achieving any particular level of improvement was consistently higher for divalproex sodium than for placebo. For example, 45% of patients treated with divalproex sodium had a ≥ 50% reduction in complex partial seizure rate compared to 23% of patients treated with placebo.
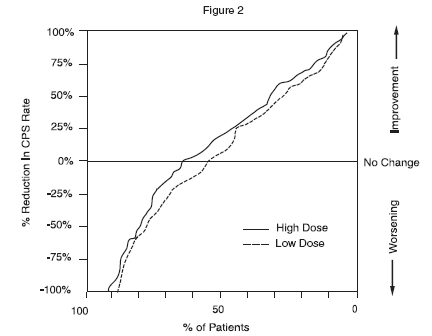
The second study assessed the capacity of divalproex sodium to reduce the incidence of CPS when administered as the sole AED. The study compared the incidence of CPS among patients randomized to either a high or low dose treatment arm. Patients qualified for entry into the randomized comparison phase of this study only if 1) they continued to experience 2 or more CPS per 4 weeks during an 8 to 12 week long period of monotherapy with adequate doses of an AED (i.e., phenytoin, carbamazepine, phenobarbital, or primidone) and 2) they made a successful transition over a two week interval to divalproex sodium. Patients entering the randomized phase were then brought to their assigned target dose, gradually tapered off their concomitant AED and followed for an interval as long as 22 weeks. Less than 50% of the patients randomized, however, completed the study. In patients converted to divalproex sodium monotherapy, the mean total valproate concentrations during monotherapy were 71 and 123 μg/mL in the low dose and high dose groups, respectively.
The following table presents the findings for all patients randomized who had at least one postrandomization assessment.
- *
- *Reduction from baseline statistically significantly greater for high dose than low dose at p ≤ 0.05 level.
Monotherapy Study
Median Incidence of CPS per 8 WeeksTreatment Number
of PatientsBaseline
IncidenceRandomized Phase
IncidenceHigh dose divalproex sodium 131 13.2 10.7* * Low dose divalproex sodium 134 14.2 13.8 Figure 2 presents the proportion of patients (X axis) whose percentage reduction from baseline in complex partial seizure rates was at least as great as that indicated on the Y axis in the monotherapy study. A positive percent reduction indicates an improvement (i.e., a decrease in seizure frequency), while a negative percent reduction indicates worsening. Thus, in a display of this type, the curve for a more effective treatment is shifted to the left of the curve for a less effective treatment. This figure shows that the proportion of patients achieving any particular level of reduction was consistently higher for high dose divalproex sodium than for low dose divalproex sodium. For example, when switching from carbamazepine, phenytoin, phenobarbital or primidone monotherapy to high dose divalproex sodium monotherapy, 63% of patients experienced no change or a reduction in complex partial seizure rates compared to 54% of patients receiving low dose divalproex sodium.
-
INDICATIONS AND USAGE
Valproic acid is indicated as monotherapy and adjunctive therapy in the treatment of patients with complex partial seizures that occur either in isolation or in association with other types of seizures. Valproic acid is indicated for use as sole and adjunctive therapy in the treatment of simple and complex absence seizures, and adjunctively in patients with multiple seizure types which include absence seizures.
Simple absence is defined as very brief clouding of the sensorium or loss of consciousness accompanied by certain generalized epileptic discharges without other detectable clinical signs. Complex absence is the term used when other signs are also present.
SEE FOR STATEMENT REGARDING FATAL HEPATIC DYSFUNCTION. WARNINGS
-
CONTRAINDICATIONS
VALPROIC ACID SHOULD NOT BE ADMINISTERED TO PATIENTS WITH HEPATIC DISEASE OR SIGNIFICANT HEPATIC DYSFUNCTION.
Valproic acid is contraindicated in patients with known hypersensitivity to the drug.
Valproic acid is contraindicated in patients with known urea cycle disorders (see ). WARNINGS
-
WARNINGS
Hepatotoxicity
Hepatic failure resulting in fatalities has occurred in patients receiving valproic acid. These incidents usually have occurred during the first six months of treatment. Serious or fatal hepatotoxicity may be preceded by non-specific symptoms such as malaise, weakness, lethargy, facial edema, anorexia, and vomiting. In patients with epilepsy, a loss of seizure control may also occur. Patients should be monitored closely for appearance of these symptoms. Liver function tests should be performed prior to therapy and at frequent intervals thereafter, especially during the first six months. However, healthcare providers should not rely totally on serum biochemistry since these tests may not be abnormal in all instances, but should also consider the results of careful interim medical history and physical examination.
Caution should be observed when administering valproic acid to patients with a prior history of hepatic disease. Patients on multiple anticonvulsants, children, those with congenital metabolic disorders, those with severe seizure disorders accompanied by mental retardation, and those with organic brain disease may be at particular risk. Experience has indicated that children under the age of two years are at considerably increased risk of developing fatal hepatotoxicity, especially those with the aforementioned conditions. When valproic acid products are used in this patient group, they should be used with extreme caution and as a sole agent. The benefits of therapy should be weighed against the risks. Above this age group, experience has indicated that the incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups.
The drug should be discontinued immediately in the presence of significant hepatic dysfunction, suspected or apparent. In some cases, hepatic dysfunction has progressed in spite of discontinuation of drug.
Usage in Pregnancy
VALPROATE CAN PRODUCE TERATOGENIC EFFECTS. DATA SUGGEST THAT THERE IS AN INCREASED INCIDENCE OF CONGENITAL MALFORMATIONS ASSOCIATED WITH THE USE OF VALPROATE BY WOMEN WITH SEIZURE DISORDERS DURING PREGNANCY WHEN COMPARED TO THE INCIDENCE IN WOMEN WITH SEIZURE DISORDERS WHO DO NOT USE ANTIEPILEPTIC DRUGS DURING PREGNANCY, THE INCIDENCE IN WOMEN WITH SEIZURE DISORDERS WHO USE OTHER ANTIEPILEPTIC DRUGS, AND THE BACKGROUND INCIDENCE FOR THE GENERAL POPULATION. THEREFORE, VALPROATE SHOULD BE CONSIDERED FOR WOMEN OF CHILDBEARING POTENTIAL ONLY AFTER THE RISKS HAVE BEEN THOROUGHLY DISCUSSED WITH THE PATIENT AND WEIGHED AGAINST THE POTENTIAL BENEFITS OF TREATMENT.
THERE ARE MULTIPLE REPORTS IN THE CLINICAL LITERATURE THAT INDICATE THE USE OF ANTIEPILEPTIC DRUGS DURING PREGNANCY RESULTS IN AN INCREASED INCIDENCE OF CONGENITAL MALFORMATIONS IN OFFSPRING. ANTIEPILEPTIC DRUGS, INCLUDING VALPROATE, SHOULD BE ADMINISTERED TO WOMEN OF CHILDBEARING POTENTIAL ONLY IF THEY ARE CLEARLY SHOWN TO BE ESSENTIAL IN THE MANAGEMENT OF THEIR MEDICAL CONDITION.
Antiepileptic drugs should not be discontinued abruptly in patients in whom the drug is administered to prevent major seizures because of the strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life. In individual cases where the severity and frequency of the seizure disorder are such that the removal of medication does not pose a serious threat to the patient, discontinuation of the drug may be considered prior to and during pregnancy, although it cannot be said with any confidence that even minor seizures do not pose some hazard to the developing embryo or fetus.
Human Data
Congenital Malformations
The North American Antiepileptic Drug Pregnancy Registry reported 16 cases of congenital malformations among the offspring of 149 women with epilepsy who were exposed to valproic acid monotherapy during the first trimester of pregnancy at doses of approximately 1,000 mg per day, for a prevalence rate of 10.7% (95% CI 6.3%-16.9%). Three of the 149 offspring (2%) had neural tube defects and 6 of the 149 (4%) had less severe malformations. Among epileptic women who were exposed to other antiepileptic drug monotherapies during pregnancy (1,048 patients) the malformation rate was 2.9% (95% CI 2.0% to 4.1%). There was a 4-fold increase in congenital malformations among infants with valproic acid-exposed mothers compared with those treated with other antiepileptic monotherapies as a group (Odds Ratio 4.0; 95% CI 2.1 to 7.4). This increased risk does not reflect a comparison versus any specific antiepileptic drug, but the risk versus the heterogeneous group of all other antiepileptic drug monotherapies combined. The increased teratogenic risk from valproic acid in women with epilepsy is expected to be reflected in an increased risk in other indications (e.g., migraine or bipolar disorder).
THE STRONGEST ASSOCIATION OF MATERNAL VALPROATE USAGE WITH CONGENITAL MALFORMATIONS IS WITH NEURAL TUBE DEFECTS (AS DISCUSSED UNDER THE NEXT SUBHEADING). HOWEVER, OTHER CONGENITAL ANOMALIES (E.G. CRANIOFACIAL DEFECTS, CARDIOVASCULAR MALFORMATIONS AND ANOMALIES INVOLVING VARIOUS BODY SYSTEMS), COMPATIBLE AND INCOMPATIBLE WITH LIFE, HAVE BEEN REPORTED. SUFFICIENT DATA TO DETERMINE THE INCIDENCE OF THESE CONGENITAL ANOMALIES IS NOT AVAILABLE.
Neural Tube Defects
THE INCIDENCE OF NEURAL TUBE DEFECTS IN THE FETUS IS INCREASED IN MOTHERS RECEIVING VALPROATE DURING THE FIRST TRIMESTER OF PREGNANCY. THE CENTERS FOR DISEASE CONTROL (CDC) HAS ESTIMATED THE RISK OF VALPROIC ACID EXPOSED WOMEN HAVING CHILDREN WITH SPINA BIFIDA TO BE APPROXIMATELY 1 TO 2%. THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS (ACOG) ESTIMATES THE GENERAL POPULATION RISK FOR CONGENITAL NEURAL TUBE DEFECTS AS 0.14% TO 0.2%.
Tests to detect neural tube and other defects using current accepted procedures should be considered a part of routine prenatal care in pregnant women receiving valproate.
Evidence suggests that pregnant women who receive folic acid supplementation may be at decreased risk for congenital neural tube defects in their offspring compared to pregnant women not receiving folic acid. Whether the risk of neural tube defects in the offspring of women receiving valproate specifically is reduced by folic acid supplementation is unknown. DIETARY FOLIC ACID SUPPLEMENTATION BOTH PRIOR TO AND DURING PREGNANCY SHOULD BE ROUTINELY RECOMMENDED TO PATIENTS CONTEMPLATING PREGNANCY.
Other Adverse Pregnancy Effects
PATIENTS TAKING VALPROATE MAY DEVELOP CLOTTING ABNORMALITIES (SEE and ). A PATIENT WHO HAD LOW FIBRINOGEN WHEN TAKING MULTIPLE ANTICONVULSANTS INCLUDING VALPROATE GAVE BIRTH TO AN INFANT WITH AFIBRINOGENEMIA WHO SUBSEQUENTLY DIED OF HEMORRHAGE. IF VALPROATE IS USED IN PREGNANCY, THE CLOTTING PARAMETERS SHOULD BE MONITORED CAREFULLY. PRECAUTIONS - GENERALWARNINGS
PATIENTS TAKING VALPROATE MAY DEVELOP HEPATIC FAILURE (SEE and ). FATAL HEPATIC FAILURES, IN A NEWBORN AND IN AN INFANT, HAVE BEEN REPORTED FOLLOWING THE MATERNAL USE OF VALPROATE DURING PREGNANCY. PRECAUTIONS - HEPATOTOXICITYBOXED WARNING
There have been reports of developmental delay, autism and/or autism spectrum disorder in the offspring of women exposed to valproate during pregnancy.
Animal Data
Animal studies have demonstrated valproate-induced teratogenicity. Increased frequencies of malformations, as well as intrauterine growth retardation and death, have been observed in mice, rats, rabbits, and monkeys following prenatal exposure to valproate. Malformations of the skeletal system are the most common structural abnormalities produced in experimental animals, but neural tube closure defects have been seen in mice exposed to maternal plasma valproate concentrations exceeding 230 μg/mL (2.3 times the upper limit of the human therapeutic range) during susceptible periods of embryonic development. Administration of an oral dose of 200 mg/kg/day or greater (50% of the maximum human daily dose or greater on a mg/m basis) to pregnant rats during organogenesis produced malformations (skeletal, cardiac, and urogenital) and growth retardation in the offspring. These doses resulted in peak maternal plasma valproate levels of approximately 340 μg/mL or greater (3.4 times the upper limit of the human therapeutic range or greater). Behavioral deficits have been reported in the offspring of rats given a dose of 200 mg/kg/day throughout most of pregnancy. An oral dose of 350 mg/kg/day (approximately 2 times the maximum human daily dose on a mg/m basis) produced skeletal and visceral malformations in rabbits exposed during organogenesis. Skeletal malformations, growth retardation, and death were observed in rhesus monkeys following administration of an oral dose of 200 mg/kg/day (equal to the maximum human daily dose on a mg/m basis) during organogenesis. This dose resulted in peak maternal plasma valproate levels of approximately 280 μg/mL (2.8 times the upper limit of the human therapeutic range). 222
Pancreatitis
Cases of life-threatening pancreatitis have been reported in both children and adults receiving valproate. Some of the cases have been described as hemorrhagic with rapid progression from initial symptoms to death. Some cases have occurred shortly after initial use as well as after several years of use. The rate based upon the reported cases exceeds that expected in the general population and there have been cases in which pancreatitis recurred after rechallenge with valproate. In clinical trials, there were 2 cases of pancreatitis without alternative etiology in 2416 patients, representing 1044 patient-years experience. Patients and guardians should be warned that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis that require prompt medical evaluation. If pancreatitis is diagnosed, valproate should ordinarily be discontinued. Alternative treatment for the underlying medical condition should be initiated as clinically indicated (see ). BOXED WARNING
Urea Cycle Disorders (UCD)
Valproic acid is contraindicated in patients with known urea cycle disorders.
Hyperammonemic encephalopathy, sometimes fatal, has been reported following initiation of valproate therapy in patients with urea cycle disorders, a group of uncommon genetic abnormalities, particularly ornithine transcarbamylase deficiency. Prior to the initiation of valproate therapy, evaluation for UCD should be considered in the following patients: 1) those with a history of unexplained encephalopathy or coma, encephalopathy associated with a protein load, pregnancy-related or postpartum encephalopathy, unexplained mental retardation, or history of elevated plasma ammonia or glutamine; 2) those with cyclical vomiting and lethargy, episodic extreme irritability, ataxia, low BUN, or protein avoidance; 3) those with a family history of UCD or a family history of unexplained infant deaths (particularly males); 4) those with other signs or symptoms of UCD. Patients who develop symptoms of unexplained hyperammonemic encephalopathy while receiving valproate therapy should receive prompt treatment (including discontinuation of valproate therapy) and be evaluated for underlying urea cycle disorders (see and ). CONTRAINDICATIONSPRECAUTIONS
Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including valproic acid, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 1 shows absolute and relative risk by indication for all evaluated AEDs.
Table 1
Risk by indication for antiepileptic drugs in the pooled analysis
Indication Placebo Patients with Events Per 1000 Patients Drug Patients with Events Per 1000 Patients Incidence of Events in Drug Patients/Incidence in Placebo Patients Relative Risk:
Additional Drug Patients with Events Per 1000 Patients Risk Difference:
Epilepsy 1.0 3.4 3.5 2.4 Psychiatric 5.7 8.5 1.5 2.9 Other 1.0 1.8 1.9 0.9 Total 2.4 4.3 1.8 1.9 The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing valproic acid or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Interaction with Carbapenem Antibiotics
Carbapenem antibiotics (ertapenem, imipenem, meropenem) may reduce serum valproic acid concentrations to subtherapeutic levels, resulting in loss of seizure control. Serum valproic acid concentrations should be monitored frequently after initiating carbapenem therapy. Alternative antibacterial or anticonvulsant therapy should be considered if serum valproic acid concentrations drop significantly or seizure control deteriorates (see ). PRECAUTIONS - Drug Interactions
Somnolence in the Elderly
In a double-blind, multicenter trial of valproate in elderly patients with dementia (mean age = 83 years), doses were increased by 125 mg/day to a target dose of 20 mg/kg/day. A significantly higher proportion of valproate patients had somnolence compared to placebo, and although not statistically significant, there was a higher proportion of patients with dehydration. Discontinuations for somnolence were also significantly higher than with placebo. In some patients with somnolence (approximately one-half), there was associated reduced nutritional intake and weight loss. There was a trend for the patients who experienced these events to have a lower baseline albumin concentration, lower valproate clearance, and a higher BUN. In elderly patients, dosage should be increased more slowly and with regular monitoring for fluid and nutritional intake, dehydration, somnolence, and other adverse events. Dose reductions or discontinuation of valproate should be considered in patients with decreased food or fluid intake and in patients with excessive somnolence (see ). DOSAGE AND ADMINISTRATION
Thrombocytopenia
The frequency of adverse effects (particularly elevated liver enzymes and thrombocytopenia (see ) may be dose-related. In a clinical trial of divalproex sodium as monotherapy in patients with epilepsy, 34/126 patients (27%) receiving approximately 50 mg/kg/day on average, had at least one value of platelets ≤ 75 x 109/L. Approximately half of these patients had treatment discontinued, with return of platelet counts to normal. In the remaining patients, platelet counts normalized with continued treatment. In this study, the probability of thrombocytopenia appeared to increase significantly at total valproate concentrations of ≥ 110 μg/mL (females) or ≥ 135 μg/mL (males). The therapeutic benefit which may accompany the higher doses should therefore be weighed against the possibility of a greater incidence of adverse effects. PRECAUTIONS
-
PRECAUTIONS
Hypothermia
Hypothermia, defined as an unintentional drop in body core temperature to <35°C (95°F), has been reported in association with valproate therapy both in conjunction with and in the absence of hyperammonemia. This adverse reaction can also occur in patients using concomitant topiramate with valproate after starting topiramate treatment or after increasing the daily dose of topiramate (see ). Consideration should be given to stopping valproate in patients who develop hypothermia, which may be manifested by a variety of clinical abnormalities including lethargy, confusion, coma, and significant alterations in other major organ systems such as the cardiovascular and respiratory systems. Clinical management and assessment should include examination of blood ammonia levels. Drug Interactions - Topiramate
Hyperammonemia
Hyperammonemia has been reported in association with valproate therapy and may be present despite normal liver function tests. In patients who develop unexplained lethargy and vomiting or changes in mental status, hyperammonemic encephalopathy should be considered and an ammonia level should be measured. Hyperammonemia should also be considered in patients who present with hypothermia (see ). If ammonia is increased, valproate therapy should be discontinued. Appropriate interventions for treatment of hyperammonemia should be initiated, and such patients should undergo investigation for underlying urea cycle disorders (see and and ). PRECAUTIONS - HypothermiaCONTRAINDICATIONSWARNINGS - Urea Cycle Disorders (UCD)PRECAUTIONS - Hyperammonemia and Encephalopathy Associated with Concomitant Topiramate Use
Asymptomatic elevations of ammonia are more common and when present, require close monitoring of plasma ammonia levels. If the elevation persists, discontinuation of valproate therapy should be considered.
Hyperammonemia and Encephalopathy Associated with Concomitant Topiramate Use
Concomitant administration of topiramate and valproic acid has been associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. Hypothermia can also be a manifestation of hyperammonemia (see ). In most cases, symptoms and signs abated with discontinuation of either drug. This adverse event is not due to a pharmacokinetic interaction. It is not known if topiramate monotherapy is associated with hyperammonemia. Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at an increased risk for hyperammonemia with or without encephalopathy. Although not studied, an interaction of topiramate and valproic acid may exacerbate existing defects or unmask deficiencies in susceptible persons. In patients who develop unexplained lethargy, vomiting, or changes in mental status, hyperammonemic encephalopathy should be considered and an ammonia level should be measured. (see and and ). PRECAUTIONS - HypothermiaCONTRAINDICATIONSWARNINGS - Urea Cycle DisordersPRECAUTIONS - Hyperammonemia
General
Because of reports of thrombocytopenia (see ), inhibition of the secondary phase of platelet aggregation, and abnormal coagulation parameters, (e.g., low fibrinogen), platelet counts and coagulation tests are recommended before initiating therapy and at periodic intervals. It is recommended that patients receiving valproic acid be monitored for platelet count and coagulation parameters prior to planned surgery. In a clinical trial of divalproex sodium as monotherapy in patients with epilepsy, 34/126 patients (27%) receiving approximately 50 mg/kg/day on average, had at least one value of platelets ≤ 75 x 109/L. Approximately half of these patients had treatment discontinued, with return of platelet counts to normal. In the remaining patients, platelet counts normalized with continued treatment. In this study, the probability of thrombocytopenia appeared to increase significantly at total valproate concentrations of ≤ 110 µg/mL (females) or ≥ 135 µg/mL (males). Evidence of hemorrhage, bruising, or a disorder of hemostasis/coagulation is an indication for reduction of the dosage or withdrawal of therapy. WARNINGS
Since valproate may interact with concurrently administered drugs which are capable of enzyme induction, periodic plasma concentration determinations of valproate and concomitant drugs are recommended during the early course of therapy (see ). PRECAUTIONS - Drug Interactions
Valproate is partially eliminated in the urine as a keto-metabolite which may lead to a false interpretation of the urine ketone test.
There have been reports of altered thyroid function tests associated with valproate. The clinical significance of these is unknown.
There are studies that suggest valproate stimulates the replication of the HIV and CMV viruses under certain experimental conditions. The clinical consequence, if any, is not known. Additionally, the relevance of these findings is uncertain for patients receiving maximally suppressive antiretroviral therapy. Nevertheless, these data should be borne in mind when interpreting the results from regular monitoring of the viral load in HIV infected patients receiving valproate or when following CMV infected patients clinically. in vitroin vitro
Multi-organ Hypersensitivity Reaction
Multi-organ hypersensitivity reactions have been rarely reported in close temporal association to the initiation of valproate therapy in adult and pediatric patients (median time to detection 21 days: range 1 to 40 days). Although there have been a limited number of reports, many of these cases resulted in hospitalization and at least one death has been reported. Signs and symptoms of this disorder were diverse; however, patients typically, although not exclusively, presented with fever and rash associated with other organ system involvement. Other associated manifestations may include lymphadenopathy, hepatitis, liver function test abnormalities, hematological abnormalities (e.g., eosinophilia, thrombocytopenia, neutropenia), pruritis, nephritis, oliguria, hepato-renal syndrome, arthralgia, and asthenia. Because the disorder is variable in its expression, other organ system symptoms and signs, not noted here, may occur. If this reaction is suspected, valproate should be discontinued and an alternative treatment started. Although the existence of cross sensitivity with other drugs that produce this syndrome is unclear, the experience amongst drugs associated with multi-organ hypersensitivity would indicate this to be a possibility.
Information for patients
Since valproic acid has been associated with certain types of birth defects, female patients of childbearing age considering the use of valproic acid should be advised of the risk and of alternative therapeutic options and to read the , which appears as the last section of the labeling. Patient Information LeafletThis is especially important when the treatment of a spontaneously reversible condition not ordinarily associated with permanent injury or risk of death (e.g., migraine) is considered.
Patients should be encouraged to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334 (see ). PRECAUTIONS - Pregnancy
Patients and guardians should be warned that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis and, therefore, require further medical evaluation promptly.
Suicidal Thinking and Behavior
Patients, their caregivers, and families should be counseled that AEDs, including valproic acid, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to the healthcare providers (see ). WARNINGS
Patients should be informed of the signs and symptoms associated with hyperammonemic encephalopathy (see ) and be told to inform the prescriber if any of these symptoms occur. PRECAUTIONS - Hyperammonemia
Since valproic acid products may produce CNS depression, especially when combined with another CNS depressant (e.g., alcohol), patients should be advised not to engage in hazardous activities, such as driving an automobile or operating dangerous machinery, until it is known that they do not become drowsy from the drug.
Patients should be instructed that a fever associated with other organ system involvement (rash, lymphadenopathy, etc.) may be drug-related and should be reported to the physician immediately (see ). PRECAUTIONS - Multi-organ Hypersensitivity Reaction
Drug Interactions
Effects of Co-Administered Drugs on Valproate Clearance
Drugs that affect the level of expression of hepatic enzymes, particularly those that elevate levels of glucuronosyltransferases, may increase the clearance of valproate. For example, phenytoin, carbamazepine, and phenobarbital (or primidone) can double the clearance of valproate. Thus, patients on monotherapy will generally have longer half-lives and higher concentrations than patients receiving polytherapy with antiepilepsy drugs.
In contrast, drugs that are inhibitors of cytochrome P450 isozymes, e.g., antidepressants, may be expected to have little effect on valproate clearance because cytochrome P450 microsomal mediated oxidation is a relatively minor secondary metabolic pathway compared to glucuronidation and beta-oxidation.
Because of these changes in valproate clearance, monitoring of valproate and concomitant drug concentrations should be increased whenever enzyme inducing drugs are introduced or withdrawn.
The following list provides information about the potential for an influence of several commonly prescribed medications on valproate pharmacokinetics. The list is not exhaustive nor could it be, since new interactions are continuously being reported.
Drugs for Which a Potentially Important Interaction Has Been Observed
Aspirin
A study involving the co-administration of aspirin at antipyretic doses (11 to 16 mg/kg) with valproate to pediatric patients (n = 6) revealed a decrease in protein binding and an inhibition of metabolism of valproate. Valproate free fraction was increased 4-fold in the presence of aspirin compared to valproate alone. The ß-oxidation pathway consisting of 2-E-valproic acid, 3-OH-valproic acid, and 3-keto valproic acid was decreased from 25% of total metabolites excreted on valproate alone to 8.3% in the presence of aspirin. Caution should be observed if valproate and aspirin are to be co-administered.
Felbamate
A study involving the co-administration of 1200 mg/day of felbamate with valproate to patients with epilepsy (n = 10) revealed an increase in mean valproate peak concentration by 35% (from 86 to 115 μg/mL) compared to valproate alone. Increasing the felbamate dose to 2400 mg/day increased the mean valproate peak concentration to 133 μg/mL (another 16% increase). A decrease in valproate dosage may be necessary when felbamate therapy is initiated.
Carbapenem Antibiotics
A clinically significant reduction in serum valproic acid concentration has been reported in patients receiving carbapenem antibiotics (ertapenem, imipenem, meropenem) and may result in loss of seizure control. The mechanism of this interaction is not well understood. Serum valproic acid concentrations should be monitored frequently after initiating carbapenem therapy. Alternative antibacterial or anticonvulsant therapy should be considered if serum valproic acid concentrations drop significantly or seizure control deteriorates (See ). WARNINGS
Drugs for Which Either No Interaction or a Likely Clinically Unimportant Interaction Has Been Observed
Antacids
A study involving the co-administration of valproate 500 mg with commonly administered antacids (Maalox, Trisogel, and Titralac - 160 mEq doses) did not reveal any effect on the extent of absorption of valproate.
Chlorpromazine
A study involving the administration of 100 to 300 mg/day of chlorpromazine to schizophrenic patients already receiving valproate (200 mg BID) revealed a 15% increase in trough plasma levels of valproate.
Effects of Valproate on Other Drugs
Valproate has been found to be a weak inhibitor of some P450 isozymes, epoxide hydrase, and glucuronyltransferases.
The following list provides information about the potential for an influence of valproate coadministration on the pharmacokinetics or pharmacodynamics of several commonly prescribed medications. The list is not exhaustive, since new interactions are continuously being reported.
Drugs for Which a Potentially Important Valproate Interaction Has Been Observed
Amitriptyline/Nortriptyline
Administration of a single oral 50 mg dose of amitriptyline to 15 normal volunteers (10 males and 5 females) who received valproate (500 mg BID) resulted in a 21% decrease in plasma clearance of amitriptyline and a 34% decrease in the net clearance of nortriptyline. Rare postmarketing reports of concurrent use of valproate and amitriptyline resulting in an increased amitriptyline level have been received. Concurrent use of valproate and amitriptyline has rarely been associated with toxicity. Monitoring of amitriptyline levels should be considered for patients taking valproate concomitantly with amitriptyline. Consideration should be given to lowering the dose of amitriptyline/nortriptyline in the presence of valproate.
Carbamazepine/carbamazepine-10,11-Epoxide
Serum levels of carbamazepine (CBZ) decreased 17% while that of carbamazepine-10,11-epoxide (CBZ-E) increased by 45% upon coadministration of valproate and CBZ to epileptic patients.
Clonazepam
The concomitant use of valproic acid and clonazepam may induce absence status in patients with a history of absence type seizures.
Diazepam
Valproate displaces diazepam from its plasma albumin binding sites and inhibits its metabolism. Co-administration of valproate (1500 mg daily) increased the free fraction of diazepam (10 mg) by 90% in healthy volunteers (n = 6). Plasma clearance and volume of distribution for free diazepam were reduced by 25% and 20%, respectively, in the presence of valproate. The elimination half-life of diazepam remained unchanged upon addition of valproate.
Ethosuximide
Valproate inhibits the metabolism of ethosuximide. Administration of a single ethosuximide dose of 500 mg with valproate (800 to 1600 mg/day) to healthy volunteers (n = 6) was accompanied by a 25% increase in elimination half-life of ethosuximide and a 15% decrease in its total clearance as compared to ethosuximide alone. Patients receiving valproate and ethosuximide, especially along with other anticonvulsants, should be monitored for alterations in serum concentrations of both drugs.
Lamotrigine
In a steady-state study involving 10 healthy volunteers, the elimination half-life of lamotrigine increased from 26 to 70 hours with valproate co-administration (a 165% increase). The dose of lamotrigine should be reduced when co-administered with valproate. Serious skin reactions (such as Stevens-Johnson Syndrome and toxic epidermal necrolysis) have been reported with concomitant lamotrigine and valproate administration. See lamotrigine package insert for details on lamotrigine dosing with concomitant valproate administration.
Phenobarbital
Valproate was found to inhibit the metabolism of phenobarbital. Co-administration of valproate (250 mg BID for 14 days) with phenobarbital to normal subjects (n = 6) resulted in a 50% increase in half-life and a 30% decrease in plasma clearance of phenobarbital (60 mg single-dose). The fraction of phenobarbital dose excreted unchanged increased by 50% in presence of valproate.
There is evidence for severe CNS depression, with or without significant elevations of barbiturate or valproate serum concentrations. All patients receiving concomitant barbiturate therapy should be closely monitored for neurological toxicity. Serum barbiturate concentrations should be obtained, if possible, and the barbiturate dosage decreased, if appropriate.
Primidone, which is metabolized to a barbiturate, may be involved in a similar interaction with valproate.
Phenytoin
Valproate displaces phenytoin from its plasma albumin binding sites and inhibits its hepatic metabolism. Co-administration of valproate (400 mg TID) with phenytoin (250 mg) in normal volunteers (n = 7) was associated with a 60% increase in the free fraction of phenytoin. Total plasma clearance and apparent volume of distribution of phenytoin increased 30% in the presence of valproate. Both the clearance and apparent volume of distribution of free phenytoin were reduced by 25%.
In patients with epilepsy, there have been reports of breakthrough seizures occurring with the combination of valproate and phenytoin. The dosage of phenytoin should be adjusted as required by the clinical situation.
Tolbutamide
From in vitro experiments, the unbound fraction of tolbutamide was increased from 20% to 50% when added to plasma samples taken from patients treated with valproate. The clinical relevance of this displacement is unknown.
Topiramate
Concomitant administration of valproic acid and topiramate has been associated with hyperammonemia with and without encephalopathy (see and and and ). Concomitant administration of topiramate with valproic acid has also been associated with hypothermia in patients who have tolerated either drug alone. It may be prudent to examine blood ammonia levels in patients in whom the onset of hypothermia has been reported (see and ). CONTRAINDICATIONSWARNINGS - Urea Cycle DisordersPRECAUTIONS - Hyperammonemia- Hyperammonemia and Encephalopathy Associated with Concomitant Topiramate UsePRECAUTIONS - HypothermiaHyperammonemia
Drugs for Which Either No Interaction or a Likely Clinically Unimportant Interaction Has Been Observed
Acetaminophen
Valproate had no effect on any of the pharmacokinetic parameters of acetaminophen when it was concurrently administered to three epileptic patients.
Clozapine
In psychotic patients (n = 11), no interaction was observed when valproate was coadministered with clozapine.
Lithium
Co-administration of valproate (500 mg BID) and lithium carbonate (300 mg TID) to normal male volunteers (n = 16) had no effect on the steady-state kinetics of lithium.
Carcinogenesis, mutagenesis, impairment of fertility
Carcinogenesis
Valproic acid was administered orally to Sprague Dawley rats and ICR (HA/ICR) mice at doses of 80 and 170 mg/kg/day (approximately 10 to 50% of the maximum human daily dose on a mg/m basis) for two years. A variety of neoplasms were observed in both species. The chief findings were a statistically significant increase in the incidence of subcutaneous fibrosarcomas in high dose male rats receiving valproic acid and a statistically significant dose-related trend for benign pulmonary adenomas in male mice receiving valproic acid. The significance of these findings for humans is unknown. 2
Mutagenesis
Valproate was not mutagenic in an in vitro bacterial assay (Ames test), did not produce dominant lethal effects in mice, and did not increase chromosome aberration frequency in an in vivo cytogenetic study in rats. Increased frequencies of sister chromatid exchange (SCE) have been reported in a study of epileptic children taking valproate, but this association was not observed in another study conducted in adults. There is some evidence that increased SCE frequencies may be associated with epilepsy. The biological significance of an increase in SCE frequency is not known.
Fertility
Chronic toxicity studies in juvenile and adult rats and dogs demonstrated reduced spermatogenesis and testicular atrophy at oral doses of 400 mg/kg/day or greater in rats (approximately equivalent to or greater than the maximum human daily dose on a mg/m basis) and 150 mg/kg/day or greater in dogs (approximately 1.4 times the maximum human daily dose or greater on a mg/m basis). Segment I fertility studies in rats have shown oral doses up to 350 mg/kg/day (approximately equal to the maximum human daily dose on a mg/m basis) for 60 days to have no effect on fertility. THE EFFECT OF VALPROATE ON TESTICULAR DEVELOPMENT AND ON SPERM PRODUCTION AND FERTILITY IN HUMANS IS UNKNOWN. 222
Pregnancy
Pregnancy Category D: See . WARNINGS
To provide information regarding the effects of exposure to valproic acid, healthcare providers are advised to recommend that pregnant patients taking valproic acid enroll in the NAAED Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/. in utero
Nursing mothers
Valproate is excreted in breast milk. Concentrations in breast milk have been reported to be 1-10% of serum concentrations. It is not known what effect this would have on a nursing infant. Consideration should be given to discontinuing nursing when valproic acid is administered to a nursing woman.
Pediatric use
Experience has indicated that pediatric patients under the age of two years are at a considerably increased risk of developing fatal hepatotoxicity, especially those with the aforementioned conditions (see ). When valproic acid is used in this patient group, it should be used with extreme caution and as a sole agent. The benefits of therapy should be weighed against the risks. Above the age of 2 years, experience in epilepsy has indicated that the incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups. BOXED WARNING
Younger children, especially those receiving enzyme-inducing drugs, will require larger maintenance doses to attain targeted total and unbound valproic acid concentrations.
The variability in free fraction limits the clinical usefulness of monitoring total serum valproic acid concentrations. Interpretation of valproic acid concentrations in children should include consideration of factors that affect hepatic metabolism and protein binding.
The basic toxicology and pathologic manifestations of valproate sodium in neonatal (4-day old) and juvenile (14-day old) rats are similar to those seen in young adult rats. However, additional findings, including renal alterations in juvenile rats and renal alterations and retinal dysplasia in neonatal rats, have been reported. These findings occurred at 240 mg/kg/day, a dosage approximately equivalent to the human maximum recommended daily dose on a mg/m basis. They were not seen at 90 mg/kg, or 40% of the maximum human daily dose on a mg/m basis. 22
Geriatric use
No patients above the age of 65 years were enrolled in double-blind prospective clinical trials of mania associated with bipolar illness. In a case review study of 583 patients, 72 patients (12%) were greater than 65 years of age. A higher percentage of patients above 65 years of age reported accidental injury, infection, pain, somnolence, and tremor. Discontinuation of valproate was occasionally associated with the latter two events. It is not clear whether these events indicate additional risk or whether they result from preexisting medical illness and concomitant medication use among these patients.
A study of elderly patients with dementia revealed drug related somnolence and discontinuation for somnolence (see ). The starting dose should be reduced in these patients, and dosage reductions or discontinuation should be considered in patients with excessive somnolence (see ). WARNINGS - Somnolence in the ElderlyDOSAGE AND ADMINISTRATION
-
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Hi-Tech Pharmacal Co., Inc. at 1-800-262-9010 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Epilepsy
The data described in the following section were obtained using divalproex sodium tablets.
Based on a placebo-controlled trial of adjunctive therapy for treatment of complex partial seizures, divalproex sodium was generally well tolerated with most adverse events rated as mild to moderate in severity. Intolerance was the primary reason for discontinuation in the divalproex sodium-treated patients (6%), compared to 1% of placebo-treated patients.
Table 2 lists treatment-emergent adverse events which were reported by ≥ 5% of divalproex sodium-treated patients and for which the incidence was greater than in the placebo group, in a placebo-controlled trial of adjunctive therapy for the treatment of complex partial seizures. Since patients were also treated with other antiepilepsy drugs, it is not possible, in most cases, to determine whether the following adverse events can be ascribed to divalproex sodium alone, or the combination of divalproex sodium and other antiepilepsy drugs.
Table 2
≥ Adverse Events Reported by5% of Patients Treated
with Divalproex Sodium During Placebo-Controlled Trial of
Adjunctive Therapy for Complex Partial SeizuresBody System/Even Divalproex Sodium (%)
(n = 77)Placebo (%)
(n = 70)Body as a Whole Headache 31 21 Asthenia 27 7 Fever 6 4 Gastrointestinal System Nausea 48 14 Vomiting 27 7 Abdominal Pain 23 6 Diarrhea 13 6 Anorexia 12 0 Dyspepsia 8 4 Constipation 5 1 Nervous System Somnolence 27 11 Tremor 25 6 Dizziness 25 13 Diplopia 16 9 Amblyopia/Blurred Vision 12 9 Ataxia 8 1 Nystagmus 8 1 Emotional Lability 6 4 Thinking Abnormal 6 0 Amnesia 5 1 Respiratory System Flu Syndrome 12 9 Infection 12 6 Bronchitis 5 1 Rhinitis 5 4 Other Alopecia 6 1 Weight Loss 6 0 Table 3 lists treatment-emergent adverse events which were reported by ≥ 5% of patients in the high dose divalproex sodium group, and for which the incidence was greater than in the low dose group, in a controlled trial of divalproex sodium monotherapy treatment of complex partial seizures. Since patients were being titrated off another antiepilepsy drug during the first portion of the trial, it is not possible, in many cases, to determine whether the following adverse events can be ascribed to divalproex sodium alone, or the combination of divalproex sodium and other antiepilepsy drugs.
- *
- 1 Headache was the only adverse event that occurred in ≥ 5% of patients in the high dose group and at an equal or greater incidence in the low dose group.
Table 3
≥ Adverse Events Reported by5% of Patients in the High Dose
Group in the Controlled Trial of Divalproex Sodium Monotherapy for
Complex Partial Seizures 1*Body System/Event High Dose (%)
(n = 131)Low Dose (%)
(n = 134)Body as a Whole Asthenia 21 10 Digestive System Nausea 34 26 Diarrhea 23 19 Vomiting 23 15 Abdominal Pain 12 9 Anorexia 11 4 Dyspepsia 11 10 Hemic/Lymphatic System Thrombocytopenia 24 1 Ecchymosis 5 4 Metabolic/Nutritional Weight Gain 9 4 Peripheral Edema 8 3 Nervous System Tremor 57 19 Somnolence 30 18 Dizziness 18 13 Insomnia 15 9 Nervousness 11 7 Amnesia 7 4 Nystagmus 7 1 Depression 5 4 Respiratory System Infection 20 13 Pharyngitis 8 2 Dyspnea 5 1 Skin and Appendages Alopecia 24 13 Special Senses Amblyopia/Blurred Vision 8 4 Tinnitus 7 1 The following additional adverse events were reported by greater than 1% but less than 5% of the 358 patients treated with divalproex sodium in the controlled trials of complex partial seizures:
Digestive System:
Increased appetite, flatulence, hematemesis, eructation, pancreatitis, periodontal abscess.
Other Patient Populations
Adverse events that have been reported with all dosage forms of valproate from epilepsy trials, spontaneous reports, and other sources are listed below by body system.
Gastrointestinal:
The most commonly reported side effects at the initiation of therapy are nausea, vomiting, and indigestion. These effects are usually transient and rarely require discontinuation of therapy. Diarrhea, abdominal cramps, and constipation have been reported. Both anorexia with some weight loss and increased appetite with weight gain have also been reported. The administration of delayed-release divalproex sodium may result in reduction of gastrointestinal side effects in some patients.
CNS Effects:
Sedative effects have occurred in patients receiving valproate alone but occur most often in patients receiving combination therapy. Sedation usually abates upon reduction of other antiepileptic medication. Tremor (may be dose-related), hallucinations, ataxia, headache, nystagmus, diplopia, asterixis, "spots before eyes", dysarthria, dizziness, confusion, hypesthesia, vertigo, incoordination, and Parkinsonism have been reported with the use of valproate. Rare cases of coma have occurred in patients receiving valproate alone or in conjunction with phenobarbital. In rare instances encephalopathy with or without fever has developed shortly after the introduction of valproate monotherapy without evidence of hepatic dysfunction or inappropriately high plasma valproate levels. Although recovery has been described following drug withdrawal, there have been fatalities in patients with hyperammonemic encephalopathy, particularly in patients with underlying urea cycle disorders (see and ). WARNINGS - Urea Cycle DisordersPRECAUTIONS
Several reports have noted reversible cerebral atrophy and dementia in association with valproate therapy.
Dermatologic:
Transient hair loss, skin rash, photosensitivity, generalized pruritus, erythema multiforme, and Stevens-Johnson syndrome. Rare cases of toxic epidermal necrolysis have been reported including a fatal case in a 6 month old infant taking valproate and several other concomitant medications. An additional case of toxic epidermal necrosis resulting in death was reported in a 35 year old patient with AIDS taking several concomitant medications and with a history of multiple cutaneous drug reactions. Serious skin reactions have been reported with concomitant administration of lamotrigine and valproate (see ). PRECAUTIONS - Drug Interactions
Psychiatric:
Emotional upset, depression, psychosis, aggression, hyperactivity, hostility, and behavioral deterioration.
Hematologic:
Thrombocytopenia and inhibition of the secondary phase of platelet aggregation may be reflected in altered bleeding time, petechiae, bruising, hematoma formation, epistaxis, and frank hemorrhage (see and ). Relative lymphocytosis, macrocytosis, hypofibrinogenemia, leukopenia, eosinophilia, anemia including macrocytic with or without folate deficiency, bone marrow suppression, pancytopenia, aplastic anemia, agranulocytosis, and acute intermittent porphyria. PRECAUTIONS - GeneralDrug Interactions
Hepatic:
Minor elevations of transaminases (e.g., SGOT and SGPT) and LDH are frequent and appear to be dose-related. Occasionally, laboratory test results include increases in serum bilirubin and abnormal changes in other liver function tests. These results may reflect potentially serious hepatotoxicity (see ). WARNINGS
Endocrine:
Irregular menses, secondary amenorrhea, breast enlargement, galactorrhea, and parotid gland swelling. Abnormal thyroid function tests (see ). PRECAUTIONS
There have been rare spontaneous reports of polycystic ovary disease. A cause and effect relationship has not been established.
Metabolic:
Hyperammonemia (see ), hyponatremia, and inappropriate ADH secretion. PRECAUTIONS
There have been rare reports of Fanconi's syndrome occurring chiefly in children.
Decreased carnitine concentrations have been reported although the clinical relevance is undetermined.
Hyperglycinemia has occurred and was associated with a fatal outcome in a patient with preexistent nonketotic hyperglycemia.
Mania
Although valproic acid has not been evaluated for safety and efficacy in the treatment of manic episodes associated with bipolar disorder, the following adverse events not listed above were reported by 1% or more of patients from two placebo-controlled clinical trials of divalproex sodium tablets.
-
OVERDOSAGE
Overdosage with valproate may result in somnolence, heart block, and deep coma. Fatalities have been reported; however, patients have recovered from valproate levels as high as 2120 μg/mL.
In overdose situations, the fraction of drug not bound to protein is high and hemodialysis or tandem hemodialysis plus hemoperfusion may result in significant removal of drug. The benefit of gastric lavage or emesis will vary with the time since ingestion. General supportive measures should be applied with particular attention to the maintenance of adequate urinary output.
Naloxone has been reported to reverse the CNS depressant effects of valproate overdosage. Because naloxone could theoretically also reverse the antiepileptic effects of valproate, it should be used with caution in patients with epilepsy.
-
DOSAGE AND ADMINISTRATION
Valproic acid is administered orally. Valproic acid is indicated as monotherapy and adjunctive therapy in complex partial seizures in adults and pediatric patients down to the age of 10 years, and in simple and complex absence seizures. As the valproic acid dosage is titrated upward, concentrations of phenobarbital, carbamazepine, and/or phenytoin may be affected (see ). PRECAUTIONS - Drug Interactions
Monotherapy (Initial Therapy):
Valproic acid has not been systematically studied as initial therapy. Patients should initiate therapy at 10 to 15 mg/kg/day. The dosage should be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 μg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made.
The probability of thrombocytopenia increases significantly at total trough valproate plasma concentrations above 110 μg/mL in females and 135 μg/mL in males. The benefit of improved seizure control with higher doses should be weighed against the possibility of a greater incidence of adverse reactions.
Conversion to Monotherapy:
Patients should initiate therapy at 10 to 15 mg/kg/day. The dosage should be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 μg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made. Concomitant antiepilepsy drug (AED) dosage can ordinarily be reduced by approximately 25% every 2 weeks. This reduction may be started at initiation of valproic acid therapy, or delayed by 1 to 2 weeks if there is a concern that seizures are likely to occur with a reduction. The speed and duration of withdrawal of the concomitant AED can be highly variable, and patients should be monitored closely during this period for increased seizure frequency.
Adjunctive Therapy:
Valproic acid may be added to the patient's regimen at a dosage of 10 to 15 mg/kg/day. The dosage may be increased by 5 to 10 mg/kg/week to achieve optimal clinical response. Ordinarily, optimal clinical response is achieved at daily doses below 60 mg/kg/day. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the usually accepted therapeutic range (50 to 100 μg/mL). No recommendation regarding the safety of valproate for use at doses above 60 mg/kg/day can be made. If the total daily dose exceeds 250 mg, it should be given in divided doses.
In a study of adjunctive therapy for complex partial seizures in which patients were receiving either carbamazepine or phenytoin in addition to divalproex sodium tablets, no adjustment of carbamazepine or phenytoin dosage was needed (see ). However, since valproate may interact with these or other concurrently administered AEDs as well as other drugs (see ), periodic plasma concentration determinations of concomitant AEDs are recommended during the early course of therapy (see ). CLINICAL STUDIESDrug InteractionsPRECAUTIONS - Drug Interactions
Simple and Complex Absence Seizures:
The recommended initial dose is 15 mg/kg/day, increasing at one week intervals by 5 to 10 mg/kg/day until seizures are controlled or side effects preclude further increases. The maximum recommended dosage is 60 mg/kg/day. If the total daily dose exceeds 250 mg, it should be given in divided doses.
A good correlation has not been established between daily dose, serum concentrations, and therapeutic effect. However, therapeutic valproate serum concentrations for most patients with absence seizures is considered to range from 50 to 100 μg/mL. Some patients may be controlled with lower or higher serum concentrations (see ). CLINICAL PHARMACOLOGY
As the valproic acid dosage is titrated upward, blood concentrations of phenobarbital and/or phenytoin may be affected (see ). PRECAUTIONS
Antiepilepsy drugs should not be abruptly discontinued in patients in whom the drug is administered to prevent major seizures because of the strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life.
The following table is a guide for the initial daily dose of valproic acid (15 mg/kg/day):
(Kg) (Lb) Weight
Dose (mg) Total
Daily
of Oral Solution Number of Teaspoonfuls
Dose 1 Dose 2 Dose 3 10 - 24.9 22 - 54.9 250 0 0 1 25 - 39.9 55 - 87.9 500 1 0 1 40 - 59.9 88 - 131.9 750 1 1 1 60 - 74.9 132 - 164.9 1,000 1 1 2 75 - 89.9 165 - 197.9 1,250 2 1 2 General Dosing Advice
Dosing in Elderly Patients
Due to a decrease in unbound clearance of valproate and possibly a greater sensitivity to somnolence in the elderly, the starting dose should be reduced in these patients. Dosage should be increased more slowly and with regular monitoring for fluid and nutritional intake, dehydration, somnolence, and other adverse events. Dose reductions or discontinuation of valproate should be considered in patients with decreased food or fluid intake and in patients with excessive somnolence. The ultimate therapeutic dose should be achieved on the basis of both tolerability and clinical response (see ). WARNINGS
Dose-Related Adverse Events
The frequency of adverse effects (particularly elevated liver enzymes and thrombocytopenia) may be dose-related. The probability of thrombocytopenia appears to increase significantly at total valproate concentrations of ≥ 110 μg/mL (females) or ≥ 135 μg/mL (males) (see ). The benefit of improved therapeutic effect with higher doses should be weighed against the possibility of a greater incidence of adverse reactions. PRECAUTIONS
-
PATIENT INFORMATION LEAFLET
Important Information for Women Who Could Become Pregnant About the Use of Valproic Acid Oral Solution, USP
Please read this leaflet carefully before you take valproic acid oral solution, USP. This leaflet provides a summary of important information about taking valproic acid oral solution, USP to women who could become pregnant. If you have any questions or concerns, or want more information about valproic acid oral solution, USP, contact your doctor or pharmacist.
Information for Women Who Could Become Pregnant
Valproic acid oral solution, USP can be obtained only by prescription from your doctor. The decision to use valproic acid oral solution, USP is one that you and your doctor should make together, taking into account your individual needs and medical condition.
Before using valproic acid oral solution, USP, women who can become pregnant should consider the fact that these medications have been associated with birth defects, in particular, with spina bifida and other defects related to failure of the spinal canal to close normally. Approximately 1 to 2% of children born to women with epilepsy taking divalproex sodium in the first 12 weeks of pregnancy had these defects (based on data from the Centers for Disease Control, a U.S. agency based in Atlanta). The incidence in the general population is 0.1 to 0.2%.
Valproic acid oral solution, USP has also been associated with other birth defects such as defects of the heart, the bones, and other parts of the body. Information suggests that birth defects may be more likely to occur with these medications than some other drugs that treat your medical condition.
Information for Women Who Are Planning to Get Pregnant
- Women taking valproic acid oral solution, USP who are planning to get pregnant should discuss the treatment options with their doctor.
Information for Women Who Become Pregnant
- If you become pregnant while taking valproic acid oral solution, USP you should contact your doctor immediately.
Other Important Information
- Valproic acid oral solution, USP should be taken exactly as prescribed by your doctor to get the most benefit from your medication and reduce the risk of side effects.
- If you have taken more than the prescribed dose of valproic acid oral solution, USP, contact your hospital emergency room or local poison center immediately.
- Valproic acid oral solution, USP was prescribed for your particular condition. Do not use it for another condition or give the drug to others.
Facts About Birth Defects
It is important to know that birth defects may occur even in children of individuals not taking any medications or without any additional risk factors.
This summary provides important information about the use of valproic acid oral solution, USP to women who could become pregnant. If you would like more information about the other potential risks and benefits of valproic acid oral solution, USP, ask your doctor or pharmacist to let you read the professional labeling and then discuss it with them. If you have any questions or concerns about taking valproic acid oral solution, USP, you should discuss them with your doctor.
Call your doctor for medical advice about side effects. You may report side effects to Hi-Tech Pharmacal Co., Inc. at 1-800-262-9010 or FDA at 1-800-FDA-1088.
DISTRIBUTED BY:
ATLANTIC BIOLOGICALS CORP.
MIAMI, FL 33179
-
Medication Guide
Valproic Acid Oral Solution, USP
(val • pro • ic acid)
Revised 06/2022
Read this Medication Guide before you start taking Valproic Acid Oral Solution, USP and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about Valproic Acid Oral Solution, USP?
Do not stop taking Valproic Acid Oral Solution, USP without first talking to your healthcare provider.
Stopping Valproic Acid Oral Solution, USP suddenly can cause serious problems.
Valproic Acid Oral Solution, USP can cause serious side effects, including:
1.Serious liver damage that can cause death, especially in children younger than 2 years old.The risk of getting this serious liver damage is more likely to happen within the first 6 months of treatment.
Call your healthcare provider right away if you get any of thefollowing symptoms:
•nausea or vomiting that does not go away•loss of appetite•pain on the right side of your stomach (abdomen)•dark urine•swelling of your face•yellowing of your skin or the whites of your eyes
In some cases, liver damage may continue despite stopping the drug.
1.Valproic Acid Oral Solution, USP may harm your unborn baby.2.If you take Valproic Acid Oral Solution, USP during pregnancy for any medical condition, your baby is at risk for serious birth defects that affect the brain and spinal cord and are called spina bifida or neural tube defects. These defects occur in 1 to 2 out of every 100 babies born to mothers who use this medicine during pregnancy. These defects can begin in the first month, even before you know you are pregnant. Other birth defects that affect the structures of the heart, head, arms, legs, and the opening where the urine comes out (urethra) on the bottom of the penis can also happen. Decreased hearing or hearing loss can also happen.3.Birth defects may occur even in children born to women who are not taking any medicines and do not have other risk factors.4.Taking folic acid supplements before getting pregnant and during early pregnancy can lower the chance of having a baby with a neural tube defect.5.If you take Valproic Acid Oral Solution, USP during pregnancy for any medical condition, your child is at risk for having a lower IQ and may be at risk for developing autism or attention deficit/hyperactivity disorder.6.There may be other medicines to treat your condition that have a lower chance of causing birth defects, decreased IQ, or other disorders in your child.7.Women who are pregnant must not take Valproic Acid Oral Solution, USP to prevent migraine headaches.8.All women of childbearing age (including girls from the start of puberty) should talk to their healthcare provider about using other possible treatments instead of Valproic Acid Oral Solution, USP. If the decision is made to use Valproic Acid Oral Solution, USP, you should use effective birth control (contraception).9.Tell your healthcare provider right away if you become pregnant while taking Valproic Acid Oral Solution, USP. You and your healthcare provider should decide if you will continue to take Valproic Acid Oral Solution, USP while you are pregnant.10.Pregnancy Registry: If you become pregnant while taking Valproic Acid Oral Solution, USP, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling toll-free 1-888-233-2334 or by visiting the website, http://www.aedpregnancyregistry.org/. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy.11.Inflammation of your pancreas that can cause death.
Call your healthcare provider right away if you have any of these symptoms:
•severe stomach pain that you may also feel in your back•nausea or vomiting that does not go away•Like other antiepileptic drugs, Valproic Acid Oral Solution, USP, may cause suicidal thoughts or actions in avery small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
•thoughts about suicide or dying•attempts to commit suicide•new or worse depression•new or worse anxiety•feeling agitated or restless•panic attacks•trouble sleeping (insomnia)•new or worse irritability•acting aggressive, being angry, or violent•acting on dangerous impulses•an extreme increase in activity and talking (mania)•other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
•Pay attention to any changes, especially sudden changes in mood, behaviors, thoughts, or feelings.•Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Do not stop Valproic Acid Oral Solution, USP without first talking to a healthcare provider. Stopping Valproic Acid Oral Solution, USP suddenly can cause serious problems. Stopping a seizure medicine suddenly in a patient who has epilepsy can cause seizures that do not stop (status epilepticus).
Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
What is Valproic Acid Oral Solution, USP?
Valproic Acid Oral Solution, USP is prescription medicines used alone or with other medicines, to treat:
•complex partial seizures in adults and children 10 years of age and older•simple and complex absence seizures, with or without other seizure types
Who should not take Valproic Acid Oral Solution, USP?
Do not take Valproic Acid Oral Solution, USP if you:
•have liver problems•have or think you have a genetic liver problem caused by a mitochondrial disorder (e.g. Alpers-Huttenlocher syndrome)•are allergic to divalproex sodium, valproic acid, sodium valproate, or any of the ingredients in Valproic Acid Oral Solution, USP. See the end of this leaflet for a complete list of ingredients in Valproic Acid Oral Solution, USP.•have a genetic problem called urea cycle disorder•are taking it to prevent migraine headaches and are either pregnant or may become pregnant because you are not using effective birth control (contraception)
What should I tell my healthcare provider before taking Valproic Acid Oral Solution, USP?
Before you take Valproic Acid Oral Solution, USP, tell your healthcare provider if you:
•have a genetic liver problem caused by a mitochondrial disorder (e.g. Alpers-Huttenlocher syndrome)•drink alcohol•are pregnant or breastfeeding. Valproic Acid Oral Solution, USP can pass into breast milk. Talk to your healthcare provider about the best way to feed your baby if you take Valproic Acid Oral Solution, USP•have or have had depression, mood problems, or suicidal thoughts or behavior•have any other medical conditions
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, herbal supplements and medicines that you take for a short period of time.
Taking Valproic Acid Oral Solution, USP with certain other medicines can cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist each time you get a new medicine.
How should I take Valproic Acid Oral Solution, USP?
•Take Valproic Acid Oral Solution, USP exactly as your healthcare provider tells you. Your healthcare provider will tell you how much Valproic Acid Oral Solution, USP to take and when to take it.•Your healthcare provider may change your dose.•Do not change your dose of Valproic Acid Oral Solution, USP without talking to your healthcare provider.•Do not stop taking Valproic Acid Oral Solution, USP without first talking to your healthcare provider.Stopping Valproic Acid Oral Solution, USP suddenly can cause serious problems.•If you take too much Valproic Acid Oral Solution, USP, call your healthcare provider or local Poison Control Center right away.
What should I avoid while taking Valproic Acid Oral Solution, USP?
•Valproic Acid Oral Solution, USP can cause drowsiness and dizziness. Do not drink alcohol or take other medicines that make you sleepy or dizzy while taking Valproic Acid Oral Solution, USP, until you talk with your doctor. Taking Valproic Acid Oral Solution, USP with alcohol or drugs that cause sleepiness or dizziness may make your sleepiness or dizziness worse.•Do not drive a car or operate dangerous machinery until you know how Valproic Acid Oral Solution, USP affects you. Valproic Acid Oral Solution, USP can slow your thinking and motor skills.
What are the possible side effects of Valproic Acid Oral Solution, USP?
•See “What is the most important information I should know about Valproic Acid Oral Solution, USP?”
Valproic Acid Oral Solution, USP can cause other serious side effects including:
•Bleeding problems: red or purple spots on your skin, bruising, pain and swelling into your joints due to bleeding or bleeding from your mouth or nose.•High ammonia levels in your blood: feeling tired, vomiting, changes in mental status.•Low body temperature (hypothermia): drop in your body temperature to less than 95°F, feeling tired, confusion, coma.•Allergic (hypersensitivity) reactions: fever, skin rash, hives, sores in your mouth, skin blistering and peeling of your skin, swelling of your lymph nodes, swelling of your face, eyes, lips, tongue, or throat, trouble swallowing or breathing.•Drowsiness or sleepiness in the elderly.This extreme drowsiness may cause you to eat or drink less than you normally would. Tell your doctor if you are not able to eat or drink as you normally do. Your doctor may start you at a lower dose of Valproic Acid Oral Solution, USP.
Call your healthcare provider right away, if you have any of the symptoms listed above.
The common side effects of Valproic Acid Oral Solution, USP include:
•nausea•headache•sleepiness•vomiting•weakness•tremor•dizziness•stomach pain•blurry vision•double vision•diarrhea•increased appetite•weight gain•hair loss•loss of appetite•problems with walking or coordinationThese are not all of the possible side effects of Valproic Acid Oral Solution, USP. For more information, ask your healthcare provider or pharmacist.Tell your healthcare provider if you have any side effect that bothers you or that does not go away.Call your doctor for medical advice about side effects. You may report side effects to Akorn Operating Company LLC at 1-800-932-5676 or FDA at 1-800-FDA-1088.How should I store Valproic Acid Oral Solution, USP?Store Valproic Acid Oral Solution, USP below 86°F (30°C).Keep Valproic Acid Oral Solution, USP and all medicines out of the reach of children.General information about the safe and effective use of Valproic Acid Oral Solution, USPMedicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Valproic Acid Oral Solution, USP for a condition for which it was not prescribed. Do not give Valproic Acid Oral Solution, USP to other people, even if they have the same symptoms that you have. It may harm them.This Medication Guide summarizes the most important information about Valproic Acid Oral Solution, USP. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about Valproic Acid Oral Solution, USP that is written for health professionals.What are the ingredients in Valproic Acid Oral Solution, USP?Active ingredient: valproic acidInactive ingredients: FD&C Red No. 40, methylparaben, natural and artificial raspberry flavor, propylparaben, purified water, sodium hydroxide, sorbitol, and sucrose.This Medication Guide has been approved by the U.S. Food and Drug Administration.Dispense the accompanying Medication Guide to each patient.Distributed by:Akorn Operating Company LLCGurnee, ILRevised 06/2022
- VALPROIC ACID SOLUTION
-
INGREDIENTS AND APPEARANCE
VALPROIC ACID
valproic acid solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:17856-0792(NDC:50383-792) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VALPROIC ACID (UNII: 614OI1Z5WI) (VALPROIC ACID - UNII:614OI1Z5WI) VALPROIC ACID 250 mg in 5 mL Inactive Ingredients Ingredient Name Strength FD&C RED NO. 40 (UNII: WZB9127XOA) METHYLPARABEN (UNII: A2I8C7HI9T) RASPBERRY (UNII: 4N14V5R27W) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) SORBITOL (UNII: 506T60A25R) SUCROSE (UNII: C151H8M554) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:17856-0792-2 72 in 1 BOX, UNIT-DOSE 02/01/2023 11/29/2024 1 NDC:17856-0792-1 10 mL in 1 CUP; Type 0: Not a Combination Product 2 NDC:17856-0792-6 72 in 1 BOX, UNIT-DOSE 02/01/2023 11/29/2024 2 NDC:17856-0792-5 5 mL in 1 CUP; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074060 01/13/1995 Labeler - ATLANTIC BIOLOGICALS CORP. (047437707) Establishment Name Address ID/FEI Business Operations ATLANTIC BIOLOGICALS CORP. 047437707 repack(17856-0792)