Label: THIOTEPA injection, powder, lyophilized, for solution
- NDC Code(s): 65219-029-20
- Packager: Fresenius Kabi USA, LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated March 28, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use THIOTEPA FOR INJECTION safely and effectively. See full prescribing information for THIOTEPA FOR INJECTION.
THIOTEPA for injection, for intravenous, intracavitary, or intravesical use.
Initial U.S. Approval: 1959
WARNING: SEVERE MYELOSUPPRESSION, CARCINOGENICITY
See full prescribing information for complete boxed warning.
· May cause severe marrow suppression or ablation with resulting infection or bleeding. Monitor hematologic laboratory parameters [see Warnings and Precautions (5.1)]
· Potentially carcinogenic in humans [see Warnings and Precautions (5.7)]
INDICATIONS AND USAGE
Thiotepa for injection is an alkylating drug indicated:
• For treatment of adenocarcinoma of the breast or ovary. (1.2)
• For controlling intracavitary effusions secondary to diffuse or localized neoplastic diseases of various serosal cavities. (1.3)
• For treatment of superficial papillary carcinoma of the urinary bladder. (1.4)DOSAGE AND ADMINISTRATION
• The recommended dose of thiotepa for injection for treatment of adenocarcinoma of the breast or ovary is 0.3 to 0.4 mg/kg intravenously. (2.1)
• The recommended dose of thiotepa for injection for treatment of malignant effusions is 0.6 to 0.8 mg/kg intracavitary. (2.1)
• The recommended dose of thiotepa for injection for treatment of superficial papillary carcinoma of the urinary bladder is 60 mg in 30 to 60 mL of Sodium Chloride Injection into the bladder by catheter. (2.1)DOSAGE FORMS AND STRENGTHS
• For injection: 100 mg, lyophilized white powder in single-dose vial for reconstitution. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
The most common adverse reactions (incidence greater than 10%) were neutropenia, anemia, thrombocytopenia, elevated alanine aminotransferase, elevated aspartate aminotransferase, elevated bilirubin, mucositis, cytomegalovirus infection, hemorrhage, diarrhea, hematuria and rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
• Lactation: Breastfeeding is not recommended. (8.2)
• Moderate or severe renal impairment: Monitor patients more frequently for toxicity. (8.6, 12.2)
• Moderate or severe hepatic impairment: Monitor patients more frequently for toxicity. (8.7, 12.2)
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 2/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.2 Adenocarcinoma of the Breast or Ovary
1.3 Malignant Effusions
1.4 Superficial Papillary Carcinoma of the Urinary Bladder
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Preparation Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
5.2 Hypersensitivity
5.3 Cutaneous Toxicity
5.4 Concomitant Use of Live and Attenuated Vaccines
5.5 Hepatic Veno-Occlusive Disease
5.6 Central Nervous System Toxicity
5.7 Carcinogenicity
5.8 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effect of Cytochrome CYP3A Inhibitors and Inducers
7.2 Effect of Thiotepa on Cytochrome CYP2B6 Substrates
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SEVERE MYELOSUPPRESSION, CARCINOGENICITY
• Thiotepa may cause severe marrow suppression, and high doses may cause marrow ablation with resulting infection or bleeding. Monitor hematologic laboratory parameters. Hematopoietic progenitor (stem) cell transplantation (HSCT) is required to prevent potentially fatal complications of the prolonged myelosuppression after high doses of thiotepa [see Warnings and Precautions (5.1)]
• Thiotepa should be considered potentially carcinogenic in humans [see Warnings and Precautions (5.7)] -
1 INDICATIONS AND USAGE
1.2 Adenocarcinoma of the Breast or Ovary
Thiotepa for injection is indicated for treatment of adenocarcinoma of the breast or ovary.
1.3 Malignant Effusions
Thiotepa for injection is indicated for controlling intracavitary effusions secondary to diffuse or localized neoplastic diseases of various serosal cavities.
1.4 Superficial Papillary Carcinoma of the Urinary Bladder
Thiotepa for injection is indicated for treatment of superficial papillary carcinoma of the urinary bladder.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information. -
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Adenocarcinoma of the Breast or Ovary
The recommended dose of thiotepa for injection for treatment of adenocarcinoma of the breast or ovary is 0.3 to 0.4 mg/kg intravenously. Doses should be given at 1 to 4 week intervals. Initially the higher dose in the given range is commonly administered. The maintenance dose should be adjusted weekly on the basis of pretreatment control blood counts and subsequent blood counts. Maintenance doses should not be administered more frequently than weekly.
Malignant Effusions
The recommended dose of thiotepa for injection for treatment of malignant effusions is 0.6 to 0.8 mg/kg intracavitary. Administration is usually effected through the same tubing which is used to remove the fluid from the cavity involved. Doses should be given at 1 to 4 week intervals. Initially the higher dose in the given range is commonly administered. The maintenance dose should be adjusted weekly on the basis of pretreatment control blood counts and subsequent blood counts. Maintenance doses should not be administered more frequently than weekly.
Superficial Papillary Carcinoma of the Urinary Bladder
The recommended dose of thiotepa for injection for treatment of superficial papillary carcinoma of the urinary bladder is 60 mg in 30 to 60 mL of Sodium Chloride Injection into the bladder by catheter. The solution should be retained for 2 hours. If the patient finds it impossible to retain 60 mL for 2 hours, the dose may be given in a volume of 30 mL. The patient may be repositioned every 15 minutes for maximum area contact. The usual course of treatment is once a week for 4 weeks. The course may be repeated if necessary, but second and third courses must be given with caution since bone-marrow depression may be increased.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.2.2 Preparation Instructions
Thiotepa for injection is a cytotoxic drug. Follow applicable special handling and disposal procedures1.
Reconstitution
Reconstitute thiotepa for injection 100 mg with 10 ml of sterile water for injection. Using a syringe fitted with a needle, aseptically withdraw 10 ml of sterile water for injection. Inject the content of the syringe into the vial through the rubber stopper. Remove the syringe and needle, and mix manually by repeated inversions.
The reconstituted solution is hypotonic and must be diluted in saline prior to administration. Reconstituted solutions, free of visible particulate matter, may occasionally show opalescence; such solutions can still be used for further dilution.
If not used immediately after reconstitution, the product is stable for 8 hours when stored at 2°C to 8°C (36° to 46°F).
Dilution in the infusion bag
Prior to administration, dilute the reconstituted solution further with an appropriate volume of sodium chloride 0.9% solution for injection to obtain a final thiotepa for injection concentration between 0.5 and 1 mg/mL. Dilute thiotepa for injection as recommended in Table 2.
Table 2: Dilution of Thiotepa for Injection in the infusion bag
Calculated Thiotepa for Injection Dose
Dilution Volume (Sodium Chloride 0.9% solution for injection)
Less than 250 mg
Appropriate volume to obtain a final concentration of 0.5 to 1 mg/mL
250 mg to 500 mg
500 mL or appropriate volume to obtain a final concentration of 0.5 to 1 mg/mL
Greater than 500 mg
1000 mL or appropriate volume to obtain a final concentration of 0.5 to 1 mg/mL
After dilution the product is stable for 24 hours when stored at 2°C to 8°C (36° to 46°F) and for 4 hours when stored at 25°C (77°F). From a microbiological point of view, the product should be used immediately.
Inspect the diluted solution visually for particulate matter and discoloration prior to administration. Use thiotepa for injection diluted solutions only if free of visible particulate matter. Filter using a 0.2 micron filter prior to administration. Filtering does not alter solution potency - 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Thiotepa for injection is contraindicated in:
• Patients with severe hypersensitivity to thiotepa [see Warnings and Precautions (5.2)]
• Concomitant use with live or attenuated vaccines [see Warnings and Precautions (5.4)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
The consequence of treatment with high doses of thiotepa together with other chemotherapy is profound myelosuppression occurring in all patients. Monitor complete blood counts, and provide supportive care for infections, anemia and thrombocytopenia until there is adequate hematopoietic recovery.
For patients receiving thiotepa for treatment of adenocarcinoma of the breast, adenocarcinoma of the ovary, malignant effusions and superficial papillary carcinoma of the urinary bladder, if the bone marrow has been compromised by prior irradiation or chemotherapy, or is recovering from chemotherapy, the risk of severe myelosuppression with thiotepa may be increased. Perform periodic complete blood counts during the course of treatment with thiotepa. Provide supportive care for infections, bleeding, and symptomatic anemia [see Adverse Reactions (6.1)].
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.
5.2 Hypersensitivity
Clinically significant hypersensitivity reactions, including anaphylaxis, have occurred following administration of thiotepa. If anaphylactic or other clinically significant allergic reaction occurs, discontinue treatment with thiotepa, initiate appropriate therapy, and monitor until signs and symptoms resolve [see Contraindications (4), Adverse Reactions (6.1)].
5.3 Cutaneous Toxicity
Thiotepa and/or its active metabolites may be excreted in part via skin patients receiving high-dose therapy. Treatment with thiotepa may cause skin discoloration, pruritus, blistering, desquamation, and peeling that may be more severe in the groin, axillae, skin folds, in the neck area, and under dressings. Instruct patients to shower or bathe with water at least twice daily through 48 hours after administration of thiotepa. Change occlusive dressing and clean the covered skin at least twice daily through 48 hours after administration of thiotepa. Change bed sheets daily during treatment.
Skin reactions associated with accidental exposure to thiotepa may also occur. Wash the skin thoroughly with soap and water in case thiotepa solution contacts the skin. Flush mucous membranes in case of thiotepa contact with mucous membranes.5.4 Concomitant Use of Live and Attenuated Vaccines
Do not administer live or attenuated viral or bacterial vaccines to a patient treated with thiotepa until the immunosuppressive effects have resolved.
5.5 Hepatic Veno-Occlusive Disease
Hepatic veno-occlusive disease may occur in patients who have received high-dose thiotepa in conjunction with busulfan and cyclophosphamide. Monitor by physical examination, serum transaminases and bilirubin and provide supportive care to patients who develop hepatic veno-occlusive disease.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.
5.6 Central Nervous System Toxicity
Fatal encephalopathy has occurred in patients treated with high doses of thiotepa. Other central nervous system toxicities, such as headache, apathy, psychomotor retardation, disorientation, confusion, amnesia, hallucinations, drowsiness, somnolence, seizures, coma, inappropriate behaviour and forgetfulness have been reported to occur in a dose-dependent manner during or shortly after administration of high-dose thiotepa. Do not exceed the recommended dose of thiotepa. If severe or life-threatening central nervous system toxicity occurs, discontinue administration of thiotepa and provide supportive care.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.5.7 Carcinogenicity
Like many alkylating agents, thiotepa has been reported to be carcinogenic when administered to laboratory animals [see Nonclinical Toxicity (13.1)]. Carcinogenicity is shown most clearly in studies using mice, but there is some evidence of carcinogenicity in man. There is an increased risk of a secondary malignancy with use of thiotepa.
5.8 Embryo-Fetal Toxicity
Based on the mechanism of action and findings in animals, thiotepa can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of thiotepa in pregnant women. Thiotepa given by the intraperitoneal (IP) route was teratogenic in mice at doses ≥ 1 mg/kg (3.2 mg/m2), approximately 8-fold less than the maximum recommended human therapeutic dose (0.8 mg/kg, 27 mg/m2), based on body-surface area. Thiotepa given by the IP route was teratogenic in rats at doses ≥ 3 mg/kg (21 mg/m2), approximately equal to the maximum recommended human therapeutic dose, based on body-surface area. Thiotepa was lethal to rabbit fetuses at a dose of 3 mg/kg (41 mg/m2), approximately two times the maximum recommended human therapeutic dose based on body-surface area.
Advise pregnant women of the potential risk to the fetus [see Use in Specific Populations (8.1, 8.3)]. Advise females of reproductive potential to use highly effective contraception during and after treatment with thiotepa for at least 6 months after therapy. Advise males of reproductive potential to use effective contraception during and after treatment with thiotepa for at least 1 year after therapy [see Use in Specific Populations (8.1, 8.3)]. -
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
· Myelosuppression [see Warnings and Precautions (5.1)]
· Infection [see Warnings and Precautions (5.1)]
· Hypersensitivity [see Warnings and Precautions (5.2)]
· Cutaneous Toxicity [see Warnings and Precautions (5.3)]
· Hepatic Veno-Occlusive Disease [see Warnings and Precautions (5.5)]
· Central Nervous System Toxicity [see Warnings and Precautions (5.6)]
· Carcinogenicity [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions with Treatment of adenocarcinoma of the breast, adenocarcinoma of the ovary, malignant effusions and superficial papillary carcinoma of the urinary bladder
Gastrointestinal: Nausea, vomiting, abdominal pain, anorexia.
General: Fatigue, weakness. Febrile reaction and discharge from a subcutaneous lesion may occur as the result of breakdown of tumor tissue.
Hypersensitivity Reactions: Allergic reactions - rash, urticaria, laryngeal edema, asthma, anaphylactic shock, wheezing.
Local Reactions: Contact dermatitis, pain at the injection site.
Neurologic: Dizziness, headache, blurred vision.
Renal: Dysuria, urinary retention, chemical cystitis or hemorrhagic cystitis.
Reproductive: Amenorrhea, interference with spermatogenesis.
Respiratory: Prolonged apnea has been reported when succinylcholine was administered prior to surgery, following combined use of thiotepa and other anticancer agents. It was theorized that this was caused by decrease of pseudocholinesterase activity caused by the anticancer drugs.
Skin: Dermatitis, alopecia. Skin depigmentation has been reported following topical use.
Special Senses: Conjunctivitis.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been identified during post approval use of thiotepa in preparative regimens prior to allogeneic or autologous hematopoietic progenitor (stem) cell transplantation (HSCT) in patients.
Blood and lymphatic system disorders: Febrile bone marrow aplasia.
Cardiac disorders: Bradycardia, cardiac failure congestive, cardio-respiratory arrest, pericardial effusion, pericarditis, right ventricular hypertrophy.
Congenital, familial and genetic disorders: Aplasia.
Ear and labyrinth disorders: Deafness.
Eye disorders: Blindness, eyelid ptosis, papilledema, strabismus.
Gastrointestinal disorders: Ascites, dysphagia, enterocolitis, gastritis, palatal disorder.
General disorders and administration site conditions: Device related infection, gait disturbance, malaise, multi-organ failure, pain.
Hepatobiliary disorders: Hepatomegaly.
Immune system disorders: Bone marrow transplant rejection, immunosuppression.
Infections and infestations: Acute sinusitis, bronchopulmonary aspergillosis, candida sepsis, enterococcal infection, Epstein-Barr virus infection, Escherichia sepsis, Fusarium infection, gastroenteritis, infection, lower respiratory tract infection fungal, lower respiratory tract infection viral, parainfluenza virus infection, Pneumonia legionella, relapsing fever, respiratory tract infection, sepsis, septic shock, Staphylococcal bacteremia, Staphylococcal infection, systemic candida, urinary tract infection.
Injury, poisoning and procedural complications: Refractoriness to platelet transfusion, subdural hematoma.
Investigations: Coagulation test abnormal, hemoglobin decreased, Klebsiella test positive, nuclear magnetic resonance imaging brain abnormal, transaminases increased, weight increased.
Metabolism and nutrition disorders: Hyponatremia.
Neoplasms benign, malignant and unspecified (incl. cysts and polyps): Breast cancer metastatic, central nervous system lymphoma, leukemia recurrent, lymphoma, malignant neoplasm progression, metastatic neoplasm, post transplant lymphoproliferative disorder.
Nervous system disorders: Aphasia, brain injury, bulbar palsy, central nervous system lesion, cerebral microangiopathy, cerebral ventricle dilatation, cerebrovascular accident, cognitive disorder, convulsion, coordination abnormal, encephalitis, encephalopathy, hemiplegia, hypotonia, leukoencephalopathy, memory impairment, motor dysfunction, neurotoxicity, quadriparesis, speech disorder, tremor, VIIth nerve paralysis, white matter lesion.
Psychiatric disorders: Delirium, depression, disorientation, suicidal ideation.
Renal and urinary disorders: Renal failure, nephropathy toxic.
Respiratory, thoracic and mediastinal disorders: Acute respiratory distress, aspiration, dyspnea exertional, interstitial lung disease, lung disorder, pneumonitis, pulmonary arteriopathy, pulmonary sepsis, pulmonary veno-occlusive disease, respiratory distress, respiratory failure, pulmonary hypertension.
Skin and subcutaneous tissue disorders: Stevens-Johnson syndrome and toxic epidermal necrolysis.
Vascular disorders: Capillary leak syndrome.
Pediatric use information is approved for Adienne SA’s TEPADINA (thiotepa) for Injection. However, due to Adienne SA’s marketing exclusivity rights, the drug product is not labeled with that information.
-
7 DRUG INTERACTIONS
7.1 Effect of Cytochrome CYP3A Inhibitors and Inducers
In vitro studies suggest that thiotepa is metabolized by CYP3A4 and CYP2B6 to its active metabolite TEPA. Avoid coadministration of strong CYP3A4 inhibitors (e.g., itraconazole, clarithromycin, ritonavir) and strong CYP3A4 inducers (e.g., rifampin, phenytoin) with thiotepa due to the potential effects on efficacy and toxicity [see Clinical Pharmacology (12.2)]. Consider alternative medications with no or minimal potential to inhibit or induce CYP3A4. If concomitant use of strong CYP3A4 modulators cannot be avoided, closely monitor for adverse drug reactions.
7.2 Effect of Thiotepa on Cytochrome CYP2B6 Substrates
In vitro studies suggest that thiotepa inhibits CYP2B6. Thiotepa may increase the exposure of drugs that are substrates of CYP2B6 in patients; however, the clinical relevance of this in vitro interaction is unknown [see Clinical Pharmacology (12.2)].
The administration of thiotepa with cyclophosphamide in patients reduces the conversion of cyclophosphamide to the active metabolite, 4-hydroxycyclophosphamide; the effect appears sequence dependent with a greater reduction in the conversion to 4-hydroxycyclophosphamide when thiotepa is administered 1.5 hours prior to the intravenous administration of cyclophosphamide compared to administration of thiotepa after intravenous cyclophosphamide [see Clinical Pharmacology (12.2)]. The reduction in 4-hydroxycyclophosphamide levels may potentially reduce efficacy of cyclophosphamide treatment.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Thiotepa can cause fetal harm when administered to a pregnant woman based on findings from animals and the drug’s mechanism of action [see Clinical Pharmacology (12.1)]. Limited available data with thiotepa use in pregnant women are insufficient to inform a drug-associated risk of major birth defects and miscarriage. In animal reproduction studies, administration of thiotepa to pregnant mice and rats during organogenesis produced teratogenic effects (neural tube defects and malformations of the skeletal system of the fetus) at doses approximately 0.125 and 1 times, respectively, the maximum recommended human daily dose on a mg/m2 basis. Thiotepa was lethal to rabbit fetuses at approximately 2 times the maximum recommended human therapeutic dose based on body-surface area [see Data]. Consider the benefits and risks of thiotepa for the mother and possible risks to the fetus when prescribing thiotepa to a pregnant woman.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Thiotepa given by the IP route in mice at doses ≥ 1 mg/kg (3.2 mg/m2), approximately 8-fold less than the maximum recommended human therapeutic dose based on body-surface area, and in rats at doses ≥ 3 mg/kg (21 mg/m2), approximately equal to the maximum recommended human therapeutic dose based on body-surface area, resulted in various malformations including neural tube defects, omphalocele, renal agenesis, atresia ani, limb and digit defects, cleft palate, micrognathia, other skeletal anomalies in the skull, vertebrae and ribs, and reduced skeletal ossification. Thiotepa was lethal to rabbit fetuses at a dose of 3 mg/kg (41 mg/m2), approximately 2 times the maximum recommended human therapeutic dose based on body-surface area.
8.2 Lactation
Risk Summary
There is no information regarding the presence of thiotepa in human milk, the effects on the breastfed infant, or the effects on milk production.
Because of the potential for serious adverse reactions, including the potential for tumorigenicity shown for thiotepa in animal studies, advise patients not to breastfeed during thiotepa treatment.
8.3 Females and Males of Reproductive Potential
Pregnancy testing
Thiotepa can cause fetal harm when administered to a pregnant female. Verify the pregnancy status of females of reproductive potential prior to initiating thiotepa therapy.
Contraception
Females
Advise females of reproductive potential to avoid pregnancy during thiotepa treatment and for at least 6 months after the final dose of thiotepa. Advise females to immediately report pregnancy [see Use in Specific Populations (8.1)].
Males
Thiotepa may damage spermatozoa and testicular tissue, resulting in possible genetic abnormalities. Males with female sexual partners of reproductive potential should use effective contraception during thiotepa treatment and for at least 1 year after the final dose of thiotepa [see Nonclinical Toxicology (13.1)].
Infertility
Based on nonclinical findings, male and female fertility may be compromised by treatment with thiotepa. Inform male patients about the possibility of sperm conservation before the start of therapy [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness of thiotepa in neonates have not been established.
Safety and effectiveness of thiotepa for treatment of adenocarcinoma of the breast, adenocarcinoma of the ovary, malignant effusions and superficial papillary carcinoma of the urinary bladder in pediatric patients have not been established.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information.8.5 Geriatric Use
Clinical studies of thiotepa for treatment of adenocarcinoma of the breast, adenocarcinoma of the ovary, malignant effusions and superficial papillary carcinoma of the urinary bladder did not include sufficient numbers of subjects aged 65 and over to determine whether elderly subjects respond differently from younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreasing hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
In patients with moderate (creatinine clearance (CLcr) of 30 mL/min to 59 mL/min) renal impairment, decreased renal excretion may result in increased plasma levels of thiotepa and TEPA [see Clinical Pharmacology (12.2)]. This may result in increased toxicity. Monitor patients with moderate to severe (CLcr < 30 mL/min) renal impairment for signs and symptoms of toxicity following treatment with thiotepa for an extended period of time.
8.7 Hepatic Impairment
Thiotepa is extensively metabolized in the liver. Patients with moderate (bilirubin levels greater than 1.5 times to 3 times the upper limit of normal and any AST) hepatic impairment may have increased plasma levels of thiotepa [see Clinical Pharmacology (12.2)]. This may result in toxicity. Monitor patients with moderate to severe (bilirubin levels greater than 3 times upper limit of normal and any AST) hepatic impairment for signs and symptoms of toxicity following treatment with thiotepa for an extended period of time.
-
10 OVERDOSE
There is no experience with overdoses of thiotepa. The most important adverse reactions expected in case of overdose are myeloablation and pancytopenia [see Nonclinical Toxicology (13.2)]. There is no known antidote for thiotepa. Monitor the hematological status closely and provide vigorous supportive measures as medically indicated.
-
11 DESCRIPTION
Thiotepa is an alkylating agent. Thiotepa for injection, USP is supplied as a non-pyrogenic, sterile lyophilized white powder for intravenous, intracavitary, or intravesical use after reconstitution and dilution.
Thiotepa for Injection, USP is available in a single-dose vial containing:
• 100 mg thiotepa. After reconstitution with 10 ml of water for injection, each ml contains 10 mg thiotepa.
Thiotepa is a synthetic product with antitumor activity. The chemical name for thiotepa is Tris(1-aziridinyl)phosphine sulfide. Thiotepa has the following structural formula:
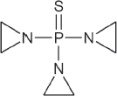
Thiotepa, USP has the molecular formula C6H12N3PS, and a molecular weight of 189.23, and it appears as fine, white crystalline flakes, with a melting range of 52°C to 57°C. It is soluble in water and organic solvents. When reconstituted with sterile water for injection, the resulting solution has a pH of approximately 5.5 to 7.5. Thiotepa is unstable in acid medium.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Thiotepa is a cytotoxic agent of the polyfunctional type, related chemically and pharmacologically to the nitrogen mustard. The radiomimetic action of thiotepa is believed to occur through the release of ethyleneimine radicals which, like irradiation, disrupt the bonds of DNA. One of the principle bond disruptions is initiated by alkylation of guanine at the N-7 position, which severs the linkage between the purine base and the sugar and liberates alkylated guanines.
12.2 Pharmacokinetics
Absorption
Thiotepa reached maximal concentrations close to the end infusion following an intravenous infusion.
Distribution
The binding of thiotepa to plasma proteins is approximately 10% to 20%. In adults administered intravenous thiotepa between 20 mg to 250 mg/m2 as an intravenous bolus or infusion up to 4 hours, the mean volume of distribution of thiotepa ranged from 1.0 L/kg (30%) to 1.9 L/kg (17%).
Elimination
In adults administered intravenous thiotepa between 20 mg to 250 mg/m2 as an intravenous bolus or infusion up to 4 hours, the mean thiotepa clearance ranged from 14.6 L/hr/m2 (23%) to 27.9 L/hr/m2 (69%). In adult population, the mean terminal elimination half-life ranged from 1.4 hours (7%) to 3.7 hours (14%) for thiotepa and from 4.9 hours to 17.6 hours (20%) for TEPA.
Metabolism
Thiotepa undergoes hepatic metabolism. In vitro data suggests that CYP3A4 and CYP2B6 may be responsible for the metabolism of thiotepa to TEPA, a major active metabolite.
Excretion
In adult patients, urinary excretion of thiotepa accounted for less than 2% of the dose and TEPA accounted for 11% or less of the dose.
Specific Populations
Hepatic Impairment
The exposure (as measured by area under the curve (AUC)) of thiotepa increased by 1.6-fold and 1.8-fold following administration of multiple thiotepa doses of 7 mg/kg administered every 2 days with cyclophosphamide in two adult patients who had liver metastases with moderate hepatic impairment compared to the exposure observed in one patient with normal hepatic function. The effect of severe hepatic impairment on thiotepa exposure is unknown.
Renal Impairment
The exposure (as measured by AUC) of thiotepa increased by 1.4-fold and TEPA increased by 2.6-fold following administration of multiple doses of 120 mg/m2/day in one patient with moderate renal impairment (CLcr = 38 mL/min) administered cyclophosphamide plus thiotepa plus carboplatin, compared to exposure of thiotepa in patients with normal renal function. The effects of severe renal impairment or end-stage renal disease on thiotepa exposure are unknown.
Drug Interactions
The clinical relevance of in vitro inhibition of the cytochrome P450 enzymes described below is unknown, but it cannot be excluded that the systemic exposure of thiotepa or medicinal products that are substrates for these enzymes may be affected with concomitant administration with thiotepa.
Effect of Cytochrome P450 Modulators on Thiotepa
In vitro data demonstrates that CYP3A4 and CYP2B6 inhibitors decrease the metabolism of thiotepa [see Drug Interactions (7.1)].
Effect of Thiotepa on Cytochrome P450 2B6
In vitro data demonstrates that thiotepa inhibits CYP2B6.
Effect of Thiotepa on Cyclophosphamide
The administration of thiotepa 1.5 hours prior to intravenous cyclophosphamide in patients administered cyclophosphamide plus thiotepa plus carboplatin decreased the AUC of 4-hydroxycyclophosphamide by 26% and maximal concentrations of 4hydroxycyclophosphamide by 62%, compared to administration of cyclophosphamide prior to thiotepa.
Pediatric use information is approved for Adienne SA' s TEPADINA (thiotepa) for Injection. However, due to Adienne SA's marketing exclusivity rights, the drug product is not labeled with that information. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In mice, repeated intraperitoneal (IP) administration of thiotepa (1.15 or 2.3 mg/kg three times per week for 52 or 43 weeks, respectively) produced a significant increase in the combined incidence of squamous-cell carcinomas of the skin, preputial gland, and ear canal, and combined incidence of lymphoma and lymphocytic leukemia. In other studies in mice, repeated IP administration of thiotepa (4 or 8 mg/kg three times per week for 4 weeks followed by a 20 week observation period or 1.8 mg/kg three times per week for 4 weeks followed by a 35 week observation period) resulted in an increased incidence of lung tumors. In rats, repeated IP administration of thiotepa (0.7 or 1.4 mg/kg three times per week for 52 or 34 weeks, respectively) produced significant increases in the incidence of squamous-cell carcinomas of the skin or ear canal, combined hematopoietic neoplasms, and uterine adenocarcinomas. Thiotepa given intravenously (IV) to rats (1 mg/kg once per week for 52 weeks) produced an increased incidence of malignant tumors (abdominal cavity sarcoma, lymphosarcoma myelosis, seminoma, fibrosarcoma, salivary gland hemangioendothelioma, mammary sarcoma, pheochromocytoma) and benign tumors.
The lowest reported carcinogenic dose in mice (1.15 mg/kg, 3.68 mg/m2) is approximately 7-fold less than the maximum recommended human therapeutic dose based on body-surface area. The lowest reported carcinogenic dose in rats (0.7 mg/kg, 4.9 mg/m2) is approximately 6-fold less than the maximum recommended human therapeutic dose based on body-surface area.
Thiotepa was mutagenic in in vitro assays in Salmonella typhimurium, E coli, Chinese hamster lung and human lymphocytes. Chromosomal aberrations and sister chromatid exchanges were observed in vitro with thiotepa in bean root tips, human lymphocytes, Chinese hamster lung, and monkey lymphocytes.
Mutations were observed with oral thiotepa in mouse at doses > 2.5 mg/kg (8 mg/m2). The mouse micronucleus test was positive with intraperitoneal administration of > 1 mg/kg (3.2 mg/m2). Other positive in vivo chromosomal aberration or mutation assays included Drosophila melanogaster, Chinese hamster marrow, murine marrow, monkey lymphocyte, and murine germ cell.
Thiotepa impaired fertility in male mice at oral or intraperitoneal doses ≥ 0.7 mg/kg (2.24 mg/m2), approximately 12-fold less than the maximum recommended human therapeutic dose based on body-surface area. Thiotepa (0.5 mg) inhibited implantation in female rats when instilled into the uterine cavity. Thiotepa interfered with spermatogenesis in mice at IP doses ≥ 0.5 mg/kg (1.6 mg/m2), approximately 17-fold less than the maximum recommended human therapeutic dose based on body-surface area. Thiotepa interfered with spermatogenesis in hamsters at an IP dose of 1 mg/kg (4.1 mg/m2), approximately 7-fold less than the maximum recommended human therapeutic dose based on body-surface area.
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Hypersensitivity
Counsel patients on the signs and symptoms of hypersensitivity and to seek immediate emergency assistance if they develop any of these signs and symptoms [see Warnings and Precautions (5.2)].
Myelosuppression
Inform patients of the possibility of developing low blood cell counts and the need for hematopoietic progenitor cell infusion. Instruct patients to immediately report to their healthcare provider if bleeding or fever occurs [see Warnings and Precautions (5.1)].
Females and Males of Reproductive Potential
Thiotepa for injection can cause fetal harm. Advise females receiving thiotepa for injection to avoid pregnancy during thiotepa for injection treatment and for at least 6 months after the final dose of thiotepa for injection [see Warnings and Precautions (5.8)].
Advise males with female sexual partners of reproductive potential to use effective contraception during thiotepa for injection treatment and for at least 1 year after the final dose of thiotepa for injection [see Use in Specific Populations (8.3)].
Advise females to report pregnancy immediately [see Warnings and Precautions (5.8)].
Advise patients that thiotepa for injection can produce infertility. Inform male patients about the possibility of sperm conservation before the start of therapy [see Use in Specific Populations (8.3)].
Lactation
Advise patients to avoid breastfeeding while receiving thiotepa for injection [see Use in Specific Populations (8.2)].
Secondary malignancies
Inform patients that thiotepa for injection can increase the risk of secondary malignancy [see Warnings and Precautions (5.7)].
Manufactured for:
Lake Zurich, IL 60047
www.fresenius-kabi.com/us
451728
Revised: February 2022
Made in IndiaPSLEA-020604-00
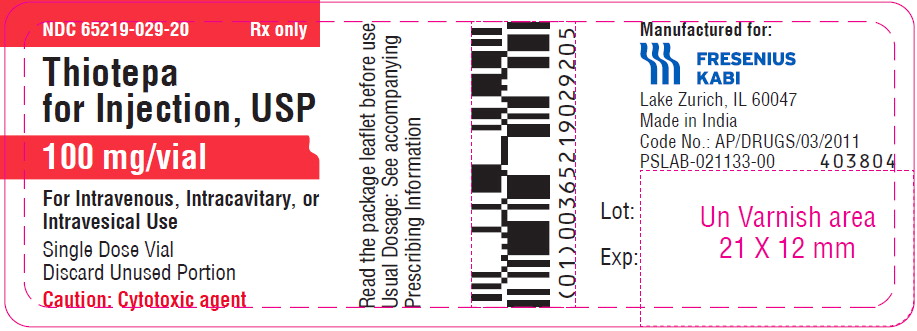
- PRINCIPAL DISPLAY PANEL
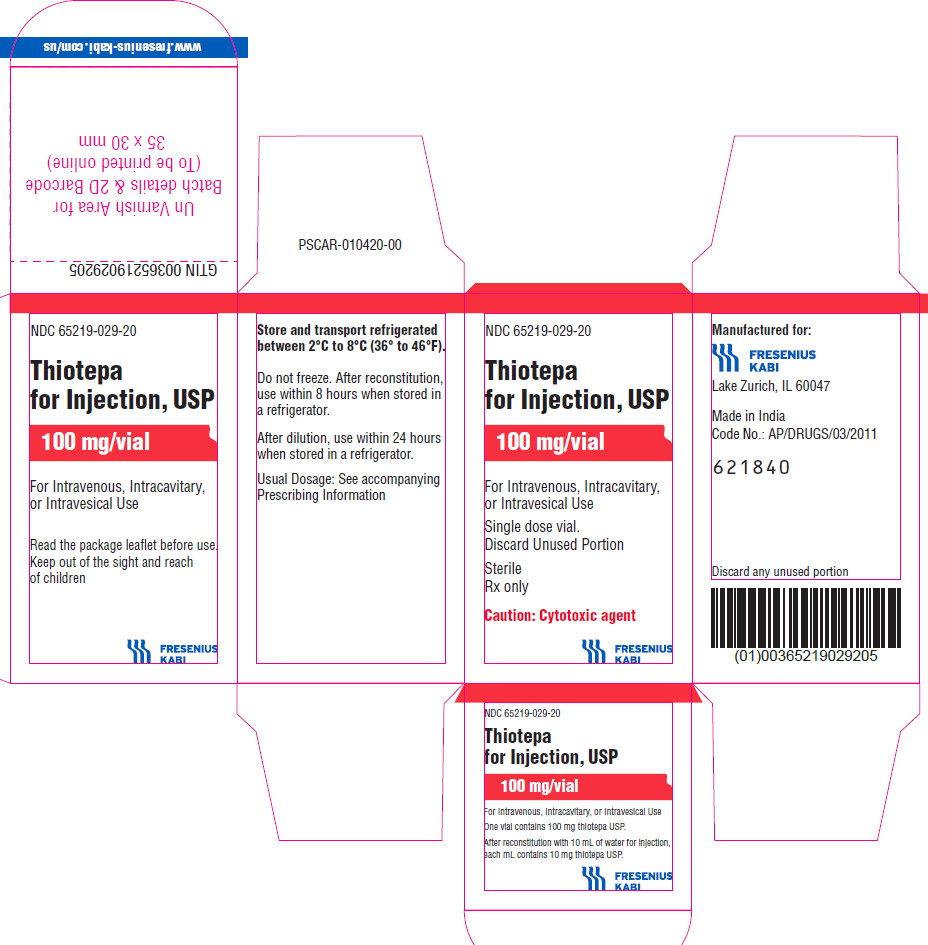
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
THIOTEPA
thiotepa injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:65219-029 Route of Administration INTRAVENOUS, INTRACAVITARY, INTRAVESICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength THIOTEPA (UNII: 905Z5W3GKH) (THIOTEPA - UNII:905Z5W3GKH) THIOTEPA 100 mg Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:65219-029-20 1 in 1 CARTON 04/11/2022 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214222 04/11/2022 Labeler - Fresenius Kabi USA, LLC (013547657) Establishment Name Address ID/FEI Business Operations Gland Pharma Limited 650540227 ANALYSIS(65219-029) , MANUFACTURE(65219-029) , PACK(65219-029)