Cardiac Failure
-
Sympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing ...
Cardiac Failure
Sympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure.
IN PATIENTS WITHOUT A HISTORY OF CARDIAC FAILURE, continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, patients should be treated appropriately according to currently recommended guidelines, and the response observed closely. If cardiac failure continues despite adequate treatment, atenolol and chlorthalidone should be withdrawn. (See DOSAGE AND ADMINISTRATION.)
Renal and Hepatic Disease and Electrolyte Disturbances
Since atenolol is excreted via the kidneys, atenolol and chlorthalidone should be used with caution in patients with impaired renal function.
In patients with renal disease, thiazides may precipitate azotemia. Since cumulative effects may develop in the presence of impaired renal function, if progressive renal impairment becomes evident, atenolol and chlorthalidone should be discontinued.
In patients with impaired hepatic function or progressive liver disease, minor alterations in fluid and electrolyte balance may precipitate hepatic coma. Atenolol and chlorthalidone should be used with caution in these patients.
Ischemic Heart Disease
Following abrupt cessation of therapy with certain beta-blocking agents in patients with coronary artery disease, exacerbations of angina pectoris and, in some cases, myocardial infarction have been reported. Therefore, such patients should be cautioned against interruption of therapy without the physician's advice. Even in the absence of overt angina pectoris, when discontinuation of atenolol and chlorthalidone is planned, the patient should be carefully observed and should be advised to limit physical activity to a minimum. Atenolol and chlorthalidone should be reinstated if withdrawal symptoms occur. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue atenolol and chlorthalidone therapy abruptly even in patients treated only for hypertension.
Concomitant Use of Calcium Channel Blockers
Bradycardia and heart block can occur and the left ventricular end diastolic pressure can rise when beta-blockers are administered with verapamil or diltiazem. Patients with pre-existing conduction abnormalities or left ventricular dysfunction are particularly susceptible. (See PRECAUTIONS.)
Bronchospastic Diseases
PATIENTS WITH BRONCHOSPASTIC DISEASE SHOULD, IN GENERAL, NOT RECEIVE BETA-BLOCKERS. Because of its relative beta1-selectivity, however, atenolol and chlorthalidone may be used with caution in patients with bronchospastic disease who do not respond to or cannot tolerate, other antihypertensive treatment. Since beta1-selectivity is not absolute, the lowest possible dose of atenolol and chlorthalidone should be used and a beta2-stimulating agent (bronchodilator) should be made available. If dosage must be increased, dividing the dose should be considered in order to achieve lower peak blood levels.
Major Surgery
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Metabolic and Endocrine Effects
Beta-blockers may prevent early warning signs of hypoglycemia, such as tachycardia, and increase the risk for severe or prolonged hypoglycemia at any time during treatment, especially in patients with diabetes mellitus or children and patients who are fasting (i.e., surgery, not eating regularly, or are vomiting). If severe hypoglycemia occurs, patients should be instructed to seek emergency treatment.
Insulin requirements in diabetic patients may be increased, decreased or unchanged; latent diabetes mellitus may become manifest during chlorthalidone administration.
Beta-adrenergic blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Abrupt withdrawal of beta blockade might precipitate a thyroid storm; therefore, patients suspected of developing thyrotoxicosis from whom atenolol and chlorthalidone therapy is to be withdrawn should be monitored closely.
Because calcium excretion is decreased by thiazides, atenolol and chlorthalidone should be discontinued before carrying out tests for parathyroid function. Pathologic changes in the parathyroid glands, with hypercalcemia and hypophosphatemia, have been observed in a few patients on prolonged thiazide therapy; however, the common complications of hyperparathyroidism such as renal lithiasis, bone resorption, and peptic ulceration have not been seen.
Hyperuricemia may occur, or acute gout may be precipitated in certain patients receiving thiazide therapy.
Untreated Pheochromocytoma
Atenolol and chlorthalidone should not be given to patients with untreated pheochromocytoma.
Pregnancy and Fetal Injury
Atenolol can cause fetal harm when administered to a pregnant woman. Atenolol crosses the placental barrier and appears in cord blood. Administration of atenolol, starting in the second trimester of pregnancy, has been associated with the birth of infants that are small for gestational age. No studies have been performed on the use of atenolol in the first trimester and the possibility of fetal injury cannot be excluded. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Neonates born to mothers who are receiving atenolol at parturition or breastfeeding may be at risk for hypoglycemia and bradycardia. Caution should be exercised when atenolol and chlorthalidone is administered during pregnancy or to a woman who is breastfeeding. (See PRECAUTIONS, Nursing Mothers.)
Atenolol and chlorthalidone was studied for teratogenic potential in the rat and rabbit. Doses of atenolol/chlorthalidone of 8/2 mg/kg/day, 80/20 mg/kg/day, and 240/60 mg/kg/day were administered orally to pregnant rats with no evidence of embryo fetotoxicity observed. Two studies were conducted in rabbits. In the first study, pregnant rabbits were dosed with 8/2 mg/kg/day, 80/20 mg/kg/day, and 160/40 mg/kg/day of atenolol/chlorthalidone. No teratogenic effects were noted, but embryonic resorptions were observed at all dose levels (ranging from approximately 5 times to 100 times the maximum recommended human dose*). In the second rabbit study, doses of atenolol/chlorthalidone were 4/1 mg/kg/day, 8/2 mg/kg/day, and 20/5 mg/kg/day. No teratogenic or embryotoxic effects were demonstrated.
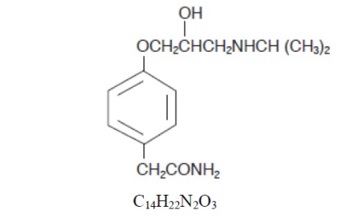
Atenolol
Atenolol has been shown to produce a dose-related increase in embryo/fetal resorptions in rats at doses equal to or greater than 50 mg/kg/day or 25 or more times the maximum recommended human antihypertensive dose*. Although similar effects were not seen in rabbits, the compound was not evaluated in rabbits at doses above 25 mg/kg/day or 12.5 times the maximum recommended human antihypertensive dose*.
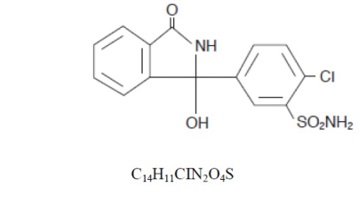
Chlorthalidone
Thiazides cross the placental barrier and appear in cord blood. The use of chlorthalidone and related drugs in pregnant women requires that the anticipated benefits of the drug be weighed against possible hazards to the fetus. These hazards include fetal or neonatal jaundice, thrombocytopenia and possibly other adverse reactions which have occurred in the adult.
*Based on the maximum dose of 100 mg/day in a 50 kg patient.
Close