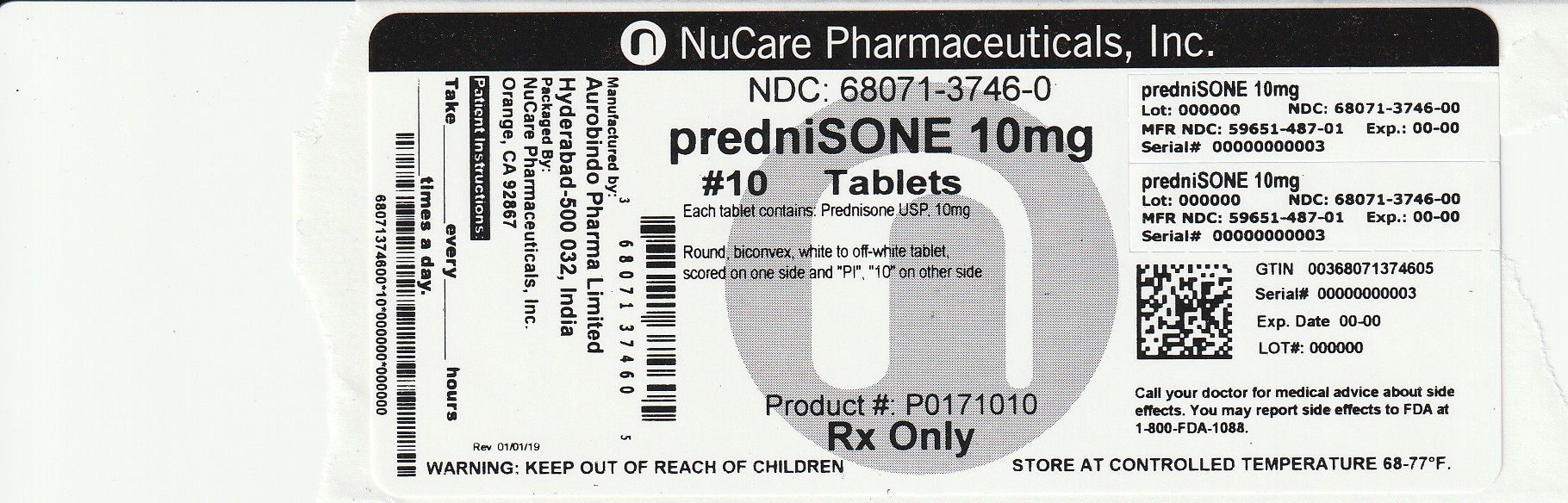
Label: PREDNISONE tablet
- NDC Code(s): 68071-3746-0
- Packager: NuCare Pharmaceuticals, Inc.
- This is a repackaged label.
- Source NDC Code(s): 59651-487
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated December 13, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
DESCRIPTION
Prednisone tablets, USP are available for oral administration containing either 2.5 mg, 5 mg, 10 mg, 20 mg or 50 mg of prednisone USP. Each tablet contains the following inactive ingredients: lactose monohydrate, magnesium stearate, microcrystalline cellulose, pregelatinized starch (maize), and sodium starch glycolate. In addition, 2.5 mg contains D&C yellow No.10 aluminum lake and 5 mg contains FD&C yellow # 6 aluminum lake.
Prednisone tablets, USP contain prednisone USP which is a glucocorticoid. Glucocorticoids are adrenocortical steroids, both naturally occurring and synthetic, which are readily absorbed from the gastrointestinal tract. The chemical name for prednisone is 17,21-dihydroxypregna-1,4-dienne-3,11,20-trione. The structural formula is represented below:
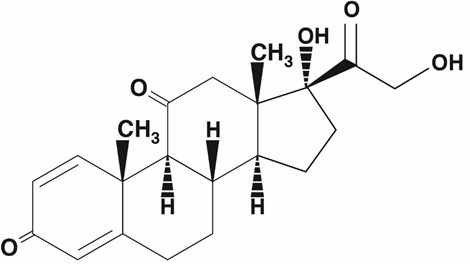
C 21H 26O 5M.W. 358.44
Prednisone USP is a white to partially white, odorless crystalline powder. It is very slightly soluble in water; slightly soluble in alcohol, chloroform, dioxane, and methanol.
FDA approved dissolution test specifications differ from USP. -
CLINICAL PHARMACOLOGY
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems.
Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli.
-
INDICATIONS AND USAGE
Prednisone tablets are indicated in the following conditions:
Endocrine Disorders
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance)
Congenital adrenal hyperplasia
Hypercalcemia associated with cancer
Nonsuppurative thyroiditis
Rheumatic Disorders
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Psoriatic arthritis
Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy)
Ankylosing spondylitis
Acute and subacute bursitis
Acute nonspecific tenosynovitis
Acute gouty arthritis
Post-traumatic osteoarthritis
Synovitis of osteoarthritis
Epicondylitis.
Collagen Diseases
During an exacerbation or as maintenance therapy in selected cases of:
Systemic lupus erythematosus
Systemic dermatomyositis (polymyositis)
Acute rheumatic carditis
Dermatologic Diseases
Pemphigus
Bullous dermatitis herpetiformis
Severe erythema multiforme (Stevens-Johnson syndrome)
Exfoliative dermatitis
Mycosis fungoides
Severe psoriasis
Severe seborrheic dermatitis
Allergic States
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional
treatment:
Seasonal or perennial allergic rhinitis
Bronchial asthma
Contact dermatitis
Atopic dermatitis
Serum sickness
Drug hypersensitivity reactions
Ophthalmic Diseases
Severe acute and chronic allergic and inflammatory processes involving the eye and its adnexa such as:
Allergic corneal marginal ulcers
Herpes zoster ophthalmicus
Anterior segment inflammation
Diffuse posterior uveitis and choroiditis
Sympathetic ophthalmia
Allergic conjunctivitis
Keratitis
Chorioretinitis
Optic neuritis
Iritis and iridocyclitis
Respiratory Diseases
Symptomatic sarcoidosis
Loeffler’s syndrome not manageable by other means
Berylliosis
Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy
Aspiration pneumonitis
Hematologic Disorders
Idiopathic thrombocytopenic purpura in adults
Secondary thrombocytopenia in adults
Acquired (autoimmune) hemolytic anemia
Erythroblastopenia (RBC anemia)
Congenital (erythroid) hypoplastic anemia
Neoplastic Diseases
For palliative management of:
Leukemias and lymphomas in adults
Acute leukemia of childhood
Edematous States
To induce a diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
Gastrointestinal Diseases
To tide the patient over a critical period of the disease in:
Ulcerative colitis
Regional enteritis
Nervous System
Acute exacerbations of multiple sclerosis
Miscellaneous
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy
Trichinosis with neurologic or myocardial involvement
- CONTRAINDICATIONS
-
WARNINGS
In patients on corticosteroid therapy subject to any unusual stress, increased dosage of rapidly acting corticosteroids before, during and after the stressful situation is indicated.
Immunosuppression and Increased Risk of Infection
Corticosteroids, including prednisone, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
- Reduce resistance to new infections
- Exacerbate existing infections
- Increase the risk of disseminated infections
- Increase the risk of reactivation or exacerbation of latent infections
- Mask some signs of infection
Corticosteroid-associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
Monitor for the development of infection and consider prednisone withdrawal or dosage reduction as needed.
Tuberculosis
If prednisone is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of tuberculosis may occur. Closely monitor such patients for reactivation. During prolonged prednisone therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella Zoster and Measles Viral Infections
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including prednisone. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
- If a prednisone-treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin may be indicated. If varicella develops, treatment with antiviral agents may be considered.
- If a prednisone-treated patient is exposed to measles, prophylaxis with immunoglobulin may be indicated.
Hepatitis B Virus Reactivation
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including prednisone. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with prednisone. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Fungal Infections
Corticosteroids, including prednisone, may exacerbate systemic fungal infections; therefore, avoid prednisone use in the presence of such infections unless prednisone is needed to control drug reactions. For patients on chronic prednisone therapy who develop systemic fungal infections, prednisone withdrawal or dosage reduction is recommended.
Amebiasis
Corticosteroids, including prednisone, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating prednisone in patients who have spent time in the tropics or patients with unexplained diarrhea.
Strongyloides Infestation
Corticosteroids, including prednisone, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Cerebral Malaria
Avoid corticosteroids, including prednisone, in patients with cerebral malaria.
Kaposi’s Sarcoma
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Prolonged use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to fungi or viruses.
Usage in pregnancy
Since adequate human reproduction studies have not been done with corticosteroids, the use of these drugs in pregnancy, nursing mothers or women of child-bearing potential requires that the possible benefits of the drug be weighed against the potential hazards to the mother and embryo or fetus. Infants born of mothers who have received substantial doses of corticosteroids during pregnancy, should be carefully observed for signs of hypoadrenalism.
Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
While on corticosteroid therapy patients should not be vaccinated against smallpox. Other immunization procedures should not be undertaken in patients who are on corticosteroids, especially on high dose, because of possible hazards of neurological complications and a lack of antibody response.
-
PRECAUTIONS
General Precautions
Drug-induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, inany situation of stress occurring during that period, hormone therapy should be reinstituted. Since mineralocorticoid secretion may be impaired, salt and/or a mineralocorticoid should be administered concurrently.
There is an enhanced effect of corticosteroids on patients with hypothyroidism and in those with cirrhosis.
Corticosteroids should be used cautiously in patients with ocular herpes simplex because of possible corneal perforation.
The lowest possible dose of corticosteroid should be used to control the condition under treatment, and when reduction in dosage is possible, the reduction should be gradual.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression, to frank psychotic manifestations. Also existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia.
Steroids should be used with caution in nonspecific ulcerative colitis, if there is a probability of impending perforation, abscess or other pyogenic infection: diverticulitis; fresh intestinal anastomoses; active or latent peptic ulcer; renal insufficiency; hypertension; osteoporosis: and myasthenia gravis.
Growth and development of infants and children on prolonged corticosteroid therapy should be carefully observed.
Although controlled clinical trials have shown corticosteroids to be effective in speeding the resolution of acute exacerbations of multiple sclerosis, they do not show that corticosteroids affect the ultimate outcome or natural history of the disease. The studies do show that relatively high doses of corticosteroids are necessary to demonstrate a significant effect (See DOSAGE AND ADMINISTRATION).
Since complications of treatment with glucocorticoids are dependent on the size of the dose and the duration of treatment, a risk/benefit decision must be made in each individual case as to dose and duration of treatment and as to whether daily or intermittent therapy should be used.
Convulsions have been reported with concurrent use of methylprednisolone and cyclosporine. Since concurrent use of these agents results in a mutual inhibition of metabolism, it is possible that adverse events associated with the individual use of either drug may be more apt to occur.
-
ADVERSE REACTIONS
Fluid and Electrolyte Disturbances
Sodium retention
Fluid retention
Congestive heart failure in susceptible patients
Potassium loss
Hypokalemic alkalosis
Hypertension
Musculoskeletal
Muscle weakness
Steroid myopathy
Loss of muscle mass
Osteoporosis
Vertebral compression fractures
Aseptic necrosis of femoral and humeral heads
Pathologic fracture of long bones
Gastrointestinal
Peptic ulcer with possible perforation and hemorrhage
Pancreatitis
Abdominal distention
Ulcerative esophagitis
Dermatologic
Impaired wound healing
Thin fragile skin
Petechiae and ecchymoses
Facial erythema
Increased sweating
May suppress reactions to skin tests
Metabolic
Negative nitrogen balance due to protein catabolism
Neurological
Increased intracranial pressure with papilledema (pseudo-tumor cerebri) usually after treatment
Convulsions
Vertigo
Headache
Endocrine
Menstrual irregularities
Development of Cushingoid state
Secondary adrenocortical and pituitary unresponsiveness, particularly in times of stress, as in trauma, surgery or illness
Suppression of growth in children
Decreased carbohydrate tolerance
Manifestations of latent diabetes mellitus
Increased requirements for insulin or oral hypoglycemic agents in diabetics
Ophthalmic
Posterior subcapsular cataracts
Increased intraocular pressure
Glaucoma
Exophthalmos
AdditionalReactions
Urticaria and other allergic, anaphylactic or hypersensitivity reactions
-
DOSAGE AND ADMINISTRATION
The initial dosage of prednisone may vary from 5 mg to 60 mg prednisone per day, depending on the specific disease entity being treated. In situations of less severity lower doses will generally suffice, while in selected patients higher initial doses may be required. The initial dosage should be maintained or adjusted until a satisfactory response is noted. If after a reasonable period of time there is a lack of satisfactory clinical response, prednisone should be discontinued and the patient transferred to other appropriate therapy. IT SHOULD BE EMPHASIZED THAT DOSAGE REQUIREMENTS AREVARIABLE AND MUST BE INDIVIDUALIZED ON THE BASIS OF THE DISEASE UNDERTREATMENT AND THE RESPONSE OF THE PATIENT.After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. It should be kept in mind that constant monitoring is needed in regard to drug dosage. Included in the situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient’s individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment; in this latter situation, it may be necessary to increase the dosage of prednisone for a period of time consistent with the patient’s condition. If after long-term therapy the drug is to be stopped it is recommended that it be withdrawn gradually rather than abruptly.
Multiple Sclerosis
In the treatment of acute exacerbations of multiple sclerosis daily doses of 200 mg of prednisolone for a week followed by 80 mg every other day for 1 month have been shown to be effective. (Dosage range is the same for prednisone and prednisolone.)
Alternate Day Therapy
Alternate day therapy is a corticosteroid dosing regimen in which twice the usual daily dose of corticoid is administered every other morning. The purpose of this mode of therapy is to provide the patient requiring long-term pharmacologic dose treatment with the beneficial effects of corticoids while minimizing certain undesirable effects, including pituitary-adrenal suppression, the Cushingoid state, corticoid withdrawal symptoms, and growth suppression in children.
The rationale for this treatment schedule is based on two major premises: (a) the anti-inflammatory or therapeutic effect of corticoids persists longer than their physical presence and metabolic effects and (b) administration of the corticosteroid every other morning allows for re-establishment of more nearly normal hypothalamic-pituitary-adrenal (HPA) activity on the off-steroid day.
A brief review of the HPA physiology may be helpful in understanding this rationale. Acting primarily through the hypothalamus a fall in free cortisol stimulates the pituitary gland to produce increasing amounts of corticotropin (ACTH) while a rise in free cortisol inhibits ACTH secretion. Normally the HPA system is characterized by diurnal (circadian) rhythm. Serum levels of ACTH rise from a low point about 10 pm to a peak level about 6 am. Increasing levels of ACTH stimulate adrenocortical activity resulting in a rise in plasma cortisol with maximal levels occurring between 2 am and 8 am. This rise in cortisol dampens ACTH production and in turn adrenocortical activity. There is a gradual fall in plasma corticoids during the day with lowest levels occurring about midnight.
The diurnal rhythm of the HPA axis is lost in Cushing’s disease, a syndrome of adrenocortical hyperfunction characterized by obesity with centripetal fat distribution, thinning of the skin with easy bruisability, muscle wasting with weakness, hypertension, latent diabetes, osteoporosis, electrolyte imbalance, etc. The same clinical findings of hyperadrenocorticism may be noted during long-term pharmacologic dose corticoid therapy administered in conventional daily divided doses. It would appear, then, that a disturbance in the diurnal cycle with maintenance of elevated corticoid values during the night may play a significant role in the development of undesirable corticoid effects. Escape from these constantly elevated plasma levels for even short periods of time may be instrumental in protecting against undesirable pharmacologic effects.
During conventional pharmacologic dose corticosteroid therapy, ACTH production is inhibited with subsequent suppression of cortisol production by the adrenal cortex. Recovery time for normal HPA activity is variable depending upon the dose and duration of treatment. During this time the patient is vulnerable to any stressful situation. Although it has been shown that there is considerably less adrenal suppression following a single morning dose of prednisolone (10 mg) as opposed to a quarter of that dose administered every 6 hours, there is evidence that some suppressive effect on adrenal activity may be carried over into the following day when pharmacologic doses are used. Further, it has been shown that a single dose of certain corticosteroids will produce adrenocortical suppression for two or more days. Other corticoids, including methylprednisolone, hydrocortisone, prednisone, and prednisolone, are considered to be short acting (producing adrenocortical suppression for 1¼ to 1½ days following a single dose) and thus are recommended for alternate day therapy.
The following should be kept in mind when considering alternate day therapy:
- Basic principles and indications for corticosteroid therapy should apply. The benefits of alternate day therapy should not encourage the indiscriminate use of steroids.
- Alternate day therapy is a therapeutic technique primarily designed for patients in whom long-term pharmacologic corticoid therapy is anticipated.
- In less severe disease processes in which corticoid therapy is indicated, it may be possible to initiate treatment with alternate day therapy. More severe disease states usually will require daily divided high dose therapy for initial control of the disease process. The initial suppressive dose level should be continued until satisfactory clinical response is obtained, usually four to ten days in the case of many allergic and collagen diseases. It is important to keep the period of initial suppressive dose as brief as possible particularly when subsequent use of alternate day therapy is intended. Once control has been established, two courses are available: (a) change to alternate day therapy and then gradually reduce the amount of corticoid given every other day or (b) following control of the disease process reduce the daily dose of corticoid to the lowest effective level as rapidly as possible and then change over to an alternate day schedule. Theoretically, course (a) may be preferable.
- Because of the advantages of alternate day therapy, it may be desirable to try patients on this form of therapy who have been on daily corticoids for long periods of time (e.g., patients with rheumatoid arthritis). Since these patients may already have a suppressed HPA axis, establishing them on alternate day therapy may be difficult and not always successful. However, it is recommended that regular attempts be made to change them over. It may be helpful to triple or even quadruple the daily maintenance dose and administer this every other day rather than just doubling the daily dose if difficulty is encountered. Once the patient is again controlled, an attempt should be made to reduce this dose to a minimum.
- As indicated above, certain corticosteroids, because of their prolonged suppressive effect on adrenal activity, are not recommended for alternate day therapy (e.g., dexamethasone and betamethasone).
- The maximal activity of the adrenal cortex is between 2 am and 8 am, and it is minimal between 4 pm and midnight. Exogenous corticosteroids suppress adrenocortical activity the least, when given at the time of maximal activity (am).
- In using alternate day therapy it is important, as in all therapeutic situations to individualize and tailor the therapy to each patient. Complete control of symptoms will not be possible in all patients. An explanation of the benefits of alternate day therapy will help the patient to understand and tolerate the possible flare-up in symptoms which may occur in the latter part of the off-steroid day. Other symptomatic therapy may be added or increased at this time if needed.
- In the event of an acute flare-up of the disease process, it may be necessary to return to a full suppressive daily divided corticoid dose for control. Once control is again established alternate day therapy may be re-instituted.
- Although many of the undesirable features of corticosteroid therapy can be minimized by alternate day therapy, as in any therapeutic situation, the physician must carefully weigh the benefit-risk ratio for each patient in whom corticoid therapy is being considered.
- HOW SUPPLIED
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 10 mg (100 Tablet Bottle)
-
INGREDIENTS AND APPEARANCE
PREDNISONE
prednisone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68071-3746(NDC:59651-487) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PREDNISONE (UNII: VB0R961HZT) (PREDNISONE - UNII:VB0R961HZT) PREDNISONE 10 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) Product Characteristics Color white (white to off-white) Score 2 pieces Shape ROUND (Biconvex) Size 7mm Flavor Imprint Code PI;10 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68071-3746-0 10 in 1 BOTTLE; Type 0: Not a Combination Product 12/13/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA215672 03/28/2022 Labeler - NuCare Pharmaceuticals, Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals, Inc. 010632300 repack(68071-3746)