Label: ELLENCE- epirubicin hydrochloride injection, solution
- NDC Code(s): 0009-5091-01, 0009-5093-01
- Packager: Pharmacia & Upjohn Company LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated April 25, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ELLENCE safely and effectively. See full prescribing information for ELLENCE.
ELLENCE® (epirubicin hydrochloride injection)
Initial U.S. Approval: 1999WARNING: CARDIAC TOXICITY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
See full prescribing information for complete boxed warning.
- •
- Cardiac Toxicity: Myocardial damage, including acute left ventricular failure, can occur with ELLENCE. The risk of cardiomyopathy is proportional to the cumulative exposure with incidence rates from 0.9% at a cumulative dose of 550 mg/m2, 1.6% at 700 mg/m2, and 3.3% at 900 mg/m2. The risk of cardiomyopathy is further increased with concomitant cardiotoxic therapy. Assess left ventricular ejection fraction (LVEF) before and regularly during and after treatment with ELLENCE (5.1).
- •
- Secondary Malignancies: Secondary acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) occur at a higher incidence in patients treated with anthracyclines, including ELLENCE (5.2).
- •
- Extravasation and Tissue Necrosis: Extravasation of ELLENCE can result in severe local tissue injury and necrosis requiring wide excision of the affected area and skin grafting. Immediately terminate the drug and apply ice to the affected area (5.3).
- •
- Severe myelosuppression resulting in serious infection, septic shock, requirement for transfusions, hospitalization, and death may occur (5.4).
INDICATIONS AND USAGE
ELLENCE is an anthracycline topoisomerase inhibitor indicated as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement following resection of primary breast cancer (1).
DOSAGE AND ADMINISTRATION
- •
- The recommended starting dose of ELLENCE is 100 to 120 mg/m2. Dosage reductions are possible when given in certain combinations (2.2).
- •
- Administer intravenously in repeated 3- to 4-week cycles, either total dose on Day 1 of each cycle or divided equally and given on Days 1 and 8 of each cycle (2.2).
- •
- Consider use of antiemetics when given in conjunction with other emetigenic drugs (2.1).
- •
- Patients administered the 120 mg/m2 regimen of ELLENCE should receive prophylactic antibiotic therapy (2.1).
- •
- Adjust dosage after the first treatment cycle based on hematologic and nonhematologic toxicities (2.3).
- •
- Reduce dose in patients with hepatic impairment (2.3, 8.6).
- •
- Consider lower doses in patients with severe renal impairment (2.3, 8.7).
DOSAGE FORMS AND STRENGTHS
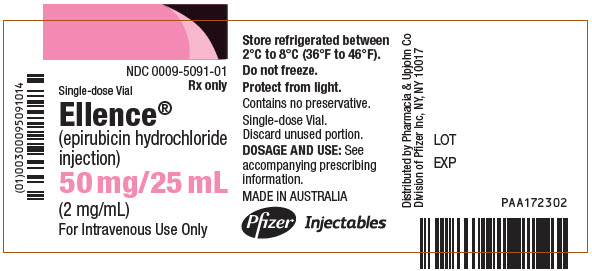
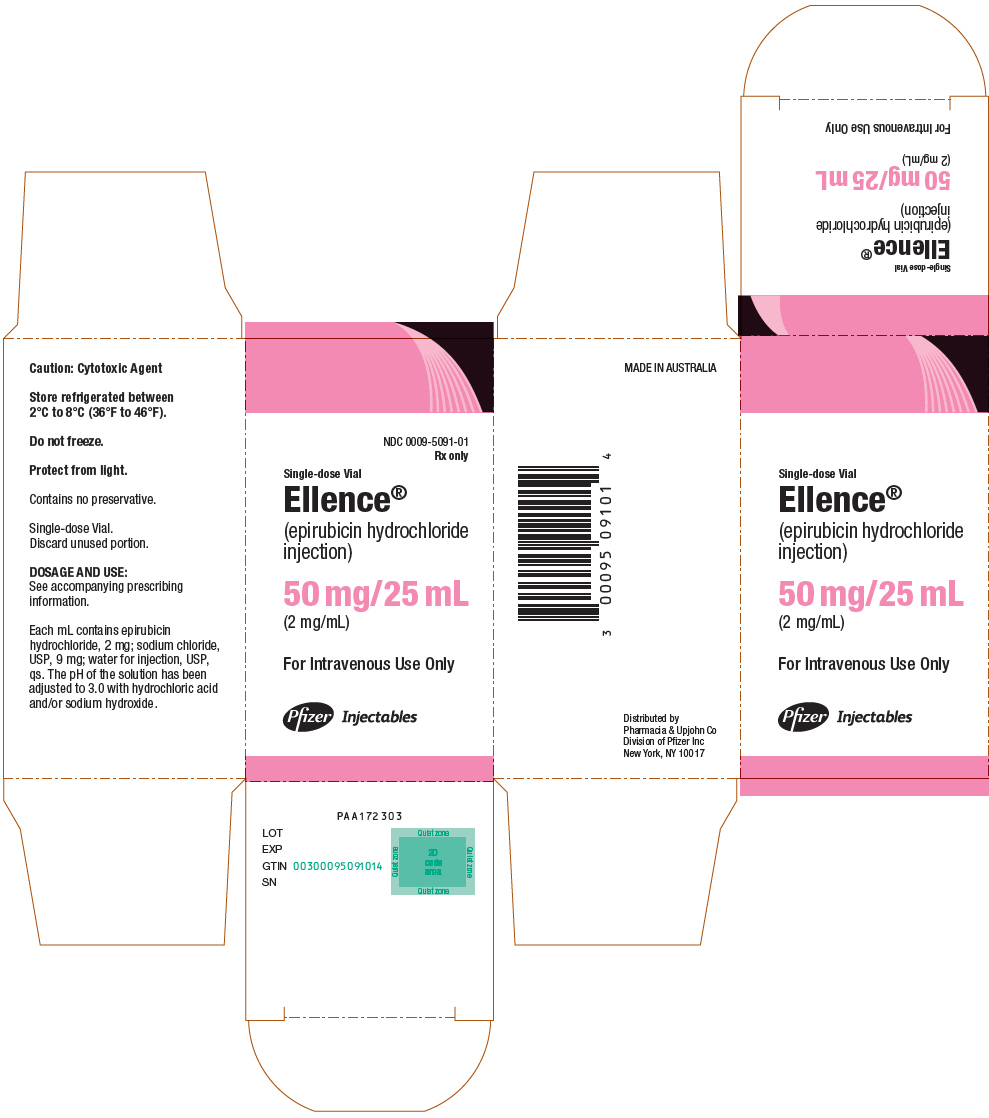
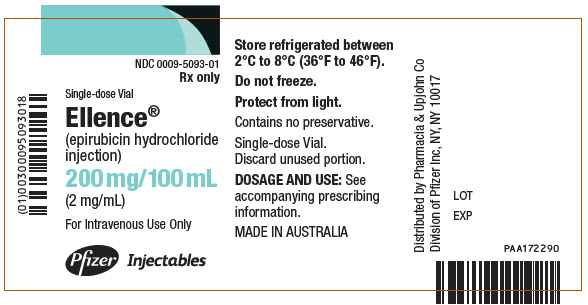
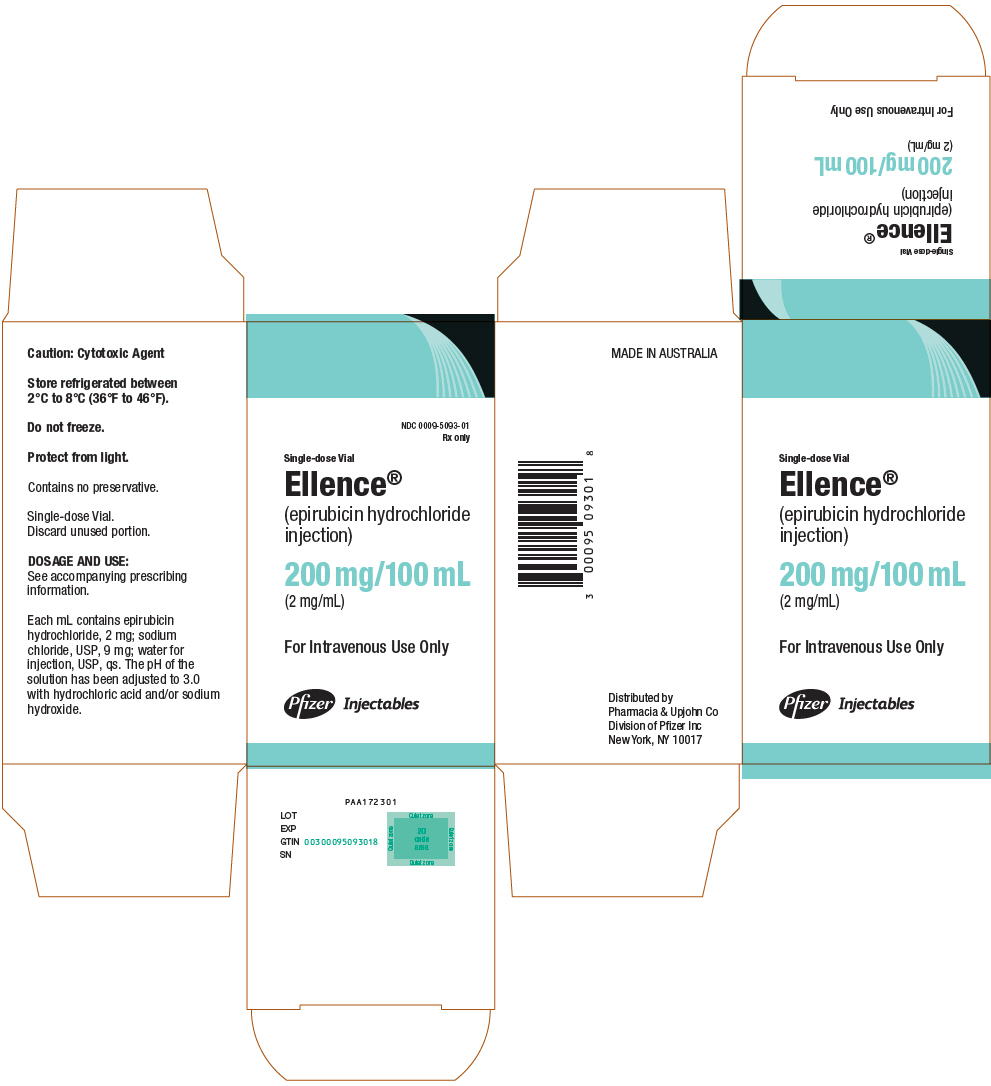
Injection: 50 mg/25 mL (2 mg/mL), 200 mg/100 mL (2 mg/mL) solution in single-dose vials (3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- •
- Use in Patients with Hepatic Impairment: Monitor serum total bilirubin and AST levels before and during treatment with ELLENCE. In patients with elevated serum AST or serum total bilirubin, dosage reductions or discontinuation may be required (2.3, 5.5).
- •
- Tumor Lysis Syndrome: Evaluate blood uric acid levels, potassium, calcium, phosphate, and creatinine after initial treatment. Consider hydration, urine alkalinization, and prophylaxis with allopurinol to minimize potential complications of hyperuricemia and tumor lysis syndrome (5.7).
- •
- Thrombophlebitis and Thromboembolic Events: Thrombophlebitis and thromboembolic events, including pulmonary embolism (in some cases fatal) have been reported with the use of ELLENCE. Venous sclerosis may result from an injection into a small vessel or from repeated injections into the same vein (5.9).
- •
- Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents including ELLENCE, may result in serious or fatal infections (5.7).
- •
- Potentiation of Radiation Toxicity and Radiation Recall: Administration of ELLENCE after previous radiation therapy may induce an inflammatory recall reaction at the site of the irradiation (5.10).
- •
- Embryo-Fetal Toxicity: ELLENCE can cause fetal harm. Advise patients of the potential risk to a fetus and to use effective contraception. (5.11, 8.1, 8.3).
ADVERSE REACTIONS
The most common adverse reactions (≥10%) are leukopenia, neutropenia, anemia, thrombocytopenia, amenorrhea, lethargy, nausea/vomiting, mucositis, diarrhea, infection, conjunctivitis/keratitis, alopecia, local skin toxicity, and rash/itch (6).
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 8/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CARDIAC TOXICITY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Recommended Dose
2.3 Dose Modifications
2.4 Preparation and Administration Precautions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Toxicity
5.2 Secondary Malignancies
5.3 Extravasation and Tissue Necrosis
5.4 Severe Myelosuppression
5.5 Use in Patients with Hepatic Impairment
5.6 Use in Patients with Renal Impairment
5.7 Tumor-Lysis Syndrome
5.8 Immunosuppressant Effects/Increased Susceptibility to Infections
5.9 Thrombophlebitis and Thromboembolic Events
5.10 Potentiation of Radiation Toxicity and Radiation Recall
5.11 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Cardiotoxic Agents
7.2 Cimetidine
7.3 Other Cytotoxic Drugs
7.4 Radiation Therapy
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adjuvant Treatment of Breast Cancer
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CARDIAC TOXICITY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
- •
- Cardiac Toxicity: Myocardial damage, including acute left ventricular failure, can occur with ELLENCE. The risk of cardiomyopathy is proportional to the cumulative exposure with incidence rates from 0.9% at a cumulative dose of 550 mg/m2, 1.6% at 700 mg/m2, and 3.3% at 900 mg/m2. The risk of cardiomyopathy is further increased with concomitant cardiotoxic therapy. Assess left ventricular ejection fraction (LVEF) before and regularly during and after treatment with ELLENCE [see Warnings and Precautions (5.1)].
- •
- Secondary Malignancies: Secondary acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) occur at a higher incidence in patients treated with anthracyclines, including ELLENCE [see Warnings and Precautions (5.2)].
- •
- Extravasation and Tissue Necrosis: Extravasation of ELLENCE can result in severe local tissue injury and necrosis requiring wide excision of the affected area and skin grafting. Immediately terminate the drug and apply ice to the affected area [see Warnings and Precautions (5.3)].
- •
- Severe myelosuppression resulting in serious infection, septic shock, requirement for transfusions, hospitalization, and death may occur [see Warnings and Precautions (5.4)].
-
1 INDICATIONS AND USAGE
ELLENCE is indicated as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement following resection of primary breast cancer [see Clinical Studies (14.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
When possible, to reduce the risk of developing cardiotoxicity in patients receiving ELLENCE after stopping treatment with other cardiotoxic agents, especially those with long half-lives such as trastuzumab, delay ELLENCE-based therapy until the other agents have cleared from the circulation [see Warnings and Precautions (5.1)].
Antiemetics may reduce nausea and vomiting; consider use of antiemetics before administration of ELLENCE or when clinically indicated, particularly when given in conjunction with other emetigenic drugs [see Adverse Reactions (6.1)].
Patients administered the 120 mg/m2 regimen of ELLENCE should receive prophylactic antibiotic therapy.
2.2 Recommended Dose
The recommended dose of ELLENCE is 100 to 120 mg/m2 administered as an intravenous bolus [see Dosage and Administration (2.4)].
The following regimens are recommended:
CEF-120:
Cyclophosphamide
75 mg/m2 oral on Days 1 to 14
ELLENCE
60 mg/m2 intravenously on Days 1 and 8
5-Fluorouracil
500 mg/m2 intravenously on Days 1 and 8
Repeat every 28 days for 6 cycles
FEC-100:
5-Fluorouracil
500 mg/m2 intravenously on Day 1
ELLENCE
100 mg/m2 intravenously on Day 1
Cyclophosphamide
500 mg/m2 intravenously on Day 1
Repeat every 21 days for 6 cycles
Administer ELLENCE in repeated 3- to 4-week cycles. The total dose of ELLENCE may be given on Day 1 of each cycle or divided equally and given on Days 1 and 8 of each cycle.
2.3 Dose Modifications
ELLENCE dosage adjustments for hematologic and non-hematologic toxicities within a cycle of treatment, is based on nadir platelet counts <50,000/mm3, absolute neutrophil counts (ANC) <250/mm3, neutropenic fever, or Grades 3/4 nonhematologic toxicity. Reduce ELLENCE Day 1 dose in subsequent cycles to 75% of the Day 1 dose given in the current cycle. Delay Day 1 chemotherapy in subsequent courses of treatment until platelet counts are ≥100,000/mm3, ANC ≥1500/mm3, and nonhematologic toxicities have recovered to ≤ Grade 1.
Cardiac Toxicity
Discontinue ELLENCE in patients who develop signs or symptoms of cardiomyopathy [see Warnings and Precautions (5.1)].
Bone Marrow Dysfunction
Consider administering a lower starting dose (75–90 mg/m2) for heavily pretreated patients, patients with pre-existing bone marrow depression, or in the presence of neoplastic bone marrow infiltration [see Warnings and Precautions (5.4)]. For patients receiving a divided dose of ELLENCE (Day 1 and Day 8), the Day 8 dose should be 75% of Day 1 if platelet counts are 75,000–100,000/mm3 and ANC is 1000 to 1499/mm3. If Day 8 platelet counts are <75,000/mm3, ANC <1000/mm3, or Grades 3/4 nonhematologic toxicity has occurred, omit the Day 8 dose.
Hepatic Impairment
In patients with elevated serum AST or serum total bilirubin concentrations [see Warnings and Precautions (5.5) and Clinical Pharmacology (12.3)], reduce dosage as follows:
- •
- Bilirubin 1.2 to 3 mg/dL or AST 2 to 4 times upper limit of normal 1/2 of recommended starting dose
- •
- Bilirubin > 3 mg/dL or AST > 4 times upper limit of normal 1/4 of recommended starting dose
Renal Impairment
Consider lower doses in patients with severe renal impairment (serum creatinine > 5 mg/dL) [see Warnings and Precautions (5.6) and Clinical Pharmacology (12.3)].
2.4 Preparation and Administration Precautions
Preparation
Storage of the solution for injection at refrigerated conditions can result in the formation of a gelled product. This gelled product will return to a slightly viscous to mobile solution after 2 to a maximum of 4 hours equilibration at controlled room temperature (15–25°C).
Inspect parenteral drug products visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
ELLENCE is a cytotoxic drug. Follow applicable special handling and disposable procedures1 [see References (15)].
Incompatibilities
Avoid prolonged contact with any solution of an alkaline pH as it will result in hydrolysis of the drug. Do not mix ELLENCE with heparin or fluorouracil due to chemical incompatibility that may lead to precipitation.
ELLENCE can be used in combination with other antitumor agents, but do not mix with other drugs in the same syringe.
Administration
Administer ELLENCE into the tubing of a freely flowing intravenous infusion (0.9% sodium chloride or 5% glucose solution). Patients receiving initial therapy at the recommended starting doses of 100–120 mg/m2 should generally have ELLENCE infused over 15–20 minutes.
For patients who require lower ELLENCE starting doses due to organ dysfunction or who require modification of ELLENCE doses during therapy, the ELLENCE infusion time may be proportionally decreased, but should not be less than 3 minutes. This technique is intended to minimize the risk of thrombosis or perivenous extravasation, which could lead to severe cellulitis, vesication, or tissue necrosis.
A direct push injection is not recommended due to the risk of extravasation, which may occur even in the presence of adequate blood return upon needle aspiration. Venous sclerosis may result from injection into small vessels or repeated injections into the same vein [see Warnings and Precautions (5.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
ELLENCE is contraindicated in patients with:
- •
- Severe myocardial insufficiency [see Warnings and Precautions (5.1)]
- •
- Recent myocardial infarction or severe arrhythmias, or previous treatment with maximum cumulative dose of anthracyclines [see Warnings and Precautions (5.1)]
- •
- Severe persistent drug-induced myelosuppression [see Warnings and Precautions (5.4)]
- •
- Severe hepatic impairment (defined as Child-Pugh Class C or serum bilirubin level greater than 5 mg/dL) [see Warnings and Precautions (5.5)]
- •
- Severe hypersensitivity to ELLENCE, other anthracyclines, or anthracenediones [see Adverse Reactions (6.1)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Toxicity
ELLENCE and other anthracycline drugs can result in either early (or acute) or late (delayed) cardiac toxicity.
The principal manifestations of early cardiac toxicity are sinus tachycardia and/or electrocardiogram (ECG) abnormalities such as non-specific ST-T wave changes. However, tachycardia (including premature ventricular contractions and ventricular tachycardia), bradycardia, as well as atrioventricular and bundle-branch block have been reported. Early cardiac toxicity does not usually predict the subsequent occurrence of delayed cardiotoxicity and generally should not be considered a reason for suspending treatment with ELLENCE.
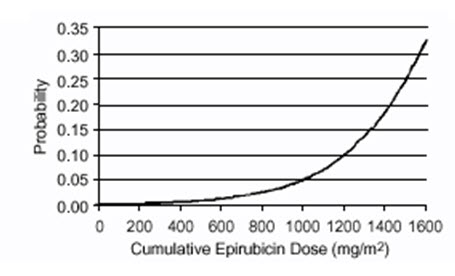
Delayed cardiac toxicity is manifested by reduced left ventricular ejection fraction (LVEF) and/or signs and symptoms of congestive heart failure (CHF). If it occurs, late cardiotoxicity usually develops late during therapy with ELLENCE or within 2 to 3 months after completion of treatment, but there are reports of it occurring several months to years after treatment termination. In a retrospective survey, including 9144 patients, mostly with solid tumors in advanced stages, the probability of developing CHF increased with increasing cumulative doses of ELLENCE (Figure 1). In another retrospective survey of 469 ELLENCE-treated patients with metastatic or early breast cancer, the reported risk of CHF was comparable to that observed in the larger study of over 9000 patients.
Given the risk of cardiac toxicity, cumulative doses of 900 mg/m2 ELLENCE should generally be avoided.
- Figure 1. Risk of CHF in 9144 Patients Treated with ELLENCE
Prior history of cardiovascular disease, prior or concomitant radiotherapy to the mediastinal/pericardial area, previous therapy with other anthracyclines or anthracenediones, and concomitant use of other cardiotoxic drugs, increase the risk of developing late cardiac toxicity. Avoid administration of ELLENCE in combination with other cardiotoxic drugs. Although not formally tested, it is probable that the toxicity of ELLENCE and other anthracyclines or anthracenediones is additive. Cardiac toxicity with ELLENCE may occur at lower cumulative doses whether or not cardiac risk factors are present. Patients receiving ELLENCE after stopping treatment with other cardiotoxic drugs, especially those with long half-lives such as trastuzumab, may be at increased risk of developing cardiotoxicity [see Dosage and Administration (2) and Drug Interaction (7.1)].
Perform a baseline ECG and evaluation of LVEF prior to initiating treatment with ELLENCE. Monitor LVEF during the course of treatment and consider discontinuation of ELLENCE if LVEF decrease and/or signs or symptoms of CHF develop. Closely monitor patients with other risk factors for cardiac toxicity, particularly prior administration of anthracycline or anthracenedione.
5.2 Secondary Malignancies
The risk of developing secondary acute myelogenous leukemia and myelodysplastic syndrome (MDS), is increased following treatment with ELLENCE and other anthracyclines. Cumulative risk of secondary acute myelogenous leukemia or myelodysplastic syndrome (AML/MDS) of about 0.27% at 3 years, 0.46% at 5 years, and 0.55% at 8 years. These leukemias generally occur within 1 to 3 years of treatment [see Adverse Reactions (6.1)].
5.3 Extravasation and Tissue Necrosis
Extravasation of ELLENCE can result in severe local tissue injury manifesting as blistering, ulceration, and necrosis requiring wide excision of the affected area and skin grafting. Extravasation should be considered if a patient experiences a burning or stinging sensation or shows other evidence indicating peri-venous infiltration or extravasation; however, extravasation may be present in patients who do not experience a stinging or burning sensation or when blood return is present on aspiration of the infusion needle.
Venous sclerosis may result from an injection into a small vessel or from repeated injections into the same vein. Administer ELLENCE slowly into the tubing of a freely running intravenous infusion. Patients receiving initial therapy at the recommended starting doses of 100–120 mg/m2 should have ELLENCE infused over 15–20 minutes. For patients who require lower ELLENCE starting doses due to organ dysfunction or who require modification of ELLENCE doses during therapy, the ELLENCE infusion time may be proportionally decreased, but should not be less than 3 minutes [see Dosage and Administration (2.3)]. If possible, avoid veins over joints or in extremities with compromised venous or lymphatic drainage. Facial flushing, as well as local erythematous streaking along the vein, may be indicative of excessively rapid administration. It may precede local phlebitis or thrombophlebitis.
Immediately terminate infusion and restart in another vein if a burning or stinging sensation indicates perivenous infiltration. Perivenous infiltration may occur without causing pain. If extravasation is suspected, immediately discontinue the intravenous injection or continuous intravenous infusion [see Dosage and Administration (2.3)]. Apply ice to the site intermittently for 15 minutes, 4 times a day for 3 days. If appropriate, administer dexrazoxane at the site of extravasation as soon as possible and within the first 6 hours after extravasation.
5.4 Severe Myelosuppression
ELLENCE can cause severe myelosuppression [see Adverse Reactions (6.1). Obtain complete blood counts prior to each treatment and carefully monitor patients during treatment for possible clinical complications due to myelosuppression. Delay the next dose of ELLENCE if severe myelosuppression has not improved. Consider dose reduction for patients with prolonged myelosuppression based on the severity of reaction [see Dosage and Administration (2.3)].
5.5 Use in Patients with Hepatic Impairment
The major route of elimination of epirubicin is the hepatobiliary system [see Clinical Pharmacology (12.3)]. Evaluate serum total bilirubin and AST levels before and during treatment with ELLENCE. Patients with elevated bilirubin or AST may experience slower clearance of drug with an increase in overall toxicity. Lower doses are recommended in these patients [see Dosage and Administration (2.2)]. Patients with severe hepatic impairment have not been evaluated; therefore, do not use ELLENCE in this patient population [see Contraindications (4)].
5.6 Use in Patients with Renal Impairment
Assess serum creatinine before and during therapy. Dosage adjustment is necessary in patients with serum creatinine >5 mg/dL [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)]. Patients undergoing dialysis have not been studied.
5.7 Tumor-Lysis Syndrome
ELLENCE can induce tumor lysis syndrome in patients with rapidly growing tumors. Evaluate blood uric acid levels, potassium, calcium, phosphate, and creatinine after initial treatment. Consider hydration, urine alkalinization, and prophylaxis with allopurinol to minimize hyperuricemia and potential complications of tumor lysis syndrome.
5.8 Immunosuppressant Effects/Increased Susceptibility to Infections
Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents including epirubicin, may result in serious or fatal infections. Avoid vaccination with a live vaccine in patients receiving ELLENCE. Killed or inactivated vaccines may be administered; however, the response to such vaccines may be diminished.
5.9 Thrombophlebitis and Thromboembolic Events
Thrombophlebitis and thromboembolic events, including pulmonary embolism (in some cases fatal) have been reported with the use of ELLENCE.
5.10 Potentiation of Radiation Toxicity and Radiation Recall
ELLENCE can increase radiation-induced toxicity to the myocardium, mucosa, skin, and liver. Radiation recall, including but not limited to cutaneous and pulmonary toxicity, can occur in patients who receive ELLENCE after prior radiation therapy.
5.11 Embryo-Fetal Toxicity
- Based on findings from animals and its mechanism of action, ELLENCE can cause fetal harm when administered to a pregnant woman; avoid the use of ELLENCE during the 1st trimester. Available human data do not establish the presence or absence of major birth defects and miscarriage related to the use of epirubicin during the 2nd and 3rd trimesters. In animal reproduction studies, epirubicin was embryo-fetal lethal and caused structural abnormalities in rats and rabbits at doses less than the maximum recommended human dose on a body surface area basis. Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise female patients of reproductive potential to use effective contraception during treatment and for 6 months after the last dose of ELLENCE. Advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of ELLENCE. Advise male patients with pregnant partners to use condoms during treatment and for at least 7 days after the last dose of ELLENCE [see Use in Specific Populations (8.1, 8.3), Clinical Pharmacology (12.1), and Nonclinical Toxicology (13.1)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- •
- Cardiac Toxicity [see Warnings and Precautions (5.1)]
- •
- Secondary Malignancies [see Warnings and Precautions (5.2)]
- •
- Extravasation and Tissue Necrosis [see Warnings and Precautions (5.3)]
- •
- Severe Myelosuppression [see Warnings and Precautions (5.4)]
- •
- Tumor-Lysis Syndrome [see Warnings and Precautions (5.7)]
- •
- Thrombophlebitis and Thromboembolic Events [see Warnings and Precautions (5.9)]
- •
- Potentiation of Radiation Toxicity and Radiation Recall [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of ELLENCE was evaluated in two studies (Studies MA-5 and GFEA-05) evaluating combination regimens in patients with early breast cancer [see Clinical Studies (14.1)]. Of the 1260 patients treated in these studies, 620 patients received the higher-dose ELLENCE regimen (FEC-100/CEF-120), 280 patients received the lower-dose ELLENCE regimen (FEC-50), and 360 patients received CMF. Serotonin-specific antiemetic therapy and colony-stimulating factors were not used in these trials. Clinically relevant adverse reactions are summarized in Table 1.
Table 1. Adverse Reactions in Patients with Early Breast Cancer Event % of Patients FEC-100/CEF-120
(N=620)FEC-50
(N=280)CMF
(N=360)Grades 1–4 Grades 3/4 Grades 1–4 Grades 3/4 Grades 1–4 Grades 3/4 FEC & CEF = cyclophosphamide + ELLENCE + fluorouracil; CMF = cyclophosphamide + methotrexate + fluorouracil; NA = not available Grade 1 or 2 changes in transaminase levels were observed but were more frequently seen with CMF than with CEF. Hematologic
Leukopenia
80
59
50
1.5
98
60
Neutropenia
80
67
54
11
96
78
Anemia
72
6
13
0
71
0.9
Thrombocytopenia
49
5
4.6
0
51
3.6
Endocrine
Amenorrhea
72
0
69
0
68
0
Hot flashes
39
4
5
0
69
6
Body as a Whole
Lethargy
46
1.9
1.1
0
73
0.3
Fever
5
0
1.4
0
4.5
0
Gastrointestinal
Nausea/vomiting
92
25
83
22
85
6
Mucositis
59
9
9
0
53
1.9
Diarrhea
25
0.8
7
0
51
2.8
Anorexia
2.9
0
1.8
0
6
0.3
Infection
Infection
22
1.6
15
0
26
0.6
Febrile neutropenia
NA
6
0
0
NA
1.1
Ocular
Conjunctivitis/keratitis
15
0
1.1
0
38
0
Skin
Alopecia
96
57
70
19
84
7
Local toxicity
20
0.3
2.5
0.4
8
0
Rash/itch
9
0.3
1.4
0
14
0
Skin changes
4.7
0
0.7
0
7
0
Delayed Events
Table 2 describes the incidence of delayed adverse reactions in patients participating in the MA-5 and GFEA-05 trials.
Table 2. Long-Term Adverse Reactions in Patients with Early Breast Cancer Event % of Patients FEC-100/CEF-120
(N=620)FEC-50
(N=280)CMF
(N=360)Two cases of acute lymphoid leukemia (ALL) were also observed in patients receiving ELLENCE. However, an association between anthracyclines such as ELLENCE and ALL has not been clearly established. - *
- In study MA-5, cardiac function was not monitored after 5 years.
Cardiac events
Asymptomatic drops in LVEF
2.1*
1.4
0.8*
CHF
1.5
0.4
0.3
Leukemia
AML
0.8
0
0.3
Hematologic
Dose-dependent, reversible leukopenia and/or neutropenia is the predominant manifestation of hematologic toxicity associated with ELLENCE and represents the most common acute dose-limiting toxicity of this drug. In most cases, the white blood cell (WBC) nadir is reached 10 to 14 days from drug administration. Leukopenia/neutropenia is usually transient, with WBC and neutrophil counts generally returning to normal values by Day 21 after drug administration. As with other cytotoxic agents, ELLENCE at the recommended dose in combination with cyclophosphamide and fluorouracil can produce severe leukopenia and neutropenia. Severe thrombocytopenia and anemia may also occur. Clinical consequences of severe myelosuppression include fever, infection, septicemia, septic shock, hemorrhage, tissue hypoxia, symptomatic anemia, or death. If myelosuppressive complications occur, use appropriate supportive measures (e.g., intravenous antibiotics, colony-stimulating factors, transfusions). Myelosuppression requires careful monitoring. Assess total and differential WBC, red blood cell (RBC), and platelet counts before and during each cycle of therapy with ELLENCE [see Warnings and Precautions (5.4)].
Gastrointestinal
A dose-dependent mucositis (mainly oral stomatitis, less often esophagitis) may occur in patients treated with ELLENCE. Clinical manifestations of mucositis may include a pain or burning sensation, erythema, erosions, ulcerations, bleeding, or infections. Mucositis generally appears early after drug administration and, if severe, may progress over a few days to mucosal ulcerations; most patients recover from this adverse event by the third week of therapy. Hyperpigmentation of the oral mucosa may also occur. Nausea, vomiting, and occasionally diarrhea and abdominal pain can also occur. Severe vomiting and diarrhea may produce dehydration. Antiemetics may reduce nausea and vomiting; consider prophylactic use of antiemetics before therapy [see Dosage and Administration (2.1)].
Cutaneous and Hypersensitivity Reactions
Alopecia occurs frequently, but is usually reversible, with hair regrowth occurring within 2 to 3 months from the termination of therapy. Flushes, skin and nail hyperpigmentation, photosensitivity, and hypersensitivity to irradiated skin (radiation-recall reaction) have been observed. Urticaria and anaphylaxis have been reported in patients treated with ELLENCE; signs and symptoms of these reactions may vary from skin rash and pruritus to fever, chills, and shock.
Cardiovascular
Serious drug-related cardiovascular adverse events that occurred during clinical trials with ELLENCE, administered in different indications, include ventricular tachycardia, AV block, bundle branch block, bradycardia and thromboembolism.
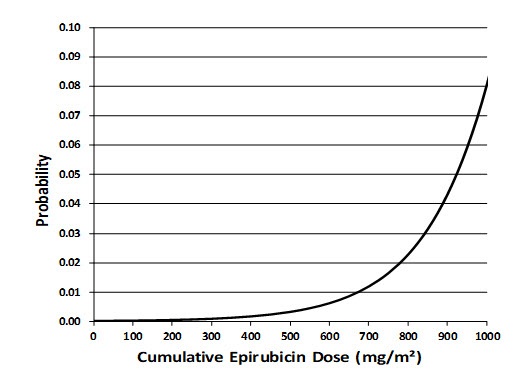
Secondary Leukemia
An analysis of 7110 patients who received adjuvant treatment with ELLENCE in controlled clinical trials as a component of poly-chemotherapy regimens for early breast cancer, showed a cumulative risk of secondary acute myelogenous leukemia or myelodysplastic syndrome (AML/MDS) of about 0.27% (approximate 95% CI, 0.14–0.40) at 3 years, 0.46% (approximate 95% CI, 0.28–0.65) at 5 years, and 0.55% (approximate 95% CI, 0.33–0.78) at 8 years. The risk of developing AML/MDS increased with increasing ELLENCE cumulative doses as shown in Figure 2.
- Figure 2. Risk of AML/MDS in 7110 Patients Treated with ELLENCE
The cumulative probability of developing AML/MDS was found to be particularly increased in patients who received more than the maximum recommended cumulative dose of ELLENCE (720 mg/m2) or cyclophosphamide (6,300 mg/m2), as shown in Table 3.
Table 3. Cumulative Probability of AML/MDS in Relation to Cumulative Doses of ELLENCE and Cyclophosphamide Years from Treatment Start Cumulative Probability of Developing AML/MDS
% (95% CI)Cyclophosphamide Cumulative Dose
≤6,300 mg/m2Cyclophosphamide Cumulative Dose
>6,300 mg/m2ELLENCE Cumulative Dose
≤720 mg/m2
N=4760ELLENCE Cumulative Dose
>720 mg/m2
N=111ELLENCE Cumulative Dose
≤720 mg/m2
N=890ELLENCE Cumulative Dose
>720 mg/m2
N=2613
0.12 (0.01–0.22)
0.00 (0.00–0.00)
0.12 (0.00–0.37)
4.37 (1.69–7.05)
5
0.25 (0.08–0.42)
2.38 (0.00–6.99)
0.31 (0.00–0.75)
4.97 (2.06–7.87)
8
0.37 (0.13–0.61)
2.38 (0.00–6.99)
0.31 (0.00–0.75)
4.97 (2.06–7.87)
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of ELLENCE. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Infections and infestations: sepsis, pneumonia
Immune system disorders: anaphylaxis
Metabolism and nutrition disorders: dehydration, hyperuricemia
Vascular disorders: shock, hemorrhage, embolism arterial, thrombophlebitis, phlebitis
Respiratory, thoracic and mediastinal disorders: pulmonary embolism
Gastrointestinal disorders: erosions, ulcerations, pain or burning sensation, bleeding, hyperpigmentation of the oral mucosa
Skin and subcutaneous tissue disorders: erythema, flushes, skin and nail hyperpigmentation, photosensitivity, hypersensitivity to irradiated skin (radiation-recall reaction), urticaria
Renal and urinary disorders: red coloration of urine for 1 to 2 days after administration
General disorders and administration site conditions: fever, chills
Injury, poisoning and procedural complications: chemical cystitis (following intravesical administration)
-
7 DRUG INTERACTIONS
7.1 Cardiotoxic Agents
Closely monitor cardiac function when ELLENCE is used in combination with other cardiotoxic agents. Patients receiving ELLENCE after stopping treatment with other cardiotoxic agents, especially those with long half-lives such as trastuzumab, may be at an increased risk of developing cardiotoxicity [see Dosage and Administration (2) and Warnings and Precautions (5.1)]. Trastuzumab may persist in the circulation for up to 7 months. Therefore, avoid anthracycline-based therapy for up to 7 months after stopping trastuzumab when possible. Monitor the patient's cardiac function closely if anthracyclines are used before this time.
Concomitant use of ELLENCE with other cardioactive compounds that could cause heart failure (e.g., calcium channel blockers), requires close monitoring of cardiac function throughout treatment.
7.2 Cimetidine
Cimetidine increases the exposure to epirubicin [see Clinical Pharmacology (12.3)]. Discontinue cimetidine during treatment with ELLENCE.
7.3 Other Cytotoxic Drugs
ELLENCE used in combination with other cytotoxic drugs may show on-treatment additive toxicity, especially hematologic and gastrointestinal effects.
Paclitaxel:
The administration of epirubicin immediately prior to or after paclitaxel increased the systemic exposure of epirubicin, epirubicinol and 7-deoxydoxorubicin aglycone [see Clinical Pharmacology (12.3)].
Docetaxel:
The administration of epirubicin immediately prior to or after docetaxel did not have an effect on the systemic exposure of epirubicin, but increased the systemic exposure of epirubicinol and 7-deoxydoxorubicin aglycone [see Clinical Pharmacology (12.3)].
7.4 Radiation Therapy
There are few data regarding the coadministration of radiation therapy and ELLENCE. In adjuvant trials of ELLENCE-containing CEF-120 or FEC-100 chemotherapies, breast irradiation was delayed until after chemotherapy was completed. This practice resulted in no apparent increase in local breast cancer recurrence relative to published accounts in the literature. A small number of patients received ELLENCE-based chemotherapy concomitantly with radiation therapy but had chemotherapy interrupted in order to avoid potential overlapping toxicities. It is likely that use of ELLENCE with radiotherapy may sensitize tissues to the cytotoxic actions of irradiation. Administration of ELLENCE after previous radiation therapy may induce an inflammatory recall reaction at the site of the irradiation.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and its mechanism of action, ELLENCE can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]; avoid the use of ELLENCE during the 1st trimester. Available human data do not establish the presence or absence of major birth defects and miscarriage related to the use of epirubicin during the 2nd and 3rd trimesters. There are reports of fetal and/or neonatal cardiotoxicity following in utero exposure to epirubicin (see Clinical Considerations). In animal reproduction studies in pregnant rats, epirubicin was embryo-fetal lethal and caused structural abnormalities when administered during organogenesis at doses less than the maximum recommended human dose on a body surface area basis (see Data). Advise pregnant women and females of reproductive potential of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Fetal/Neonatal Adverse Reactions
There have been rare reports of fetal and/or neonatal transient ventricular hypokinesia, transient elevation of cardiac enzymes, and a case of fetal demise from suspected anthracycline-induced cardiotoxicity following in utero exposure to epirubicin in 2nd and/or 3rd trimesters. Cardiotoxicity is a known risk of anthracycline treatment in adults [see Warnings and Precautions (5.1)]. Monitor the fetus and/or neonate for cardiotoxicity and perform testing consistent with community standards of care.
Animal Data
Intravenous administration of 0.8 mg/kg/day epirubicin(about 0.04 times the maximum recommended single human dose on a body surface area basis) to rats during Days 5 to 15 of gestation resulted in embryofetal lethality (increased resorptions and post-implantation loss) and caused fetal growth retardation (decreased body weight).Intravenous administration of 2 mg/kg/day epirubicin (about 0.1 times the maximum recommended single human dose on a body surface area basis) to rats on Days 9 and 10 of gestation resulted in embryo-fetal lethality (increased late resorptions, post-implantation losses, and dead fetuses; and decreased live fetuses), retarded fetal growth (decreased body weight), and caused decreased placental weight and numerous external (anal atresia, misshapen tail, abnormal genital tubercle), visceral (primarily gastrointestinal, urinary, and cardiovascular systems), and skeletal (deformed long bones and girdles, rib abnormalities, irregular spinal ossification) malformations. Administration of intravenous epirubicin to rabbits at doses up to 0.2 mg/kg/day (about 0.02 times the maximum recommended single human dose on a body surface area basis) during Days 6 to 18 of gestation was not teratogenic, but a maternally toxic dose of 0.32 mg/kg/day increased abortions and delayed ossification. Administration of a maternally toxic intravenous dose of 1 mg/kg/day epirubicin to rabbits (about 0.1 times the maximum recommended single human dose on a body surface area basis) on Days 10 to 12 of gestation induced abortion, but no other signs of teratogenicity were observed. When doses up to 0.5 mg/kg/day epirubicin were administered to rat dams from Day 17 of gestation to Day 21 after delivery (about 0.025 times the maximum recommended single human dose on a body surface area basis), no permanent changes were observed in the development, functional activity, behavior, or reproductive performance of the offspring.
8.2 Lactation
Risk Summary
There are no data on the presence of epirubicin in human milk, the effects on the breastfed child, or the effects on milk production. Epirubicin is present in rat milk (see Data). When a drug is present in animal milk it is likely the drug will be present in human milk. Because of the potential for serious adverse reactions in the breastfed child, advise lactating women not to breastfeed during treatment with ELLENCE and for at least 7 days after the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status in female patients of reproductive potential prior to initiating ELLENCE.
Contraception
Females
ELLENCE can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise female patients of reproductive potential to use effective contraception during treatment and for 6 months after the last dose of ELLENCE.
Males
Based on clinical findings and animal studies, ELLENCE may cause oligospermia, azoospermia, and permanent loss of fertility. Sperm counts have been reported to return to normal levels in some men. This may occur several years after the end of therapy [see Nonclinical Toxicology (13.1)].
Infertility
Females
Based on clinical findings and animal studies, ELLENCE may impair female fertility and result in amenorrhea. Premature menopause can occur. Recovery of menses and ovulation is related to age at treatment [see Nonclinical Toxicology (13.1)].
Males
Based on its mechanism of action and genotoxicity studies, advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of ELLENCE. Advise male patients with pregnant partners use condoms during treatment and for at least 7 days after the last dose of ELLENCE [see Clinical Pharmacology (12.1) and Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness of ELLENCE have not been established in pediatric patients. Pediatric patients may be at greater risk for anthracycline-induced acute manifestations of cardiotoxicity or late cardiovascular dysfunction. The pharmacokinetics of epirubicin in pediatric patients have not been evaluated.
8.5 Geriatric Use
Clinical experience in patients who were 65 years of age and older who received ELLENCE chemotherapy regimens for primary breast cancer showed no overall differences in safety and effectiveness compared with younger patients.
In elderly female patients, closely monitor for increased toxicity due to the risk of decreased clearance of epirubicin [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
Epirubicin is eliminated by both hepatic metabolism and biliary excretion and clearance is reduced in patients with hepatic dysfunction. Do not treat patients with severe hepatic impairment with ELLENCE [see Contraindications (4)]. Reduce the starting dose for patients with less severe hepatic impairment [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
8.7 Renal Impairment
No significant alterations in the pharmacokinetics of epirubicin or its major metabolite, epirubicinol, have been observed in patients with serum creatinine <5 mg/dL. Consider lower doses in patients with severe renal impairment (serum creatinine >5 mg/dL), as a reduction in plasma clearance was reported in these patients [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)]. Patients on dialysis have not been studied.
-
10 OVERDOSAGE
There is no known antidote for overdoses of ELLENCE. A 36-year-old man with non-Hodgkin's lymphoma received a daily 95 mg/m2 dose of ELLENCE for 5 consecutive days. Five days later, he developed bone marrow aplasia, grade 4 mucositis, and gastrointestinal bleeding. No signs of acute cardiac toxicity were observed. He was treated with antibiotics, colony-stimulating factors, and antifungal agents, and recovered completely. A 63-year-old woman with breast cancer and liver metastasis received a single 320 mg/m2 dose of ELLENCE. She was hospitalized with hyperthermia and developed multiple organ failure (respiratory and renal), with lactic acidosis, increased lactate dehydrogenase, and anuria. Death occurred within 24 hours after administration of ELLENCE. Additional instances of administration of doses higher than recommended have been reported at doses ranging from 150 to 250 mg/m2. The observed adverse events in these patients were qualitatively similar to known toxicities of epirubicin. Most of the patients recovered with appropriate supportive care.
If an overdose occurs, provide supportive treatment (including antibiotic therapy, blood and platelet transfusions, colony-stimulating factors, and intensive care as needed) until the recovery of toxicities. Delayed CHF has been observed months after anthracycline administration. Observe patients carefully over time for signs of CHF and provided with appropriate supportive therapy.
-
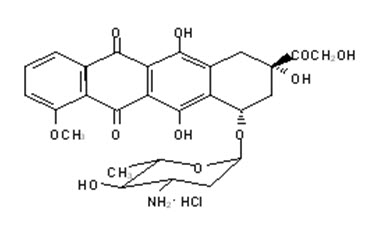
11 DESCRIPTION
ELLENCE (epirubicin hydrochloride injection) is an anthracycline topoisomerase inhibitor for intravenous administration. ELLENCE is supplied as a sterile, clear, red solution and is available in polypropylene vials containing 50 and 200 mg of epirubicin hydrochloride as a preservative-free, ready-to-use solution. Each milliliter of solution contains 2 mg of epirubicin hydrochloride. Inactive ingredients include 9 mg sodium chloride, USP, and water for injection, USP. The pH of the solution has been adjusted to 3.0 with hydrochloric acid and/or sodium hydroxide, NF.
Epirubicin hydrochloride is the 4-epimer of doxorubicin and is a semi-synthetic derivative of daunorubicin. The chemical name is (8S-cis)-10-[(3-amino-2,3,6-trideoxy-α-L- arabino-hexopyranosyl)oxy]-7,8,9,10-tetrahydro6,8,11-trihydroxy-8-(hydroxyacetyl)-1-methoxy-5,12-naphthacenedione hydrochloride. The active ingredient is a red-orange hygroscopic powder, with the empirical formula C27 H29 NO11 HCl and a molecular weight of 579.95. The structural formula is as follows:
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Epirubicin is an anthracycline cytotoxic agent. Although it is known that anthracyclines can interfere with a number of biochemical and biological functions within eukaryotic cells, the precise mechanisms of epirubicin's cytotoxic and/or antiproliferative properties have not been completely elucidated.
Epirubicin forms a complex with DNA by intercalation of its planar rings between nucleotide base pairs, with consequent inhibition of nucleic acid (DNA and RNA) and protein synthesis.
Such intercalation triggers DNA cleavage by topoisomerase II, resulting in cytocidal activity. Epirubicin also inhibits DNA helicase activity, preventing the enzymatic separation of double-stranded DNA and interfering with replication and transcription. Epirubicin is also involved in oxidation/reduction reactions by generating cytotoxic free radicals. The antiproliferative and cytotoxic activity of epirubicin is thought to result from these or other possible mechanisms.
Epirubicin is cytotoxic in vitro to a variety of established murine and human cell lines and primary cultures of human tumors. It is also active in vivo against a variety of murine tumors and human xenografts in athymic mice, including breast tumors.
12.3 Pharmacokinetics
Epirubicin pharmacokinetics are linear over the dose range of 60 to 150 mg/m2 and plasma clearance is not affected by the duration of infusion or administration schedule. Pharmacokinetic parameters for epirubicin following 6- to 10-minute, single-dose intravenous infusions of ELLENCE at doses of 60 to 150 mg/m2 in patients with solid tumors are shown in Table 4. The plasma concentration declined in a triphasic manner with mean half-lives for the alpha, beta, and gamma phases of about 3 minutes, 2.5 hours, and 33 hours, respectively.
Table 4. Summary of Mean (±SD) Pharmacokinetic Parameters in Patients * with Solid Tumors Receiving Intravenous ELLENCE 60 to 150 mg/m2 Dose †
(mg/m2 )Cmax‡
(µg/mL)AUC §
(µg∙h/mL)t1/2¶
(hours)CL#
(L/hour)VssÞ
(L/kg)60
5.7 ± 1.6
1.6 ± 0.2
35.3 ± 9
65 ± 8
21 ± 2
75
5.3 ± 1.5
1.7 ± 0.3
32.1 ± 5
83 ± 14
27 ± 11
120
9.0 ± 3.5
3.4 ± 0.7
33.7 ± 4
65 ± 13
23 ± 7
150
9.3 ± 2.9
4.2 ± 0.8
31.1 ± 6
69 ± 13
21 ± 7
Distribution
Following intravenous administration, epirubicin is rapidly and widely distributed into the tissues. Binding of epirubicin to plasma proteins, predominantly albumin, is about 77% and is not affected by drug concentration. Epirubicin also appears to concentrate in red blood cells; whole blood concentrations are approximately twice those of plasma.
Metabolism
Epirubicin is extensively and rapidly metabolized by the liver and is also metabolized by other organs and cells, including red blood cells. Four main metabolic routes have been identified:
(1) reduction of the C-13 keto-group with the formation of the 13(S)-dihydro derivative, epirubicinol; (2) conjugation of both the unchanged drug and epirubicinol with glucuronic acid; (3) loss of the amino sugar moiety through a hydrolytic process with the formation of the doxorubicin and doxorubicinol aglycones; and (4) loss of the amino sugar moiety through a redox process with the formation of the 7-deoxy-doxorubicin aglycone and 7-deoxy-doxorubicinol aglycone. Epirubicinol has in vitro cytotoxic activity one-tenth that of epirubicin. As plasma levels of epirubicinol are lower than those of the unchanged drug, they are unlikely to reach in vivo concentrations sufficient for cytotoxicity. No significant activity or toxicity has been reported for the other metabolites.
Excretion
Epirubicin and its major metabolites are eliminated through biliary excretion and, to a lesser extent, by urinary excretion. Mass-balance data from 1 patient found about 60% of the total radioactive dose in feces (34%) and urine (27%). These data are consistent with those from 3 patients with extrahepatic obstruction and percutaneous drainage, in whom approximately 35% and 20% of the administered dose were recovered as epirubicin or its major metabolites in bile and urine, respectively, in the 4 days after treatment.
Effect of Age
A population analysis of plasma data from 36 cancer patients (13 males and 23 females, 20 to 73 years) showed that age affects plasma clearance of epirubicin in female patients. The predicted plasma clearance for a female patient of 70 years of age was about 35% lower than that for a female patient of 25 years of age. An insufficient number of males > 50 years of age were included in the study to draw conclusions about age-related alterations in clearance in males. Although a lower ELLENCE starting dose does not appear necessary in elderly female patients, and was not used in clinical trials, particular care should be taken in monitoring toxicity when ELLENCE is administered to female patients > 70 years of age.
Effect of Gender
In patients ≤ 50 years of age, mean clearance values in adult male and female patients were similar. The clearance of epirubicin is decreased in elderly women.
Effect of Hepatic Impairment
Epirubicin is eliminated by both hepatic metabolism and biliary excretion and clearance is reduced in patients with hepatic dysfunction. In a study of the effect of hepatic dysfunction, patients with solid tumors were classified into 3 groups. Patients in Group 1 (n=22) had serum AST (SGOT) levels above the upper limit of normal (median: 93 IU/L) and normal serum bilirubin levels (median: 0.5 mg/dL) and were given ELLENCE doses of 12.5 to 90 mg/m2. Patients in Group 2 had alterations in both serum AST (median: 175 IU/L) and bilirubin levels (median: 2.7 mg/dL) and were treated with an ELLENCE dose of 25 mg/m2 (n=8). Their pharmacokinetics were compared to those of patients with normal serum AST and bilirubin values, who received ELLENCE doses of 12.5 to 120 mg/m2. The median plasma clearance of epirubicin was decreased compared to patients with normal hepatic function by about 30% in patients in Group 1 and by 50% in patients in Group 2. Patients with more severe hepatic impairment have not been evaluated [see Dosage and Administration (2.3), and Warnings and Precautions (5.5)].
Effect of Renal Impairment
No significant alterations in the pharmacokinetics of epirubicin or its major metabolite, epirubicinol, have been observed in patients with serum creatinine < 5 mg/dL. A 50% reduction in plasma clearance was reported in four patients with serum creatinine ≥ 5 mg/dL [see Warnings and Precautions (5.6) and Dosing and Administration (2.2)]. Patients on dialysis have not been studied.
Effect of Paclitaxel
The administration of paclitaxel (175–225 mg/m2 as a 3-hour infusion) immediately before or after epirubicin (90 mg/m2 as bolus) caused variable increases in the systemic exposure (mean AUC) of epirubicin ranging from 5% to 109%. At same doses of epirubicin and paclitaxel, the mean AUC of the inactive metabolites of epirubicin (epirubicinol and 7-deoxy-aglycone) increased by 120% and 70%, respectively, when paclitaxel was immediately administered after epirubicin. Epirubicin had no effect on the exposure of paclitaxel whether it was administered before or after paclitaxel.
Effect of Docetaxel
The administration of docetaxel (70 mg/m2 as 1-hour infusion) immediately before or after epirubicin (90 mg/m2 as bolus) had no effect on the systemic exposure (mean AUC) of epirubicin. However, the mean AUC of epirubicinol and 7-deoxy-aglycone increased by 22.5% and 95%, respectively, when docetaxel was immediately administered after epirubicin compared to epirubicin alone. Epirubicin had no effect on the exposure of docetaxel whether it was administered before or after docetaxel.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Conventional long-term animal studies to evaluate the carcinogenic potential of epirubicin have not been conducted, but intravenous administration of a single 3.6 mg/kg epirubicin dose to female rats (about 0.2 times the maximum recommended human dose on a body surface area basis) approximately doubled the incidence of mammary tumors (primarily fibroadenomas) observed at 1 year. Administration of 0.5 mg/kg epirubicin intravenously to rats (about 0.025 times the maximum recommended human dose on a body surface area basis) every 3 weeks for ten doses increased the incidence of subcutaneous fibromas in males over an 18-month observation period. In addition, subcutaneous administration of 0.75 or 1.0 mg/kg/day (about 0.015 times the maximum recommended human dose on a body surface area basis) to newborn rats for 4 days on both the first and tenth day after birth for a total of eight doses increased the incidence of animals with tumors compared to controls during a 24-month observation period.
Epirubicin was mutagenic in vitro to bacteria (Ames test) either in the presence or absence of metabolic activation and to mammalian cells (HGPRT assay in V79 Chinese hamster lung fibroblasts) in the absence but not in the presence of metabolic activation. Epirubicin was clastogenic in vitro (chromosome aberrations in human lymphocytes) both in the presence and absence of metabolic activation and was also clastogenic in vivo (chromosome aberration in mouse bone marrow).
In fertility studies in rats, males were given epirubicin daily for 9 weeks and mated with females that were given epirubicin daily for 2 weeks prior to mating and through Day 7 of gestation. When 0.3 mg/kg/day (about 0.015 times the maximum recommended human single dose on a body surface area basis) was administered to both sexes, no pregnancies resulted. No effects on mating behavior or fertility were observed at 0.1 mg/kg/day, but male rats had atrophy of the testes and epididymis, and reduced spermatogenesis. The 0.1 mg/kg/day dose also caused embryolethality. An increased incidence of fetal growth retardation was observed in these studies at 0.03 mg/kg/day (about 0.0015 times the maximum recommended human single dose on a body surface area basis). Multiple daily doses of epirubicin to rabbits and dogs also caused atrophy of male reproductive organs. Single 20.5 and 12 mg/kg doses of intravenous epirubicin caused testicular atrophy in mice and rats, respectively (both approximately 0.5 times the maximum recommended human dose on a body surface area basis). A single dose of 16.7 mg/kg epirubicin caused uterine atrophy in rats.
-
14 CLINICAL STUDIES
14.1 Adjuvant Treatment of Breast Cancer
Two randomized, open-label, multicenter studies evaluated the use of ELLENCE 100 to 120 mg/m2 in combination with cyclophosphamide and fluorouracil for the adjuvant treatment of patients with axillary-node positive breast cancer and no evidence of distant metastatic disease (Stage II or III). Study MA-5 evaluated 120 mg/m2 of ELLENCE per course in combination with cyclophosphamide and fluorouracil (CEF-120 regimen). This study randomized premenopausal and perimenopausal women with one or more positive lymph nodes to an ELLENCE-containing CEF-120 regimen or to a CMF regimen. Study GFEA-05 evaluated the use of 100 mg/m2 of ELLENCE per course in combination with fluorouracil and cyclophosphamide (FEC-100). This study randomized pre- and postmenopausal women to the FEC-100 regimen or to a lower-dose FEC-50 regimen. In the GFEA-05 study, eligible patients were either required to have ≥ 4 nodes involved with tumor or, if only 1 to 3 nodes were positive, to have negative estrogen- and progesterone-receptors and a histologic tumor grade of 2 or 3. A total of 1281 women participated in these studies. Patients with T4 tumors were not eligible for either study. Table 5 shows the treatment regimens that the patients received. Relapse-free survival was defined as time to occurrence of a local, regional, or distant recurrence, or disease-related death. Patients with contralateral breast cancer, second primary malignancy, or death from causes other than breast cancer were censored at the time of the last visit prior to these events.
Table 5. Treatment Regimens Used in Phase 3 Studies of Patients with Early Breast Cancer Treatment Groups Agent Regimen - *
- In women who underwent lumpectomy, breast irradiation was to be administered after completion of study chemotherapy.
- †
- Patients also received prophylactic antibiotic therapy with trimethoprim-sulfamethoxazole or fluoroquinolone for the duration of their chemotherapy.
- ‡
- All women were to receive breast irradiation after the completion of chemotherapy.
MA-5*
N=716CEF-120 (total, 6 cycles)† N=356
CMF (total, 6 cycles) N=360Cyclophosphamide
ELLENCE
Fluorouracil
Cyclophosphamide
Methotrexate
Fluorouracil75 mg/m2 PO, d 1–14, q 28 days
60 mg/m2 IV, d 1 & 8, q 28 days
500 mg/m2 IV, d 1 & 8, q 28 days
100 mg/m2 PO, d 1–14, q 28 days
40 mg/m2 IV, d 1 & 8, q 28 days
600 mg/m2 IV, d 1 & 8, q 28 daysGFEA-05‡
N=565FEC-100 (total, 6 cycles)
N=276
FEC-50 (total, 6 cycles)
N=289
Tamoxifen 30 mg daily × 3 years, postmenopausal women, any receptor statusFluorouracil
ELLENCE
Cyclophosphamide
Fluorouracil
ELLENCE
Cyclophosphamide500 mg/m2 IV, d 1, q 21 days
100 mg/m2 IV, d 1, q 21 days
500 mg/m2 IV, d 1, q 21 days
500 mg/m2 IV, d 1, q 21 days
50 mg/m2 IV, d 1, q 21 days
500 mg/m2 IV, d 1, q 21 daysIn the MA-5 trial, the median age of the study population was 45 years. Approximately 60% of patients had 1 to 3 involved nodes and approximately 40% had ≥ 4 nodes involved with tumor. In the GFEA-05 study, the median age was 51 years and approximately half of the patients were postmenopausal. About 17% of the study population had 1 to 3 positive nodes and 80% of patients had ≥ 4 involved lymph nodes. Demographic and tumor characteristics were well-balanced between treatment arms in each study.
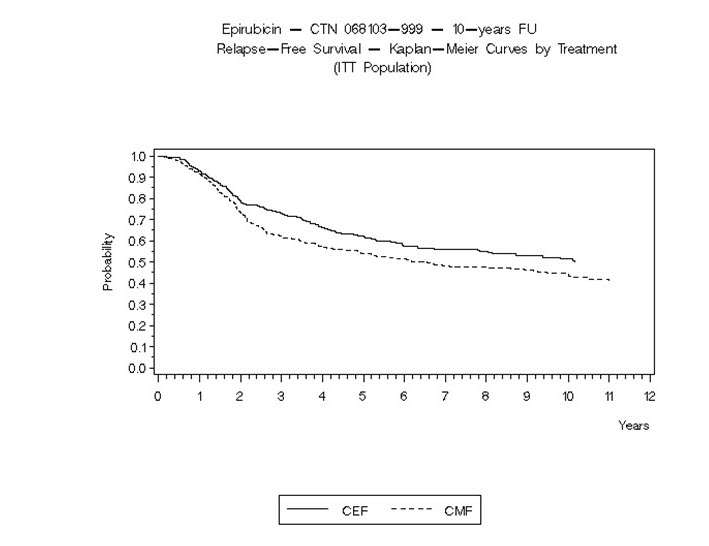
Relapse-free survival (RFS) and overall survival (OS) were analyzed using Kaplan-Meier methods in the intent-to-treat (ITT) patient populations in each study. Results were initially analyzed after up to 5 years of follow-up and these results are presented in the text below and in Table 6. Results after up to 10 years of follow-up are presented in Table 6. In Study MA-5, ELLENCE-containing combination therapy (CEF-120) showed significantly longer RFS than CMF (5-year estimates were 62% versus 53%, stratified logrank for the overall RFS p=0.013). The estimated reduction in the risk of relapse was 24% at 5 years. The OS was also greater for the ELLENCE-containing CEF-120 regimen than for the CMF regimen (5-year estimate 77% versus 70%; stratified logrank for overall survival p=0.043; non-stratified logrank p=0.13). The estimated reduction in the risk of death was 29% at 5 years.
In Study GFEA-05, patients treated with the higher-dose ELLENCE regimen (FEC-100) had a significantly longer 5-year RFS (estimated 65% versus 52%, logrank for the overall RFS p=0.007) and OS (estimated 76% versus 65%, logrank for the overall survival p=0.007) than patients given the lower dose regimen (FEC-50). The estimated reduction in risk of relapse was 32% at 5 years. The estimated reduction in the risk of death was 31% at 5 years. Results of follow-up up to 10 years (median follow-up = 8.8 years and 8.3 years, respectively, for Study MA-5 and Study GFEA-05) are presented in Table 6.
Although the trials were not powered for subgroup analyses, in the MA-5 study, improvements in favor of CEF-120 vs. CMF were observed, in RFS and OS both in patients with 1–3 node positive and in those with ≥4 node positive tumor involvement. In the GFEA-05 study, improvements in RFS and OS were observed in both pre-and postmenopausal women treated with FEC-100 compared to FEC-50.
Table 6. Efficacy Results from Phase 3 Studies of Patients with Early Breast Cancer* MA-5 Study GFEA-05 Study CEF-120
N=356CMF
N=360FEC-100
N=276FEC-50
N=289- *
- Based on Kaplan-Meier estimates
- †
- Hazard ratio: CMF:CEF-120 in MA-5, FEC-50:FEC-100 in GFEA-05
- ‡
- Patients in MA-5 were stratified by nodal status (1–3, 4–10, and >10 positive nodes), type of initial surgery (lumpectomy versus mastectomy), and by hormone receptor status (ER or PR positive (≥10 fmol), both negative (<10 fmol), or unknown status). Patients in GFEA-05 were stratified by nodal status (1–3, 4–10, and >10 positive nodes).
RFS at 5 yrs (%)
62
53
65
52
Hazard ratio†
0.76
0.68
2-sided 95% CI
(0.60, 0.96)
(0.52, 0.89)
Logrank Test stratified‡
(p = 0.013)
(p = 0.007)
OS at 5 yrs (%)
77
70
76
65
Hazard ratio†
0.71
0.69
2-sided 95% CI
(0.52, 0.98)
(0.51, 0.92)
Logrank Test stratified‡
(p = 0.043)
(p = 0.007)
(unstratified p = 0.13)
RFS at 10 yrs (%)
51
44
49
43
Hazard ratio†
0.78
0.78
2-sided 95% CI
(0.63, 0.95)
(0.62, 0.99)
Logrank Test stratified‡
(p = 0.017)
(p = 0.040)
(unstratified p = 0.023)
(unstratified p = 0.09)
OS at 10 yrs (%)
61
57
56
50
Hazard ratio†
0.82
0.75
2-sided 95% CI
(0.65, 1.04)
(0.58, 0.96)
Logrank Test stratified‡
(p = 0.100)
(p = 0.023)
(unstratified p = 0.18)
(unstratified p = 0.039)
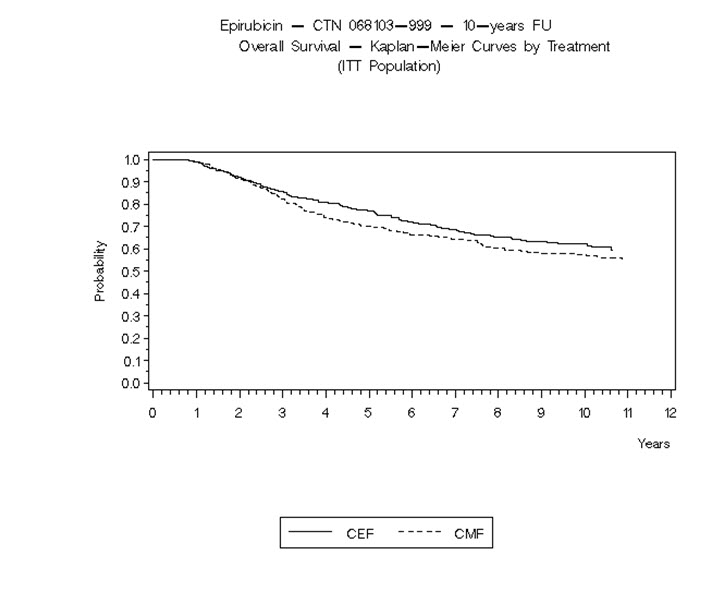
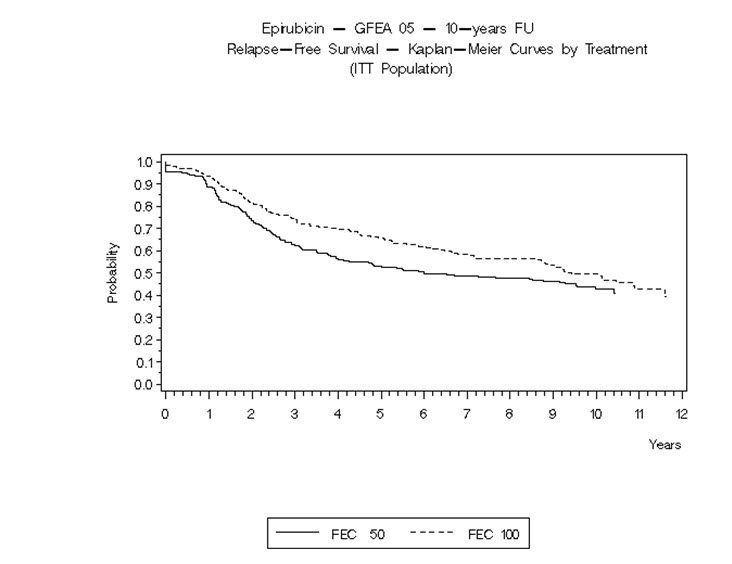
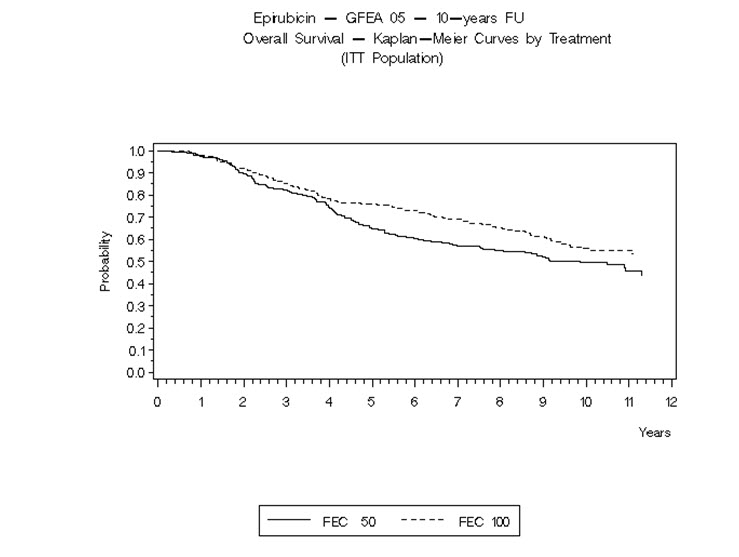
The Kaplan-Meier curves for RFS and OS from Study MA-5 are shown in Figures 3 and 4 and those for Study GFEA-05 are shown in Figures 5 and 6.
- Figure 3. Relapse-Free Survival in Study MA-5
- Figure 4. Overall Survival in Study MA-5
- Figure 5. Relapse-Free Survival in Study GFEA-05
- Figure 6. Overall Survival in Study GFEA-05
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ELLENCE is available in polypropylene single-dose CYTOSAFE™ vials containing 2 mg epirubicin hydrochloride per mL as a sterile, preservative-free, ready-to-use, clear, red solution in the following strengths:
50 mg/25 mL Carton of one single-dose vial
NDC 0009-5091-01
200 mg/100 mL Carton of one single-dose vial
NDC 0009-5093-01
Discard unused portion.
Store refrigerated between 2°C and 8°C (36°F and 46°F). Do not freeze. Protect from light.
Storage of the solution for injection at refrigerated conditions can result in the formation of a gelled product. This gelled product will return to a slightly viscous to mobile solution after 2 to a maximum of 4 hours equilibration at controlled room temperature (15–25°C). Solution for injection should be used within 24 hours after removal from refrigeration.
ELLENCE is a cytotoxic drug. Follow applicable special handling and disposal procedures1 [see References (15)].
-
17 PATIENT COUNSELING INFORMATION
Cardiac Toxicity
Inform patients that there is a risk of irreversible myocardial damage associated with treatment with ELLENCE. Advise patients to immediately contact their healthcare provider or to go to an emergency room for new onset of chest pain, shortness of breath, dizziness, or lightheadedness [see Warnings and Precautions (5.1)].
Secondary Malignancies
Inform patients that there is an increased risk of treatment-related leukemia from ELLENCE [see Warnings and Precautions (5.2)].
Extravasation and Tissue Necrosis
Inform patients that ELLENCE can cause severe injection site reactions. Advise patients to contact a healthcare provider if injection site pain occurs after receiving ELLENCE [see Warnings and Precautions (5.3)].
Severe Myelosuppression
Inform patients that ELLENCE can cause leukopenia, thrombocytopenia, or anemia. Advise patients to contact a healthcare provider for new onset fever or symptoms of infection [see Warnings and Precautions (5.4)].
Nausea and Vomiting
Inform patients that ELLENCE can cause nausea or vomiting. Advise patients to contact a healthcare provider should they develop any severe symptoms [see Adverse Reactions (6.1)].
Common Adverse Reactions
Inform patients of the expected adverse effects of ELLENCE, including diarrhea, stomatitis, and alopecia [see Adverse Reactions (6.1)].
Red Coloration of Urine
Advise patients that their urine may appear red for 1 to 2 days after administration of ELLENCE and that they should not be alarmed [see Adverse Reactions (6.2)].
Embryo-Fetal Toxicity
- •
- Advise pregnant women and females of reproductive potential of the potential risk to a fetus, and to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.11) and Use in Specific Populations (8.1)].
- •
- Advise female patients of reproductive potential to use effective contraception during treatment with ELLENCE and for 6 months after the last dose [see Warnings and Precautions (5.11) and Use in Specific Populations (8.3)].
- •
- Advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of ELLENCE. Advise male patients with pregnant partners to use condoms during treatment and for at least 7 days after the last dose of ELLENCE [see Use in Specific Populations (8.3)].
Lactation
Advise female patients not to breastfeed during treatment with ELLENCE and for at least 7 days after the last dose [see Use in Specific Populations (8.2)].
Infertility
Women treated with ELLENCE may develop irreversible amenorrhea, or premature menopause. Advise patients that ELLENCE may impair female and male fertility [see Use in Specific Populations (8.3)].
-
SPL UNCLASSIFIED SECTION
This product's labeling may have been updated. For the most recent prescribing information, please visit www.pfizer.com.
LAB-0078-14.0
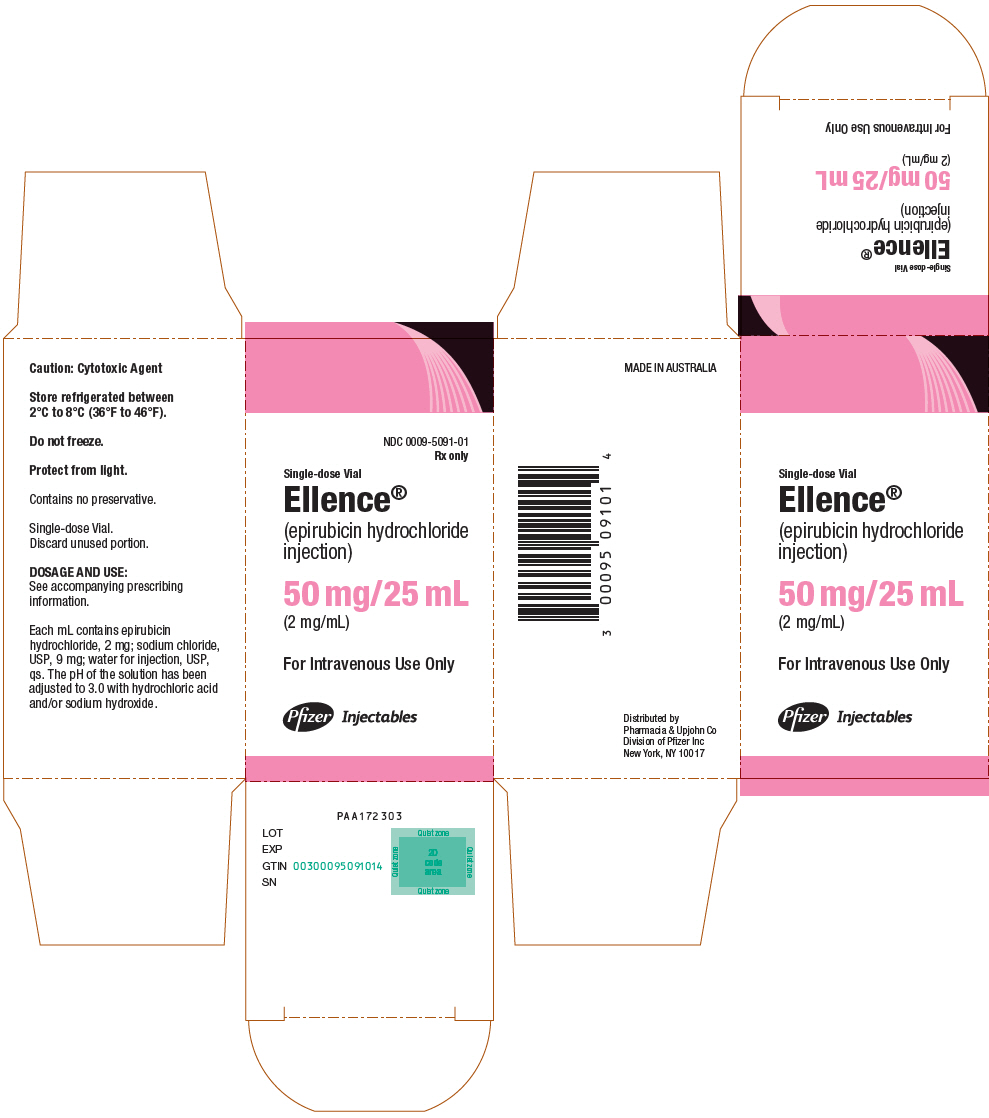
- PRINCIPAL DISPLAY PANEL - 50 mg/25 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 50 mg/25 mL Vial Carton
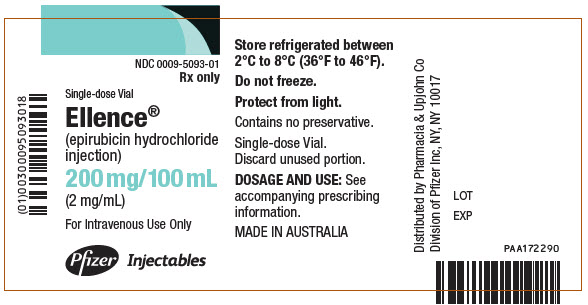
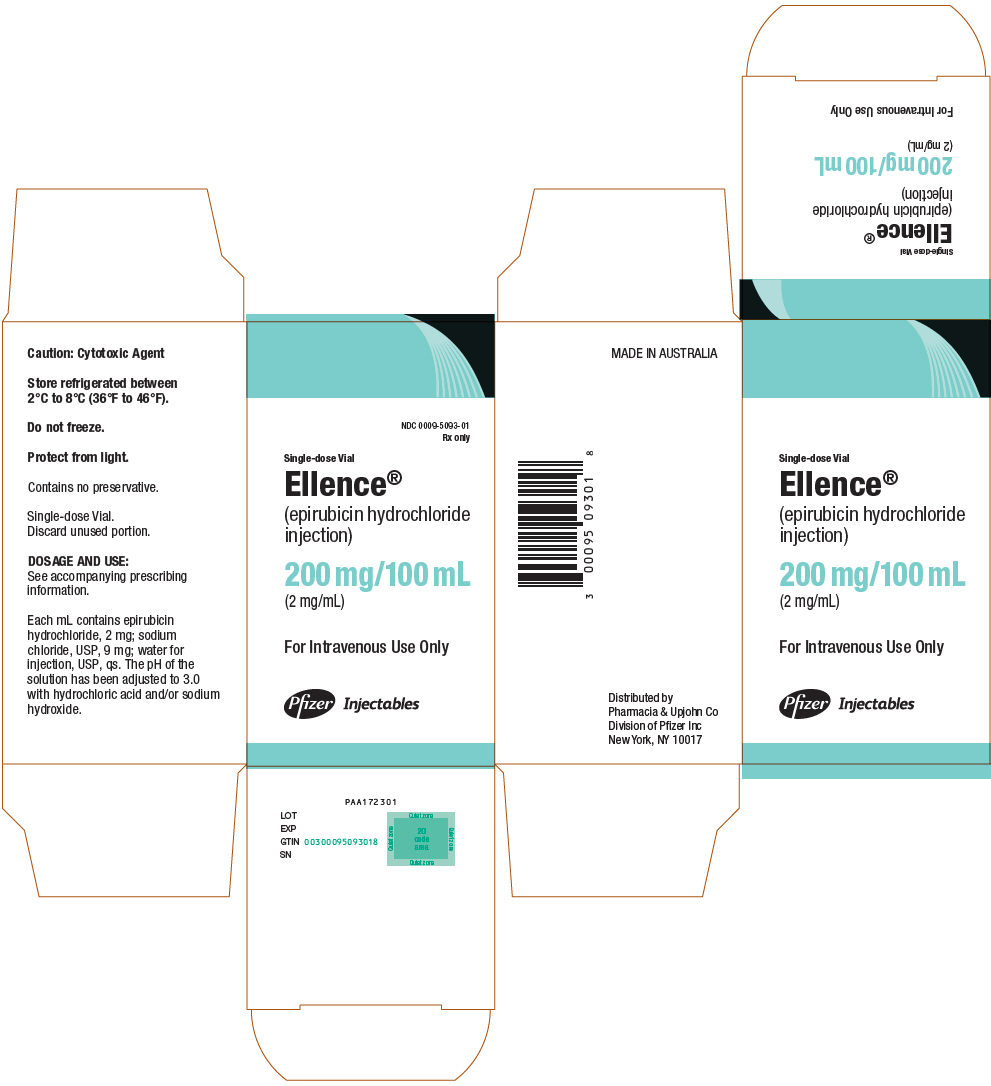
- PRINCIPAL DISPLAY PANEL - 200 mg/100 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 200 mg/100 mL Vial Carton
-
INGREDIENTS AND APPEARANCE
ELLENCE
epirubicin hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0009-5091 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength EPIRUBICIN HYDROCHLORIDE (UNII: 22966TX7J5) (EPIRUBICIN - UNII:3Z8479ZZ5X) EPIRUBICIN HYDROCHLORIDE 2 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0009-5091-01 1 in 1 CARTON 09/15/1999 1 25 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050778 09/15/1999 ELLENCE
epirubicin hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0009-5093 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength EPIRUBICIN HYDROCHLORIDE (UNII: 22966TX7J5) (EPIRUBICIN - UNII:3Z8479ZZ5X) EPIRUBICIN HYDROCHLORIDE 2 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0009-5093-01 1 in 1 CARTON 09/15/1999 1 100 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050778 09/15/1999 Labeler - Pharmacia & Upjohn Company LLC (618054084)