Label: PROCHLORPERAZINE EDISYLATE injection
-
Contains inactivated NDC Code(s)
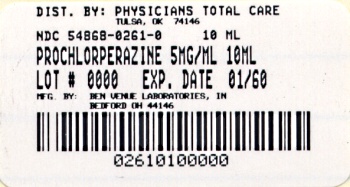
NDC Code(s): 54868-0261-0 - Packager: Physicians Total Care, Inc.
- This is a repackaged label.
- Source NDC Code(s): 55390-077
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated April 21, 2010
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
SPL UNCLASSIFIED SECTION
Rx ONLY
WARNING
Increased Mortality in Elderly Patients with Dementia-Related Psychosis — Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10 week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is
not clear. Prochlorperazine Edisylate Injection is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS).
-
DESCRIPTION
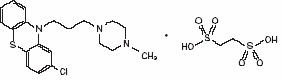
Prochlorperazine Edisylate Injection USP, 2-Chloro-10-[3-(4-methyl-1-piperazinyl)propyl]phenothiazine 1,2-ethanedisulfonate (1:1), has the following structural formula:
Molecular Formula: C20H24CIN3S•C2H6O6S2 M.W. = 564.14
Prochlorperazine Edisylate Injection, an antiemetic and antipsychotic, is a sterile solution intended for intramuscular or intravenous administration.
Each mL contains, in aqueous solution, 5 mg prochlorperazine as the edisylate salt, 5 mg sodium biphosphate, 12 mg sodium tartrate, 0.9 mg sodium saccharin and 0.75% benzyl alcohol as preservative. The pH range is 4.2 to 6.2.
-
CLINICAL PHARMACOLOGY
Prochlorperazine is a propylpiperazine derivative of phenothiazine. Like other phenothiazines, it exerts an antiemetic effect through a depressant action on the chemoreceptor trigger zone. It also has a clinically useful antipsychotic effect. Following intramuscular administration of prochlorperazine edisylate, the drug has an onset of action within ten to twenty minutes and a duration of action of three to four hours.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Do not use in patients with known hypersensitivity to phenothiazines.
Do not use in comatose states or in the presence of large amounts of central nervous system depressants (alcohol, barbiturates, narcotics, etc.).
Do not use in pediatric surgery.
Do not use in pediatric patients under 2 years of age or under 20 lbs. Do not use in children for conditions for which dosage has not been established.
-
WARNINGS
Increased Mortality in Elderly Patients with Dementia-Related Psychosis: Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Prochlorperazine Edisylate Injection is not approved for the treatment of patients with dementia-related psychosis (see BOXED WARNING).
The extrapyramidal symptoms which can occur secondary to prochlorperazine may be confused with the central nervous system signs of an undiagnosed primary disease responsible for the vomiting, e.g., Reye's syndrome or other encephalopathy. The use of prochlorperazine and other potential hepatotoxins should be avoided in children and adolescents whose signs and symptoms suggest Reye's syndrome.
Tardive Dyskinesia
Tardive dyskinesia, a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements, may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic drug treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic drug treatment is withdrawn. Antipsychotic drug treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying disease process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotic drugs should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on PRECAUTIONS and ADVERSE REACTIONS.
Neuroleptic Malignant Syndrome (NMS)
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
General
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine should not receive any phenothiazine, including prochlorperazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazards.
Prochlorperazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
Phenothiazines may intensify or prolong the action of central nervous system depressants (e.g., alcohol, anesthetics, narcotics).
- Nursing Mothers
-
Geriatric Use
Geriatric Use: Clinical studies of prochlorperazine did not include sufficient numbers of subjects aged 65 and over to determine whether elderly subjects respond differently from younger subjects. Geriatric patients are more sensitive to the side effects of antipsychotics, including prochlorperazine. These adverse events include hypotension, anticholinergic effects (such as urinary retention, constipation, and confusion), and neuromuscular reactions (such as parkinsonism and tardive dyskinesia) (see PRECAUTIONS and ADVERSE REACTIONS). Also, postmarketing safety experience suggests that the incidence of agranulocytosis may be higher in geriatric patients compared to younger individuals who received prochlorperazine. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy (see DOSAGE AND ADMINISTRATION).
-
PRECAUTIONS
Leukopenia, Neutropenia and Agranulocytosis: In clinical trial and postmarketing experience, events of leukopenia/neutropenia and agranulocytosis have been reported temporally related to antipsychotic agents.
Possible risk factors for leukopenia/neutropenia include preexisting low white blood cell count (WBC) and history of drug induced leukopenia/neutropenia. Patients with a preexisting low WBC or a history of drug induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue Prochlorperazine Edisylate Injection USP at the first sign of a decline in WBC in the absence of other causative factors.
Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000/mm3) should discontinue Prochlorperazine Edisylate Injection USP and have their WBC followed until recovery.
Prochlorperazine's antiemetic action may mask signs and symptoms of overdosage of other drugs and may obscure the diagnosis and treatment of other conditions such as intestinal obstruction, brain tumor and Reye's syndrome (see WARNINGS).
When prochlorperazine is used with cancer chemotherapeutic drugs, vomiting as a sign of the toxicity of these agents may be obscured by the antiemetic effect of prochlorperazine.
Because hypotension may occur, large doses and parenteral administration should be used cautiously in patients with impaired cardiovascular systems. To minimize the occurrence of hypotension after injection, keep patient lying down and observe for at least 1/2 hour. If hypotension occurs after parenteral dosing, place patient in head-low position with legs raised. If a vasoconstrictor is required, norepinephrine and phenylephrine are suitable. Other pressor agents, including epinephrine, should not be used because they may cause a paradoxical further lowering of blood pressure.
Aspiration of vomitus has occurred in a few post-surgical patients who have received prochlorperazine as an antiemetic. Although no causal relationship has been established, this possibility should be borne in mind during surgical aftercare.
Deep sleep, from which patients can be aroused, and coma have been reported, usually with overdosage.
Antipsychotic drugs elevate prolactin levels; the elevation persists during chronic administration. Tissue culture experiments indicate that approximately one third of human breast cancers are prolactin-dependent in vitro, a factor of potential importance if the prescribing of these drugs is contemplated in a patient with a previously detected breast cancer. Although disturbances such as galactorrhea, amenorrhea, gynecomastia and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients. An increase in mammary neoplasms has been found in rodents after chronic administration of antipsychotic drugs. Neither clinical nor epidemiologic studies conducted to date, however, have shown an association between chronic administration of these drugs and mammary tumorigenesis; the available evidence is considered too limited to be conclusive at this time.
Chromosomal aberrations in spermatocytes and abnormal sperm have been demonstrated in rodents treated with certain antipsychotics.
As with all drugs which exert an anticholinergic effect, and/or cause mydriasis, prochlorperazine should be used with caution in patients with glaucoma.
Because phenothiazines may interfere with thermoregulatory mechanisms, use with caution in persons who will be exposed to extreme heat.
Phenothiazines can diminish the effect of oral anticoagulants.
Phenothiazines can produce alpha-adrenergic blockade.
Thiazide diuretics may accentuate the orthostatic hypotension that may occur with phenothiazines.
Antihypertensive effects of guanethidine and related compounds may be counteracted when phenothiazines are used concomitantly.
Concomitant administration of propranolol with phenothiazines results in increased plasma levels of both drugs.
Phenothiazines may lower the convulsive threshold; dosage adjustments of anticonvulsants may be necessary. Potentiation of anti-convulsant effects does not occur. However, it has been reported that phenothiazines may interfere with the metabolism of phenytoin and thus precipitate phenytoin toxicity.
The presence of phenothiazines may produce false-positive phenylketonuria (PKU) test results.
Long-Term Therapy
Given the likelihood that some patients exposed chronically to antipsychotics will develop tardive dyskinesia, it is advised that all patients in whom chronic use is contemplated be given, if possible, full information about this risk. The decision to inform patients and/or their guardians must obviously take into account the clinical circumstances and the competency of the patient to understand the information provided.
To lessen the likelihood of adverse reactions related to cumulative drug effect, patients with a history of long-term therapy with prochlorperazine and/or other antipsychotics should be evaluated periodically to decide whether the maintenance dosage could be lowered or drug therapy discontinued.
Children with acute illnesses (e.g., chickenpox, CNS infections, measles, gastroenteritis) or dehydration seem to be much more susceptible to neuromuscular reactions, particularly dystonias, than are adults. In such patients, the drug should be used only under close supervision.
Drugs which lower the seizure threshold, including phenothiazine derivatives, should not be used with metrizamide. As with other phenothiazine derivatives, prochlorperazine should be discontinued at least 48 hours before myelography, should not be resumed for at least 24 hours postprocedure, and should not be used for the control of nausea and vomiting occurring either prior to myelography with metrizamide, or postprocedure.
Pregnancy: Non-teratogenic Effects
Neonates exposed to antipsychotic drugs, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. There have been reports of agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization.
Prochlorperazine edisylate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
-
ADVERSE REACTIONS
Drowsiness, dizziness, amenorrhea, blurred vision, skin reactions and hypotension may occur. Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs (see WARNINGS).
Cholestatic jaundice has occurred. If fever with grippe-like symptoms occurs, appropriate liver studies should be conducted. If tests indicate an abnormality, stop treatment. There have been a few observations of fatty changes in the livers of patients who have died while receiving the drug. No causal relationship has been established.
Leukopenia and agranulocytosis have occurred. Warn patients to report the sudden appearance of sore throat or other signs of infection. If white blood cell and differential counts indicate leukocyte depression, stop treatment and start antibiotic and other suitable therapy.
Neuromuscular (Extrapyramidal) Reactions
These symptoms are seen in a significant number of hospitalized mental patients. They may be characterized by motor restlessness, be of the dystonic type, or they may resemble parkinsonism.
Depending on the severity of symptoms, dosage should be reduced or discontinued. If therapy is reinstituted, it should be at a lower dosage. Should these symptoms occur in children or pregnant patients, the drug should be stopped and not reinstituted. In most cases barbiturates by suitable route of administration will suffice, or injectable diphenhydramine may be useful.
In more severe cases, the administration of an anti-parkinsonism agent, except levodopa, usually produces rapid reversal of symptoms. Suitable supportive measures such as maintaining a clear airway and adequate hydration should be employed.
Motor Restlessness
Symptoms may include agitation or jitteriness and sometimes insomnia. These symptoms often disappear spontaneously. At times these symptoms may be similar to the original neurotic or psychotic symptoms. Dosage should not be increased until these side effects have subsided.
If these symptoms become too troublesome, they can usually be controlled by a reduction of dosage or change of drug. Treatment with antiparkinsonian agents, benzodiazepines or propranolol may be helpful.
Dystonia
Class effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Pseudo-parkinsonism
Symptoms may include: mask-like facies; drooling; tremors; pillrolling motion; cogwheel rigidity; and shuffling gait. Reassurance and sedation are important. In most cases these symptoms are readily controlled when an anti-parkinsonism agent is administered concomitantly. Anti-parkinsonism agents should be used only when required. Generally, therapy of a few weeks to 2 or 3 months will suffice. After this time patients should be evaluated to determine their need for continued treatment. (Note: Levodopa has not been found effective in pseudo-parkinsonism.) Occasionally it is necessary to lower the dosage of prochlorperazine or to discontinue the drug.
Tardive Dyskinesia
As with all antipsychotic agents, tardive dyskinesia may appear in some patients on long-term therapy or may appear after drug therapy has been discontinued. The syndrome can also develop, although much less frequently, after relatively brief treatment periods at low doses. This syndrome appears in all age groups. Although its prevalence appears to be highest among elderly patients, especially elderly women, it is impossible to rely upon prevalence estimates to predict at the inception of antipsychotic treatment which patients are likely to develop the syndrome. The symptoms are persistent and in some patients appear to be irreversible. The syndrome is characterized by rhythmical involuntary movements of the tongue, face, mouth or jaw (e.g., protrusion of tongue, puffing of cheeks, puckering of mouth, chewing movements). Sometimes these may be accompanied by involuntary movements of extremities. In rare instances, these involuntary movements of the extremities are the only manifestations of tardive dyskinesia. A variant of tardive dyskinesia, tardive dystonia, has also been described.
There is no known effective treatment for tardive dyskinesia; anti-parkinsonism agents do not alleviate the symptoms of this syndrome. It is suggested that all antipsychotic agents be discontinued if these symptoms appear. Should it be necessary to reinstitute treatment, or increase the dosage of the agent, or switch to a different antipsychotic agent, the syndrome may be masked.
It has been reported that fine vermicular movements of the tongue may be an early sign of the syndrome and if the medication is stopped at that time the syndrome may not develop.
Contact Dermatitis
Avoid getting the injection solution on hands or clothing because of the possibility of contact dermatitis.
Adverse Reactions Reported with Prochlorperazine or Other Phenothiazine Derivatives
Adverse reactions with different phenothiazines vary in type, frequency and mechanism of occurrence, i.e., some are dose-related, while others involve individual patient sensitivity. Some adverse reactions may be more Iikely to occur, or occur with greater intensity, in patients with special medical problems, e.g., patients with mitral insufficiency or pheochromocytoma have experienced severe hypotension following recommended doses of certain phenothiazines.
Not all of the following adverse reactions have been observed with every phenothiazine derivative, but they have been reported with 1 or more and should be borne in mind when drugs of this class are administered: extrapyramidal symptoms (opisthotonos, oculogyric crisis, hyperreflexia, dystonia, akathisia, dyskinesia, parkinsonism) some of which have lasted months and even years -- particularly in elderly patients with previous brain damage; grand mal and petit mal convulsions, particularly in patients with EEG abnormalities or history of such disorders; altered cerebrospinal fluid proteins; cerebral edema; intensification and prolongation of the action of central nervous system depressants (opiates, analgesics, antihistamines, barbiturates, alcohol), atropine, heat, organophosphorus insecticides; autonomic reactions (dryness of mouth, nasal congestion, headache, nausea, constipation, obstipation, adynamic ileus, ejaculatory disorders/impotence, priapism, atonic colon, urinary retention, miosis and mydriasis); reactivation of psychotic processes, catatonic-like states; hypotension (sometimes fatal); cardiac arrest; blood dyscrasias (pancytopenia, thrombocytopenic purpura, leukopenia, agranulocytosis, eosinophilia, hemolytic anemia, aplastic anemia; liver damage (jaundice, biliary stasis); endocrine disturbances (hyperglycemia, hypoglycemia, glycosuria, lactation, galactorrhea, gynecomastia, menstrual irregularities, false-positive pregnancy tests); skin disorders (photosensitivity, itching, erythema, urticaria, eczema up to exfoliative dermatitis); other allergic reactions (asthma, laryngeal edema, angioneurotic edema, anaphylactoid reactions); peripheral edema; reversed epinephrine effect; hyperpyrexia; mild fever after large I.M. doses; increased appetite; increased weight; a systemic lupus erythematosus-like syndrome; pigmentary retinopathy; with prolonged administration of substantial doses, skin pigmentation, epithelial keratopathy, and lenticular and corneal deposits.
EKG changes -- particularly nonspecific, usually reversible Q and T wave distortions -- have been observed in some patients receiving phenothiazine tranquilizers.
Although phenothiazines cause neither psychic nor physical dependence, sudden discontinuance in long-term psychiatric patients may cause temporary symptoms, e.g., nausea and vomiting, dizziness, tremulousness.
Note: There have been occasional reports of sudden death in patients receiving phenothiazines. In some cases, the cause appeared to be cardiac arrest or asphyxia due to failure of the cough reflex.
-
OVERDOSAGE
(See also ADVERSE REACTIONS.)
SYMPTOMS
Primarily involvement of the extrapyramidal mechanism producing some of the dystonic reactions described above. Symptoms of central nervous system depression to the point of somnolence or coma. Agitation and restlessness may also occur. Other possible manifestations include convulsions, EKG changes and cardiac arrhythmias, fever and autonomic reactions such as hypotension, dry mouth and ileus.
TREATMENT
It is important to determine other medications taken by the patient since multiple-drug therapy is common in overdosage situations. Treatment is essentially symptomatic and supportive. Keep patient under observation and maintain an open airway, since involvement of the extrapyramidal mechanism may produce dysphagia and respiratory difficulty in severe overdosage. Extrapyramidal symptoms may be treated with anti-parkinsonism drugs, barbiturates or diphenhydramine hydrochloride. See prescribing information for these products. Care should be taken to avoid increasing respiratory depression.
If administration of a stimulant is desirable, amphetamine, dextroamphetamine or caffeine and sodium benzoate is recommended.
Stimulants that may cause convulsions (e.g., picrotoxin or pentylenetetrazol) should be avoided.
If hypotension occurs, the standard measures for managing circulatory shock should be initiated. If it is desirable to administer a vasoconstrictor, norepinephrine and phenylephrine are most suitable. Other pressor agents, including epinephrine, are not recommended because phenothiazine derivatives may reverse the usual elevating action of these agents and cause a further lowering of blood pressure.
Limited experience indicates that phenothiazines are not dialyzable.
-
DOSAGE AND ADMINISTRATION
Notes on Injection
For intramuscular administration, inject deeply into the upper, outer quadrant of the buttock. Subcutaneous administration is not advisable because of local irritation.
ADULTS
(For children's dosage and administration, see below.) Dosage should be increased more gradually in debilitated or emaciated patients.
Elderly Patients
In general, dosages in the lower range are sufficient for most elderly patients. Since they appear to be more susceptible to hypotension and neuromuscular reactions, such patients should be observed closely. Dosage should be tailored to the individual, response carefully monitored and dosage adjusted accordingly. Dosage should be increased more gradually in elderly patients.
To Control Severe Nausea and Vomiting: Adjust dosage to the response of the individual. Begin with the lowest recommended dosage.
I.M. Dosage: Initially 5 to 10 mg (1 to 2 mL) injected deeply into the upper outer quadrant of the buttock. If necessary, repeat every 3 or 4 hours. Total I.M. dosage should not exceed 40 mg per day.
I.V. Dosage: 2.5 to 10 mg (0.5 to 2 mL) by slow I.V. injection or infusion at a rate not to exceed 5 mg per minute. Prochlorperazine edisylate injection may be administered either undiluted or diluted in isotonic solution. A single dose of the drug should not exceed 10 mg; total I.V. dosage should not exceed 40 mg per day. When administered I.V., do not use bolus injection. Hypotension is a possibility if the drug is given by I.V. injection or infusion.
Subcutaneous administration is not advisable because of local irritation.Adult Surgery (for severe nausea and vomiting): Total parenteral dosage should not exceed 40 mg per day. Hypotension is a possibility if the drug is given by I.V. injection or infusion.
I.M. Dosage: 5 to 10 mg (1 to 2 mL) 1 to 2 hours before induction of anesthesia (repeat once in 30 minutes, if necessary), or to control acute symptoms during and after surgery (repeat once if necessary).
I.V. Dosage: 5 to 10 mg (1 to 2 mL) as a slow I.V. injection or infusion 15 to 30 minutes before induction of anesthesia, or to control acute symptoms during or after surgery. Repeat once if necessary. Prochlorperazine may be administered either undiluted or diluted in isotonic solution, but a single dose of the drug should not exceed 10 mg. The rate of administration should not exceed 5 mg per minute. When administered I.V., do not use bolus injection.In Adult Psychiatric Disorders: Adjust dosage to the response of the individual and according to the severity of the condition. Begin with the lowest recommended dose. Although response ordinarily is seen within a day or 2, longer treatment is usually required before maximal improvement is seen.
I.M. Dosage: For immediate control of adult schizophrenic patients with severe symptomatology, inject an initial dose of 10 to 20 mg (2 to 4 mL) deeply into the upper outer quadrant of the buttock. Many patients respond shortly after the first injection. If necessary, however, repeat the initial dose every 2 to 4 hours (or, in resistant cases, every hour) to gain control of the patient. More than three or four doses are seldom necessary. After control is achieved, switch patient to an oral form of the drug at the same dosage level or higher. If, in rare cases, parenteral therapy is needed for a prolonged period, give 10 to 20 mg (2 to 4 mL) every 4 to 6 hours. Pain and irritation at the site of injection have seldom occurred.
Subcutaneous administration is not advisable because of local irritation.CHILDREN
DO NOT USE IN PEDIATRIC SURGERY.
Children seem more prone to develop extrapyramidal reactions, even on moderate doses. Therefore, use lowest effective dosage. Tell parents not to exceed prescribed dosage, since the possibility of adverse reactions increases as dosage rises.
Occasionally the patient may react to the drug with signs of restlessness and excitement; if this occurs, do not administer additional doses. Take particular precaution in administering the drug to children with acute illnesses or dehydration (see under PRECAUTIONS and Dystonia).
Severe Nausea and Vomiting in Children: Prochlorperazine should not be used in pediatric patients under 20 pounds in weight or 2 years of age. It should not be used in conditions for which children's dosages have not been established. Dosage and frequency of administration should be adjusted according to the severity of the symptoms and the response of the patient. The duration of activity following intramuscular administration may last up to 12 hours. Subsequent doses may be given by the same route if necessary.
I.M. Dosage: Calculate each dose on the basis of 0.06 mg of the drug per lb of body weight; give by deep I.M. injection. Control is usually obtained with one dose.Children with Schizophrenia:
I.M. Dosage: For ages under 12, calculate each dose on the basis of 0.06 mg of prochlorperazine per lb of body weight; give by deep I.M. injection. Control is usually obtained with one dose. After control is achieved, switch the patient to an oral form of the drug at the same dosage level or higher.Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
-
HOW SUPPLIED
Prochlorperazine Edisylate Injection USP is supplied as follows:
10 mL (5 mg/mL), individually boxed: NDC 54868-0261
Store prochlorperazine vials at 20° to 25°C (68° to 77°F). See USP controlled room temperature. Do not freeze. Protect from light.
Manufactured for: Manufactured by:
Bedford Laboratories™
Ben Venue Laboratories, Inc. Bedford, OH 44146
Bedford, OH 44146
December 2010
PCLP-P05
Additional barcode labeling by:
Physicians Total Care, Inc.
Tulsa, OK 74146
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PROCHLORPERAZINE EDISYLATE
prochlorperazine edisylate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:54868-0261(NDC:55390-077) Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PROCHLORPERAZINE EDISYLATE (UNII: PG20W5VQZS) (PROCHLORPERAZINE - UNII:YHP6YLT61T) PROCHLORPERAZINE EDISYLATE 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) 7.5 mg in 1 mL SODIUM PHOSPHATE, MONOBASIC ANHYDROUS (UNII: KH7I04HPUU) 5 mg in 1 mL SODIUM TARTRATE (UNII: QTO9JB4MDD) 12 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:54868-0261-0 1 in 1 BOX, UNIT-DOSE 1 10 mL in 1 VIAL Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040540 07/26/2004 Labeler - Physicians Total Care, Inc. (194123980) Establishment Name Address ID/FEI Business Operations Physicians Total Care, Inc. 194123980 relabel, repack