Label: LODOCO- colchicine tablets 0.5 mg tablet
- NDC Code(s): 82867-001-01, 82867-001-02
- Packager: AGEPHA Pharma USA, LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated August 24, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- 1. INDICATIONS AND USAGE
- 2. DOSAGE AND ADMINISTRATION
- 3. DOSAGE FORMS AND STRENGTHS
-
4. CONTRAINDICATIONS
Concurrent use of strong CYP3A4 inhibitors or P-glycoprotein inhibitors with LODOCO is contraindicated, because life-threatening and fatal colchicine toxicity has been reported in these patients with colchicine taken in therapeutic doses [see Drug interactions (7)].
LODOCO use is contraindicated in patients with renal failure (Creatinine clearance less than 15 mL/minute) and severe hepatic impairment.
LODOCO is contraindicated in patients with pre-existing blood dyscrasias and in patients hypersensitive to this drug or any inactive ingredient of LODOCO [see Description (11)].
-
5. WARNINGS AND PRECAUTIONS
5.1 Blood Dyscrasias
LODOCO can cause myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, and aplastic anemia, which can be life-threatening or fatal [see Adverse Reactions (6)]. Gastrointestinal symptoms often are the first sign of colchicine toxicity, so new symptoms should prompt an evaluation for toxicity. Concomitant use of drugs that reduce the metabolism of colchicine or the presence of hepatic or renal impairment increases the risk of developing blood dyscrasias.
Use of LODOCO in patients with pre-existing blood dyscrasias, renal failure (Creatinine clearance less than 15 mL/minute), or severe hepatic dysfunction, and concomitant use of strong CYP3A4 inhibitors or P-glycoprotein inhibitors is contraindicated. [see Contraindications (4)].
Concomitant use of moderate CYP3A4 inhibitors with LODOCO should be avoided in patients with risk factors for increased systemic exposure of colchicine. Monitor patients with any degree of renal impairment and hepatic impairment for colchicine toxicity [see Use in Specific Populations (8.6, 8.7)].
5.2 Neuromuscular Toxicity
LODOCO can cause neuromuscular toxicity and rhabdomyolysis. Concomitant use of drugs that reduce the metabolism of colchicine or the presence of hepatic or renal impairment increases the risk of developing neuromuscular toxicity. Gastrointestinal symptoms often are the first sign of colchicine toxicity, so new symptoms should prompt evaluation for toxicity. Use of LODOCO in patients with renal failure (Creatinine clearance less than 15 mL/minute), or severe hepatic dysfunction, and concomitant use of strong CYP3A4 inhibitors or P-glycoprotein inhibitors is contraindicated [see Contraindications (4)]. Concomitant use of moderate CYP3A4 inhibitors with LODOCO should be avoided in patients with risk factors for increased systemic exposure of colchicine [see Use in Specific Populations (8.6, 8.7) and Drug Interactions (7)].
If a patient develops signs of neuromuscular toxicity, discontinue LODOCO, investigate other causes, and treat appropriately. Concomitant use of LODOCO and HMG CoA reductase inhibitors, gemfibrozil, and fenofibric acid or cyclosporine may potentiate the development of myopathy [see Drug interactions (7)].
Monitor patients with any degree of renal and hepatic impairment for adverse effects of LODOCO.
-
6. ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying and controlled conditions, adverse reaction rates observed in clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not predict the rates observed in a broader patient population in clinical practice.
In the LoDoCo2 trial, myalgia was reported for 21.2% of individuals randomized to colchicine and 18.5% of individuals randomized to matching placebo (hazard ratio 1.15, 95% CI 1.01-1.31).
6.2 Postmarketing Experience
The following adverse reactions have been identified with colchicine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency reliably or establish a causal relationship to drug exposure.
These most often occur with excessive accumulation or overdosage [see Overdosage (10)].
Neuromuscular: myotoxicity, weakness, numbness, paresthesia, rhabdomyolysis.
Gastrointestinal: diarrhea, vomiting, abdominal cramping, abdominal pain.Renal: acute renal impairment
Dermatology: rashes and alopecia
Hematological: thrombocytopenia, leukopenia, pancytopenia -
7. DRUG INTERACTIONS
Colchicine is a substrate for the efflux transporter P-glycoprotein (P-gp). CYP3A4 is the primary enzyme involved in the metabolism of colchicine. If LODOCO is administered with drugs that inhibit P-gp, most of which also inhibit CYP3A4, increased concentrations of colchicine are likely (Table 1).
Table 1: Drug Interactions
Drug class Outcome/effect Clinical comment Strong CYP3A4 Inhibitors†
atazanavir
clarithromycin
darunavir/ritonavir
indinavir
itraconazole
ketoconazole
lopinavir/ritonavir
nefazodone
nelfinavir
ritonavir
saquinavir
telithromycin
tipranavir/ritonavirSignificant increases in colchicine plasma levels [see Clinical Pharmacology (12.3)]. Concomitant use of LODOCO with strong CYP3A4 inhibitors is contraindicated [see Contraindications (4)]. Moderate CYP3A4
Inhibitorsamprenavir
aprepitant
diltiazem
erythromycin
fluconazole,
fosamprenavir (prodrug of
amprenavir)
verapamilSignificant increase in colchicine plasma concentration is anticipated. Monitor patients receiving moderate CYP3A4 inhibitors for
signs of colchicine toxicity. Avoid use in patients with existing renal or hepatic impairment [see Warnings and Precautions (5)].Grapefruit
grapefruit juice
Grapefruit juice increases exposure to colchicine. Advise patients to avoid grapefruit or grapefruit juice when taking LODOCO. P- glycoprotein Inhibitors†
cyclosporine
ranolazineSignificant increase in colchicine plasma levels is anticipated with P-gp inhibitors. Concomitant use of LODOCO with strong P-gp inhibitors is
contraindicated [see Contraindications (4)].HMG-Co A Reductase
InhibitorsPharmacokinetic and/or pharmacodynamic interaction: the addition of one drug to a stable long term regimen of the other has resulted in myopathy and rhabdomyolysis (including fatality). Monitor patients for signs or symptoms of muscle pain toxicity. Other Lipid Lowering drugs
fibrates
gemfibrozilDigitalis Glycosides
digoxin
P-gp substrate; rhabdomyolysis has been reported. Oral contraceptives
Ethinyl estradiol and
norethindrone (Ortho-Novum
1/35)In healthy female volunteers given coadministered with 0.6 mg colchicine twice daily, hormone concentrations are not affected [see Clinical Pharmacology (12.3)]. Colchicine can interact with oral contraceptives like norethindrone/ethinyl estradiol and can cause adverse events like diarrhea, nausea, upper abdominal pain, cold sweat etc. Females using oral contraceptives
should be prescribed LODOCO with caution and observed for adverse events.† Patients with renal or hepatic impairment should not be given LODOCO in conjunction with strong CYP3A4 or P-gp inhibitors [see Contraindications (4)].
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk summary
Available human data from published literature on colchicine use in pregnancy over several decades have not identified any drug associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). Colchicine crosses the human placenta. Although animal reproduction and developmental studies were not conducted with LODOCO (colchicine), published animal reproduction and development studies indicate that colchicine causes embryofetal toxicity and altered postnatal development at exposures within or above the clinical therapeutic range.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human DataAvailable data from published observational studies, case series, and case reports over several decades do not suggest an increased risk for major birth defects or miscarriage in pregnant women with rheumatic diseases (such as rheumatoid arthritis, Behcet’s disease, or Familial Mediterranean fever (FMF)) treated with colchicine at therapeutic doses during pregnancy.
Limitations of these data include the lack of randomization and inability to control for confounders such as underlying maternal disease and maternal use of concomitant medications.
8.2 Lactation
Risk summary
Colchicine is present in human milk (see Data). Adverse events in breastfed infants have not been reported in the published literature after administration of colchicine to lactating women. There are no data on the effects of colchicine on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for LODOCO and any potential adverse effects on the breastfed infant from LODOCO or from the underlying maternal condition.
Data
Limited published data from case reports and a small lactation study demonstrate colchicine is present in breastmilk. A systematic review of literature reported no adverse effects in 149 breastfed children and advised to reconsider breastfeeding if the infant has diarrhea. In a prospective observational cohort study, no gastrointestinal or other symptoms were reported in 38 colchicineexposed
breastfed infants.8.3 Females and Males of Reproductive Potential
Infertility
Case reports and epidemiology studies in human male subjects on colchicine therapy indicated that infertility from colchicine is rare and may be reversible.8.4 Pediatric Use
Safety and effectiveness have not been established in pediatric patients.8.5 Geriatric Use
The total number of subjects included in the LoDoCo2 study who were 65 and over and 75 and over were 3098 (56.1%). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some
older individuals cannot be ruled out.This drug is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, it may be useful to monitor renal function.
8.6 Renal Impairment
Colchicine is known to be excreted renally. In renally impaired patients, the total clearance of colchicine is significantly reduced. In patients, with renal impairment, elevated plasma concentrations of colchicine were observed, and may lead to the development of colchicine toxicity and adverse reactions like myeloneuropathy characterized by proximal weakness and elevated serum creatinine, and possibly rhabdomyolysis [see Warnings and Precautions (5)].
LODOCO is contraindicated in patients with renal failure (Creatinine clearance less than 15 mL/minute). Patients with renal impairment should be monitored closely for adverse effects of colchicine [see Contraindications (4)].
Avoid use in patients with moderate renal impairment receiving moderate CYP3A4 inhibitors [see Contraindications (4), Warnings and Precautions (5) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Colchicine is primarily metabolized in liver. The clearance of colchicine may be significantly reduced, and plasma half-life prolonged in patients with chronic hepatic impairment, compared to healthy subjects [see Clinical Pharmacology (12.3)]. In patients with hepatic impairment, monitor closely for adverse reactions with LODOCO. LODOCO use in severe hepatic impairment is contraindicated. Avoid use in patients with any degree of hepatic impairment and receiving strong P-gp inhibitors or strong or moderate CYP3A4 inhibitors [see Contraindications (4) and Clinical Pharmacology (12.3)]. -
10. OVERDOSAGE
Acute overdose exceeding 0.5 mg/kg (35 mg for a 70 kg average adult) is usually fatal. Fatalities have been reported with as little as 7 mg.
Symptoms: Colchicine poisoning presents in three sequential and usually overlapping phases. The first stage of acute colchicine toxicity typically occurs within 24 hours of ingestion and includes gastrointestinal symptoms such as abdominal pain, nausea, vomiting, and diarrhea, and significant fluid loss, leading to volume depletion. Peripheral leukocytosis may also be seen. The second stage develops 24 to 72 hours after ingestion and is characterized by multi-organ failure. Death is usually a result of respiratory depression and cardiovascular collapse. Recovery may be accompanied by rebound leukocytosis about one week after the initial ingestion.
Treatment: No specific antidote is known. Elimination of toxins by gastric lavage followed by activated charcoal should be attempted within 1-2 hours of ingestion. Colchicine is not effectively removed by hemodialysis.
-
11. DESCRIPTION
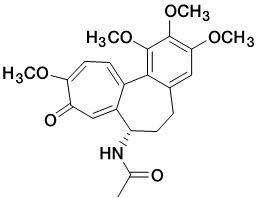
LODOCO contains colchicine, which is an alkaloid chemically described as (S)-N-(5,6,7,9- tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo[a]heptalen-7-yl)acetamide with a molecular formula of C 22H 25NO 6 and a molecular weight of 399.4 g/mol. The structural formula of colchicine is given below.
Colchicine occurs as white to pale yellow powder, very soluble in water.
LODOCO (colchicine) tablets are supplied for oral administration as white to slightly yellow, round, biconvex tablets debossed with ‘L1’ on one side and plain on the other side containing 0.5 mg of colchicine USP as the active ingredient and the following inactive ingredients: gelatin, lactose monohydrate, magnesium stearate, potato starch, and talc.
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of colchicine in the prevention of major cardiovascular events is not understood. However, it is known that colchicine disrupts cytoskeletal functions through inhibition of β-tubulin polymerization into microtubules and consequently prevents the activation, degranulation, and migration of neutrophils. Colchicine may also interfere with the intracellular assembly of the inflammasome complex in neutrophils and monocytes that mediates activation of interleukin-1β. These anti-inflammatory effects are consistent with clinical data demonstrating that colchicine reduces high sensitivity C- reactive protein (hs-CRP).
12.2 Pharmacodynamics
The pharmacodynamics of colchicine in the intended indication is not completely understood.12.3 Pharmacokinetics
In healthy adults, colchicine exhibits linear pharmacokinetics within a dose range of 0.5 to 1.5 mg.
Mean pharmacokinetic parameter values of LODOCO in healthy adults are shown in table 2.Table 2: Summary of LODOCO Pharmacokinetic Parameters in Healthy Adults under Fasting and Fed Conditions
BE studies
C max
ng/ml
T max*
hours
t ½
hours
AUC 0-t
ng·h/ml
Single dose of 0.5 mg
(fasting)
2.1± 1.0
1.0
(Range 0.5-2.3)
31.9
18.6± 7.0
Single dose of 0.5 mg (fed)
1.8± 0.4
1.7
(Range 0.7- 3.5)
31.0
16.4 ± 4.4
*Median and range are presented
Absorption
Oral colchicine intake undergoes an entero-hepatic recirculation. In healthy adults, LODOCO is absorbed when given orally, reaching a mean Cmax 2.1 ng/ml in approximately 1 hour after a single dose administered under fasting conditions.
The mean absolute bioavailability of colchicine is reported to be approximately 45%.Effect of food
When LODOCO was administered with or following a high-fat, high-calorie meal in a bioavailability study, the results showed a lack of a significant food effect, see Table 2, above.
LODOCO may be administered with or without food.
The mean peak plasma concentration of LODOCO under fed conditions was found to be 1.8 ng/ml in approximately 1.75 hour.Distribution
The mean apparent volume of distribution in healthy volunteers is approximately 1300 L.
Colchicine binding to serum protein is 39 ± 5%, primarily to albumin regardless of concentration. After reabsorption, is rapidly removed from the plasma and distributed to various tissues.
Colchicine is found in high concentrations in leucocytes, kidneys, the liver, and spleen.
Colchicine crosses the placenta. Colchicine also distributes into breast milk. Colchicine can also cross the blood-brain barrier and accumulate within the brain, which contains large amount of tubulin [see Use in Specific Populations (8.1, 8.2)].Elimination
Metabolism
Colchicine is demethylated to two primary metabolites, 2-O-demethylcolchicine and 3-O-demethylcolchicine (2- and 3-DMC, respectively) and one minor metabolite, 10-O-demethylcolchicine (also known as colchiceine). In vitro studies using human liver microsomes have shown that CYP3A4 is involved in the metabolism of colchicine to 2- and 3-DMC. Plasma levels of these metabolites are (less than 5% of parent drug).Excretion
In healthy volunteers (n=12), 40 to 65% of 1 mg orally administered colchicine was recovered unchanged in urine. Enterohepatic recirculation and biliary excretion are also postulated to play a role in colchicine elimination. Following single oral dose of 0.5 mg daily, the mean effective half-life in healthy volunteers is 19 hours. Colchicine is a substrate of P-gp.Colchicine is not removed by hemodialysis.
Specific Populations
Geriatric Patients
The pharmacokinetic studies of LODOCO were not conducted in elderly patients. In a study, conducted to compare the relative bioavailability in between 18 elderly subjects and 20 young subjects, the following pharmacokinetic parameter values (mean ± SD) were observed for colchicine in the young and elderly subjects, respectively: AUC (ng/.hr/mL) 22.4 ± 7.0 and 25.0 ± 6.9; Cmax (ng/mL) 2.6 ± 0.7 and 2.6 ± 1.0; Tmax (h) 1.4 ± 0.4 and 1.3 ± 0.4; apparent elimination half-life (h) 24.9 ± 5.3 and 30.1 ± 10.8. No statistical difference in the pharmacokinetic parameters were found between the groups and it was concluded that no dosing adjustments were required in elderly patients.Another study illustrated that after IV administration of 0.5 mg colchicine to six healthy male adults and 1mg colchicine to four elderly group the absorption is similar in healthy volunteers and elderly subjects. However, a 31 percent decrease in volume of distribution at steady state (2.9 vs 4.2 L/kg) and 48 percent decrease in total body clearance (5.5 vs 10.5 L/h) was seen in elderly
patients when compared to healthy volunteers.Pediatric Patients
The sponsor did not conduct any pharmacokinetic studies in pediatric patients. No literature was found in the database on pharmacokinetics of colchicine in pediatric patients with the intended indication.
Patients with Renal Impairment
The exposure of colchicine was similar for normal renal function and mild impairment (24.7–27.2 ng.h/mL) but doubled in subjects with moderate or severe renal impairment (48.9 and 48.0 ng.h/mL, respectively). The same study showed an unexpected result that subjects with ESRD, prior to and during hemodialysis, only have a modest increase in exposure to colchicine (30.6 – 31.7 ng.h/mL) compared to healthy control. The reason for this is not clear. A small amount of the colchicine dose (mean of 5.2 %) was recovered in dialysate [see Use in Specific Population (8.6)].
In another study, subjects with end-stage renal disease requiring dialysis had 75% lower colchicine clearance (0.17 vs 0.73 L/hr/kg) and prolonged plasma elimination half-life (18.8 vs 4.4 hours) as compared to subjects with normal renal function.Patients with Hepatic Impairment
From the published literature, in some subjects with mild to moderate cirrhosis, healthy subjects had a mean clearance of 10.7 ml/min.kg, whereas cirrhotic patients had a mean clearance of 4.2 ml/min.kg. The mean half-life was about 57 minutes in control subjects vs. about 114 minutes in cirrhotic patients. Volume of distribution was not different in the two groups (0.7 ± 0.1 L/kg in control subjects; 0.7 ± 0.2 L/kg in cirrhotic patients). The study concluded that cirrhosis impairs colchicine clearance. No pharmacokinetic data are available for patients with severe hepatic impairment [see Use in Specific Population (8.7)].Drug Interaction Studies
In vitro drug interactions:
In vitro studies in human liver microsomes have shown that colchicine is not an inhibitor or inducer of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A4 activity.In vivo drug interactions:
The effects of co-administration of other drugs with LODOCO on Cmax, AUC, and Cmin are summarized in Table 3 (effect of other drugs on colchicine). For information regarding clinical recommendations, see Table 1 [see Drug interactions (7)].
Table 3: Effect of other drugs on colchicine pharmacokinetics
Co-administered drug
Dose of Co-administered drug
Dose of Colchicine
Mean pharmacokinetic parameters (%CV) substrate drug
% Change in Colchicine
Concentrations from Baseline
(Range: Min - Max)
C max (ng/ml)
AUC 0-t
(ng/
hour/
ml)
T 1/2 (hours)
Cl/F
(L/
hour)
C max
AUC 0-t
Cyclosporine
100 mg OD
0.6 mg, single dose
2.7
12.6
6.8
48.2
270
(62 to 606.9)
259
(75.8 to 511.9)
Clarithromycin
250 mg BID
0.6 mg, single dose
2.8
12.4
8.9
46.8
227.2 (65.7 to 591.1)
281.5 (88.7 to 851.6)
Ketoconazole
200 mg BID
0.6 mg, single dose
2.8
12.0
6.3
49.3
101.7 (19.6 to 219)
212.2
(76.7 to 419.6)
Ritonavir
100 mg BID
0.6 mg, single dose
1.9
8.4
5.2
67.9
184.4
(79.2 to 447.4)
296
(53.8 to 924.4)
Verapamil
240 mg OD
0.6 mg, single dose
3.0
13.1
4.3
43.9
40.1
(-47.1 to 149.5)
103.3
(-9.8 to 217.2)
Diltiazem
240 mg OD
0.6 mg, single dose
2.2
10.0
5.5
58.9
44.2
(-46 to 318.3)
93.4
(-30.2 to 338.6)
Azithromycin
500 mg OD
0.6 mg, single dose
2.7
12.0
6.1
50.2
21.6
(-41.7 to 222)
57.1 (-24.3 to 241.1)
Atorvastatin
40 mg OD
0.6 mg, single dose
2.5
10.7
4.3
58.6
130.60
(111.1-153.5)
127.3
(109.1–148.7)
Grapefruit juice
240 mL twice daily, 4 days
0.6 mg, single dose
-
-
-
-
-2.6
(-53.4 to 55.0)
-2.4
(-4.6 to 62.2)
Estrogen-containing oral contraceptives: In healthy female volunteers given ethinyl estradiol and norethindrone (Ortho-Novum 1/35) co-administered with colchicine 0.6 mg b.i.d. × 14 days, hormone concentrations are not affected.
-
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year studies were conducted in mice and rats to assess the carcinogenic potential of colchicine. No evidence of colchicine-related tumorigenicity was observed in mice or rats at colchicine oral doses up to 3 and 2 mg/kg/day, respectively, approximately 29 and 38 times, the recommended human dose of 0.5 mg on a mg/m 2 basis.
Mutagenesis
Colchicine was negative for mutagenicity in the bacterial reverse mutation assay. In a chromosomal aberration assay in cultured human white blood cells, colchicine treatment resulted in the formation of micronuclei. Since published studies demonstrated that colchicine induces aneuploidy from the process of mitotic nondisjunction without structural DNA changes, colchicine is not considered clastogenic, although micronuclei are formed.
Impairment of Fertility
No studies of colchicine effects on fertility were conducted with LODOCO. However, published nonclinical studies demonstrated that colchicine-induced disruption of microtubule formation affects meiosis and mitosis. Reproductive studies also reported abnormal sperm morphology and reduced sperm counts in males, and interference with sperm penetration, second meiotic division
and normal cleavage in females when exposed to colchicine. Colchicine administered to pregnant animals resulted in fetal death and teratogenicity. These effects were dose-dependent, with the timing of exposure critical for the effects on embryofetal development. The nonclinical doses evaluated were generally higher than an equivalent human therapeutic dose, but safety margins for reproductive and developmental toxicity could not be determined. -
14. CLINICAL STUDIES
The evidence for the efficacy of colchicine in patients with cardiovascular events is derived from published literature (LoDoCo2) along with other supportive studies.
The LoDoCo2 trial was an investigator-initiated, randomized, placebo controlled, double-blind, event-driven trial conducted to assess the efficacy of colchicine 0.5mg once daily orally in patients with stable coronary artery disease. The study included 5522 patients, in which 2762 were assigned to the colchicine group and 2760 to placebo. The baseline characteristics of the patients were balanced between the trial groups. Patients were treated for chronic coronary disease, with 99.7% taking an antiplatelet agent or an anticoagulant, 96.6% a lipid-lowering agent, 97.3% of which were statins, 62.1% a beta-blocker, and 71.7% an inhibitor of the renin–angiotensin system.
LoDoCo2 assessed the efficacy of colchicine 0.5 mg once daily in patients with stable coronary artery disease. Patients between 35-85 years were eligible for participation in the LoDoCo2 trial if they had proven coronary artery disease, were clinically stable for at least 6 months, without comorbidities that would preclude follow-up, or contraindication to colchicine use. The mean (±SD) age of the patients was 66±8.6 years, and 846 (15.3%) were female. The median time on study medication was 28.6 months. The primary end point of LoDoCo2 trial was a composite of cardiovascular death, spontaneous (nonprocedural) myocardial infarction, ischemic stroke, or ischemia-driven coronary revascularization.In the LoDoCo2 trial, 0.5 mg of colchicine once daily resulted in a 31% lower relative risk (RRR) of the primary composite endpoint events compared to placebo (HR, 0.69; 95% [CI] 0.57 to 0.83; p<0.001) and the number needed to treat (NNT) was 36.
Figure 1: Cumulative Incidence of Primary End point in LoDoCo2 trial
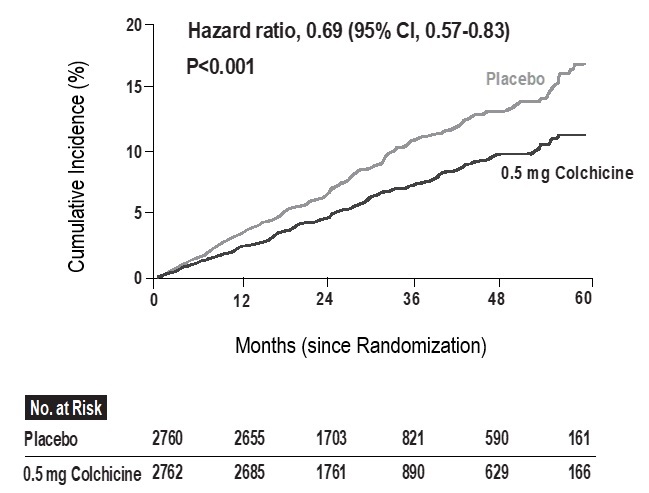
The results of the primary endpoint are summarized in Table 4.
Table 4: Summary of efficacy results of LoDoCo2 trial
LoDoCo2 Trial End Point
Colchicine
(N=2762)
No. of
patients (%)Placebo
(N=2760)
No. of
patients (%)Hazard
ratio
(95% Cl)P value Primary end point
Cardiovascular death, myocardial infarction, ischemic stroke, or ischemia driven
coronary revascularization187 (6.8) 264 (9.6) 0.69
(0.57–0.83)<0.001 Ischemia-driven coronary revascularization 135 (4.9) 177 (6.4) 0.75
(0.60–0.94)Myocardial infarction 83 (3.0) 116 (4.2) 0.70
(0.53–0.93)Ischemic stroke 16 (0.6) 24 (0.9) 0.66
(0.35–1.25)Cardiovascular death 20 (0.7) 25 (0.9) 0.80
(0.44–1.44)Myocardial infarction refers to spontaneous (non-procedural) myocardial infarction.
-
16. HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
LODOCO (colchicine) tablets 0.5 mg are white to slightly yellow, round, and biconvex and debossed with ‘L1’ on one side and plain on the other side and they are available as a single Aluminum/PVC blister pack of 30 tablets, which is secondary packaged in a carton: NDC 82867-001-01.16.2 Storage
Store LODOCO at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F), [See USP Controlled Room Temperature].
Store LODOCO tablets in the original package in order to protect from light.
-
17. PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Dosing Instructions
Advise patients to take LODOCO as prescribed, and patients should not alter or discontinue the medication without consulting their healthcare provider.
Advise patients that if the dose of LODOCO is missed, they should take the missed dose as soon as possible and return to the normal dosing schedule.
If a dose is skipped advise patient not to double the next dose.
Drug and food interactions
Patients should be advised that many drugs or other substances may interact with LODOCO and some interactions could be fatal. Therefore, patients should report to their healthcare provider all of the current medications they are taking and check with their healthcare provider before starting any new medications, particularly antibiotics. Patients should also be advised to report the use of nonprescription medication or herbal products. Advise patients that grapefruit and grapefruit juice may also interact and should not be consumed during LODOCO treatment.
Colchicine Toxicity
Advise patients that gastrointestinal symptoms are often the first sign of colchicine toxicity. Patients should be instructed to contact their healthcare provider if new symptoms develop.
Neuromuscular Toxicity
Inform patients that muscle pain or weakness, tingling or numbness in fingers or toes may occur with LODOCO alone or when it is used with certain other drugs. Concomitant use of LODOCO and HMG CoA reductase inhibitors, gemfibrozil, and fenofibric acid or cyclosporine may potentiate the development of myopathy (muscles weakness, fatigue). Patients developing any of these signs or symptoms must discontinue LODOCO and seek medical evaluation immediately.
Concomitant use of interacting drugs, including statins, or renal or hepatic insufficiency increases the risk of developing toxicity.Infertility
Advise males of reproductive potential that LODOCO may rarely and transiently impair fertility [see Use in Specific Populations (8.3)].
------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Distributed by:
AGEPHA Pharma USA, LLC
181 New Road, Suite 304
Parsippany, NJ 07054 -
PATIENT INFORMATION
PATIENT INFORMATION
LODOCO (Low-Doe-Co)
(colchicine)
tablets, for oral useWhat is LODOCO?
LODOCO is a prescription medicine used to reduce the risk of heart attack, stroke, certain types of heart procedures, and cardiovascular death in adults with:
known buildup of plaque inside the arteries (atherosclerotic disease), or
with multiple risk factors for cardiovascular disease.Do not take LODOCO if you:
take certain medicines called strong CYP3A4 inhibitors or P-glycoprotein inhibitors. Ask your healthcare provider if you are not sure. Taking certain medicines with LODOCO may cause your level of LODOCO to be too high in your body and cause life-threatening side effects or death.
have severe kidney or liver problems.
have blood problems.
are allergic to colchicine or any of the ingredients in LODOCO. See the end of this leaflet for a complete list of ingredients in LODOCO.Before taking LODOCO, tell your healthcare provider about all your medical conditions, including if you:
have liver or kidney problems.
are pregnant or plan to become pregnant. It is not known if LODOCO will harm your unborn baby.are breastfeeding or plan to breastfeed. LODOCO can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with LODOCO.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take:
certain medicines called moderate CYP3A4 inhibitors
cholesterol lowering medicines
cyclosporineantibiotics
Ask your healthcare provider or pharmacist if you are not sure if you take any of the medicines listed above. This is not a complete list of all the medicines that can interact with LODOCO.
Taking LODOCO with certain other medicines can affect each other and cause serious side effects or death.
Do not start a new medicine without talking to your healthcare provider. Your healthcare provider can tell you if it is safe to take LODOCO with other medicines.Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take LODOCO?
Take LODOCO exactly as your healthcare provider tells you to take it.
If you take too much LODOCO, go to the nearest hospital emergency room right away.
Do not change your dose or stop taking LODOCO without talking to your healthcare provider first.
Take LODOCO by mouth 1 time each day.
If you miss a dose of LODOCO, take it as soon you remember and then take your next dose at your regular time. Do not take 2 doses of LODOCO at the same time to make up for a missed dose.What should I avoid while taking LODOCO?
Avoid eating grapefruit or drinking grapefruit juice while taking LODOCO. Grapefruit and grapefruit juice may increase your chance of side effects while taking LODOCO.What are the possible side effects of LODOCO?
LODOCO may cause serious side effects, including:
Blood problems. LODOCO can cause low red blood cell counts, low white blood cell counts, and low platelet counts, which can be life-threatening or may lead to death.
Muscle weakness (neuromuscular toxicity). LODOCO can cause muscle weakness and muscle problems. Stop taking LODOCO and get medical help right away if you get muscle pain or weakness, or tingling or numbness in your fingers or toes.The most common side effects of LODOCO include:
diarrhea, vomiting, and stomach-area (abdominal) cramping. Tell your healthcare provider right away if you develop any of these symptoms, they are often the first sign of having too much LODOCO in your body.
muscle painLODOCO may cause temporary fertility problems in males. This may affect your ability to father a child. Talk to your healthcare provider if this is a concern for you.
Tell your healthcare provider if you have any side effect that is new, that bothers you or that does not go away. These are not all of the possible side effects of LODOCO.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
You may also report side effects to AGEPHA Pharma FZ LLC at 1-800-963-0353.
How should I store LODOCO?
Store LODOCO at room temperature between 68°F to 77°F (20°C to 25°C).
Keep LODOCO and all medicines out of the reach of children.
Store LODOCO in the original package in order to protect from light.General information about the safe and effective use of LODOCO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use LODOCO for a condition for which it was not prescribed. Do not give LODOCO to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about LODOCO that is written for health professionals.What are the ingredients in LODOCO?
Active Ingredient: colchicine.
Inactive Ingredients: gelatin, lactose monohydrate, magnesium stearate, potato starch, and talc.
Distributed by: AGEPHA Pharma USA, LLC, 181 New Road, Suite 304, Parsippany, NJ 07054 For more information, go to www.LODOCO.com or call 1-800-963-0353.This Patient Information has been approved by the U.S. Food and Drug Administration. Issued: 06/2023
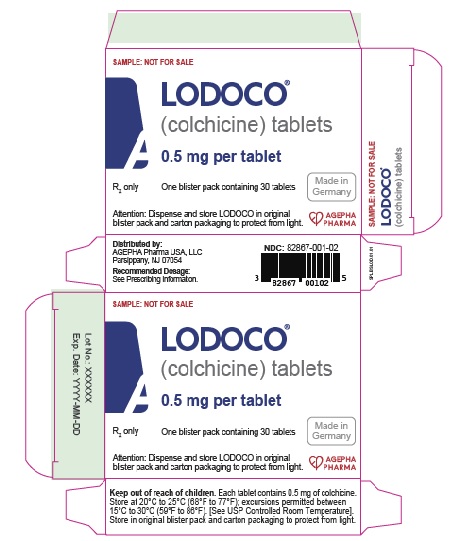
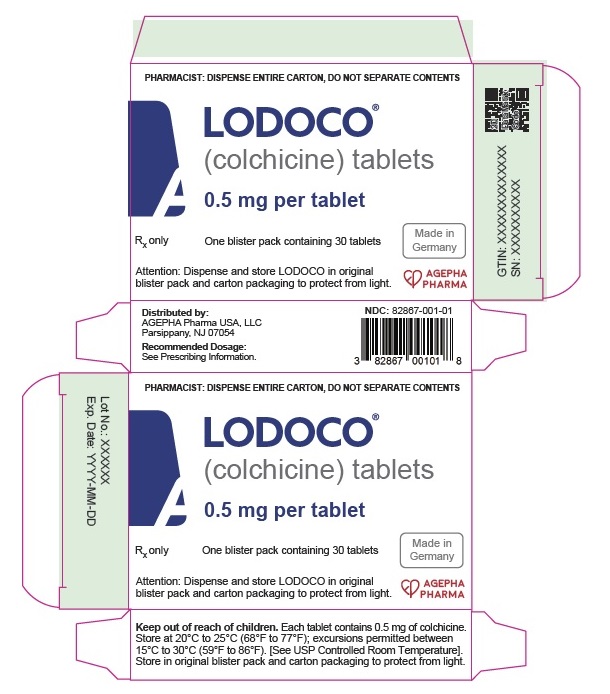
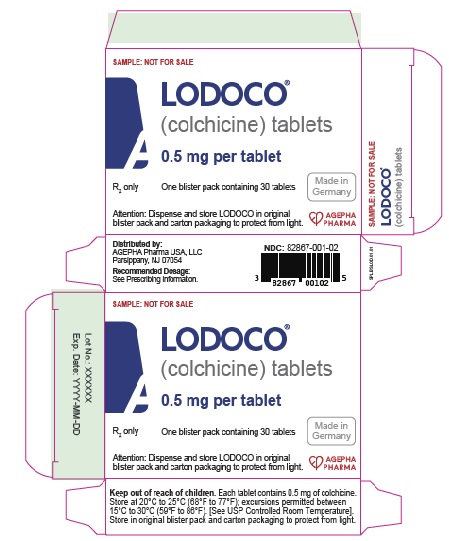
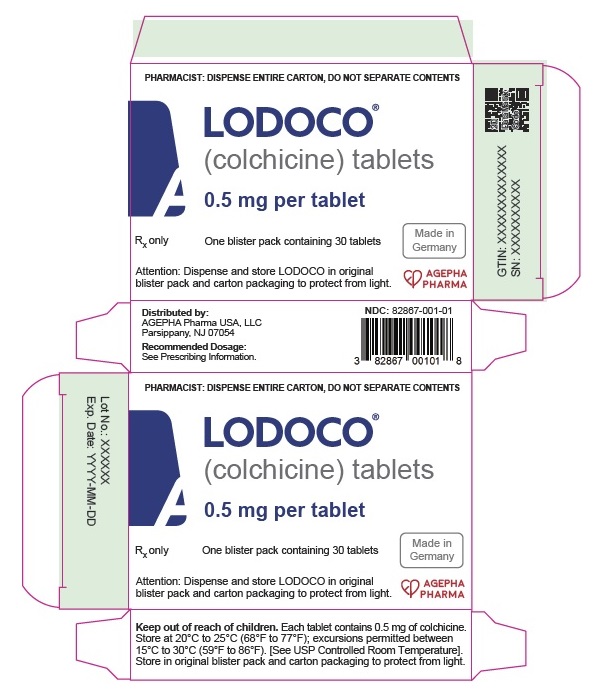
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
LODOCO
colchicine tablets 0.5 mg tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:82867-001 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength COLCHICINE (UNII: SML2Y3J35T) (COLCHICINE - UNII:SML2Y3J35T) COLCHICINE 0.5 mg Product Characteristics Color white (white to slightly yellow) Score score with uneven pieces Shape ROUND (Biconvex) Size 6mm Flavor Imprint Code L1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:82867-001-01 1 in 1 CARTON 06/16/2023 1 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 2 NDC:82867-001-02 1 in 1 CARTON 06/16/2023 2 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 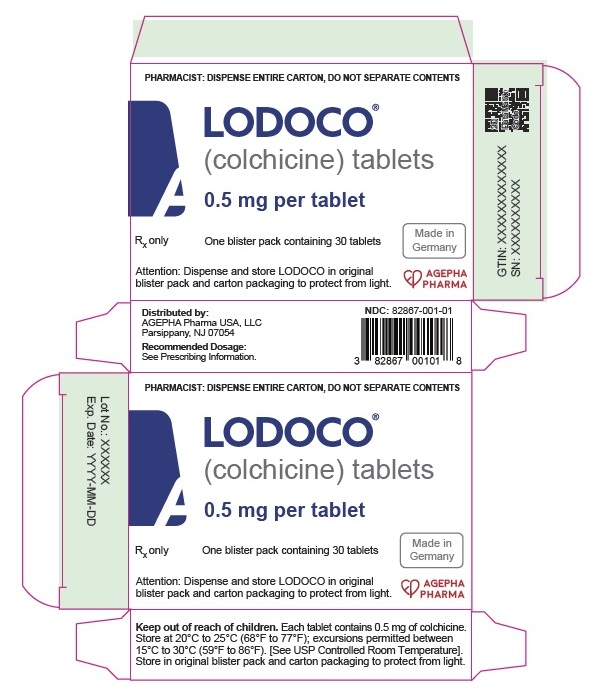
Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215727 06/16/2023 Labeler - AGEPHA Pharma USA, LLC (117633746) Registrant - Agepha Pharma FZ LLC (849784577)