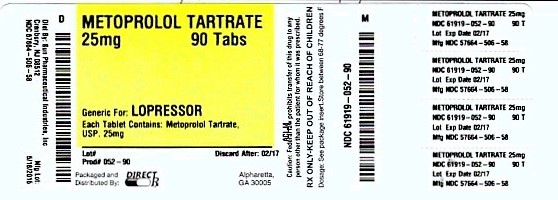
Label: METOPROLOL TARTRATE tablet
-
Contains inactivated NDC Code(s)
NDC Code(s): 61919-052-60, 61919-052-82, 61919-052-90 - Packager: DIRECT RX
- This is a repackaged label.
- Source NDC Code(s): 57664-506
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated July 14, 2016
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
BOXED WARNING
(What is this?)
BOXED WARNING SECTION
Ischemic Heart Disease: Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction have occurred. When discontinuing chronically administered metoprolol, particularly in patients with ischemic heart disease, the dosage should be gradually reduced over a period of 1 to 2 weeks and the patient should be carefully monitored. If angina markedly worsens or acute coronary insufficiency develops, metoprolol administration should be reinstated promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Patients should be warned against interruption or discontinuation of therapy without the physician’s advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue metoprolol therapy abruptly even in patients treated only for hypertension.
-
DESCRIPTION SECTION
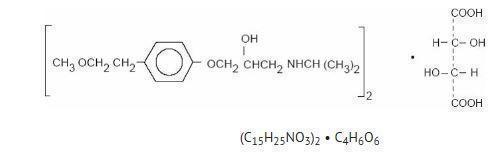
Metoprolol tartrate, USP is a selective beta1-adrenoreceptor blocking agent, available as 25, 50 and 100 mg tablets for oral administration. Metoprolol tartrate is (±)-1-(isopropylamino)-3-[p-(2-methoxyethyl) phenoxy]-2-propanol (2:1) dextro-tartrate salt, and its structural formula is:
Metoprolol tartare, USP is a white, practically odorless, crystalline powder with a molecular weight of 684.82. It is very soluble in water; freely soluble in methylene chloride, in chloroform, and in alcohol; slightly soluble in acetone; and insoluble in ether.
Inactive Ingredients. Tablets contain colloidal silicon dioxide, hydroxypropyl methylcellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate, povidone, sodium starch glycolate, talc and titanium dioxide.
- CLINICAL PHARMACOLOGY SECTION
-
INDICATIONS & USAGE SECTION
Metoprolol tartrate tablets are indicated for the treatment of hypertension. They may be used alone or in combination with other antihypertensive agents.
Angina Pectoris
Metoprolol tartrate tablets are indicated in the long-term treatment of angina pectoris.
Myocardial Infarction
Metoprolol tartrate injection and tablets are indicated in the treatment of hemodynamically stable patients with definite or suspected acute myocardial infarction to reduce cardiovascular mortality. Treatment with intravenous metoprolol tartrate can be initiated as soon as the patient’s clinical condition allows (see DOSAGE AND ADMINISTRATION, CONTRAINDICATIONS, and WARNINGS). Alternatively, treatment can begin within 3 to 10 days of the acute event (see DOSAGE AND ADMINISTRATION).
-
CONTRAINDICATIONS SECTION
Hypertension and Angina
Metoprolol tartrate is contraindicated in sinus bradycardia, heart block greater than first degree, cardiogenic shock, and overt cardiac failure (see WARNINGS).
Hypersensitivity to metoprolol and related derivatives, or to any of the excipients; hypersensitivity to other beta-blockers (cross sensitivity between beta-blockers can occur).
Sick-sinus syndrome.
Severe peripheral arterial circulatory disorders.
Myocardial Infarction
Metoprolol is contraindicated in patients with a heart rate < 45 beats/min; second- and third-degree heart block; significant first-degree heart block (P-R interval ≥ 0.24 sec); systolic blood pressure < 100 mmHg; or moderate-to-severe cardiac failure (see WARNINGS).
-
WARNINGS SECTION
Hypertension and AnginaCardiac Failure:
Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure.
In Patients Without a History of Cardiac Failure
Continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, fully digitalize patients and/or given a diuretic. The response should be observed closely. If cardiac failure continues, despite adequate digitalization and diuretic therapy, metoprolol should be withdrawn.
Ischemic Heart Disease: Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction have occurred. When discontinuing chronically administered metoprolol, particularly in patients with ischemic heart disease, the dosage should be gradually reduced over a period of 1 to 2 weeks and the patient should be carefully monitored. If angina markedly worsens or acute coronary insufficiency develops, metoprolol administration should be reinstated promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Patients should be warned against interruption or discontinuation of therapy without the physician’s advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue metoprolol therapy abruptly even in patients treated only for hypertension.
Bronchospastic Diseases: PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS, including Metoprolol tartrate. Because of its relative beta1 selectivity, however, metoprolol may be used with caution in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Since beta1 selectivity is not absolute, a beta2-stimulating agent should be administered concomitantly, and the lowest possible dose of metoprolol tartrate should be used. In these circumstances it would be prudent initially to administer metoprolol in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval (see DOSAGE AND ADMINISTRATION).
Major Surgery:
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Diabetes and Hypoglycemia:
Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
Pheochromocytoma:
If metoprolol is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
Thyrotoxicosis:
Beta-adrenergic blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm.
Myocardial InfarctionCardiac Failure:
Sympathetic stimulation is a vital component supporting circulatory function, and beta blockade carries the potential hazard of depressing myocardial contractility and precipitating or exacerbating minimal cardiac failure.
During treatment with metoprolol, the hemodynamic status of the patient should be carefully monitored. If heart failure occurs or persists despite appropriate treatment, metoprolol should be discontinued.
Bradycardia:
Metoprolol produces a decrease in sinus heart rate in most patients; this decrease is greatest among patients with high initial heart rates and least among patients with low initial heart rates. Acute myocardial infarction (particularly inferior infarction) may in itself produce significant lowering of the sinus rate. If the sinus rate decreases to < 40 beats/min, particularly if associated with evidence of lowered cardiac output, atropine (0.25 to 0.5 mg) should be administered intravenously. If treatment with atropine is not successful, metoprolol should be discontinued, and cautious administration of isoproterenol or installation of a cardiac pacemaker should be considered.
AV Block:
Metoprolol slows AV conduction and may produce significant first- (P-R interval ≥ 0.26 sec), second-, or third-degree heart block. Acute myocardial infarction also produces heart block.
If heart block occurs, metoprolol should be discontinued and atropine (0.25 to 0.5 mg) should be administered intravenously. If treatment with atropine is not successful, cautious administration of isoproterenol or installation of a cardiac pacemaker should be considered.
Hypotension:
If hypotension (systolic blood pressure ≤ 90 mmHg) occurs, metoprolol should be discontinued, and the hemodynamic status of the patient and the extent of myocardial damage carefully assessed. Invasive monitoring of central venous, pulmonary capillary wedge, and arterial pressures may be required. Appropriate therapy with fluids, positive inotropic agents, balloon counterpulsation, or other treatment modalities should be instituted. If hypotension is associated with sinus bradycardia or AV block, treatment should be directed at reversing these (see above).
-
PRECAUTIONS SECTION
General
Start at a low dose and uptitrate slowly in patients with impaired hepatic function.
Information for Patients
Patients should be advised to take metoprolol regularly and continuously, as directed, with or immediately following meals. If a dose should be missed, the patient should take only the next scheduled dose (without doubling it). Patients should not discontinue metoprolol without consulting the physician.
Patients should be advised (1) to avoid operating automobiles and machinery or engaging in other tasks requiring alertness until the patient’s response to therapy with metoprolol has been determined; (2) to contact the physician if any difficulty in breathing occurs; (3) to inform the physician or dentist before any type of surgery that he or she is taking metoprolol.
Drug Interactions
Catecholamine-depleting drugs: Catecholamine-depleting drugs (e.g., reserpine) may have an additive effect when given with beta-blocking agents or monoamine oxidase (MAO) inhibitors. Observe patients treated with Metoprolol Tartrate plus a catecholamine depletor for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension. In addition, possibly significant hypertension may theoretically occur up to 14 days following discontinuation of the concomitant administration with an irreversible MAO inhibitor.
Digitalis glycosides and beta blockers: Both digitalis glycosides and beta blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia. Monitor heart rate and PR interval.
Calcium channel blockers: Concomitant administration of a beta-adrenergic antagonist with a calcium channel blocker may produce an additive reduction in myocardial contractility because of negative chronotropic and inotropic effects.
Risk of Anaphylactic Reaction: While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
General Anesthetics: Some inhalation anesthetics may enhance the cardiodepressant effect of beta blockers (see WARNINGS, Major Surgery).
CYP2D6 Inhibitors: Potent inhibitors of the CYP2D6 enzyme may increase the plasma concentration of Metoprolol Tartrate which would mimic the pharmacokinetics of CYP2D6 poor metabolizer (see Pharmacokinetics section). Increase in plasma concentrations of metoprolol would decrease the cardioselectivity of metoprolol. Known clinically significant potent inhibitors of CYP2D6 are antidepressants such as fluvoxamine, fluoxetine, paroxetine, sertraline,bupropion, clomipramine, and desipramine; antipsychotics such as chlorpromazine, fluphenazine, haloperidol, and thioridazine; antiarrhythmics such as quinidine or propafenone; antiretrovirals such as ritonavir; antihistamines such as diphenhydramine; antimalarials such as hydroxychloroquine or quinidine; antifungals such as terbinafine.
Hydralazine: Concomitant administration of hydralazine may inhibit presystemic metabolism of metoprolol leading to increased concentrations of metoprolol.
Alpha-adrenergic agents: Antihypertensive effect of alpha-adrenergic blockers such as guanethidine, betanidine, reserpine, alpha-methyldopa or clonidine may be potentiated by beta-blockers including Metoprolol Tartrate. Beta- adrenergic blockers may also potentiate the postural hypotensive effect of the first dose of prazosin, probably by preventing reflex tachycardia. On the contrary, beta adrenergic blockers may also potentiate the hypertensive response to withdrawal of clonidine in patients receiving concomitant clonidine and beta-adrenergic blocker. If a patient is treated with clonidine and Metoprolol Tartrate concurrently, and clonidine treatment is to be discontinued, stop Metoprolol Tartrate several days before clonidine is withdrawn. Rebound hypertension that can follow withdrawal of clonidine may be increased in patients receiving concurrent beta-blocker treatment.
Ergot alkaloid: Concomitant administration with beta-blockers may enhance the vasoconstrictive action of ergot alkaloids
Dipyridamole: In general, administration of a beta-blocker should be withheld before dipyridamole testing, with careful monitoring of heart rate following the dipyridamole injection.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have been conducted to evaluate carcinogenic potential. In a 2-year study in rats at three oral dosage levels of up to 800 mg/kg per day, there was no increase in the development of spontaneously occurring benign or malignant neoplasms of any type. The only histologic changes that appeared to be drug related were an increased incidence of generally mild focal accumulation of foamy macrophages in pulmonary alveoli and a slight increase in biliary hyperplasia. In a 21-month study in Swiss albino mice at three oral dosage levels of up to 750 mg/kg per day, benign lung tumors (small adenomas) occurred more frequently in female mice receiving the highest dose than in untreated control animals. There was no increase in malignant or total (benign plus malignant) lung tumors, or in the overall incidence of tumors or malignant tumors. This 21-month study was repeated in CD-1 mice, and no statistically or biologically significant differences were observed between treated and control mice of either sex for any type of tumor.
All mutagenicity tests performed (a dominant lethal study in mice, chromosome studies in somatic cells, a Salmonella/mammalian-microsome mutagenicity test, and a nucleus anomaly test in somatic interphase nuclei) were negative.
Reproduction toxicity studies in mice, rats and rabbits did not indicate teratogenic potential for metoprolol tartrate. Embryotoxicity and/or fetotoxicity in rats and rabbits were noted starting at doses of 50 mg/kg in rats and 25 mg/kg in rabbits, as demonstrated by increases in preimplantation loss, decreases in the number of viable fetuses per dose, and/or decreases in neonatal survival. High doses were associated with some maternal toxicity, and growth delay of the offspring in utero, which was reflected in minimally lower weights at birth. The oral NOAELs for embryo-fetal development in mice, rats, and rabbits were considered to be 25, 200, and 12.5 mg/kg. This corresponds to dose levels that are approximately 0.3, 4, and 0.5 times, respectively, when based on surface area, the maximum human oral dose (8 mg/kg/day) of metoprolol tartrate. Metoprolol tartrate has been associated with reversible adverse effects on spermatogenesis starting at oral dose levels of 3.5 mg/kg in rats (a dose that is only 0.1-times the human dose, when based on surface area), although other studies have shown no effect of metoprolol tartrate on reproductive performance in male rats.
Pregnancy Category C
Upon confirming the diagnosis of pregnancy, women should immediately inform the doctor.
Metoprolol has been shown to increase postimplantation loss and decrease neonatal survival in rats at doses up to 11 times the maximum daily human dose of 450 mg, when based on surface area. Distribution studies in mice confirm exposure of the fetus when metoprolol is administered to the pregnant animal. These limited animal studies do not indicate direct or indirect harmful effects with respect to teratogenicity (see Carcinogenesis, Mutagenesis, Impairment of Fertility).
There are no adequate and well-controlled studies in pregnant women. The amount of data on the use of metoprolol in pregnant women is limited. The risk to the fetus/mother is unknown. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Metoprolol is excreted in breast milk in a very small quantity. An infant consuming 1 liter of breast milk daily would receive a dose of less than 1 mg of the drug.
Fertility:
The effects of Metoprolol Tartrate on the fertility of human have not been studied
Metoprolol Tartrate showed effects on spermatogenesis in male rats at a therapeutic dose level, but had no effect on rates of conception at higher doses in animal fertility studies (see Carcinogenesis, Mutagenesis, Impairment of Fertility).Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical trials of metoprolol tartrate USP, in hypertension did not include sufficient numbers of elderly patients to determine whether patients over 65 years of age differ from younger subjects in their response to metoprolol tartrate. Other reported clinical experience in elderly hypertensive patients has not identified any difference in response from younger patients.
In worldwide clinical trials of metoprolol tartrate in myocardial infarction, where approximately 478 patients were over 65 years of age (0 over 75 years of age), no age related differences in safety and effectiveness were found. Other reported clinical experience in myocardial infarction has not identified differences in response between the elderly and younger patients. However, greater sensitivity of some elderly individuals taking metoprolol tartrate cannot be categorically ruled out. Therefore, in general, it is recommended that dosing proceed with caution in this population.
-
ADVERSE REACTIONS SECTION
Hypertension and Angina
Most adverse effects have been mild and transient.
Central Nervous System: Tiredness and dizziness have occurred in about 10 of 100 patients. Depression has been reported in about 5 of 100 patients. Mental confusion and short-term memory loss have been reported. Headache, nightmares, and insomnia have also been reported.
Cardiovascular: Shortness of breath and bradycardia have occurred in approximately 3 of 100 patients. Cold extremities; arterial insufficiency, usually of the Raynaud type; palpitations; congestive heart failure; peripheral edema; and hypotension have been reported in about 1 of 100 patients. Gangrene in patients with pre-existing severe peripheral circulatory disorders has also been reported very rarely. (see CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS.)
Respiratory: Wheezing (bronchospasm) and dyspnea have been reported in about 1 of 100 patients (see WARNINGS). Rhinitis has also been reported.
Gastrointestinal: Diarrhea has occurred in about 5 of 100 patients. Nausea, dry mouth, gastric pain, constipation, flatulence, and heartburn have been reported in about 1 of 100 patients. Vomiting was a common occurrence. Post-marketing experience reveals very rare reports of hepatitis, jaundice and non-specific hepatic dysfunction. Isolated cases of transaminase, alkaline phosphatase and lactic dehydrogenase elevations have also been reported.
Hypersensitive Reactions: Pruritus or rash have occurred in about 5 of 100 patients. Very rarely, photosensitivity and worsening of psoriasis has been reported.
Miscellaneous: Peyronie’s disease has been reported in fewer than 1 of 100,000 patients. Musculoskeletal pain, blurred vision, and tinnitus have also been reported.
There have been rare reports of reversible alopecia, agranulocytosis, and dry eyes. Discontinuation of the drug should be considered if any such reaction is not otherwise explicable. There have been very rare reports of weight gain, arthritis, and retroperitoneal fibrosis (relationship to metoprolol has not been definitely established).
The oculomucocutaneous syndrome associated with the beta blocker practolol has not been reported with metoprolol.
Myocardial Infarction
Central Nervous System: Tiredness has been reported in about 1 of 100 patients. Vertigo, sleep disturbances, hallucinations, headache, dizziness, visual disturbances, confusion, and reduced libido have also been reported, but a drug relationship is not clear.
Cardiovascular: In the randomized comparison of metoprolol and placebo described in the CLINICAL PHARMACOLOGY section, the following adverse reactions were reported:
Metoprolol Placebo Hypotension
(systolic BP < 90 mmHg)27.4% 23.2% Bradycardia
(heart rate < 40 beats/min)15.9% 6.7% Second- or
third-degree heart block4.7% 4.7% First-degree
heart block (P-R ≥ 0.26 sec)5.3% 1.9% Heart failure 27.5% 29.6% Respiratory: Dyspnea of pulmonary origin has been reported in fewer than 1 of 100 patients.
Gastrointestinal: Nausea and abdominal pain have been reported in fewer than 1 of 100 patients.
Dermatologic: Rash and worsened psoriasis have been reported, but a drug relationship is not clear.
Miscellaneous: Unstable diabetes and claudication have been reported, but a drug relationship is not clear.
Potential Adverse Reactions
A variety of adverse reactions not listed above have been reported with other beta-adrenergic blocking agents and should be considered potential adverse reactions to metoprolol.
Central Nervous System: Reversible mental depression progressing to catatonia; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics.
Cardiovascular: Intensification of AV block (see CONTRAINDICATIONS).
Hematologic: Agranulocytosis, nonthrombocytopenic purpura, thrombocytopenic purpura.
Hypersensitive Reactions: Fever combined with aching and sore throat, laryngospasm, and respiratory distress.
Postmarketing Experience
The following adverse reactions have been reported during postapproval use of metoprolol tartrate: confusional state, an increase in blood triglycerides and a decrease in High Density Lipoprotein (HDL). Because these reports are from a population of uncertain size and are subject to confounding factors, it is not possible to reliably estimate their frequency.
-
OVERDOSAGE SECTION
Acute Toxicity
Several cases of overdosage have been reported, some leading to death.
Oral LD50’s (mg/kg): mice, 1158 to 2460; rats, 3090 to 4670.
Signs and Symptoms
Potential signs and symptoms associated with overdosage with metoprolol are bradycardia, hypotension, bronchospasm, myocardial infarction, cardiac failure and death. .
Management
There is no specific antidote.
In general, patients with acute or recent myocardial infarction may be more hemodynamically unstable than other patients and should be treated accordingly (see WARNINGS, Myocardial Infarction).
On the basis of the pharmacologic actions of metoprolol, the following general measures should be employed:
Elimination of the Drug: Gastric lavage should be performed.
Other clinical manifestations of overdose should be managed symptomatically based on modern methods of intensive care.
Hypotension: A vasopressor should be administered, e.g., levarterenol or dopamine.
Bronchospasm: A beta2 -stimulating agent and/or a theophylline derivative should be administered.
Cardiac Failure: A digitalis glycoside and diuretic should be administered. In shock resulting from inadequate cardiac contractility, administration of dobutamine, isoproterenol, or glucagon may be considered.
-
DOSAGE & ADMINISTRATION SECTION
Hypertension
The dosage of metoprolol tartrate tablets should be individualized. Metoprolol tartrate tablets should be taken with or immediately following meals.
The usual initial dosage of Metoprolol tartrate tablets is 100 mg daily in single or divided doses, whether used alone or added to a diuretic. The dosage may be increased at weekly (or longer) intervals until optimum blood pressure reduction is achieved. In general, the maximum effect of any given dosage level will be apparent after 1 week of therapy. The effective dosage range of Metoprolol tartrate tablets is 100 to 450 mg per day. Dosages above 450 mg per day have not been studied. While once-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, lower doses (especially 100 mg) may not maintain a full effect at the end of the 24-hour period, and larger or more frequent daily doses may be required. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. Beta1 selectivity diminishes as the dose of metoprolol is increased.
Angina Pectoris
The dosage of metoprolol tartrate tablets should be individualized. Metoprolol tartrate tablets should be taken with or immediately following meals.
The usual initial dosage of Metoprolol tartrate tablets is 100 mg daily, given in two divided doses. The dosage may be gradually increased at weekly intervals until optimum clinical response has been obtained or there is pronounced slowing of the heart rate. The effective dosage range of Metoprolol tartrate tablets is 100 to 400 mg per day. Dosages above 400 mg per day have not been studied. If treatment is to be discontinued, the dosage should be reduced gradually over a period of 1 to 2 weeks (see WARNINGS).
Myocardial InfarctionEarly Treatment
During the early phase of definite or suspected acute myocardial infarction, treatment with metoprolol tartrate can be initiated as soon as possible after the patient’s arrival in the hospital. Such treatment should be initiated in a coronary care or similar unit immediately after the patient’s hemodynamic condition has stabilized.
Treatment in this early phase should begin with the intravenous administration of three bolus injections of 5 mg of metoprolol tartrate each; the injections should be given at approximately 2-minute intervals. During the intravenous administration of metoprolol, blood pressure, heart rate, and electrocardiogram should be carefully monitored.
In patients who tolerate the full intravenous dose (15 mg), metoprolol tartrate tablets, 50 mg every 6 hours, should be initiated 15 minutes after the last intravenous dose and continued for 48 hours. Thereafter, patients should receive a maintenance dosage of 100 mg twice daily (see Late Treatment below).
Patients who appear not to tolerate the full intravenous dose should be started on metoprolol tartrate tablets either 25 mg or 50 mg every 6 hours (depending on the degree of intolerance) 15 minutes after the last intravenous dose or as soon as their clinical condition allows. In patients with severe intolerance, treatment with metoprolol should be discontinued (see WARNINGS).
Late Treatment
Patients with contraindications to treatment during the early phase of suspected or definite myocardial infarction, patients who appear not to tolerate the full early treatment, and patients in whom the physician wishes to delay therapy for any other reason should be started on metoprolol tartrate tablets, 100 mg twice daily, as soon as their clinical condition allows. Therapy should be continued for at least 3 months. Although the efficacy of metoprolol beyond 3 months has not been conclusively established, data from studies with other beta blockers suggest that treatment should be continued for 1 to 3 years.
Special populations
Pediatric patients: No pediatric studies have been performed. The safety and efficacy of Metoprolol Tartrate in pediatric patients have not been established.
Renal impairment: No dose adjustment of Metoprolol Tartrate is required in patients with renal impairment.
Hepatic impairment: Metoprolol Tartrate blood levels are likely to increase substantially in patients with hepatic impairment. Therefore, Metoprolol Tartrate should be initiated at low doses with cautious gradual dose titration according to clinical response.
Geriatric patients (>65 years): In general, use a low initial starting dose in elderly patients given their greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Method of administration:
For oral treatment, the tablets should be swallowed un-chewed with a glass of water. Metoprolol Tartrate should always be taken in standardized relation with meals. If the physician asks the patient to take Metoprolol Tartrate either before breakfast or with breakfast, then the patient should continue taking Metoprolol Tartrate with the same schedule during the course of therapy.
-
HOW SUPPLIED SECTION
Metoprolol Tartrate Tablets USP, 25 mg - White, circular, film coated tablets debossed with “1” on one side and plain on the other side
Bottles of 30 NDC 57664-506-54
Bottles of 90 NDC 57664-506-59
Bottles of 100 NDC 57664-506-52
Bottles of 1000 NDC 57664-506-58
Samples, when available, are identified by the word SAMPLE appearing on each bottle.
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F) [See USP Controlled Room Temperature]. Dispense in tight, light-resistant container (USP). Protect from Moisture.
To report SUSPECTED ADVERSE REACTIONS, contact Caraco Pharmaceutical Laboratories, Ltd. at 1-800-818-4555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Manufactured by:
Sun Pharmaceutical Industries
Dadra 396 191, India
Distributed by:
Caraco Pharmaceutical Laboratories, Ltd.
1150 Elijah McCoy Drive C.S. No.: 5094T86
Detroit, MI 48202
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
METOPROLOL TARTRATE
metoprolol tartrate tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:61919-052(NDC:57664-506) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METOPROLOL TARTRATE (UNII: W5S57Y3A5L) (METOPROLOL - UNII:GEB06NHM23) METOPROLOL TARTRATE 25 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOLS (UNII: 3WJQ0SDW1A) POLYSORBATE 20 (UNII: 7T1F30V5YH) POVIDONE (UNII: FZ989GH94E) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white Score no score Shape ROUND Size 5mm Flavor Imprint Code 1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:61919-052-90 90 in 1 BOTTLE; Type 0: Not a Combination Product 01/29/2015 2 NDC:61919-052-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/29/2015 3 NDC:61919-052-82 180 in 1 BOTTLE; Type 0: Not a Combination Product 01/01/2014 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076670 01/01/2014 Labeler - DIRECT RX (079254320) Establishment Name Address ID/FEI Business Operations DIRECT RX 079254320 relabel(61919-052) , repack(61919-052)