Label: ZIDOVUDINE syrup
-
Contains inactivated NDC Code(s)
NDC Code(s): 53104-0105-9 - Packager: Cipla Ltd.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated November 27, 2018
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Zidovudine safely and effectively. See full prescribing information for Zidovudine.
ZIDOVUDINE Syrup [zidovudine oral solution] 50mg/5mL, for oral use
Rx only
Initial U.S. Approval: 1987
WARNING: RISK OF HEMATOLOGICAL TOXICITY, MYOPATHY, LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS.
See full prescribing information for complete boxed warning.
- Hematologic toxicity including neutropenia and severe anemia have been associated with the use of zidovudine. (5.1)
- Symptomatic myopathy associated with prolonged use of zidovudine. (5.3)
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues including zidovudine. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occur. (5.4)
RECENT MAJOR CHANGES
Dosage and Administration, Prevention of Maternal-Fetal HIV-1 Transmission (2.3) - 09/2018
Warnings and Precautions, Allergic Reaction to Latex 11/2017 (5.2)
Warnings and Precautions, Lactic Acidosis and Severe Hepatomegaly with Steatosis (5.4) - 11/2017
Warnings and Precautions, Lipoatrophy (5.7) – 11/2017
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Treatment of HIV-1 infection:
Adults: Recommended oral dosage is 300 mg twice a day with other antiretroviral agents. (2.1)
Pediatric patients (aged 4 weeks to less than 18 years): Dosage should be calculated based on body weight not to exceed adult dose. (2.2)
- Prevention of maternal-fetal HIV-1 transmission: Specific dosage instructions for mother and infant. (2.3)
- Patients with severe anemia and/or neutropenia: Dosage interruption may be necessary. (2.4)
- Renal impairment: Recommended oral dosage in hemodialysis or peritoneal dialysis or in patients with creatinine clearance (CrCl) less than 15 mL per minute is 100 mg every 6 to 8 hours. (2.5)
DOSAGE FORMS AND STRENGTHS
Oral Solution 50mg/5mL (3)
CONTRAINDICATIONS
Hypersensitivity to zidovudine or any of the components (e.g., anaphylaxis, Stevens-Johnson syndrome). (4)
WARNINGS AND PRECAUTIONS
- See boxed warning for information about the following: hematologic toxicity, myopathy, and lactic acidosis and severe hepatomegaly. (5.1,5.3, 5.4)
- Exacerbation of anemia has been reported in HIV-1/HCV co-infected patients receiving ribavirin and zidovudine. Coadministration of ribavirin and zidovudine is not advised. (5.5)
- Hepatic decompensation, (some fatal), has occurred in HIV-1/HCV co-infected patients receiving combination antiretroviral therapy and interferon alfa with/without ribavirin. Discontinue zidovudine as medically appropriate and consider dose reduction or discontinuation of interferon alfa, ribavirin, or both. (5.5)
- Immune reconstitution syndrome (5.6) and lipoarthropy (5.7) have been reported in patients treated with combination antiretroviral therapy.
ADVERSE REACTIONS
- Most commonly reported adverse reactions (incidence greater than or equal to 15%) in adult HIV-1 clinical trials were headache, malaise, nausea, anorexia, and vomiting. (6.1)
- Most commonly reported adverse reactions (incidence greater than or equal to 15%) in pediatric HIV-1 clinical trials were fever and cough. (6.1)
- Most commonly reported adverse reactions in neonates (incidence greater than or equal to 15%) in the prevention of maternal-fetal transmission of HIV-1 clinical trial were anemia and neutropenia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Cipla Ltd. at 1-866-604-3268 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Lactation: Women infected with HIV should be instructed not to breastfeed due to potential for HIV transmission. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF HEMATOLOGICAL TOXICITY, MYOPATHY, LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS
1 INDICATIONS AND USAGE
1.1 Treatment of HIV-1
1.2 Prevention of Maternal-Fetal HIV-1 Transmission
2 DOSAGE AND ADMINISTRATION
2.1 Adults - Treatment of HIV-1 Infection
2.2 Pediatric Patients (Aged 4 Weeks to Less than 18 Years)
2.3 Prevention of Maternal-Fetal HIV-1 Transmission
2.4 Patients with Severe Anemia and/or Neutropenia
2.5 Patients with Renal Impairment
2.6 Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hematologic Toxicity/Bone Marrow Suppression
5.3 Myopathy
5.4 Lactic Acidosis and Severe Hepatomegaly with Steatosis
5.5 Use with Interferon- and Ribavirin-Based Regimens in HIV-1/HCV Co-infected Patients
5.6 Immune Reconstitution Syndrome
5.7 Lipoatrophy
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Antiretroviral Agents
7.2 Doxorubicin
7.3 Hematologic/Bone Marrow Suppressive/Cytotoxic Agents
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adults
14.2 Pediatric Patients
14.3 Prevention of Maternal-Fetal HIV-1 Transmission
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF HEMATOLOGICAL TOXICITY, MYOPATHY, LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS
Zidovudine Oral Solution has been associated with hematologic toxicity including neutropenia and severe anemia, particularly in patients with advanced HIV-1 disease [see Warnings and Precautions (5.1)].
Prolonged use of zidovudine has been associated with symptomatic myopathy [see Warnings and Precautions (5.3)].
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including zidovudine and other antiretrovirals. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occur [see Warnings and Precautions (5.4)].
-
1 INDICATIONS AND USAGE
1.1 Treatment of HIV-1
Zidovudine Syrup (Zidovudine oral solution), a nucleoside reverse transcriptase inhibitor, is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection.
1.2 Prevention of Maternal-Fetal HIV-1 Transmission
Zidovudine Syrup (Zidovudine oral solution) is indicated for the prevention of maternal-fetal HIV-1 transmission [see Dosage and Administration (2.3)]. The indication is based on a dosing regimen that included 3 components:
- antepartum therapy of HIV-1 infected mothers
- intrapartum therapy of HIV-1 infected mothers
- post-partum therapy of HIV-1 exposed neonate.
Points to consider prior to initiating zidovudine in pregnant women for the prevention of maternal-fetal HIV-1 transmission include:
- In most cases, zidovudine for prevention of maternal-fetal HIV-1 transmission should be given in combination with other antiretroviral drugs.
- Prevention of HIV-1 transmission in women who have received zidovudine for a prolonged period before pregnancy has not been evaluated.
- Because the fetus is most susceptible to the potential teratogenic effects of drugs during the first 10 weeks of gestation and the risks of therapy with zidovudine during that period are not fully known, women in the first trimester of pregnancy who do not require immediate initiation of antiretroviral therapy for their own health may consider delaying use; this indication is based on use after 14 weeks' gestation.
-
2 DOSAGE AND ADMINISTRATION
2.1 Adults - Treatment of HIV-1 Infection
The recommended oral dose of zidovudine is 300 mg twice daily in combination with other antiretroviral agents.
2.2 Pediatric Patients (Aged 4 Weeks to Less than 18 Years)
Healthcare professionals should pay special attention to accurate calculation of the dose of zidovudine, transcription of the medication order, dispensing information, and dosing instructions to minimize risk for medication dosing errors.
Prescribers should calculate the appropriate dose of zidovudine for each child based on body weight (kg) and should not exceed the recommended adult dose.
Before prescribing zidovudine capsules, children should be assessed for the ability to swallow capsules. If a child is unable to reliably swallow a zidovudine capsule, the zidovudine syrup formulation should be prescribed.
The recommended oral dosage in pediatric patients aged 4 weeks to less than 18 years and weighing greater than or equal to 4 kg is provided in Table 1. Zidovudine syrup should be used to provide accurate dosage when capsules are not appropriate.
Table 1: Recommended Pediatric Oral Dosage of Zidovudine Body Weight (kg)
Total Daily Dose
Dosage Regimen and Dose
b.i.d.
t.i.d.
4 to <9
24 mg/kg/day
12 mg/kg
8 mg/kg
≥9 to <30
18 mg/kg/day
9 mg/kg
6 mg/kg
≥30
600 mg/day
300 mg
200 mg
Alternatively, dosing for zidovudine can be based on body surface area (BSA) for each child. The recommended oral dose of zidovudine is 480 mg per m2 per day in divided doses (240 mg per m2 twice daily or 160 mg per m2 three times daily). In some cases the dose calculated by mg per kg will not be the same as that calculated by BSA.
2.3 Prevention of Maternal-Fetal HIV-1 Transmission
The recommended dosage regimen for administration to pregnant women (greater than 14 weeks of pregnancy) and their neonates is:
Maternal Dosing
100 mg orally 5 times per day until the start of labor [see Clinical Studies (14.3)]. During labor and delivery, intravenous zidovudine should be administered at 2 mg per kg (total body weight) over 1 hour followed by a continuous intravenous infusion of 1 mg per kg per hour (total body weight) until clamping of the umbilical cord.
Neonatal Dosing
Start neonatal dosing within 12 hours after birth and continue through 6 weeks of age. Neonates unable to receive oral dosing may be administered zidovudine intravenously. See Table 2 for dosing recommendations.
Table 2: Recommended Neonatal Dosages of Zidovudine Route
Total Daily Dose
Dose and Dosage Regimen
Oral
8 mg/kg/day
2 mg/kg every 6 hours
Intravenous
6 mg/kg/day
1.5 mg/kg infused over 30 minutes, every 6 hours
Use an appropriate-sized syringe with 0.1-mL graduation to ensure accurate dosing of the syrup formulation in neonates.
2.4 Patients with Severe Anemia and/or Neutropenia
Significant anemia (hemoglobin less than 7.5 g per dL or reduction greater than 25% of baseline) and/or significant neutropenia (granulocyte count less than 750 cells per mm3 or reduction greater than 50% from baseline) may require a dose interruption until evidence of marrow recovery is observed [see Warnings and Precautions (5.1)]. In patients who develop significant anemia, dose interruption does not necessarily eliminate the need for transfusion. If marrow recovery occurs following dose interruption, resumption in dose may be appropriate using adjunctive measures such as epoetin alfa at recommended doses, depending on hematologic indices such as serum erythropoietin level and patient tolerance.
2.5 Patients with Renal Impairment
In patients maintained on hemodialysis or peritoneal dialysis or with creatinine clearance (CrCl) by Cockcroft-Gault less than 15 mL per min, the recommended oral dosage is 100 mg every 6 to 8 hours [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
2.6 Patients with Hepatic Impairment
There are insufficient data to recommend dose adjustment of zidovudine in patients with impaired hepatic function or liver cirrhosis. Frequent monitoring of hematologic toxicities is advised [see Use in Specific Populations (8.7)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hematologic Toxicity/Bone Marrow Suppression
Zidovudine oral solution should be used with caution in patients who have bone marrow compromise evidenced by granulocyte count less than 1,000 cells per mm3 or hemoglobin less than 9.5 g per dL. Hematologic toxicities appear to be related to pretreatment bone marrow reserve and to dose and duration of therapy. In patients with advanced symptomatic HIV-1 disease, anemia and neutropenia were the most significant adverse events observed. In patients who experience hematologic toxicity, a reduction in hemoglobin may occur as early as 2 to 4 weeks, and neutropenia usually occurs after 6 to 8 weeks. There have been reports of pancytopenia associated with the use of zidovudine, which was reversible in most instances after discontinuance of the drug. However, significant anemia, in many cases requiring dose adjustment, discontinuation of zidovudine, and/or blood transfusions, has occurred during treatment with zidovudine alone or in combination with other antiretrovirals.
Frequent blood counts are strongly recommended to detect severe anemia or neutropenia in patients with poor bone marrow reserve, particularly in patients with advanced HIV-1 disease who are treated with zidovudine. For HIV-1-infected individuals and patients with asymptomatic or early HIV-1 disease, periodic blood counts are recommended. If anemia or neutropenia develops, dosage interruption may be needed [see Dosage and Administration (2.4)].
5.3 Myopathy
Myopathy and myositis with pathological changes, similar to that produced by HIV-1 disease, have been associated with prolonged use of zidovudine.
5.4 Lactic Acidosis and Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues, including zidovudine. A majority of these cases have been in women. Female sex and obesity may be risk factors for the development of lactic acidosis and severe hepatomegaly with steatosis in patients treated with antiretroviral nucleoside analogues. Treatment with zidovudine should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity, which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations.
5.5 Use with Interferon- and Ribavirin-Based Regimens in HIV-1/HCV Co-infected Patients
In vitro studies have shown ribavirin can reduce the phosphorylation of pyrimidine nucleoside analogues such as zidovudine. Although no evidence of a pharmacokinetic or pharmacodynamic interaction (e.g., loss of HIV-1/HCV virologic suppression) was seen when ribavirin was coadministered with zidovudine in HIV-1/HCV co-infected subjects [see Clinical Pharmacology (12.3)], exacerbation of anemia due to ribavirin has been reported when zidovudine is part of the HIV regimen. Coadministration of ribavirin and zidovudine is not advised. Consideration should be given to replacing zidovudine in established combination HIV-1/HCV therapy, especially in patients with a known history of zidovudine-induced anemia.
Hepatic decompensation (some fatal) has occurred in HIV-1/HCV co-infected patients receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin. Patients receiving interferon alfa with or without ribavirin and zidovudine should be closely monitored for treatment-associated toxicities, especially hepatic decompensation, neutropenia, and anemia.
Discontinuation of zidovudine should be considered as medically appropriate. Dose reduction or discontinuation of interferon alfa, ribavirin, or both should also be considered if worsening clinical toxicities are observed, including hepatic decompensation (e.g., Child-Pugh greater than 6) (See the full prescribing information for interferon and ribavirin).
5.6 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including zidovudine. During the initial phase of combination antiretroviral treatment, patients whose immune systems respond may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves disease, polymyositis, and Guillain-Barre syndrome) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.7 Lipoatrophy
Treatment with zidovudine has been associated with loss of subcutaneous fat. The incidence and severity of lipoatrophy are related to cumulative exposure. This fat loss, which is most evident in the face, limbs, and buttocks, may be only partially reversible and improvement may take months to years after switching to a non-zidovudine-containing regimen. Patients should be regularly assessed for signs of lipoatrophy during therapy with zidovudine and other zidovudine-containing products, and if feasible, therapy should be switched to an alternative regimen if there is suspicion of lipoatrophy.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Hematologic toxicity, including neutropenia and anemia[see Boxed Warning, Warnings and Precautions (5.1)] .
- Symptomatic myopathy[see Boxed Warning, Warnings and Precautions (5.3)] .
- Lactic acidosis and severe hepatomegaly with steatosis[see Boxed Warning, Warnings and Precautions (5.4)] .
- Hepatic decompensation in patients co-infected with HIV-1 and hepatitis C[see Warnings and Precautions (5.5)] .
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
The frequency and severity of adverse reactions associated with the use of zidovudine are greater in patients with more advanced infection at the time of initiation of therapy.
Table 3 summarizes adverse reactions reported at a statistically significant greater incidence for subjects receiving oral zidovudine in a monotherapy trial.
Table 3: Percentage (%) of Subjects with Adverse Reactions (Greater than or Equal to 5% Frequency) in Asymptomatic HIV-1 Infection (ACTG019) a Not statistically significant versus placebo.
Adverse Reaction
Zidovudine 500 mg/day
(n = 453)
Placebo
(n = 428)
Body as a whole
Asthenia
9% a
6%
Headache
63%
53%
Malaise
53%
45%
Gastrointestinal
Anorexia
20%
11 %
Constipation
6% a
4%
Nausea
51 %
30%
Vomiting
17%
10%
In addition to the adverse reactions listed in Table 3, adverse reactions observed at an incidence of greater than or equal to 5% in any treatment arm in clinical trials (NUCA3001, NUCA3002, NUCB3001, and NUCB3002) were abdominal cramps, abdominal pain, arthralgia, chills, dyspepsia, fatigue, insomnia, musculoskeletal pain, myalgia, and neuropathy. Additionally, in these trials hyperbilirubinemia was reported at an incidence of less than or equal to 0.8%.
Selected laboratory abnormalities observed during a clinical trial of monotherapy with oral zidovudine are shown in Table 4.
Table 4: Frequencies of Selected (Grade 3/4) Laboratory Abnormalities in Subjects with Asymptomatic HIV-1 Infection (ACTG 019) ULN = Upper limit of normal.
Test
(Abnormal Level)
Zidovudine 500 mg/day
(n = 453)
Placebo
(n = 428)
Anemia (Hgb<8 g/dL)
1%
<1%
Granulocytopenia (<750 cells/mm3)
2%
2%
Thrombocytopenia (platelets<50,000/mm3)
0%
<1%
ALT (>5 x ULN)
3%
3%
AST (>5 x ULN)
1%
2%
The clinical adverse reactions reported among adult recipients of zidovudine may also occur in pediatric patients.
Trial ACTG 300: Selected clinical adverse reactions and physical findings with a greater than or equal to 5% frequency during therapy with EPIVIR (lamivudine) oral suspension 4 mg per kg twice daily plus zidovudine 160 mg per m2 3 times daily compared with didanosine in therapy-naive (less than or equal to 56 days of antiretroviral therapy) pediatric subjects are listed in Table 5.
Table 5: Selected Clinical Adverse Reactions and Physical Findings (Greater than or Equal to 5% Frequency) in Pediatric Subjects in Trial ACTG 300 a Includes pain, discharge, erythema, or swelling of an ear.
Adverse Reaction
EPIVIR plus Zidovudine
(n = 236)
Didanosine
(n = 235)
Body as a whole
Fever
25%
32%
Digestive
Hepatomegaly
11%
11%
Nausea & vomiting
8%
7%
Diarrhea
8%
6%
Stomatitis
6%
12%
Splenomegaly
5%
8%
Respiratory
Cough
15%
18%
Abnormal breath sounds/wheezing
7%
9%
Ear, Nose, and Throat
Signs or symptoms of earsa
7%
6%
Nasal discharge or congestion
8%
11%
Other
Skin rashes
12%
14%
Lymphadenopathy
9%
11%
Selected laboratory abnormalities experienced by therapy-naive (less than or equal to 56 days of antiretroviral therapy) pediatric subjects are listed in Table 6.
Table 6. Frequencies of Selected (Grade 3/4) Laboratory Abnormalities in Pediatric Subjects in Trial ACTG 300 ULN = Upper limit of normal.
ANC = Absolute neutrophil count.
Test
(Abnormal Level)
EPIVIR plus Zidovudine
Didanosine
Neutropenia (ANC<400 cells/mm3)
8%
3%
Anemia (Hgb<7.0 g/dL)
4%
2%
Thrombocytopenia (platelets<50,000/mm3)
1%
3%
ALT (>10 x ULN)
1%
3%
AST (>10 x ULN)
2%
4%
Lipase (>2.5 x ULN)
3%
3%
Total amylase (>2.5 x ULN)
3%
3%
Macrocytosis was reported in the majority of pediatric subjects receiving zidovudine 180 mg per m2 every 6 hours in open-label trials. Additionally, adverse reactions reported at an incidence of less than 6% in these trials were congestive heart failure, decreased reflexes, ECG abnormality, edema, hematuria, left ventricular dilation, nervousness/irritability, and weight loss.
Use for the Prevention of Maternal-Fetal Transmission of HIV-1
In a randomized, double-blind, placebo-controlled trial in HIV-1-infected women and their neonates conducted to determine the utility of zidovudine for the prevention of maternal-fetal HIV-1 transmission, zidovudine syrup at 2 mg per kg was administered every 6 hours for 6 weeks to neonates beginning within 12 hours following birth. The most commonly reported adverse reactions were anemia (hemoglobin less than 9.0 g per dL) and neutropenia (less than 1,000 cells per mm3). Anemia occurred in 22% of the neonates who received zidovudine and in 12% of the neonates who received placebo. The mean difference in hemoglobin values was less than 1.0 g per dL for neonates receiving zidovudine compared with neonates receiving placebo. No neonates with anemia required transfusion and all hemoglobin values spontaneously returned to normal within 6 weeks after completion of therapy with zidovudine. Neutropenia in neonates was reported with similar frequency in the group that received zidovudine (21%) and in the group that received placebo (27%). The long-term consequences of in utero and infant exposure to zidovudine are unknown.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of zidovudine. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole
Back pain, chest pain, flu-like syndrome, generalized pain, redistribution/accumulation of body fat [see Warnings and Precautions (5.7)].
Cardiovascular
Cardiomyopathy, syncope.
Eye
Macular edema.
Gastrointestinal
Constipation, dysphagia, flatulence, oral mucosa pigmentation, mouth ulcer.
General
Sensitization reactions including anaphylaxis and angioedema, vasculitis.
Hematologic
Aplastic anemia, hemolytic anemia, leukopenia, lymphadenopathy, pancytopenia with marrow hypoplasia, pure red cell aplasia.
Hepatobiliary
Hepatitis, hepatomegaly with steatosis, jaundice, lactic acidosis, pancreatitis.
Musculoskeletal
Increased CPK, increased LDH, muscle spasm, myopathy and myositis with pathological changes (similar to that produced by HIV-1 disease), rhabdomyolysis, tremor.
Nervous
Anxiety, confusion, depression, dizziness, loss of mental acuity, mania, paresthesia, seizures, somnolence, vertigo.
Reproductive System and Breast
Gynecomastia.
Respiratory
Dyspnea, rhinitis, sinusitis.
Skin and Subcutaneous Tissue
Changes in skin and nail pigmentation, pruritus, Stevens-Johnson syndrome, toxic epidermal necrolysis, sweating, urticaria.
Special Senses
Amblyopia, hearing loss, photophobia, taste perversion.
Renal and Urinary
Urinary frequency, urinary hesitancy.
-
7 DRUG INTERACTIONS
7.1 Antiretroviral Agents
Concomitant use of zidovudine with stavudine should be avoided since an antagonistic relationship has been demonstrated in vitro.
Nucleoside Analogues Affecting DNA Replication
Some nucleoside analogues affecting DNA replication, such as ribavirin, antagonize the in vitro antiviral activity of zidovudine against HIV-1; concomitant use of such drugs should be avoided.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to zidovudine during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Available data from the APR show no difference in the overall risk of birth defects for zidovudine compared with the background rate for birth defects of 2.7% in the Metropolitan Atlanta Congenital Defects Program (MACDP) reference population (see Data). The APR uses the MACDP as the U.S. reference population for birth defects in the general population. The MACDP evaluates women and infants from a limited geographic area and does not include outcomes for births that occurred at less than 20 weeks' gestation. The rate of miscarriage is not reported in the APR. The estimated background rate of miscarriage in clinically recognized pregnancies in the U.S. general population is 15% to 20%. The background risk for major birth defects and miscarriage for the indicated population is unknown.
Hyperlactatemia, which may be due to mitochondrial dysfunction, has been reported in infants with in utero exposure to zidovudine-containing products. These events were transient and asymptomatic in most cases. There have been few reports of developmental delay, seizures, and other neurological disease. However, a causal relationship between these events and exposure to zidovudine-containing products in utero or peri-partum has not been established (see Data).
In an animal reproduction study, administration of oral zidovudine to female rats prior to mating and throughout gestation resulted in embryotoxicity at doses that produced systemic exposure (AUC) approximately 33 times higher than exposure at the recommended clinical dose. However, no embryotoxicity was observed after oral administration of zidovudine to pregnant rats during organogenesis at doses that produced systemic exposure (AUC) approximately 117 times higher than exposures at the recommended clinical dose. Administration of oral zidovudine to pregnant rabbits during organogenesis resulted in embryotoxicity at doses that produced systemic exposure (AUC) approximately 108 times higher than exposure at the recommended clinical dose. However, no embryotoxicity was observed at doses that produced systemic exposure (AUC) approximately 23 times higher than exposures at the recommended clinical dose (see Data).
Data
Human Data: Based on prospective reports to the APR of over 13,000 exposures to zidovudine during pregnancy resulting in live births (including over 4,000 exposed in the first trimester), there was no difference between the overall risk of birth defects for zidovudine compared with the background birth defect rate of 2.7% in a U.S. reference population of the MACDP. The prevalence of birth defects in live births was 3.2% (95% CI: 2.7% to 3.8%) following first trimester exposure to zidovudine-containing regimens and 2.8% (95% CI: 2.5% to 3.2%) following second/third trimester exposure to zidovudine-containing regimens.
A randomized, double-blind, placebo-controlled trial was conducted in HIV-1-infected pregnant women to determine the utility of zidovudine for the prevention of maternal-fetal HIV-1-transmission [see Clinical Studies (14.3)]. Zidovudine treatment during pregnancy reduced the rate of maternal-fetal HIV-1 transmission from 24.9% for infants born to placebo-treated mothers to 7.8% for infants born to mothers treated with zidovudine. There were no differences in pregnancy-related adverse events between the treatment groups. Of the 363 neonates that were evaluated, congenital abnormalities occurred with similar frequency between neonates born to mothers who received zidovudine and neonates born to mothers who received placebo. The observed abnormalities included problems in embryogenesis (prior to 14 weeks) or were recognized on ultrasound before or immediately after initiation of study drug.
Zidovudine has been shown to cross the placenta and concentrations in neonatal plasma at birth were essentially equal to those in maternal plasma at delivery [see Clinical Pharmacology (12.3)]. There have been reports of mild, transient elevations in serum lactate levels, which may be due to mitochondrial dysfunction, in neonates and infants exposed in utero or peri-partum to zidovudine-containing products. There have been few reports of developmental delay, seizures, and other neurological disease. However, a causal relationship between these events and exposure to zidovudine-containing products in utero or peri-partum has not been established. The clinical relevance of transient elevations in serum lactate is unknown.
Animal Data: A study in pregnant rats (at 50, 150, or 450 mg per kg per day starting 26 days prior to mating through gestation to postnatal Day 21) showed increased fetal resorptions at doses that produced systemic exposures (AUC) approximately 33 times higher than exposure at the recommended daily human dose (300 mg twice daily). However, in an oral embryo-fetal development study in rats (at 125, 250, or 500 mg per kg per day on gestation Days 6 through 15), no fetal resorptions were observed at doses that produced systemic exposure (AUC) approximately 117 times higher than exposures at the recommended daily human dose. An oral embryo-fetal development study in rabbits (at 75, 150, or 500 mg per kg per day on gestation Day 6 through 18) showed increased fetal resorptions at the 500-mg-per-kg-per-day dose, which produced systemic exposures (AUC) approximately 108 times higher than exposure at the recommended daily human dose; however, no fetal resorptions were noted at doses up to 150 mg per kg per day, which produced systemic exposure (AUC) approximately 23 times higher than exposures at the recommended daily human dose. These oral embryo-fetal development studies in the rat and rabbit revealed no evidence of fetal malformations with zidovudine. In another developmental toxicity study, pregnant rats (dosed at 3,000 mg per kg per day from Days 6 through 15 of gestation) showed marked maternal toxicity and an increased incidence of fetal malformations at exposures greater than 300 times the recommended daily human dose based on AUC. However, there were no signs of fetal malformations at doses up to 600 mg per kg per day.
8.2 Lactation
The Centers for Disease Control and Prevention recommends that HIV-1-infected mothers in the United States not breastfeed their infants to avoid risking postnatal transmission of HIV-1 infection. Zidovudine is present in human milk. There is no information on the effects of zidovudine on the breastfed infant or the effects of the drug on milk production. Because of the potential for (1) HIV-1 transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants), and (3) adverse reactions in a breastfed infant instruct mothers not to breastfeed if they are receiving zidovudine.
8.4 Pediatric Use
Zidovudine has been studied in HIV-1-infected pediatric subjects aged at least 6 weeks who had HIV-1-related symptoms or who were asymptomatic with abnormal laboratory values indicating significant HIV-1-related immunosuppression. Zidovudine has also been studied in neonates perinatally exposed to HIV-1 [see Dosage and Administration (2.2), Adverse Reactions (6.1);Clinical Pharmacology (12.3);Clinical Studies (14.2); (14.3)].
8.5 Geriatric Use
Clinical studies of zidovudine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
Unchanged zidovudine and its glucuronide metabolite (formed in the liver) are primarily eliminated from the body by renal excretion. In patients with severely impaired renal function (CrCl less than 15 mL per min), dosage reduction is recommended [see Dosage and Administration (2.5), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Zidovudine is primarily eliminated by hepatic metabolism and zidovudine concentrations appear to be increased in patients with impaired hepatic function, which may increase the risk of hematologic toxicity. Frequent monitoring of hematologic toxicities is advised. There are insufficient data to recommend dose adjustment of zidovudine in patients with impaired hepatic function or liver cirrhosis [see Dosage and Administration (2.6), Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Acute overdoses of zidovudine have been reported in pediatric patients and adults. These involved exposures up to 50 grams. No specific symptoms or signs have been identified following acute overdosage with zidovudine apart from those listed as adverse events such as fatigue, headache, vomiting, and occasional reports of hematological disturbances. Patients recovered without permanent sequelae. Hemodialysis and peritoneal dialysis appear to have a negligible effect on the removal of zidovudine while elimination of its primary metabolite, 3′- azido-3′-deoxy-5′-O-β-D-glucopyranuronosylthymidine (GZDV), is enhanced. If overdose occurs, the patient should be monitored for evidence of toxicity and given standard supportive treatment as required.
-
11 DESCRIPTION
Zidovudine (formerly called azidothymidine [AZT]) is a pyrimidine nucleoside analogue active against HIV-1. The chemical name of zidovudine is 3'-azido-3'-deoxythymidine; it has the following structural formula:
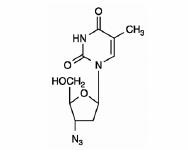
Zidovudine
Zidovudine is a white to beige, odorless, crystalline solid with a molecular weight of 267.24 and a solubility of 20.1 mg per mL in water at 25°C. The molecular formula is C10H13N5O4.
Zidovudine Syrup (Zidovudine oral solution USP) is for oral administration. Each teaspoonful (5 mL) of Zidovudine Syrup (Zidovudine oral solution USP) contains 50 mg of zidovudine and the inactive ingredients are sodium benzoate 0.2% (added as a preservative), citric acid, flavors, glycerin, and sucrose.
Complies with HPLC Procedure 2 of the USP monograph.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Absorption and Bioavailability
In adults, following oral administration, zidovudine is rapidly absorbed and extensively distributed, with peak serum concentrations occurring within 0.5 to 1.5 hours. The AUC was equivalent when zidovudine was administered as zidovudine tablets or syrup compared with zidovudine capsules. The pharmacokinetic properties of zidovudine in fasting adult subjects are summarized in Table 7.
Table 7. Zidovudine Pharmacokinetic Parameters in Adult Subjects aMedian [range] for 50 paired samples drawn 1 to 8 hours after the last dose in subjects on chronic therapy with zidovudine.
bApproximate range
Parameter
Mean ± SD
(except where noted)
Oral bioavailability (%)
64 ± 10
(n = 5)
Apparent volume of distribution (L/kg)
1.6 ± 0.6
(n = 8)
Cerebrospinal fluid (CSF): plasma ratioa
0.6 [0.04 to 2.62]
(n = 39)
Systemic clearance (L/h/kg)
1.6 ± 0.6
(n = 6)
Renal clearance (L/h/kg)
0.34 ± 0.05
(n = 9)
Elimination half-life (h)b
0.5 to 3
(n = 19)
The apparent volume of distribution of zidovudine, is 1.6 ± 0.6 L per kg (Table 7) and binding to plasma protein is low (less than 38%).
Metabolism and Elimination
Zidovudine is primarily eliminated by hepatic metabolism. The major metabolite of zidovudine is GZDV. GZDV AUC is about 3-fold greater than the zidovudine AUC. Urinary recovery of zidovudine and GZDV accounts for 14% and 74%, respectively, of the dose following oral administration. A second metabolite, 3′-amino-3′-deoxythymidine (AMT), has been identified in the plasma following single-dose IV administration of zidovudine. The AMT AUC was one-fifth of the zidovudine AUC. Pharmacokinetics of zidovudine were dose independent at oral dosing regimens ranging from 2 mg per kg every 8 hours to 10 mg per kg every 4 hours.
Effect of Food on Absorption
Zidovudine may be administered with or without food. The zidovudine AUC was similar when a single dose of zidovudine was administered with food.
Specific Populations
Patients with Renal Impairment: Zidovudine clearance was decreased resulting in increased zidovudine and GZDV half-life and AUC in subjects with impaired renal function (n = 14) following a single 200-mg oral dose (Table 8). Plasma concentrations of AMT were not determined. No dose adjustment is recommended for patients with CrCl greater than or equal to 15 mL per min.
Table 8. Zidovudine Pharmacokinetic Parameters in Subjectswith Severe Renal Impairmenta aData are expressed as mean ± standard deviation.
Parameter
Control Subjects
(Normal Renal Function)
Subjects With Renal Impairment
(n = 6)
(n = 14)
CrCl (mL/min)
120 ± 8
18 ± 2
Zidovudine AUC (ng•h/mL)
1,400 ± 200
3,100 ± 300
Zidovudine half-life (h)
1.0 ± 0.2
1.4 ± 0.1
Hemodialysis and Peritoneal Dialysis: The pharmacokinetics and tolerance of zidovudine were evaluated in a multiple-dose trial in subjects undergoing hemodialysis (n = 5) or peritoneal dialysis (n = 6) receiving escalating oral doses up to 200 mg 5 times daily for 8 weeks. Daily doses of 500 mg or less were well tolerated despite significantly elevated GZDV plasma concentrations. Apparent zidovudine oral clearance was approximately 50% of that reported in subjects with normal renal function. Hemodialysis and peritoneal dialysis appeared to have a negligible effect on the removal of zidovudine, whereas GZDV elimination was enhanced. A dosage adjustment is recommended for patients undergoing hemodialysis or peritoneal dialysis [see Dosage and Administration (2.5)].
Patients with Hepatic Impairment: Data describing the effect of hepatic impairment on the pharmacokinetics of zidovudine are limited. However, zidovudine is eliminated primarily by hepatic metabolism and it appears that zidovudine clearance is decreased and plasma concentrations are increased in subjects with hepatic impairment. There are insufficient data to recommend dose adjustment of zidovudine in patients with impaired hepatic function or liver cirrhosis [see Dosage and Administration (2.6)].
Pediatric Patients: Zidovudine pharmacokinetics have been evaluated in HIV-1-infected pediatric subjects (Table 9).
Patients Aged 3 Months to 12 Years: Overall, zidovudine pharmacokinetics in pediatric patients older than 3 months are similar to those in adult patients. Proportional increases in plasma zidovudine concentrations were observed following administration of oral solution from 90 to 240 mg per m2 every 6 hours. Oral bioavailability, terminal half-life, and oral clearance were comparable to adult values. As in adult subjects, the major route of elimination was by metabolism to GZDV. After IV dosing, about 29% of the dose was excreted in the urine unchanged, and about 45% of the dose was excreted as GZDV [see Dosage and Administration (2.2)].
Patients Aged Less than 3 Months: Zidovudine pharmacokinetics have been evaluated in pediatric subjects from birth to 3 months of life. Zidovudine elimination was determined immediately following birth in 8 neonates who were exposed to zidovudine in utero. The half-life was 13.0 ± 5.8 hours. In neonates less than or equal to 14 days old, bioavailability was greater, total body clearance was slower, and half-life was longer than in pediatric subjects older than 14 days. For dose recommendations for neonates [see Dosage and Administration (2.3)].
Table 9. Zidovudine Pharmacokinetic Parameters in Pediatric Subjectsa aData presented as mean ± standard deviation except where noted.
bMedian [range]
Parameter
Birth to 14 Days of Age
14 Days to 3 Months of Age
3 Months to 12 Years of Age
Oral bioavailability (%)
89 ± 19
(n = 15)
61 ± 19
(n = 17)
65 ± 24
(n = 18)
CSF:plasma ratio
no data
no data
0.68 [0.03 to 3.25]b
(n = 38)
CL (L/h/kg)
0.65 ± 0.29
(n = 18)
1.14 ± 0.24
(n = 16)
1.85 ± 0.47
(n = 20)
Elimination half-life (h)
3.1 ± 1.2
(n = 21)
1.9 ± 0.7
(n = 18)
1.5 ± 0.7
(n = 21)
Pregnant Women: Zidovudine pharmacokinetics have been studied in a Phase I trial of 8 women during the last trimester of pregnancy. Zidovudine pharmacokinetics were similar to those of nonpregnant adults. Consistent with passive transmission of the drug across the placenta, zidovudine concentrations in neonatal plasma at birth were essentially equal to those in maternal plasma at delivery [see Use in Specific Populations (8.1)].
Although data are limited, methadone maintenance therapy in 5 pregnant women did not appear to alter zidovudine pharmacokinetics.
Geriatric Patients: Zidovudine pharmacokinetics have not been studied in subjects over 65 years of age.
Male and Female Patients: A pharmacokinetic trial in healthy male (n = 12) and female (n = 12) subjects showed no differences in zidovudine AUC when a single dose of zidovudine was administered as a 300-mg zidovudine tablet.
Drug Interaction Studies
[See Drug Interactions (7)].
Table 10. Effect of Co-administered Drugs on Zidovudine AUC* ↑ = Increase; ↓ = Decrease; ↔ = No significant change; AUC = Area under the concentration versus time curve; CI = Confidence interval.
Note: ROUTINE DOSE MODIFICATION OF ZIDOVUDINE IS NOT WARRANTED WITH COADMINISTRATION OF THE FOLLOWING DRUGS.
Coadministered Drug and Dose
Zidovudine Oral Dose
n
Zidovudine
Concentrations
Concentration of Coadministered Drug
AUC
Variability
Atovaquone
750 mg every 12 h with food
200 mg every 8 h
14
↑31%
Range:
23% to 78%†
↔
Clarithromycin 500 mg twice daily
100 mg every 4 h x 7 days
4
↓12%
Range:
↓34% to ↑14% b
Not Reported
Fluconazole
400 mg daily
200 mg every 8 h
12
↑74%
95%
CI: 54% to 98%
Not Reported
Lamivudine 300 mg every 12 h
single 200 mg
12
↑13%
90%
CI: 2% to 27%
↔
Methadone
30 to 90 mg daily
200 mg every 4 h
9
↑43%
Range:
16% to 64%†
↔
Nelfinavir
750 mg every 8 h x 7 to 10 days
single 200 mg
11
↓35%
Range:
28% to 41% b
↔
Probenecid
500 mg every 6 h x 2 days
2 mg/kg every 8 h x 3 days
3
↑106%
Range:
100% to 170%†
Not Assessed
Rifampin
600 mg daily x 14 days
200 mg every 8 h x 14 days
8
↓47%
90% CI:
41% to 53%
Not Assessed
Ritonavir
300 mg every 6 h x 4 days
200 mg every 8 h x 4 days
9
↓25%
95% CI:
15% to 34%
↔
Valproic acid
250 mg or 500 mg every 8 h x 4 days
100 mg every 8 h x 4 days
6
↑80%
Range:
64% to 130%†
Not Assessed
Phenytoin: Phenytoin plasma levels have been reported to be low in some patients receiving zidovudine, while in one case a high level was documented. However, in a pharmacokinetic interaction trial in which 12 HIV-1-positive volunteers received a single 300-mg phenytoin dose alone and during steady-state zidovudine conditions (200 mg every 4 hours), no change in phenytoin kinetics was observed. Although not designed to optimally assess the effect of phenytoin on zidovudine kinetics, a 30% decrease in oral zidovudine clearance was observed with phenytoin.
Ribavirin: In vitro data indicate ribavirin reduces phosphorylation of lamivudine, stavudine, and zidovudine. However, no pharmacokinetic (e.g., plasma concentrations or intracellular triphosphorylated active metabolite concentrations) or pharmacodynamic (e.g., loss of HIV-1 /HCV virologic suppression) interaction was observed when ribavirin and lamivudine (n = 18), stavudine (n = 10), or zidovudine (n = 6) were coadministered as part of a multi-drug regimen to HIV-1/HCV co-infected subjects [see Warnings and Precautions (5.5)].
12.4 Microbiology
Zidovudine is a synthetic nucleoside analogue. Intracellularly, zidovudine is phosphorylated to its active 5'-triphosphate metabolite, zidovudine triphosphate (ZDV-TP). The principal mode of action of ZDV-TP is inhibition of reverse transcriptase (RT) via DNA chain termination after incorporation of the nucleotide analogue. ZDV-TP is a weak inhibitor of the cellular DNA polymerases α and γ and has been reported to be incorporated into the DNA of cells in culture.
Antiviral Activity
The antiviral activity of zidovudine against HIV-1 was assessed in a number of cell lines including monocytes and fresh human peripheral blood lymphocytes. The EC50 and EC90 values for zidovudine were 0.01 to 0.49 microM (1 microM = 0.27 mcg per mL) and 0.1 to 9 microM, respectively. HIV-1 from therapy-naive subjects with no amino acid substitutions associated with resistance gave median EC50 values of 0.011 microM (range: 0.005 to 0.110 microM) from Virco (n = 92 baseline samples) and 0.0017 microM (range: 0.006 to 0.0340 microM) from Monogram Biosciences (n = 135 baseline samples). The EC50 values of zidovudine against different HIV-1 clades (A-G) ranged from 0.00018 to 0.02 microM, and against HIV-2 isolates from 0.00049 to 0.004 microM. Zidovudine was not antagonistic to tested anti-HIV agents with the exception of stavudine where an antagonistic relationship with zidovudine has been demonstrated in cell culture. Ribavirin has been found to inhibit the phosphorylation of zidovudine in cell culture.
Resistance
HIV-1 isolates with reduced susceptibility to zidovudine have been selected in cell culture and were also recovered from subjects treated with zidovudine. Genotypic analyses of the isolates selected in cell culture and recovered from zidovudine-treated subjects showed thymidine analog mutation (TAMs) substitutions in the HIV-1 RT (M41L, D67N, K70R, L210W, T215Y or F, and K219E/R/H/Q/N/Q) that confer zidovudine resistance. In general, higher levels of resistance were associated with greater number of substitutions. In some subjects harboring zidovudine-resistant virus at baseline, phenotypic sensitivity to zidovudine was restored by 12 weeks of treatment with lamivudine and zidovudine.
Cross-Resistance
Cross-resistance has been observed among NRTIs. TAM substitutions are selected by zidovudine and confer cross-resistance to abacavir, didanosine, stavudine, and tenofovir.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Zidovudine was administered orally at 3 dosage levels to separate groups of mice and rats (60 females and 60 males in each group). Initial single daily doses were 30, 60, and 120 mg per kg per day in mice and 80, 220, and 600 mg per kg per day in rats. The doses in mice were reduced to 20, 30, and 40 mg per kg per day after Day 90 because of treatment-related anemia, whereas in rats only the high dose was reduced to 450 mg per kg per day on Day 91 and then to 300 mg per kg per day on Day 279.
In mice, 7 late-appearing (after 19 months) vaginal neoplasms (5 non-metastasizing squamous cell carcinomas, 1 squamous cell papilloma, and 1 squamous polyp) occurred in animals given the highest dose. One late-appearing squamous cell papilloma occurred in the vagina of a middle-dose animal. No vaginal tumors were found at the lowest dose.
In rats, 2 late-appearing (after 20 months), non-metastasizing vaginal squamous cell carcinomas occurred in animals given the highest dose. No vaginal tumors occurred at the low or middle dose in rats. No other drug-related tumors were observed in either sex of either species.
At doses that produced tumors in mice and rats, the estimated drug exposure (as measured by AUC) was approximately 3 times (mouse) and 24 times (rat) the estimated human exposure at the recommended therapeutic dose of 100 mg every 4 hours.
It is not known how predictive the results of rodent carcinogenicity studies may be for humans.
Two transplacental carcinogenicity studies were conducted in mice. One study administered zidovudine at doses of 20 mg per kg per day or 40 mg per kg per day from gestation Day 10 through parturition and lactation with dosing continuing in offspring for 24 months postnatally. The doses of zidovudine administered in this study produced zidovudine exposures approximately 3 times the estimated human exposure at recommended doses. After 24 months, an increase in incidence of vaginal tumors was noted with no increase in tumors in the liver or lung or any other organ in either gender. These findings are consistent with results of the standard oral carcinogenicity study in mice, as described earlier. A second study administered zidovudine at maximum tolerated doses of 12.5 mg per day or 25 mg per day (approximately 1,000 mg per kg nonpregnant body weight or approximately 450 mg per kg of term body weight) to pregnant mice from Days 12 through 18 of gestation. There was an increase in the number of tumors in the lung, liver, and female reproductive tracts in the offspring of mice receiving the higher dose level of zidovudine.
Mutagenesis
Zidovudine was mutagenic in a 5178Y/TK+/- mouse lymphoma assay, positive in an in vitro cell transformation assay, clastogenic in a cytogenetic assay using cultured human lymphocytes, and positive in mouse and rat micronucleus tests after repeated doses. It was negative in a cytogenetic study in rats given a single dose.
Impairment of Fertility
Zidovudine, administered to male and female rats at doses up to 450 mg per kg per day, which is 7 times the recommended adult dose (300 mg twice daily) based on body surface area, had no effect on fertility based on conception rates.
-
14 CLINICAL STUDIES
Therapy with zidovudine has been shown to prolong survival and decrease the incidence of opportunistic infections in patients with advanced HIV-1 disease and to delay disease progression in asymptomatic HIV-1-infected patients.
14.1 Adults
Zidovudine in combination with other antiretroviral agents has been shown to be superior to monotherapy for one or more of the following endpoints: delaying death, delaying development of AIDS, increasing CD4+ cell counts, and decreasing plasma HIV-1 RNA.
The clinical efficacy of a combination regimen that includes zidovudine was demonstrated in trial ACTG 320. This trial was a multi-center, randomized, double-blind, placebo-controlled trial that compared zidovudine 600 mg per day plus EPIVIR 300 mg per day with zidovudine plus EPIVIR plus indinavir 800 mg three times daily. The incidence of AIDS-defining events or death was lower in the triple-drug–containing arm compared with the 2-drug–containing arm (6.1% versus 10.9%, respectively).
Monotherapy
In controlled trials of treatment-naive subjects conducted between 1986 and 1989, monotherapy with zidovudine, as compared with placebo, reduced the risk of HIV-1 disease progression, as assessed using endpoints that included the occurrence of HIV-1-related illnesses, AIDS-defining events, or death. These trials enrolled subjects with advanced disease (BW 002), and asymptomatic or mildly symptomatic disease in subjects with CD4+ cell counts between 200 and 500 cells per mm3 (ACTG 016 and ACTG 019). A survival benefit for monotherapy with zidovudine was not demonstrated in the latter 2 trials. Subsequent trials showed that the clinical benefit of monotherapy with zidovudine was time limited.
14.2 Pediatric Patients
ACTG 300 was a multi-center, randomized, double-blind trial that provided for comparison of EPIVIR plus zidovudine to didanosine monotherapy. A total of 471 symptomatic, HIV-1-infected therapy-naive pediatric subjects were enrolled in these 2 treatment arms. The median age was 2.7 years (range: 6 weeks to 14 years), the mean baseline CD4+ cell count was 868 cells per mm3, and the mean baseline plasma HIV-1 RNA was 5.0 log10 copies per mL. The median duration that subjects remained on trial was approximately 10 months. Results are summarized in Table 11.
Table 11. Number of Subjects (%) Reaching a Primary Clinical Endpoint (Disease Progression or Death) Endpoint
EPIVIR plus Zidovudine
Didanosine
(n = 236)
(n = 235)
HIV disease progression or death (total)
15 (6.4%)
37 (15.7%)
Physical growth failure
7 (3.0%)
6 (2.6%)
Central nervous system deterioration
4 (1.7%)
12 (5.1%)
CDC Clinical Category C
2 (0.8%)
8 (3.4%)
Death
2 (0.8%)
11 (4.7%)
14.3 Prevention of Maternal-Fetal HIV-1 Transmission
The utility of zidovudine for the prevention of maternal-fetal HIV-1 transmission was demonstrated in a randomized, double-blind, placebo-controlled trial (ACTG 076) conducted in HIV-1-infected pregnant women with CD4+ cell counts of 200 to 1,818 cells per mm3 (median in the treated group: 560 cells per mm3) who had little or no previous exposure to zidovudine. Oral zidovudine was initiated between 14 and 34 weeks of gestation (median 11 weeks of therapy) followed by IV administration of zidovudine during labor and delivery. Following birth, neonates received zidovudine oral solution for 6 weeks. The trial showed a statistically significant difference in the incidence of HIV-1 infection in the neonates (based on viral culture from peripheral blood) between the group receiving zidovudine and the group receiving placebo. Of 363 neonates evaluated in the trial, the estimated risk of HIV-1 infection was 7.8% in the group receiving zidovudine and 24.9% in the placebo group, a relative reduction in transmission risk of 68.7%. Zidovudine was well tolerated by mothers and infants. There was no difference in pregnancy-related adverse events between the treatment groups.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Zidovudine Syrup (Zidovudine oral solution USP) (colorless to pale yellow strawberry flavored clear solution) containing 50mg of Zidovudine in each teaspoon (5mL) in plastic bottles of 240 mL [NDC no. 53104-0105-9].
Store at 20° to 25°C (68° to 77 °F). (see USP Controlled Room Temperature).
Preserve in tight, light-resistant container.
-
17 PATIENT COUNSELING INFORMATION
Inform patients that potentially life-threatening hypersensitivity reactions (e.g., anaphylaxis, Stevens-Johnson syndrome) can occur while receiving zidovudine. Instruct patients to immediately contact their healthcare provider if they develop rash, as it may be a sign of a more serious reaction. Advise patients that it is very important that they remain under a healthcare provider's care during treatment with zidovudine [see Contraindications (4)].
Neutropenia and Anemia
Inform patients that the major toxicities of zidovudine are neutropenia and/or anemia. The frequency and severity of these toxicities are greater in patients with more advanced disease and in those who initiate therapy later in the course of their infection. Advise patients that if toxicity develops, they may require transfusions or drug discontinuation. Advise patients of the extreme importance of having their blood counts followed closely while on therapy, especially for patients with advanced symptomatic HIV-1 disease [see Boxed Warning, Warnings and Precautions (5.1)].
Myopathy
Inform patients that myopathy and myositis with pathological changes, similar to that produced by HIV-1 disease, have been associated with prolonged use of zidovudine [see Boxed Warning, Warnings and Precautions (5.3)].
Lactic Acidosis/Hepatomegaly with Steatosis
Advise patients that lactic acidosis and severe hepatomegaly with steatosis have been reported with use of nucleoside analogues and other antiretrovirals. Advise patients to stop taking zidovudine if they develop clinical symptoms suggestive of lactic acidosis or pronounced hepatotoxicity [see Boxed Warning, Warnings and Precautions (5.4)].
HIV-1/HCV Co-infection
Inform patients with HIV-1/HCV co-infection that hepatic decompensation (some fatal) has occurred in HIV-1/HCV co-infected patients receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin [see Warnings and Precautions (5.5)].
Immune Reconstitution Syndrome
Advise patients to inform their healthcare provider immediately of any signs and symptoms of infection as inflammation from previous infection may occur soon after combination antiretroviral therapy, including when zidovudine is started [see Warnings and Precautions (5.6)].
Lipoatrophy
Advise patients that loss of subcutaneous fat may occur in patients receiving zidovudine and that they will be regularly assessed during therapy [see Warnings and Precautions (5.7)].
Common Adverse Reactions
Inform patients that the most commonly reported adverse reactions in adult patients being treated with zidovudine were headache, malaise, nausea, anorexia, and vomiting. The most commonly reported adverse reactions in pediatric patients receiving zidovudine were fever, cough, and digestive disorders. Patients also should be encouraged to contact their physician if they experience muscle weakness, shortness of breath, symptoms of hepatitis or pancreatitis, or any other unexpected adverse events while being treated with zidovudine [see Adverse Reactions (6)].
Drug Interactions
Advise patients that other medications may interact with zidovudine and certain medications, including ganciclovir, interferon alfa, and ribavirin, may exacerbate the toxicity of zidovudine [see Drug Interactions (7)].
Dosage and Administration in Neonates
Due to the small volume of zidovudine administered to neonates, advise caregivers to use an appropriate-sized syringe with 0.1-mL graduation to ensure accurate dosing of the syrup formulation [see Dosage and Administration (2.3)].
Pregnancy
Inform pregnant women considering the use of zidovudine during pregnancy for prevention of HIV-1 transmission to their infants that transmission may still occur in some cases despite therapy.
Pregnancy Registry
Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to zidovudine during pregnancy [see Use in Specific Populations (8.1)].
Lactation
Instruct women with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in the breast milk [see Use in Specific Populations (8.2)].
Missed Dose
Instruct patients that if they miss a dose of zidovudine, to take it as soon as they remember. Advise patients not to double their next dose or take more than the prescribed dose [see Dosage and Administration (2)].
Disclaimer: Other brands listed are the registered trademarks of their respective owners and are not trademarks of Cipla Limited.
Rev. 11/2018
Mfd. by CIPLA LTD.
Indore SEZ.
Pithampur (M.P.) 454 775
INDIA
-
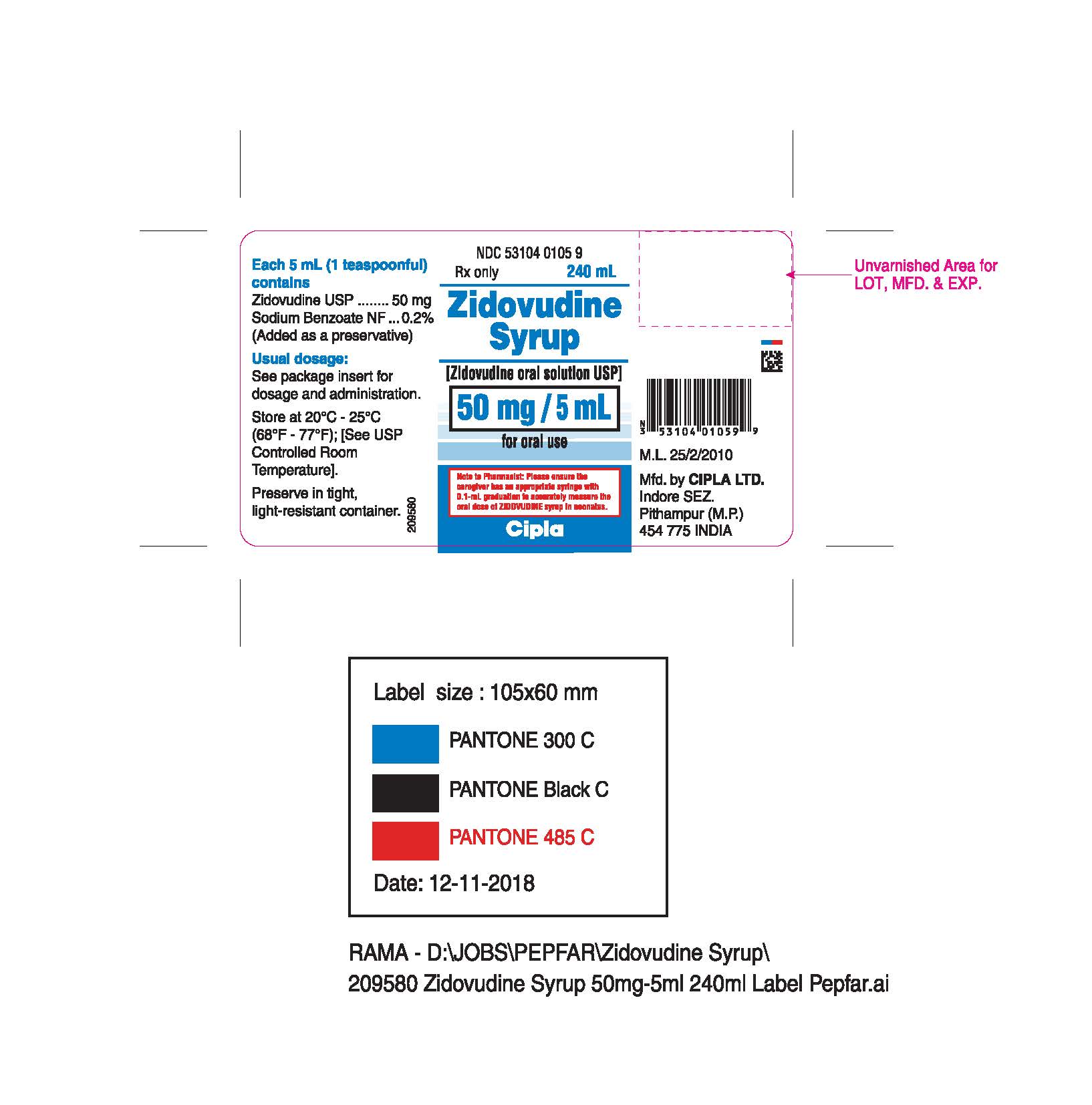
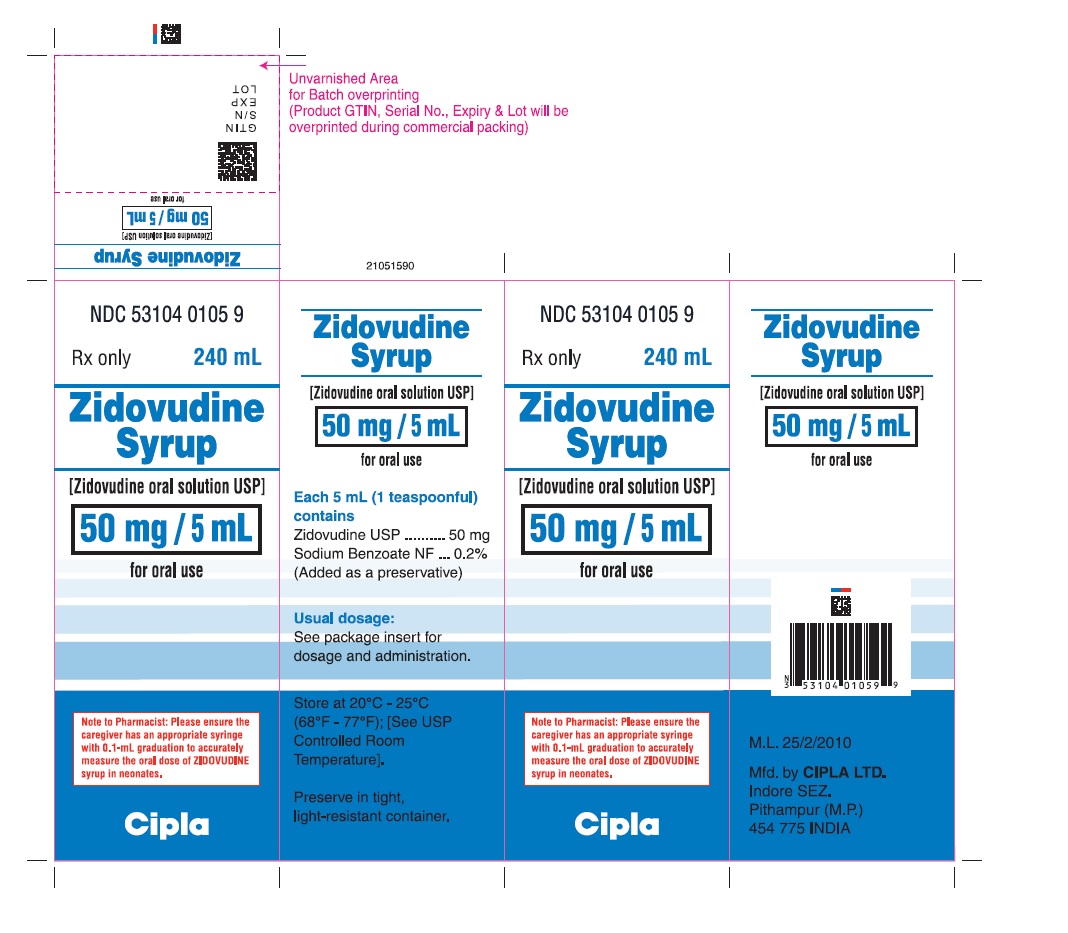
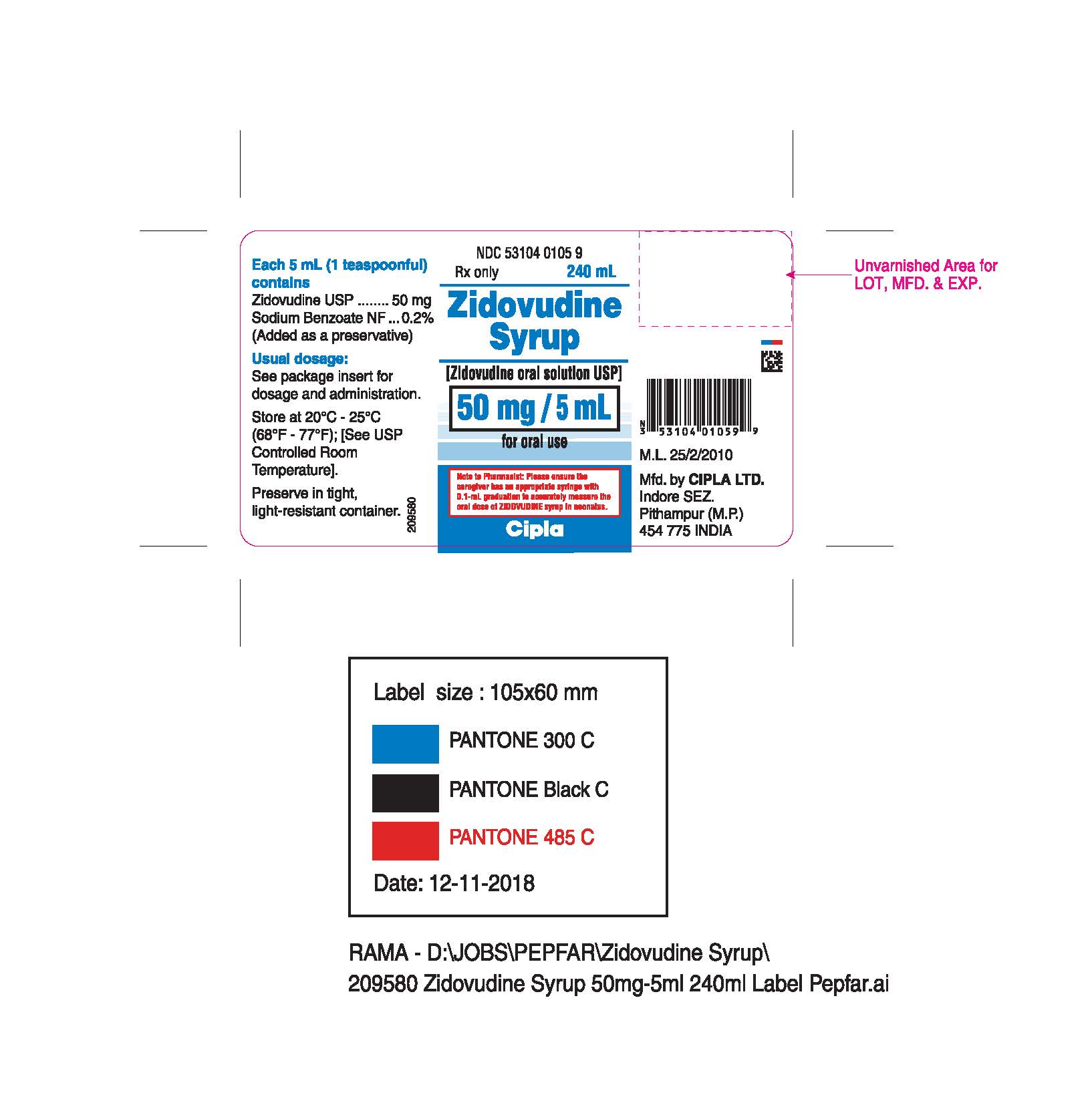
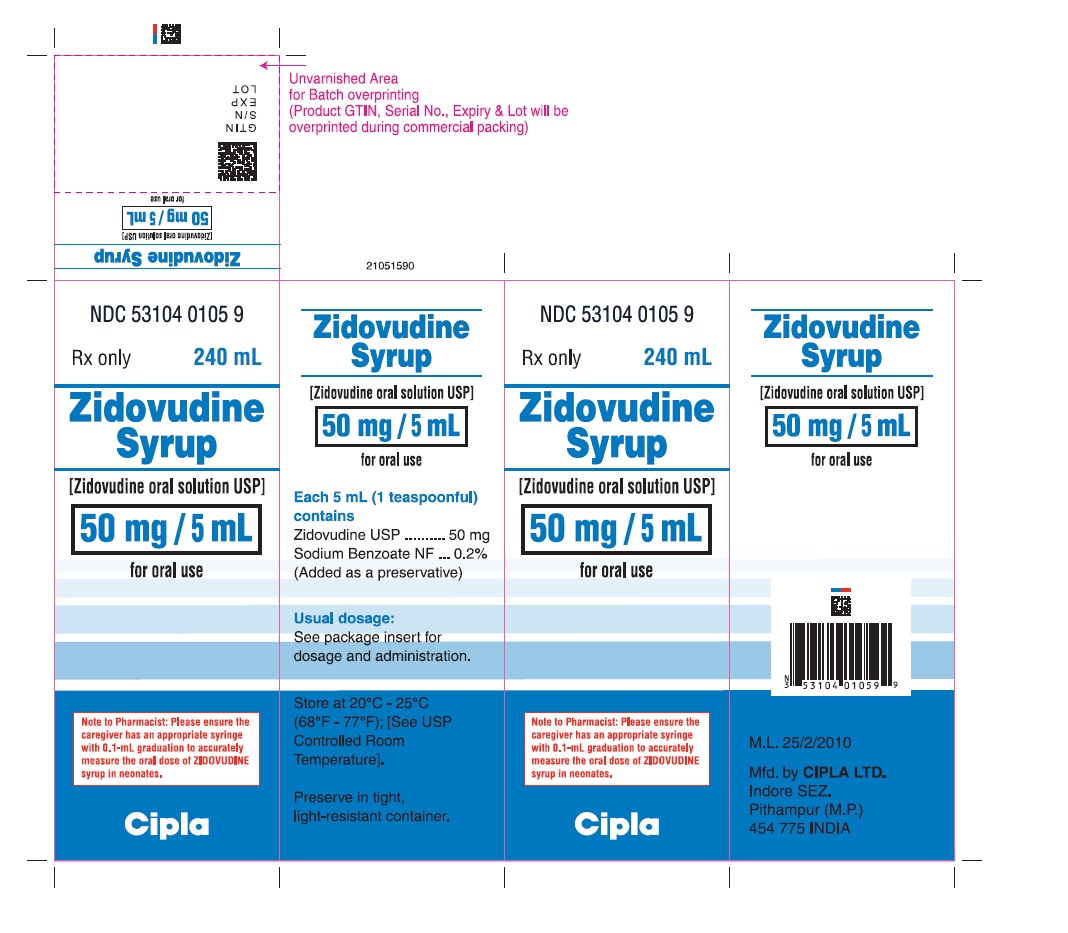
PRINCIPAL DISPLAY PANEL
Zidovudine Syrup (Zidovudine Oral Solution USP) 50mg/5ml for oral use
Rx Only
240 mL
Each 5mL (1 teaspoonful) contains
Zidovudine USP 50mg
Sodium Benzoate NF 0.2% [Added as a preservative]
See prescribing information for dosage information.
Store at 20°C to 25°C (68° to 77°F) [See USP Controlled Room Temperature]
Preserve in tight, light-resistant container.
Cipla Limited
India.
Revised: 11/2018.
-
INGREDIENTS AND APPEARANCE
ZIDOVUDINE
zidovudine syrupProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:53104-0105 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ZIDOVUDINE (UNII: 4B9XT59T7S) (ZIDOVUDINE - UNII:4B9XT59T7S) ZIDOVUDINE 50 mg in 5 mL Inactive Ingredients Ingredient Name Strength SODIUM BENZOATE (UNII: OJ245FE5EU) GLYCERIN (UNII: PDC6A3C0OX) SUCROSE (UNII: C151H8M554) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) Product Characteristics Color YELLOW (colorless to pale yellow) Score Shape Size Flavor STRAWBERRY (strawberry) Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:53104-0105-9 240 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077981 06/26/2008 Labeler - Cipla Ltd. (650138746) Registrant - Cipla Ltd. (650138746) Establishment Name Address ID/FEI Business Operations Cipla Limited- Indore 918596409 ANALYSIS(53104-0105) , MANUFACTURE(53104-0105) , LABEL(53104-0105) , PACK(53104-0105)