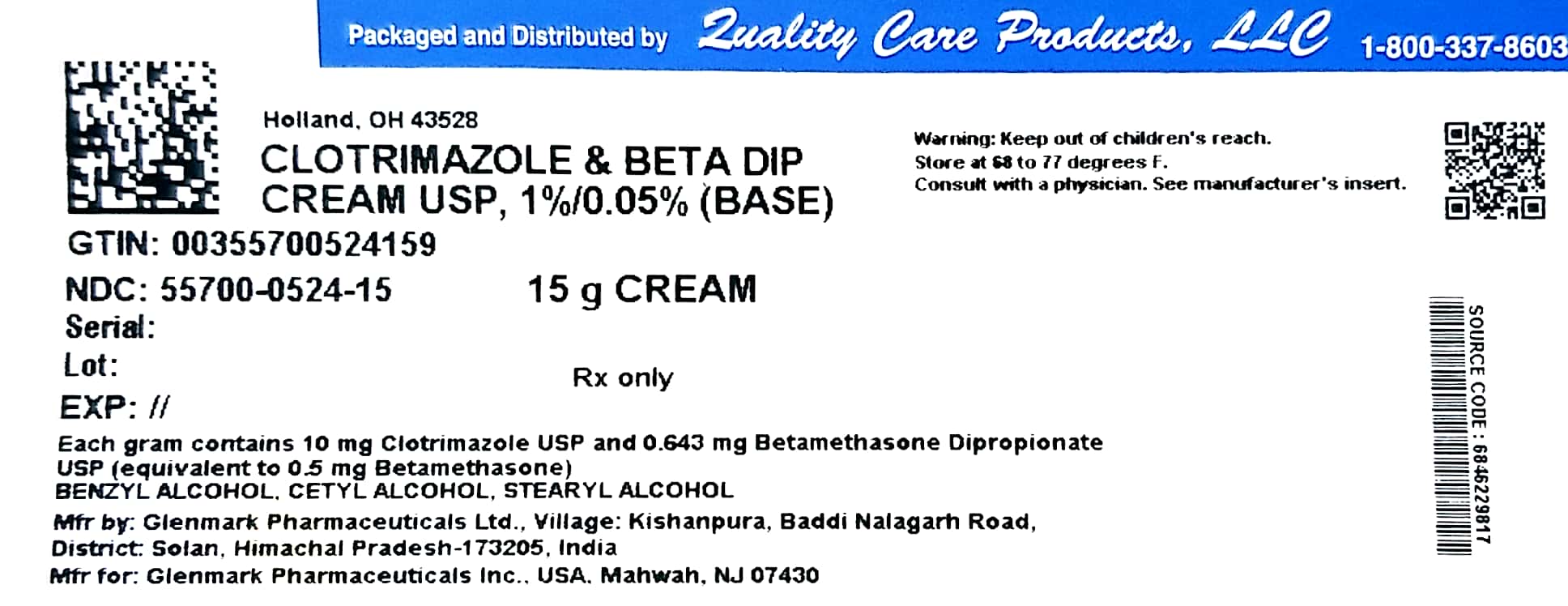
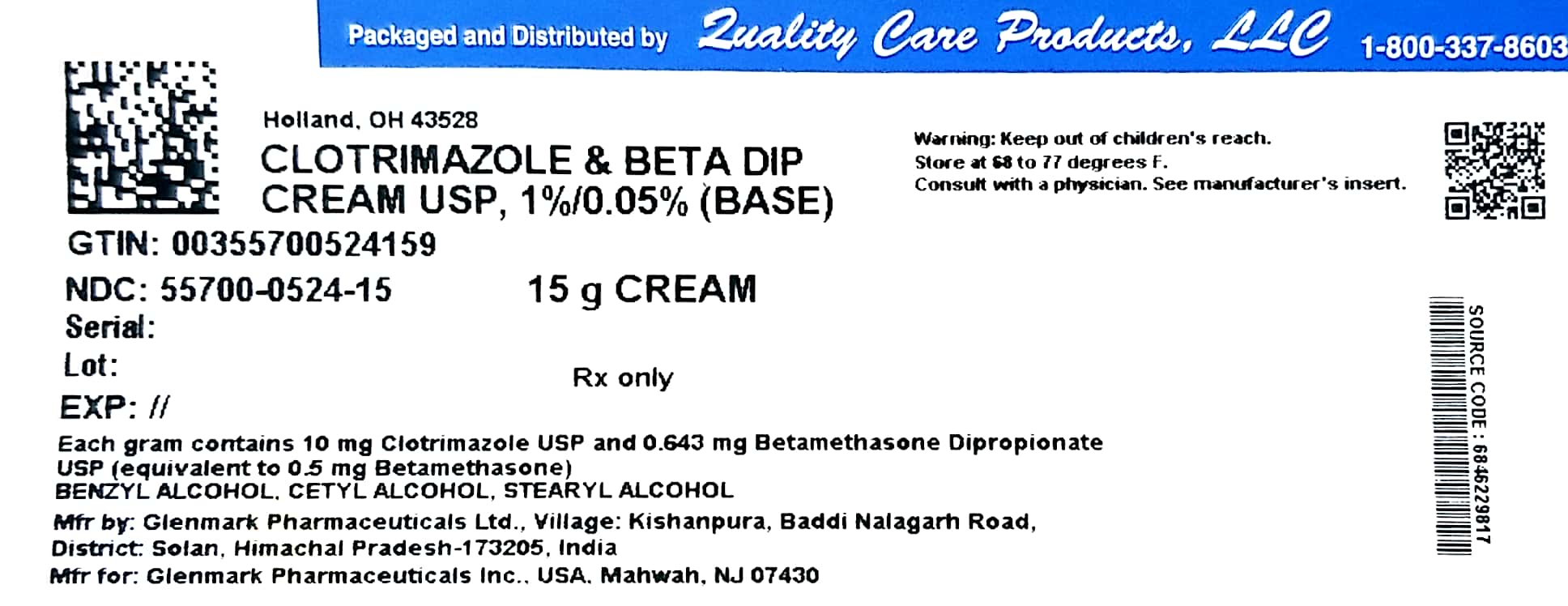
Label: CLOTRIMAZOLE AND BETAMETHASONE DIPROPIONATE cream
- NDC Code(s): 55700-524-15
- Packager: Lake Erie Medical DBA Quality Care Products LLC
- This is a repackaged label.
- Source NDC Code(s): 68462-298
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated February 21, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use clotrimazole and betamethasone dipropionate cream safely and effectively. See full prescribing information for clotrimazole and betamethasone dipropionate cream.
CLOTRIMAZOLE AND BETAMETHASONE DIPROPIONATE Cream USP, 1%/0.05% (base), for topical use
Initial U.S. Approval: 1984INDICATIONS AND USAGE
Clotrimazole and betamethasone dipropionate cream USP contains a combination of clotrimazole USP, an azole antifungal, and betamethasone dipropionate USP, a corticosteroid, and is indicated for the topical treatment of symptomatic inflammatory tinea pedis, tinea cruris, and tinea corporis due to Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum in patients 17 years and older. (1)
DOSAGE AND ADMINISTRATION
• Tinea pedis: Apply a thin film to the affected skin areas twice a day for 2 weeks. (2)
• Tinea cruris and tinea corporis: Apply a thin film to the affected skin area twice a day for 1 week. (2)
• Clotrimazole and betamethasone dipropionate cream should not be used longer than 2 weeks in the treatment of tinea corporis or tinea cruris, and longer than 4 weeks in the treatment of tinea pedis. (2)
• Do not use with occlusive dressings unless directed by a physician. (2)
• Not for ophthalmic, oral or intravaginal use. (2)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
• Clotrimazole and betamethasone dipropionate cream can cause reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency during and after withdrawal of the treatment. Risk factor(s) are: use of high-potency topical corticosteroid, use over a large surface area or to areas under occlusion, prolonged use, altered skin barrier, liver failure, and young age. Modify use should HPA axis suppression develop. (5.1, 8.4)
• Pediatric patients may be more susceptible to systemic toxicity. (5.1, 8.4)
• The use of clotrimazole and betamethasone dipropionate cream in the treatment of diaper dermatitis is not recommended. (5.2)
ADVERSE REACTIONS
Most common adverse reactions reported for clotrimazole and betamethasone dipropionate cream were paraesthesia in 1.9% of patients and rash, edema, and secondary infections each in less than 1% of patients. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Glenmark Pharmaceuticals Inc., USA at 1-888-721-7115 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Revised: 6/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Endocrine System
5.2 Diaper Dermatitis
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Clotrimazole and betamethasone dipropionate cream USP is a combination of an azole antifungal and corticosteroid and is indicated for the topical treatment of symptomatic inflammatory tinea pedis, tinea cruris, and tinea corporis due to Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum in patients 17 years and older.
-
2 DOSAGE AND ADMINISTRATION
Treatment of tinea corporis or tinea cruris:
- •
- Apply a thin film of clotrimazole and betamethasone dipropionate cream into the affected skin areas twice a day for one week.
- •
- Do not use more than 45 grams per week. Do not use with occlusive dressings.
- •
- If a patient shows no clinical improvement after 1 week of treatment with clotrimazole and betamethasone dipropionate cream, the diagnosis should be reviewed.
- •
- Do not use longer than 2 weeks.
Treatment of tinea pedis:
- •
- Gently massage a sufficient amount of clotrimazole and betamethasone dipropionate cream into the affected skin areas twice a day for two weeks.
- •
- Do not use more than 45 grams per week. Do not use with occlusive dressings.
- •
- If a patient shows no clinical improvement after 2 weeks of treatment with clotrimazole and betamethasone dipropionate cream, the diagnosis should be reviewed.
- •
- Do not use longer than 4 weeks.
Clotrimazole and betamethasone dipropionate cream is for topical use only. It is not for oral, ophthalmic, or intravaginal use.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Effects on Endocrine System
Clotrimazole and betamethasone dipropionate cream can cause reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency. This may occur during treatment or after withdrawal of treatment. Cushing’s syndrome and hyperglycemia may also occur due to the systemic effect of corticosteroids while on treatment. Factors that predispose a patient to HPA axis suppression include the use of high-potency steroids, large treatment surface areas, prolonged use, use of occlusive dressing, altered skin barrier, liver failure, and young age.
Because of the potential for systemic corticosteroid effects, patients may need to be periodically evaluated for HPA axis suppression. This may be done by using the adrenocorticotropic hormone (ACTH) stimulation test.
In a small trial, clotrimazole and betamethasone dipropionate cream was applied using large dosages, 7 g daily for 14 days (BID) to the crural area of normal adult subjects. Three of the 8 normal subjects on whom clotrimazole and betamethasone dipropionate cream was applied exhibited low morning plasma cortisol levels during treatment. One of these subjects had an abnormal cosyntropin test. The effect on morning plasma cortisol was transient and subjects recovered 1 week after discontinuing dosing. In addition, 2 separate trials in pediatric subjects demonstrated adrenal suppression as determined by cosyntropin testing [see Use in Specific Populations (8.4)].
If HPA axis suppression is documented, gradually withdraw the drug, reduce the frequency of application, or substitute with a less potent corticosteroid.
Pediatric patients may be more susceptible to systemic toxicity due to their larger skin-surface-to-body mass ratios [see Use in Specific Populations (8.4)].
-
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials common adverse reaction reported for clotrimazole and betamethasone dipropionate cream was paresthesia in 1.9% of patients. Adverse reactions reported at a frequency < 1% included rash, edema, and secondary infection.
6.2 Postmarketing Experience
Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following local adverse reactions have been reported with topical corticosteroids: itching, irritation, dryness, folliculitis, hypertrichosis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, maceration of the skin, skin atrophy, striae, miliaria, capillary fragility (ecchymoses), telangiectasia, and sensitization (local reactions upon repeated application of product).
Adverse reactions reported with the use of clotrimazole are: erythema, stinging, blistering, peeling, edema, pruritus, urticaria, and general irritation of the skin.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic effects,
Pregnancy Category CThere are no adequate and well-controlled studies with clotrimazole and betamethasone dipropionate cream in pregnant women. Therefore, clotrimazole and betamethasone dipropionate cream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
There have been no teratogenic studies performed in animals or humans with the combination of clotrimazole and betamethasone dipropionate. Corticosteroids are generally teratogenic in laboratory animals when administered at relatively low dosage levels.
Studies in pregnant rats with intravaginal doses up to 100 mg/kg (15 times the maximum human dose) revealed no evidence of fetotoxicity due to clotrimazole exposure.
No increase in fetal malformations was noted in pregnant rats receiving oral (gastric tube) clotrimazole doses up to 100 mg/kg/day during gestation Days 6 to 15. However, clotrimazole dosed at 100 mg/kg/day was embryotoxic (increased resorptions), fetotoxic (reduced fetal weights), and maternally toxic (reduced body weight gain) to rats. Clotrimazole dosed at 200 mg/kg/day (30 times the maximum human dose) was maternally lethal, and therefore, fetuses were not evaluated in this group. Also in this study, doses up to 50 mg/kg/day (8 times the maximum human dose) had no adverse effects on dams or fetuses. However, in the combined fertility, teratogenicity, and postnatal development study described above, 50 mg/kg clotrimazole was associated with reduced maternal weight gain and reduced numbers of offspring reared to 4 weeks.
Oral clotrimazole doses of 25, 50, 100, and 200 mg/kg/day (2-15 times the maximum human dose) were not teratogenic in mice. No evidence of maternal toxicity or embryotoxicity was seen in pregnant rabbits dosed orally with 60, 120, or 180 mg/kg/day (18-55 times the maximum human dose).
Betamethasone dipropionate has been shown to be teratogenic in rabbits when given by the intramuscular route at doses of 0.05 mg/kg. This dose is approximately one-fifth the maximum human dose. The abnormalities observed included umbilical hernias, cephalocele, and cleft palates.
Betamethasone dipropionate has not been tested for teratogenic potential by the dermal route of administration. Some corticosteroids have been shown to be teratogenic after dermal application to laboratory animals.
8.3 Nursing Mothers
Systemically administered corticosteroids appear in human milk and can suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids can result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when clotrimazole and betamethasone dipropionate cream is administered to a nursing woman.
8.4 Pediatric Use
The use of clotrimazole and betamethasone dipropionate cream in patients under 17 years of age is not recommended.
Adverse events consistent with corticosteroid use have been observed in pediatric patients treated with clotrimazole and betamethasone dipropionate cream. In open-label trials, 17 of 43 (39.5%) evaluable pediatric subjects (aged 12-16 years old) using clotrimazole and betamethasone dipropionate cream for treatment of tinea pedis demonstrated adrenal suppression as determined by cosyntropin testing. In another open-label trial, 8 of 17 (47.1%) evaluable pediatric subjects (aged 12-16 years old) using clotrimazole and betamethasone dipropionate cream for treatment of tinea cruris demonstrated adrenal suppression as determined by cosyntropin testing.
Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA axis suppression when they are treated with topical corticosteroids. They are, therefore also at greater risk of adrenal insufficiency during and/or after withdrawal of treatment. Pediatric patients may be more susceptible than adults to skin atrophy, including striae, when they are treated with topical corticosteroids.
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in pediatric patients receiving topical corticosteroids [see Warnings and Precautions (5.1)].
Avoid use of clotrimazole and betamethasone dipropionate cream in the treatment of diaper dermatitis.
8.5 Geriatric Use
Clinical studies of clotrimazole and betamethasone dipropionate cream did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. However, greater sensitivity of some older individuals cannot be ruled out. The use of clotrimazole and betamethasone dipropionate cream under occlusion, such as in diaper dermatitis, is not recommended.
Postmarket adverse event reporting for clotrimazole and betamethasone dipropionate cream in patients aged 65 and above includes reports of skin atrophy and rare reports of skin ulceration. Caution should be exercised with the use of these corticosteroid-containing topical products on thinning skin.
-
11 DESCRIPTION
Clotrimazole and betamethasone dipropionate cream USP, 1%/0.05% (base), contains combinations of clotrimazole USP, an azole antifungal, and betamethasone dipropionate USP, a corticosteroid, for topical use.
Chemically, clotrimazole USP is 1-[(2-Chlorophenyl)diphenylmethyl]-1H-imidazole, with the empirical formula C22H17ClN2, a molecular weight of 344.84, and the following structural formula:
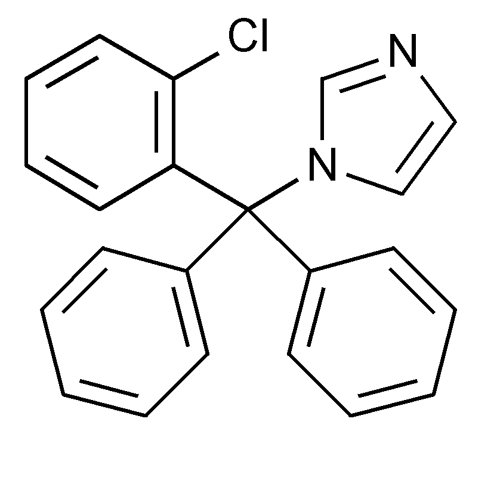
Clotrimazole USP is a white to pale yellow, crystalline powder, odorless, practically insoluble in water, freely soluble in methanol, in acetone, in chloroform, and in alcohol.
Betamethasone dipropionate USP has the chemical name 9-fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 17,21-dipropionate, with the empirical formula C28H37FO7, a molecular weight of 504.59, and the following structural formula:
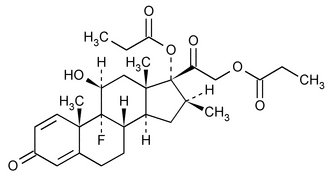
Betamethasone dipropionate USP is a white to almost white crystalline powder, practically insoluble in water, freely soluble in acetone and in methylene chloride, sparingly soluble in alcohol.
Each gram of clotrimazole and betamethasone dipropionate cream USP, 1%/0.05% (base) contains 10 mg of clotrimazole USP and 0.643 mg of betamethasone dipropionate USP (equivalent to 0.5 mg of betamethasone), in a white to off-white, hydrophilic cream consisting of benzyl alcohol, cetyl alcohol plus stearyl alcohol, ceteareth-30, mineral oil, monobasic sodium phosphate monohydrate, phosphoric acid, propylene glycol, sodium hydroxide, white petrolatum and purified water.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Clotrimazole is an azole antifungal [see Clinical Pharmacology (12.4)].
Betamethasone dipropionate is a corticosteroid. Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action for the treatment of tinea pedis, tinea cruris and tinea corporis is unknown.
12.2 Pharmacodynamics
Vasoconstrictor Assay:
Studies performed with clotrimazole and betamethasone dipropionate cream indicate that these topical combination antifungal/corticosteroids may have vasoconstrictor potencies in a range that is comparable to high-potency topical corticosteroids. However, similar blanching scores do not necessarily imply therapeutic equivalence.12.3 Pharmacokinetics
Skin penetration and systemic absorption of clotrimazole and betamethasone dipropionate following topical application of clotrimazole and betamethasone dipropionate cream has not been studied.
The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin may increase percutaneous absorption of topical corticosteroids. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids [see Dosage and Administration (2)].
Once absorbed through the skin, the pharmacokinetics of topical corticosteroids are similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted into the bile.
12.4 Microbiology
Mechanism of Action:
Clotrimazole, an azole antifungal agent, inhibits 14-α-demethylation of lanosterol in fungi by binding to one of the cytochrome P-450 enzymes. This leads to the accumulation of 14-α-methylsterols and reduced concentrations of ergosterol, a sterol essential for a normal fungal cytoplasmic membrane. The methylsterols may affect the electron transport system, thereby inhibiting growth of fungi.Activity In Vitro and In Vivo:
Clotrimazole has been shown to be active against most strains of the following dermatophytes, both in vitro and in clinical infections, Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton rubrum [see Indications and Usage (1)].Drug Resistance:
Strains of dermatophytes having a natural resistance to clotrimazole have not been reported. Resistance to azoles, including clotrimazole, has been reported in some Candida species.No single-step or multiple-step resistance to clotrimazole has developed during successive passages of Trichophyton mentagrophytes.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
There are no adequate laboratory animal studies with either the combination of clotrimazole and betamethasone dipropionate or with either component individually to evaluate carcinogenesis.
Betamethasone was negative in the bacterial mutagenicity assay (Salmonella typhimurium and Escherichia coli) and in the mammalian cell mutagenicity assay (CHO/HGPRT). It was positive in the in vitro human lymphocyte chromosome aberration assay, and equivocal in the in vivo mouse bone marrow micronucleus assay.
Reproductive studies with betamethasone dipropionate carried out in rabbits at doses of 1.0 mg/kg by the intramuscular route and in mice up to 33 mg/kg by the intramuscular route indicated no impairment of fertility except for dose-related increases in fetal resorption rates in both species. These doses are approximately 5- and 38-fold the maximum human dose based on body surface areas, respectively.
In a combined study of the effects of clotrimazole on fertility, teratogenicity, and postnatal development, male and female rats were dosed orally (diet admixture) with levels of 5, 10, 25, or 50 mg/kg/day (approximately 1-8 times the maximum dose in a 60-kg adult based on body surface area) from 10 weeks prior to mating until 4 weeks postpartum. No adverse effects on the duration of estrous cycle, fertility, or duration of pregnancy were noted.
-
14 CLINICAL STUDIES
In clinical trials of tinea corporis, tinea cruris, and tinea pedis, subjects treated with clotrimazole and betamethasone dipropionate cream showed a better clinical response at the first return visit than subjects treated with clotrimazole cream. In tinea corporis and tinea cruris, the subject returned 3 to 5 days after starting treatment, and in tinea pedis, after 1 week. Mycological cure rates observed in subjects treated with clotrimazole and betamethasone dipropionate cream were as good as, or better than, in those subjects treated with clotrimazole cream. In these same clinical studies, patients treated with clotrimazole and betamethasone dipropionate cream showed better clinical responses and mycological cure rates when compared with subjects treated with betamethasone dipropionate cream.

- 16 HOW SUPPLIED/STORAGE AND HANDLING
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
CLOTRIMAZOLE AND BETAMETHASONE DIPROPIONATE
clotrimazole and betamethasone dipropionate creamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55700-524(NDC:68462-298) Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOTRIMAZOLE (UNII: G07GZ97H65) (CLOTRIMAZOLE - UNII:G07GZ97H65) CLOTRIMAZOLE 10 mg in 1 g BETAMETHASONE DIPROPIONATE (UNII: 826Y60901U) (BETAMETHASONE - UNII:9842X06Q6M) BETAMETHASONE 0.5 mg in 1 g Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) CETOSTEARYL ALCOHOL (UNII: 2DMT128M1S) CETEARETH-30 (UNII: 1R9DCZ5FOX) MINERAL OIL (UNII: T5L8T28FGP) SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) PHOSPHORIC ACID (UNII: E4GA8884NN) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM HYDROXIDE (UNII: 55X04QC32I) PETROLATUM (UNII: 4T6H12BN9U) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55700-524-15 15 g in 1 TUBE; Type 0: Not a Combination Product 06/01/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202894 11/06/2015 Labeler - Lake Erie Medical DBA Quality Care Products LLC (831276758) Establishment Name Address ID/FEI Business Operations Lake Erie Medical DBA Quality Care Products LLC 831276758 relabel(55700-524)