Label: FIBRYGA (fibrinogen- human powder, for solution
- NDC Code(s): 68982-349-01, 68982-349-81
- Packager: Octapharma USA Inc
- Category: PLASMA DERIVATIVE
- DEA Schedule: None
- Marketing Status: Biologic Licensing Application
Drug Label Information
Updated November 28, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FIBRYGA safely and effectively. See full prescribing information for FIBRYGA.
FIBRYGA® [fibrinogen (human)]
Lyophilized Powder for Reconstitution, For Intravenous Use
Initial U.S. Approval: 2017RECENT MAJOR CHANGES
INDICATIONS AND USAGE
FIBRYGA is a human fibrinogen concentrate indicated for:
• fibrinogen supplementation in bleeding patients with acquired fibrinogen deficiency
• treatment of acute bleeding episodes in patients with congenital fibrinogen deficiency, including afibrinogenemia and hypofibrinogenemia ( 1 ).
• Limitation of Use:
• FIBRYGA is not indicated for dysfibrinogenemia ( 1 ).
DOSAGE AND ADMINISTRATION
For intravenous use after reconstitution only. ( 2 )
Acquired Fibrinogen Deficiency
• Recommended dose ( 2.1 )
• For adults: 4g
• For adolescents age ≥ 12 years: 50 mg/kg body weight
• For children age <12 years: 70 mg/kg body weight
• Administer additional doses as needed to bleeding patients when plasma fibrinogen level is ≤200 mg/dL or thromboelastometry FIBTEM A10 is ≤10 mm (or equivalent values generated by other viscoelastic testing methods) ( 2.1 ).
• Dosing may be adjusted depending on plasma fibrinogen levels or viscoelastic testing, severity of bleeding, body weight, or patient’s clinical condition ( 2.1 ).
• The injection rate should not exceed 20 mL per minute ( 2.3 ).
• Monitoring of patient’s plasma fibrinogen level or the viscoelastic properties of the fibrin-based clot is recommended during treatment ( 2.1 ).
Congenital Fibrinogen Deficiency
• Dose when plasma fibrinogen level is known ( 2.1 ):
Adults and adolescents 12 years of age and above:
Dose (mg/kg body weight) =
[Target fibrinogen level (mg/dL) - measured fibrinogen level (mg/dL)]
1.8 (mg/dL per mg/kg body weight)
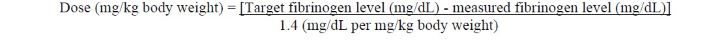
Children <12 years of age:
Dose (mg/kg body weight) =
[Target fibrinogen level (mg/dL) - measured fibrinogen level (mg/dL)]
1.4 (mg/dL per mg/kg body weight)
The recommended target plasma fibrinogen level is 100 mg/dL for minor bleeding and 150 mg/dL for major bleeding.
• Dose when plasma fibrinogen level is unknown: 70 mg/kg body weight ( 2.1 ).
• The injection rate should not exceed 5 mL per minute ( 2.3 ).
• Monitoring of patient’s plasma fibrinogen level is recommended during treatment.
DOSAGE FORMS AND STRENGTHS
FIBRYGA is available as a lyophilized powder in single-dose bottles containing approximately 1 g fibrinogen concentrate per bottle ( 3 ).
CONTRAINDICATIONS
Anaphylactic or severe reactions to FIBRYGA or its components (Sodium Citrate Dihydrate; Glycine; L-Arginine Hydrochloride) ( 4 ).
WARNINGS AND PRECAUTIONS
• Monitor patients for early signs of hypersensitivity or allergic reactions. If necessary, discontinue administration and institute appropriate treatment ( 5.1 ).
• Thrombotic events have been reported in patients receiving FIBRYGA. Treatment with human fibrinogen concentrate has been associated with thrombosis at target plasma fibrinogen levels that were below 150 mg/dL. The thrombotic risks may be greater when the target fibrinogen plasma level is 150 mg/dL. Weigh the benefits of administration versus the risks of thrombosis ( 5.2 ).
• FIBRYGA is made from pooled human plasma. Products made from human plasma may contain infectious agents, e.g., viruses and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent ( 5.3 ).
ADVERSE REACTIONS
• The most serious adverse reactions that may be observed with FIBRYGA are thromboembolic episodes and anaphylactic-type reactions.
• The most common adverse reactions observed in clinical studies with FIBRYGA in acquired fibrinogen deficiency (> 5% of patients) were abnormal hepatic function, acute kidney injury, anemia, atrial fibrillation, delirium and renal failure ( 6 ).
• The most common adverse reactions observed in clinical studies with FIBRYGA in congenital fibrinogen deficiency (> 5% of patients) were nausea, vomiting, pyrexia (fever), and thrombocytosis ( 6 ).
To report SUSPECTED ADVERSE REACTIONS, contact Octapharma at 1-866-766-4860 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
Pediatric: There was no difference in the pharmacokinetics of FIBRYGA between adults and adolescents (12-17 years of age). Lower recovery, shorter half-life and faster clearance were observed in children aged 1 to < 12 years; higher doses may be required in this age group in patients with acquired or congenital fibrinogen deficiency ( 8.4 ).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Acquired Fibrinogen Deficiency
1.2 Congenital Fibrinogen Deficiency
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
2.2 Preparation and Handling
2.3 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
5.2 Thrombosis
5.3 Transmissible Infectious Agents
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- SPL UNCLASSIFIED SECTION
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For intravenous use after reconstitution only.
2.1 Dosage
Acquired Fibrinogen Deficiency:
The recommended dose is as follows:
- For adults: 4g
- For adolescents age ≥ 12 years: 50 mg/kg body weight
- For children age <12 years: 70 mg/kg body weight
Administer additional doses of 4 g in adults, 50 mg/kg body weight in adolescents 12 years of age and above, and 70 mg/kg body weight in children <12 years of age as needed to bleeding patients when plasma fibrinogen level is ≤200 mg/dL or thromboelastometry FIBTEM A10 is ≤10 mm (or equivalent values generated by other viscoelastic testing methods). Dosing may be adjusted depending on plasma fibrinogen levels or viscoelastic testing, severity of bleeding, body weight, or patient’s clinical condition.
Monitor the patient’s plasma fibrinogen level or the viscoelastic properties of the fibrin-based clot during treatment with FIBRYGA.
Congenital Fibrinogen Deficiency:
FIBRYGA dosing, duration of dosing, and frequency of administration should be individualized based on the extent of bleeding, laboratory values, and the clinical condition of the patient.
The recommended target plasma fibrinogen level is 100 mg/dL for minor bleeding and 150 mg/dL for major bleeding.
FIBRYGA dose when baseline fibrinogen level is known
Dose should be individually calculated for each patient based on the target plasma fibrinogen level for the type of bleeding, actual measured plasma fibrinogen level and body weight , using the following age-specific formulas [see Clinical pharmacology ( 12.3 )] :
Adults and adolescents 12 years of age and above:
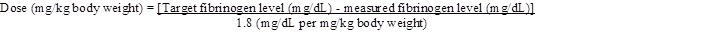
Children <12 years of age:
FIBRYGA dose when baseline fibrinogen level is not known
If the patient’s fibrinogen level is not known, the recommended dose is 70 mg/kg of body weight administered intravenously.
Monitor the patient’s fibrinogen level during treatment with FIBRYGA.
Additional infusions of FIBRYGA should be administered if the plasma fibrinogen level is below the accepted lower limit (80 mg/dL for minor bleeding, 130 mg/dL for major bleeding) of the target level until hemostasis is achieved.
2.2 Preparation and Handling
FIBRYGA package contains:
- 1 single-dose bottle of FIBRYGA concentrate
- 1 vial of diluent (sterile Water for Injection)
- 1 transfer device (Nextaro ® )
Reconstitute FIBRYGA with diluent (sterile Water for Injection).
Do not use FIBRYGA beyond the expiration date. FIBRYGA contains no preservatives. Use aseptic technique when preparing and reconstituting FIBRYGA.
The procedures below are provided as general guidelines for preparation and reconstitution of FIBRYGA.
Reconstitute FIBRYGA as follows:
1. Warm both the powder and sterile Water for Injection (sWFI) in their closed bottles to room temperature. This temperature should be maintained during reconstitution. If a water bath is used for warming, prevent water from coming into contact with the rubber stoppers or the caps of the bottles. The temperature of the water bath should not exceed +37°C (98°F).
2. Remove the flip cap from the FIBRYGA bottle and the sWFI vial and disinfect the rubber stoppers with an alcohol swab and allow to dry.
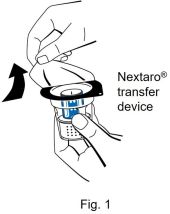
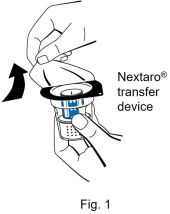
3. Open the Nextaro ® transfer device package by peeling off the lid (Fig. 1). To maintain sterility, do not remove the Nextaro ® transfer device from the blister package. Do not touch the spike.
4. Place the diluent vial on an even, clean surface and hold it firmly. Without removing the blister package, place the blue part of the transfer device on top of the diluent vial. Press straight and firmly down until it snaps into place (Fig. 2). Do not twist while attaching.
Note:
The transfer device must be attached to the diluent vial first and then to the lyophilized powder bottle. Otherwise, loss of vacuum occurs, and transfer of the diluent does not take place. If diluent is not completely transferred to the lyophilized powder bottle during this process, contact your Octapharma representative.

5. While holding onto the diluent vial, carefully remove the blister package from the Nextaro ® transfer device by pulling vertically upwards. Make sure to leave the transfer device attached firmly to the diluent vial (Fig. 3).
6. Place the FIBRYGA bottle on an even, clean surface and hold it firmly. Take the diluent vial with the attached transfer device and turn it upside down. Place the white part of the transfer device connector on top of the FIBRYGA bottle and press firmly down until it snaps into place (Fig. 4). Do not twist while attaching. The diluent will flow automatically into the FIBRYGA bottle.
7. With the diluent vial still attached, gently swirl the FIBRYGA bottle until the powder is fully dissolved. To avoid foam formation, do not shake the bottle. The powder should be dissolved completely within approx. 5 minutes. Unscrew the Nextaro ® transfer device (blue part) counterclockwise into two parts (Fig. 5). Do not touch the Luer lock connector on the white part of the transfer device.
8. Dispose of the empty diluent vial together with the blue part of the transfer device.- After reconstitution, the FIBRYGA solution should be almost colorless and slightly opalescent. Inspect the reconstituted FIBRYGA solution in the syringe for visible particulate matter and discoloration prior to administration. Do not use if particulate matter or discoloration are observed.
The powder should be reconstituted only directly before injection. After reconstitution, do not refrigerate or freeze the FIBRYGA solution. Use the reconstituted FIBRYGA solution immediately or within 4 hours after reconstitution. Discard any remaining FIBRYGA solution.
2.3 Administration
For intravenous use only after reconstitution.
Instructions for infusion:

1. Carefully attach a syringe to the Luer lock connector on the white part of the Nextaro ® transfer device (Fig. 6).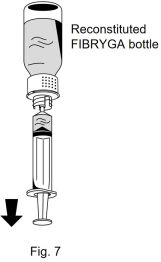
2. Turn the FIBRYGA bottle upside down and draw the solution into the syringe (Fig. 7).
3. Once the solution has been transferred, firmly hold the barrel of the syringe (keeping the syringe plunger facing down) and remove the syringe from the Nextaro ® transfer device (Fig. 8).
4. Dispose of the white part of the transfer device together with the empty FIBRYGA bottle.- Do not administer FIBRYGA in the same tubing or container as other medications.
- Use aseptic technique when administering FIBRYGA.
- Administer FIBRYGA at room temperature by slow intravenous injection at a rate not exceeding 20 mL per minute in patients with acquired fibrinogen deficiency and 5 mL per minute in patients with congenital fibrinogen deficiency.
- No blood should enter the syringe due to the risk of fibrin clot formation.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Hypersensitivity reactions may occur. If early signs of hypersensitivity reactions (including hives, generalized urticaria, tightness of the chest, wheezing, hypotension, and anaphylaxis) or symptoms of allergic reactions occur, immediately discontinue administration [see Patient Counseling Information ( 17 )] . The treatment required depends on the nature and severity of the reaction.
5.2 Thrombosis
Thrombosis may occur spontaneously in patients with acquired or congenital fibrinogen deficiency with or without the use of fibrinogen replacement therapy. Thrombotic events have been reported in patients receiving FIBRYGA.
In the FIBRES study, there were 32 patients (8.6%) in the FIBRYGA group who experienced a total of 37 thromboembolic adverse events: cerebrovascular accident (n=17 events); intestinal ischemia (n=4); deep vein thrombosis (n=3); myocardial infarction (n=3); peripheral ischemia (n=2); pulmonary embolism (n=3); transient ischemic attack (n=1); cardiac arrest (n=1); disseminated intravascular coagulation (n=1); ischemic hepatitis (n=1); and thrombophlebitis (n=1). In the cryoprecipitate group, 45 patients (12.4%) experienced a total of 50 thromboembolic adverse events: cerebrovascular accident (n =18 events); venous thrombosis (n=13); cardiac arrest (n=4); myocardial infarction (n=4); intestinal ischemia (n=3); transient ischemic attack (n=1); amaurosis fugax (n=1); aortic thrombosis (n=1); medullar ischemia (n=1); optic ischemic neuropathy (n=1); peripheral artery occlusion (n=1); peripheral ischemia (n=1); and vascular graft occlusion (n=1).
Treatment with human fibrinogen concentrate in congenital fibrinogen deficiency has been associated with risk of thrombosis at target fibrinogen levels that were less than 150 mg/dL. The risk of thrombosis may be greater when the target fibrinogen plasma level is 150 mg/dL. Weigh the benefits of FIBRYGA administration versus the risks of thrombosis. Patients receiving FIBRYGA should be monitored for signs and symptoms of thrombosis. [see Patient Counseling Information ( 17 )]
5.3 Transmissible Infectious Agents
FIBRYGA is made from human plasma. Products made from human plasma may contain infectious agents (e.g., viruses and the CJD agent that can cause disease). Also, unknown infectious agents may be present in such products [see Patient Counseling Information ( 17 )] . The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current virus infections, and by a process demonstrated to inactivate and/or remove certain viruses during manufacturing [see Description ( 11 )] . Despite these measures, such products may transmit disease. All infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Octapharma at 1-866-766-4860.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rate in the clinical trials of another drug and may not reflect the rates observed in practice.
Four hundred twenty-eight patients received at least one dose of FIBRYGA for the treatment of bleeding and/or for perioperative management. In total, 677 doses were infused in five studies [ 1 - 5 ].
The safety of FIBRYGA was investigated in FIBRES, a randomized controlled trial comparing FIBRYGA to cryoprecipitate in adult patients with acquired fibrinogen deficiency who were experiencing clinically significant bleeding and hypofibrinogenemia after cardiac surgery [ 1 ]. In total, 1296 adverse events occurred in 512 patients during the study after receipt of fibrinogen supplementation: 623 events in 248 (66.7%) patients in the FIBRYGA group, and 673 events in 264 (72.7%) patients in the cryoprecipitate group.
Deaths
A total of 35 (9.41%) patients died in the period up to postoperative day 28 in the FIBRYGA group and 27 (7.44%) patients died in the cryoprecipitate group. After postoperative day 28, an additional 5 patients died after receiving FIBRYGA and an additional 2 patients died after receiving cryoprecipitate.
Adverse Events
Serious adverse reactions occurred in 117 (31.5%) patients in the FIBRYGA group compared to 126 (34.7%) patients in the cryoprecipitate group.
The most common adverse reactions are shown in Table 1.
Table 1: Adverse Reactions Reported in More Than 5% of Patients Following FIBRYGA or Cryoprecipitate Administration in the FIBRES Study
FIBRYGA Patients (N=372)
n (%)Cryoprecipitate Patients (N=363)
n (%)Cardiac disorders Atrial fibrillation 108 (29.0%) 122 (33.6%) Blood and lymphatic system disorders Anemia 58 (15.6%) 52 (14.3%) Thrombocytopenia 15 (4.0%) 20 (5.5%) Psychiatric disorders Delirium 56 (15.1%) 54 (14.9%) Renal and urinary disorders Acute kidney injury 29 (7.8%) 29 (8.0%) Renal failure 19 (5.1%) 19 (5.2%) Hepatobiliary disorders Hepatic function abnormal 27 (7.3%) 26 (7.2%) Infections and infestations Pneumonia 18 (4.8%) 19 (5.2%) In the congenital fibrinogen deficiency studies [ 3 - 5 ], one patient had a mild skin reaction (itchiness and redness) after FIBRYGA administration for a bleeding episode and was treated with diphenhydramine and hydrocortisone. Thereafter, the patient received another infusion of FIBRYGA for the treatment of the same bleeding episode and another FIBRYGA infusion for surgical management during the next week. For both of those FIBRYGA infusions the patient was treated with diphenhydramine and hydrocortisone prophylactically and did not experience any drug reactions.
Further adverse reactions included one case each of digital foot ischemia, portal vein thrombosis following splenectomy, and peripheral phlebitis of the upper limbs.
The following serious adverse reactions are described elsewhere in the labeling:
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no data with FIBRYGA use in pregnant women to determine whether there is a drug-associated risk. Animal reproduction studies have not been conducted with FIBRYGA. It is not known whether FIBRYGA can cause fetal harm when administered to a pregnant woman or can affect fertility. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of FIBRYGA in human milk, the effect on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for FIBRYGA and any potential adverse effects on the breastfed infant from FIBRYGA or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of FIBRYGA have been established in pediatric patients <18 years of age for fibrinogen supplementation in acquired and congenital fibrinogen deficiency. Use of FIBRYGA is supported by evidence from adequate and well-controlled studies in adults with acquired fibrinogen deficiency and safety data in pediatric patients in congenital fibrinogen deficiency [see Clinical Studies ( 14 )].
Pharmacokinetic studies were only performed in patients with congenital fibrinogen deficiency. There was no difference in the pharmacokinetics of FIBRYGA between adults and adolescents (12-17 years of age).
Lower incremental in vivo recovery (IVR), faster clearance and shorter half-life were observed in children aged 1 to < 12 years, compared to adults and adolescents. As higher doses of FIBRYGA were administered for the treatment of bleeding episodes in children aged 1 to < 12 years, higher doses may be required in this age group in patients with acquired or congenital fibrinogen deficiency [see Dosage and Administration ( 2.1 )].
8.5 Geriatric Use
A total of 177 patients >65 years were treated with FIBRYGA in clinical studies in acquired fibrinogen deficiency, representing 47.6% of the patients in the FIBRYGA group.
Clinical studies of FIBRYGA in congenital fibrinogen deficiency did not include sufficient numbers of patients aged 65 years and over to provide conclusive evidence as to whether or not they respond differently than younger patients.
-
11 DESCRIPTION
FIBRYGA is a human plasma-derived, sterile, purified, virus-inactivated and nanofiltered (20 nm) fibrinogen concentrate.
FIBRYGA is supplied as a lyophilized powder for reconstitution for intravenous injection. FIBRYGA contains no preservatives. Each bottle contains approximately 1 g of fibrinogen. The diluent for reconstitution of the lyophilized powder is sterile Water for Injection.
The nominal composition of FIBRYGA is as follows:
Component Quantity/ mL Human Fibrinogen 20 mg Sodium Chloride 6 mg Sodium Citrate Dihydrate 1.5 mg Glycine 10 mg L-Arginine Hydrochloride 10 mg All units of human plasma used in the manufacture of FIBRYGA are provided by FDA-approved blood establishments, and are tested by FDA-licensed serological tests for Hepatitis B surface antigen (HBsAg), antibodies to Hepatitis C Virus (HCV) and Human Immunodeficiency Virus (HIV)-1/2. As an additional safety measure, the plasma is tested with Nucleic Acid Tests (NATs) for Hepatitis A Virus (HAV), Hepatitis B Virus (HBV), HCV and HIV-1 and found to be non-reactive (negative). The plasma is also screened for Human Parvovirus (B19V) by NAT. The limit for B19V DNA in the mini-pool is set not to exceed 10 3 IU/mL. Only plasma that passed virus screening is used for production.
The FIBRYGA manufacturing process includes a solvent/detergent (S/D) step for virus inactivation, and a nanofiltration step (Planova 20N nanofilter or Pegasus SV4 nanofilter) for virus removal. The mean cumulative virus reduction factors of these steps are summarized in Table 2 below.
Table 2: Cumulative Virus Reduction Factors (Log 10 ) During FIBRYGA Manufacture
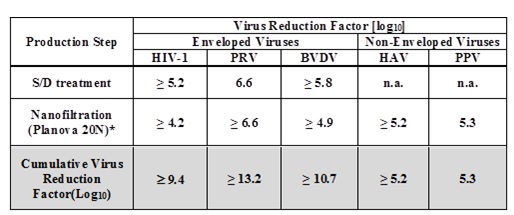
PRV: Pseudorabies Virus, model for large enveloped DNA viruses
BVDV: Bovine Virus Diarrhea Virus, model for HCV
PPV: Porcine Parvovirus, model for B19V
n.a.: not applicable
* When the nanofiltration step was performed using a Pegasus SV4 nanofilter, the virus reduction factors for HIV-1, PRV, BVDV, HAV, and PPV were ≥ 3.9, ≥ 6.3, ≥ 5.0, ≥ 5.2, and 4.5, respectively. The cumulative virus reduction factors (S/D treatment + Pegasus SV4 nanofiltration) were ≥ 9.0, ≥ 12.9, ≥ 10.8, ≥ 5.2, and 4.5, respectively.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fibrinogen (Factor I) is a soluble plasma protein that, during the coagulation process, is converted to fibrin, one of the key components of the blood clot. Fibrinogen is a heterohexamer with a molecular weight of 340 kDa and composed of two sets of A alpha , B beta , and gamma polypeptide chains.
Following coagulation activation and thrombin generation, fibrinogen is cleaved by thrombin at specific sites on the A alpha and B beta chains to remove fibrinopeptide A (FPA) and fibrinopeptide B (FPB). The removal of FPA and FPB exposes binding sites on the fibrinogen molecule and leads to the formation of fibrin monomers that subsequently undergo polymerization. The resulting fibrin is stabilized by activated factor XIII. Factor XIIIa acts on fibrin to form cross links between fibrin polymers and renders the fibrin clot more resistant to fibrinolysis. The end product of the coagulation cascade is cross-linked fibrin which stabilizes the primary platelet plug and achieves secondary hemostasis.
12.2 Pharmacodynamics
Administration of FIBRYGA to patients with congenital fibrinogen deficiency supplements the missing coagulation factor or increases low plasma fibrinogen levels. Normal plasma fibrinogen level is in the range of 200-450 mg/dL.
An open-label, prospective, randomized, controlled, two-arm, cross-over study was conducted in 22 patients with congenital fibrinogen deficiency (afibrinogenemia), ranging in age from 12 to 53 years (6 adolescents, 16 adults). Each patient received a single intravenous 70 mg/kg dose of FIBRYGA and the comparator product. Blood samples were drawn from the patients to measure the fibrinogen activity at baseline and up to 14 days after the infusion. Maximum Clot Firmness (MCF) was measured by thromboelastometry (ROTEM).
For each patient, MCF was determined before (baseline) and one hour after the single dose administration of FIBRYGA. In this cross-over study, the results were compared with another fibrinogen concentrate available on the US market. The results of the study demonstrated that the MCF values were significantly higher after administration of FIBRYGA than at baseline (see Table 3). The mean change from pre-infusion to 1 hour post-infusion was 9.7 mm in the primary analysis (9.0 mm for patients < 18 years old and 9.9 mm for patients ≥ 18 to < 65 years old).
Table 3: MCF [mm] (ITT population) n=22
Time point Mean ± SD Median (range) Pre-infusion 0 ± 0 0 (0-0) 1 hour post-infusion 9.7 ± 3.0 10.0 (4.0-16.0) Mean change (primary analysis) a 9.7 ± 3.0 10.0 (4.0-16.0) MCF = maximum clot firmness; mm = millimeter; ITT = intention-to-treat.
a p-value was <0.0001, 95% CI 8.37, 10.99
12.3 Pharmacokinetics
An open-label, prospective, randomized, controlled, two-arm, cross-over study was conducted in 22 patients with congenital fibrinogen deficiency (afibrinogenemia), ranging in age from 12 to 53 years (6 adolescents, 16 adults), where each patient received a single intravenous 70 mg/kg dose of FIBRYGA and the comparator product [ 5 ]. In addition, a prospective, open-label, uncontrolled, multicenter clinical study was conducted in 14 pediatric patients with afibrinogenemia, ranging in age from 1 to 10 years [ 3 ]. Thirteen patients each received a single intravenous 70 mg/kg dose of FIBRYGA. In both studies, blood samples were drawn from the patients to determine the fibrinogen activity at baseline and up to 14 days after the infusion. The pharmacokinetic parameters of FIBRYGA (n=34) are summarized in Table 4.
In the study of adult and adolescent patients, the incremental in vivo recovery (IVR) was determined from levels obtained up to 4 hours post-infusion. The median incremental IVR was a 1.8 mg/dL (range 1.1-2.6 mg/dL) increase per mg/kg. The median in vivo recovery indicates that a dose of 70 mg/kg will increase patients’ fibrinogen plasma concentration by approximately 125 mg/dL. In pediatric patients, the incremental in vivo recovery (IVR) was determined from levels obtained up to 3 hours post-infusion. The median incremental IVR was a 1.4 mg/dL (range 1.3-2.1 mg/dL) increase per mg/kg.
Table 4: Pharmacokinetic Parameters for Fibrinogen Activity
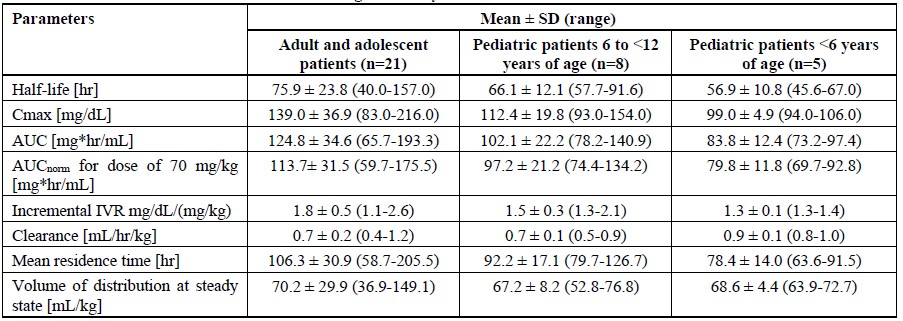
C max = maximum plasma concentration; AUC = area under the curve; AUC norm = area under the curve normalized to the dose administered; SD = standard deviation
No difference in fibrinogen activity was observed between males and females. There was no difference in the pharmacokinetics of FIBRYGA between adults and adolescents (12-17 years of age). Lower recovery, shorter half-life and faster clearance were observed in children aged 1 to < 12 years, compared to adults and adolescents. Other parameters, such as Cmax (maximum plasma concentration), AUC (area under the curve) and AUCnorm (area under the curve normalized to the dose administered), were also lower in children. Such differences may be expected for the younger age subgroup owing to physiological differences in body size and composition.
-
14 CLINICAL STUDIES
Acquired Fibrinogen Deficiency
FIBRYGA was investigated in a prospective, multicenter, randomized, controlled, single-blinded study conducted in adult cardiac surgical patients for whom fibrinogen supplementation was ordered in accordance with accepted clinical standards (significant hemorrhage and known or presumed hypofibrinogenemia). A total of 195 patients 17–65 years of age were included in the FIBRYGA group and 203 in the cryoprecipitate group. There were 177 patients >65 years of age included in the FIBRYGA group and 160 in the cryoprecipitate group. A pre-planned interim analysis was conducted based on 302 in the FIBRYGA group and 303 in the cryoprecipitate group.
Hypofibrinogenemia was defined as a plasma fibrinogen level <2.0 g/L by the Clauss method or by clot amplitude at 10 minutes of the fibrin-based clot <10 mm by thromboelastometry. Patients were randomly assigned to receive either FIBRYGA, 4 g infused over approximately 10 minutes (infusion rate 20 mL per minute), or cryoprecipitate, 10 units infused according to local practice. The doses were to be repeated as needed.
Patients received a median of 4 g (range 2.0–20.0) of fibrinogen concentrate and 10 units (range 10.0–120.0) of cryoprecipitate. The fibrinogen level increased from 1.7 ± 0.6 g/L to 2.5 ± 0.6 g/L in the FIBRYGA group and from 1.7 ± 0.6 g/L to 2.3 ± 0.6 g/L for the cryoprecipitate group, representing a mean increase of 0.9 ± 0.4 g/L in the FIBRYGA group and 0.7 ± 0.4 g/L in the cryoprecipitate group.
FIBRYGA was demonstrated to be non-inferior to cryoprecipitate based on the total number of units of allogeneic blood products (ABPs) administered during the first 24 hours after termination of cardiopulmonary bypass (CPB) (see Table 5).
Table 5: Primary Outcome: Comparison of the Total Number of Allogeneic Blood Product Units Transfused Within 24 Hours After Termination of CPB
Mean ± SD Median (IQR) ABP mean ratio estimate* FIBRYGA (n=302) 17.0 ± 17.7 12.0 (6.0-23.0) 0.98 Cryoprecipitate (n=303) 17.4 ± 17.0 14.0 (6.0-23.0) CPB = cardiopulmonary bypass; SD = standard deviation; IQR = interquartile range; ABP = allogeneic blood product; CI = confidence interval
*Using ordinary Poisson regression, the 99.742% upper CI limit was calculated to be 1.04, below the pre-specified 1.20 non-inferiority margin, demonstrating FIBRYGA was non-inferior to cryoprecipitate (p<0.0001, compared to the pre-specified alpha level of 0.00258)
Congenital Fibrinogen Deficiency
The following data come from patients with congenital fibrinogen deficiency (afibrinogenemia and hypofibrinogenemia) treated in two prospective, open-label, uncontrolled, multicenter clinical studies to assess efficacy of FIBRYGA for treatment of bleeding events (BEs), one study evaluated 24 adolescents and adults ages 12 to 54 years, and one evaluated 8 children 1 to 10 years of age [ 3 , 4 ].
Efficacy of FIBRYGA in treating BEs was measured using an objective 4-point hemostatic efficacy-scale based on criteria such as bleeding cessation, changes in hemoglobin, and use of any other hemostatic means. In the adult and adolescent study, 24 patients received FIBRYGA treatment for 87 evaluable BEs one of which was major and 86 minor. Major bleeding included spontaneous intracranial hemorrhage, while minor bleeding included spontaneous occult gastrointestinal bleeding, mild hemarthrosis, superficial muscle, soft tissue or oral bleeding. Sixty-five (75%) of evaluable BEs were spontaneous and 22 (25%) BEs were traumatic. The major BE (intracranial hemorrhage) required two infusions. The median number of infusions for minor BEs was one. Four (4.5%) minor BEs required 2 infusions and one (1.1%) minor BE (gastrointestinal bleeding) required 7 infusions. The treatment of one BE was classified as failure (moderate efficacy) and 86 of 87 (98.9%) of evaluable BEs were assessed as having a successful efficacy outcome (8 ratings of good and 78 ratings of excellent efficacy).
Ten BEs were treated in the study of children, 2 were major and 8 minor. Major bleeds were thigh hematoma, and intraperitoneal bleed from splenic rupture, while minor bleeding included soft tissue or oral bleeding. Five (50.0%) BEs were spontaneous and five (50.0%) were traumatic. The median (range) number of infusions per BE was 1 (1-4). Of the two major treated BEs, one required three infusions, while the other received four infusions, both achieved a hemostatic efficacy score of good. Three of 10 BEs in children were assessed as having a good hemostatic efficacy score, and seven as having an excellent hemostatic efficacy score, therefore 10 (100%) had a successful efficacy outcome (rating of good or excellent efficacy).
-
15 REFERENCES
- Callum J, Farkouh ME, Scales DC, Heddle NM, Crowther M, Rao V, Hucke HP, Carroll J, Grewal D, Brar S, Bussières J, Grocott H, Harle C, Pavenski K, Rochon A, Saha T, Shepherd L, Syed S, Tran D, Wong D, Zeller M, Karkouti K; FIBRES Research Group. Effect of Fibrinogen Concentrate vs Cryoprecipitate on Blood Component Transfusion After Cardiac Surgery: The FIBRES Randomized Clinical Trial. JAMA. 2019 Nov 26;322(20):1966-1976.
- Roy A, Stanford S, Nunn S, Alves S, Sargant N, Rangarajan S, Smith EA, Bell J, Dayal S, Cecil T, Tzivanakis A, Kruzhkova I, Solomon C, Knaub S, Moran B, Mohamed F. Efficacy of fibrinogen concentrate in major abdominal surgery - A prospective, randomized, controlled study in cytoreductive surgery for pseudomyxoma peritonei. J Thromb Haemost. 2020 Feb;18(2):352-363
- Djambas Khayat C, Lohade S, D'Souza F, Shamanur LG, Zekavat OR, Kruzhkova I, Schwartz B, Solomon C, Knaub S, Peyvandi F. Efficacy and safety of fibrinogen concentrate for on-demand treatment of bleeding and surgical prophylaxis in paediatric patients with congenital fibrinogen deficiency. Haemophile. 2021 Mar;27(2):283-292.
- Lissitchkov T, Madan B, Djambas Khayat C, Zozulya N, Ross C, Karimi M, Kavakli K, De Angulo GR, Almomen A, Subramanian K, D'Souza F, Viswabandya A, Hoorfar H, Schwartz BA, Solomon C, Knaub S, Peyvandi F. Fibrinogen concentrate for treatment of bleeding and surgical prophylaxis in congenital fibrinogen deficiency patients. J Thromb Haemost. 2020 Apr;18(4):815-824
- Ross C, Rangarajan S, Karimi M, Toogeh G, Apte S, Lissitchkov T, Acharya S, Manco-Johnson MJ, Srivastava A, Brand B, Schwartz BA, Knaub S, Peyvandi F. Pharmacokinetics, clot strength and safety of a new fibrinogen concentrate: randomized comparison with active control in congenital fibrinogen deficiency. J Thromb Haemost. 2018 Feb;16(2):253-261.
-
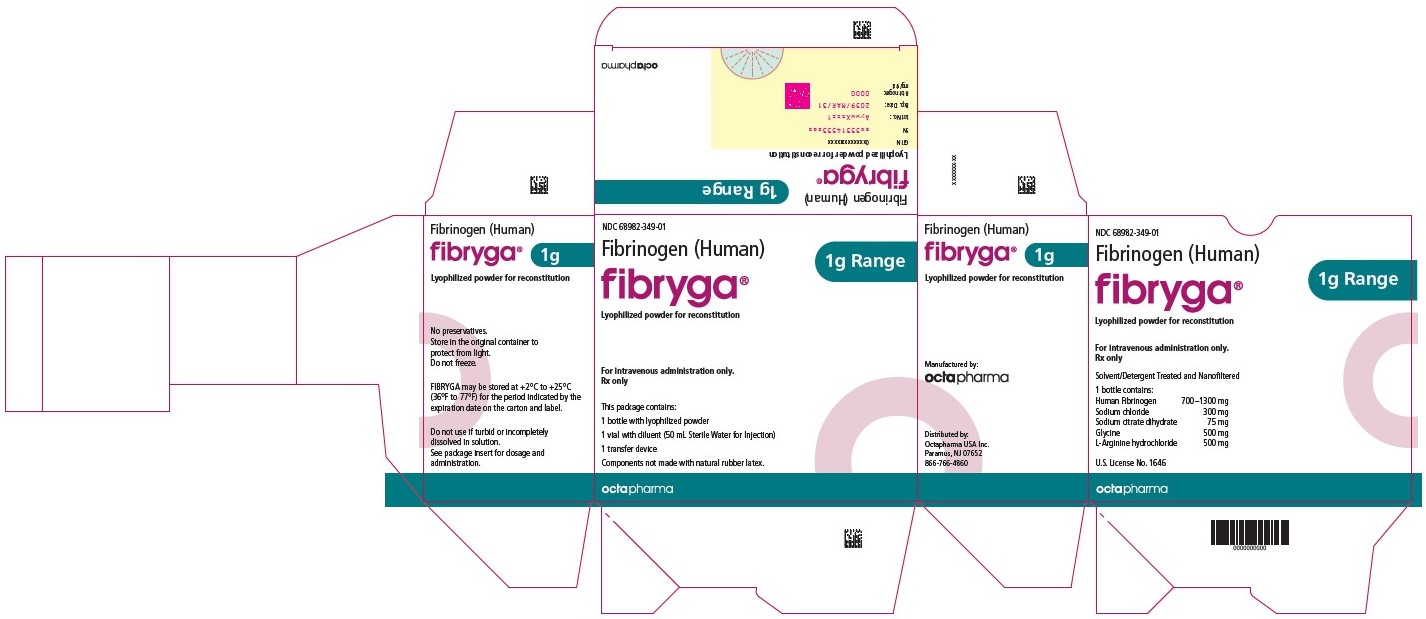
16 HOW SUPPLIED/STORAGE AND HANDLING
How supplied:
FIBRYGA is supplied in a single-dose bottle.
The following nominal dosage form is available:
Carton NDC Number FIBRYGA 1g 68982-349-01 - The actual potency of fibrinogen in mg is stated on each FIBRYGA carton and bottle.
- FIBRYGA is supplied in a package with a single-dose bottle of lyophilized powder and a vial of diluent (sterile Water for Injection), together with a transfer device.
- Components used in the packaging of FIBRYGA are not made with natural rubber latex.
Storage and Handling:
- Store FIBRYGA for up to 48 months at +2°C to + 25°C (36°F to 77°F) from the date of manufacture.
- Do not use FIBRYGA beyond the expiration date printed on the carton and bottle.
- Do not freeze. Store in the original container to protect from light.
- After reconstitution, do not refrigerate or freeze the FIBRYGA solution. Use the reconstituted FIBRYGA solution immediately or within 4 hours after reconstitution.
- Dispose of any unused product or waste material in accordance with local requirements.
-
17 PATIENT COUNSELING INFORMATION
- Inform patients of the early signs of hypersensitivity or allergic reactions to FIBRYGA, including hives, chest tightness, wheezing, hypotension, and anaphylaxis [see Warnings and Precautions ( 5.1 )] . Advise them to notify their physician immediately if they experience any of these symptoms.
- Inform patients that blood clots with or without consequent obstruction of blood flow may occur with FIBRYGA. Any symptoms of blood clots such as unexplained chest and/or leg pain or swelling of the legs or arms, coughing up blood, shortness of breath, increased rate of breathing or unexplained symptoms related to the nervous system such as stroke or weakness following administration of FIBRYGA should be reported to their physician immediately [see Warnings and Precautions ( 5.2 )] .
- Inform patients that FIBRYGA is made from human plasma (part of the blood) and may contain infectious agents, e.g., viruses and, theoretically, the Creutzfeldt-Jakob Disease agent, that can cause disease. Explain that the risk FIBRYGA may transmit an infectious agent has been reduced by screening the plasma donors, by testing the donated plasma for certain virus infections, and by two processes demonstrated to inactivate and/or remove certain viruses during manufacturing [see Warnings and Precautions ( 5.3 )] . Symptoms of a possible virus infection include headache, fever, nausea, vomiting, weakness, malaise, diarrhea, or, in the case of hepatitis, jaundice.
Manufactured by:
Octapharma Pharmazeutika Produktionsges.m.b.H.
Oberlaaer Strasse 235
A-1100 Vienna, Austria
Octapharma AB
Lars Forssells gata 23
SE-112 75, Sweden
U.S. License No. 1646
Distributed by:
Octapharma USA Inc.
117 West Century Road
Paramus, NJ 07652
Instructions for Use
FIBRYGA / fye bri ' gah /
Fibrinogen (Human)
Read these instructions carefully before using FIBRYGA for the first time. The general guidelines for mixing and infusing FIBRYGA are listed below. If you are unsure of any of these steps, please contact the manufacturer before using FIBRYGA.
FIBRYGA is supplied as a powder. Before it can be infused, it must be mixed with sterile Water for Injection.
FIBRYGA is provided with the Nextaro transfer device for reconstitution of the FIBRYGA powder in sterile Water for Injection.
Instructions for Mixing FIBRYGA
1. Warm both the powder and sterile Water for Injection (sWFI) in their closed bottles to room temperature. This temperature should be maintained during reconstitution. If a water bath is used for warming, prevent water from coming into contact with the rubber stoppers or the caps of the bottles. The temperature of the water bath should not exceed +37°C (98°F).
2. Remove the flip cap from the FIBRYGA bottle and the sWFI vial and disinfect the rubber stoppers with an alcohol swab and allow to dry.
3. Open the Nextaro ® transfer device package by peeling off the lid (Fig. 1). To maintain sterility, do not remove the Nextaro ® transfer device from the blister package. Do not touch the spike.
4. Place the diluent vial on an even, clean surface and hold it firmly. Without removing the blister package, place the blue part of the transfer device on top of the diluent vial. Press straight and firmly down until it snaps into place (Fig. 2). Do not twist while attaching.
Note:
The transfer device must be attached to the diluent vial first and then to the lyophilized powder bottle. Otherwise, loss of vacuum occurs, and transfer of the diluent does not take place. If diluent is not completely transferred to the lyophilized powder bottle during this process, contact your Octapharma representative.

5. While holding onto the diluent vial, carefully remove the blister package from the Nextaro ® transfer device by pulling vertically upwards. Make sure to leave the transfer device attached firmly to the diluent vial (Fig. 3).
6. Place the FIBRYGA bottle on an even, clean surface and hold it firmly. Take the diluent vial with the attached transfer device and turn it upside down. Place the white part of the transfer device connector on top of the FIBRYGA bottle and press firmly down until it snaps into place (Fig. 4). Do not twist while attaching. The diluent will flow automatically into the FIBRYGA bottle.
7. With the diluent vial still attached, gently swirl the FIBRYGA bottle until the powder is fully dissolved. To avoid foam formation, do not shake the bottle. The powder should be dissolved completely within approx. 5 minutes. Unscrew the Nextaro ® transfer device (blue part) counterclockwise into two parts (Fig. 5). Do not touch the Luer lock connector on the white part of the transfer device.
8. Dispose of the empty diluent vial together with the blue part of the transfer device.- After reconstitution, the FIBRYGA solution should be almost colorless and slightly opalescent. Inspect the reconstituted FIBRYGA solution in the syringe for visible particulate matter and discoloration prior to administration. Do not use if particulate matter or discoloration are observed.
The powder should be reconstituted only directly before injection. After reconstitution, do not refrigerate or freeze the FIBRYGA solution. Use the reconstituted FIBRYGA solution immediately or within 4 hours after reconstitution. Discard any remaining FIBRYGA solution.
Instructions for infusion
For intravenous use only after reconstitution.

1. Carefully attach a syringe to the Luer lock connector on the white part of the Nextaro ® transfer device (Fig. 6).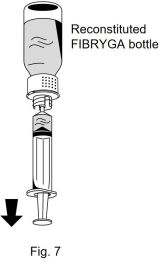
2. Turn the FIBRYGA bottle upside down and draw the solution into the syringe (Fig. 7).
3. Once the solution has been transferred, firmly hold the barrel of the syringe (keeping the syringe plunger facing down) and remove the syringe from the Nextaro ® transfer device (Fig. 8).
4. Dispose of the white part of the transfer device together with the empty FIBRYGA bottle.5. Inspect the reconstituted FIBRYGA solution in the syringe for visible particulate matter and discoloration prior to administration. Do not use if particulate matter or discoloration are observed.
6. Do not administer FIBRYGA in the same tubing or container as other medications.
7. Use aseptic technique when administering FIBRYGA.
8. Clean the chosen injection site with an alcohol swab.
9. Attach a standard infusion set to the syringe. Insert the needle of the infusion set into the chosen vein.
10. Perform intravenous infusion. The rate of administration should be determined by the patient’s comfort level, at a recommended maximum rate of 20 mL per minute in patients with acquired fibrinogen deficiency and 5 mL per minute in patients with congenital fibrinogen deficiency.
11. No blood should enter the syringe due to the risk of fibrin clot formation.
12. After infusing FIBRYGA, remove and properly discard the infusion set. After the infusion, remove the peel-off label containing the batch number from the FIBRYGA bottle, and place it in the log book for record keeping. Discard the empty bottle.
Manufactured by:
Octapharma Pharmazeutika Produktionsges.m.b.H.
Oberlaaer Strasse 235
A-1100 Vienna, Austria
Octapharma AB
Lars Forssells gata 23
SE-112 75, Sweden
U.S. License No. 1646
Distributed by:
Octapharma USA, Inc.
117 West Century Road
Paramus, NJ 07652
FIBRYGA is a registered trademark of Octapharma.
Issued November 2024.
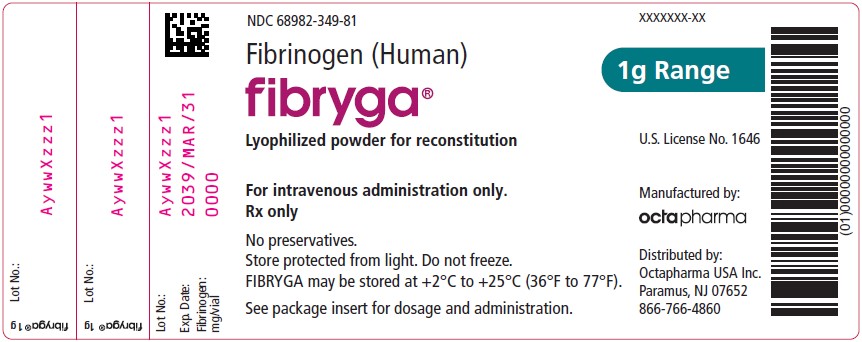
- PACKAGE LABEL - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FIBRYGA
fibrinogen (human) powder, for solutionProduct Information Product Type PLASMA DERIVATIVE Item Code (Source) NDC:68982-349 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FIBRINOGEN HUMAN (UNII: N94833051K) (FIBRINOGEN HUMAN - UNII:N94833051K) FIBRINOGEN HUMAN 20 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68982-349-01 1 in 1 CARTON 1 NDC:68982-349-81 50 mL in 1 BOTTLE, GLASS; Type 9: Other Type of Part 3 Combination Product (e.g., Drug/Device/Biological Product) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125612 12/20/2024 Labeler - Octapharma USA Inc (606121163)