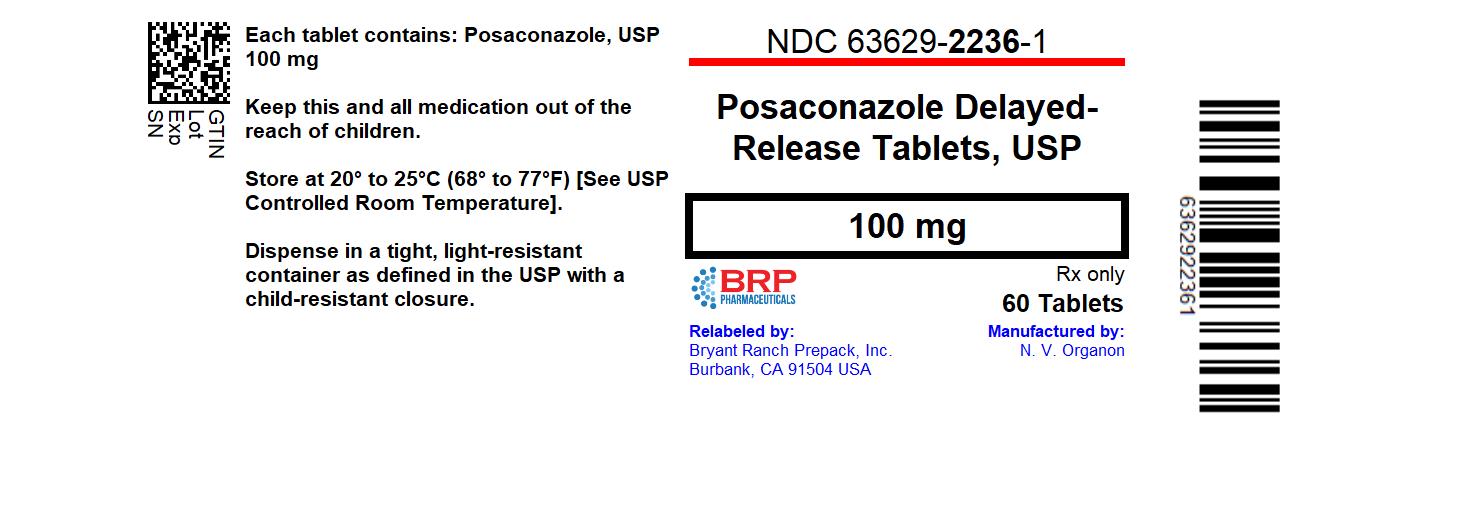
Label: POSACONAZOLE tablet, coated
- NDC Code(s): 63629-2236-1
- Packager: Bryant Ranch Prepack
- This is a repackaged label.
- Source NDC Code(s): 0254-2045
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application Authorized Generic
Drug Label Information
Updated December 4, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use POSACONAZOLE delayed-release tablets safely and effectively. See full prescribing information for POSACONAZOLE delayed-release tablets.
Posaconazole delayed-release tablets, for oral use
Initial U.S. Approval: 2006RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Posaconazole is an azole antifungal indicated as follows:
- Posaconazole delayed-release tablets are indicated for the treatment of invasive aspergillosis in adults and pediatric patients 13 years of age and older. (1.1)
-
Posaconazole is indicated for the prophylaxis of invasive Aspergillus and Candida infections in patients who are at high risk of developing these infections due to being severely immunocompromised, such as hematopoietic stem cell transplant (HSCT) recipients with graft-versus-host disease (GVHD) or those with hematologic malignancies with prolonged neutropenia from chemotherapy as follows: (1.2)
- Posaconazole delayed-release tablets: adults and pediatric patients 2 years of age and older who weigh greater than 40 kg
DOSAGE AND ADMINISTRATION
- Posaconazole delayed-release tablets and oral suspension are not substitutable due to the differences in the dosing of each formulation. Therefore, follow the specific dosage recommendations for each of the formulations. (2.1, 2.2, 2.3)
- Administer Posaconazole delayed-release tablets with or without food. (2)
Indication Dose and Duration of Therapy Treatment of invasive Aspergillosis Posaconazole Delayed-Release Tablets:
Loading dose: 300 mg (three 100 mg delayed-release tablets) twice a day on the first day.
Maintenance dose: 300 mg (three 100 mg delayed-release tablets) once a day thereafter. Recommended total duration of therapy is 6 to 12 weeks. (2.2)
Switching between the intravenous and delayed-release tablets is acceptable. A loading dose is not required when switching between formulations. (2.2)Prophylaxis of invasive Aspergillus and Candida infections Posaconazole Delayed-Release Tablets:
Loading dose: 300 mg (three 100 mg delayed-release tablets) twice a day on the first day.
Maintenance dose: 300 mg (three 100 mg delayed-release tablets) once a day, starting on the second day. Duration of therapy is based on recovery from neutropenia or immunosuppression. (2.2)DOSAGE FORMS AND STRENGTHS
- Posaconazole delayed-release tablet: 100 mg (3)
CONTRAINDICATIONS
- Known hypersensitivity to posaconazole or other azole antifungal agents. (4.1)
- Coadministration of posaconazole with the following drugs is contraindicated: posaconazole increases concentrations and toxicities of:
- Sirolimus (4.2, 5.1, 7.1)
- CYP3A4 substrates (pimozide, quinidine): can result in QTc interval prolongation and cases of torsades de pointes (TdP) (4.3, 5.2, 7.2)
- HMG-CoA Reductase Inhibitors Primarily Metabolized through CYP3A4 (4.4, 7.3)
- Ergot alkaloids (4.5, 7.4)
- Venetoclax: In patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) at initiation and during the ramp-up phase (4.6, 5.9, 7.15)
WARNINGS AND PRECAUTIONS
- Calcineurin-Inhibitor Toxicity: Posaconazole increases concentrations of cyclosporine or tacrolimus; reduce dose of cyclosporine and tacrolimus and monitor concentrations frequently. (5.1)
- Arrhythmias and QTc Prolongation: Posaconazole has been shown to prolong the QTc interval and cause cases of TdP. Administer with caution to patients with potentially proarrhythmic conditions. Do not administer with drugs known to prolong QTc interval and metabolized through CYP3A4. (5.2)
- Electrolyte Disturbances: Monitor and correct, especially those involving potassium (K+), magnesium (Mg++), and calcium (Ca++), before and during posaconazole therapy. (5.3)
- Hepatic Toxicity: Elevations in liver tests may occur. Discontinuation should be considered in patients who develop abnormal liver tests or monitor liver tests during treatment. (5.4)
- Concomitant Use with Midazolam: Posaconazole can prolong hypnotic/sedative effects. Monitor patients and benzodiazepine receptor antagonists should be available. (5.6, 7.5)
- Vincristine Toxicity: Concomitant administration of azole antifungals, including posaconazole, with vincristine has been associated with neurotoxicity and other serious adverse reactions; reserve azole antifungals, including posaconazole, for patients receiving a vinca alkaloid, including vincristine, who have no alternative antifungal treatment options. (5.7, 7.10)
- Breakthrough Fungal Infections: Monitor patients with severe diarrhea or vomiting when receiving Posaconazole delayed-release tablets. (5.8)
- Venetoclax Toxicity: Concomitant administration of Posaconazole with venetoclax may increase venetoclax toxicities, including the risk of tumor lysis syndrome, neutropenia, and serious infections; monitor for toxicity and reduce venetoclax dose. (4.6, 5.9, 7.15)
ADVERSE REACTIONS
- Common adverse reactions in studies with posaconazole are diarrhea, nausea, fever, vomiting, headache, coughing, and hypokalemia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
DRUG INTERACTIONS
Interaction Drug Interaction - *
- The drug interactions with esomeprazole and metoclopramide do not apply to Posaconazole tablets.
Rifabutin, phenytoin, efavirenz, cimetidine, esomeprazole* Avoid coadministration unless the benefit outweighs the risks (7.6, 7.7, 7.8, 7.9) Other drugs metabolized by CYP3A4 Consider dosage adjustment and monitor for adverse effects and toxicity (7.1, 7.10, 7.11) Digoxin Monitor digoxin plasma concentrations (7.12) Fosamprenavir, metoclopramide* Monitor for breakthrough fungal infections (7.6, 7.13) USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Treatment of Invasive Aspergillosis
1.2 Prophylaxis of Invasive Aspergillus and Candida Infections
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosage and Administration Instructions for Posaconazole Delayed-Release Tablets
2.3 Non-substitutability between Posaconazole Delayed-Release Tablets and Posaconazole Oral Suspension
2.4 Dosage Adjustments in Patients with Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Use with Sirolimus
4.3 QT Prolongation with Concomitant Use with CYP3A4 Substrates
4.4 HMG-CoA Reductase Inhibitors Primarily Metabolized Through CYP3A4
4.5 Use with Ergot Alkaloids
4.6 Use with Venetoclax
5 WARNINGS AND PRECAUTIONS
5.1 Calcineurin-Inhibitor Toxicity
5.2 Arrhythmias and QT Prolongation
5.3 Electrolyte Disturbances
5.4 Hepatic Toxicity
5.5 Renal Impairment
5.6 Midazolam Toxicity
5.7 Vincristine Toxicity
5.8 Breakthrough Fungal Infections
5.9 Venetoclax Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Immunosuppressants Metabolized by CYP3A4
7.2 CYP3A4 Substrates
7.3 HMG-CoA Reductase Inhibitors (Statins) Primarily Metabolized Through CYP3A4
7.4 Ergot Alkaloids
7.5 Benzodiazepines Metabolized by CYP3A4
7.6 Anti-HIV Drugs
7.7 Rifabutin
7.8 Phenytoin
7.9 Gastric Acid Suppressors/Neutralizers
7.10 Vinca Alkaloids
7.11 Calcium Channel Blockers Metabolized by CYP3A4
7.12 Digoxin
7.13 Gastrointestinal Motility Agents
7.14 Glipizide
7.15 Venetoclax
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Gender
8.9 Race
8.10 Weight
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Treatment of Invasive Aspergillosis with Noxafil Injection and Noxafil Delayed-Release Tablets
14.2 Prophylaxis of Aspergillus and Candida Infections with Noxafil Oral Suspension
14.3 Treatment of Oropharyngeal Candidiasis with Noxafil Oral Suspension
14.4 Noxafil Oral Suspension Treatment of Oropharyngeal Candidiasis Refractory to Treatment with Fluconazole or Itraconazole
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Treatment of Invasive Aspergillosis
Posaconazole delayed-release tablets are indicated for the treatment of invasive aspergillosis in adults and pediatric patients 13 years of age and older.
1.2 Prophylaxis of Invasive Aspergillus and Candida Infections
Posaconazole is indicated for the prophylaxis of invasive Aspergillus and Candida infections in patients who are at high risk of developing these infections due to being severely immunocompromised, such as hematopoietic stem cell transplant (HSCT) recipients with graft-versus-host disease (GVHD) or those with hematologic malignancies with prolonged neutropenia from chemotherapy [see Clinical Studies (14.1)] as follows:
Posaconazole delayed-release tablets: adults and pediatric patients 2 years of age and older who weigh greater than 40 kg
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Non-substitutable
Posaconazole delayed-release tablets and oral suspension are not substitutable due to the differences in the dosing of each formulation [see Dosage and Administration (2.2, 2.3, 2.4)].
Posaconazole delayed-release tablets
- Swallow tablets whole. Do not divide, crush, or chew.
- Administer with or without food [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
- For patients who cannot eat a full meal, Posaconazole delayed-release tablets should be used instead of Posaconazole oral suspension for the prophylaxis indication. Posaconazole delayed-release tablets generally provide higher plasma drug exposures than posaconazole oral suspension under both fed and fasted conditions [see Dosage and Administration (2.2)].
2.2 Dosage and Administration Instructions for Posaconazole Delayed-Release Tablets
Dosage:
Table 1: Dosage for Posaconazole Delayed-Release Tablets Indication Weight/Age Dose and Frequency Duration of Therapy Treatment of invasive Aspergillosis 13 years of age and older regardless of weight Loading dose: 300 mg (three 100 mg delayed-release tablets) twice a day on the first day.
Maintenance dose: 300 mg (three 100 mg delayed-release tablets) once a day, starting on the second day.
Switching between the intravenous and delayed-release tablets is acceptable. A loading dose is not required when switching between formulations.Loading dose:
1 day
Maintenance dose:
Recommended total duration of therapy is 6 to 12 weeks.Prophylaxis of invasive Aspergillus and Candida infections 2 years of age and older who weigh greater than 40 kg Loading dose: 300 mg (three 100 mg delayed-release tablets) twice a day on the first day.
Maintenance dose: 300 mg (three 100 mg delayed-release tablets) once a day, starting on the second day.Loading dose:
1 day
Maintenance dose:
Duration of therapy is based on recovery from neutropenia or immunosuppression.Administration Instructions for Posaconazole Delayed-Release Tablets:
- Swallow tablets whole. Do not divide, crush, or chew.
- Administer Posaconazole delayed-release tablets with or without food [see Clinical Pharmacology (12.3)].
2.3 Non-substitutability between Posaconazole Delayed-Release Tablets and Posaconazole Oral Suspension
Posaconazole delayed-release tablets and oral suspension are not substitutable due to the differences in the dosing of each formulation. Therefore, follow the specific dosage recommendations for each of the formulations [see Dosage and Administration (2.2, 2.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Posaconazole is contraindicated in persons with known hypersensitivity to posaconazole or other azole antifungal agents.
4.2 Use with Sirolimus
Posaconazole is contraindicated with sirolimus. Concomitant administration of posaconazole with sirolimus increases the sirolimus blood concentrations by approximately 9-fold and can result in sirolimus toxicity [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
4.3 QT Prolongation with Concomitant Use with CYP3A4 Substrates
Posaconazole is contraindicated with CYP3A4 substrates that prolong the QT interval. Concomitant administration of posaconazole with the CYP3A4 substrates, pimozide and quinidine may result in increased plasma concentrations of these drugs, leading to QTc prolongation and cases of torsades de pointes [see Warnings and Precautions (5.2) and Drug Interactions (7.2)].
4.4 HMG-CoA Reductase Inhibitors Primarily Metabolized Through CYP3A4
Coadministration with the HMG-CoA reductase inhibitors that are primarily metabolized through CYP3A4 (e.g., atorvastatin, lovastatin, and simvastatin) is contraindicated since increased plasma concentration of these drugs can lead to rhabdomyolysis [see Drug Interactions (7.3) and Clinical Pharmacology (12.3)].
4.5 Use with Ergot Alkaloids
Posaconazole may increase the plasma concentrations of ergot alkaloids (ergotamine and dihydroergotamine) which may lead to ergotism [see Drug Interactions (7.4)].
4.6 Use with Venetoclax
Coadministration of posaconazole with venetoclax at initiation and during the ramp-up phase is contraindicated in patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) due to the potential for increased risk of tumor lysis syndrome [see Warnings and Precautions (5.9) and Drug Interactions (7.15)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Calcineurin-Inhibitor Toxicity
Concomitant administration of posaconazole with cyclosporine or tacrolimus increases the whole blood trough concentrations of these calcineurin-inhibitors [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)]. Nephrotoxicity and leukoencephalopathy (including deaths) have been reported in clinical efficacy studies in patients with elevated cyclosporine or tacrolimus concentrations. Frequent monitoring of tacrolimus or cyclosporine whole blood trough concentrations should be performed during and at discontinuation of posaconazole treatment and the tacrolimus or cyclosporine dose adjusted accordingly.
5.2 Arrhythmias and QT Prolongation
Some azoles, including posaconazole, have been associated with prolongation of the QT interval on the electrocardiogram. In addition, cases of torsades de pointes have been reported in patients taking posaconazole.
Results from a multiple time-matched ECG analysis in healthy volunteers did not show any increase in the mean of the QTc interval. Multiple, time-matched ECGs collected over a 12-hour period were recorded at baseline and steady-state from 173 healthy male and female volunteers (18-85 years of age) administered Noxafil oral suspension 400 mg twice daily with a high-fat meal. In this pooled analysis, the mean QTc (Fridericia) interval change from baseline was –5 msec following administration of the recommended clinical dose. A decrease in the QTc(F) interval (–3 msec) was also observed in a small number of subjects (n=16) administered placebo. The placebo-adjusted mean maximum QTc(F) interval change from baseline was <0 msec (–8 msec). No healthy subject administered Noxafil had a QTc(F) interval ≥500 msec or an increase ≥60 msec in their QTc(F) interval from baseline.
Posaconazole should be administered with caution to patients with potentially proarrhythmic conditions. Do not administer with drugs that are known to prolong the QTc interval and are metabolized through CYP3A4 [see Contraindications (4.3) and Drug Interactions (7.2)].
5.3 Electrolyte Disturbances
Electrolyte disturbances, especially those involving potassium, magnesium or calcium levels, should be monitored and corrected as necessary before and during posaconazole therapy.
5.4 Hepatic Toxicity
Hepatic reactions (e.g., mild to moderate elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, total bilirubin, and/or clinical hepatitis) have been reported in clinical trials. The elevations in liver tests were generally reversible on discontinuation of therapy, and in some instances these tests normalized without drug interruption. Cases of more severe hepatic reactions including cholestasis or hepatic failure including deaths have been reported in patients with serious underlying medical conditions (e.g., hematologic malignancy) during treatment with posaconazole. These severe hepatic reactions were seen primarily in subjects receiving the Posaconazole oral suspension 800 mg daily (400 mg twice daily or 200 mg four times a day) in clinical trials.
Liver tests should be evaluated at the start of and during the course of posaconazole therapy. Patients who develop abnormal liver tests during posaconazole therapy should be monitored for the development of more severe hepatic injury. Patient management should include laboratory evaluation of hepatic function (particularly liver tests and bilirubin). Discontinuation of posaconazole must be considered if clinical signs and symptoms consistent with liver disease develop that may be attributable to posaconazole.
5.5 Renal Impairment
Due to the variability in exposure with Posaconazole delayed-release tablets and Posaconazole oral suspension, patients with severe renal impairment should be monitored closely for breakthrough fungal infections [see Dosage and Administration (2.4) and Use in Specific Populations (8.6)].
5.6 Midazolam Toxicity
Concomitant administration of posaconazole with midazolam increases the midazolam plasma concentrations by approximately 5-fold. Increased plasma midazolam concentrations could potentiate and prolong hypnotic and sedative effects. Patients must be monitored closely for adverse effects associated with high plasma concentrations of midazolam and benzodiazepine receptor antagonists must be available to reverse these effects [see Drug Interactions (7.5) and Clinical Pharmacology (12.3)].
5.7 Vincristine Toxicity
Concomitant administration of azole antifungals, including posaconazole, with vincristine has been associated with neurotoxicity and other serious adverse reactions, including seizures, peripheral neuropathy, syndrome of inappropriate antidiuretic hormone secretion, and paralytic ileus. Reserve azole antifungals, including posaconazole, for patients receiving a vinca alkaloid, including vincristine, who have no alternative antifungal treatment options [see Drug Interactions (7.10)].
5.8 Breakthrough Fungal Infections
Patients who have severe diarrhea or vomiting should be monitored closely for breakthrough fungal infections when receiving Posaconazole delayed-release tablets.
5.9 Venetoclax Toxicity
Concomitant administration of posaconazole, a strong CYP3A4 inhibitor, with venetoclax may increase venetoclax toxicities, including the risk of tumor lysis syndrome (TLS), neutropenia, and serious infections. In patients with CLL/SLL, administration of posaconazole during initiation and the ramp-up phase of venetoclax is contraindicated [see Contraindications (4.6)]. Refer to the venetoclax labeling for safety monitoring and dose reduction in the steady daily dosing phase in CLL/SLL patients.
For patients with acute myeloid leukemia (AML), dose reduction and safety monitoring are recommended across all dosing phases when coadministering posaconazole with venetoclax [see Drug Interactions (7.15)]. Refer to the venetoclax prescribing information for dosing instructions.
-
6 ADVERSE REACTIONS
The following serious and otherwise important adverse reactions are discussed in detail in another section of the labeling:
- Hypersensitivity [see Contraindications (4.1)]
- Arrhythmias and QT Prolongation [see Warnings and Precautions (5.2)]
- Hepatic Toxicity [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of Noxafil cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trial Experience in Adults
Clinical Trial Experience with Noxafil Injection and Noxafil Delayed-Release Tablets for the Treatment of Invasive Aspergillosis
The safety of Noxafil injection and Noxafil delayed-release tablet was assessed in a randomized, double-blind, active-controlled clinical study of Noxafil injection and Noxafil delayed-release tablets versus voriconazole for treatment of invasive aspergillosis (Aspergillosis Treatment Study). A total of 575 (288 in Noxafil arm, 287 in voriconazole arm) adult and pediatric patients 13 years of age and older with proven, probable or possible invasive aspergillosis were included. The median duration of treatment was 67 days for Noxafil injection or Noxafil delayed-release tablet and 64 days for voriconazole, with 55% to 60% of subjects starting treatment with the IV formulation of either drug. The median duration of the first instance of IV treatment (before switching to oral treatment or discontinuing or completing study treatment) was 9 days for both groups. Table 2 presents adverse reactions reported at an incidence of ≥10% in either one of the groups in Aspergillosis Treatment Study.
Adverse reactions leading to treatment discontinuation were reported for 33.9% of subjects. The most commonly reported adverse reactions (>2% of subjects) leading to treatment discontinuation were septic shock, respiratory failure, and bronchopulmonary aspergillosis in the Noxafil arm, and septic shock and acute myeloid leukemia in the voriconazole arm.
Table 2: Noxafil Invasive Aspergillosis Treatment Study: Adverse Reactions in at Least 10% of Subjects Treated with Noxafil Injection or Noxafil Delayed-Release Tablets System Organ Class Noxafil injection or tablet
(N = 288), n (%)Voriconazole injection or oral
(N = 287), n (%)Blood and lymphatic system disorders Anemia 25 (8.7) 29 (10.1) Febrile neutropenia 42 (14.6) 38 (13.2) Gastrointestinal disorders Abdominal pain 29 (10.1) 24 (8.4) Constipation 32 (11.1) 23 (8.0) Diarrhea 52 (18.1) 52 (18.1) Nausea 65 (22.6) 51 (17.8) Vomiting 52 (18.1) 39 (13.6) General disorders and administration site conditions Edema peripheral 32 (11.1) 24 (8.4) Pyrexia 81 (28.1) 72 (25.1) Infections and infestations Pneumonia 36 (12.5) 26 (9.1) Investigations Alanine aminotransferase increased 42 (14.6) 37 (12.9) Aspartate aminotransferase increased 38 (13.2) 36 (12.5) Blood alkaline phosphatase increased 21 (7.3) 29 (10.1) Metabolism and nutrition disorders Hypokalemia 82 (28.5) 49 (17.1) Hypomagnesemia 29 (10.1) 18 (6.3) Nervous system disorders Headache 35 (12.2) 25 (8.7) Respiratory, thoracic and mediastinal disorders Cough 30 (10.4) 24 (8.4) Epistaxis 32 (11.1) 17 (5.9) The most frequently reported adverse reactions in the Noxafil-treated group were pyrexia (28%), hypokalemia (28%), and nausea (23%).
Clinical Trial Experience with Noxafil Delayed-Release Tablets for Prophylaxis
The safety of Noxafil delayed-release tablets has been assessed in 230 patients in clinical trials. Patients were enrolled in a non-comparative pharmacokinetic and safety trial of Noxafil delayed-release tablets when given as antifungal prophylaxis (Noxafil Delayed-Release Tablet Study). Patients were immunocompromised with underlying conditions including hematological malignancy, neutropenia post-chemotherapy, GVHD, and post HSCT. This patient population was 62% male, had a mean age of 51 years (range 19-78 years, 17% of patients were ≥65 years of age), and were 93% white and 16% Hispanic. Posaconazole therapy was given for a median duration of 28 days. Twenty patients received 200 mg daily dose and 210 patients received 300 mg daily dose (following twice daily dosing on Day 1 in each cohort). Table 3 presents adverse reactions observed in patients treated with 300 mg daily dose at an incidence of ≥10% in Noxafil Delayed-Release Tablet Study.
Table 3: Noxafil Delayed-Release Tablet Study: Adverse Reactions in at Least 10% of Subjects Treated with 300 mg Daily Dose Body System Noxafil delayed-release tablet (300 mg)
n=210 (%)Subjects Reporting any Adverse Reaction 207 (99) Blood and Lymphatic System Disorder Anemia 22 (10) Thrombocytopenia 29 (14) Gastrointestinal Disorders Abdominal Pain 23 (11) Constipation 20 (10) Diarrhea 61 (29) Nausea 56 (27) Vomiting 28 (13) General Disorders and Administration Site Conditions Asthenia 20 (10) Chills 22 (10) Mucosal Inflammation 29 (14) Edema Peripheral 33 (16) Pyrexia 59 (28) Metabolism and Nutrition Disorders Hypokalemia 46 (22) Hypomagnesemia 20 (10) Nervous System Disorders Headache 30 (14) Respiratory, Thoracic and Mediastinal Disorders Cough 35 (17) Epistaxis 30 (14) Skin and Subcutaneous Tissue Disorders Rash 34 (16) Vascular Disorders Hypertension 23 (11) The most frequently reported adverse reactions (>25%) with Noxafil delayed-release tablets 300 mg once daily were diarrhea, pyrexia, and nausea.
The most common adverse reaction leading to discontinuation of Noxafil delayed-release tablets 300 mg once daily was nausea (2%).
Clinical Trial Safety Experience with Noxafil Oral Suspension
The safety of Noxafil oral suspension has been assessed in 1844 patients. This includes 605 patients in the active-controlled prophylaxis studies, 557 patients in the active-controlled OPC studies, 239 patients in refractory OPC studies, and 443 patients from other indications. This represents a heterogeneous population, including immunocompromised patients, e.g., patients with hematological malignancy, neutropenia post-chemotherapy, GVHD post HSCT, and HIV infection, as well as non-neutropenic patients. This patient population was 71% male, had a mean age of 42 years (range 8-84 years, 6% of patients were ≥65 years of age and 1% was <18 years of age), and were 64% white, 16% Hispanic, and 36% non-white (including 14% black). Noxafil therapy was given to 171 patients for ≥6 months, with 58 patients receiving Noxafil therapy for ≥12 months. Table 4 adverse reactions observed at an incidence of >10% in Noxafil prophylaxis studies. Table 5 presents adverse reactions observed at an incidence of at least 10% in the OPC/rOPC studies.
Prophylaxis of Aspergillus and Candida: In the 2 randomized, comparative prophylaxis studies (Noxafil Oral Suspension Studies 1 and 2), the safety of Noxafil oral suspension 200 mg three times a day was compared to fluconazole 400 mg once daily or itraconazole 200 mg twice a day in severely immunocompromised patients.
The most frequently reported adverse reactions (>30%) in the prophylaxis clinical trials were fever, diarrhea, and nausea.
The most common adverse reactions leading to discontinuation of Noxafil in the prophylaxis studies were associated with GI disorders, specifically, nausea (2%), vomiting (2%), and hepatic enzymes increased (2%).
Table 4: Noxafil Oral Suspension Study 1 and Study 2. Adverse Reactions in at Least 10% of the Noxafil Oral Suspension or Fluconazole Treatment Groups (Pooled Prophylaxis Safety Analysis) Body System Noxafil Oral Suspension
n=605 (%)Fluconazole
n=539 (%)Itraconazole
n=58 (%)- *
- Percentages of sex-specific adverse reactions are based on the number of males/females.
Subjects Reporting any Adverse Reaction 595 (98) 531 (99) 58 (100) Body as a Whole - General Disorders Fever 274 (45) 254 (47) 32 (55) Headache 171 (28) 141 (26) 23 (40) Rigors 122 (20) 87 (16) 17 (29) Fatigue 101 (17) 98 (18) 5 (9) Edema Legs 93 (15) 67 (12) 11 (19) Anorexia 92 (15) 94 (17) 16 (28) Dizziness 64 (11) 56 (10) 5 (9) Edema 54 (9) 68 (13) 8 (14) Weakness 51 (8) 52 (10) 2 (3) Cardiovascular Disorders, General Hypertension 106 (18) 88 (16) 3 (5) Hypotension 83 (14) 79 (15) 10 (17) Disorders of Blood and Lymphatic System Anemia 149 (25) 124 (23) 16 (28) Neutropenia 141 (23) 122 (23) 23 (40) Disorders of the Reproductive System and Breast Vaginal Hemorrhage* 24 (10) 20 (9) 3 (12) Gastrointestinal System Disorders Diarrhea 256 (42) 212 (39) 35 (60) Nausea 232 (38) 198 (37) 30 (52) Vomiting 174 (29) 173 (32) 24 (41) Abdominal Pain 161 (27) 147 (27) 21 (36) Constipation 126 (21) 94 (17) 10 (17) Dyspepsia 61 (10) 50 (9) 6 (10) Heart Rate and Rhythm Disorders Tachycardia 72 (12) 75 (14) 3 (5) Infection and Infestations Pharyngitis 71 (12) 60 (11) 12 (21) Liver and Biliary System Disorders Bilirubinemia 59 (10) 51 (9) 11 (19) Metabolic and Nutritional Disorders Hypokalemia 181 (30) 142 (26) 30 (52) Hypomagnesemia 110 (18) 84 (16) 11 (19) Hyperglycemia 68 (11) 76 (14) 2 (3) Hypocalcemia 56 (9) 55 (10) 5 (9) Musculoskeletal System Disorders Musculoskeletal Pain 95 (16) 82 (15) 9 (16) Arthralgia 69 (11) 67 (12) 5 (9) Back Pain 63 (10) 66 (12) 4 (7) Platelet, Bleeding and Clotting Disorders Thrombocytopenia 175 (29) 146 (27) 20 (34) Petechiae 64 (11) 54 (10) 9 (16) Psychiatric Disorders Insomnia 103 (17) 92 (17) 11 (19) Respiratory System Disorders Coughing 146 (24) 130 (24) 14 (24) Dyspnea 121 (20) 116 (22) 15 (26) Epistaxis 82 (14) 73 (14) 12 (21) Skin and Subcutaneous Tissue Disorders Rash 113 (19) 96 (18) 25 (43) Pruritus 69 (11) 62 (12) 11 (19) HIV Infected Subjects with OPC: In 2 randomized comparative studies in OPC, the safety of Noxafil oral suspension at a dose of less than or equal to 400 mg once daily in 557 HIV-infected patients was compared to the safety of fluconazole in 262 HIV-infected patients at a dose of 100 mg once daily.
An additional 239 HIV-infected patients with refractory OPC received Noxafil oral suspension in 2 non-comparative trials for refractory OPC (rOPC). Of these subjects, 149 received the 800-mg/day dose and the remainder received the less than or equal to 400 mg once daily dose.
In the OPC/rOPC studies, the most common adverse reactions were fever, diarrhea, nausea, headache, vomiting, and coughing.
The most common adverse reactions that led to treatment discontinuation of Noxafil in the Controlled OPC Pool included respiratory impairment (1%) and pneumonia (1%). In the refractory OPC pool, the most common adverse reactions that led to treatment discontinuation of Noxafil were AIDS (7%) and respiratory impairment (3%).
Table 5: Adverse Reactions in at Least 10% of the Treated Population in OPC Studies with Noxafil Oral Suspension Body System Number (%) of Subjects Controlled OPC Pool Refractory OPC Pool Noxafil Oral Suspension Fluconazole Noxafil Oral Suspension n=557 n=262 n=239 OPC=oropharyngeal candidiasis - *
- Number of subjects reporting adverse reactions at least once during the study, without regard to relationship to treatment. Subjects may have reported more than 1 event.
Subjects Reporting any Adverse Reaction* 356 (64) 175 (67) 221 (92) Body as a Whole – General Disorders Fever 34 (6) 22 (8) 82 (34) Headache 44 (8) 23 (9) 47 (20) Anorexia 10 (2) 4 (2) 46 (19) Fatigue 18 (3) 12 (5) 31 (13) Asthenia 9 (2) 5 (2) 31 (13) Rigors 2 (<1) 4 (2) 29 (12) Pain 4 (1) 2 (1) 27 (11) Disorders of Blood and Lymphatic System Neutropenia 21 (4) 8 (3) 39 (16) Anemia 11 (2) 5 (2) 34 (14) Gastrointestinal System Disorders Diarrhea 58 (10) 34 (13) 70 (29) Nausea 48 (9) 30 (11) 70 (29) Vomiting 37 (7) 18 (7) 67 (28) Abdominal Pain 27 (5) 17 (6) 43 (18) Infection and Infestations Candidiasis, Oral 3 (1) 1 (<1) 28 (12) Herpes Simplex 16 (3) 8 (3) 26 (11) Pneumonia 17 (3) 6 (2) 25 (10) Metabolic and Nutritional Disorders Weight Decrease 4 (1) 2 (1) 33 (14) Dehydration 4 (1) 7 (3) 27 (11) Psychiatric Disorders Insomnia 8 (1) 3 (1) 39 (16) Respiratory System Disorders Coughing 18 (3) 11 (4) 60 (25) Dyspnea 8 (1) 8 (3) 28 (12) Skin and Subcutaneous Tissue Disorders Rash 15 (3) 10 (4) 36 (15) Sweating Increased 13 (2) 5 (2) 23 (10) Adverse reactions were reported more frequently in the pool of patients with refractory OPC. Among these highly immunocompromised patients with advanced HIV disease, serious adverse reactions (SARs) were reported in 55% (132/239). The most commonly reported SARs were fever (13%) and neutropenia (10%).
Other clinically significant adverse reactions reported in less than 5% of patients in clinical trials of Noxafil are listed below:
- Blood and lymphatic system disorders: hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, neutropenia aggravated
- Endocrine disorders: adrenal insufficiency
- Nervous system disorders: paresthesia
- Immune system disorders: allergic reaction [see Contraindications (4.1)]
- Cardiac disorders: torsades de pointes [see Warnings and Precautions (5.2)]
- Vascular disorders: pulmonary embolism
- Gastrointestinal disorders: pancreatitis
- Liver and Biliary System Disorders: hepatic enzymes increased, hepatic function abnormal, hepatitis, hepatomegaly, jaundice
- Renal & Urinary System Disorders: renal failure acute
Clinical Laboratory Values: In healthy volunteers and patients, elevation of liver test values did not appear to be associated with higher plasma concentrations of posaconazole.
For the prophylaxis studies, the number of patients with changes in liver tests from Common Toxicity Criteria (CTC) Grade 0, 1, or 2 at baseline to Grade 3 or 4 during the study is presented in Table 6.
Table 6: Noxafil Oral Suspension Study 1 and Study 2. Changes in Liver Test Results from CTC Grade 0, 1, or 2 at Baseline to Grade 3 or 4 Number (%) of Patients with Change* CTC = Common Toxicity Criteria; AST= Aspartate Aminotransferase; ALT= Alanine Aminotransferase. - *
- Change from Grade 0 to 2 at baseline to Grade 3 or 4 during the study. These data are presented in the form X/Y, where X represents the number of patients who met the criterion as indicated, and Y represents the number of patients who had a baseline observation and at least one post-baseline observation.
Noxafil Oral Suspension Study 1 Laboratory Parameter Noxafil Oral Suspension
n=301Fluconazole
n=299AST 11/266 (4) 13/266 (5) ALT 47/271 (17) 39/272 (14) Bilirubin 24/271 (9) 20/275 (7) Alkaline Phosphatase 9/271 (3) 8/271 (3) Noxafil Oral Suspension Study 2 Laboratory Parameter Noxafil Oral Suspension
(n=304)Fluconazole/Itraconazole
(n=298)AST 9/286 (3) 5/280 (2) ALT 18/289 (6) 13/284 (5) Bilirubin 20/290 (7) 25/285 (9) Alkaline Phosphatase 4/281 (1) 1/276 (<1) The number of patients treated for OPC with clinically significant liver test abnormalities at any time during the studies is provided in Table 7 (liver test abnormalities were present in some of these patients prior to initiation of the study drug).
Table 7: Noxafil Oral Suspension Studies: Clinically Significant Laboratory Test Abnormalities without Regard to Baseline Value Laboratory Test Controlled Refractory Noxafil Oral Suspension Fluconazole Noxafil Oral Suspension n=557 (%) n=262 (%) n=239 (%) ALT= Alanine Aminotransferase; AST= Aspartate Aminotransferase. ALT > 3.0 × ULN 16/537 (3) 13/254 (5) 25/226 (11) AST > 3.0 × ULN 33/537 (6) 26/254 (10) 39/223 (17) Total Bilirubin > 1.5 × ULN 15/536 (3) 5/254 (2) 9/197 (5) Alkaline Phosphatase > 3.0 × ULN 17/535 (3) 15/253 (6) 24/190 (13) The number of patients treated for invasive aspergillosis with clinically significant liver test abnormalities at any time during the Aspergillosis Treatment Study is provided in Table 8. Liver test abnormalities present prior to the initiation of study drug included ALT (22%), AST (13%), and bilirubin (13%).
Table 8: Aspergillosis Treatment Study: Changes in Liver Test Results from CTC Grade 0, 1, or 2 at Baseline to Grade 3 or 4 Number (%) of Patients with Change* Laboratory Parameter Noxafil
n/N (%)Voriconazole
n/N (%)N=Number of subjects for a given laboratory test with a baseline value of CTC Grade 0, 1, or 2 and at least one post-baseline value.
CTC = Common Toxicity Criteria; AST= Aspartate Aminotransferase; ALT= Alanine Aminotransferase.- *
- Change from Grade 0 to 2 at baseline to Grade 3 or 4 during the study. These data are presented in the form n/N, where n represents the number of patients who met the criterion as indicated, and N represents the number of patients who had a baseline observation and at least one post-baseline observation.
AST 22/281 (8) 21/285 (7) ALT 29/281(10) 23/282 (8) Bilirubin 26/280 (9) 25/284 (9) Alkaline Phosphatase 12/282 (4) 20/284 (7) Clinical Trial Experience in Pediatrics
Clinical Trial Experience in Pediatric Patients (2 to less than 18 Years of Age)
The safety of Noxafil injection and Noxafil PowderMix for delayed-release oral suspension for prophylaxis of invasive fungal infections has been assessed in an open label uncontrolled dose-ranging PK and safety study (Noxafil injection/ Noxafil PowderMix for delayed-release oral suspension Pediatric Study 1, NCT02452034); hereinafter referred to as Noxafil Pediatric Study) in 115 immunocompromised pediatric patients 2 to less than 18 years of age with known or expected neutropenia. Noxafil injection and Noxafil PowderMix for delayed-release oral suspension was administered at daily doses of up to 6 mg/kg (twice daily on day 1) in three dose cohorts. All 115 subjects initially received Noxafil injection for at least 7 days, and 63 subjects were transitioned to Noxafil PowderMix for delayed-release oral suspension. The mean overall treatment duration for all treated subjects was 20.6 days with 14.3 days (range: 1 to 28 days) on Noxafil injection and 11.6 days (range: 2 to 18 days) on Noxafil PowderMix for delayed-release oral suspension.
Reported adverse reaction profile of Noxafil in pediatric patients was consistent with the safety profile of Noxafil in adults.
6.2 Postmarketing Experience
The following adverse reaction has been identified during the post-approval use of posaconazole. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency.
Endocrine Disorders: Pseudoaldosteronism
-
7 DRUG INTERACTIONS
Posaconazole is primarily metabolized via UDP glucuronosyltransferase and is a substrate of p-glycoprotein (P-gp) efflux. Therefore, inhibitors or inducers of these clearance pathways may affect posaconazole plasma concentrations. Coadministration of drugs that can decrease the plasma concentrations of posaconazole should generally be avoided unless the benefit outweighs the risk. If such drugs are necessary, patients should be monitored closely for breakthrough fungal infections.
Posaconazole is also a strong inhibitor of CYP3A4. Therefore, plasma concentrations of drugs predominantly metabolized by CYP3A4 may be increased by posaconazole [see Clinical Pharmacology (12.3)].
The following information was derived from data with Noxafil oral suspension or early tablet formulation unless otherwise noted. All drug interactions with Posaconazole oral suspension, except for those that affect the absorption of posaconazole (via gastric pH and motility), are considered relevant to Posaconazole injection, Posaconazole delayed-release tablet, and Posaconazole PowderMix for delayed-release oral suspension as well [see Drug Interactions (7.9) and (7.13)].
7.1 Immunosuppressants Metabolized by CYP3A4
Sirolimus: Concomitant administration of posaconazole with sirolimus increases the sirolimus blood concentrations by approximately 9-fold and can result in sirolimus toxicity. Therefore, posaconazole is contraindicated with sirolimus [see Contraindications (4.2) and Clinical Pharmacology (12.3)].
Tacrolimus: Posaconazole has been shown to significantly increase the Cmax and AUC of tacrolimus. At initiation of posaconazole treatment, reduce the tacrolimus dose to approximately one-third of the original dose. Frequent monitoring of tacrolimus whole blood trough concentrations should be performed during and at discontinuation of posaconazole treatment and the tacrolimus dose adjusted accordingly [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
Cyclosporine: Posaconazole has been shown to increase cyclosporine whole blood concentrations in heart transplant patients upon initiation of posaconazole treatment. It is recommended to reduce cyclosporine dose to approximately three-fourths of the original dose upon initiation of posaconazole treatment. Frequent monitoring of cyclosporine whole blood trough concentrations should be performed during and at discontinuation of posaconazole treatment and the cyclosporine dose adjusted accordingly [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
7.2 CYP3A4 Substrates
Concomitant administration of posaconazole with CYP3A4 substrates such as pimozide and quinidine may result in increased plasma concentrations of these drugs, leading to QTc prolongation and cases of torsades de pointes. Therefore, posaconazole is contraindicated with these drugs [see Contraindications (4.3) and Warnings and Precautions (5.2)].
7.3 HMG-CoA Reductase Inhibitors (Statins) Primarily Metabolized Through CYP3A4
Concomitant administration of posaconazole with simvastatin increases the simvastatin plasma concentrations by approximately 10-fold. Therefore, posaconazole is contraindicated with HMG-CoA reductase inhibitors primarily metabolized through CYP3A4 [see Contraindications (4.4) and Clinical Pharmacology (12.3)].
7.4 Ergot Alkaloids
Most of the ergot alkaloids are substrates of CYP3A4. Posaconazole may increase the plasma concentrations of ergot alkaloids (ergotamine and dihydroergotamine) which may lead to ergotism. Therefore, posaconazole is contraindicated with ergot alkaloids [see Contraindications (4.5)].
7.5 Benzodiazepines Metabolized by CYP3A4
Concomitant administration of posaconazole with midazolam increases the midazolam plasma concentrations by approximately 5-fold. Increased plasma midazolam concentrations could potentiate and prolong hypnotic and sedative effects. Concomitant use of posaconazole and other benzodiazepines metabolized by CYP3A4 (e.g., alprazolam, triazolam) could result in increased plasma concentrations of these benzodiazepines. Patients must be monitored closely for adverse effects associated with high plasma concentrations of benzodiazepines metabolized by CYP3A4 and benzodiazepine receptor antagonists must be available to reverse these effects [see Warnings and Precautions (5.6) and Clinical Pharmacology (12.3)].
7.6 Anti-HIV Drugs
Efavirenz: Efavirenz induces UDP-glucuronidase and significantly decreases posaconazole plasma concentrations [see Clinical Pharmacology (12.3)]. It is recommended to avoid concomitant use of efavirenz with posaconazole unless the benefit outweighs the risks.
Ritonavir and Atazanavir: Ritonavir and atazanavir are metabolized by CYP3A4 and posaconazole increases plasma concentrations of these drugs [see Clinical Pharmacology (12.3)]. Frequent monitoring of adverse effects and toxicity of ritonavir and atazanavir should be performed during coadministration with posaconazole.
Fosamprenavir: Combining fosamprenavir with posaconazole may lead to decreased posaconazole plasma concentrations. If concomitant administration is required, close monitoring for breakthrough fungal infections is recommended [see Clinical Pharmacology (12.3)].
7.7 Rifabutin
Rifabutin induces UDP-glucuronidase and decreases posaconazole plasma concentrations. Rifabutin is also metabolized by CYP3A4. Therefore, coadministration of rifabutin with posaconazole increases rifabutin plasma concentrations [see Clinical Pharmacology (12.3)]. Concomitant use of posaconazole and rifabutin should be avoided unless the benefit to the patient outweighs the risk. However, if concomitant administration is required, close monitoring for breakthrough fungal infections as well as frequent monitoring of full blood counts and adverse reactions due to increased rifabutin plasma concentrations (e.g., uveitis, leukopenia) are recommended.
7.8 Phenytoin
Phenytoin induces UDP-glucuronidase and decreases posaconazole plasma concentrations. Phenytoin is also metabolized by CYP3A4. Therefore, coadministration of phenytoin with posaconazole increases phenytoin plasma concentrations [see Clinical Pharmacology (12.3)]. Concomitant use of posaconazole and phenytoin should be avoided unless the benefit to the patient outweighs the risk. However, if concomitant administration is required, close monitoring for breakthrough fungal infections is recommended and frequent monitoring of phenytoin concentrations should be performed while coadministered with posaconazole and dose reduction of phenytoin should be considered.
7.9 Gastric Acid Suppressors/Neutralizers
Posaconazole Delayed-Release Tablet:
No clinically relevant effects on the pharmacokinetics of posaconazole were observed when Posaconazole delayed-release tablets are concomitantly used with antacids, H2-receptor antagonists and proton pump inhibitors [see Clinical Pharmacology (12.3)]. No dosage adjustment of Posaconazole delayed-release tablets is required when Posaconazole delayed-release tablets are concomitantly used with antacids, H2-receptor antagonists and proton pump inhibitors.
7.10 Vinca Alkaloids
Most of the vinca alkaloids (e.g., vincristine and vinblastine) are substrates of CYP3A4. Concomitant administration of azole antifungals, including posaconazole, with vincristine has been associated with serious adverse reactions [see Warnings and Precautions (5.7)]. Posaconazole may increase the plasma concentrations of vinca alkaloids which may lead to neurotoxicity and other serious adverse reactions. Therefore, reserve azole antifungals, including posaconazole, for patients receiving a vinca alkaloid, including vincristine, who have no alternative antifungal treatment options.
7.11 Calcium Channel Blockers Metabolized by CYP3A4
Posaconazole may increase the plasma concentrations of calcium channel blockers metabolized by CYP3A4 (e.g., verapamil, diltiazem, nifedipine, nicardipine, felodipine). Frequent monitoring for adverse reactions and toxicity related to calcium channel blockers is recommended during coadministration. Dose reduction of calcium channel blockers may be needed.
7.12 Digoxin
Increased plasma concentrations of digoxin have been reported in patients receiving digoxin and posaconazole. Therefore, monitoring of digoxin plasma concentrations is recommended during coadministration.
7.13 Gastrointestinal Motility Agents
Posaconazole Delayed-Release Tablet:
Concomitant administration of metoclopramide with Posaconazole delayed-release tablets did not affect the pharmacokinetics of posaconazole [see Clinical Pharmacology (12.3)]. No dosage adjustment of Posaconazole delayed-release tablets is required when given concomitantly with metoclopramide.
7.14 Glipizide
Although no dosage adjustment of glipizide is required, it is recommended to monitor glucose concentrations when posaconazole and glipizide are concomitantly used.
7.15 Venetoclax
Concomitant use of venetoclax (a CYP3A4 substrate) with posaconazole increases venetoclax Cmax and AUC0-INF, which may increase venetoclax toxicities [see Contraindications (4.6), Warnings and Precautions (5.9)]. Refer to the venetoclax prescribing information for more information on the dosing instructions and the extent of increase in venetoclax exposure.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal data, posaconazole may cause fetal harm when administered to pregnant women. Available data for use of Noxafil in pregnant women are insufficient to establish a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. In animal reproduction studies, skeletal malformations (cranial malformations and missing ribs) and maternal toxicity (reduced food consumption and reduced body weight gain) were observed when posaconazole was dosed orally to pregnant rats during organogenesis at doses ≥1.4 times the 400 mg twice daily oral suspension regimen based on steady-state plasma concentrations of Noxafil in healthy volunteers. In pregnant rabbits dosed orally during organogenesis, increased resorptions, reduced litter size, and reduced body weight gain of females were seen at doses 5 times the exposure achieved with the 400 mg twice daily oral suspension regimen. Doses of ≥ 3 times the clinical exposure caused an increase in resorptions in these rabbits (see Data). Based on animal data, advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Posaconazole resulted in maternal toxicity (reduced food consumption and reduced body weight gain) and skeletal malformations (cranial malformations and missing ribs) when given orally to pregnant rats during organogenesis (Gestational Days 6 through 15) at doses ≥27 mg/kg (≥1.4 times the 400 mg twice daily oral suspension regimen based on steady-state plasma concentrations of drug in healthy volunteers). The no-effect dose for malformations and maternal toxicity in rats was 9 mg/kg, which is 0.7 times the exposure achieved with the 400 mg twice daily oral suspension regimen. No malformations were seen in rabbits dosed during organogenesis (Gestational Days 7 through 19) at doses up to 80 mg/kg (5 times the exposure achieved with the 400 mg twice daily oral suspension regimen). In the rabbit, the no-effect dose was 20 mg/kg, while high doses of 40 mg/kg and 80 mg/kg (3 or 5 times the clinical exposure) caused an increase in resorptions. In rabbits dosed at 80 mg/kg, a reduction in body weight gain of females and a reduction in litter size were seen.
8.2 Lactation
Risk Summary
There are no data on the presence of posaconazole in human milk, the effects on the breastfed infant, or the effects on milk production. Posaconazole is excreted in the milk of lactating rats. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for posaconazole and any potential adverse effects on the breastfed child from posaconazole or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of Posaconazole oral suspension and Posaconazole delayed-release tablets for the prophylaxis of invasive Aspergillus and Candida infections have been established in pediatric patients aged 2 and older who are at high risk of developing these infections due to being severely immunocompromised, such as HSCT recipients with GVHD or those with hematologic malignancies with prolonged neutropenia from chemotherapy.
The safety and effectiveness of Posaconazole injection and Posaconazole delayed-release tablets for the treatment of invasive aspergillosis have been established in pediatric patients aged 13 years and older.
Use of posaconazole in these age groups is supported by evidence from adequate and well-controlled studies of Noxafil in adults and pediatric patients and additional pharmacokinetic and safety data in pediatric patients 2 years of age and older [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)]. The safety and effectiveness of posaconazole have not been established in pediatric patients younger than 2 years of age.
8.5 Geriatric Use
No overall differences in the safety of Noxafil delayed-release tablets and Noxafil oral suspension were observed between geriatric patients and younger adult patients in the clinical trials; therefore, no dosage adjustment is recommended for any formulation of posaconazole in geriatric patients. No clinically meaningful differences in the pharmacokinetics of Noxafil were observed in geriatric patients compared to younger adult patients during clinical trials [see Clinical Pharmacology (12.3)].
Of the 230 patients treated with Noxafil delayed-release tablets, 38 (17%) were greater than 65 years of age.
Of the 605 patients randomized to Noxafil oral suspension in Noxafil Oral Suspension Study 1 and Study 2, 63 (10%) were ≥65 years of age. In addition, 48 patients treated with greater than or equal to 800-mg/day Noxafil oral suspension in another indication were ≥65 years of age. Of the 288 patients randomized to Noxafil injection/Noxafil delayed-release tablets in the Aspergillosis Treatment Study, 85 (29%) were ≥65 years of age.
No overall differences in the pharmacokinetics and safety were observed between elderly and young subjects during clinical trials, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Following single-dose administration of 400 mg of the Noxafil oral suspension, there was no significant effect of mild (eGFR: 50-80 mL/min/1.73 m2, n=6) or moderate (eGFR: 20-49 mL/min/1.73 m2, n=6) renal impairment on posaconazole pharmacokinetics; therefore, no dose adjustment is required in patients with mild to moderate renal impairment. In subjects with severe renal impairment (eGFR: <20 mL/min/1.73 m2), the mean plasma exposure (AUC) was similar to that in patients with normal renal function (eGFR: >80 mL/min/1.73 m2); however, the range of the AUC estimates was highly variable (CV=96%) in these subjects with severe renal impairment as compared to that in the other renal impairment groups (CV<40%). Due to the variability in exposure, patients with severe renal impairment should be monitored closely for breakthrough fungal infections [see Dosage and Administration (2)]. Similar recommendations apply to Posaconazole delayed-release tablets; however, a specific study has not been conducted with the Posaconazole delayed-release tablets.
8.7 Hepatic Impairment
After a single oral dose of Noxafil oral suspension 400 mg, the mean AUC was 43%, 27%, and 21% higher in subjects with mild (Child-Pugh Class A, N=6), moderate (Child-Pugh Class B, N=6), or severe (Child-Pugh Class C, N=6) hepatic impairment, respectively, compared to subjects with normal hepatic function (N=18). Compared to subjects with normal hepatic function, the mean Cmax was 1% higher, 40% higher, and 34% lower in subjects with mild, moderate, or severe hepatic impairment, respectively. The mean apparent oral clearance (CL/F) was reduced by 18%, 36%, and 28% in subjects with mild, moderate, or severe hepatic impairment, respectively, compared to subjects with normal hepatic function. The elimination half-life (t½) was 27 hours, 39 hours, 27 hours, and 43 hours in subjects with normal hepatic function and mild, moderate, or severe hepatic impairment, respectively.
It is recommended that no dose adjustment of posaconazole is needed in patients with mild to severe hepatic impairment (Child-Pugh Class A, B, or C) [see Dosage and Administration (2) and Warnings and Precautions (5.4)]. Similar recommendations apply to Posaconazole delayed-release tablets; however, a specific study has not been conducted with the Posaconazole delayed-release tablets.
8.8 Gender
The pharmacokinetics of posaconazole are comparable in males and females. No adjustment in the dosage of posaconazole is necessary based on gender.
8.9 Race
The pharmacokinetic profile of posaconazole is not significantly affected by race. No adjustment in the dosage of posaconazole is necessary based on race.
8.10 Weight
Pharmacokinetic modeling suggests that patients weighing greater than 120 kg may have lower posaconazole plasma drug exposure. It is, therefore, suggested to closely monitor for breakthrough fungal infections particularly when using Posaconazole oral suspension [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
There is no experience with overdosage of Posaconazole delayed-release tablets.
During the clinical trials, some patients received Noxafil oral suspension up to 1600 mg/day with no adverse reactions noted that were different from the lower doses. In addition, accidental overdose was noted in one patient who took 1200 mg twice daily Noxafil oral suspension for 3 days. No related adverse reactions were noted by the investigator.
Posaconazole is not removed by hemodialysis.
-
11 DESCRIPTION
Posaconazole is an azole antifungal agent available as delayed-release tablet or suspension for oral administration.
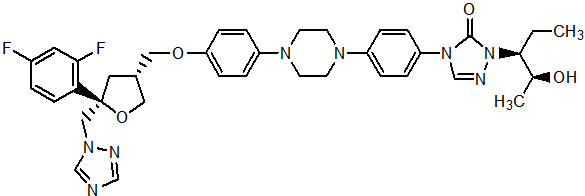
Posaconazole is designated chemically as 4-[4-[4-[4-[[ (3R,5R)-5- (2,4-difluorophenyl)tetrahydro-5- (1H-1,2,4-triazol-1-ylmethyl)-3-furanyl]methoxy]phenyl]-1-piperazinyl]phenyl]-2-[(1S,2S)-1-ethyl-2-hydroxypropyl]-2,4-dihydro-3H-1,2,4-triazol-3-one with an empirical formula of C37H42F2N8O4 and a molecular weight of 700.8. The chemical structure is:
Posaconazole Delayed-Release Tablets
Posaconazole is a white powder with a low aqueous solubility.
Posaconazole delayed-release tablet is a yellow, coated, oblong tablet containing 100 mg of posaconazole. Each delayed-release tablet contains the inactive ingredients: croscarmellose sodium, hydroxypropylcellulose, hypromellose acetate succinate, iron oxide yellow, Macrogol/PEG 3350, magnesium stearate, microcrystalline cellulose, polyvinyl alcohol partially hydrolyzed, silicon dioxide, talc, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Posaconazole is an azole antifungal agent [see Clinical Pharmacology (12.4)].
12.2 Pharmacodynamics
Exposure Response Relationship Prophylaxis: In clinical studies of neutropenic patients who were receiving cytotoxic chemotherapy for acute myelogenous leukemia (AML) or myelodysplastic syndromes (MDS) or hematopoietic stem cell transplant (HSCT) recipients with Graft versus Host Disease (GVHD), a wide range of plasma exposures to posaconazole was noted following administration of Noxafil oral suspension. A pharmacokinetic-pharmacodynamic analysis of patient data revealed an apparent association between average posaconazole concentrations (Cavg) and prophylactic efficacy (Table 9). A lower Cavg may be associated with an increased risk of treatment failure, defined as treatment discontinuation, use of empiric systemic antifungal therapy (SAF), or occurrence of breakthrough invasive fungal infections.
Table 9: Noxafil Oral Suspension Exposure Analysis (Cavg) in Prophylaxis Trials Prophylaxis in AML/MDS* Prophylaxis in GVHD† Cavg Range (ng/mL) Treatment Failure‡ (%) Cavg Range (ng/mL) Treatment Failure‡ (%) Cavg = the average posaconazole concentration when measured at steady state Quartile 1 90-322 54.7 22-557 44.4 Quartile 2 322-490 37.0 557-915 20.6 Quartile 3 490-734 46.8 915-1563 17.5 Quartile 4 734-2200 27.8 1563-3650 17.5 Exposure Response Relationship Treatment of Invasive Aspergillosis:
Across a range of posaconazole plasma minimum concentrations (Cmin, range: 244 to 5663 ng/mL) following administration of Noxafil injection and Noxafil delayed-release tablets in patients treated for invasive aspergillosis in Aspergillosis Treatment Study, there was no association between posaconazole Cmin and treatment efficacy [see Clinical Pharmacology (12.3) and Clinical Studies (14.1)]. Similarly, across a range of population pharmacokinetic model-predicted steady-state plasma average concentrations (Cavg, range: 589 to 6315 ng/mL), there was no association between posaconazole Cavg and treatment efficacy.
12.3 Pharmacokinetics
General Pharmacokinetic Characteristics
Posaconazole Delayed-Release Tablets
Noxafil delayed-release tablets exhibit dose proportional pharmacokinetics after single and multiple dosing up to 300 mg. The mean pharmacokinetic parameters of posaconazole at steady state following administration of Noxafil delayed-release tablets 300 mg twice daily on Day 1, then 300 mg once daily thereafter in healthy volunteers and in neutropenic patients who are receiving cytotoxic chemotherapy for AML or MDS or HSCT recipients with GVHD are shown in Table 10.
Table 10: Arithmetic Mean (%CV) of Steady State PK Parameters in Healthy Volunteers and Patients Following Administration of Noxafil Delayed-Release Tablets (300 mg)* N AUC0-24 hr
(ng∙hr/mL)Cav†
(ng/mL)Cmax
(ng/mL)Cmin
(ng/mL)Tmax‡
(hr)t1/2
(hr)CL/F
(L/hr)CV = coefficient of variation expressed as a percentage (%CV); AUC0-T = Area under the plasma concentration-time curve from time zero to 24 hr; Cmax = maximum observed concentration; Cmin = minimum observed plasma concentration; Tmax = time of maximum observed concentration; t½ = terminal phase half-life; CL/F = Apparent total body clearance Healthy Volunteers 12 51618
(25)2151
(25)2764
(21)1785
(29)4
(3-6)31
(40)7.5
(26)Patients 50 37900
(42)1580
(42)2090
(38)1310
(50)4 (1.3-8.3) - 9.39
(45)Posaconazole Oral Suspension
Dose-proportional increases in plasma exposure (AUC) to Noxafil oral suspension were observed following single oral doses from 50 mg to 800 mg and following multiple-dose administration from 50 mg twice daily to 400 mg twice daily in healthy volunteers. No further increases in exposure were observed when the dose of the oral suspension increased from 400 mg twice daily to 600 mg twice daily in febrile neutropenic patients or those with refractory invasive fungal infections.
The mean (%CV) [min-max] Noxafil oral suspension average steady-state plasma concentrations (Cavg) and steady-state pharmacokinetic parameters in patients following administration of 200 mg three times a day and 400 mg twice daily of the oral suspension are provided in Table 11.
Table 11: The Mean (%CV) [min-max] Posaconazole Steady-State Pharmacokinetic Parameters in Patients Following Oral Administration of Noxafil Oral Suspension 200 mg Three Times a Day and 400 mg Twice Daily Dose* Cavg (ng/mL) AUC† (ng∙hr/mL) CL/F (L/hr) V/F (L) t½ (hr) Cavg = the average posaconazole concentration when measured at steady state - *
- Oral suspension administration
- †
- AUC (0-24 hr) for 200 mg three times a day and AUC (0-12 hr) for 400 mg twice daily
- ‡
- HSCT recipients with GVHD
- §
- Not done
- ¶
- Neutropenic patients who were receiving cytotoxic chemotherapy for acute myelogenous leukemia or myelodysplastic syndromes
- #
- Febrile neutropenic patients or patients with refractory invasive fungal infections, Cavg n=24
The variability in average plasma posaconazole concentrations in patients was relatively higher than that in healthy subjects.
200 mg three times a day‡ (n=252) 1103 (67)
[21.5-3650]ND§ ND§ ND§ ND§ 200 mg three times a day¶ (n=215) 583 (65)
[89.7-2200]15,900 (62)
[4100-56,100]51.2 (54)
[10.7-146]2425 (39)
[828-5702]37.2 (39)
[19.1-148]400 mg twice daily# (n=23) 723 (86)
[6.70-2256]9093 (80)
[1564-26,794]76.1 (78)
[14.9-256]3088 (84)
[407-13,140]31.7 (42)
[12.4-67.3]Absorption:
Posaconazole Delayed-Release Tablets
When given orally in healthy volunteers, Noxafil delayed-release tablets are absorbed with a median Tmax of 4 to 5 hours. Steady-state plasma concentrations are attained by Day 6 at the 300 mg dose (once daily after twice daily loading dose at Day 1). The absolute bioavailability of the oral delayed-release tablet is approximately 54% under fasted conditions. The Cmax and AUC of posaconazole following administration of Noxafil delayed-release tablets is increased 16% and 51%, respectively, when given with a high fat meal compared to a fasted state (see Table 12).
Table 12: Statistical Comparison of Plasma Pharmacokinetics of Posaconazole Following Single Oral Dose Administration of 300 mg Noxafil Delayed-Release Tablet to Healthy Subjects under Fasting and Fed Conditions Fasting Conditions Fed Conditions
(High Fat Meal)*Fed/Fasting Pharmacokinetic Parameter N Mean (%CV) N Mean (%CV) GMR (90% CI) GMR=Geometric least-squares mean ratio; CI=Confidence interval Cmax (ng/mL) 14 935 (34) 16 1060 (25) 1.16 (0.96, 1.41) AUC0-72hr (hr∙ng/mL) 14 26200 (28) 16 38400 (18) 1.51 (1.33, 1.72) Tmax† (hr) 14 5.00
(3.00, 8.00)16 6.00
(5.00, 24.00)N/A Concomitant administration of Noxafil delayed-release tablets with drugs affecting gastric pH or gastric motility did not demonstrate any significant effects on posaconazole pharmacokinetic exposure (see Table 13).
Table 13: The Effect of Concomitant Medications that Affect the Gastric pH and Gastric Motility on the Pharmacokinetics of Noxafil Delayed-Release Tablets in Healthy Volunteers Coadministered Drug Administration Arms Change in Cmax
(ratio estimate*; 90% CI of the ratio estimate)Change in AUC0-last
(ratio estimate*; 90% CI of the ratio estimate)- *
- Ratio Estimate is the ratio of coadministered drug plus Noxafil to Noxafil alone for Cmax or AUC0-last.
Mylanta® Ultimate strength liquid (Increase in gastric pH) 25.4 meq/5 mL, 20 mL ↑6%
(1.06; 0.90 -1.26)↑↑4%
(1.04; 0.90 -1.20)Ranitidine (Zantac®) (Alteration in gastric pH) 150 mg (morning dose of 150 mg Ranitidine twice daily) ↑4%
(1.04; 0.88 -1.23)↑↓3%
(0.97; 0.84 -1.12)Esomeprazole (Nexium®) (Increase in gastric pH) 40 mg (every morning for 5 days, Day -4 to 1) ↑2%
(1.02; 0.88-1.17)↑↑5%
(1.05; 0.89 -1.24)Metoclopramide (Reglan®) (Increase in gastric motility) 15 mg four times daily for 2 days (Day -1 and 1) ↓14%
(0.86, 0.73,1.02)↓7%
(0.93, 0.803,1.07)Posaconazole Oral Suspension
Noxafil oral suspension is absorbed with a median Tmax of ~3 to 5 hours. Steady-state plasma concentrations are attained at 7 to 10 days following multiple-dose administration.
Following single-dose administration of 200 mg, the mean AUC and Cmax of posaconazole are approximately 3-times higher when the oral suspension is administered with a nonfat meal and approximately 4-times higher when administered with a high-fat meal (~50 gm fat) relative to the fasted state. Following single-dose administration of Noxafil oral suspension 400 mg, the mean AUC and Cmax of posaconazole are approximately 3-times higher when administered with a liquid nutritional supplement (14 gm fat) relative to the fasted state (see Table 14). In addition, the effects of varying gastric administration conditions on the Cmax and AUC of Noxafil oral suspension in healthy volunteers have been investigated and are shown in Table 15.
In order to assure attainment of adequate plasma concentrations, it is recommended to administer posaconazole oral suspension during or immediately following a full meal. In patients who cannot eat a full meal, posaconazole oral suspension should be taken with a liquid nutritional supplement or an acidic carbonated beverage (e.g., ginger ale).
Table 14: The Mean (%CV) [min-max] Posaconazole Pharmacokinetic Parameters Following Single-Dose Noxafil Oral Suspension Administration of 200 mg and 400 mg Under Fed and Fasted Conditions Dose (mg) Cmax
(ng/mL)Tmax*
(hr)AUC (I)
(ng∙hr/mL)CL/F
(L/hr)t½
(hr)200 mg fasted
(n=20)†132 (50)
[45-267]3.50
[1.5-36‡]4179 (31)
[2705-7269]51 (25)
[28-74]23.5 (25)
[15.3-33.7]200 mg nonfat
(n=20)†378 (43)
[131-834]4 [3-5] 10,753 (35)
[4579-17,092]21 (39)
[12-44]22.2 (18)
[17.4-28.7]200 mg high fat
(54 gm fat)
(n=20)†512 (34)
[241-1016]5 [4-5] 15,059 (26)
[10,341-24,476]14 (24)
[8.2-19]23.0 (19)
[17.2-33.4]400 mg fasted
(n=23)§121 (75)
[27-366]4 [2-12] 5258 (48)
[2834-9567]91 (40)
[42-141]27.3 (26)
[16.8-38.9]400 mg with liquid nutritional supplement
(14 gm fat)
(n=23)§355 (43)
[145-720]5 [4-8] 11,295 (40)
[3865-20,592]43 (56)
[19-103]26.0 (19)
[18.2-35.0]Table 15: The Effect of Varying Gastric Administration Conditions on the Cmax and AUC of Noxafil Oral Suspension in Healthy Volunteers* Study Description Administration Arms Change in Cmax
(ratio estimate†; 90% CI of the ratio estimate)Change in AUC
(ratio estimate†; 90% CI of the ratio estimate)- *
- In 5 subjects, the Cmax and AUC decreased substantially (range: -27% to -53% and -33% to -51%, respectively) when Noxafil was administered via an NG tube compared to when Noxafil was administered orally. It is recommended to closely monitor patients for breakthrough fungal infections when posaconazole is administered via an NG tube because a lower plasma exposure may be associated with an increased risk of treatment failure.
- †
- Ratio Estimate is the ratio of coadministered drug plus Noxafil to coadministered drug alone for Cmax or AUC.
- ‡
- NG = nasogastric
400-mg single dose with a high-fat meal relative to fasted state (n=12) 5 minutes before high-fat meal ↑96%
(1.96; 1.48-2.59)↑111%
(2.11; 1.60-2.78)During high-fat meal ↑339%
(4.39; 3.32-5.80)↑382%
(4.82; 3.66-6.35)20 minutes after high-fat meal ↑333%
(4.33; 3.28-5.73)↑387%
(4.87; 3.70-6.42)400 mg twice daily and 200 mg four times daily for 7 days in fasted state and with liquid nutritional supplement (BOOST®) (n=12) 400 mg twice daily with BOOST ↑65%
(1.65; 1.29-2.11)↑66%
(1.66; 1.30-2.13)200 mg four times daily with BOOST No Effect No Effect Divided daily dose from 400 mg twice daily to 200 mg four times daily for 7 days regardless of fasted conditions or with BOOST (n=12) Fasted state ↑136%
(2.36; 1.84-3.02)↑161%
(2.61; 2.04-3.35)With BOOST ↑137%
(2.37; 1.86-3.04)↑157%
(2.57; 2.00-3.30)400-mg single dose with carbonated acidic beverage (ginger ale) and/or proton pump inhibitor (esomeprazole) (n=12) Ginger ale ↑92%
(1.92; 1.51-2.44)↑70%
(1.70; 1.43-2.03)Esomeprazole ↓32%
(0.68; 0.53-0.86)↓30%
(0.70; 0.59-0.83)400-mg single dose with a prokinetic agent (metoclopramide 10 mg three times a day for 2 days) + BOOST or an antikinetic agent (loperamide 4-mg single dose) + BOOST (n=12) With metoclopramide + BOOST ↓21%
(0.79; 0.72-0.87)↓19%
(0.81; 0.72-0.91)With loperamide + BOOST ↓3%
(0.97; 0.88-1.07)↑11%
(1.11; 0.99-1.25)400-mg single dose either orally with BOOST or via an NG tube with BOOST (n=16) Via NG tube‡ ↓19%
(0.81; 0.71-0.91)↓23%
(0.77; 0.69-0.86)Concomitant administration of Noxafil oral suspension with drugs affecting gastric pH or gastric motility results in lower posaconazole exposure. (See Table 16.)
Table 16: The Effect of Concomitant Medications that Affect the Gastric pH and Gastric Motility on the Pharmacokinetics of Noxafil Oral Suspension in Healthy Volunteers Coadministered Drug (Postulated Mechanism of Interaction) Coadministered Drug Dose/Schedule Noxafil Dose/Schedule Effect on Bioavailability of Posaconazole Change in Mean Cmax
(ratio estimate*; 90% CI of the ratio estimate)Change in Mean AUC
(ratio estimate*; 90% CI of the ratio estimate)- *
- Ratio Estimate is the ratio of coadministered drug plus Noxafil to coadministered drug alone for Cmax or AUC.
- †
- The tablet refers to a non-commercial tablet formulation without polymer.
- ‡
- The drug interactions associated with the oral suspension are also relevant for the delayed-release tablet with the exception of Esomeprazole and Metoclopramide.
Cimetidine
(Alteration of gastric pH)400 mg twice daily × 10 days 200 mg (tablets) once daily × 10 days† ↓ 39%
(0.61; 0.53-0.70)↓ 39%
(0.61; 0.54-0.69)Esomeprazole (Increase in gastric pH)‡ 40 mg every morning × 3 days 400 mg (oral suspension) single dose ↓ 46%
(0.54; 0.43-0.69)↓ 32%
(0.68; 0.57-0.81)Metoclopramide (Increase in gastric motility)‡ 10 mg three times a day × 2 days 400 mg (oral suspension) single dose ↓ 21%
(0.79; 0.72-0.87)↓ 19%
(0.81; 0.72-0.91)Distribution:
Posaconazole is highly bound to human plasma proteins (>98%), predominantly to albumin.
Metabolism:
Posaconazole primarily circulates as the parent compound in plasma. Of the circulating metabolites, the majority are glucuronide conjugates formed via UDP glucuronidation (phase 2 enzymes). Posaconazole does not have any major circulating oxidative (CYP450 mediated) metabolites. The excreted metabolites in urine and feces account for ~17% of the administered radiolabeled dose.
Posaconazole is primarily metabolized via UDP glucuronidation (phase 2 enzymes) and is a substrate for p-glycoprotein (P-gp) efflux. Therefore, inhibitors or inducers of these clearance pathways may affect posaconazole plasma concentrations. A summary of drugs studied clinically with the oral suspension or an early tablet formulation, which affect posaconazole concentrations, is provided in Table 17.
Table 17: Summary of the Effect of Coadministered Drugs on Noxafil in Healthy Volunteers Coadministered Drug (Postulated Mechanism of Interaction) Coadministered Drug Dose/Schedule Noxafil Dose/Schedule Effect on Bioavailability of Posaconazole Change in Mean Cmax
(ratio estimate*; 90% CI of the ratio estimate)Change in Mean AUC
(ratio estimate*; 90% CI of the ratio estimate)Efavirenz
(UDP-G Induction)400 mg once daily × 10 and 20 days 400 mg (oral suspension) twice daily × 10 and 20 days ↓45%
(0.55; 0.47-0.66)↓ 50%
(0.50; 0.43-0.60)Fosamprenavir (unknown mechanism) 700 mg twice daily x 10 days 200 mg once daily on the 1st day, 200 mg twice daily on the 2nd day, then 400 mg twice daily x 8 Days ↓21%
0.79 (0.71-0.89)↓23%
0.77 (0.68-0.87)Rifabutin
(UDP-G Induction)300 mg once daily x 17 days 200 mg (tablets) once daily × 10 days† ↓ 43%
(0.57; 0.43-0.75)↓ 49%
(0.51; 0.37-0.71)Phenytoin
(UDP-G Induction)200 mg once daily x 10 days 200 mg (tablets) once daily × 10 days† ↓ 41%
(0.59; 0.44-0.79)↓ 50%
(0.50; 0.36-0.71)In vitro studies with human hepatic microsomes and clinical studies indicate that posaconazole is an inhibitor primarily of CYP3A4. A clinical study in healthy volunteers also indicates that posaconazole is a strong CYP3A4 inhibitor as evidenced by a >5-fold increase in midazolam AUC. Therefore, plasma concentrations of drugs predominantly metabolized by CYP3A4 may be increased by posaconazole. A summary of the drugs studied clinically, for which plasma concentrations were affected by posaconazole, is provided in Table 18[see Contraindications (4) and Drug Interactions (7.1) including recommendations].
Table 18: Summary of the Effect of Noxafil on Coadministered Drugs in Healthy Volunteers and Patients Coadministered Drug (Postulated Mechanism of Interaction is Inhibition of CYP3A4 by Posaconazole) Coadministered Drug Dose/Schedule Noxafil Dose/Schedule Effect on Bioavailability of Coadministered Drugs Change in Mean Cmax
(ratio estimate*; 90% CI of the ratio estimate)Change in Mean AUC
(ratio estimate*; 90% CI of the ratio estimate)- *
- Ratio Estimate is the ratio of coadministered drug plus Noxafil to coadministered drug alone for Cmax or AUC.
- †
- The tablet refers to a non-commercial tablet formulation without polymer.
- ‡
- The mean terminal half-life of midazolam was increased from 3 hours to 7 to 11 hours during coadministration with Noxafil.
Sirolimus 2-mg single oral dose 400 mg (oral suspension) twice daily x 16 days ↑ 572%
(6.72; 5.62-8.03)↑ 788%
(8.88; 7.26-10.9)Cyclosporine Stable maintenance dose in heart transplant recipients 200 mg (tablets) once daily x 10 days† ↑ cyclosporine whole blood trough concentrations
Cyclosporine dose reductions of up to 29% were requiredTacrolimus 0.05-mg/kg single oral dose 400 mg (oral suspension) twice daily × 7 days ↑ 121%
(2.21; 2.01-2.42)↑ 358%
(4.58; 4.03-5.19)Simvastatin 40-mg single oral dose 100 mg (oral suspension) once daily x 13 days Simvastatin
↑ 841%
(9.41, 7.13-12.44)
Simvastatin Acid
↑ 817%
(9.17, 7.36-11.43)Simvastatin
↑ 931%
(10.31, 8.40-12.67)
Simvastatin Acid
↑634%
(7.34, 5.82-9.25)200 mg (oral suspension) once daily x 13 days Simvastatin
↑ 1041%
(11.41, 7.99-16.29)
Simvastatin Acid
↑851%
(9.51, 8.15-11.10)Simvastatin
↑ 960%
(10.60, 8.63-13.02)
Simvastatin Acid
↑ 748%
(8.48, 7.04-10.23)Midazolam 0.4-mg single intravenous dose‡ 200 mg (oral suspension) twice daily x 7 days ↑ 30%
(1.3; 1.13-1.48)↑ 362%
(4.62; 4.02-5.3)0.4-mg single intravenous dose‡ 400 mg (oral suspension) twice daily x 7 days ↑62%
(1.62; 1.41-1.86)↑524%
(6.24; 5.43-7.16)2-mg single oral dose‡ 200 mg (oral suspension) once daily x 7 days ↑ 169%
(2.69; 2.46-2.93)↑ 470%
(5.70; 4.82-6.74)2-mg single oral dose‡ 400 mg (oral suspension) twice daily x 7 days ↑ 138%
(2.38; 2.13-2.66)↑ 397%
(4.97; 4.46-5.54)Rifabutin 300 mg once daily x 17 days 200 mg (tablets) once daily × 10 days† ↑ 31%
(1.31; 1.10-1.57)↑ 72%
(1.72;1.51-1.95)Phenytoin 200 mg once daily PO x 10 days 200 mg (tablets) once daily x 10 days† ↑ 16%
(1.16; 0.85-1.57)↑ 16%
(1.16; 0.84-1.59)Ritonavir 100 mg once daily x 14 days 400 mg (oral suspension)
twice daily x 7 days↑ 49%
(1.49; 1.04-2.15)↑ 80%
(1.8;1.39-2.31)Atazanavir 300 mg once daily x 14 days 400 mg (oral suspension) twice daily x 7 days ↑ 155%
(2.55; 1.89-3.45)↑ 268%
(3.68; 2.89-4.70)Atazanavir/ ritonavir boosted regimen 300 mg/100 mg once daily x 14 days 400 mg (oral suspension) twice daily x 7 days ↑ 53%
(1.53; 1.13-2.07)↑ 146%
(2.46; 1.93-3.13)Additional clinical studies demonstrated that no clinically significant effects on zidovudine, lamivudine, indinavir, or caffeine were observed when administered with Noxafil 200 mg once daily; therefore, no dose adjustments are required for these coadministered drugs when coadministered with posaconazole 200 mg once daily.
Excretion:
Following administration of Noxafil oral suspension, posaconazole is predominantly eliminated in the feces (71% of the radiolabeled dose up to 120 hours) with the major component eliminated as parent drug (66% of the radiolabeled dose). Renal clearance is a minor elimination pathway, with 13% of the radiolabeled dose excreted in urine up to 120 hours (<0.2% of the radiolabeled dose is parent drug).
Posaconazole delayed-release tablet is eliminated with a mean half-life (t½) ranging between 26 to 31 hours.
Posaconazole oral suspension is eliminated with a mean half-life (t½) of 35 hours (range: 20-66 hours).
Specific Populations
No clinically significant differences in the pharmacokinetics of posaconazole were observed based on age, sex, renal impairment, and indication (prophylaxis or treatment).
Race/Ethnicity:
In a population pharmacokinetic analysis of posaconazole, AUC was found to be 25% higher in Chinese patients relative to patients from other races/ethnicities. This higher exposure is not expected to be clinically relevant given the expected variability in posaconazole exposure.
Patients Weighing More Than 120 kg:
Weight has a clinically significant effect on posaconazole clearance. Relative to 70 kg patients, the Cavg is decreased by 25% in patients greater than 120 kg. Patients administered posaconazole weighing more than 120 kg may be at higher risk for lower posaconazole plasma concentrations compared to lower weight patients [see Use in Specific Populations (8.10)].
12.4 Microbiology
Mechanism of Action:
Posaconazole blocks the synthesis of ergosterol, a key component of the fungal cell membrane, through the inhibition of cytochrome P-450 dependent enzyme lanosterol 14α-demethylase responsible for the conversion of lanosterol to ergosterol in the fungal cell membrane. This results in an accumulation of methylated sterol precursors and a depletion of ergosterol within the cell membrane thus weakening the structure and function of the fungal cell membrane. This may be responsible for the antifungal activity of posaconazole.
Resistance:
Clinical isolates of Candida albicans and Candida glabrata with decreased susceptibility to posaconazole were observed in oral swish samples taken during prophylaxis with posaconazole and fluconazole, suggesting a potential for development of resistance. These isolates also showed reduced susceptibility to other azoles, suggesting cross-resistance between azoles. The clinical significance of this finding is not known.
Antimicrobial Activity:
Posaconazole has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)].
Susceptibility Testing:
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see:
https://www.fda.gov/STIC . -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No drug-related neoplasms were recorded in rats or mice treated with posaconazole for 2 years at doses higher than the clinical dose. In a 2-year carcinogenicity study, rats were given posaconazole orally at doses up to 20 mg/kg (females), or 30 mg/kg (males). These doses are equivalent to 3.9- or 3.5-times the exposure achieved with a 400-mg twice daily oral suspension regimen, respectively, based on steady-state AUC in healthy volunteers administered a high-fat meal (400-mg twice daily oral suspension regimen). In the mouse study, mice were treated at oral doses up to 60 mg/kg/day or 4.8-times the exposure achieved with a 400-mg twice daily oral suspension regimen.
Mutagenesis
Posaconazole was not genotoxic or clastogenic when evaluated in bacterial mutagenicity (Ames), a chromosome aberration study in human peripheral blood lymphocytes, a Chinese hamster ovary cell mutagenicity study, and a mouse bone marrow micronucleus study.
Impairment of Fertility
Posaconazole had no effect on fertility of male rats at a dose up to 180 mg/kg (1.7 x the 400-mg twice daily oral suspension regimen based on steady-state plasma concentrations in healthy volunteers) or female rats at a dose up to 45 mg/kg (2.2 x the 400-mg twice daily oral suspension regimen).
13.2 Animal Toxicology and/or Pharmacology
In a nonclinical study using intravenous administration of posaconazole in very young dogs (dosed from 2 to 8 weeks of age), an increase in the incidence of brain ventricle enlargement was observed in treated animals as compared with concurrent control animals. No difference in the incidence of brain ventricle enlargement between control and treated animals was observed following the subsequent 5-month treatment-free period. There were no neurologic, behavioral or developmental abnormalities in the dogs with this finding, and a similar brain finding was not seen with oral posaconazole administration to juvenile dogs (4 days to 9 months of age). There were no drug-related increases in the incidence of brain ventricle enlargement when treated, and control animals were compared in a separate study of 10-week old dogs dosed with intravenous posaconazole for 13 weeks with a 9-week recovery period or a follow-up study of 31-week old dogs dosed for 3 months.
-
14 CLINICAL STUDIES
14.1 Treatment of Invasive Aspergillosis with Noxafil Injection and Noxafil Delayed-Release Tablets
Aspergillosis Treatment Study (NCT01782131) was a randomized, double-blind, controlled trial which evaluated the safety and efficacy of Noxafil injection and Noxafil delayed-release tablets versus voriconazole for primary treatment of invasive fungal disease caused by Aspergillus species. Eligible patients had proven, probable, or possible invasive fungal infections per the European Organization for Research and Treatment of Cancer/Mycoses Study Group, EORTC/MSG criteria. Patients were stratified by risk for mortality or poor outcome where high risk included a history of allogeneic bone marrow transplant, liver transplant, or relapsed leukemia undergoing salvage chemotherapy. The median age of patients was 57 years (range 14-91 years), with 27.8% of patients aged ≥65 years; 5 patients were pediatric patients 14-16 years of age, of whom 3 were treated with Noxafil and 2 with voriconazole. The majority of patients were male (59.8%) and white (67.1%). With regard to risk factors for invasive aspergillosis, approximately two-thirds of the patients in the study had a recent history of neutropenia, while approximately 20% with a history of an allogeneic stem cell transplant. Over 80% of subjects in each treatment group had infection limited to the lower respiratory tract (primarily lung), while approximately 11% to 13% also had infection in another organ. Invasive aspergillosis was proven or probable in 58.1% of patients as classified by independent adjudicators blinded to study treatment assignment. At least one Aspergillus species was identified in 21% of the patients; A. fumigatus and A. flavus were the most common pathogens identified.
Patients randomized to receive Noxafil were given a dose of 300 mg once daily (twice daily on Day 1) IV or tablet. Patients randomized to receive voriconazole were given a dose of 6 mg/kg twice daily Day 1 followed by 4 mg/kg twice daily IV, or oral 300 mg twice daily Day 1 followed by 200 mg twice daily. The recommended initial route of administration was IV; however, patients could begin oral therapy if clinically stable and able to tolerate oral dosing. The transition from IV to oral therapy occurred when the patient was clinically stable. The protocol recommended duration of therapy was 84 days with a maximum allowed duration of 98 days. Median treatment duration was 67 days for Noxafil patients and 64 days for voriconazole patients. Overall, 55% to 60% of patients began treatment with the IV formulation with a median duration of 9 days for the initial IV dosing.
The Intent to Treat (ITT) population included all patients randomized and receiving at least one dose of study treatment. All-cause mortality through Day 42 in the overall population (ITT) was 15.3% for Noxafil patients compared to 20.6% for voriconazole patients for an adjusted treatment difference of -5.3% with a 95% confidence interval of -11.6 to 1.0%. Consistent results were seen in patients with proven or probable invasive aspergillosis per EORTC criteria (see Table 19).
Table 19: Noxafil Injection and Noxafil Delayed-Release Tablets Invasive Aspergillosis Treatment Study: All-Cause Mortality Through Day 42 Noxafil Injection and Delayed-Release Tablets Voriconazole Population N n (%) N n (%) Difference* (95% CI) - *
- Adjusted treatment difference based on Miettinen and Nurminen’s method stratified by randomization factor (risk for mortality/poor outcome), using Cochran-Mantel-Haenszel weighting scheme.
Intent to Treat 288 44 (15.3) 287 59 (20.6) -5.3 (-11.6, 1.0) Proven/Probable Invasive Aspergillosis 163 31 (19.0) 171 32 (18.7) 0.3 (-8.2, 8.8) Global clinical response at Week 6 was assessed by a blinded, independent adjudication committee based upon prespecified clinical, radiologic, and mycologic criteria. In the subgroup of patients with proven or probable invasive aspergillosis per EORTC criteria, the global clinical response of success (complete or partial response) at Week 6 was seen in 44.8% for Noxafil-treated patients compared to 45.6% for voriconazole-treated patients (see Table 20).
Table 20: Noxafil Injection and Noxafil Delayed-Release Tablets Invasive Aspergillosis Treatment Study: Successful Global Clinical Response* at Week 6 Posaconazole Voriconazole Population N Success N Success Difference† (95% CI) Proven/Probable Invasive Aspergillosis 163 73 (44.8) 171 78 (45.6) -0.6 (-11.2, 10.1) 14.2 Prophylaxis of Aspergillus and Candida Infections with Noxafil Oral Suspension
Two randomized, controlled studies were conducted using Noxafil as prophylaxis for the prevention of invasive fungal infections (IFIs) among patients at high risk due to severely compromised immune systems.
The first study (Noxafil Oral Suspension Study 1) was a randomized, double-blind trial that compared Noxafil oral suspension (200 mg three times a day) with fluconazole capsules (400 mg once daily) as prophylaxis against invasive fungal infections in allogeneic hematopoietic stem cell transplant (HSCT) recipients with Graft versus Host Disease (GVHD). Efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy (patients may have met more than one of these criteria). This assessed all patients while on study therapy plus 7 days and at 16 weeks post-randomization. The mean duration of therapy was comparable between the 2 treatment groups (80 days, Noxafil oral suspension; 77 days, fluconazole). Table 21 contains the results from Noxafil Oral Suspension Study 1.
Table 21: Results from Blinded Clinical Study in Prophylaxis of IFI in All Randomized Patients with Hematopoietic Stem Cell Transplant (HSCT) and Graft-vs.-Host Disease (GVHD): Noxafil Oral Suspension Study 1 Posaconazole
n=301Fluconazole
n=299- *
- Patients may have met more than one criterion defining failure.
- †
- Use of systemic antifungal therapy (SAF) criterion is based on protocol definitions (empiric/IFI usage >4 consecutive days).
- ‡
- 95% confidence interval (posaconazole-fluconazole) = (-11.5%, +3.7%).
- §
- Patients who are lost to follow-up (not observed for 112 days), and who did not meet another clinical failure endpoint. These patients were considered failures.
On therapy plus 7 days Clinical Failure* 50 (17%) 55 (18%) Failure due to: Proven/Probable IFI 7 (2%) 22 (7%) (Aspergillus) 3 (1%) 17 (6%) (Candida) 1 (<1%) 3 (1%) (Other) 3 (1%) 2 (1%) All Deaths 22 (7%) 24 (8%) Proven/probable fungal infection prior to death 2 (<1%) 6 (2%) SAF† 27 (9%) 25 (8%) Through 16 weeks Clinical Failure*,‡ 99 (33%) 110 (37%) Failure due to: Proven/Probable IFI 16 (5%) 27 (9%) (Aspergillus) 7 (2%) 21 (7%) (Candida) 4 (1%) 4 (1%) (Other) 5 (2%) 2 (1%) All Deaths 58 (19%) 59 (20%) Proven/probable fungal infection prior to death 10 (3%) 16 (5%) SAF† 26 (9%) 30 (10%) Event free lost to follow-up§ 24 (8%) 30 (10%) The second study (Noxafil Oral Suspension Study 2) was a randomized, open-label study that compared Noxafil oral suspension (200 mg 3 times a day) with fluconazole suspension (400 mg once daily) or itraconazole oral solution (200 mg twice a day) as prophylaxis against IFIs in neutropenic patients who were receiving cytotoxic chemotherapy for AML or MDS. As in Noxafil Oral Suspension Study 1, efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy (Patients might have met more than one of these criteria). This study assessed patients while on treatment plus 7 days and 100 days postrandomization. The mean duration of therapy was comparable between the 2 treatment groups (29 days, posaconazole; 25 days, fluconazole or itraconazole). Table 22 contains the results from Noxafil Oral Suspension Study 2.
Table 22: Results from Open-Label Clinical Study 2 in Prophylaxis of IFI in All Randomized Patients with Hematologic Malignancy and Prolonged Neutropenia: Noxafil Oral Suspension Study 2 Posaconazole
n=304Fluconazole/Itraconazole
n=298- *
- 95% confidence interval (posaconazole-fluconazole/itraconazole) = (-22.9%, -7.8%).
- †
- Patients may have met more than one criterion defining failure.
- ‡
- Use of systemic antifungal therapy (SAF) criterion is based on protocol definitions (empiric/IFI usage >3 consecutive days).
- §
- Patients who are lost to follow-up (not observed for 100 days), and who did not meet another clinical failure endpoint. These patients were considered failures.
On therapy plus 7 days Clinical Failure*,† 82 (27%) 126 (42%) Failure due to: Proven/Probable IFI 7 (2%) 25 (8%) (Aspergillus) 2 (1%) 20 (7%) (Candida) 3 (1%) 2 (1%) (Other) 2 (1%) 3 (1%) All Deaths 17 (6%) 25 (8%) Proven/probable fungal infection prior to death 1 (<1%) 2 (1%) SAF‡ 67 (22%) 98 (33%) Through 100 days postrandomization Clinical Failure† 158 (52%) 191 (64%) Failure due to: Proven/Probable IFI 14 (5%) 33 (11%) (Aspergillus) 2 (1%) 26 (9%) (Candida) 10 (3%) 4 (1%) (Other) 2 (1%) 3 (1%) All Deaths 44 (14%) 64 (21%) Proven/probable fungal infection prior to death 2 (1%) 16 (5%) SAF‡ 98 (32%) 125 (42%) Event free lost to follow-up§ 34 (11%) 24 (8%) In summary, 2 clinical studies of prophylaxis were conducted with the Noxafil oral suspension. As seen in the accompanying tables (Tables 21 and 22), clinical failure represented a composite endpoint of breakthrough IFI, mortality and use of systemic antifungal therapy. In Noxafil Oral Suspension Study 1 (Table 21), the clinical failure rate of posaconazole (33%) was similar to fluconazole (37%), (95% CI for the difference posaconazole–comparator -11.5% to 3.7%) while in Noxafil Oral Suspension Study 2 (Table 22) clinical failure was lower for patients treated with posaconazole (27%) when compared to patients treated with fluconazole or itraconazole (42%), (95% CI for the difference posaconazole–comparator -22.9% to -7.8%).
All-cause mortality was similar at 16 weeks for both treatment arms in Noxafil Oral Suspension Study 1 [POS 58/301 (19%) vs. FLU 59/299 (20%)]; all-cause mortality was lower at 100 days for Noxafil-treated patients in Noxafil Oral Suspension Study 2 [POS 44/304 (14%) vs. FLU/ITZ 64/298 (21%)]. Both studies demonstrated fewer breakthrough infections caused by Aspergillus species in patients receiving Noxafil prophylaxis when compared to patients receiving fluconazole or itraconazole.
14.3 Treatment of Oropharyngeal Candidiasis with Noxafil Oral Suspension
Noxafil Oral Suspension Study 3 was a randomized, controlled, evaluator-blinded study in HIV-infected patients with oropharyngeal candidiasis. Patients were treated with Noxafil or fluconazole oral suspension (both Noxafil and fluconazole were given as follows: 100 mg twice a day for 1 day followed by 100 mg once a day for 13 days).
Clinical and mycological outcomes were assessed after 14 days of treatment and at 4 weeks after the end of treatment. Patients who received at least 1 dose of study medication and had a positive oral swish culture of Candida species at baseline were included in the analyses (see Table 23). The majority of the subjects had C. albicans as the baseline pathogen.
Clinical success at Day 14 (complete or partial resolution of all ulcers and/or plaques and symptoms) and clinical relapse rates (recurrence of signs or symptoms after initial cure or improvement) 4 weeks after the end of treatment were similar between the treatment arms (see Table 23).
Mycologic eradication rates (absence of colony forming units in quantitative culture at the end of therapy, Day 14), as well as mycologic relapse rates (4 weeks after the end of treatment) were also similar between the treatment arms (see Table 23).
Table 23: Noxafil Oral Suspension Clinical Success, Mycological Eradication, and Relapse Rates in Oropharyngeal Candidiasis Noxafil Fluconazole Clinical Success at End of Therapy (Day 14) 155/169 (91.7%) 148/160 (92.5%) Clinical Relapse (4 Weeks after End of Therapy) 45/155 (29.0%) 52/148 (35.1%) Mycological Eradication (absence of CFU) at End of Therapy (Day 14) 88/169 (52.1%) 80/160 (50.0%) Mycological Relapse (4 Weeks after End of Treatment) 49/88 (55.6%) 51/80 (63.7%) Mycologic response rates, using a criterion for success as a posttreatment quantitative culture with ≤20 colony forming units (CFU/mL) were also similar between the two groups (Noxafil 68.0%, fluconazole 68.1%). The clinical significance of this finding is unknown.
14.4 Noxafil Oral Suspension Treatment of Oropharyngeal Candidiasis Refractory to Treatment with Fluconazole or Itraconazole
Noxafil Oral Suspension Study 4 was a noncomparative study of Noxafil oral suspension in HIV-infected subjects with OPC that was refractory to treatment with fluconazole or itraconazole. An episode of OPC was considered refractory if there was failure to improve or worsening of OPC after a standard course of therapy with fluconazole greater than or equal to 100 mg/day for at least 10 consecutive days or itraconazole 200 mg/day for at least 10 consecutive days and treatment with either fluconazole or itraconazole had not been discontinued for more than 14 days prior to treatment with Noxafil. Of the 199 subjects enrolled in this study, 89 subjects met these strict criteria for refractory infection.
Forty-five subjects with refractory OPC were treated with Noxafil oral suspension 400 mg twice daily for 3 days, followed by 400 mg once daily for 25 days with an option for further treatment during a 3-month maintenance period. Following a dosing amendment, a further 44 subjects were treated with Noxafil 400 mg twice daily for 28 days. The efficacy of Noxafil was assessed by the clinical success (cure or improvement) rate after 4 weeks of treatment. The clinical success rate was 74.2% (66/89). The clinical success rates for both the original and the amended dosing regimens were similar (73.3% and 75.0%, respectively).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Delayed-Release TabletsPosaconazole delayed-release tablets are available as yellow, coated, oblong, debossed with "100" on one side containing 100 mg of posaconazole. Bottles with child-resistant closures of 60 delayed-release tablets (NDC 63629-2236-1).
16.2 Storage and Handling
Posaconazole Delayed-Release TabletsStore at 20°C to 25°C (68°F to 77°F), excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Important Administration Instructions
Posaconazole Delayed-Release Tablets
Advise patients that Posaconazole delayed-release tablets must be swallowed whole and not divided, crushed, or chewed.
Instruct patients that if they miss a dose, they should take it as soon as they remember. If they do not remember until it is within 12 hours of the next dose, they should be instructed to skip the missed dose and go back to the regular schedule. Patients should not double their next dose or take more than the prescribed dose.
Drug Interactions
Advise patients to inform their physician immediately if they:
- develop severe diarrhea or vomiting.
- are currently taking drugs that are known to prolong the QTc interval and are metabolized through CYP3A4.
- are currently taking a cyclosporine or tacrolimus, or they notice swelling in an arm or leg or shortness of breath.
- are taking other drugs or before they begin taking other drugs as certain drugs can decrease or increase the plasma concentrations of posaconazole.
Serious and Potentially Serious Adverse Reactions
Advise patients to inform their physician immediately if they:
- notice a change in heart rate or heart rhythm, or have a heart condition or circulatory disease. Posaconazole can be administered with caution to patients with potentially proarrhythmic conditions.
- are pregnant, plan to become pregnant, or are nursing.
- have liver disease or develop itching, nausea or vomiting, their eyes or skin turn yellow, they feel more tired than usual or feel like they have the flu.
- have ever had an allergic reaction to other antifungal medicines such as ketoconazole, fluconazole, itraconazole, or voriconazole.
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 01/2022 Patient Information
Posaconazole delayed-release tabletsWhat is posaconazole?
Posaconazole delayed-release tablets are a prescription medicine used in adults and children to help prevent or treat fungal infections that can spread throughout your body (invasive fungal infections). These infections are caused by fungi called Aspergillus or Candida. Posaconazole is used in people who have an increased chance of getting these infections due to a weak immune system. These include people who have had a hematopoietic stem cell transplantation (bone marrow transplant) with graft versus host disease or those with a low white blood cell count due to chemotherapy for blood cancers (hematologic malignancies).
Posaconazole delayed-release tablets are used for:- prevention of fungal infections in adults and children 2 years of age and older who weigh greater than 88 lbs (40 kg).
- treatment of fungal infections in adults and children 13 years of age and older.
Who should not take posaconazole?
Do not take posaconazole if you:- are allergic to posaconazole, any of the ingredients in posaconazole, or other azole antifungal medicines. See the end of this leaflet for a complete list of ingredients in posaconazole.
- are taking any of the following medicines:
- sirolimus
- pimozide
- quinidine
- certain statin medicines that lower cholesterol (atorvastatin, lovastatin, simvastatin)
- ergot alkaloids (ergotamine, dihydroergotamine)
- have chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) and you have just started taking venetoclax or your venetoclax dose is being slowly increased.
Do not start taking a new medicine without talking to your healthcare provider or pharmacist.What should I tell my healthcare provider before taking posaconazole?
Before you take posaconazole, tell your healthcare provider if you:- are taking certain medicines that lower your immune system like cyclosporine or tacrolimus.
- are taking certain drugs for HIV infection, such as ritonavir, atazanavir, efavirenz, or fosamprenavir. Efavirenz and fosamprenavir can cause a decrease in the posaconazole levels in your body. Efavirenz and fosamprenavir should not be taken with posaconazole.
- are taking midazolam, a hypnotic and sedative medicine.
- are taking vincristine, vinblastine and other "vinca alkaloids" (medicines used to treat cancer).
- are taking venetoclax, a medicine used to treat cancer.
- have or had liver problems.
- have or had kidney problems.
- have or had an abnormal heart rate or rhythm, heart problems, or blood circulation problems.
- are pregnant or plan to become pregnant. It is not known if posaconazole will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if posaconazole passes into your breast milk. You and your healthcare provider should decide if you will take posaconazole or breastfeed. You should not do both.
Especially tell your healthcare provider if you take:- rifabutin or phenytoin. If you are taking these medicines, you should not take Posaconazole delayed-release tablets.
Know the medicines you take. Keep a list of them with you to show your healthcare provider or pharmacist when you get a new medicine.How will I take posaconazole? - Do not switch between taking Posaconazole delayed-release tablets and Posaconazole oral suspension.
- Take posaconazole exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how much posaconazole to take and when to take it.
- Take posaconazole for as long as your healthcare provider tells you to take it.
- If you take too much posaconazole, call your healthcare provider or go to the nearest hospital emergency room right away.
-
Posaconazole delayed-release tablets:
- Take Posaconazole delayed-release tablets with or without food.
- Take Posaconazole delayed-release tablets whole. Do not break, crush, or chew Posaconazole delayed-release tablets before swallowing. If you cannot swallow Posaconazole delayed-release tablets whole, tell your healthcare provider. You may need a different medicine.
- If you miss a dose, take it as soon as you remember and then take your next scheduled dose at its regular time. If it is within 12 hours of your next dose, do not take the missed dose. Skip the missed dose and go back to your regular schedule. Do not double your next dose or take more than your prescribed dose.
What are the possible side effects of posaconazole?
Posaconazole may cause serious side effects, including:- drug interactions with cyclosporine or tacrolimus. If you take posaconazole with cyclosporine or tacrolimus, your blood levels of cyclosporine or tacrolimus may increase. Serious side effects can happen in your kidney or brain if you have high levels of cyclosporine or tacrolimus in your blood. Your healthcare provider should do blood tests to check your levels of cyclosporine or tacrolimus if you are taking these medicines while taking posaconazole. Tell your healthcare provider right away if you have swelling in your arm or leg or shortness of breath.
- problems with the electrical system of your heart (arrhythmias and QTc prolongation). Certain medicines used to treat fungus called azoles, including posaconazole, the active ingredient in posaconazole, may cause heart rhythm problems. People who have certain heart problems or who take certain medicines have a higher chance for this problem. Tell your healthcare provider right away if your heartbeat becomes fast or irregular.
- changes in body salt (electrolytes) levels in your blood. Your healthcare provider should check your electrolytes while you are taking posaconazole.
- liver problems. Some people who also have other serious medical problems may have severe liver problems that may lead to death, especially if you take certain doses of posaconazole. Your healthcare provider should do blood tests to check your liver while you are taking posaconazole. Call your healthcare provider right away if you have any of the following symptoms of liver problems:
- itchy skin
- nausea or vomiting
- yellowing of your eyes or skin
- feeling very tired
- flu-like symptoms
- increased amounts of midazolam in your blood. If you take posaconazole with midazolam, posaconazole increases the amount of midazolam in your blood. This can make your sleepiness last longer. Your healthcare provider should check you closely for side effects if you take midazolam with posaconazole.
- diarrhea
- nausea
- fever
- vomiting
- headache
- coughing
- low potassium levels in the blood
If you take Posaconazole delayed-release tablets, tell your healthcare provider right away if you have diarrhea or vomiting.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of posaconazole. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store posaconazole?
Posaconazole delayed-release tablets:- Store Posaconazole delayed-release tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Safely throw away medicine that is out of date or no longer needed.
General information about the safe and effective use of posaconazole.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use posaconazole for a condition for which it was not prescribed. Do not give posaconazole to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about posaconazole that is written for health professionals.What are the ingredients in posaconazole?
Active ingredient: posaconazole
Inactive ingredients:
Posaconazole delayed-release tablets: croscarmellose sodium, hydroxypropylcellulose, hypromellose acetate succinate, iron oxide yellow, Macrogol/PEG 3350, magnesium stearate, microcrystalline cellulose, polyvinyl alcohol partially hydrolyzed, silicon dioxide, talc, and titanium dioxide.
Manufactured for: Par Pharmaceutical, Chestnut Ridge, NY 10977, USA
Delayed-Release Tablets: Manuf. by: N. V. Organon, Kloosterstraat 6, 5349 AB Oss, Netherlands
usppi-gmk5592-t-2201r003
PI2045-01-78-03 - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
POSACONAZOLE
posaconazole tablet, coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63629-2236(NDC:0254-2045) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POSACONAZOLE (UNII: 6TK1G07BHZ) (POSACONAZOLE - UNII:6TK1G07BHZ) POSACONAZOLE 100 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE ACETATE SUCCINATE 06081224 (3 MM2/S) (UNII: 6N003M473W) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (YELLOW (C48330)) Score no score Shape OVAL (oblong) Size 17mm Flavor Imprint Code 100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63629-2236-1 60 in 1 BOTTLE; Type 0: Not a Combination Product 09/01/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA205053 08/30/2019 Labeler - Bryant Ranch Prepack (171714327) Registrant - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(63629-2236) , RELABEL(63629-2236)