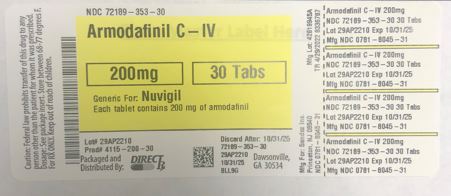
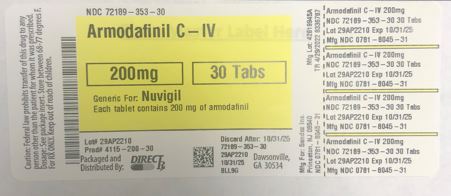
Label: ARMODAFINIL tablet
- NDC Code(s): 72189-353-30
- Packager: DirectRx
- This is a repackaged label.
- Source NDC Code(s): 0781-8045
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: CIV
- Marketing Status: New Drug Application Authorized Generic
Drug Label Information
Updated May 19, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
INDICATIONS & USAGE
Armodafinil tablets are indicated to improve wakefulness in adult patients with excessive sleepiness associated with obstructive sleep apnea (OSA), narcolepsy, or shift work disorder (SWD).
Limitations of Use
In OSA, armodafinil tablets are indicated to treat excessive sleepiness and not as treatment for the underlying obstruction. If continuous positive airway pressure (CPAP) is the treatment of choice for a patient, a maximal effort to treat with CPAP for an adequate period of time should be made prior to initiating armodafinil tablets for excessive sleepiness.
-
DOSAGE FORMS & STRENGTHS
2.1 Dosage in Obstructive Sleep Apnea (OSA) and Narcolepsy
The recommended dosage of armodafinil tablets for patients with OSA or narcolepsy is 150 mg to 250 mg taken orally once a day as a single dose in the morning.In patients with OSA, doses up to 250 mg/day, given as a single dose, have been well tolerated, but there is no consistent evidence that these doses confer additional benefit beyond that of the 150 mg/day dose [see Clinical Pharmacology (12.3) and Clinical Studies (14.1, 14.2)].
2.2 Dosage in Shift Work Disorder (SWD)
The recommended dosage of armodafinil tablets for patients with SWD is 150 mg taken orally once a day as a single dose approximately 1 hour prior to the start of their work shift.2.3 Dosage Modification in Patients with Severe Hepatic Impairment
In patients with severe hepatic impairment, the dosage of armodafinil tablets should be reduced [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].2.4 Use in Geriatric Patients
Consideration should be given to the use of lower doses and close monitoring in geriatric patients [see Use in Specific Populations (8.5)]. -
DOSAGE FORMS & STRENGTHS
50 mg – round, white to off-white tablet with
formw
on one side and "205" on the other
150 mg – oval, white to off-white tablet with
formw
on one side and "215" on the other
200 mg – rounded, rectangular, white to off-white tablet with
formw
on one side and "220" on the other
250 mg – oval, white to off-white tablet with
formw
on one side and "225" on the other - CONTRAINDICATIONS
-
WARNINGS AND PRECAUTIONS
5.1 Serious Dermatologic Reactions, including Stevens-Johnson Syndrome and Toxic Epidermal Necrosis
Serious rash requiring hospitalization and discontinuation of treatment has been reported in association with the use of armodafinil or modafinil (the racemic mixture of S- and R-enantiomers).Armodafinil has not been studied in pediatric patients in any setting and is not approved for use in pediatric patients for any indication.
In clinical trials of modafinil, the incidence of rash resulting in discontinuation was approximately 0.8% (13 per 1,585) in pediatric patients (age <17 years); these rashes included 1 case of possible Stevens-Johnson syndrome (SJS) and 1 case of apparent multi-organ hypersensitivity reaction/Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) [see Warnings and Precautions (5.2)]. Several of the cases were associated with fever and other abnormalities (e.g., vomiting, leukopenia). The median time to rash that resulted in discontinuation was 13 days. No such cases were observed among 380 pediatric patients who received placebo.
Skin and mouth sores, blistering, and ulceration have been reported with modafinil and armodafinil in the postmarketing setting. Recurrence of signs and symptoms of serious dermatologic reactions following rechallenge has been reported in some cases.
Rare cases of serious or life-threatening rash, including SJS and toxic epidermal necrolysis (TEN), have been reported in adults and children in worldwide postmarketing experience with modafinil and armodafinil.
There are no factors, including duration of therapy, that are known to predict the risk of occurrence or the severity of rash associated with modafinil or armodafinil. In cases where the time to onset was reported, serious rash occurred 1 day to 2 months after initiation of treatment, but isolated cases of serious dermatologic reactions have been reported with symptoms beginning after prolonged treatment (e.g., 3 months).
Although benign rashes also occur with armodafinil, it is not possible to reliably predict which rashes will prove to be serious. Accordingly, armodafinil should be discontinued at the first sign of rash, skin or mouth sores, or blistering or ulceration, unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring.
5.2 Drug Reaction with Eosinophilia and System Symptoms (DRESS)/Multiorgan Hypersensitivity
DRESS, also known as multi-organ hypersensitivity, has been reported with armodafinil. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling, in association with other organ system involvement, such as hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis, sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present even though rash is not evident.One fatal case of DRESS that occurred in close temporal association (3 weeks) with the initiation of armodafinil treatment has been reported in the postmarketing setting. In addition, multi-organ hypersensitivity reactions, including at least one fatality in postmarketing experience, have occurred in close temporal association (median time to detection 13 days; range 4-33) to the initiation of modafinil. Although there have been a limited number of reports, multi-organ hypersensitivity reactions may result in hospitalization or be life-threatening.
If a multi-organ hypersensitivity reaction is suspected, armodafinil should be discontinued. Although there are no case reports to indicate cross‑sensitivity with other drugs that produce this syndrome, the experience with drugs associated with multi-organ hypersensitivity would indicate this to be a possibility.
5.3 Angioedema and Anaphylaxis Reactions
Angioedema and hypersensitivity (with rash, dysphagia, and bronchospasm), were observed with armodafinil. Patients should be advised to discontinue therapy and immediately report to their physician any signs or symptoms suggesting angioedema or anaphylaxis (e.g., swelling of face, eyes, lips, tongue or larynx; difficulty in swallowing or breathing; hoarseness).5.4 Persistent Sleepiness
Patients with abnormal levels of sleepiness who take armodafinil should be advised that their level of wakefulness may not return to normal. Patients with excessive sleepiness, including those taking armodafinil, should be frequently reassessed for their degree of sleepiness and, if appropriate, advised to avoid driving or any other potentially dangerous activity. Prescribers should also be aware that patients may not acknowledge sleepiness or drowsiness until directly questioned about drowsiness or sleepiness during specific activities.5.5 Psychiatric Symptoms
In pre-approval narcolepsy, OSA and SWD controlled trials of armodafinil, anxiety, agitation, nervousness, and irritability were reasons for treatment discontinuation more often in patients on armodafinil compared to placebo (armodafinil 1.2% and placebo 0.3%). Depression was also a reason for treatment discontinuation more often in patients on armodafinil compared to placebo (armodafinil 0.6% and placebo 0.2%). Cases of suicidal ideation were observed in clinical trials.Caution should be exercised when armodafinil is given to patients with a history of psychosis, depression, or mania. If psychiatric symptoms develop in association with armodafinil administration, consider discontinuing armodafinil.
Psychiatric adverse reactions have been reported in patients treated with modafinil. Modafinil and armodafinil are very closely related. Therefore, the incidence and type of psychiatric symptoms associated with armodafinil are expected to be similar to the incidence and type of these events with modafinil.
Postmarketing adverse reactions associated with the use of armodafinil, some of which have resulted in hospitalization, have included mania, delusions, hallucinations, suicidal ideation, and aggression. Many, but not all, patients who developed psychiatric adverse reactions had a prior psychiatric history. In these cases, reported armodafinil total daily doses ranged from 50 mg to 450 mg, which includes doses below and above the recommended dosages.
5.6 Effects on Ability to Drive and Use Machinery
Although armodafinil has not been shown to produce functional impairment, any drug affecting the central nervous system (CNS) may alter judgment, thinking or motor skills. Patients should be cautioned about operating an automobile or other hazardous machinery until it is reasonably certain that armodafinil therapy will not adversely affect their ability to engage in such activities.5.7 Cardiovascular Events
In clinical studies of modafinil, cardiovascular adverse reactions, including chest pain, palpitations, dyspnea and transient ischemic T-wave changes on ECG were observed in three subjects in association with mitral valve prolapse or left ventricular hypertrophy. It is recommended that armodafinil tablets not be used in patients with a history of left ventricular hypertrophy or in patients with mitral valve prolapse who have experienced the mitral valve prolapse syndrome when previously receiving CNS stimulants. Findings suggestive of mitral valve prolapse syndrome include but are not limited to ischemic ECG changes, chest pain, or arrhythmia. If new onset of any of these findings occurs, consider cardiac evaluation.Blood pressure monitoring in short term (≤3 months) pre-approval controlled trials of OSA, SWD, and narcolepsy showed small average increases in mean systolic and diastolic blood pressure in patients receiving armodafinil as compared to placebo (1.2 to 4.3 mmHg in the various experimental groups). There was also a slightly greater proportion of patients on armodafinil requiring new or increased use of antihypertensive medications (2.9%) compared to patients on placebo (1.8%). There was a small, but consistent, average increase in pulse rate over placebo in pre-approval controlled trials. This increase varied from 0.9 to 3.5 BPM. Increased monitoring of heart rate and blood pressure may be appropriate in patients on armodafinil. Caution should be exercised when prescribing armodafinil to patients with known cardiovascular disease.
-
ADVERSE REACTIONS
The following serious adverse reactions are described below and elsewhere in the labeling:
Serious Dermatologic Reactions [see Warnings and Precautions (5.1)]
Drug Reaction with Eosinophilia and System Symptoms (DRESS)/Multiorgan Hypersensitivity [see Warnings and Precautions (5.2)]
Angioedema and Anaphylaxis Reactions [see Warnings and Precautions (5.3)]
Persistent Sleepiness [see Warnings and Precautions (5.4)]
Psychiatric Symptoms [see Warnings and Precautions (5.5)]
Effects on Ability to Drive and Use Machinery [see Warnings and Precautions (5.6)]
Cardiovascular Events [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Armodafinil has been evaluated for safety in over 1,100 patients with excessive sleepiness associated with OSA, SWD, and narcolepsy.
Most Common Adverse Reactions
In the placebo-controlled clinical trials, the most common adverse reactions (≥5%) associated with the use of armodafinil more frequently than in placebo-treated patients were headache, nausea, dizziness, and insomnia. The adverse reaction profile was similar across the studies.
Table 1 presents the adverse reactions that occurred at a rate of 1% or more and were more frequent in armodafinil-treated patients than in placebo-treated patients in the placebo-controlled clinical trials.
Table 1 Adverse Reactions in Pooled Placebo-Controlled Clinical Trials* in OSA, Narcolepsy, and SWD with Armodafinil (150 mg and 250 mg)
Armodafinil
(%)
N=645 Placebo
(%)
N=445
*Adverse reactions that occurred in > 1% of armodafinil-treated patients and greater incidence than that of placebo.
Headache
17
9
Nausea
7
3
Dizziness
5
2
Insomnia
5
1
Anxiety
4
1
Diarrhea
4
2
Dry Mouth
4
1
Depression
2
0
Dyspepsia
2
0
Fatigue
2
1
Palpitations
2
1
Rash
2
0
Upper Abdominal Pain
2
1
Agitation
1
0
Anorexia
1
0
Constipation
1
0
Contact Dermatitis
1
0
Decreased Appetite
1
0
Depressed Mood
1
0
Disturbance In Attention
1
0
Dyspnea
1
0
Hyperhydrosis
1
0
Increased Gamma-Glutamyltransferase
1
0
Increased Heart Rate
1
0
Influenza-Like Illness
1
0
Loose Stools
1
0
Migraine
1
0
Nervousness
1
0
Pain
1
0
Paresthesia
1
0
Polyuria
1
0
Pyrexia
1
0
Seasonal Allergy
1
0
Thirst
1
0
Tremor
1
0
Vomiting
1
0
Dose-Dependent Adverse Reactions
In the placebo-controlled clinical trials which compared doses of 150 mg/day and 250 mg/day of armodafinil and placebo, the following adverse reactions were dose-related: headache, rash, depression, dry mouth, insomnia, and nausea. See Table 2 for additional information.
Table 2 Dose-Dependent Adverse Reactions in Pooled Placebo-Controlled Clinical Trials in OSA, Narcolepsy and SWD
Armodafinil
250 mg
(%)
N=198 Armodafinil
150 mg
(%)
N=447 Armodafinil
Combined
(%)
N=645
Placebo
(%)
N=445
Headache
23
14
17
9
Nausea
9
6
7
3
Insomnia
6
4
5
1
Dry Mouth
7
2
4
<1
Rash
4
1
2
<1
Depression
3
1
2
<1
Adverse Reactions Resulting in Discontinuation of Treatment
In placebo-controlled clinical trials, 44 of the 645 patients (7%) who received armodafinil discontinued due to an adverse reaction compared to 16 of the 445 (4%) of patients that received placebo. The most frequent reason for discontinuation was headache (1%).
Laboratory Abnormalities
Clinical chemistry, hematology, and urinalysis parameters were monitored in the studies. Mean plasma levels of gamma glutamyltransferase (GGT) and alkaline phosphatase (AP) were found to be higher following administration of armodafinil, but not placebo. Few patients, however, had GGT or AP elevations outside of the normal range. No differences were apparent in alanine aminotransferase (ALT), aspartate aminotransferase (AST), total protein, albumin, or total bilirubin, although there were rare cases of isolated elevations of AST and/or ALT. A single case of mild pancytopenia was observed after 35 days of treatment and resolved with drug discontinuation. A small mean decrease from baseline in serum uric acid compared to placebo was seen in clinical trials. The clinical significance of this finding is unknown.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of armodafinil. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular
Stroke
Gastrointestinal Disorders
Mouth Sores (including mouth blistering and ulceration)
-
DESCRIPTION
Armodafinil tablets are a wakefulness‑promoting agent for oral administration. Armodafinil is the R-enantiomer of modafinil which is a 1:1 mixture of the R- and S-enantiomers. The chemical name for armodafinil is 2‑[(R)-(diphenylmethyl)sulfinyl]acetamide. The molecular formula is C15H15NO2S and the molecular weight is 273.35.
The chemical structure is:
chemical structure
Armodafinil is a white to off-white, crystalline powder that is slightly soluble in water, sparingly soluble in acetone, and soluble in methanol.
Armodafinil tablets contain 50, 150, 200 or 250 mg of armodafinil and the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, and pregelatinized starch.
-
OVERDOSAGE
Fatal overdoses involving modafinil alone or involving armodafinil or modafinil in combination with other drugs have been reported in the postmarketing setting. Symptoms most often accompanying armodafinil or modafinil overdose, alone or in combination with other drugs, have included anxiety, dyspnea, insomnia; central nervous system symptoms such as restlessness, disorientation, confusion, excitation and hallucination; digestive changes such as nausea and diarrhea; and cardiovascular changes such as tachycardia, bradycardia, hypertension, and chest pain.
No specific antidote exists for the toxic effects of an armodafinil overdose. Such overdoses should be managed with primarily supportive care, including cardiovascular monitoring.
-
HOW SUPPLIED
16.1 How Supplied
Armodafinil tablets are available as follows:50 mg
Each round, white to off-white tablet is debossed with formw on one side and "205" on the other.
NDC 0781-8029-31 – Bottles of 30150 mg
Each oval, white to off-white tablet is debossed with formw on one side and "215" on the other.
NDC 0781-8037-31 – Bottles of 30200 mg
Each rounded, rectangular, white to off-white tablet is debossed with C on one side and "220" on the other.
NDC 0781-8045-31 – Bottles of 30250 mg
Each oval, white to off-white tablet is debossed with formw on one side and "225" on the other.
NDC 0781-8053-31 – Bottles of 3016.2 Storage
Store at 20o to 25o C (68o to 77o F). -
MEDICATION GUIDE
Armodafinil tablets, for oral use, C-IV
(are-moe-DAFF-ih-nil)
What is the most important information I should know about armodafinil tablets?
Armodafinil tablets are a federal controlled substance (C-IV) because it can be abused or lead to dependence. Keep armodafinil tablets in a safe place to prevent misuse and abuse. Selling or giving away armodafinil tablets may harm others, and is against the law. Tell your doctor if you have ever abused or been dependent on alcohol, prescription medicines or street drugs.Armodafinil tablets may cause serious side effects including a serious rash or a serious allergic reaction that may affect parts of your body such as your liver or blood cells. Any of these may need to be treated in a hospital and may be life-threatening.
Stop taking armodafinil tablets and call your doctor right away or get emergency help if you have any of these symptoms:
skin rash, hives, sores in your mouth, or your skin blisters and peels
swelling of your face, eyes, lips, tongue, or throat
trouble swallowing, breathing or hoarseness
fever, shortness of breath, swelling of the legs, yellowing of the skin or whites of the eyes, or dark urine.
If you have a severe rash with armodafinil tablets, stopping the medicine may not keep the rash from becoming life-threatening or causing you to be permanently disabled or disfigured.Armodafinil tablets are not approved for use in children for any medical condition.
It is not known if armodafinil tablets are safe and effective in children under the age of 18.
What are armodafinil tablets?
Armodafinil tablets are a prescription medicine used to improve wakefulness in adults who are very sleepy due to one of the following diagnosed sleep disorders:narcolepsy
obstructive sleep apnea (OSA). Armodafinil tablets are used with other medical treatments for this sleep disorder. Armodafinil tablets do not take the place of using your CPAP machine or other treatments that your doctor has prescribed for this condition. It is important that you continue to use these treatments as prescribed by your doctor.
shift work disorder (SWD)
Armodafinil tablets will not cure these sleep disorders. Armodafinil tablets may help the sleepiness caused by these conditions, but it may not stop all your sleepiness. Armodafinil tablets do not take the place of getting enough sleep. Follow your doctor’s advice about good sleep habits and using other treatments.
Do not take armodafinil tablets if you:
are allergic to any of its ingredients. See the end of this Medication Guide for a complete list of ingredients in armodafinil tablets.
have had a rash or allergic reaction to either armodafinil tablets (NUVIGIL®) or modafinil (PROVIGIL®). These medicines are very similar.
Before you take armodafinil tablets, tell your doctor about all of your medical conditions, including if you:
have a history of mental health problems, including psychosis
have heart problems or had a heart attack
have high blood pressure. Your blood pressure may need to be checked more often while taking armodafinil tablets.
have liver or kidney problems
have a history of drug or alcohol abuse or addiction
are pregnant or planning to become pregnant. It is not known if armodafinil tablets will harm your unborn baby.
Pregnancy Registry: There is a registry for women who become pregnant during treatment with armodafinil tablets. The purpose of this registry is to collect information about the safety of armodafinil tablets during pregnancy. Contact the registry as soon as you learn that you are pregnant, or ask your doctor to contact the registry for you. You or your doctor can get information and enroll you in the registry by calling 1-866-404-4106.are breastfeeding. It is not known if armodafinil passes into your milk. Talk to your doctor about the best way to feed your baby if you take armodafinil tablets.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Armodafinil tablets and many other medicines can interact with each other, sometimes causing side effects. Armodafinil tablets may affect the way other medicines work, and other medicines may affect how armodafinil tablets works. Your dose of armodafinil tablets or certain other medicines may need to be changed.
Especially, tell your doctor if you use or take:a hormonal birth control method, such as birth control pills, shots, implants, patches, vaginal rings, and intrauterine devices (IUDs). Hormonal birth control methods may not work while you take armodafinil tablets. Women who use one of these methods of birth control may have a higher chance for getting pregnant while taking armodafinil tablets, and for one month after stopping armodafinil tablets. You should use effective birth control while taking armodafinil tablets and for one month after your final dose. Talk to your doctor about birth control choices that are right for you while taking armodafinil tablets.
Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine. Your doctor or pharmacist will tell you if it is safe to take armodafinil tablets and other medicines together. Do not start any new medicines with armodafinil tablets unless your doctor has told you it is okay.
How should I take armodafinil tablets?Take armodafinil tablets exactly as prescribed by your doctor. Your doctor will prescribe the dose of armodafinil tablets that is right for you. Do not change your dose of armodafinil tablets without talking to your doctor.
Your doctor will tell you the right time of day to take armodafinil tablets.
People with narcolepsy or OSA usually take armodafinil tablets one time each day in the morning.
People with SWD usually take armodafinil tablets about 1 hour before their work shift.
Do not change the time of day you take armodafinil tablets unless you have talked to your doctor. If you take armodafinil tablets too close to your bedtime, you may find it harder to go to sleep.
You can take armodafinil tablets with or without food.
If you take more than your prescribed dose or if you take an overdose of armodafinil tablets, call your doctor or poison control center right away.
Symptoms of an overdose of armodafinil tablets may include:● Trouble sleeping ● Restlessness
● Confusion ● Feeling disoriented
● Feeling excited ● Hearing, seeing, feeling, or sensing things that are not really there (hallucinations)
● Nausea and diarrhea ● A fast or slow heartbeat
● Chest pain ● Increased blood pressure
● Anxiety ● Shortness of breath
What should I avoid while taking armodafinil tablets?
Do not drive a car or do other dangerous activities until you know how armodafinil tablets affect you. People with sleep disorders should always be careful about doing things that could be dangerous. Do not change your daily habits until your doctor tells you it is okay.
You should avoid drinking alcohol. It is not known how drinking alcohol will affect you when taking armodafinil tablets.
What are the possible side effects of armodafinil tablets?Armodafinil tablets may cause serious side effects. Stop taking armodafinil tablets and call your doctor right away or get emergency help if you get any of the following:
a serious rash or serious allergic reaction. (See “What is the most important information I should know about armodafinil tablets?”)
mental (psychiatric) symptoms, including:
depression º feeling anxious
hearing, seeing, feeling, or sensing things º an extreme increase in activity and talking (mania)
that are not really there (hallucinations) º aggressive behavior
thoughts of suicide
other mental problems
symptoms of a heart problem, including chest pain, abnormal heart beats, and trouble breathing.
The most common side effects of armodafinil tablets include:headache • nausea
dizziness • trouble sleeping
These are not all the possible side effects of armodafinil tablets.Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store armodafinil tablets?
Store armodafinil tablets at room temperature between 68° to 77°F (20° to 25°C).
Keep armodafinil tablets and all medicines out of the reach of children.
General information about the safe and effective use of armodafinil tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use armodafinil tablets for a condition for which it was not prescribed. Do not give armodafinil tablets to other people, even if they have the same symptoms that you have. It may harm them and is against the law.You can ask your pharmacist or healthcare provider for information about armodafinil tablets that is written for health professionals.
What are the ingredients in armodafinil tablets?
Active Ingredient: armodafinilInactive Ingredients: lactose monohydrate, microcrystalline cellulose, pregelatinized starch, croscarmellose sodium, povidone, and magnesium stearate.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Rev. October 2018The brands listed are the registered trademarks of their respective owners and are not trademarks of Sandoz Inc.
Distributed by Sandoz Inc.
Princeton, NJ 08540 - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
ARMODAFINIL
armodafinil tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:72189-353(NDC:0781-8045) Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ARMODAFINIL (UNII: V63XWA605I) (ARMODAFINIL - UNII:V63XWA605I) ARMODAFINIL 200 mg Inactive Ingredients Ingredient Name Strength POVIDONE K30 (UNII: U725QWY32X) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) STARCH, CORN (UNII: O8232NY3SJ) MAGNESIUM STEARATE (UNII: 70097M6I30) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color white ((white to off-white)) Score no score Shape RECTANGLE ((rounded, rectangular)) Size 12mm Flavor Imprint Code C;220 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:72189-353-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 04/29/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA021875 04/29/2022 Labeler - DirectRx (079254320) Registrant - DirectRx (079254320) Establishment Name Address ID/FEI Business Operations DirectRx 079254320 repack(72189-353)