Label: AZOR- amlodipine besylate and olmesartan medoxomil tablet, film coated
-
Contains inactivated NDC Code(s)
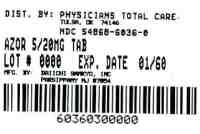
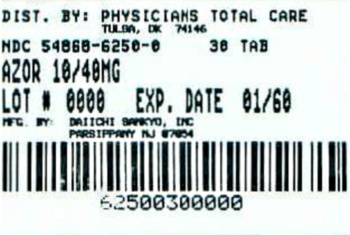
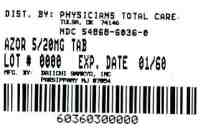
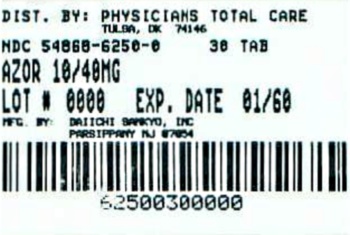
NDC Code(s): 54868-6036-0, 54868-6250-0 - Packager: Physicians Total Care, Inc.
- This is a repackaged label.
- Source NDC Code(s): 65597-110, 65597-113
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated January 9, 2012
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Azor safely and effectively. See full prescribing information for Azor. Azor (amlodipine and olmesartan medoxomil) tablet, film coated for oral use Initial U.S. Approval: 2007
USE IN PREGNANCY
See full prescribing information for complete boxed warning.
When pregnancy is detected, discontinue Azor as soon as possible. When used in pregnancy during the second and third trimesters, drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus (5.1).
RECENT MAJOR CHANGES
Indications and Usage (1) 11/2011
INDICATIONS AND USAGE
-
Azor is a dihydropyridine calcium channel blocker and angiotensin II receptor blocker combination product indicated for the treatment of hypertension, alone or with other antihypertensive agents, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. (1).
-
Azor is indicated as initial therapy in patients likely to need multiple antihypertensive agents to achieve their blood pressure goals (1).
DOSAGE AND ADMINISTRATION
- Substitute Azor for its individually titrated components for patients on amlodipine and olmesartan medoxomil. Azor may also be given with increased amounts of amlodipine, olmesartan medoxomil, or both, as needed (2).
- Azor may be used to provide additional blood pressure lowering for patients not adequately controlled with amlodipine (or another dihydropyridine calcium channel blocker) alone or with olmesartan medoxomil (or another angiotensin receptor blocker) alone (2).
- Dosage may be increased after 2 weeks to a maximum dose of 10/40 mg once daily, usually by increasing one component at a time but both components can be raised to achieve more rapid control (2).
- Maximum antihypertensive effects are attained within 2 weeks after a change in dose (2).
- Initial therapy: Initiate with 5/20 mg once daily for 1 to 2 weeks and titrate as needed up to a maximum of 10/40 mg once daily (2).
DOSAGE FORMS AND STRENGTHS
Tablets: (amlodipine/olmesartan medoxomil content) 5/20 mg; 10/20mg; 5/40 mg; and 10/40 mg (3).
CONTRAINDICATIONS
None (4).
WARNINGS AND PRECAUTIONS
- Hypotension in volume- or salt-depleted patients with treatment initiation may be anticipated. Start treatment under close supervision (5.2).
- Increased angina or myocardial infarction with calcium channel blockers may occur upon dosage initiation or increase (5.4).
- Impaired renal function: changes in renal function may be anticipated in susceptible individuals (5.6).
ADVERSE REACTIONS
Most common adverse reaction (incidence ≥3%) is edema (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Daiichi Sankyo, Inc. at 1-877-437-7763 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
USE IN SPECIFIC POPULATIONS
- In patients with an activated renin-angiotensin system, such as volume- or salt-depletion, renin-angiotensin-aldosterone system (RAAS) blockers such as olmesartan medoxomil can cause excessive hypotension. In susceptible patients, e.g. with renal artery stenosis, RAAS blockers can cause renal failure (5.2, 5.6).
- Start amlodipine alone or add amlodipine at 2.5 mg in patients ≥75 years old or in hepatically impaired patients. Elderly and patients with hepatic impairment have decreased clearance of amlodipine. Initial therapy with Azor is not recommended in patients ≥75 years old or hepatically impaired patients (8.5, 8.6).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2011
-
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Fetal/Neonatal Morbidity and Mortality
5.2 Hypotension in Volume- or Salt-Depleted Patients
5.3 Vasodilation
5.4 Patients with Severe Obstructive Coronary Artery Disease
5.5 Patients with Congestive Heart Failure
5.6 Patients with Impaired Renal Function
5.7 Patients with Hepatic Impairment
5.8 Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Drug Interactions with Azor
7.2 Drug Interactions with Amlodipine
7.3 Drug Interactions with Olmesartan Medoxomil
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
8.8 Black Patients
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Azor
14.2 Amlodipine
14.3 Olmesartan Medoxomil
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
Azor®
USE IN PREGNANCY
(amlodipine and olmesartan medoxomil) tabletsWhen pregnancy is detected, discontinue Azor as soon as possible. When used in pregnancy during the second and third trimesters, drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus [see Warning and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Azor is indicated for the treatment of hypertension, alone or with other antihypertensive agents , to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including the class to which this drug principally belongs. There are no controlled trials demonstrating risk reduction with Azor.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Azor may also be used as initial therapy in patients who are likely to need multiple antihypertensive agents to achieve their blood pressure goals.
Patients with moderate or severe hypertension are at relatively high risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure, and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal, and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient’s risk.
Data from an 8-week, placebo-controlled, parallel-group factorial study [see Clinical Studies (14.1)] provide estimates of the probability of reaching a blood pressure goal with Azor compared to amlodipine or olmesartan medoxomil monotherapy. The figures below provide estimates of the likelihood of achieving the targeted systolic or diastolic blood pressure goals with Azor 10/40 mg compared with amlodipine or olmesartan medoxomil monotherapy, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling from all available data of that treatment group. The right tail of each curve is less reliable because of small numbers of subjects with high baseline blood pressures.
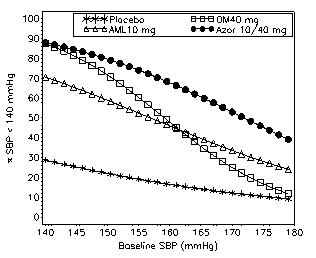
Figure 1: Probability of Achieving Systolic Blood Pressure (SBP) <140 mmHg at Week 8 With LOCF
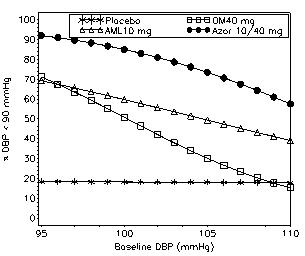
Figure 2: Probability of Achieving Diastolic Blood Pressure (DBP) <90 mmHg at Week 8 With LOCF
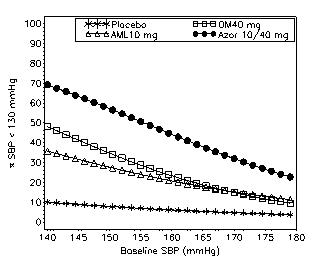
Figure 3: Probability of Achieving Systolic Blood Pressure (SBP) <130 mmHg at Week 8 With LOCF
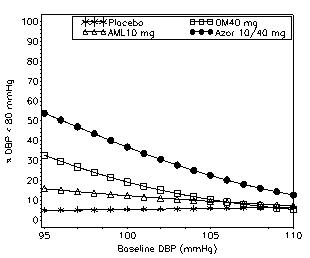
Figure 4: Probability of Achieving Diastolic Blood Pressure (DBP) <80 mmHg at Week 8 With LOCF
The figures above provide an approximation of the likelihood of reaching a targeted blood pressure goal (e.g., Week 8 SBP <140 mmHg or <130 mmHg or a DBP <90 mmHg or <80 mmHg) for the high-dose treatment groups evaluated in the study. Azor 5/20 mg, the lowest dose combination treatment group, increases the probability of reaching blood pressure goal compared with the highest dose monotherapies, amlodipine 10 mg and olmesartan medoxomil 40 mg.
For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 48% likelihood of achieving a goal of <140 mmHg (systolic) and a 51% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with olmesartan medoxomil 40 mg, and about a 46% likelihood of achieving a goal of <140 mmHg (systolic) and a 60% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with amlodipine 10 mg. The likelihood of achieving these same goals increases to 63% (systolic) and 71% (diastolic) on Azor 5/20 mg, and to 68% (systolic) and 85% (diastolic) on Azor 10/40 mg.
-
2 DOSAGE AND ADMINISTRATION
General Considerations
The side effects of olmesartan medoxomil are generally rare and apparently independent of dose. Those of amlodipine are generally dose-dependent (mostly edema).
Maximum antihypertensive effects are attained within 2 weeks after a change in dose.
Azor may be taken with or without food.
Azor may be administered with other antihypertensive agents.
Dosage may be increased after 2 weeks. The maximum recommended dose of Azor is 10/40 mg.
Replacement Therapy
Azor may be substituted for its individually titrated components.
When substituting for individual components, the dose of one or both of the components can be increased if blood pressure control has not been satisfactory.
Add-on Therapy
Azor may be used to provide additional blood pressure lowering for patients not adequately controlled with amlodipine (or another dihydropyridine calcium channel blocker) alone or with olmesartan medoxomil (or another angiotensin receptor blocker) alone.
Initial Therapy
The usual starting dose of Azor is 5/20 mg once daily. The dosage can be increased after 1 to 2 weeks of therapy to a maximum dose of one 10/40 mg tablet once daily as needed to control blood pressure [See Clinical Studies (14.1)].
Initial therapy with Azor is not recommended in patients ≥75 years old or with hepatic impairment [See Warnings and Precautions (5.7) and Use in Specific Populations (8.5, 8.6)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
Enter section text here
5.1 Fetal/Neonatal Morbidity and Mortality
Olmesartan medoxomil. Drugs that act directly on the renin-angiotensin system can cause fetal and neonatal morbidity and death when administered to pregnant women. There have been several dozen cases reported in the world literature of patients who were taking angiotensin converting enzyme inhibitors. When pregnancy is detected, discontinue Azor as soon as possible.
During the second and third trimesters of pregnancy, these drugs have been associated with fetal injury that includes hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to exposure to the drug.
These adverse effects do not appear to have resulted from intrauterine drug exposure that has been limited to the first trimester. Mothers whose embryos and fetuses are exposed to an angiotensin II receptor antagonist only during the first trimester should be so informed. Nonetheless, when patients become pregnant, physicians should have the patient discontinue the use of Azor as soon as possible.
Rarely (probably less often than once in every thousand pregnancies), no alternative to a drug acting on the renin-angiotensin system will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses and serial ultrasound examinations should be performed to assess the intra-amniotic environment.
If oligohydramnios is observed, discontinue Azor unless it is considered life-saving for the mother. Contraction stress testing (CST), a non-stress test (NST), or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to an angiotensin II receptor antagonist should be closely observed for hypotension, oliguria, and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function.
No teratogenic effects were observed when olmesartan medoxomil was administered to pregnant rats at oral doses up to 1000 mg/kg/day (240 times the maximum recommended human dose (MRHD) on a mg/m2 basis) or pregnant rabbits at oral doses up to 1 mg/kg/day (half the MRHD on a mg/m2 basis; higher doses could not be evaluated for effects on fetal development as they were lethal to the does). In rats, significant decreases in pup birth weight and weight gain were observed at doses ≥1.6 mg/kg/day, and delays in developmental milestones (delayed separation of ear auricular, eruption of lower incisors, appearance of abdominal hair, descent of testes, and separation of eyelids) and dose-dependent increases in the incidence of dilation of the renal pelvis were observed at doses ≥8 mg/kg/day. The no observed effect dose for developmental toxicity in rats is 0.3 mg/kg/day, about one-tenth the MRHD of 40 mg/day.
5.2 Hypotension in Volume- or Salt-Depleted Patients
Olmesartan medoxomil. Symptomatic hypotension may be anticipated after initiation of treatment with olmesartan medoxomil. Patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics) may be particularly vulnerable. Initiate treatment with Azor under close medical supervision. If hypotension does occur, place the patient in the supine position and, if necessary, give an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
5.3 Vasodilation
Amlodipine. Since the vasodilation attributable to amlodipine in Azor is gradual in onset, acute hypotension has rarely been reported after oral administration. Nonetheless, exercise caution, as with any other peripheral vasodilator, when administering Azor, particularly in patients with severe aortic stenosis.
5.4 Patients with Severe Obstructive Coronary Artery Disease
Patients, particularly those with severe obstructive coronary artery disease, may develop increased frequency, duration, or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy or at the time of dosage increase. The mechanism of this effect has not been elucidated.
5.5 Patients with Congestive Heart Failure
Amlodipine. In general, calcium channel blockers should be used with caution in patients with heart failure. Amlodipine (5-10 mg per day) has been studied in a placebo-controlled trial of 1153 patients with NYHA Class III or IV heart failure on stable doses of ACE inhibitor, digoxin, and diuretics. Follow-up was at least 6 months, with a mean of about 14 months. There was no overall adverse effect on survival or cardiac morbidity (as defined by life-threatening arrhythmia, acute myocardial infarction, or hospitalization for worsened heart failure). Amlodipine has been compared to placebo in four 8-12 week studies of patients with NYHA class II/III heart failure, involving a total of 697 patients. In these studies, there was no evidence of worsening of heart failure based on measures of exercise tolerance, NYHA classification, symptoms, or LVEF.
5.6 Patients with Impaired Renal Function
Azor. There are no studies of Azor in patients with renal impairment.
Olmesartan medoxomil. Changes in renal function may be anticipated in susceptible individuals treated with olmesartan medoxomil as a consequence of inhibiting the renin-angiotensin-aldosterone system. In patients whose renal function may depend upon the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with angiotensin converting enzyme inhibitors and angiotensin receptor antagonists has been associated with oliguria or progressive azotemia and (rarely) with acute renal failure and/or death. Similar effects may occur in patients treated with Azor because of the olmesartan medoxomil component [See Clinical Pharmacology (12.3)].
In studies of ACE inhibitors in patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or blood urea nitrogen (BUN) have been reported. There has been no long-term use of olmesartan medoxomil in patients with unilateral or bilateral renal artery stenosis, but similar effects would be expected with olmesartan medoxomil and Azor.
5.7 Patients with Hepatic Impairment
Amlodipine. Since amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t1/2) is 56 hours in patients with severely impaired hepatic function, exercise caution when administering Azor to patients with severe hepatic impairment.
Patients with hepatic impairment have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in hepatically impaired patients is recommended. The lowest dose of Azor is 5/20 mg; therefore, initial therapy with Azor is not recommended in hepatically impaired patients [See Use in Specific Populations (8.6)].
5.8 Laboratory Tests
Azor. There was a greater decrease in hemoglobin and hematocrit in the combination product compared to either component. Other laboratory changes can usually be attributed to either monotherapy component.
Amlodipine. In post-marketing experience, hepatic enzyme elevations have been reported (6.2).
Olmesartan medoxomil. In post-marketing experience, increased blood creatinine levels and hyperkalemia have been reported.
-
6 ADVERSE REACTIONS
Enter section text here
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
AzorThe data described below reflect exposure to Azor in more than 1600 patients including more than 1000 exposed for at least 6 months and more than 700 exposed for 1 year. Azor was studied in one placebo-controlled factorial trial (see Section 14.1). The population had a mean age of 54 years and included approximately 55% males. Seventy-one percent were Caucasian and 25% were Black. Patients received doses ranging from 5/20 mg to 10/40 mg orally once daily.
The overall incidence of adverse reactions on therapy with Azor was similar to that seen with corresponding doses of the individual components of Azor, and to placebo. The reported adverse reactions were generally mild and seldom led to discontinuation of treatment (2.6% for Azor and 6.8% for placebo).
Edema
Edema is a known, dose-dependent adverse effect of amlodipine but not of olmesartan medoxomil.
The placebo-subtracted incidence of edema during the 8-week, randomized, double-blind treatment period was highest with amlodipine 10 mg monotherapy. The incidence was significantly reduced when 20 mg or 40 mg of olmesartan medoxomil was added to the 10 mg amlodipine dose.
Placebo-Subtracted Incidence of Edema during the Double-Blind Treatment Period
Olmesartan Medoxomil
Placebo 20 mg 40 mg Amlodipine Placebo –%* -2.4% 6.2% 5mg 0.7% 5.7% 6.2% 10 mg 24.5% 13.3% 11.2% *12.3% = actual placebo incidence
Across all treatment groups, the frequency of edema was generally higher in women than men, as has been observed in previous studies of amlodipine.
Adverse reactions seen at lower rates during the double-blind period also occurred in the patients treated with Azor at about the same or greater incidence as in patients receiving placebo. These included hypotension, orthostatic hypotension, rash, pruritus, palpitation, urinary frequency, and nocturia.
The adverse event profile obtained from 44 weeks of open-label combination therapy with amlodipine plus olmesartan medoxomil was similar to that observed during the 8-week, double-blind, placebo-controlled period.
Initial Therapy
Analyzing the data described above specifically for initial therapy, it was observed that higher doses of Azor caused slightly more hypotension and orthostatic symptoms, but not at the recommended starting dose of Azor 5/20 mg. No increase in the incidence of syncope or near syncope was observed. The incidences of discontinuation because of any treatment emergent adverse events in the double blind phase are summarized in the table below.
*1Hypertension is counted as treatment failure and not as treatment emergent adverse event.Discontinuation for any Treatment Emergent Adverse Event1
Olmesartan Medoxomil
Placebo 10 mg 20 mg 40 mg Amlodipine Placebo 4.9% 4.3% 5.6% 3.1% 5mg 3.7% 0.0% 1.2% 3.7% 10 mg 5.5% 6.8% 2.5% 5.6%
N=160-163 subjects per treatment group.
Amlodipine
Amlodipine has been evaluated for safety in more than 11,000 patients in U.S. and foreign clinical trials. Most adverse reactions reported during therapy with amlodipine were of mild or moderate severity. In controlled clinical trials directly comparing amlodipine (N=1730) in doses up to 10 mg to placebo (N=1250), discontinuation of amlodipine due to adverse reactions was required in only about 1.5% of amlodipine-treated patients and about 1% of placebo-treated patients. The most common side effects were headache and edema. The incidence (%) of dose-related side effects was as follows:
Adverse Event
Placebo
N=5202.5 mg
N=2755.0 mg
N=29610.0 mg
N=268Edema 0.6 1.8 3.0 10.8 Dizziness 1.5 1.1 3.4 3.4 Flushing 0.0 0.7 1.4 2.6 Palpitation 0.6 0.7 1.4 4.5 For several adverse experiences that appear to be drug- and dose-related, there was a greater incidence in women than men associated with amlodipine treatment as shown in the following table;
Olmesartan medoxomilAdverse Event
Placebo
Amlodipine
Male=%
(N=914)Female=%
(N=336)Male=%
(N=1218)Female=%
(N=512)Edema 1.4 5.1 5.6 14.6 Flushing 0.3 0.9 1.5 4.5 Palpitation 0.9 0.9 1.4 3.3 Somnolence 0.8 0.3 1.3 1.6
Olmesartan medoxomil has been evaluated for safety in more than 3825 patients/subjects, including more than 3275 patients treated for hypertension in controlled trials. This experience included about 900 patients treated for at least 6 months and more than 525 for at least 1 year. Treatment with olmesartan medoxomil was well tolerated, with an incidence of adverse events similar to that seen with placebo. Events were generally mild, transient, and without relationship to the dose of olmesartan medoxomil.
The overall frequency of adverse events was not dose-related. Analysis of gender, age, and race groups demonstrated no differences between olmesartan medoxomil- and placebo-treated patients. The rate of withdrawals due to adverse events in all trials of hypertensive patients was 2.4% (i.e., 79/3278) of patients treated with olmesartan medoxomil and 2.7% (i.e., 32/1179) of control patients. In placebo-controlled trials, the only adverse event that occurred in more than 1% of patients treated with olmesartan medoxomil and at a higher incidence in olmesartan medoxomil treated patients vs. placebo was dizziness (3% vs 1%).
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of the individual components of Azor. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Amlodipine. The following post-marketing event has been reported infrequently where a causal relationship is uncertain: gynecomastia. In post-marketing experience, jaundice and hepatic enzyme elevations (mostly consistent with cholestasis or hepatitis), in some cases severe enough to require hospitalization, have been reported in association with use of amlodipine.
Olmesartan medoxomil. The following adverse reactions have been reported in post-marketing experience:
Body as a Whole: asthenia, angioedema
Gastrointestinal: vomiting
Musculoskeletal: rhabdomyolysis
Urogenital System: acute renal failure
Skin and Appendages: alopecia, pruritus, urticaria
-
7 DRUG INTERACTIONS
Enter section text here
7.1 Drug Interactions with Azor
The pharmacokinetics of amlodipine and olmesartan medoxomil are not altered when the drugs are co-administered.
No drug interaction studies have been conducted with Azor and other drugs, although studies have been conducted with the individual amlodipine and olmesartan medoxomil components of Azor, as described below, and no significant drug interactions have been observed.
7.2 Drug Interactions with Amlodipine
In vitro data indicate that amlodipine has no effect on the human plasma protein binding of digoxin, phenytoin, warfarin, and indomethacin.
Effect of Other Agents on Amlodipine
Cimetidine: Co-administration of amlodipine with cimetidine did not alter the pharmacokinetics of amlodipine.
Grapefruit juice: Co-administration of 240 mL of grapefruit juice with a single oral dose of amlodipine 10 mg in 20 healthy volunteers had no significant effect on the pharmacokinetics of amlodipine.
Maalox® (antacid): Co-administration of the antacid Maalox® with a single dose of amlodipine had no significant effect on the pharmacokinetics of amlodipine.
Sildenafil: A single 100 mg dose of sildenafil in subjects with essential hypertension had no effect on the pharmacokinetic parameters of amlodipine. When amlodipine and sildenafil were used in combination, each agent independently exerted its own blood pressure lowering effect.
Effect of Amlodipine on Other Agents
Atorvastatin: Co-administration of multiple 10 mg doses of amlodipine with 80 mg of atorvastatin resulted in no significant change in the steady state pharmacokinetic parameters of atorvastatin.
Digoxin: Co-administration of amlodipine with digoxin did not change serum digoxin levels or digoxin renal clearance in normal volunteers.
Ethanol (alcohol): Single and multiple 10 mg doses of amlodipine had no significant effect on the pharmacokinetics of ethanol.
Warfarin: Co-administration of amlodipine with warfarin did not change the warfarin prothrombin response time.
In clinical trials, amlodipine has been safely administered with thiazide diuretics, beta-blockers, angiotensin-converting enzyme inhibitors, long-acting nitrates, sublingual nitroglycerin, digoxin, warfarin, non-steroidal anti-inflammatory drugs, antibiotics, and oral hypoglycemic drugs.
7.3 Drug Interactions with Olmesartan Medoxomil
No significant drug interactions were reported in studies in which olmesartan medoxomil was co-administered with digoxin or warfarin in healthy volunteers.
The bioavailability of olmesartan medoxomil was not significantly altered by the co-administration of antacids [Al(OH)3/Mg(OH)2].
Olmesartan medoxomil is not metabolized by the cytochrome P450 system and has no effects on P450 enzymes; thus, interactions with drugs that inhibit, induce, or are metabolized by those enzymes are not expected.
-
8 USE IN SPECIFIC POPULATIONS
Enter section text here
8.1 Pregnancy
Olmesartan medoxomil. Pregnancy Categories C (first trimester) and D (second and third trimesters). [See Warnings and Precautions (5.1)].
Amlodipine. No evidence of teratogenicity or other embryo/fetal toxicity was found when pregnant rats and rabbits were treated orally with amlodipine maleate at doses of up to 10 mg amlodipine/kg/day (respectively about 10 and 20 times the maximum recommended human dose of 10 mg amlodipine on a mg/m2 basis) during their respective periods of major organogenesis. (Calculations based on a patient weight of 60 kg). However, litter size was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly increased (about 5-fold) in rats receiving amlodipine maleate at a dose equivalent to 10 mg amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine maleate has been shown to prolong both the gestational period and the duration of labor in rats at this dose. There are no adequate and well-controlled studies in pregnant women. Amlodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
8.3 Nursing Mothers
It is not known whether the amlodipine or olmesartan medoxomil components of Azor are excreted in human milk, but olmesartan is secreted at low concentration in the milk of lactating rats. Because of the potential for adverse effects on the nursing infant, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of Azor in pediatric patients have not been established.
Amlodipine. The effect of amlodipine on blood pressure in patients less than 6 years of age is not known.
Olmesartan medoxomil. Safety and effectiveness of olmesartan medoxomil in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of subjects in the double-blind clinical study of Azor, 20% (384/1940) were 65 years of age or older and 3% (62/1940) were 75 years or older. No overall differences in safety or effectiveness were observed between subjects 65 years of age or older and younger subjects.
Elderly patients have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in patients ≥75 years old is recommended. The lowest dose of Azor is 5/20 mg; therefore, initial therapy with Azor is not recommended in patients ≥75 years old.
Amlodipine. Reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40% to 60%, and a lower initial dose may be required.
Olmesartan medoxomil. Of the total number of hypertensive patients receiving olmesartan medoxomil in clinical studies, more than 20% were 65 years of age and over, while more than 5% were 75 years of age and older. No overall differences in effectiveness or safety were observed between elderly patients and younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
There are no studies of Azor in patients with hepatic insufficiency, but both amlodipine and olmesartan medoxomil show moderate increases in exposure in patients with hepatic impairment. Use caution when administering Azor to patients with severe hepatic impairment.
Patients with hepatic impairment have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in patients with hepatic impairment is recommended. The lowest dose of Azor is 5/20 mg; therefore, initial therapy with Azor is not recommended in hepatically impaired patients.
8.7 Renal Impairment
There are no studies of Azor in patients with renal impairment.
Amlodipine. The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose.
Olmesartan medoxomil. Patients with renal insufficiency have elevated serum concentrations of olmesartan compared with patients with normal renal function. After repeated dosing, AUC was approximately tripled in patients with severe renal impairment (creatinine clearance <20 mL/min). No initial dosage adjustment is recommended for patients with moderate to marked renal impairment (creatinine clearance <40 mL/min).
8.8 Black Patients
Of the total number of subjects in the double-blind clinical study of Azor, 25% (481/1940) were black patients. Azor was effective in treating black patients (usually a low-renin population), and the magnitude of blood pressure reduction in black patients approached that observed for non-black patients.
-
10 OVERDOSAGE
There is no information on overdosage with Azor in humans.
Amlodipine. Single oral doses of amlodipine maleate equivalent to 40 mg amlodipine/kg and 100 mg amlodipine/kg in mice and rats, respectively, caused deaths. Single oral amlodipine maleate doses equivalent to 4 or more mg amlodipine/kg or higher in dogs (11 or more times the maximum recommended human dose on a mg/m2 basis) caused a marked peripheral vasodilation and hypotension.
Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension and possibly a reflex tachycardia. In humans, experience with intentional overdosage of amlodipine is limited.
If massive overdose should occur, active cardiac and respiratory monitoring should be instituted. Frequent blood pressure measurements are essential. Should hypotension occur, cardiovascular support including elevation of the extremities and the judicious administration of fluids should be initiated. If hypotension remains unresponsive to these conservative measures, administration of vasopressors (such as phenylephrine) should be considered with attention to circulating volume and urine output. Intravenous calcium gluconate may help to reverse the effects of calcium entry blockade. As amlodipine is highly protein bound, hemodialysis is not likely to be of benefit.
Olmesartan medoxomil. Limited data are available related to overdosage in humans. The most likely manifestations of overdosage would be hypotension and tachycardia; bradycardia could be encountered if parasympathetic (vagal) stimulation occurs. If symptomatic hypotension should occur, supportive treatment should be initiated. The dialyzability of olmesartan is unknown.
-
11 DESCRIPTION
Azor is a combination of the calcium channel receptor blocker (CCB) amlodipine besylate and the angiotensin II receptor blocker (ARB) olmesartan medoxomil.
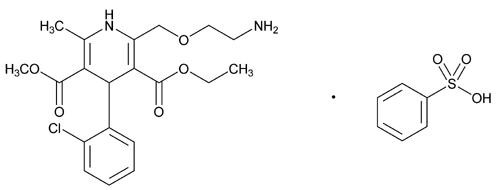
The amlodipine besylate component of Azor is chemically described as 3-ethyl-5-methyl (±)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-1,4-dihydro-6-methyl-3,5-pyridinedicarboxylate, monobenzenesulphonate. Its empirical formula is C20H25CIN2O5•C6H6O3S.
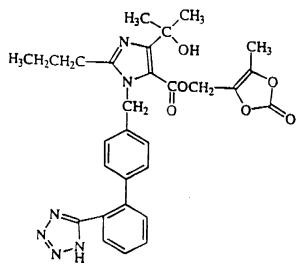
Olmesartan medoxomil, a prodrug, is hydrolyzed to olmesartan during absorption from the gastrointestinal tract.
The olmesartan medoxomil component of Azor is chemically described as 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2-propyl-1-[p-(o-1H-tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3-carbonate. Its empirical formula is C29H30N6O6.
The structural formula for amlodipine besylate is:
The structural formula for olmesartan medoxomil is:
Azor contains amlodipine besylate, a white to off-white crystalline powder, and olmesartan medoxomil, a white to light yellowish-white powder or crystalline powder. The molecular weights of amlodipine besylate and olmesartan medoxomil are 567.1 and 558.59, respectively. Amlodipine besylate is slightly soluble in water and sparingly soluble in ethanol. Olmesartan medoxomil is practically insoluble in water and sparingly soluble in methanol.
Each tablet of Azor also contains the following inactive ingredients: silicified microcrystalline cellulose, pregelatinized starch, croscarmellose sodium, and magnesium stearate. The color coatings contain polyvinyl alcohol, macrogol/polyethylene glycol 3350, titanium dioxide, talc, iron oxide yellow (5/40 mg, 10/20 mg, 10/40 mg tablets), iron oxide red (10/20 mg and 10/40 mg tablets), and iron oxide black (10/20 mg tablets).
-
12 CLINICAL PHARMACOLOGY
Enter section text here
12.1 Mechanism of Action
Azor. Azor is a combination of two antihypertensive drugs: a dihydropyridine calcium antagonist (calcium ion antagonist or slow-channel blocker), amlodipine besylate, and an angiotensin II receptor blocker, olmesartan medoxomil. The amlodipine component of Azor inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle, and the olmesartan medoxomil component of Azor blocks the vasoconstrictor effects of angiotensin II.
Amlodipine. Experimental data suggests that amlodipine binds to both dihydropyridine and nonhydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure.
Olmesartan medoxomil. Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation and renal reabsorption of sodium. Olmesartan blocks the vasoconstrictor effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor in vascular smooth muscle. Its action is, therefore, independent of the pathways for angiotensin II synthesis.
An AT2 receptor is found also in many tissues, but this receptor is not known to be associated with cardiovascular homeostasis. Olmesartan has more than a 12,500-fold greater affinity for the AT1 receptor than for the AT2 receptor.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is a mechanism of many drugs used to treat hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because olmesartan does not inhibit ACE (kininase II), it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and circulating angiotensin II levels do not overcome the effect of olmesartan on blood pressure.
12.2 Pharmacodynamics
Amlodipine. Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing.
With chronic once daily oral administration, antihypertensive effectiveness is maintained for at least 24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The magnitude of reduction in blood pressure with amlodipine is also correlated with the height of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105-114 mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure 90-104 mmHg). Normotensive subjects experienced no clinically significant change in blood pressures (+1/-2 mmHg).
In hypertensive patients with normal renal function, therapeutic doses of amlodipine resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and effective renal plasma flow without change in filtration fraction or proteinuria.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and man, even when co-administered with beta-blockers to man. Similar findings, however, have been observed in normals or well-compensated patients with heart failure with agents possessing significant negative inotropic effects.
Amlodipine does not change sinoatrial nodal function or atrioventricular conduction in intact animals or man. In clinical studies in which amlodipine was administered in combination with beta-blockers to patients with either hypertension or angina, no adverse effects on electrocardiographic parameters were observed.
Olmesartan medoxomil. Olmesartan medoxomil doses of 2.5 mg to 40 mg inhibit the pressor effects of angiotensin I infusion. The duration of the inhibitory effect was related to dose, with doses of olmesartan medoxomil >40 mg giving >90% inhibition at 24 hours.
Plasma concentrations of angiotensin I and angiotensin II and plasma renin activity (PRA) increase after single and repeated administration of olmesartan medoxomil to healthy subjects and hypertensive patients. Repeated administration of up to 80 mg olmesartan medoxomil had minimal influence on aldosterone levels and no effect on serum potassium.
12.3 Pharmacokinetics
The pharmacokinetics of amlodipine and olmesartan medoxomil from Azor are equivalent to the pharmacokinetics of amlodipine and olmesartan medoxomil when administered separately. The bioavailability of both components is well below 100%, but neither component is affected by food. The effective half-lives of amlodipine (45±11 hours) and olmesartan (7±1 hours) result in a 2- to 3- fold accumulation for amlodipine and negligible accumulation for olmesartan with once-daily dosing.
Amlodipine. After oral administration of therapeutic doses of amlodipine, absorption produces peak plasma concentrations between 6 and 12 hours. Absolute bioavailability is estimated as between 64% and 90%.
Olmesartan medoxomil. Olmesartan medoxomil is rapidly and completely bioactivated by ester hydrolysis to olmesartan during absorption from the gastrointestinal tract. The absolute bioavailability of olmesartan medoxomil is approximately 26%. After oral administration, the peak plasma concentration (Cmax) of olmesartan is reached after 1 to 2 hours. Food does not affect the bioavailability of olmesartan medoxomil.
DistributionAmlodipine. Ex vivo studies have shown that approximately 93% of the circulating drug is bound to plasma proteins in hypertensive patients. Steady-state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily dosing.
Olmesartan medoxomil. The volume of distribution of olmesartan is approximately 17 L. Olmesartan is highly bound to plasma proteins (99%) and does not penetrate red blood cells. The protein binding is constant at plasma olmesartan concentrations well above the range achieved with recommended doses.
In rats, olmesartan crossed the blood-brain barrier poorly, if at all. Olmesartan passed across the placental barrier in rats and was distributed to the fetus. Olmesartan was distributed to milk at low levels in rats.
Metabolism and ExcretionAmlodipine. Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism. Elimination from the plasma is biphasic with a terminal elimination half-life of about 30 to 50 hours. Ten percent of the parent compound and 60% of the metabolites are excreted in the urine.
Olmesartan medoxomil. Following the rapid and complete conversion of olmesartan medoxomil to olmesartan during absorption, there is virtually no further metabolism of olmesartan. Total plasma clearance of olmesartan is 1.3 L/h, with a renal clearance of 0.6 L/h. Approximately 35% to 50% of the absorbed dose is recovered in urine while the remainder is eliminated in feces via the bile.
Olmesartan appears to be eliminated in a biphasic manner with a terminal elimination half-life of approximately 13 hours. Olmesartan shows linear pharmacokinetics following single oral doses of up to 320 mg and multiple oral doses of up to 80 mg. Steady-state levels of olmesartan are achieved within 3 to 5 days and no accumulation in plasma occurs with once-daily dosing.
GeriatricThe pharmacokinetic properties of Azor in the elderly are similar to those of the individual components.
Amlodipine. Elderly patients have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%, and a lower initial dose may be required.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil were studied in the elderly (>65 years). Overall, maximum plasma concentrations of olmesartan were similar in young adults and the elderly. Modest accumulation of olmesartan was observed in the elderly with repeated dosing; AUCѕѕ, τ was 33% higher in elderly patients, corresponding to an approximate 30% reduction in CLR.
PediatricAmlodipine. Sixty-two hypertensive patients aged 6 to 17 years received doses of amlodipine between 1.25 mg and 20 mg. Weight-adjusted clearance and volume of distribution were similar to values in adults.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil have not been investigated in patients <18 years of age.
GenderPopulation pharmacokinetic analysis indicated that female patients had approximately 15% smaller clearances of olmesartan than male patients. Gender had no effect on the clearance of amlodipine.
Olmesartan medoxomil. Minor differences were observed in the pharmacokinetics of olmesartan medoxomil in women compared to men. AUC and Cmax were 10% to 15% higher in women than in men.
Renal InsufficiencyAmlodipine. The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose.
Olmesartan medoxomil. In patients with renal insufficiency, serum concentrations of olmesartan were elevated compared to subjects with normal renal function. After repeated dosing, the AUC was approximately tripled in patients with severe renal impairment (creatinine clearance <20 mL/min). The pharmacokinetics of olmesartan medoxomil in patients undergoing hemodialysis has not been studied. No initial dosage adjustment is recommended for patients with moderate to marked renal impairment (creatinine clearance <40 mL/min).
Hepatic InsufficiencyAmlodipine. Patients with hepatic insufficiency have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%.
Olmesartan medoxomil. Increases in AUC0-∞ and Cmax were observed in patients with moderate hepatic impairment compared to those in matched controls, with an increase in AUC of about 60%.
Heart FailureAmlodipine. Patients with heart failure have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%.
-
13 NONCLINICAL TOXICOLOGY
Enter section text here
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Amlodipine. Rats and mice treated with amlodipine maleate in the diet for up to two years, at concentrations calculated to provide daily dosage levels of amlodipine 0.5, 1.25, and 2.5 mg/kg/day showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on a mg/m2 basis, similar to the maximum recommended human dose (MRHD) of amlodipine 10 mg/day. For the rat, the highest dose was, on a mg/m2 basis, about two and a half times the MRHD. (Calculations based on a 60 kg patient.)
Mutagenicity studies conducted with amlodipine maleate revealed no drug related effects at either the gene or chromosome level.
There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days and females for 14 days prior to mating) at doses of amlodipine up to 10 mg/kg/day (about 10 times the MRHD of 10 mg/day on a mg/m2 basis).
Olmesartan medoxomil. Olmesartan was not carcinogenic when administered by dietary administration to rats for up to 2 years. The highest dose tested (2000 mg/kg/day) was, on a mg/m2 basis, about 480 times the maximum recommended human dose (MRHD) of 40 mg/day. Two carcinogenicity studies conducted in mice, a 6-month gavage study in the p53 knockout mouse and a 6-month dietary administration study in the Hras2 transgenic mouse, at doses of up to 1000 mg/kg/day (about 120 times the MRHD), revealed no evidence of a carcinogenic effect of olmesartan. Both olmesartan medoxomil and olmesartan tested negative in the in vitro Syrian hamster embryo cell transformation assay and showed no evidence of genetic toxicity in the Ames (bacterial mutagenicity) test. However, both were shown to induce chromosomal aberrations in cultured cells in vitro (Chinese hamster lung) and tested positive for thymidine kinase mutations in the in vitro mouse lymphoma assay. Olmesartan medoxomil tested negative in vivo for mutations in the MutaMouse intestine and kidney and for clastogenicity in mouse bone marrow (micronucleus test) at oral doses of up to 2000 mg/kg (olmesartan not tested).
Fertility of rats was unaffected by administration of olmesartan at dose levels as high as 1000 mg/kg/day (240 times the MRHD) in a study in which dosing was begun 2 (female) or 9 (male) weeks prior to mating.
-
14 CLINICAL STUDIES
Enter section text here
14.1 Azor
An 8-week multicenter, randomized, double-blind, placebo controlled, parallel group factorial study in patients with mild to severe hypertension was conducted to determine if treatment with Azor was associated with clinically significant reduction in blood pressure compared to the respective monotherapies. The study randomized 1940 patients equally to one of the following 12 treatment arms: placebo, monotherapy treatment with amlodipine 5 mg or 10 mg, monotherapy treatment with olmesartan medoxomil 10 mg, 20 mg, or 40 mg, or combination therapy with amlodipine/olmesartan medoxomil at doses of 5/10 mg, 5/20 mg, 5/40 mg, 10/10 mg, 10/20 mg, and 10/40 mg. Patients discontinued their prior antihypertensive treatment. The mean baseline blood pressure of the study population was 164/102 mmHg. Of the total cohort, 970 patients were treated with the combination as initial therapy.
Treatment with Azor resulted in statistically significant greater reductions in diastolic and systolic blood pressure compared to the respective monotherapy components.
The following table presents the results for mean reduction in seated systolic and diastolic blood pressure following 8 weeks of treatment with Azor. Placebo-adjusted reductions from baseline in blood pressure were progressively greater with increases in dose of both amlodipine and olmesartan medoxomil components of Azor.
Reduction in Seated Systolic/Diastolic Blood Pressure (mmHg): Combination Therapy vs. Monotherapy Components (Double-Blind Treatment Period)
Olmesartan medoxomil (mmHg) Placebo 10 mg 20 mg 40 mg Amlodipine Placebo Mean Change -5/-3 -12/-8 -14/-9 -16/-10
Placebo-Adjusted Mean Change -- -8/-5 -10/-6 -13/-7 5 mg Mean Change -15/-9 -24/-14 -24/-14 -25/-16
Placebo-Adjusted Mean Change -12/-7 -20/-11 -20/-11 -22/-13 10mg Mean Change -20/-13 -25/-16 -29/-17 -30/-19
Placebo-Adjusted Mean Change -16/-10 -22/-13 -25/-14 -26/-16 The antihypertensive effect of Azor was similar in patients with and without prior antihypertensive medication use, in patients with and without diabetes, in patients >65 years of age and <65 years of age, and in women and men. Limited data exist in patients >75 years of age.
Azor was effective in treating black patients (usually a low-renin population), and the magnitude of blood pressure reduction in black patients approached that observed for non-Black patients. This effect in black patients has been seen with ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
The blood pressure lowering effect was maintained throughout the 24-hour period with Azor once daily, with trough-to-peak ratios for systolic and diastolic response between 71% and 82%.
Upon completing the 8-week, double-blind, placebo-controlled study, 1684 patients entered a 44-week open-label extension and received combination therapy with amlodipine 5 mg plus olmesartan medoxomil 40 mg. During the open-label extension, patients whose blood pressure was not adequately controlled (i.e., did not achieve a blood pressure goal of <140/90 mmHg, or <130/80 mmHg for those patients with diabetes) on amlodipine/olmesartan medoxomil 5/40 mg were titrated to amlodipine/olmesartan medoxomil 10/40 mg. Patients whose blood pressure was still not adequately controlled were offered additional hydrochlorothiazide 12.5 mg and subsequently 25 mg as required to achieve adequate blood pressure goal.
14.2 Amlodipine
The antihypertensive efficacy of amlodipine has been demonstrated in a total of 15 double-blind, placebo-controlled, randomized studies involving 800 patients on amlodipine and 538 on placebo. Once daily administration produced statistically significant placebo-corrected reductions in supine and standing blood pressures at 24 hours postdose, averaging about 12/6 mmHg in the standing position and 13/7 mmHg in the supine position in patients with mild to moderate hypertension. Maintenance of the blood pressure effect over the 24-hour dosing interval was observed, with little difference in peak and trough effect.
14.3 Olmesartan Medoxomil
The antihypertensive effects of olmesartan medoxomil have been demonstrated in seven placebo-controlled studies at doses ranging from 2.5 mg to 80 mg for 6 to 12 weeks, each showing statistically significant reductions in peak and trough blood pressure. A total of 2693 patients (2145 olmesartan medoxomil; 548 placebo) with essential hypertension were studied. The blood pressure lowering effect was maintained throughout the 24-hour period with olmesartan medoxomil once daily, with trough-to-peak ratios for systolic and diastolic response between 60% and 80%.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Azor tablets contain amlodipine besylate at a dose equivalent to 5 or 10 mg amlodipine and olmesartan medoxomil in the strengths described below.
Azor tablets are differentiated by tablet color/size and are debossed with an individual product tablet code on one side. Azor tablets are supplied for oral administration in the following strength and package configurations:
Tablet Strength
(amlodipine equivalent/
olmesartan
medoxomil) mgPackage Configuration
NDC#
Product Code
Tablet Color
5/20 mg
Bottle of 30
54868-6036-0 C73 White 10/40 mg Bottle of 30
54868-6250-0 C77 Brownish Red Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Physicians should instruct female patients of childbearing age about the consequences of second and third trimester exposure to drugs that act on the renin-angiotensin system and they should be told that these consequences do not appear to have resulted from intrauterine drug exposure that has been limited to the first trimester. These patients should be informed to report pregnancies to their physicians as soon as possible. [See Warnings and Precautions (5.1) and Use in Specific Populations (8.1) ].
Manufactured for Daiichi Sankyo, Inc., Parsippany, New Jersey 07054
Manufactured by Daiichi Sankyo Europe GmbH, GermanyCopyright © Daiichi Sankyo, Inc. 2007. All rights reserved.
Relabeling of "Additional" barcode label by: Physicians Total Care, Inc., Tulsa, OK 74146
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:54868-6036(NDC:65597-110) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 5 mg OLMESARTAN MEDOXOMIL (UNII: 6M97XTV3HD) (OLMESARTAN - UNII:8W1IQP3U10) OLMESARTAN MEDOXOMIL 20 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TALC (UNII: 7SEV7J4R1U) Product Characteristics Color white (white) Score no score Shape ROUND (round) Size 6mm Flavor Imprint Code C73 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:54868-6036-0 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022100 06/02/2009 AZOR
amlodipine besylate and olmesartan medoxomil tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:54868-6250(NDC:65597-113) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 10 mg OLMESARTAN MEDOXOMIL (UNII: 6M97XTV3HD) (OLMESARTAN - UNII:8W1IQP3U10) OLMESARTAN MEDOXOMIL 40 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) STARCH, CORN (UNII: O8232NY3SJ) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color red Score no score Shape ROUND Size 8mm Flavor Imprint Code C77 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:54868-6250-0 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022100 04/26/2011 Labeler - Physicians Total Care, Inc. (194123980) Establishment Name Address ID/FEI Business Operations Physicians Total Care, Inc. 194123980 relabel