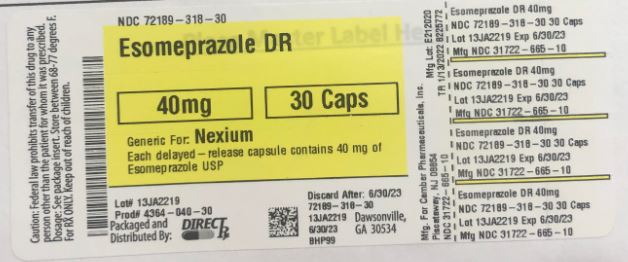
Label: ESOMEPRAZOLE MAGNESIUM capsule, delayed release
- NDC Code(s): 72189-318-30
- Packager: Direct Rx
- This is a repackaged label.
- Source NDC Code(s): 31722-665
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated March 3, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
INDICATIONS & USAGE
1.1 Treatment of Gastroesophageal Reflux Disease (GERD)
Healing of Erosive Esophagitis
Esomeprazole magnesium delayed-release capsules are indicated for the short-term treatment (4 to 8 weeks) in the healing and symptomatic resolution of diagnostically confirmed erosive esophagitis. For those patients who have not healed after 4 to 8 weeks of treatment, an additional 4 to 8 week course of esomeprazole magnesium delayed-release capsules may be considered.
Maintenance of Healing of Erosive Esophagitis
Esomeprazole magnesium delayed-release capsules are indicated to maintain symptom resolution and healing of erosive esophagitis. Controlled studies do not extend beyond 6 months.
Symptomatic Gastroesophageal Reflux Disease
Esomeprazole magnesium delayed-release capsules are indicated for short-term treatment (4 to 8 weeks) of heartburn and other symptoms associated with GERD in adults and children 1 year or older.1.2 Risk Reduction of NSAID-Associated Gastric Ulcer
Esomeprazole magnesium delayed-release capsules are indicated for the reduction in the occurrence of gastric ulcers associated with continuous NSAID therapy in patients at risk for developing gastric ulcers. Patients are considered to be at risk due to their age (≥ 60) and/or documented history of gastric ulcers. Controlled studies do not extend beyond 6 months.
1.3 H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Triple Therapy (esomeprazole magnesium delayed-release capsules plus amoxicillin and clarithromycin): Esomeprazole magnesium delayed-release capsules, in combination with amoxicillin and clarithromycin, is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or history of within the past 5 years) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Dosage and Administration (2) and Clinical Studies (14)].
In patients who fail therapy, susceptibility testing should be done. If resistance to clarithromycin is demonstrated or susceptibility testing is not possible, alternative antimicrobial therapy should be instituted [see Clinical Pharmacology (12.4) and the prescribing information for clarithromycin].1.4 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
Esomeprazole magnesium delayed-release capsules are indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison Syndrome.
-
DOSAGE & ADMINISTRATION
Esomeprazole magnesium is supplied as delayed-release capsules for oral administration. The recommended dosages are outlined in Table 1. Esomeprazole magnesium delayed-release capsules should be taken at least one hour before meals.
The duration of proton pump inhibitor administration should be based on available safety and efficacy data specific to the defined indication and dosing frequency, as described in the prescribing information, and individual patient medical needs. Proton pump inhibitor treatment should only be initiated and continued if the benefits outweigh the risks of treatment.
Table 1: Recommended Dosage Schedule for Esomeprazole Magnesium Delayed-Release Capsules
Indication
Dose
Frequency
Gastroesophageal Reflux Disease (GERD)
Healing of Erosive Esophagitis
20 mg or 40 mg
Once Daily for 4 to 8 Weeks1
Maintenance of Healing of Erosive Esophagitis
20 mg
Once Daily2
Symptomatic Gastroesophageal Reflux Disease
20 mg
Once Daily for 4 Weeks3
Pediatric GERD
12 to 17 Year Olds
Healing of Erosive Esophagitis
20 mg or 40 mg
Once Daily for 4 to 8 Weeks
Symptomatic GERD
20 mg
Once Daily for 4 Weeks
1 to 11 Year Olds4
Short-term Treatment of Symptomatic GERD
10 mg
Once Daily for up to 8 Weeks
Healing of Erosive Esophagitis
weight < 20 kg
10 mg
Once Daily for 8 Weeks
weight ≥ 20 kg
10 mg or 20 mg
Once Daily for 8 Weeks
Risk Reduction of NSAID-Associated Gastric Ulcer
20 mg or 40 mg
Once Daily for up to 6 months2
H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Triple Therapy:
Esomeprazole
40 mg
Once Daily for 10 Day
Amoxicillin
1000 mg
Twice Daily for 10 Days
Clarithromycin
500 mg
Twice Daily for 10 Days
Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
40 mg6
Twice Daily71[See Clinical Studies (14.1)]The majority of patients are healed within 4 to 8 weeks. For patients who do not heal after 4 to 8 weeks, an additional 4 to 8 weeks of treatment may be considered.
2 Controlled studies did not extend beyond six months.
3 If symptoms do not resolve completely after 4 weeks, an additional 4 weeks of treatment may be considered.
4 Doses over 1 mg/kg/day have not been studied.
5. Doses over 1.33 mg/kg/day have not been studied.
6 The dosage of esomeprazole magnesium delayed-release capsules in patients with pathological hypersecretory conditions varies with the individual patient. Dosage regimens should be adjusted to individual patient needs.
7 Doses up to 240 mg daily have been administered [see Drug Interactions (7)] .
Please refer to amoxicillin and clarithromycin prescribing information for Contraindications, Warnings, and dosing in elderly and renally-impaired patients.Specific Populations
Hepatic Insufficiency
In patients with mild to moderate liver impairment (Child-Pugh Classes A and B), no dosage adjustment is necessary. For patients with severe liver impairment (Child-Pugh Class C), a dose of 20 mg of esomeprazole magnesium delayed-release capsules should not be exceeded [see Clinical Pharmacology (12.3)] .Directions for use specific to the route and available methods of administration for each of these dosage forms are presented in Table 2.
Table 2: Administration Options
Administration Options
(See text following table for additional instructions.)
Dosage Form
Route
Options
Delayed-Release Capsules
Oral
Capsule can be swallowed whole.
-or-
Capsule can be opened and mixed with applesauce.
Delayed-Release Capsules
Nasogastric Tube
Capsule can be opened and the intact granules emptied into a syringe and delivered through the nasogastric tube.Esomeprazole Magnesium Delayed-Release Capsules
Esomeprazole Magnesium Delayed-Release Capsules should be swallowed whole.
Alternatively, for patients who have difficulty swallowing capsules, one tablespoon of applesauce can be added to an empty bowl and the esomeprazole magnesium delayed-release capsule can be opened, and the granules inside the capsule carefully emptied onto the applesauce. The granules should be mixed with the applesauce and then swallowed immediately: do not store for future use. The applesauce used should not be hot and should be soft enough to be swallowed without chewing. The granules should not be chewed or crushed. If the granules/applesauce mixture is not used in its entirety, the remaining mixture should be discarded immediately.
For patients who have a nasogastric tube in place, esomeprazole magnesium delayed-release capsules can be opened and the intact granules emptied into a 60 mL catheter tipped syringe and mixed with 50 mL of water. It is important to only use a catheter tipped syringe when administering esomeprazole magnesium delayed-release capsules through a nasogastric tube. Replace the plunger and shake the syringe vigorously for 15 seconds. Hold the syringe with the tip up and check for granules remaining in the tip. Attach the syringe to a nasogastric tube and deliver the contents of the syringe through the nasogastric tube into the stomach. After administering the granules, the nasogastric tube should be flushed with additional water. Do not administer the granules if they have dissolved or disintegrated.
The mixture must be used immediately after preparation.
-
DOSAGE FORMS & STRENGTHS
Esomeprazole magnesium delayed-release capsules USP, 20 mg are white opaque size '4' hard gelatin capsule imprinted with "H" on cap and 'E2' on body filled with off white to pale yellow pellets.
Esomeprazole magnesium delayed-release capsules USP, 40 mg are white opaque size '3' hard gelatin capsule imprinted with "H" on cap and 'E3' on body filled with off white to pale yellow pellets.
-
CONTRAINDICATIONS
Esomeprazole magnesium delayed-release capsules are contraindicated in patients with known hypersensitivity to substituted benzimidazoles or to any component of the formulation. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute interstitial nephritis, and urticaria [see Adverse Reactions (6)].
For information about contraindications of antibacterial agents (clarithromycin and amoxicillin) indicated in combination with esomeprazole magnesium delayed-release capsules, refer to the CONTRAINDICATIONS section of their package inserts. -
WARNINGS AND PRECAUTIONS
5.1 Presence of Gastric Malignancy
In adults, symptomatic response to therapy with esomeprazole magnesium delayed-release capsules does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing in adult patients who have a suboptimal response or an early symptomatic relapse after completing treatment with a PPI. In older patients, also consider an endoscopy.
5.2 Acute Interstitial Nephritis
Acute interstitial nephritis has been observed in patients taking PPIs including esomeprazole magnesium delayed-release capsules. Acute interstitial nephritis may occur at any point during PPI therapy and is generally attributed to an idiopathic hypersensitivity reaction. Discontinue esomeprazole magnesium delayed-release capsules if acute interstitial nephritis develops [see Contraindications (4)].
5.3 Clostridium difficile-Associated Diarrhea
Published observational studies suggest that PPI therapy like esomeprazole magnesium delayed-release capsules may be associated with an increased risk of Clostridium difficile-associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2) ].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents. For more information specific to antibacterial agents (clarithromycin and amoxicillin) indicated for use in combination with esomeprazole magnesium delayed-release capsules, refer to Warnings and Precautions section of the corresponding prescribing information.5.4 Bone Fracture
Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2) and Adverse Reactions (6.2)].
5.5 Cutaneous and Systemic Lupus Erythematosus
Cutaneous lupus erythematosus (CLE) and systemic lupus erythematosus (SLE) have been reported in patients taking PPIs, including esomeprazole. These events have occurred as both new onset and an exacerbation of existing autoimmune disease. The majority of PPI-induced lupus erythematosus cases were CLE.
The most common form of CLE reported in patients treated with PPIs was subacute CLE (SCLE) and occurred within weeks to years after continuous drug therapy in patients ranging from infants to the elderly. Generally, histological findings were observed without organ involvement.
Systemic lupus erythematosus (SLE) is less commonly reported than CLE in patients receiving PPIs. PPI associated SLE is usually milder than non-drug induced SLE. Onset of SLE typically occurred within days to years after initiating treatment primarily in patients ranging from young adults to the elderly. The majority of patients presented with rash; however, arthralgia and cytopenia were also reported.
Avoid administration of PPIs for longer than medically indicated. If signs or symptoms consistent with CLE or SLE are noted in patients receiving esomeprazole magnesium delayed-release capsules, discontinue the drug and refer the patient to the appropriate specialist for evaluation. Most patients improve with discontinuation of the PPI alone in 4 to 12 weeks. Serological testing (e.g., ANA) may be positive and elevated serological test results may take longer to resolve than clinical manifestations.5.6 Interaction with Clopidogrel
Avoid concomitant use of esomeprazole magnesium delayed-release capsules with clopidogrel. Clopidogrel is a prodrug. Inhibition of platelet aggregation by clopidogrel is entirely due to an active metabolite. The metabolism of clopidogrel to its active metabolite can be impaired by use with concomitant medications, such as esomeprazole, that inhibit CYP2C19 activity. Concomitant use of clopidogrel with 40 mg esomeprazole reduces the pharmacological activity of clopidogrel. When using esomeprazole magnesium delayed-release capsules consider alternative anti-platelet therapy [see Drug Interactions (7.3) and Clinical Pharmacology (12.3)].
5.7 Cyanocobalamin (Vitamin B-12) Deficiency
Daily treatment with any acid-suppressing medications over a long period of time (e.g., longer than 3 years) may lead to malabsorption of cyanocobalamin (vitamin B-12) caused by hypo- or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed.
5.8 Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].5.9 Interaction with St. John’s Wort or Rifampin
Drugs which induce CYP2C19 or CYP3A4 (such as St. John's Wort or rifampin) can substantially decrease esomeprazole concentrations [see Drug Interactions (7.3)] . Avoid concomitant use of esomeprazole magnesium delayed-release capsules with St. John's Wort or rifampin.
5.10 Interactions with Diagnostic Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop esomeprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g., for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary [see Clinical Pharmacology (12.2)].
5.11 Interaction with Methotrexate
Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (7.7)].
5.12 Fundic Gland Polyps
PPI use is associated with an increased risk of fundic gland polyps that increases with long-term use, especially beyond one year. Most PPI users who developed fundic gland polyps were asymptomatic and fundic gland polyps were identified incidentally on endoscopy. Use the shortest duration of PPI therapy appropriate to the condition being treated.
-
ADVERSE REACTIONS
The following serious adverse reactions are described below and elsewhere in labeling:
• Acute Interstitial Nephritis [see Warnings and Precautions (5.2)]
• Clostridium difficile-Associated Diarrhea [see Warnings and Precautions (5.3)]
• Bone Fracture [see Warnings and Precautions (5.4)]
• Cutaneous and Systemic Lupus Erythematosus [see Warnings and Precautions (5.5)]
• Cyanocobalamin (Vitamin B-12) Deficiency [see Warnings and Precautions (5.7)]
• Hypomagnesemia [see Warnings and Precautions (5.8)]• Fundic Gland Polyps [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
The safety of esomeprazole magnesium delayed-release capsules were evaluated in over 15,000 patients (aged 18 to 84 years) in clinical trials worldwide including over 8,500 patients in the United States and over 6,500 patients in Europe and Canada. Over 2,900 patients were treated in long-term studies for up to 6 to 12 months. In general, esomeprazole magnesium delayed-release capsules were well tolerated in both short and long-term clinical trials.
The safety in the treatment of healing of erosive esophagitis was assessed in four randomized comparative clinical trials, which included 1,240 patients on esomeprazole magnesium delayed-release capsules 20 mg, 2,434 patients on esomeprazole magnesium delayed-release capsules 40 mg, and 3,008 patients on omeprazole 20 mg daily. The most frequently occurring adverse reactions (≥1%) in all three groups were headache (5.5, 5, and 3.8, respectively) and diarrhea (no difference among the three groups). Nausea, flatulence, abdominal pain, constipation, and dry mouth occurred at similar rates among patients taking esomeprazole magnesium delayed-release capsules or omeprazole.
Additional adverse reactions that were reported as possibly or probably related to esomeprazole magnesium delayed-release capsules with an incidence <1% are listed below by body system:
Body as a Whole: abdomen enlarged, allergic reaction, asthenia, back pain, chest pain, substernal chest pain, facial edema, peripheral edema, hot flushes, fatigue, fever, flu-like disorder, generalized edema, leg edema, malaise, pain, rigors;
Cardiovascular: flushing, hypertension, tachycardia;
Endocrine: goiter;
Gastrointestinal: bowel irregularity, constipation aggravated, dyspepsia, dysphagia, dysplasia GI, epigastric pain, eructation, esophageal disorder, frequent stools, gastroenteritis, GI hemorrhage, GI symptoms not otherwise specified, hiccup, melena, mouth disorder, pharynx disorder, rectal disorder, serum gastrin increased, tongue disorder, tongue edema, ulcerative stomatitis, vomiting;
Hearing: earache, tinnitus;
Hematologic: anemia, anemia hypochromic, cervical lymphadenopathy, epistaxis, leukocytosis, leukopenia, thrombocytopenia;
Hepatic: bilirubinemia, hepatic function abnormal, SGOT increased, SGPT increased;
Metabolic/Nutritional: glycosuria, hyperuricemia, hyponatremia, increased alkaline phosphatase, thirst, vitamin B12 deficiency, weight increase, weight decrease;
Musculoskeletal: arthralgia, arthritis aggravated, arthropathy, cramps, fibromyalgia syndrome, hernia, polymyalgia rheumatica;
Nervous System/Psychiatric: anorexia, apathy, appetite increased, confusion, depression aggravated, dizziness, hypertonia, nervousness, hypoesthesia, impotence, insomnia, migraine, migraine aggravated, paresthesia, sleep disorder, somnolence, tremor, vertigo, visual field defect;
Reproductive: dysmenorrhea, menstrual disorder, vaginitis;
Respiratory: asthma aggravated, coughing, dyspnea, larynx edema, pharyngitis, rhinitis, sinusitis;
Skin and Appendages: acne, angioedema, dermatitis, pruritus, pruritus ani, rash, rash erythematous, rash maculo-papular, skin inflammation, sweating increased, urticaria;
Special Senses: otitis media, parosmia, taste loss, taste perversion;
Urogenital: abnormal urine, albuminuria, cystitis, dysuria, fungal infection, hematuria, micturition frequency, moniliasis, genital moniliasis, polyuria;
Visual: conjunctivitis, vision abnormal.
The following potentially clinically significant laboratory changes in clinical trials, irrespective of relationship to esomeprazole magnesium delayed-release capsules, were reported in ≤1% of patients: increased creatinine, uric acid, total bilirubin, alkaline phosphatase, ALT, AST, hemoglobin, white blood cell count, platelets, serum gastrin, potassium, sodium, thyroxine and thyroid stimulating hormone [see Clinical Pharmacology (12) ].Decreases were seen in hemoglobin, white blood cell count, platelets, potassium, sodium, and thyroxine.
Endoscopic findings that were reported as adverse reactions include: duodenitis, esophagitis, esophageal stricture, esophageal ulceration, esophageal varices, gastric ulcer, gastritis, hernia, benign polyps or nodules, Barrett’s esophagus, and mucosal discoloration.
The incidence of treatment-related adverse reactions during 6-month maintenance treatment was similar to placebo. There were no differences in types of related adverse reactions seen during maintenance treatment up to 12 months compared to short-term treatment.
Two placebo-controlled studies were conducted in 710 patients for the treatment of symptomatic gastroesophageal reflux disease. The most common adverse reactions that were reported as possibly or probably related to esomeprazole magnesium delayed-release capsules were diarrhea (4.3%), headache (3.8%), and abdominal pain (3.8%).
Pediatrics
The safety of esomeprazole magnesium delayed-release capsules were evaluated in 316 pediatric and adolescent patients aged 1 to 17 years in four clinical trials for the treatment of symptomatic GERD [see Clinical Studies(14.2)]. In 109 pediatric patients aged 1 to 11 years, the most frequently reported (at least 1%) treatment-related adverse reactions in these patients were diarrhea (2.8%), headache (1.9%) and somnolence (1.9%). In 149 pediatric patients aged 12 to 17 years the most frequently reported (at least 2%) treatment-related adverse reactions in these patients were headache (8.1%), abdominal pain (2.7%), diarrhea (2%), and nausea (2%).
No new safety concerns were identified in pediatric patients.
Combination Treatment with Amoxicillin and Clarithromycin
In clinical trials using combination therapy with esomeprazole magnesium delayed-release capsules plus amoxicillin and clarithromycin, no additional adverse reactions specific to these drug combinations were observed. Adverse reactions that occurred were limited to those observed when using esomeprazole magnesium delayed-release capsules, amoxicillin, or clarithromycin alone.
The most frequently reported drug-related adverse reactions for patients who received triple therapy for 10 days were diarrhea (9.2%), taste perversion (6.6%), and abdominal pain (3.7%). No treatment-emergent adverse reactions were observed at higher rates with triple therapy than were observed with esomeprazole magnesium delayed-release capsules alone.
For more information on adverse reactions with amoxicillin or clarithromycin, refer to their package inserts, Adverse Reactions sections.
In clinical trials using combination therapy with esomeprazole magnesium delayed-release capsules plus amoxicillin and clarithromycin, no additional increased laboratory abnormalities particular to these drug combinations were observed.
For more information on laboratory changes with amoxicillin or clarithromycin, refer to their package inserts, Adverse Reactions section.6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of esomeprazole magnesium delayed-release capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reports are listed below by body system:
Blood and Lymphatic: agranulocytosis, pancytopenia;
Eye: blurred vision;
Gastrointestinal: pancreatitis; stomatitis; microscopic colitis; fundic gland polyps;
Hepatobiliary: hepatic failure, hepatitis with or without jaundice;
Immune System: anaphylactic reaction/shock; systemic lupus erythematosus;
Infections and Infestations: GI candidiasis; Clostridium difficile-associated diarrhea;
Metabolism and nutritional disorders: hypomagnesemia, with or without hypocalcemia and/or hypokalemia;
Musculoskeletal and Connective Tissue: muscular weakness, myalgia, bone fracture;
Nervous System: hepatic encephalopathy, taste disturbance;
Psychiatric: aggression, agitation, depression, hallucination;
Renal and Urinary: interstitial nephritis;
Reproductive System and Breast: gynecomastia;
Respiratory, Thoracic, and Mediastinal: bronchospasm;
Skin and Subcutaneous Tissue: alopecia, erythema multiforme, hyperhidrosis, photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal), cutaneous lupus erythematosus. -
DRUG INTERACTIONS
7.1 Interference with Antiretroviral Therapy
Concomitant use of atazanavir and nelfinavir with proton pump inhibitors is not recommended. Co-administration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and may result in a loss of therapeutic effect and the development of drug resistance. Co-administration of saquinavir with proton pump inhibitors is expected to increase saquinavir concentrations, which may increase toxicity and require dose reduction.
Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with some antiretroviral drugs. The clinical importance and the mechanisms behind these interactions are not always known. Increased gastric pH during omeprazole treatment may change the absorption of the antiretroviral drug. Other possible interaction mechanisms are via CYP2C19.
Reduced concentrations of atazanavir and nelfinavir
For some antiretroviral drugs, such as atazanavir and nelfinavir, decreased serum levels have been reported when given together with omeprazole. Following multiple doses of nelfinavir (1,250 mg, twice daily) and omeprazole (40 mg daily), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75% respectively for nelfinavir and M8. Following multiple doses of atazanavir (400 mg, daily) and omeprazole (40 mg, daily, 2 hours before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95%. Concomitant administration with omeprazole and drugs such as atazanavir and nelfinavir is therefore not recommended.
Increased concentrations of saquinavir
For other antiretroviral drugs, such as saquinavir, elevated serum levels have been reported, with an increase in AUC by 82%, in Cmax by 75%, and in Cmin by 106%, following multiple dosing of saquinavir/ritonavir (1,000/100 mg) twice daily for 15 days with omeprazole 40 mg daily co-administered days 11 to 15. Therefore, clinical and laboratory monitoring for saquinavir toxicity is recommended during concurrent use with esomeprazole magnesium delayed-release capsules. Dose reduction of saquinavir should be considered from the safety perspective for individual patients.
There are also some antiretroviral drugs of which unchanged serum levels have been reported when given with omeprazole.7.2 Drugs for Which Gastric pH Can Affect Bioavailability
Due to its effects on gastric acid secretion, esomeprazole can reduce the absorption of drugs where gastric pH is an important determinant of their bioavailability. Like with other drugs that decrease the intragastric acidity, the absorption of drugs such as ketoconazole, atazanavir, iron salts, erlotinib, and mycophenolate mofetil (MMF) can decrease, while the absorption of drugs such as digoxin can increase during treatment with esomeprazole. Esomeprazole is an enantiomer of omeprazole. Concomitant treatment with omeprazole (20 mg daily) and digoxin in healthy subjects increased the bioavailability of digoxin by 10% (30% in two subjects). Co-administration of digoxin with esomeprazole is expected to increase the systemic exposure of digoxin. Therefore, patients may need to be monitored when digoxin is taken concomitantly with esomeprazole.
Co-administration of omeprazole in healthy subjects and in transplant patients receiving MMF has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in MMF solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving esomeprazole and MMF. Use esomeprazole with caution in transplant patients receiving MMF [see Clinical Pharmacology (12.3)].7.3 Effects on Hepatic Metabolism/Cytochrome P-450 Pathways
Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. In vitro and in vivo studies have shown that esomeprazole is not likely to inhibit CYPs 1A2, 2A6, 2C9, 2D6, 2E1, and 3A4. No clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Drug interaction studies have shown that esomeprazole does not have any clinically significant interactions with phenytoin, warfarin, quinidine, clarithromycin, or amoxicillin.
However, postmarketing reports of changes in prothrombin measures have been received among patients on concomitant warfarin and esomeprazole therapy. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Esomeprazole may potentially interfere with CYP2C19, the major esomeprazole metabolizing enzyme. Co-administration of esomeprazole 30 mg and diazepam, a CYP2C19 substrate, resulted in a 45% decrease in clearance of diazepam.
Clopidogrel
Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of esomeprazole 40 mg results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition. Avoid concomitant administration of esomeprazole magnesium delayed-release capsules with clopidogrel. When using esomeprazole magnesium delayed-release capsules, consider use of alternative anti-platelet therapy [see Clinical Pharmacology (12.3) ].
Omeprazole acts as an inhibitor of CYP2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in cross-over study, increased Cmax and AUC of cilostazol by 18% and 26% respectively. Cmax and AUC of one of its active metabolites, 3,4-dihydrocilostazol, which has 4 to 7 times the activity of cilostazol, were increased by 29% and 69%, respectively. Co-administration of cilostazol with esomeprazole is expected to increase concentrations of cilostazol and its above mentioned active metabolite. Therefore, a dose reduction of cilostazol from 100 mg twice daily to 50 mg twice daily should be considered.
Concomitant administration of esomeprazole and a combined inhibitor of CYP2C19 and CYP3A4, such as voriconazole, may result in more than doubling of the esomeprazole exposure. Dose adjustment of esomeprazole is not normally required. However, in patients with Zollinger-Ellison’s Syndrome, who may require higher doses up to 240 mg/day, dose adjustment may be considered.
Drugs known to induce CYP2C19 or CYP3A4 or both (such as rifampin) may lead to decreased esomeprazole serum levels. Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with St. John’s Wort, an inducer of CYP3A4. In a cross-over study in 12 healthy male subjects, St. John’s Wort (300 mg three times daily for 14 days) significantly decreased the systemic exposure of omeprazole in CYP2C19 poor metabolisers (Cmax and AUC decreased by 37.5% and 37.9%, respectively) and extensive metabolisers (Cmax and AUC decreased by 49.6 % and 43.9%, respectively). Avoid concomitant use of St. John’s Wort or rifampin with esomeprazole magnesium delayed-release capsules.7.4 Interactions with Investigations of Neuroendocrine Tumors
Drug-induced decrease in gastric acidity results in enterochromaffin-like cell hyperplasia and increased Chromogranin A levels which may interfere with investigations for neuroendocrine tumors [see Warnings and Precautions (5.10) and Clinical Pharmacology (12.2)].
7.5 Tacrolimus
Concomitant administration of esomeprazole and tacrolimus may increase the serum levels of tacrolimus.
7.6 Combination Therapy with Clarithromycin
Co-administration of esomeprazole, clarithromycin, and amoxicillin has resulted in increases in the plasma levels of esomeprazole and 14-hydroxyclarithromycin [see Clinical Pharmacology (12.4)].
Concomitant administration of clarithromycin with other drugs can lead to serious adverse reactions due to drug interactions [see Warnings and Precautions in prescribing information for clarithromycin]. Because of these drug interactions, clarithromycin is contraindicated for co-administration with certain drugs [see Contraindications in prescribing information for clarithromycin].7.7 Methotrexate
Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of methotrexate with PPIs have been conducted [see Warnings and Precautions (5.11)].
-
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate and well-controlled studies with esomeprazole magnesium delayed-release capsules in pregnant women. Esomeprazole is the S-isomer of omeprazole. Available epidemiologic data fail to demonstrate an increased risk of major congenital malformations or other adverse pregnancy outcomes with first trimester omeprazole use. Reproduction studies in rats and rabbits resulted in dose-dependent embryo-lethality at omeprazole doses that were approximately 3.4 to 34 times an oral human dose of 40 mg (based on a body surface area for a 60 kg person).
Teratogenicity was not observed in animal reproduction studies with administration of oral esomeprazole magnesium in rats and rabbits with doses about 68 times and 42 times, respectively, an oral human dose of 40 mg (based on a body surface area basis for a 60 kg person). Changes in bone morphology were observed in offspring of rats dosed through most of pregnancy and lactation at doses equal to or greater than approximately 34 times an oral human dose of 40 mg. When maternal administration was confined to gestation only, there were no effects on bone physeal morphology in the offspring at any age [see Data].
The estimated background risks of major birth defects and miscarriage for the indicated population are unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.Data
Human Data
Esomeprazole is the S-isomer of omeprazole. Four epidemiological studies compared the frequency of congenital abnormalities among infants born to women who used omeprazole during pregnancy with the frequency of abnormalities among infants of women exposed to H2-receptor antagonists or other controls.
A population - based retrospective cohort epidemiological study from the Swedish Medical Birth Registry, covering approximately 99% of pregnancies, from 1995 to 1999, reported on 955 infants (824 exposed during the first trimester with 39 of these exposed beyond first trimester, and 131 exposed after the first trimester) whose mothers used omeprazole during pregnancy. The number of infants exposed in utero to omeprazole that had any malformation, low birth weight, low Apgar score, or hospitalization was similar to the number observed in this population. The number of infants born with ventricular septal defects and the number of stillborn infants was slightly higher in the omeprazole-exposed infants than the expected number in this population.
A population-based retrospective cohort study covering all live births in Denmark from 1996 to 2009, reported on 1,800 live births whose mothers used omeprazole during the first trimester of pregnancy and 837,317 live births whose mothers did not use any proton pump inhibitor. The overall rate of birth defects in infants born to mothers with first trimester exposure to omeprazole was 2.9% and 2.6% in infants born to mothers not exposed to any proton pump inhibitor during the first trimester.
A retrospective cohort study reported on 689 pregnant women exposed to either H2- blockers or omeprazole in the first trimester (134 exposed to omeprazole) and 1,572 pregnant women unexposed to either during the first trimester. The overall malformation rate in offspring born to mothers with first trimester exposure to omeprazole, an H2-blocker, or were unexposed was 3.6%, 5.5%, and 4.1% respectively.
A small prospective observational cohort study followed 113 women exposed to omeprazole during pregnancy (89% with first trimester exposures). The reported rate of major congenital malformations was 4% in the omeprazole group, 2% in controls exposed to non-teratogens, and 2.8% in disease paired controls. Rates of spontaneous and elective abortions, preterm deliveries, gestational age at delivery, and mean birth weight were similar among the groups.
Several studies have reported no apparent adverse short-term effects on the infant when single dose oral or intravenous omeprazole was administered to over 200 pregnant women as premedication for cesarean section under general anesthesia.Animal Data
Omeprazole
Reproductive studies conducted with omeprazole in rats at oral doses up to 138 mg/kg/day (about 34 times an oral human dose of 40 mg on a body surface area basis) and in rabbits at doses up to 69.1 mg/kg/day (about 34 times an oral human dose of 40 mg on a body surface area basis) during organogenesis did not disclose any evidence for a teratogenic potential of omeprazole. In rabbits, omeprazole in a dose range of 6.9 to 69.1 mg/kg/day (about 3.4 to 34 times an oral human dose of 40 mg on a body surface area basis) administered during organogenesis produced dose-related increases in embryo-lethality, fetal resorptions, and pregnancy disruptions. In rats, dose-related embryo/fetal toxicity and postnatal developmental toxicity were observed in offspring resulting from parents treated with omeprazole at 13.8 to 138.0 mg/kg/day (about 3.4 to 34 times an oral human dose of 40 mg on a body surface area basis), administered prior to mating through the lactation period.
Esomeprazole
No effects on embryo-fetal development were observed in reproduction studies with esomeprazole magnesium in rats at oral doses up to 280 mg/kg/day (about 68 times an oral human dose of 40 mg on a body surface area basis) or in rabbits at oral doses up to 86 mg/kg/day (about 41 times an oral human dose of 40 mg on a body surface area basis) administered during organogenesis.
A pre- and postnatal developmental toxicity study in rats with additional endpoints to evaluate bone development was performed with esomeprazole magnesium at oral doses of 14 to 280 mg/kg/day (about 3.4 to 68 times an oral human dose of 40 mg on a body surface area basis). Neonatal/early postnatal (birth to weaning) survival was decreased at doses equal to or greater than 138 mg/kg/day (about 34 times an oral human dose of 40 mg on a body surface area basis). Body weight and body weight gain were reduced and neurobehavioral or general developmental delays in the immediate post-weaning timeframe were evident at doses equal to or greater than 69 mg /kg/day (about 17 times an oral human dose of 40 mg on a body surface area basis). In addition, decreased femur length, width and thickness of cortical bone, decreased thickness of the tibial growth plate and minimal to mild bone marrow hypocellularity were noted at doses equal to or greater than 14 mg/kg/day (about 3.4 times an oral human dose of 40 mg on a body surface area basis). Physeal dysplasia in the femur was observed in offspring of rats treated with oral doses of esomeprazole magnesium at doses equal to or greater than 138 mg/kg/day (about 34 times an oral human dose of 40 mg on a body surface area basis).
Effects on maternal bone were observed in pregnant and lactating rats in a pre- and postnatal toxicity study when esomeprazole magnesium was administered at oral doses of 14 to 280 mg/kg/day (about 3.4 to 68 times an oral human dose of 40 mg on a body surface area basis). When rats were dosed from gestational day 7 through weaning on postnatal day 21, a statistically significant decrease in maternal femur weight of up to 14% (as compared to placebo treatment) was observed at doses equal to or greater than 138 mg/kg/day (about 34 times an oral human dose of 40 mg on a body surface area basis).
A pre- and postnatal development study in rats with esomeprazole strontium (using equimolar doses compared to esomeprazole magnesium study) produced similar results in dams and pups as described above.
A follow up developmental toxicity study in rats with further time points to evaluate pup bone development from postnatal day 2 to adulthood was performed with esomeprazole magnesium at oral doses of 280 mg/kg/day (about 68 times an oral human dose of 40 mg on a body surface area basis) where esomeprazole administration was from either gestational day 7 or gestational day 16 until parturition. When maternal administration was confined to gestation only, there were no effects on bone physeal morphology in the offspring at any age.8.2 Lactation
Risk Summary
Esomeprazole is the S-isomer of omeprazole and limited data suggest that omeprazole may be present in human milk. There are no clinical data on the effects of esomeprazole on the breastfed infant or on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for esomeprazole magnesium and any potential adverse effects on the breastfed infant from esomeprazole magnesium or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of esomeprazole magnesium delayed-release capsules have been established in pediatric patients 1 to 17 years of age for short-term treatment (up to eight weeks) of GERD.
1 to 17 years of age
Use of esomeprazole magnesium delayed-release capsules in pediatric and adolescent patients 1 to 17 years of age for short-term treatment (up to eight weeks) of GERD is supported by extrapolation of results from adequate and well-controlled studies for adults and safety and pharmacokinetic studies performed in pediatric and adolescent patients [see Dosage and Administration (2), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies, (14.3)]. The safety and effectiveness of esomeprazole magnesium delayed-release capsules for other pediatric uses have not been established.
Juvenile Animal Data
In a juvenile rat toxicity study, esomeprazole was administered with both magnesium and strontium salts at oral doses about 34 to 68 times a daily human dose of 40 mg based on body surface area. Increases in death were seen at the high dose, and at all doses of esomeprazole, there were decreases in body weight, body weight gain, femur weight and femur length, and decreases in overall growth [see Nonclinical Toxicology(13.2)].8.5 Geriatric Use
Of the total number of patients who received esomeprazole magnesium delayed-release capsules in clinical trials, 1,459 were 65 to 74 years of age and 354 patients were ≥ 75 years of age.
No overall differences in safety and efficacy were observed between the elderly and younger individuals, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. -
DESCRIPTION
The active ingredient in the proton pump inhibitor esomeprazole magnesium delayed-release capsules, USP for oral administration is 1H-Benzimidazole, 5-methoxy-2-[(S)-[(4-methoxy-3,5-dimethyl-2-pyridinyl]methyl] Sulfinyl], Magnesium Salt (2:1) Trihydrate. Esomeprazole is S-enantiomer of omeprazole. (Initial U.S. approval of esomeprazole magnesium: 2001). Its molecular formula is C34H36MgN6O6S2.3H2O with molecular weight of 767.17 as a trihydrate. The structural formula is:
Figure 1
[Esomeprazolemagnesiumfigure1]The magnesium salt is a white to slightly colored powder. It contains 3 moles of water. Slightly soluble in methanol, insoluble in water and in n-Heptane. The stability of esomeprazole magnesium is a function of pH; it rapidly degrades in acidic media, but it has acceptable stability under alkaline conditions.
Esomeprazole magnesium is supplied in delayed-release capsules. Each delayed-release capsule contains 20 mg, or 40 mg of esomeprazole (present as 22.25 mg, or 44.5 mg esomeprazole magnesium trihydrate, USP) in the form of enteric-coated granules with the following inactive ingredients: glyceryl monostearate, hydroxy propyl cellulose, hypromellose, magnesium stearate, methacrylic acid ethyl acrylate copolymer, polysorbate 80, simethicone, sugar spheres (contains sucrose and starch), talc and triethyl citrate. The capsule shells have the following inactive ingredients: gelatin, titanium dioxide and sodium lauryl sulfate.
The printing ink contains shellac, propylene glycol, strong ammonia solution, black iron oxide and potassium hydroxide. -
HOW SUPPLIED
Esomeprazole magnesium delayed-release capsules USP, 20 mg are White opaque size '4' hard gelatin capsule imprinted with ''H'' on cap and 'E2' on body filled with off white to pale yellow pellets.
NDC 72189-318-30 bottles of 30
NDC 72189-318-90 bottles of 90
NDC 72189-318-10 bottles of 1000Esomeprazole magnesium delayed-release capsules USP, 40 mg are white opaque size '3' hard gelatin capsule imprinted with ''H'' on cap and 'E3' on body filled with off white to pale yellow pellets.
NDC 72189-318-30 bottles of 30
NDC 72189-318-90 bottles of 90
NDC 72189-318-10 bottles of 1000 -
88436-1 - Section Title Not Found In Database
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Adverse Reactions
Advise patients to report to their healthcare provider if they experience any signs or symptoms consistent with:
• Hypersensitivity Reactions [see Contraindications (4)]
• Acute Interstitial Nephritis [see Warnings and Precautions (5.2)]
• Clostridium difficile-Associated Diarrhea [see Warnings and Precautions (5.3)]
• Bone Fracture [see Warnings and Precaution (5.4)]
• Cutaneous and Systemic Lupus Erythematosus [see Warnings and Precautions (5.5)]
• Cyanocobalamin (Vitamin B-12) Deficiency [see Warnings and Precautions (5.7)]
• Hypomagnesemia [see Warnings and Precautions(5.8)]Drug Interactions
• Advise patients to let you know if they are taking, or begin taking, other medications, because esomeprazole magnesium delayed-release capsules can interfere with antiretroviral drugs and drugs that are affected by gastric pH changes [see Drug Interactions (7.1)].Administration
• Let patients know that antacids may be used while taking esomeprazole magnesium delayed-release capsules.
• Advise patients to take esomeprazole magnesium delayed-release capsules at least one hour before a meal.
• For patients who are prescribed esomeprazole magnesium delayed-release capsules, advise them not to chew or crush the capsules.
• Advise patients that, if they open esomeprazole magnesium delayed-release capsules to mix the granules with food, the granules should only be mixed with applesauce. Use with other foods has not been evaluated and is not recommended.
• For patients who are advised to open the esomeprazole magnesium delayed- release capsules before taking them, instruct them in the proper technique for administration [see Dosage and Administration (2)] and tell them to follow the dosing instructions in the PATIENT INFORMATION insert included in the package. Instruct patients to rinse the syringe with water after each use.[camber]
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854By: HETEROTM
Hetero Labs Limited
Jeedimetla, Hyderabad – 500 055,India.
Revised: 08/2020
-
MEDICATION GUIDE
Esomeprazole Magnesium Delayed-Release Capsules, USP
(es'' oh mep' ra zole mag nee' zee um)Read the Medication Guide that comes with esomeprazole magnesium delayed-release capsules before you start taking esomeprazole magnesium delayed-release capsules and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment.
What is the most important information I should know about esomeprazole magnesium delayed-release capsules?
Esomeprazole magnesium delayed-release capsules may help your acid-related symptoms, but you could still have serious stomach problems. Talk with your doctor.
Esomeprazole magnesium delayed-release capsules can cause serious side effects, including:
• A type of kidney problem (acute interstitial nephritis). Some people who take proton pump inhibitor (PPI) medicines, including esomeprazole magnesium delayed-release capsules, may develop a kidney problem called acute interstitial nephritis that can happen at any time during treatment with esomeprazole magnesium delayed-release capsules. Call your doctor if you have a decrease in the amount that you urinate or if you have blood in your urine.
• Diarrhea. Esomeprazole magnesium delayed-release capsules may increase your risk of getting severe diarrhea. This diarrhea may be caused by an infection (Clostridium difficile) in your intestines.
Call your doctor right away if you have watery stool, stomach pain, and fever that does not go away.
• Bone fractures. People who take multiple daily doses of PPI medicines for a long period of time (a year or longer) may have an increased risk of fractures of the hip, wrist, or spine. You should take esomeprazole magnesium delayed-release capsules exactly as prescribed, at the lowest dose possible for your treatment and for the shortest time needed. Talk to your doctor about your risk of bone fracture if you take esomeprazole magnesium delayed-release capsules.
• Certain types of lupus erythematosus. Lupus erythematosus is an autoimmune disorder (the body’s immune cells attack other cells or organs in the body). Some people who take PPI medicines, including esomeprazole magnesium delayed-release capsules, may develop certain types of lupus erythematosus or have worsening of the lupus they already have. Call your doctor right away if you have new or worsening joint pain or a rash on your cheeks or arms that gets worse in the sun.
Esomeprazole magnesium delayed-release capsules can have other serious side effects. See “What are the possible side effects of esomeprazole magnesium delayed-release capsules?”
What are esomeprazole magnesium delayed-release capsules?
Esomeprazole magnesium delayed-release capsules are a prescription medicine called a proton pump inhibitor (PPI). Esomeprazole magnesium delayed-release capsules reduces the amount of acid in your stomach.
Esomeprazole magnesium delayed-release capsules are used in adults:
• for 4 to 8 weeks to treat the symptoms of gastroesophageal reflux disease (GERD). Esomeprazole magnesium delayed-release capsules may also be prescribed to heal acid-related damage to the lining of the esophagus (erosive esophagitis), and to help continue this healing.
GERD happens when acid in your stomach backs up into the tube (esophagus) that connects your mouth to your stomach. This may cause a burning feeling in your chest or throat, sour taste, or burping.
• for up to 6 months to reduce the risk of stomach ulcers in some people taking pain medicines called non-steroidal anti-inflammatory drugs (NSAIDs).
• to treat patients with a stomach infection (Helicobacter pylori), along with the antibiotics amoxicillin and clarithromycin.
• for the long-term treatment of conditions where your stomach makes too much acid, including Zollinger-Ellison Syndrome. Zollinger-Ellison Syndrome is a rare condition in which the stomach produces a more than normal amount of acid.
For children and adolescents 1 year to 17 years of age, esomeprazole magnesium delayed-release capsules may be prescribed for up to 8 weeks for short-term treatment of GERD.
Who should not take esomeprazole magnesium delayed-release capsules?
Do not take esomeprazole magnesium delayed-release capsules if you:
• are allergic to esomeprazole magnesium or any of the ingredients in esomeprazole magnesium delayed-release capsules. See the end of this Medication Guide for a complete list of ingredients in esomeprazole magnesium delayed-release capsules.
• are allergic to any other PPI medicine.
What should I tell my doctor before taking esomeprazole magnesium delayed-release capsules?
Before you take esomeprazole magnesium delayed-release capsules, tell your doctor if you:
• have been told that you have low magnesium levels in your blood.
• have liver problems.
• are pregnant or plan to become pregnant. It is not known if esomeprazole magnesium delayed-release capsules can harm your unborn baby.
• are breastfeeding or planning to breastfeed. Esomeprazole magnesium may pass into your breast milk. Talk to your doctor about the best way to feed your baby if you take esomeprazole magnesium delayed-release capsules.
Tell your doctor about all of the medicines you take, including prescription and non-prescription drugs, vitamins and herbal supplements. Esomeprazole magnesium delayed-release capsules may affect how other medicines work, and other medicines may affect how esomeprazole magnesium delayed-release capsules works.
Especially tell your doctor if you take:
• warfarin (Coumadin, Jantoven)
• ketoconazole (Nizoral)
• voriconazole (Vfend)
• atazanavir (Reyataz)
• nelfinavir (Viracept)
• saquinavir (Fortovase)
• products that contain iron
• digoxin (Lanoxin)
• St. John’s Wort (Hypericum perforatum)
• Rifampin (Rimactane, Rifater, Rifamate)
• cilostazol (Pletal)
• diazepam (Valium)
• tacrolimus (Prograf)
• erlotinib (Tarceva)
• methotrexate
• clopidogrel (Plavix)
• mycophenolate mofetil (Cellcept)
How should I take esomeprazole magnesium delayed-release capsules?
• Take esomeprazole magnesium delayed-release capsules exactly as prescribed by your doctor.
• Do not change your dose or stop esomeprazole magnesium delayed-release capsules without talking to your doctor.
• Take esomeprazole magnesium delayed-release capsules at least 1 hour before a meal.
• Swallow esomeprazole magnesium delayed-release capsules whole. Never chew or crush esomeprazole magnesium delayed-release capsules.
• If you have difficulty swallowing esomeprazole magnesium delayed-release capsules, you may open the capsule and empty the contents into a tablespoon of applesauce. Do not crush or chew the granules. Be sure to swallow the applesauce right away. Do not store it for later use.
• If you forget to take a dose of esomeprazole magnesium delayed-release capsules, take it as soon as you remember. If it is almost time for your next dose, do not take the missed dose. Take the next dose on time. Do not take a double dose to make up for a missed dose.
• If you take too much esomeprazole magnesium delayed-release capsules, call your doctor or local poison control center right away, or go to the nearest hospital emergency room.
• See the “Instructions for Use” at the end of this Medication Guide for instructions how to take esomeprazole magnesium delayed-release capsules through a nasogastric tube.
What are the possible side effects of esomeprazole magnesium delayed-release capsules?
Esomeprazole magnesium delayed-release capsules can cause serious side effects, including:
• See "What is the most important information I should know about esomeprazole magnesium delayed-release capsules?".
• Vitamin B-12 deficiency. Esomeprazole magnesium delayed-release capsules reduces the amount of acid in your stomach. Stomach acid is needed to absorb vitamin B-12 properly. Talk with your doctor about the possibility of vitamin B-12 deficiency if you have been on esomeprazole magnesium delayed-release capsules for a long time (more than 3 years).
• Low magnesium levels in your body. Low magnesium can happen in some people who take a PPI medicine for at least 3 months. If low magnesium levels happen, it is usually after a year of treatment.
You may or may not have symptoms of low magnesium. Tell your doctor right away if you have any of these symptoms:
o seizures
o dizziness
o abnormal or fast heart beat
o jitteriness
o jerking movements or shaking (tremors)
o muscle weakness
o spasms of the hands and feet
o cramps or muscle aches
o spasm of the voice box
Your doctor may check the level of magnesium in your body before you start taking esomeprazole magnesium delayed-release capsules or during treatment if you will be taking esomeprazole magnesium delayed-release capsules for a long period of time.
• Stomach growths (fundic gland polyps). People who take PPI medicines for a long time have an increased risk of developing a certain type of stomach growths called fundic gland polyps,
especially after taking PPI medicines for more than 1 year.
The most common side effects with esomeprazole magnesium delayed-release capsules may include:
o headache
o diarrhea
o nausea
o gas
o abdominal pain
o constipation
o dry mouth
o drowsiness
Other side effects:
Serious allergic reactions. Tell your doctor if you get any of the following symptoms with esomeprazole magnesium delayed-release capsules.
• rash
• face swelling
• throat tightness
• difficulty breathing
Your doctor may stop esomeprazole magnesium delayed-release capsules if these symptoms happen.
Tell your doctor if you have any side effects that bother you or that do not go away. These are not all the possible side effects with esomeprazole magnesium delayed-release capsules.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store esomeprazole magnesium delayed-release capsules?
• Store esomeprazole magnesium delayed-release capsules at 20° to 25°C (68° to 77°F)
• Keep the container of esomeprazole magnesium delayed-release capsules closed tightly.
Keep esomeprazole magnesium delayed-release capsules and all medicines out of the reach of children.
General information about esomeprazole magnesium delayed-release capsules
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use esomeprazole magnesium delayed-release capsules for a condition for which it was not prescribed. Do not give esomeprazole magnesium delayed-release capsules to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about esomeprazole magnesium delayed-release capsules. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about esomeprazole magnesium delayed-release capsules that is written for health professionals.
For more information, call 1-866-495-1995.
What are the ingredients in esomeprazole magnesium delayed-release capsules?
Active ingredient: esomeprazole magnesium trihydrate, USP
Inactive ingredients in Esomeprazole Magnesium Delayed-Release Capsules (including the capsule shells): glyceryl monostearate, hydroxy propyl cellulose, hypromellose, magnesium stearate, methacrylic acid ethyl acrylate copolymer, polysorbate 80, simethicone, sugar spheres (contains sucrose and starch), talc and triethyl citrate. The capsule shells have the following inactive ingredients: gelatin, titanium dioxide and sodium lauryl sulfate.
The printing ink contains shellac, propylene glycol, strong ammonia solution, black iron oxide and potassium hydroxide.
Instructions for Use
For instructions on taking Delayed-Release Capsules, see the section of this leaflet called "How should I take esomeprazole magnesium delayed-release capsules?"
Esomeprazole magnesium delayed-release capsules may be given through a nasogastric tube (NG tube) as prescribed by your doctor. Follow the instructions below:
Esomeprazole Magnesium Delayed-Release Capsules:
• Open the capsule and empty the granules into a 60 mL catheter tipped syringe. Mix with 50 mL of water. Use only a catheter tipped syringe to give esomeprazole magnesium delayed-release capsules through a NG tube.
• Replace the plunger and shake the syringe well for 15 seconds. Hold the syringe with the tip up and check for granules in the tip.
• Give the medicine right away.
• Do not give the granules if they have dissolved or have broken into pieces.
• Attach the syringe to the NG tube. Give the medicine in the syringe through the NG tube into the stomach.
• After giving the granules, flush the NG tube with more water.
This Medication Guide has been approved by the U.S. Food and Drug Administration.Medication Guide available at http://camberpharma.com/medication-guides
[camber]
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854
By: HETEROTM
Hetero Labs Limited
Jeedimetla, Hyderabad – 500 055,
India.
The brands listed are trademarks of their respective owners and are not trademarks of Hetero. The makers of these brands are not affiliated with and do not endorse Hetero or its products.
Revised: 08/2020
- STORAGE AND HANDLING
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
ESOMEPRAZOLE MAGNESIUM
esomeprazole magnesium capsule, delayed releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:72189-318(NDC:31722-665) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESOMEPRAZOLE MAGNESIUM (UNII: R6DXU4WAY9) (ESOMEPRAZOLE - UNII:N3PA6559FT) ESOMEPRAZOLE 40 mg Inactive Ingredients Ingredient Name Strength TRIETHYL CITRATE (UNII: 8Z96QXD6UM) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) STARCH, CORN (UNII: O8232NY3SJ) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) TALC (UNII: 7SEV7J4R1U) MAGNESIUM STEARATE (UNII: 70097M6I30) SODIUM LAURYL SULFATE (UNII: 368GB5141J) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) METHACRYLIC ACID-ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) GLYCERYL MONOSTEARATE (UNII: 230OU9XXE4) POLYSORBATE 80 (UNII: 6OZP39ZG8H) HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) GELATIN (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) AMMONIA (UNII: 5138Q19F1X) FERROSOFERRIC OXIDE (UNII: XM0M87F357) SUCROSE (UNII: C151H8M554) DIMETHICONE (UNII: 92RU3N3Y1O) SHELLAC (UNII: 46N107B71O) Product Characteristics Color white Score no score Shape CAPSULE Size 16mm Flavor Imprint Code H;E3 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:72189-318-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/19/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA211977 01/19/2022 Labeler - Direct Rx (079254320) Registrant - Direct Rx (079254320) Establishment Name Address ID/FEI Business Operations Direct Rx 079254320 repack(72189-318)