Label: ANTIZOL- fomepizole injection
-
Contains inactivated NDC Code(s)
NDC Code(s): 46129-200-01, 46129-200-02 - Packager: PALADIN LABORATORIES (USA) INC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated July 27, 2009
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Antizol® (fomepizole) Injection is a competitive inhibitor of alcohol dehydrogenase.
The chemical name of fomepizole is 4-methylpyrazole. It has the molecular formula C4H6N2 and a molecular weight of 82.1. The structural formula is:

It is a clear to yellow liquid at room temperature. Its melting point is 25° C (77° F) and it may present as solid at room temperature. Fomepizole is soluble in water and very soluble in ethanol, diethyl ether, and chloroform. Each vial contains 1.5 mL (1 g/mL) of fomepizole.
-
CLINICAL PHARMACOLOGY
Mechanism of Action: Antizol® (fomepizole) is a competitive inhibitor of alcohol dehydrogenase. Alcohol dehydrogenase catalyzes the oxidation of ethanol to acetaldehyde. Alcohol dehydrogenase also catalyzes the initial steps in the metabolism of ethylene glycol and methanol to their toxic metabolites.
Ethylene glycol, the main component of most antifreezes and coolants, is metabolized to glycoaldehyde, which undergoes subsequent sequential oxidations to yield glycolate, glyoxylate, and oxalate. Glycolate and oxalate are the metabolic byproducts primarily responsible for the metabolic acidosis and renal damage seen in ethylene glycol toxicosis. The lethal dose of ethylene glycol in humans is approximately 1.4 mL/kg.
Methanol, the main component of windshield wiper fluid, is slowly metabolized via alcohol dehydrogenase to formaldehyde with subsequent oxidation via formaldehyde dehydrogenase to yield formic acid. Formic acid is primarily responsible for the metabolic acidosis and visual disturbances (e.g., decreased visual acuity and potential blindness) associated with methanol poisoning. A lethal dose of methanol in humans is approximately 1-2 mL/kg.
Fomepizole has been shown in vitro to block alcohol dehydrogenase enzyme activity in dog, monkey, and human liver. The concentration of fomepizole at which alcohol dehydrogenase is inhibited by 50% in vitro is approximately 0.1 μmol/L.
In a study of dogs given a lethal dose of ethylene glycol, three animals each were administered fomepizole, ethanol, or left untreated (control group). The three animals in the untreated group became progressively obtunded, moribund, and died. At necropsy, all three dogs had severe renal tubular damage. Fomepizole or ethanol, given 3 hours after ethylene glycol ingestion, attenuated the metabolic acidosis and prevented the renal tubular damage associated with ethylene glycol intoxication.
Several studies have demonstrated that Antizol® plasma concentrations of approximately 10μmol/L (0.82 mg/L) in monkeys are sufficient to inhibit methanol metabolism to formate, which is also mediated by alcohol dehydrogenase. Based on these results, concentrations of Antizol® in humans in the range of 100 to 300 μmol/L (8.6-24.6 mg/L) have been targeted to assure adequate plasma concentrations for the effective inhibition of alcohol dehydrogenase.
In healthy volunteers, oral doses of Antizol® (10-20 mg/kg) significantly reduced the rate of elimination of moderate doses of ethanol, which is also metabolized through the action of alcohol dehydrogenase (see PRECAUTIONS, Drug Interactions).
Pharmacokinetics: The plasma half-life of Antizol® varies with dose, even in patients with normal renal function, and has not been calculated.
Distribution: After intravenous infusion, Antizol® rapidly distributes to total body water. The volume of distribution is between 0.6 L/kg and 1.02 L/kg.
Metabolism: In healthy volunteers, only 1-3.5% of the administered dose of Antizol® (7-20 mg/kg oral and IV) was excreted unchanged in the urine, indicating that metabolism is the major route of elimination. In humans, the primary metabolite of Antizol® is 4-carboxypyrazole (approximately 80-85% of administered dose), which is excreted in the urine. Other metabolites of Antizol® observed in the urine are 4-hydroxymethylpyrazole and the N-glucuronide conjugates of 4-carboxypyrazole and 4-hydroxymethylpyrazole.
Excretion: The elimination of Antizol® is best characterized by Michaelis-Menten kinetics after acute doses, with saturable elimination occurring at therapeutic blood concentrations [100-300 μmol/L, 8.2-24.6 mg/L].
With multiple doses, Antizol® rapidly induces its own metabolism via the cytochrome P450 mixed-function oxidase system, which produces a significant increase in the elimination rate after about 30-40 hours. After enzyme induction, elimination follows first-order kinetics.
Special Populations:
Geriatric: Antizol® (fomepizole) Injection has not been studied sufficiently to determine whether the pharmacokinetics differ for a geriatric population.
Pediatric: Antizol® has not been studied sufficiently to determine whether the pharmacokinetics differ for a pediatric population.
Gender: Antizol® has not been studied sufficiently to determine whether the pharmacokinetics differ between the genders.
Renal Insufficiency: The metabolites of Antizol® are excreted renally. Definitive pharmacokinetic studies have not been done to assess pharmacokinetics in patients with renal impairment.
Hepatic Insufficiency: Antizol® is metabolized through the liver, but no definitive pharmacokinetic studies have been done in subjects with hepatic disease.
Clinical Studies: The efficacy of Antizol® in the treatment of ethylene glycol and methanol intoxication was studied in two prospective, U.S. clinical trials without concomitant control groups. Fourteen of 16 patients in the ethylene glycol trial and 7 of 11 patients in the methanol trial underwent hemodialysis because of severe intoxication (see DOSAGE AND ADMINISTRATION). All patients received Antizol® shortly after admission.
The results of these two studies provide evidence that Antizol® blocks ethylene glycol and methanol metabolism mediated by alcohol dehydrogenase in the clinical setting. In both studies, plasma concentrations of toxic metabolites of ethylene glycol and methanol failed to rise in the initial phases of treatment. The relationship to Antizol® therapy, however, was confounded by hemodialysis and significant blood ethanol concentrations in many of the patients. Nevertheless, in the post-dialysis period(s), when ethanol concentrations were insignificant and the concentrations of ethylene glycol or methanol were > 20 mg/dL, the administration of Antizol® alone blocked any rise in glycolate or formate concentrations, respectively.
In a separate French trial, 5 patients presented with ethylene glycol concentrations ranging from 46.5 to 345 mg/dL, insignificant ethanol blood concentrations, and normal renal function. These patients were treated with fomepizole alone without hemodialysis, and none developed signs of renal injury.
-
INDICATIONS AND USAGE
Antizol® is indicated as an antidote for ethylene glycol (such as antifreeze) or methanol poisoning, or for use in suspected ethylene glycol or methanol ingestion, either alone or in combination with hemodialysis (see DOSAGE AND ADMINISTRATION).
- CONTRAINDICATIONS
-
PRECAUTIONS
General
Antizol® should not be given undiluted or by bolus injection. Venous irritation and phlebosclerosis were noted in two of six normal volunteers given bolus injections (over 5 minutes) of Antizol® at a concentration of 25 mg/mL.
Minor allergic reactions (mild rash, eosinophilia) have been reported in a few patients receiving Antizol® (see ADVERSE REACTIONS). Therefore, patients should be monitored for signs of allergic reactions.
Laboratory Tests
In addition to specific antidote treatment with Antizol®, patients intoxicated with ethylene glycol or methanol must be managed for metabolic acidosis, acute renal failure (ethylene glycol), adult respiratory distress syndrome, visual disturbances (methanol), and hypocalcemia. Fluid therapy and sodium bicarbonate administration are potential supportive therapies. In addition, potassium and calcium supplementation and oxygen administration are usually necessary. Hemodialysis is necessary in the anuric patient, or in patients with severe metabolic acidosis or azotemia (see DOSAGE AND ADMINISTRATION). Treatment success should be assessed by frequent measurements of blood gases, pH, electrolytes, BUN, creatinine, and urinalysis, in addition to other laboratory tests as indicated by individual patient conditions. At frequent intervals throughout the treatment, patients poisoned with ethylene glycol should be monitored for ethylene glycol concentrations in serum and urine, and the presence of urinary oxalate crystals. Similarly, serum methanol concentrations should be monitored in patients poisoned with methanol. Electrocardiography should be performed because acidosis and electrolyte imbalances can affect the cardiovascular system. In the comatose patient, electroencephalography may also be required. In addition, hepatic enzymes and white blood cell counts should be monitored during treatment, as transient increases in serum transaminase concentrations and eosinophilia have been noted with repeated Antizol® dosing.
Drug Interactions
Oral doses of Antizol® (10-20 mg/kg), via alcohol dehydrogenase inhibition, significantly reduced the rate of elimination of ethanol (by approximately 40%) given to healthy volunteers in moderate doses. Similarly, ethanol decreased the rate of elimination of Antizol® (by approximately 50%) by the same mechanism.
Reciprocal interactions may occur with concomitant use of Antizol® and drugs that increase or inhibit the cytochrome P450 system (e.g., phenytoin, carbamazepine, cimetidine, ketoconazole), though this has not been studied.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
There have been no long-term studies performed in animals to evaluate carcinogenic potential. There was a positive Ames test result in the Escherichia coli tester strain WP2uvrA and the Salmonella typhimurium tester strain TA102 in the absence of metabolic activation.
There was no evidence of a clastogenic effect in the in vivo mouse micronucleus assay.
In rats, fomepizole (110 mg/kg) administered orally for 40 to 42 days resulted in decreased testicular mass (approximately 8% reduction). This dose is approximately 0.6 times the human maximum daily exposure based on surface area (mg/m2). This reduction was similar for rats treated with either ethanol or fomepizole alone. When fomepizole was given in combination with ethanol, the decrease in testicular mass was significantly greater (approximately 30% reduction) compared to those rats treated exclusively with fomepizole or ethanol.
Pregnancy
Pregnancy Category C: Animal reproduction studies have not been conducted with fomepizole. It is also not known whether Antizol® can cause fetal harm when administered to pregnant women or can affect reproduction capacity. Antizol® should be given to pregnant women only if clearly needed.
-
ADVERSE REACTIONS
The most frequent adverse events reported as drug-related or unknown relationship to study drug in the 78 patients and 63 normal volunteers who received Antizol® (fomepizole) Injection were headache (14%), nausea (11%), and dizziness, increased drowsiness, and bad taste/metallic taste (6% each). All other adverse events in this population were reported in approximately 3% or fewer of those receiving Antizol® and were as follows:
Body as a Whole: Abdominal pain, fever, multiorgan system failure, pain during Antizol® injection, inflammation at injection site, lumbalgia/backache, hangover
Cardiovascular: Sinus bradycardia/bradycardia, phlebosclerosis, tachycardia, phlebitis, shock, hypotension
Gastrointestinal: Vomiting, diarrhea, dyspepsia, heartburn, decreased appetite, transient transaminitis
Hemic/Lymphatic: Eosinophilia/hypereosinophilia, lymphangitis, disseminated intravascular coagulation, anemia
Nervous: Lightheadedness, seizure, agitation, feeling drunk, facial flush, vertigo, nystagmus, anxiety, “felt strange”, decreased environmental awareness
Respiratory: Hiccups, pharyngitis
Skin/Appendages: Application site reaction, rash
Special Senses: Abnormal smell, speech/visual disturbances, transient blurred vision, roar in ear
Urogenital: Anuria
-
OVERDOSAGE
Nausea, dizziness, and vertigo were noted in healthy volunteers receiving 50 and 100 mg/kg doses of Antizol® (at plasma concentrations of 290-520 μmol/L, 23.8-42.6 mg/L). These doses are 3-6 times the recommended dose. This dose-dependent CNS effect was short-lived in most subjects and lasted up to 30 hours in one subject.
Antizol® is dialyzable, and hemodialysis may be useful in treating cases of overdosage.
-
DOSAGE AND ADMINISTRATION
Treatment Guidelines: If ethylene glycol or methanol poisoning is left untreated, the natural progression of the poisoning leads to accumulation of toxic metabolites, including glycolic and oxalic acids (ethylene glycol intoxication) and formic acid (methanol intoxication). These metabolites can induce metabolic acidosis, nausea/ vomiting, seizures, stupor, coma, calcium oxaluria, acute tubular necrosis, blindness, and death. The diagnosis of these poisonings may be difficult because ethylene glycol and methanol concentrations diminish in the blood as they are metabolized to their respective metabolites. Hence, both ethylene glycol and methanol concentrations and acid base balance, as determined by serum electrolyte (anion gap) and/or arterial blood gas analysis, should be frequently monitored and used to guide treatment.
Treatment consists of blocking the formation of toxic metabolites using inhibitors of alcohol dehydrogenase, such as Antizol®, and correction of metabolic abnormalities. In patients with high ethylene glycol or methanol concentrations (≥ 50 mg/dL), significant metabolic acidosis, or renal failure, hemodialysis should be considered to remove ethylene glycol or methanol and the respective toxic metabolites of these alcohols.
Treatment with Antizol®:
Begin Antizol® treatment immediately upon suspicion of ethylene glycol or methanol ingestion based on patient history and/or anion gap metabolic acidosis, increased osmolar gap, visual disturbances, or oxalate crystals in the urine, OR a documented serum ethylene glycol or methanol concentration greater than 20 mg/dL.
Hemodialysis: Hemodialysis should be considered in addition to Antizol® in the case of renal failure, significant or worsening metabolic acidosis, or a measured ethylene glycol or methanol concentration of greater than or equal to 50 mg/dL. Patients should be dialyzed to correct metabolic abnormalities and to lower the ethylene glycol concentrations below 50 mg/dL.
Discontinuation of Antizol® Treatment: Treatment with Antizol® may be discontinued when ethylene glycol or methanol concentrations are undetectable or have been reduced below 20 mg/dL, and the patient is asymptomatic with normal pH.
Dosing of Antizol®: A loading dose of 15 mg/kg should be administered, followed by doses of 10 mg/kg every 12 hours for 4 doses, then 15 mg/kg every 12 hours thereafter until ethylene glycol or methanol concentrations are undetectable or have been reduced below 20 mg/dL, and the patient is asymptomatic with normal pH. All doses should be administered as a slow intravenous infusion over 30 minutes (see Administration).
Dosage with Renal Dialysis: Antizol® (fomepizole) Injection is dialyzable and the frequency of dosing should be increased to every 4 hours during hemodialysis
Antizol® Dosing in Patients Requiring Hemodialysis DOSE AT THE BEGINNING OF HEMODIALYSIS
If <6 hours since last Antizol® dose
If ≥ 6 hours since last Antizol® dose
Do not administer dose
Administer next scheduled dose
DOSING DURING HEMODIALYSIS
Dose every 4 hours
DOSING AT THE TIME HEMODIALYSIS IS COMPLETED
Time between last dose and the end of hemodialysis
<1 hour
Do not administer dose at the end of hemodialysis
1-3 hours
Administer 1/2 of next scheduled dose
>3 hours
Administer next scheduled dose
MAINTENANCE DOSING OFF HEMODIALYSIS
Give next scheduled dose 12 hours from last dose administered
Administration: Antizol® solidifies at temperatures less than 25° C (77° F). If the Antizol® solution has become solid in the vial, the solution should be liquefied by running the vial under warm water or by holding in the hand. Solidification does not affect the efficacy, safety, or stability of Antizol®. Using sterile technique, the appropriate dose of Antizol® should be drawn from the vial with a syringe and injected into at least 100 mL of sterile 0.9% sodium chloride injection or dextrose 5% injection. Mix well. The entire contents of the resulting solution should be infused over 30 minutes. Antizol®, like all parenteral products, should be inspected visually for particulate matter prior to administration.
Stability: Antizol® diluted in 0.9% sodium chloride injection or dextrose 5% injection remains stable and sterile for at least 24 hours when stored refrigerated or at room temperature. Antizol® does not contain preservatives. Therefore, maintain sterile conditions, and after dilution do not use beyond 24 hours. Solutions showing haziness, particulate matter, precipitate, discoloration, or leakage should not be used.
-
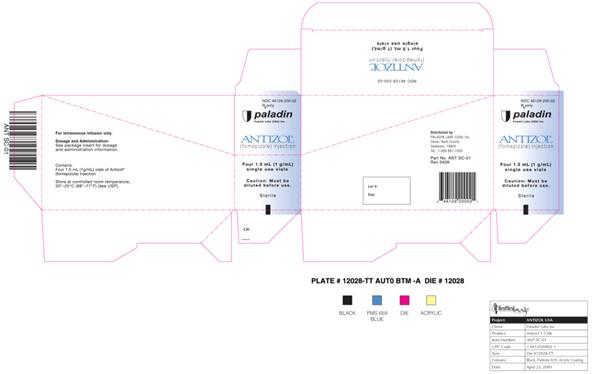
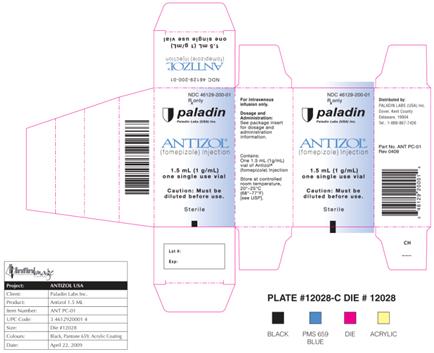
HOW SUPPLIED
Antizol® is supplied as a sterile, preservative-free solution for intravenous use as:
Supplied in packages of four vials or one vial. Each vial contains 1.5 mL (1 g/mL) of fomepizole.
NDC 46129-200-02 (four vials)
NDC 46129-200-01 (one vial)
Store at controlled room temperature, 20° to 25° C (68° to 77° F)
Distributed in the U.S. by:
Dover, Kent County,
Paladin Labs (USA) Inc.
Delaware, 19904
For questions of a medical nature, call 1-888-867-7426.
Part No. ANT PI-8511
Revision Date: April 2009 - PACKAGE LABEL.PRINCIPAL DISPLAY PANEL- 1.5 mL (4 vials)
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL- 1.5 mL (1 Vial)
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL- 1.5 mL (1 vial)
-
INGREDIENTS AND APPEARANCE
ANTIZOL
fomepizole injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:46129-200 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FOMEPIZOLE (UNII: 83LCM6L2BY) (FOMEPIZOLE - UNII:83LCM6L2BY) FOMEPIZOLE 1 g in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:46129-200-02 4 in 1 PACKAGE 1 1.5 mL in 1 VIAL 2 NDC:46129-200-01 1 in 1 PACKAGE 2 1.5 mL in 1 VIAL Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020696 07/31/2009 Labeler - PALADIN LABORATORIES (USA) INC (831011775) Registrant - Ben Venue Laboratories (004327953) Establishment Name Address ID/FEI Business Operations Ben Venue 004327953 manufacture