Label: MICONAZOLE NITRATE suppository
- NDC Code(s): 0472-1738-03
- Packager: Actavis Pharma, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated October 21, 2020
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
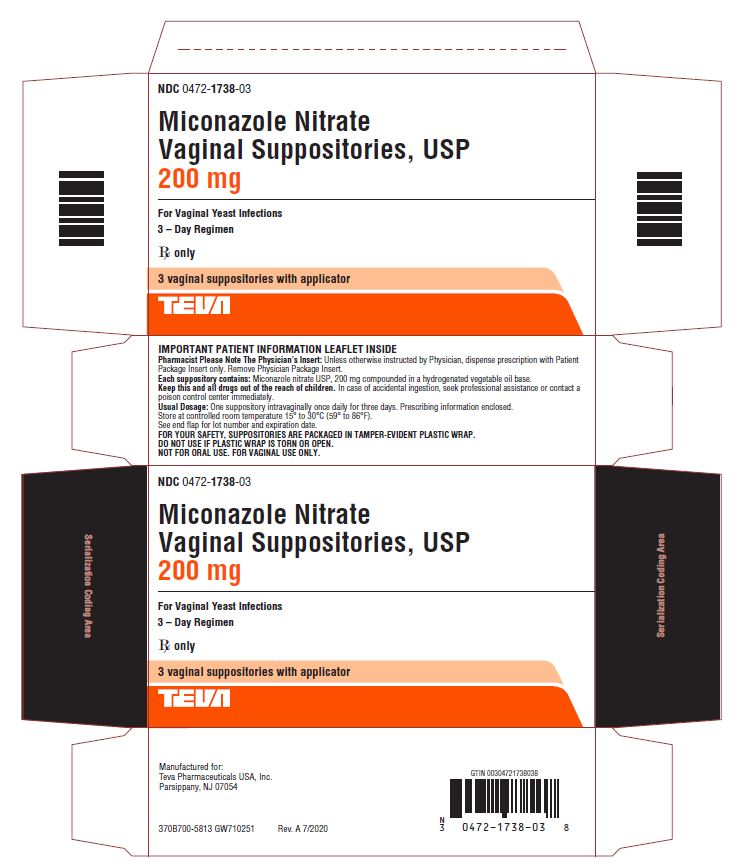
DESCRIPTION
Miconazole Nitrate Vaginal Suppositories USP, 200 mg are white to off-white suppositories, each containing the antifungal agent, miconazole nitrate, USP 1-[2,4-Dichloro-β-[(2,4- dichlorobenzyl)oxy] phenethyl]-imidazole mononitrate, 200 mg, in a hydrogenated vegetable oil base. The molecular formula is C18H14Cl4N2O•HNO3; the molecular weight is 479.14 and the structural formula may be represented as follows:
-
CLINICAL PHARMACOLOGY
Miconazole nitrate exhibits fungicidal activity in vitro against species of the genus Candida. The pharmacologic mode of action is unknown. Following intravaginal administration of miconazole nitrate, small amounts are absorbed. Administration of a single dose of miconazole nitrate vaginal suppositories (100 mg) to healthy subjects resulted in total recovery from the urine and feces of 0.85% (±0.43%) of the administered dose.
Animal studies indicate that the drug crossed the placenta and doses above those used in humans result in embryo and fetotoxicity (80 mg/kg, orally), although this has not been reported in human subjects (See PRECAUTIONS).
In multi-center clinical trials in 440 women with vulvovaginal candidiasis, the efficacy of treatment with the Miconazole Nitrate Vaginal Suppositories USP, 200 mg for 3 days was compared with treatment for 7 days with Miconazole Nitrate Vaginal Cream 2%. The clinical cure rates (free of microbiological evidence and clinical signs and symptoms of candidiasis at 8 to 10 days and 30 to 35 days post therapy) were numerically lower, although not statistically different, with the 3-Day Suppository when compared with the 7-Day Cream.
-
INDICATIONS AND USAGE
Miconazole Nitrate Vaginal Suppositories USP, 200 mg are indicated for the local treatment of vulvovaginal candidiasis (moniliasis). Effectiveness in pregnancy has not been established. As miconazole nitrate is effective only for candidal vulvovaginitis, the diagnosis should be confirmed by KOH smear and/or cultures. Other pathogens commonly associated with vulvovaginitis (Trichomonas and Haemophilus vaginalis [Gardnerella]) should be ruled out by appropriate laboratory methods.
- CONTRAINDICATIONS
-
PRECAUTIONS
General
Discontinue drug if sensitization or irritation is reported during use. The base contained in the suppository formulation may interact with certain latex products, such as that used in vaginal contraceptive diaphragms. Concurrent use is not recommended. Miconazole Nitrate Vaginal Cream USP, 2% may be considered for use under these conditions.
Laboratory Tests
If there is a lack of response to Miconazole Nitrate Vaginal Suppositories, appropriate microbiological studies (standard KOH smear and/or cultures) should be repeated to confirm the diagnosis and rule out other pathogens.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies to determine carcinogenic potential have not been performed.
Fertility (Reproduction): Oral administration of miconazole nitrate in rats has been reported to produce prolonged gestation. However, this effect was not observed in oral rabbit studies. In addition, signs of fetal and embryo toxicity were reported in rat and rabbit studies, and dystocia was reported in rat studies after oral doses at and above 80 mg per kg. Intravaginal administration did not produce these effects in rats.
Pregnancy
Since imidazoles are absorbed in small amounts from the human vagina, they should not be used in the first trimester of pregnancy unless the physician considers it essential to the welfare of the patient.
Clinical studies, during which miconazole nitrate vaginal cream and suppositories were used for up to 14 days, were reported to include 541 pregnant patients. Follow-up reports available in 471 of these patients reveal no adverse effects or complications attributable to miconazole nitrate therapy in infants born to these women.
-
ADVERSE REACTIONS
During clinical studies with Miconazole Nitrate Vaginal Suppositories USP, 200 mg, 301 patients were treated. The incidence of vulvovaginal burning, itching or irritation was 2%. Complaints of cramping (2%) and headaches (1.3%) were also reported. Other complaints (hives, skin rash) occurred with less than a 0.5% incidence. The therapy-related dropout rate was 0.3%.
To report SUSPECTED ADVERSE EVENTS, contact Teva Pharmaceuticals USA, Inc., at 1-888-838-2872 or FDA at 1-800-FDA-1088 or http://www.fda.gov/ for voluntary reporting of adverse reactions.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
Miconazole Nitrate Vaginal Suppositories USP, 200 mg: One suppository (miconazole nitrate, 200 mg) is inserted intravaginally once daily at bedtime for three consecutive days. Before prescribing another course of therapy, the diagnosis should be reconfirmed by smears and/or cultures to rule out other pathogens.
-
HOW SUPPLIED
Miconazole Nitrate Vaginal Suppositories USP, 200 mg are available as elliptically shaped white to off-white suppositories in packages of three with a vaginal applicator NDC 0472-1738-03.
Store at controlled room temperature 15° to 30°C (59° to 86°F).
Manufactured for:
Teva Pharmaceuticals USA, Inc.
Parsippany, NJ 07054Rev. A 7/2020
-
PATIENT’S INSTRUCTIONS
Miconazole Nitrate (mye konꞌ a zole nyeꞌ trate)
Vaginal Suppositories USP, 200 mg3-DAY THERAPY
Three oval suppositories, for use inside the vagina only.
Designed to be inserted into the vagina.HOW TO USE:
Place one suppository into the vagina each night at bedtime for 3 nights, as directed by your doctor. The miconazole nitrate vaginal suppository is self-lubricating and may be inserted with or without the applicator
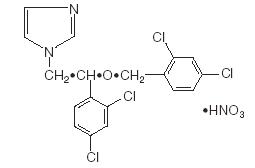
A. Insertion with the applicator1. Filling the applicator:
Tear off one suppository from the strip. Separate the plastic wrap at the pointed end with your thumb. With thumb and forefinger of each hand, hold the plastic tabs and pull apart. Gently remove the suppository from the plastic wrap.
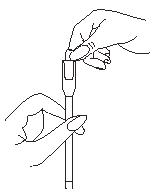
Place the flat end of the suppository into the open end of the applicator as shown. You are now ready to insert the suppository into the vagina.
2. Using the applicator:
Lie on your back with your knees drawn up toward your chest.Holding the applicator by the ribbed end of the barrel, gently insert it into the vagina as far as it will comfortably go. Press the plunger to release the suppository into the vagina.
Remove the applicator from the vagina.
3. Cleaning the applicator:
After each use, you should thoroughly clean the applicator by the following procedure:Pull the plunger out of the barrel. Wash both pieces with lukewarm, soapy water, and dry them thoroughly. Put the applicator back together by gently pushing the plunger into the barrel as far as it will go.
B. Insertion without the applicator
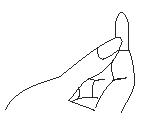
Lie on your back with your knees drawn up toward your chest. Place the suppository on the tip of your finger as shown. Insert the suppository gently into the vagina as far as it will comfortably go.
NOTE: Store at controlled room temperature 15° to 30°C (59° to 86°F).
See end flap for lot number and expiration date.A WORD ABOUT YEAST INFECTIONS
Why do yeast infections occur?
Yeast infections are caused by an organism called Candida (KAN di duh). It may be present in small and harmless amounts in the mouth, digestive track, and vagina. Sometimes the natural balance of the vagina becomes upset. This may lead to rapid growth of Candida, which results in a yeast infection. Symptoms of yeast infection include itching, burning, redness, and an abnormal discharge. Your doctor can make the diagnosis of a yeast infection by evaluating your symptoms and looking at a sample of the discharge under the microscope.
How can I prevent yeast infections?
Certain factors may increase your chance of developing a yeast infection. These factors don’t actually cause the problem, but they may create a situation that allows the yeast to grow rapidly.
Clothing: Tight jeans, nylon underwear, pantyhose, and wet bathing suits can hold in heat and moisture (two conditions in which yeast organisms thrive). Looser pants or skirts, 100% cotton underwear, and stockings may help avoid this problem.
Diet: Cutting down on sweets, milk products, and artificial sweeteners reduce the risk of yeast infections.
Antibiotics: Antibiotics work by eliminating disease-causing organisms. While they are helpful in curing other problems, antibiotics may lead to an overgrowth of Candida in the vagina.
Pregnancy: Hormonal changes in the body during pregnancy encourage the growth of yeast. This is a very common time for an infection to occur. Until the baby is born, it may be hard to completely eliminate yeast infections. If you believe you are pregnant, tell your doctor.
Menstruation: Sometimes, monthly changes in hormone levels may lead to yeast infections.
Diabetes: In addition to heat and moisture, yeast thrives on sugar. Because diabetics often have sugar in their urine, their vaginas are rich in this substance. Careful control of diabetes may help prevent yeast infection.
Controlling these factors can help eliminate yeast infections and may prevent them from coming back.
Some other helpful tips:
- For best results, be sure to use the medication as prescribed by your doctor, even if you feel better very quickly.
- Avoid sexual intercourse, if your doctor advises you to do so. The suppository formulation (not the cream) may damage the diaphragm. Therefore, use of the diaphragm during therapy with the suppository is not recommended. Consult your physician.
- If your partner has any penile itching, redness, or discomfort, he should consult his physician and mention that you are being treated for a yeast infection.
- You can use the medication even if you are having your menstrual period. However, you should not use tampons because they may absorb the medication. Instead, use external sanitary pads or napkins until you have finished your medication or if the vaginal medication leaks.
- Dry the genital area thoroughly after showering, bathing, or swimming. Change out of a wet bathing suit or damp exercise clothes as soon as possible. A dry environment is less likely to encourage the growth of yeast.
- Wipe from front to rear (away from the vagina) after a bowel movement.
- Don’t douche unless your doctor specifically tells you to do so. Douching may disturb the vaginal balance.
- Don’t scratch if you can help it. Scratching can cause more irritation and spread the infection.
- Discuss with your physician any medication you are already taking. Certain types of medication can make your vagina more susceptible to infection.
- Eat nutritious meals to promote your general health.
IF YOU HAVE A QUESTION
Contact Teva Pharmaceuticals USA, Inc. at 1-888-838-2872 or call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.Manufactured for:
Teva Pharmaceuticals USA, Inc.
Parsippany, NJ 07054Rev. A 7/2020
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
MICONAZOLE NITRATE
miconazole nitrate suppositoryProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0472-1738 Route of Administration VAGINAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MICONAZOLE NITRATE (UNII: VW4H1CYW1K) (MICONAZOLE - UNII:7NNO0D7S5M) MICONAZOLE NITRATE 200 mg Inactive Ingredients Ingredient Name Strength HYDROGENATED PALM KERNEL OIL (UNII: FM8D1RE2VP) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0472-1738-03 3 in 1 CARTON; Type 0: Not a Combination Product 01/18/1995 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA073508 01/18/1995 Labeler - Actavis Pharma, Inc. (119723554)