Label: LITHIUM CARBONATE tablet, extended release
-
Contains inactivated NDC Code(s)
NDC Code(s): 54868-5239-0, 54868-5239-1 - Packager: Physicians Total Care, Inc.
- This is a repackaged label.
- Source NDC Code(s): 0054-0021
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated June 8, 2010
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
Rx only
Lithium toxicity is closely related to serum lithium levels, and can occur at doses close to therapeutic levels. Facilities for prompt and accurate serum lithium determinations should be available before initiating therapy (see DOSAGE AND ADMINISTRATION).
-
DESCRIPTION
Lithium Carbonate Extended Release Tablets, USP contain lithium carbonate, a white, odorless alkaline powder with molecular formula Li2CO3 and molecular weight 73.89. Lithium is an element of the alkali-metal group with atomic number 3, atomic weight 6.94 and an emission line at 671 nm on the flame photometer.
Each beige-colored, extended release tablet contains 300 mg of lithium carbonate. This slowly dissolving, film-coated tablet for oral administration is designed to give lower serum lithium peak concentrations than obtained with conventional oral lithium dosage forms. Inactive ingredients consist of calcium stearate, Opadry II (Flesh), povidone, sodium chloride, sodium lauryl sulfate, and sorbitol. Opadry II (Flesh) contains hypromellose, iron oxide red, iron oxide yellow, polyethylene glycol, polydextrose, titanium dioxide, and triacetin.
The tablets meet the requirements of USP Dissolution Test 5 in the USP monograph for Lithium Carbonate Extended Release Tablets USP, 300 mg.
- CLINICAL PHARMACOLOGY
-
INDICATIONS AND USAGE
Lithium Carbonate Extended Release Tablets are indicated in the treatment of manic episodes of Bipolar Disorder. Bipolar Disorder, Manic (DSM-IV) is equivalent to Manic Depressive illness, Manic, in the older DSM-II terminology. Lithium Carbonate Extended Release Tablets are also indicated as a maintenance treatment for individuals with a diagnosis of Bipolar Disorder. Maintenance therapy reduces the frequency of manic episodes and diminishes the intensity of those episodes which may occur.
Typical symptoms of mania include pressure of speech, motor hyperactivity, reduced need for sleep, flight of ideas, grandiosity, elation, poor judgment, aggressiveness, and possibly hostility. When given to a patient experiencing a manic episode, lithium may produce a normalization of symptomatology within 1 to 3 weeks.
-
WARNINGS
Lithium should generally not be given to patients with significant renal or cardiovascular disease, severe debilitation, dehydration, sodium depletion, and to patients receiving diuretics, or angiotensin converting enzyme (ACE) inhibitors, since the risk of lithium toxicity is very high in such patients. If the psychiatric indication is life threatening, and if such a patient fails to respond to other measures, lithium treatment may be undertaken with extreme caution, including daily serum lithium determinations and adjustment to the usually low doses ordinarily tolerated by these individuals. In such instances, hospitalization is a necessity.
Chronic lithium therapy may be associated with diminution of renal concentrating ability, occasionally presenting as nephrogenic diabetes insipidus, with polyuria and polydipsia. Such patients should be carefully managed to avoid dehydration with resulting lithium retention and toxicity. This condition is usually reversible when lithium is discontinued.
Morphologic changes with glomerular and interstitial fibrosis and nephron atrophy have been reported in patients on chronic lithium therapy. Morphologic changes have also been seen in manic-depressive patients never exposed to lithium. The relationship between renal function and morphologic changes and their association with lithium therapy have not been established.
Kidney function should be assessed prior to and during lithium therapy. Routine urinalysis and other tests may be used to evaluate tubular function (e.g., urine specific gravity or osmolality following a period of water deprivation, or 24-hour urine volume) and glomerular function (e.g., serum creatinine or creatinine clearance). During lithium therapy, progressive or sudden changes in renal function, even within the normal range, indicate the need for re-evaluation of treatment.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus a neuroleptic, most notably haloperidol. In some instances, the syndrome was followed by irreversible brain damage. Because of possible causal relationship between these events and the concomitant administration of lithium and neuroleptic drugs, patients receiving such combined therapy or patients with organic brain syndrome or other CNS impairment should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as Neuroleptic Malignant Syndrome (NMS).
Lithium toxicity is closely related to serum lithium concentrations and can occur at doses close to the therapeutic concentrations (see DOSAGE AND ADMINISTRATION).
Outpatients and their families should be warned that the patient must discontinue lithium therapy and contact his physician if such clinical signs of lithium toxicity as diarrhea, vomiting, tremor, mild ataxia, drowsiness, or muscular weakness occur.
Lithium may prolong the effects of neuromuscular blocking agents. Therefore, neuromuscular blocking agents should be given with caution to patients receiving lithium.
Usage in Pregnancy
Adverse effects on nidation in rats, embryo viability in mice, and metabolism in vitro of rat testis and human spermatozoa have been attributed to lithium, as have teratogenicity in submammalian species and cleft palate in mice.
In humans, lithium may cause fetal harm when administered to a pregnant woman. Data from lithium birth registries suggest an increase in cardiac and other anomalies especially Ebstein’s anomaly. If this drug is used in women of childbearing potential, or during pregnancy, or if a patient becomes pregnant while taking this drug, the patient should be apprised by their physician of the potential hazard to the fetus.
Usage in Nursing Mothers
Lithium is excreted in human milk. Nursing should not be undertaken during lithium therapy except in rare and unusual circumstances where, in the view of the physician, the potential benefits to the mother outweigh possible hazard to the infant or neonate. Signs and symptoms of lithium toxicity such as hypertonia, hypothermia, cyanosis and ECG changes have been reported in some infants and neonates.
Pediatric Use
Safety and effectiveness in pediatric patients under 12 years of age have not been determined; its use in these patients is not recommended.
There has been a report of transient syndrome of acute dystonia and hyperreflexia occurring in a 15 kg pediatric patient who ingested 300 mg of lithium carbonate.
-
PRECAUTIONS
The ability to tolerate lithium is greater during the acute manic phase and decreases when manic symptoms subside (see DOSAGE AND ADMINISTRATION).
The distribution space of lithium approximates that of total body water. Lithium is primarily excreted in urine with insignificant excretion in feces. Renal excretion of lithium is proportional to its plasma concentration. The elimination half-life of lithium is approximately 24 hours. Lithium decreases sodium reabsorption by the renal tubules which could lead to sodium depletion. Therefore, it is essential for the patient to maintain a normal diet, including salt, and an adequate fluid intake (2500 to 3500 mL) at least during the initial stabilization period. Decreased tolerance to lithium has been reported to ensue from protracted sweating or diarrhea and, if such occur, supplemental fluid and salt should be administered under careful medical supervision and lithium intake reduced or suspended until the condition is resolved.
In addition to sweating and diarrhea, concomitant infection with elevated temperatures may also necessitate a temporary reduction or cessation of medication.
Previously existing thyroid disorders do not necessarily constitute a contraindication to lithium treatment. Where hypothyroidism preexists, careful monitoring of thyroid function during lithium stabilization and maintenance allows for correction of changing thyroid parameters and/or adjustment of lithium doses, if any. If hypothyroidism occurs during lithium stabilization and maintenance, supplemental thyroid treatment may be used. In general, the concomitant use of diuretics or angiotensin converting enzyme (ACE) inhibitors with lithium carbonate should be avoided. In those cases where concomitant use is necessary, extreme caution is advised since sodium loss from these drugs may reduce the renal clearance of lithium resulting in increased serum lithium concentrations with the risk of lithium toxicity. When such combinations are used, the lithium dosage may need to be decreased, and more frequent monitoring of lithium serum concentrations is recommended. See WARNINGS for additional caution information.
Concomitant administration of carbamazepine and lithium may increase the risk of neurotoxic side effects.
The following drugs can lower serum lithium concentrations by increasing urinary lithium excretion: acetazolamide, urea, xanthine preparations and alkalinizing agents such as sodium bicarbonate.
Concomitant extended use of iodide preparations, especially potassium iodide, with lithium may produce hypothyroidism.
Concurrent use of calcium channel blocking agents with lithium may increase the risk of neurotoxicity in the form of ataxia, tremors, nausea, vomiting, diarrhea and/or tinnitus.
Concurrent use of metronidazole with lithium may provoke lithium toxicity due to reduced renal clearance. Patients receiving such combined therapy should be monitored closely.
Concurrent use of fluoxetine with lithium has resulted in both increased and decreased serum lithium concentrations. Patients receiving such combined therapy should be monitored closely.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDS)
Lithium levels should be closely monitored when patients initiate or discontinue NSAID use. In some cases, lithium toxicity has resulted from interactions between an NSAID and lithium. Indomethacin and piroxicam have been reported to increase significantly steady-state plasma lithium concentrations. There is also evidence that other nonsteroidal anti-inflammatory agents, including the selective cyclooxygenase-2 (COX-2) inhibitors, have the same effect. In a study conducted in healthy subjects, mean steady-state lithium plasma levels increased approximately 17% in subjects receiving lithium 450 mg BID with celecoxib 200 mg BID as compared to subjects receiving lithium alone.
Lithium may impair mental and/or physical abilities. Patients should be cautioned about activities requiring alertness (e.g., operating vehicles or machinery).
Nursing Mothers
Because of the potential for serious adverse reactions in nursing infants and neonates from lithium, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother (see WARNINGS: Usage in Nursing Mothers).
Pediatric Use
Safety and effectiveness in pediatric patients below the age of 12 have not been established (see WARNINGS: Pediatric Use).
Geriatric Use
Clinical studies of lithium carbonate tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other therapy.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
-
ADVERSE REACTIONS
The occurrence and severity of adverse reactions are generally directly related to serum lithium concentrations and to individual patient sensitivity to lithium. They generally occur more frequently and with greater severity at higher concentrations.
Adverse reactions may be encountered at serum lithium concentrations below 1.5 mEq/L. Mild to moderate adverse reactions may occur at concentrations from 1.5 to 2.5 mEq/L, and moderate to severe reactions may be seen at concentrations from 2 mEq/L and above.
Fine hand tremor, polyuria and mild thirst may occur during initial therapy for the acute manic phase and may persist throughout treatment. Transient and mild nausea and general discomfort may also appear during the first few days of lithium administration.
These side effects usually subside with continued treatment or with a temporary reduction or cessation of dosage. If persistent, a cessation of lithium therapy may be required. Diarrhea, vomiting, drowsiness, muscular weakness and lack of coordination may be early signs of lithium intoxication, and can occur at lithium concentrations below 2 mEq/L. At higher concentrations, giddiness, ataxia, blurred vision, tinnitus and a large output of dilute urine may be seen. Serum lithium concentrations above 3 mEq/L may produce a complex clinical picture involving multiple organs and organ systems. Serum lithium concentrations should not be permitted to exceed 2 mEq/L during the acute treatment phase.
The following reactions have been reported and appear to be related to serum lithium concentrations, including concentrations within the therapeutic range:
Central Nervous System
tremor, muscle hyperirritability (fasciculations, twitching, clonic movements of whole limbs), hypertonicity, ataxia, choreoathetotic movements, hyperactive deep tendon reflex, extrapyramidal symptoms including acute dystonia, cogwheel rigidity, blackout spells, epileptiform seizures, slurred speech, dizziness, vertigo, downbeat nystagmus, incontinence of urine or feces, somnolence, psychomotor retardation, restlessness, confusion, stupor, coma, tongue movements, tics, tinnitus, hallucinations, poor memory, slowed intellectual functioning, startled response, worsening of organic brain syndromes. Cases of Pseudotumor Cerebri (increased intracranial pressure and papilledema) have been reported with lithium use. If undetected, this condition may result in enlargement of the blind spot, constriction of visual fields and eventual blindness due to optic atrophy. Lithium should be discontinued, if clinically possible, if this syndrome occurs.
Cardiovascular
cardiac arrhythmia, hypotension, peripheral circulatory collapse, bradycardia, sinus node dysfunction and severe bradycardia (which may result in syncope).
Gastrointestinal
anorexia, nausea, vomiting, diarrhea, gastritis, salivary gland swelling, abdominal pain, excessive salivation, flatulence, indigestion.
Genitourinary
glycosuria, decreased creatinine clearance, albuminuria, oliguria, and symptoms of nephrogenic diabetes insipidus including polyuria, thirst and polydipsia.
Dermatologic
drying and thinning of hair, alopecia, anesthesia of skin, acne, chronic folliculitis, xerosis cutis, psoriasis or its exacerbation, generalized pruritus with or without rash, cutaneous ulcers, angioedema.
Thyroid Abnormalities
euthyroid goiter and/or hypothyroidism (including myxedema) accompanied by lower T3 and T4. 131Iodine uptake may be elevated (see PRECAUTIONS). Paradoxically, rare cases of hyperthyroidism have been reported.
EEG Changes
diffuse slowing, widening of frequency spectrum, potentiation and disorganization of background rhythm.
Miscellaneous
Fatigue, lethargy, transient scotomata, exophthalmos, dehydration, weight loss, leucocytosis, headache, transient hyperglycemia, hypercalcemia, hyperparathyroidism, albuminuria, excessive weight gain, edematous swelling of ankles or wrists, metallic taste, dysgeusia/taste distortion, salty taste, thirst, swollen lips, tightness in chest, swollen and/or painful joints, fever, polyarthralgia, and dental caries.
Some reports of nephrogenic diabetes insipidus, hyperparathyroidism and hypothyroidism which persist after lithium discontinuation have been received.
A few reports have been received of the development of painful discoloration of fingers and toes and coldness of the extremities within one day of starting lithium treatment. The mechanism through which these symptoms (resembling Raynaud’s Syndrome) developed is not known. Recovery followed discontinuance.
-
OVERDOSAGE
The toxic concentrations for lithium (≥1.5 mEq/L) are close to the therapeutic concentrations (0.6 to 1.2 mEq/L). It is therefore important that patients and their families be cautioned to watch for early toxic symptoms and to discontinue the drug and inform the physician should they occur. (Toxic symptoms are listed in detail under ADVERSE REACTIONS.)
Treatment
No specific antidote for lithium poisoning is known. Treatment is supportive. Early symptoms of lithium toxicity can usually be treated by reduction or cessation of dosage of the drug and resumption of the treatment at a lower dose after 24 to 48 hours. In severe cases of lithium poisoning, the first and foremost goal of treatment consists of elimination of this ion from the patient.
Treatment is essentially the same as that used in barbiturate poisoning: 1) gastric lavage, 2) correction of fluid and electrolyte imbalance and, 3) regulation of kidney functioning. Urea, mannitol, and aminophylline all produce significant increases in lithium excretion. Hemodialysis is an effective and rapid means of removing the ion from the severely toxic patient. However, patient recovery may be slow.
Infection prophylaxis, regular chest X-rays, and preservation of adequate respiration are essential.
-
DOSAGE AND ADMINISTRATION
Acute Mania
Optimal patient response can usually be established with 1800 mg/day in the following dosages:
ACUTE MANIA Morning Afternoon Nighttime Lithium Carbonate Extended
Release Tablets3 tabs
(900 mg)3 tabs
(900 mg)Such doses will normally produce an effective serum lithium concentration ranging between 1 and 1.5 mEq/L. Dosage must be individualized according to serum concentrations and clinical response. Regular monitoring of the patient’s clinical state and of serum lithium concentrations is necessary. Serum concentrations should be determined twice per week during the acute phase, and until the serum concentrations and clinical condition of the patient have been stabilized.
Long-Term Control
Desirable serum lithium concentrations are 0.6 to 1.2 mEq/L which can usually be achieved with 900 to 1200 mg/day. Dosage will vary from one individual to another, but generally the following dosages will maintain this concentration:
LONG-TERM CONTROL Morning Afternoon Nighttime Lithium Carbonate Extended
Release Tablets2 tabs
(600 mg)2 tabs
(600 mg)Serum lithium concentrations in uncomplicated cases receiving maintenance therapy during remission should be monitored at least every two months. Patients abnormally sensitive to lithium may exhibit toxic signs at serum concentrations of 1 to 1.5 mEq/L. Geriatric patients often respond to reduced dosage, and may exhibit signs of toxicity at serum concentrations ordinarily tolerated by other patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Important Considerations
- Blood samples for serum lithium determinations should be drawn immediately prior to the next dose when lithium concentrations are relatively stable (i.e., 8 to 12 hours after previous dose). Total reliance must not be placed on serum concentrations alone. Accurate patient evaluation requires both clinical and laboratory analysis.
- Lithium Carbonate Extended Release Tablets USP must be swallowed whole and never chewed or crushed.
-
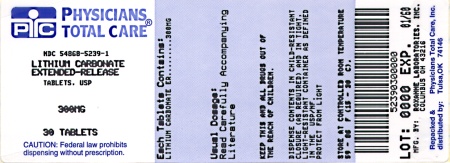
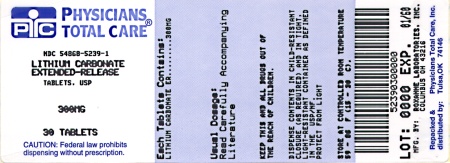
HOW SUPPLIED
Lithium Carbonate Extended Release Tablets, USP
300 mg beige-colored, biconvex, film-coated tablets
(Identified 54 107)
Bottles of 30
NDC 54868-5239-1
Bottles of 60
NDC 54868-5239-0
Storage
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.] Protect from moisture. Dispense in tight, child-resistant container as defined in USP/NF.
10002523/04October 2007
© RLI, 2007
Relabeling and Repackaging by:
Physicians Total Care, Inc.
Tulsa, OK 74146
- Package Label - Lithium Carbonate Extended Release Tablets, USP 300 mg
-
INGREDIENTS AND APPEARANCE
LITHIUM CARBONATE
lithium carbonate tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:54868-5239(NDC:0054-0021) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LITHIUM CARBONATE (UNII: 2BMD2GNA4V) (LITHIUM CATION - UNII:8H8Z5UER66) LITHIUM CARBONATE 300 mg Inactive Ingredients Ingredient Name Strength CALCIUM STEARATE (UNII: 776XM7047L) POVIDONE (UNII: FZ989GH94E) SODIUM CHLORIDE (UNII: 451W47IQ8X) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SORBITOL (UNII: 506T60A25R) Product Characteristics Color brown (beige) Score no score Shape ROUND (biconvex) Size 10mm Flavor Imprint Code 54;107 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:54868-5239-0 60 in 1 BOTTLE, PLASTIC 2 NDC:54868-5239-1 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076832 03/01/2005 Labeler - Physicians Total Care, Inc. (194123980) Establishment Name Address ID/FEI Business Operations Physicians Total Care, Inc. 194123980 relabel, repack