Label: ALVIMOPAN capsule
- NDC Code(s): 0054-0668-82
- Packager: Hikma Pharmaceuticals USA Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
Drug Label Information
Updated October 24, 2022
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ALVIMOPAN CAPSULES safely and effectively. See full prescribing information for ALVIMOPAN CAPSULES.
ALVIMOPAN capsules, for oral use
Initial U.S. Approval: 2008WARNING: POTENTIAL RISK OF MYOCARDIAL INFARCTION WITH LONG-TERM USE: FOR SHORT-TERM HOSPITAL USE ONLY
See full prescribing information for complete boxed warning.
- •
- Increased incidence of myocardial infarction was seen in a clinical trial of patients taking alvimopan for long-term use. (5.1)
- •
- Alvimopan capsules are available only through a restricted program for short-term use (15 doses) called the Alvimopan REMS Program. (5.1, 5.2)
INDICATIONS AND USAGE
Alvimopan capsules are an opioid antagonist indicated to accelerate the time to upper and lower gastrointestinal recovery following surgeries that include partial bowel resection with primary anastomosis. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Capsules: 12 mg (3)
CONTRAINDICATIONS
Patients who have taken therapeutic doses of opioids for more than 7 consecutive days prior to taking alvimopan capsules. (4)
WARNINGS AND PRECAUTIONS
- •
- Myocardial Infarction: A higher number of myocardial infarctions was reported in patients treated with alvimopan 0.5 mg twice daily compared with placebo in a 12-month study in patients treated with opioids for chronic non-cancer pain, although a causal relationship with long-term use has not been established. (5.1)
- •
- Gastrointestinal Adverse Reactions in Opioid Tolerant Patients: Patients recently exposed to opioids may be more sensitive to the effects of alvimopan and experience gastrointestinal adverse reactions (e.g., abdominal pain, nausea and vomiting, and diarrhea). (5.3)
- •
- Patients with Severe Hepatic Impairment: Increased risk of serious adverse reactions due to higher plasma concentrations; use is not recommended. (5.4, 8.6)
- •
- Patients with End-Stage Renal Disease: No studies have been conducted; use is not recommended. (5.5, 8.7)
- •
- Patients with Complete Gastrointestinal Obstruction: No studies have been conducted in patients with complete gastrointestinal obstruction or in patients who have surgery for correction of complete bowel obstruction; use is not recommended. (5.6)
- •
- Patients with Pancreatic and Gastric Anastomoses: No studies have been conducted; use is not recommended. (5.7)
ADVERSE REACTIONS
Most common adverse reaction (≥1.5%): dyspepsia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-800-962-8364 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
- •
- Hepatic Impairment: Monitor patients with mild-to-moderate impairment for gastrointestinal adverse reactions. (8.6)
- •
- Renal Impairment: Monitor patients with mild-to-severe impairment for gastrointestinal adverse reactions. (8.7)
- •
- Race/Ethnicity: Monitor Japanese patients for gastrointestinal adverse reactions. (8.8)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: POTENTIAL RISK OF MYOCARDIAL INFARCTION WITH LONG-TERM USE: FOR SHORT-TERM HOSPITAL USE ONLY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Potential Risk of Myocardial Infarction with Long-Term Use
5.2 Alvimopan REMS Program
5.3 Gastrointestinal-Related Adverse Reactions in Opioid-Tolerant Patients
5.4 Risk of Serious Adverse Reactions in Patients with Severe Hepatic Impairment
5.5 End-Stage Renal Disease
5.6 Risk of Serious Adverse Reactions in Patients with Complete Gastrointestinal Obstruction
5.7 Risk of Serious Adverse Reactions in Pancreatic and Gastric Anastomoses
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Effects of Alvimopan on Intravenous Morphine
7.2 Effects of Concomitant Acid Blockers or Antibiotics
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
8.8 Race/Ethnicity
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: POTENTIAL RISK OF MYOCARDIAL INFARCTION WITH LONG-TERM USE: FOR SHORT-TERM HOSPITAL USE ONLY
There was a greater incidence of myocardial infarction in alvimopan-treated patients compared to placebo-treated patients in a 12-month clinical trial, although a causal relationship has not been established. In short-term trials with alvimopan, no increased risk of myocardial infarction was observed [see Warnings and Precautions (5.1)].
Because of the potential risk of myocardial infarction with long-term use, alvimopan is available only through a restricted program for short-term use (15 doses) under a Risk Evaluation and Mitigation Strategy (REMS) called the Alvimopan REMS Program [see Warnings and Precautions (5.1, 5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For hospital use only. The recommended adult dosage of alvimopan capsules is 12 mg administered 30 minutes to 5 hours prior to surgery followed by 12 mg twice daily beginning the day after surgery until discharge for a maximum of 7 days. Patients should not receive more than 15 doses of alvimopan capsules.
Alvimopan capsules can be taken with or without food [see Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Alvimopan capsules are contraindicated in patients who have taken therapeutic doses of opioids for more than 7 consecutive days immediately prior to taking alvimopan capsules [see Warnings and Precautions (5.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Potential Risk of Myocardial Infarction with Long-Term Use
There were more reports of myocardial infarctions in patients treated with alvimopan 0.5 mg twice daily compared with placebo-treated patients in a 12-month study of patients treated with opioids for chronic non-cancer pain (alvimopan 0.5 mg, n = 538; placebo, n = 267). In this study, the majority of myocardial infarctions occurred between 1 and 4 months after initiation of treatment. This imbalance has not been observed in other studies of alvimopan in patients treated with opioids for chronic pain, nor in patients treated within the surgical setting, including patients undergoing surgeries that included bowel resection who received alvimopan 12 mg twice daily for up to 7 days (the indicated dose and patient population; alvimopan 12 mg, n = 1,142; placebo, n = 1,120). A causal relationship with alvimopan with long-term use has not been established.
Alvimopan capsules are available only through a program under a REMS that restricts use to enrolled hospitals [see Warnings and Precautions (5.2)].
5.2 Alvimopan REMS Program
Alvimopan capsules are available only through a program called the Alvimopan REMS Program that restricts use to enrolled hospitals because of the potential risk of myocardial infarction with long-term use of alvimopan capsules [see Warnings and Precautions (5.1)].
Notable requirements of the Alvimopan REMS Program include the following:
Alvimopan capsules are available only for short-term (15 doses) use in hospitalized patients. Only hospitals that have enrolled in and met all of the requirements for the Alvimopan REMS Program may use alvimopan capsules.
To enroll in the Alvimopan REMS Program, an authorized hospital representative must acknowledge that:
- •
- hospital staff who prescribe, dispense, or administer alvimopan capsules have been provided the educational materials on the need to limit use of alvimopan capsules to short-term, inpatient use;
- •
- patients will not receive more than 15 doses of alvimopan capsules; and
- •
- alvimopan capsules will not be dispensed to patients after they have been discharged from the hospital.
- Further information is available at www.alvimopanREMS.com or 1-800-278-0340.
5.3 Gastrointestinal-Related Adverse Reactions in Opioid-Tolerant Patients
Patients recently exposed to opioids are expected to be more sensitive to the effects of mu-opioid receptor antagonists, such as alvimopan. Since alvimopan acts peripherally, clinical signs and symptoms of increased sensitivity would be related to the gastrointestinal tract (e.g., abdominal pain, nausea and vomiting, diarrhea). Patients receiving more than 3 doses of an opioid within the week prior to surgery were not studied in the postoperative ileus clinical trials. Therefore, if alvimopan is administered to these patients, they should be monitored for gastrointestinal adverse reactions. Alvimopan is contraindicated in patients who have taken therapeutic doses of opioids for more than 7 consecutive days immediately prior to taking alvimopan [see Contraindications (4)].
5.4 Risk of Serious Adverse Reactions in Patients with Severe Hepatic Impairment
Patients with severe hepatic impairment may be at higher risk of serious adverse reactions (including dose-related serious adverse reactions) because up to 10-fold higher plasma concentrations of alvimopan have been observed in such patients compared with patients with normal hepatic function. Therefore, the use of alvimopan is not recommended in this population [see Use in Specific Populations (8.6)].
5.5 End-Stage Renal Disease
No studies have been conducted in patients with end-stage renal disease. Alvimopan is not recommended for use in these patients [see Use in Specific Populations (8.7)].
5.6 Risk of Serious Adverse Reactions in Patients with Complete Gastrointestinal Obstruction
No studies have been conducted in patients with complete gastrointestinal obstruction or in patients who have surgery for correction of complete bowel obstruction. Alvimopan is not recommended for use in these patients.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- •
- Potential Risk of Myocardial Infarction with Long-Term Use [see Warnings and Precautions (5.1)]
- •
- Gastrointestinal-Related Adverse Reactions in Opioid-Tolerant Patients [see Warnings and Precautions (5.3)]
- •
- Risk of Serious Adverse Reactions in Patients with Severe Hepatic Impairment [see Warnings and Precautions (5.4)]
- •
- Risk of Serious Adverse Reactions in Patients with Complete Gastrointestinal Obstruction [see Warnings and Precautions (5.6)]
- •
- Risk of Serious Adverse Reactions in Pancreatic and Gastric Anastomoses [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be compared directly with rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The adverse event information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
The data described below reflect exposure to alvimopan 12 mg in 1,793 patients in 10 placebo-controlled studies. The population was 19 to 97 years old, 64% were female, and 84% were Caucasian; 64% were undergoing a surgery that included bowel resection. The first dose of alvimopan was administered 30 minutes to 5 hours before the scheduled start of surgery and then twice daily until hospital discharge (or for a maximum of 7 days of postoperative treatment).
Among alvimopan-treated patients undergoing surgeries that included a bowel resection, the most common adverse reaction (incidence ≥1.5%) occurring with a higher frequency than placebo was dyspepsia (alvimopan, 1.5%; placebo, 0.8%). Adverse reactions are events that occurred after the first dose of study medication treatment and within 7 days of the last dose of study medication or events present at baseline that increased in severity after the start of study medication treatment.
-
7 DRUG INTERACTIONS
7.1 Effects of Alvimopan on Intravenous Morphine
Coadministration of alvimopan does not appear to alter the pharmacokinetics of morphine and its metabolite, morphine-6-glucuronide, to a clinically significant degree when morphine is administered intravenously. Dosage adjustment for intravenously administered morphine is not necessary when it is coadministered with alvimopan.
7.2 Effects of Concomitant Acid Blockers or Antibiotics
A population pharmacokinetic analysis suggests that the pharmacokinetics of alvimopan were not affected by concomitant administration of acid blockers (proton pump inhibitors (PPIs), histamine-2 (H2) receptor antagonists) or antibiotics. No dosage adjustments are necessary in patients taking acid blockers or antibiotics with alvimopan.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary:
Available data regarding use of alvimopan in pregnant women are limited, and are insufficient to inform a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes.
No fetal harm was observed in animal reproduction studies with oral administration of alvimopan during organogenesis to pregnant rats at doses 68 to 136 times the recommended human oral dose, or with intravenous administration during organogenesis to pregnant rats and pregnant rabbits at doses 3.4 to 6.8 times, and 5 to 10 times, respectively, the recommended human oral dose (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Animal Data
Embryo-fetal studies were performed in pregnant rats during organogenesis (gestation days 7 through 19, or 20) at oral doses up to 200 mg/kg/day (about 68 to 136 times the recommended human oral dose based on body surface area) and at intravenous doses up to 10 mg/kg/day (about 3.4 to 6.8 times the recommended human oral dose based on body surface area). A study in pregnant rabbits during organogenesis (gestation days 6 through 18) at intravenous doses up to 15 mg/kg/day (about 5 to 10 times the recommended human oral dose based on body surface area) revealed no evidence of harm to the fetus due to alvimopan.
In an intravenous pre- and postnatal development study (gestation day 7 through lactation day 20) in rats, alvimopan did not cause any adverse effect on pre- and postnatal development at doses up to 10 mg/kg/day (about 6.8 times the recommended human oral dose based on body surface area).
8.2 Lactation
Risk Summary:
There are no data on the presence of alvimopan in human milk, the effects on the breastfed infant, or the effects on milk production. Alvimopan and its ‘metabolite’ are detected in the milk of lactating rats following intravenous administration (see Data). It is unknown if alvimopan is present in rat milk following oral administration.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for alvimopan and any potential adverse effects on the breastfed child from alvimopan or from the underlying maternal condition.
Data
Following intravenous administration of alvimopan to lactating rats at 10 mg/kg/day, concentrations of alvimopan and its ‘metabolite’ in the milk were approximately 15- and 0.11-fold, respectively, the concentration of alvimopan in maternal plasma at 1-hour post-dose.
8.5 Geriatric Use
Of the total number of patients in 6 clinical efficacy studies treated with alvimopan 12 mg or placebo, 46% were 65 years of age and over, while 18% were 75 years of age and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. No dosage adjustment based on increased age is required [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
Alvimopan is not recommended for use in patients with severe hepatic impairment.
Dosage adjustment is not required for patients with mild-to-moderate hepatic impairment. Patients with mild-to-moderate hepatic impairment should be closely monitored for possible adverse reactions (e.g., diarrhea, gastrointestinal pain, cramping) that could indicate high alvimopan or ‘metabolite’ concentrations, and alvimopan should be discontinued if adverse reactions occur [see Warnings and Precautions (5.4), Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Alvimopan is not recommended for use in patients with end-stage renal disease. Dosage adjustment is not required for patients with mild-to-severe renal impairment, but they should be monitored for adverse reactions. Patients with severe renal impairment should be closely monitored for possible adverse reactions (e.g., diarrhea, gastrointestinal pain, cramping) that could indicate high alvimopan or ‘metabolite’ concentrations, and alvimopan should be discontinued if adverse reactions occur [see Clinical Pharmacology (12.3)].
8.8 Race/Ethnicity
No dosage adjustment is necessary in Black, Hispanic, and Japanese patients. However, the exposure to alvimopan in Japanese healthy male subjects was approximately 2-fold greater than in Caucasian subjects. Japanese patients should be closely monitored for possible adverse reactions (e.g., diarrhea, gastrointestinal pain, cramping) that could indicate high alvimopan or ‘metabolite’ concentrations, and alvimopan should be discontinued if adverse reactions occur [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
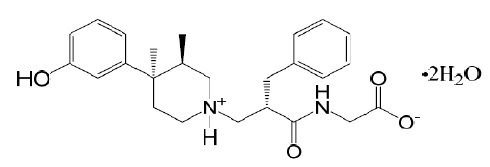
Alvimopan capsules contain alvimopan, an opioid antagonist. Chemically, alvimopan is the single stereoisomer [[2(S)-[[4(R)-(3-hydroxyphenyl)-3(R),4-dimethyl-1-piperidinyl]methyl]-1-oxo-3-phenylpropyl]amino]acetic acid dihydrate. It has the following structural formula:
Alvimopan is a white to light beige powder with a molecular weight of 460.6, and the empirical formula is C25H32N2O4•2H2O. It has a solubility of <0.1 mg/mL in water or buffered solutions between pH 3.0 and 9.0, 1 to 5 mg/mL in buffered solutions at pH 1.2, and 10 to 25 mg/mL in aqueous 0.1 N sodium hydroxide. At physiological pH, alvimopan is zwitterionic, a property that contributes to its low solubility.
Alvimopan capsules for oral administration contain 12 mg of alvimopan on an anhydrous basis suspended in the inactive ingredient polyethylene glycol 3350. The capsule shell contains FD&C Blue 1, gelatin, sodium lauryl sulfate, and titanium dioxide. The black ink contains ammonium hydroxide, ferrosoferric oxide, propylene glycol, and shellac.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Alvimopan is a selective antagonist of the cloned human µ-opioid receptor with a Ki of 0.4 nM (0.2 ng/mL) and no measurable opioid-agonist effects in standard pharmacologic assays. The dissociation of [3H]-alvimopan from the human µ-opioid receptor is slower than that of other opioid ligands, consistent with its higher affinity for the receptor. At concentrations of 1 to 10 µM, alvimopan demonstrated no activity at any of over 70 non-opioid receptors, enzymes, and ion channels.
Postoperative ileus is the impairment of gastrointestinal motility after intra-abdominal surgery or other, non-abdominal surgeries. Postoperative ileus affects all segments of the gastrointestinal tract and may last from 5 to 6 days, or even longer. This may potentially delay gastrointestinal recovery and hospital discharge until its resolution. It is characterized by abdominal distention and bloating, nausea, vomiting, pain, accumulation of gas and fluids in the bowel, and delayed passage of flatus and defecation. Postoperative ileus is the result of a multifactorial process that includes inhibitory sympathetic input and release of hormones, neurotransmitters, and other mediators (e.g., endogenous opioids). A component of postoperative ileus also results from an inflammatory reaction and the effects of opioid analgesics. Morphine and other µ-opioid receptor agonists are universally used for the treatment of acute postsurgical pain; however, they are known to have an inhibitory effect on gastrointestinal motility and may prolong the duration of postoperative ileus.
Following oral administration, alvimopan antagonizes the peripheral effects of opioids on gastrointestinal motility and secretion by competitively binding to gastrointestinal tract µ-opioid receptors. The antagonism produced by alvimopan at opioid receptors is evident in isolated guinea pig ileum preparations in which alvimopan competitively antagonizes the effects of morphine on contractility. Alvimopan achieves this selective gastrointestinal opioid antagonism without reversing the central analgesic effects of µ-opioid agonists.
12.2 Pharmacodynamics
In an exploratory study in healthy subjects, alvimopan 12 mg administered twice a day reduced the delay in small and large bowel transit induced by codeine 30 mg administered 4 times a day, as measured by gastrointestinal scintigraphy. In the same study, concomitant alvimopan did not reduce the delay in gastric emptying induced by codeine.
Cardiac Electrophysiology:
At a dosage of 24 mg twice daily (two times the approved recommended dosage) for 7 days, alvimopan does not prolong the QT interval to any clinically relevant extent. The potential for QTc effects at higher doses has not been studied.
12.3 Pharmacokinetics
Following oral administration of alvimopan, an amide hydrolysis compound is present in the systemic circulation, which is considered a product exclusively of intestinal flora metabolism. This compound is referred to as the ‘metabolite’. It is also a mu-opioid receptor antagonist with a Ki of 0.8 nM (0.3 ng/mL).
Absorption:
Following oral administration of alvimopan capsules in healthy plasma subjects, the alvimopan concentration peaked at approximately 2 hours post-dose. No significant accumulation in the concentration of alvimopan was observed following twice daily dosing. The mean peak plasma concentration was 10.98 (±6.43) ng/mL and mean AUC0-12h was 40.2 (±22.5) ng•h/mL after dosing of alvimopan at 12 mg twice daily for 5 days. The absolute bioavailability was estimated to be 6% (range, 1% to 19%). There was a delay in the appearance of the ‘metabolite’, which had a median Tmax of 36 hours following administration of a single dose of alvimopan. Concentrations of the ‘metabolite’ were highly variable between subjects and within a subject. The ‘metabolite’ accumulated after multiple doses of alvimopan. The mean Cmax for the ‘metabolite’ after alvimopan 12 mg twice daily for 5 days was 35.73 ± 35.29 ng/mL.
Concentrations of alvimopan and its ‘metabolite’ are higher (approximately 1.9-fold and 1.4-fold, respectively) in postoperative ileus patients than in healthy subjects.
Effect of Food: A high-fat meal decreased the extent and rate of alvimopan absorption. The Cmax and AUC were decreased by approximately 38% and 21%, respectively, and the Tmax was prolonged by approximately 1 hour. The clinical significance of this decreased bioavailability is unknown. In postoperative ileus clinical trials, the preoperative dose of alvimopan was administered in a fasting state. Subsequent doses were given without regard to meals.
Distribution:
The steady-state volume of distribution of alvimopan was estimated to be 30±10 L. Plasma protein binding of alvimopan and its ‘metabolite’ was independent of concentration over ranges observed clinically and averaged 80% and 94%, respectively. Both alvimopan and the ‘metabolite’ were bound to albumin and not to alpha-1 acid glycoprotein.
Elimination:
Metabolism and Excretion: In vitro data suggest that alvimopan is not a substrate of CYP enzymes. The average plasma clearance for alvimopan was 402 (±89) mL/min. Renal excretion accounted for approximately 35% of total clearance. There was no evidence that hepatic metabolism was a significant route for alvimopan elimination. Biliary secretion was considered the primary pathway for alvimopan elimination. Unabsorbed drug and unchanged alvimopan resulting from biliary excretion were then hydrolyzed to its ‘metabolite’ by gut microflora. The ‘metabolite’ was eliminated in the feces and in the urine as unchanged ‘metabolite’, the glucuronide conjugate of the ‘metabolite’, and other minor metabolites. The mean terminal phase half-life of alvimopan after multiple oral doses of alvimopan ranged from 10 to 17 hours. The terminal half-life of the ‘metabolite’ ranged from 10 to 18 hours.
Specific Populations:
Geriatric Patients: The pharmacokinetics of alvimopan, but not its ‘metabolite’, were related to age, but this effect was not clinically significant and does not warrant dosage adjustment based on increased age.
Racial or Ethnic Groups: The pharmacokinetic characteristics of alvimopan were not affected by Hispanic or Black race. Plasma ‘metabolite’ concentrations were lower in Black and Hispanic patients (by 43% and 82%, respectively) than in Caucasian patients following alvimopan administration. These changes are not considered to be clinically significant in surgical patients. Japanese healthy male subjects had an approximately 2-fold increase in plasma alvimopan concentrations, but no change in ‘metabolite’ pharmacokinetics. The pharmacokinetics of alvimopan have not been studied in subjects of other East Asian ancestry. Dosage adjustment in Japanese patients is not required [see Use in Specific Populations (8.8)].
Male and Female Patients: There was no effect of sex on the pharmacokinetics of alvimopan or the ‘metabolite’.
Patients with Hepatic Impairment: Exposure to alvimopan following a single 12 mg dose tended to be higher (1.5- to 2-fold, on average) in patients with mild or moderate hepatic impairment (as defined by Child-Pugh Class A and B, n = 8 each) compared with healthy controls (n = 4). There were no consistent effects on the Cmax or half-life of alvimopan in patients with hepatic impairment. However, 2 of 16 patients with mild-to-moderate hepatic impairment had longer than expected half-lives of alvimopan, indicating that some accumulation may occur upon multiple dosing. The Cmax of the ‘metabolite’ tended to be more variable in patients with mild or moderate hepatic impairment than in matched normal subjects. A study of 3 patients with severe hepatic impairment (Child-Pugh Class C), indicated similar alvimopan exposure in 2 patients and an approximately 10-fold increase in Cmax and exposure in 1 patient with severe hepatic impairment when compared with healthy controls [see Warnings and Precautions (5.4), Use in Specific Populations (8.6)].
Patients with Renal Impairment: There was no relationship between renal function (i.e., creatinine clearance [CrCl]) and plasma alvimopan pharmacokinetics (Cmax, AUC, or half-life) in patients with mild (CrCl 51 to 80 mL/min), moderate (CrCl 31 to 50 mL/min), or severe (CrCl less than 30 mL/min) renal impairment (n = 6 each). Renal clearance of alvimopan was related to renal function; however, because renal clearance was only a small fraction (35%) of the total clearance, renal impairment had a small effect on the apparent oral clearance of alvimopan. The half-lives of alvimopan were comparable in the mild, moderate, and control renal impairment groups but longer in the severe renal impairment group. Exposure to the ‘metabolite’ tended to be 2- to 5-fold higher in patients with moderate or severe renal impairment compared with patients with mild renal impairment or control subjects. Thus, there may be accumulation of alvimopan and ‘metabolite’ in patients with severe renal impairment receiving multiple doses of alvimopan. Patients with end-stage renal disease were not studied [see Warnings and Precautions (5.5), Use in Specific Populations (8.7)].
Patients with Crohn’s Disease: There was no relationship between disease activity in patients with Crohn’s disease (measured as Crohn’s Disease Activity Index or bowel movement frequency) and alvimopan pharmacokinetics (AUC or Cmax). Patients with active or quiescent Crohn’s disease had increased variability in alvimopan pharmacokinetics, and exposure tended to be 2-fold higher in patients with quiescent disease than in those with active disease or in normal subjects. Concentrations of the ‘metabolite’ were lower in patients with Crohn’s disease.
Drug Interaction Studies:
Potential for Drugs to Affect Alvimopan Pharmacokinetics: Concomitant administration of alvimopan with inducers or inhibitors of CYP enzymes is unlikely to alter the metabolism of alvimopan because alvimopan is metabolized mainly by non-CYP enzyme pathway. No clinical studies have been performed to assess the effect of concomitant administration of inducers or inhibitors of cytochrome P450 enzymes on alvimopan pharmacokinetics.
In vitro studies suggest that alvimopan and its ‘metabolite’ are substrates for p-glycoprotein. A population pharmacokinetic analysis did not reveal any evidence that alvimopan or ‘metabolite’ pharmacokinetics were influenced by concomitant medications that are mild-to-moderate p-glycoprotein inhibitors. No clinical studies of concomitant administration of alvimopan and strong inhibitors of p-glycoprotein (e.g., verapamil, cyclosporine, amiodarone, itraconazole, quinine, spironolactone, quinidine, diltiazem, bepridil) have been conducted.
A population pharmacokinetic analysis suggests that the pharmacokinetics of alvimopan were not affected by concomitant administration of acid blockers or antibiotics. However, plasma concentrations of the ‘metabolite’ were lower in patients receiving acid blockers or preoperative oral antibiotics (49% and 81%, respectively). No dosage adjustments are necessary in these patients.
Potential for Alvimopan to Affect the Pharmacokinetics of Other Drugs: Alvimopan and its ‘metabolite’ are not inhibitors of CYP 1A2, 2C9, 2C19, 3A4, 2D6, and 2E1 in vitro at concentrations far in excess of those observed clinically.
Alvimopan and its ‘metabolite’ are not inducers of CYP 1A2, 2B6, 2C9, 2C19, and 3A4.
In vitro studies also suggest that alvimopan and its ‘metabolite’ are not inhibitors of p-glycoprotein.
These in vitro findings suggest that alvimopan is unlikely to alter the pharmacokinetics of coadministered drugs through inhibition or induction of CYP enzymes or inhibition of p-glycoprotein.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Two-year carcinogenicity studies were conducted with alvimopan in CD-1 mice at oral doses up to 4000 mg/kg/day and in Sprague Dawley® rats at oral doses up to 500 mg/kg/day. Oral administration of alvimopan for 104 weeks produced significant increases in the incidences of fibroma, fibrosarcoma, and sarcoma in the skin/subcutis, and of osteoma/osteosarcoma in bones of female mice at 4000 mg/kg/day (about 674 times the recommended human dose based on body surface area). In rats, oral administration of alvimopan for 104 weeks did not produce any tumor up to 500 mg/kg/day (about 166 times the recommended human dose based on body surface area).
Mutagenesis: Alvimopan was not genotoxic in the Ames test, the mouse lymphoma cell (L5178Y/TK+/−) forward mutation test, the Chinese Hamster Ovary (CHO) cell chromosome aberration test, or the mouse micronucleus test. The pharmacologically active ‘metabolite’ was negative in the Ames test, chromosome aberration test in CHO cells, and mouse micronucleus test.
Impairment of Fertility: Alvimopan at intravenous doses up to 10 mg/kg/day (about 3.4 to 6.8 times the recommended human oral dose based on body surface area) was found to have no adverse effect on fertility and reproductive performance of male or female rats.
-
14 CLINICAL STUDIES
The efficacy of alvimopan in the management of postoperative ileus was evaluated in 6 multicenter, randomized, double-blind, parallel-group, placebo-controlled studies: 5 U.S. studies (Studies 1 to 4 and 6) and 1 non-U.S. study (Study 5). Patients 18 years of age or older undergoing partial large or small bowel resection surgery with primary anastomosis for colorectal or small bowel disease, total abdominal hysterectomy, or radical cystectomy for bladder cancer (in this procedure, resected segments of bowel are used for reconstruction of the urinary tract) under general anesthesia were randomly assigned to receive oral doses of alvimopan 12 mg or matching placebo. The initial dose was administered at least 30 minutes and up to 5 hours prior to the scheduled start of surgery for most patients, and subsequent doses were administered twice daily beginning on the first postoperative day and continued until hospital discharge or a maximum of 7 days. There were no limitations on the type of general anesthesia used, but intrathecal or epidural opioids or anesthetics were prohibited.
All patients in the U.S. studies were scheduled to receive intravenous patient-controlled opioid analgesia. In the non-U.S. study, patients were scheduled to receive opioids either by intravenous patient-controlled opioid analgesia or bolus parenteral administration (intravenous or intramuscular). In all studies, there was no restriction on the type of opioid used or the duration of intravenous patient-controlled opioid analgesia. A standardized accelerated postoperative care pathway was implemented: early nasogastric tube removal (before the first postoperative dose); early ambulation (day following surgery); early diet advancement (liquids offered the day following surgery for patients undergoing bowel resection and by the third day following surgery for patients undergoing radical cystectomy; solids by the second day following surgery for patients undergoing bowel resection and by the fourth day following surgery for patients undergoing radical cystectomy), as tolerated.
Patients who received more than 3 doses of an opioid (regardless of route) during the 7 days prior to surgery and patients with complete bowel obstruction or who were scheduled for a total colectomy, colostomy, or ileostomy were excluded.
The primary endpoint for all studies was time to achieve resolution of postoperative ileus, a clinically defined composite measure of both upper and lower gastrointestinal recovery. Although both 2-component (GI2: toleration of solid food and first bowel movement) and 3-component (GI3: toleration of solid food and either first flatus or bowel movement) endpoints were used in all studies, GI2 is presented as it represents the most objective and clinically relevant measure of treatment response in patients undergoing surgeries that include a bowel resection. The time from the end of surgery to when the discharge order was written represented the length of hospital stay. In the 6 studies, 1,058 patients who underwent a surgery that included a bowel resection received placebo (not including 157 for total abdominal hysterectomy) and 1,096 patients received alvimopan 12 mg (not including 143 for total abdominal hysterectomy).
The efficacy of alvimopan following total abdominal hysterectomy has not been established. Therefore, the following data are presented only for surgeries that included a bowel resection (i.e., bowel resection or radical cystectomy).
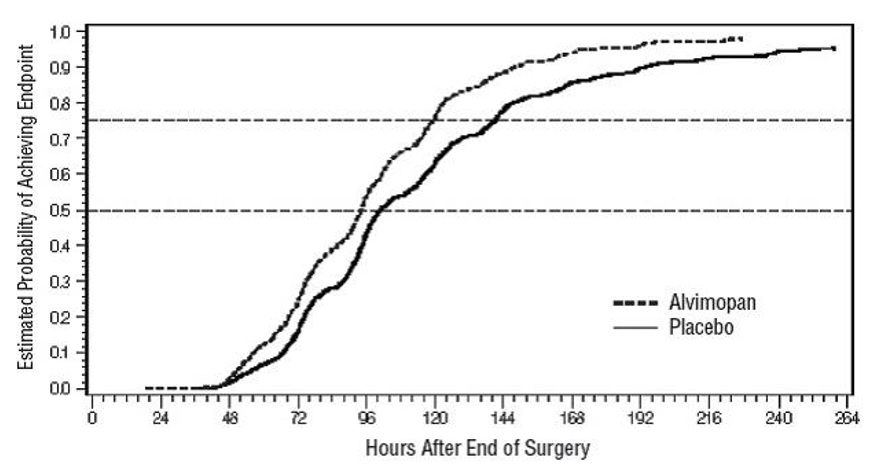
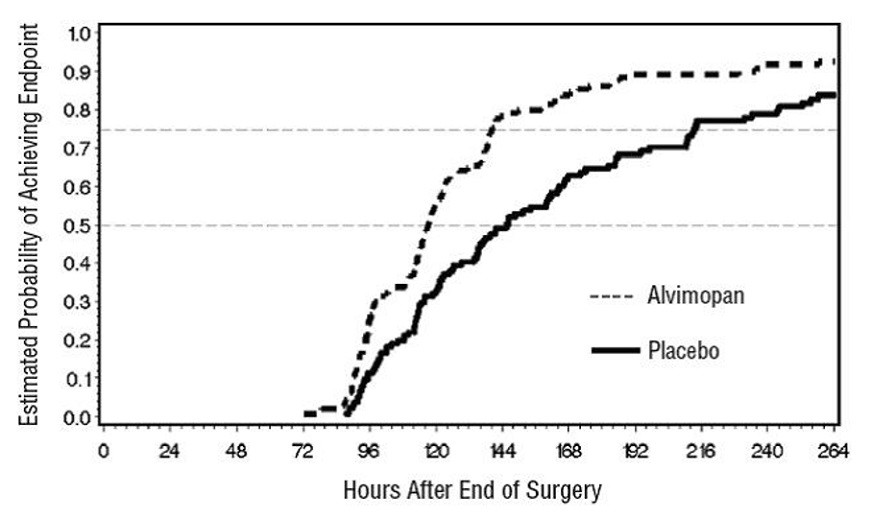
Bowel Resection or Radical Cystectomy: A total of 2,154 patients underwent a surgery that included a bowel resection. The average age was 62 years, 54% were males, and 89% were Caucasian. The most common indications for surgery were colon or rectal cancer/malignancy, bladder cancer, and diverticular disease. In the non-U.S. bowel resection study (Study 5), average daily postoperative opioid consumption was approximately 50% lower and the use of non-opioid analgesics substantially higher, as compared with the U.S. bowel resection studies (Studies 1 to 4) for both treatment groups. During the first 48 hours postoperatively, the use of non-opioid analgesics was 69% compared with 4% for the non-U.S. and U.S. bowel resection studies, respectively. In each of the 6 studies, alvimopan accelerated the time to recovery of gastrointestinal function, as measured by the composite endpoint GI2, and time to discharge order written as compared with placebo. Hazard ratios greater than 1 indicate a higher probability of achieving the event during the study period with treatment with alvimopan than with placebo. Table 1 provides the Hazard Ratios, Kaplan Meier means, medians, and mean and median treatment differences (hours) in gastrointestinal recovery between alvimopan and placebo.
Table 1: GI2 Recovery (Hours) in Bowel Resection Patients Study No.*
Alvimopan 12 mg
Placebo
Treatment Difference
Hazard Ratio
(95% CI)Mean†
Median
Mean†
Median
Means†
Medians
1
92.0
80.0
111.8
96.6
19.8
16.6
1.533
(1.293, 1.816)2
105.9
98.0
132.0
115.2
26.1
17.2
1.625
(1.256, 2.102)
3
116.4
101.8
130.3
116.8
14.0
15.0
1.365
(1.057, 1.764)
4
106.7
101.4
119.9
113.3
13.2
11.9
1.400
(1.035, 1.894)
5
98.2
92.8
108.8
95.9
10.6
3.1
1.299
(1.070, 1.575)
6
132.7
117.0
164.2
145.6
31.5
28.5
1.773
(1.359, 2.311)
* Study 1 = 14CL314; Study 2 = 14CL313; Study 3 = 14CL308; Study 4 = 14CL302; Study 5 = SB-767905/001; Study 6 = 14CL403
† The estimates of the means and differences of treatment means are biased because of the censoring of events not achieved prior to the end of the observation period (10 days). The estimates of the differences of treatment means are likely to be underestimates.
The Kaplan Meier estimate probabilities of patients receiving alvimopan who achieved GI2 were numerically higher at all times throughout the study observation period compared with those of patients receiving placebo (see Figures 1 and 2).
Figure 1: Time to GI2 Based on Results from Studies 1 through 5
Figure 2: Time to GI2 Based on Results from Study 6
In Studies 1 to 4, the differences between alvimopan and placebo patient groups in median time to ‘discharge order written’ ranged from 6 to 22 hours, in favor of alvimopan patients. The group differences in mean time to ‘discharge order written’ ranged from 13 to 21 hours. In Study 6, the median time difference was 19 hours in favor of alvimopan patients (mean time difference 22 hours).
Alvimopan did not reverse opioid analgesia as measured by visual analog scale pain intensity scores and/or amount of postoperative opioids administered across all 6 studies.
There were no sex-, age-, or race-related differences in treatment effect.
The incidence of anastomotic leak was low and comparable in patients receiving either alvimopan or placebo (0.7% and 1.0%, respectively).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
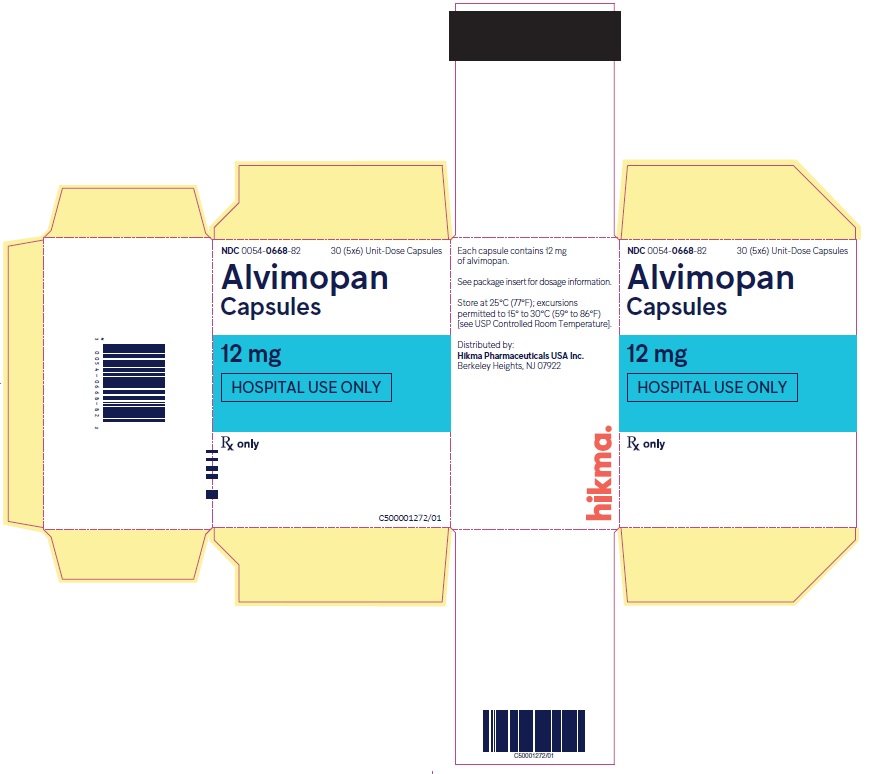
Alvimopan capsules, 12 mg, are blue, opaque hard gelatin capsules with “54 88” imprinted in black on both the body and the cap of the capsule. Alvimopan capsules are available in unit-dose packs of 30 capsules (30 doses) (NDC 0054-0668-82) for hospital use only.
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Recent Use of Opioids:
Inform patients that they must disclose long-term or intermittent opioid pain therapy to their healthcare provider, including any use of opioids in the week prior to receiving alvimopan. Inform patients that recent use of opioids may make them more susceptible to adverse reactions to alvimopan, primarily those limited to the gastrointestinal tract (e.g., abdominal pain, nausea and vomiting, diarrhea).
Hospital Use Only:
Inform patients that alvimopan capsules are available only through a program called the Alvimopan REMS Program under a REMS that restricts use to enrolled hospitals because of the potential risk of myocardial infarction with long-term use of alvimopan. Alvimopan capsules are for hospital use only for no more than 7 days after their bowel resection surgery.
Most Common Adverse Reaction:
Inform patients that the most common adverse reaction with alvimopan in patients undergoing surgeries that include bowel resection is dyspepsia.
Brands listed are the trademarks of their respective owners.
Distributed by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
C50001264/01
Revised October 2022
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
ALVIMOPAN
alvimopan capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0054-0668 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALVIMOPAN (UNII: 677C126AET) (ALVIMOPAN ANHYDROUS - UNII:Q153V49P3Z) ALVIMOPAN ANHYDROUS 12 mg Inactive Ingredients Ingredient Name Strength FD&C BLUE NO. 1 (UNII: H3R47K3TBD) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) AMMONIA (UNII: 5138Q19F1X) FERROSOFERRIC OXIDE (UNII: XM0M87F357) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) Product Characteristics Color BLUE Score no score Shape CAPSULE Size 19mm Flavor Imprint Code 54;88 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0054-0668-82 6 in 1 CARTON 02/06/2024 1 5 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA217753 02/06/2024 Labeler - Hikma Pharmaceuticals USA Inc. (080189610) Establishment Name Address ID/FEI Business Operations West-Ward Columbus Inc. 058839929 MANUFACTURE(0054-0668)