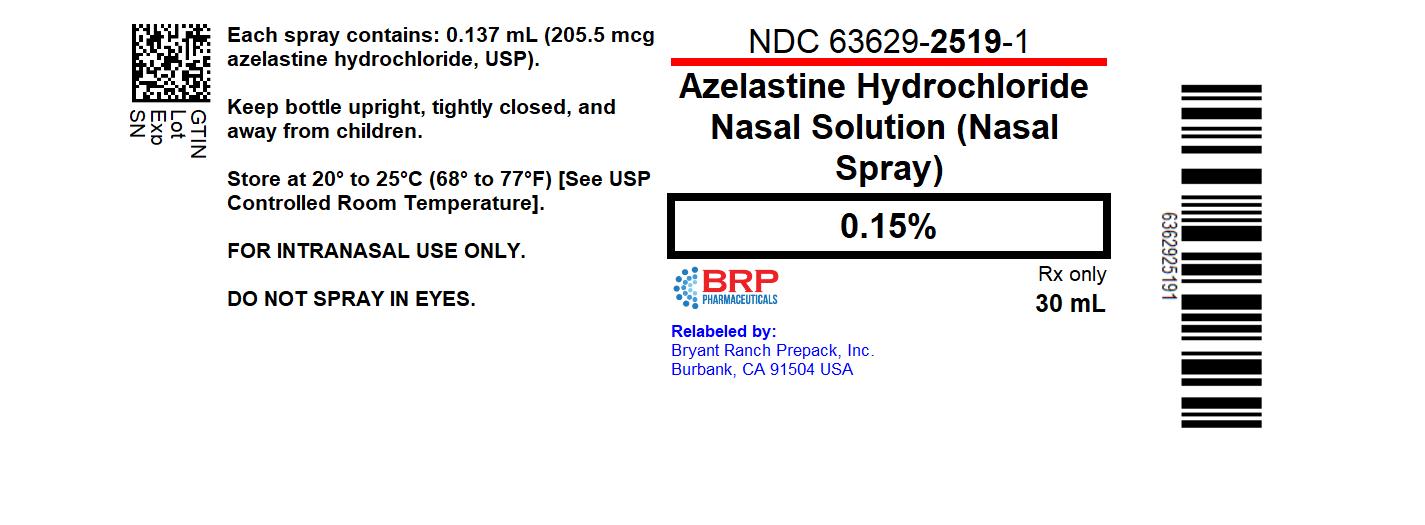
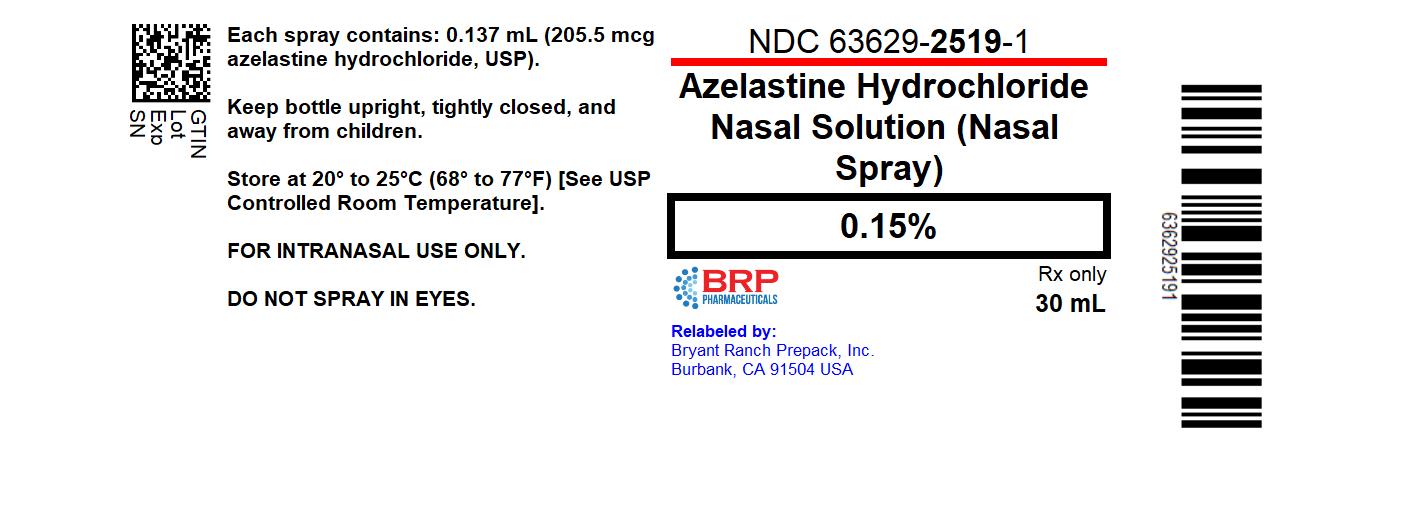
Label: AZELASTINE HCL NASAL- azelastine hcl spray
- NDC Code(s): 63629-2519-1
- Packager: Bryant Ranch Prepack
- This is a repackaged label.
- Source NDC Code(s): 45802-026
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 26, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use AZELASTINE HYDROCHLORIDE NASAL SPRAY safely and effectively. See full prescribing information for AZELASTINE HYDROCHLORIDE NASAL SPRAY.
AZELASTINE HYDROCHLORIDE nasal spray, for intranasal use
Initial U.S. Approval: 1996INDICATIONS AND USAGE
Azelastine HCl nasal spray, 0.15% is an H1-receptor antagonist indicated for the relief of the symptoms of: (1)
- •
- Seasonal allergic rhinitis in patients 6 years of age and older. (1.1)
- •
- Perennial allergic rhinitis in patients 6 years of age and older. (1.1)
DOSAGE AND ADMINISTRATION
- •
- For intranasal use only (2.3).
- •
-
Seasonal allergic rhinitis:
- ▪
- 6 to 11 years: azelastine HCl nasal spray, 0.15%: 1 spray per nostril twice daily (2.1)
- ▪
-
Adults and adolescents 12 years of age and older:
- o
- azelastine HCl nasal spray, 0.15%: 1 or 2 sprays per nostril twice daily (2.1), or
- o
- azelastine HCl nasal spray, 0.15%: 2 sprays per nostril once daily (2.1)
- •
-
Perennial allergic rhinitis:
- ▪
- 6 to 11 years: azelastine HCl nasal spray, 0.15%: 1 spray per nostril twice daily (2.2)
- ▪
- Adults and adolescents 12 years of age and older: azelastine HCl nasal spray, 0.15%: 2 sprays per nostril twice daily (2.2)
- •
- Prime azelastine HCl nasal spray, 0.15% before initial use and when it has not been used for 3 or more days. (2.3)
DOSAGE FORMS AND STRENGTHS
Nasal spray solution available in one dosage strength: (3)
- •
- Azelastine HCl nasal spray, 0.15%: 205.5 mcg of azelastine hydrochloride, USP in each 0.137 mL spray (3).
CONTRAINDICATIONS
None (4)
WARNINGS AND PRECAUTIONS
- •
- Somnolence: Avoid engaging in hazardous occupations requiring complete mental alertness such as driving or operating machinery when taking azelastine HCl nasal spray, 0.15% (5.1)
- •
- Avoid concurrent use of alcohol or other central nervous system (CNS) depressants with azelastine HCl nasal spray, 0.15% because further decreased alertness and impairment of CNS performance may occur (5.1)
ADVERSE REACTIONS
The most common adverse reactions (≥2% incidence) are: pyrexia, dysgeusia, nasal discomfort, epistaxis, headache, sneezing, fatigue, somnolence, upper respiratory infection, cough, rhinalgia, vomiting, otitis media, contact dermatitis, and oropharyngeal pain (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Perrigo at 1-866-634-9120 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Allergic Rhinitis
2 DOSAGE AND ADMINISTRATION
2.1 Seasonal Allergic Rhinitis
2.2 Perennial Allergic Rhinitis
2.3 Important Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Activities Requiring Mental Alertness
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Central Nervous System Depressants
7.2 Erythromycin and Ketoconazole
7.3 Cimetidine
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Seasonal Allergic Rhinitis
14.2 Perennial Allergic Rhinitis
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Seasonal Allergic Rhinitis
Children 6 to 11 years of age: azelastine HCl nasal spray, 0.15%, 1 spray per nostril twice daily.
Adults and adolescents 12 years of age and older: azelastine HCl nasal spray, 0.15%, 1 or 2 sprays per nostril twice daily. Azelastine HCl nasal spray, 0.15% may also be administered as 2 sprays per nostril once daily.
2.2 Perennial Allergic Rhinitis
Children 6 to 11 years of age: azelastine HCl nasal spray, 0.15%, 1 spray per nostril twice daily.
Adults and adolescents 12 years of age and older: azelastine HCl nasal spray, 0.15%, 2 sprays per nostril twice daily.
2.3 Important Administration Instructions
Administer azelastine HCl nasal spray, 0.15% by the intranasal route only.
Priming: Prime azelastine HCl nasal spray, 0.15% before initial use by releasing 6 sprays or until a fine mist appears. When azelastine HCl nasal spray, 0.15% has not been used for 3 or more days, reprime with 2 sprays or until a fine mist appears.
Avoid spraying azelastine HCl nasal spray, 0.15% into the eyes.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Activities Requiring Mental Alertness
In clinical trials, the occurrence of somnolence has been reported in some patients taking azelastine HCl nasal spray [see Adverse Reactions (6.1)]. Patients should be cautioned against engaging in hazardous occupations requiring complete mental alertness and motor coordination such as operating machinery or driving a motor vehicle after administration of azelastine HCl nasal spray, 0.15%.
Concurrent use of azelastine HCl nasal spray, 0.15% with alcohol or other central nervous system depressants should be avoided because additional reductions in alertness and additional impairment of central nervous system performance may occur [see Drug Interactions (7.1)].
-
6 ADVERSE REACTIONS
Use of azelastine HCl nasal spray has been associated with somnolence [see Warnings and Precautions (5.1)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect rates observed in practice.
Children 6 to 11 years of age
In a 4 week clinical trial, 489 patients ages 6 to 11 years with perennial allergic rhinitis, with or without concomitant seasonal allergic rhinitis, were treated with either azelastine HCl nasal spray, 0.1%, azelastine HCl nasal spray, 0.15% or placebo, one spray per nostril twice daily. Overall, adverse events were similar in the azelastine HCl nasal spray, 0.15% group (24%), azelastine HCl nasal spray, 0.1% group (26%) and the placebo group (24%). Overall, less than 1% of the combined azelastine HCl nasal spray groups discontinued due to adverse events.
Table 2 contains adverse reactions reported with frequencies greater than or equal to 2% and more frequently than placebo in children 6 to 11 years of age treated with azelastine HCl nasal spray, 0.1% or azelastine HCl nasal spray, 0.15% in the controlled trial described above.
Table 2. Adverse Reactions Reported in ≥2% Incidence in a Placebo-Controlled Trial of 4 Weeks’
Duration with azelastine HCl nasal spray, 0.1% or azelastine HCl nasal spray, 0.15% in Children 6 to 11 Years of Age with Perennial Allergic Rhinitis
1 spray twice daily
Azelastine HCl nasal spray,
0.1%
(N=166)
Azelastine HCl nasal spray,
0.15%
(N=161)
Vehicle
Placebo
(N=162)
Epistaxis
8 (5%)
7 (4%)
5 (3%)
Nasal Discomfort
1 (<1%)
7 (4%)
0 (0%)
Dysgeusia
4 (2%)
6 (4%)
1 (<1%)
Upper respiratory
infection
4 (2%)
4 (3%)
3 (2%)
Sneezing
3 (2%)
4 (3%)
2 (1%)
Children 6 months to 5 years
In a 4 week clinical trial, 191 patients ages 6 months to 5 years with either seasonal and/or perennial allergic rhinitis were treated with either azelastine HCl nasal spray, 0.1% or azelastine HCl nasal spray, 0.15% one spray per nostril twice daily. The most frequently (≥2%) reported adverse reactions were pyrexia, cough, epistaxis, sneezing, dysgeusia, rhinalgia, upper respiratory infection, vomiting, otitis media, contact dermatitis, and oropharyngeal pain. Overall, adverse events were slightly higher in the azelastine HCl nasal spray, 0.15% group (28%) compared to azelastine HCl nasal spray, 0.1% group (21%). Focused nasal examinations were performed and showed no incidence of nasal mucosal ulceration at any time point during the study. No patients had reports of nasal septal perforation. Overall, less than 3% of the combined azelastine HCl nasal spray groups discontinued due to adverse events.
Azelastine HCl nasal spray, 0.15%
The safety data described below reflect exposure to azelastine HCl nasal spray, 0.15% in 2114 patients (6 months of age and older) with seasonal or perennial allergic rhinitis from 10 clinical trials of 2 weeks to 12 months duration. In 8 double-blind, placebo-controlled clinical trials of 2 to 4 weeks duration, 1703 patients (646 males and 1059 females) with seasonal or perennial allergic rhinitis were treated with azelastine HCl nasal spray, 0.15% one or two sprays per nostril once or twice daily. In the 12 month open-label, active-controlled clinical trial, 466 patients (156 males and 310 females) with perennial allergic rhinitis were treated with azelastine HCl nasal spray, 0.15% two sprays per nostril twice daily. Of these 466 patients, 152 had participated in the 4-week placebo-controlled perennial allergic rhinitis clinical trials. In a 4-week, double-blind, placebo-controlled clinical trial, 161 patients (87 males and 74 females) ages 6 to 11 years of age with perennial allergic rhinitis, with or without concomitant seasonal allergic rhinitis, were treated with azelastine HCl nasal spray, 0.15% one spray per nostril twice daily. In a 4-week clinical trial, 95 patients (59 males and 36 females) ages 6 months to 5 years of age with seasonal and/or perennial allergic rhinitis were treated with azelastine HCl nasal spray, 0.15% one spray per nostril twice daily. The racial distribution for the 10 clinical trials was 79% white, 14% black, 2% Asian, and 5% other.
Adults and Adolescents 12 Years of Age and Older
In the 7 placebo controlled clinical trials of 2 to 4 week duration, 2343 patients with seasonal allergic rhinitis and 540 patients with perennial allergic rhinitis were treated with two sprays per nostril of either azelastine HCl nasal spray, 0.15% or placebo once or twice daily. Overall, adverse reactions were more common in the azelastine HCl nasal spray, 0.15% treatment groups (16-31%) than in the placebo groups (11-24%). Overall, less than 2% of patients discontinued due to adverse reactions and withdrawal due to adverse reactions was similar among the treatment groups.
Table 3 contains adverse reactions reported with frequencies greater than or equal to 2% and more frequently than placebo in patients treated with azelastine HCl nasal spray, 0.15% in the seasonal and perennial allergic rhinitis controlled clinical trials.
Table 3. Adverse Reactions with ≥2% Incidence in Placebo-Controlled Trials of 2 to 4 Weeks’
Duration with azelastine HCl nasal spray, 0.15% in Adult and Adolescent Patients With Seasonal or Perennial Allergic Rhinitis
2 sprays twice daily
2 sprays once daily
Azelastine HCl
nasal spray,
0.15%
(N=523)
Vehicle
Placebo
(N=523)
Azelastine HCl
nasal spray,
0.15%
(N=1021)
Vehicle
Placebo
(N=816)
Bitter Taste
31 (6%)
5 (1%)
38 (4%)
2 (<1%)
Nasal Discomfort
18 (3%)
12 (2%)
37 (4%)
7 (1%)
Epistaxis
5 (1%)
7 (1%)
21 (2%)
14 (2%)
Sneezing
9 (2%)
1 (<1%)
14 (1%)
0 (0%)
In the above trials, somnolence was reported in <1% of patients treated with azelastine HCl nasal spray, 0.15% (11 of 1544) or vehicle placebo (1 of 1339).
Long-Term (12 Month) Safety Trial:
In the 12 month, open-label, active-controlled, long-term safety trial, 466 patients (12 years of age and older) with perennial allergic rhinitis were treated with azelastine HCl nasal spray, 0.15% two sprays per nostril twice daily and 237 patients were treated with mometasone nasal spray two sprays per nostril once daily. The most frequently reported adverse reactions (>5%) with azelastine HCl nasal spray, 0.15% were bitter taste, headache, sinusitis, and epistaxis. Focused nasal examinations were performed and no nasal ulcerations or septal perforations were observed. In each treatment group, approximately 3% of patients had mild epistaxis. No patients had reports of severe epistaxis. Fifty-four patients (12%) treated with azelastine HCl nasal spray, 0.15% and 17 patients (7%) treated with mometasone nasal spray discontinued from the trial due to adverse events.
6.2 Postmarketing Experience
During the post approval use of azelastine HCl nasal spray, the following adverse reactions have been identified. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions reported include: abdominal pain, atrial fibrillation, blurred vision, chest pain, confusion, disturbance or loss of sense of smell and/or taste, dizziness, dyspnea, facial swelling, hypertension, involuntary muscle contractions, nasal burning, nausea, nervousness, palpitations, paresthesia, parosmia, pruritus, rash, sneezing, insomnia, sweet taste, tachycardia, and throat irritation.
Additionally, the following adverse reactions have been identified during the post approval use of the azelastine HCl nasal spray without sweetener brand of azelastine hydrochloride 0.1% nasal spray (total daily dose 0.55 mg to 1.1 mg). Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions reported include the following: anaphylactoid reaction, application site irritation, facial edema, paroxysmal sneezing, tolerance, urinary retention, and xerophthalmia.
-
7 DRUG INTERACTIONS
7.1 Central Nervous System Depressants
Concurrent use of azelastine HCl nasal spray, 0.15% with alcohol or other central nervous system depressants should be avoided because reductions in alertness and impairment of central nervous system performance may occur [see Warnings and Precautions (5.1)].
7.2 Erythromycin and Ketoconazole
Interaction studies investigating the cardiac effects, as measured by the corrected QT interval (QTc), of concomitantly administered oral azelastine hydrochloride and erythromycin or ketoconazole were conducted. Oral erythromycin (500 mg three times daily for 7 days) had no effect on azelastine pharmacokinetics or QTc based on analyses of serial electrocardiograms. Ketoconazole (200 mg twice daily for 7 days) interfered with the measurement of azelastine plasma concentrations on the analytic HPLC; however, no effects on QTc were observed [see Clinical Pharmacology (12.2) and (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited data from postmarketing experience over decades of use with azelastine hydrochloride in pregnant women have not identified any drug associated risks of miscarriage, birth defects, or other adverse maternal or fetal outcomes. In animal reproduction studies, there was no evidence of fetal harm at oral doses approximately 4 times the clinical daily dose. Oral administration of azelastine hydrochloride to pregnant mice, rats, and rabbits, during the period of organogenesis, produced developmental toxicity that included structural abnormalities, decreased embryo-fetal survival, and decreased fetal body weights at doses 180 times and higher than the maximum recommended human daily intranasal dose (MRHDID) of 1.644 mg. However, the relevance of these findings in animals to pregnant women was considered questionable based upon the high animal to human dose multiple.
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Animal Data
In an embryo-fetal development study in mice dosed during the period of organogenesis, azelastine hydrochloride caused embryo-fetal death, structural abnormalities (cleft palate; short or absent tail; fused, absent or branched ribs), delayed ossification, and decreased fetal weight at approximately 200 times the maximum recommended human daily intranasal dose (MRHDID) in adults (on a mg/m2 basis at a maternal oral dose of 68.6 mg/kg/day), which also caused maternal toxicity as evidenced by decreased maternal body weight. Neither fetal nor maternal effects occurred in mice at approximately 9 times the MRHDID in adults (on a mg/m2 basis at a maternal oral dose of 3 mg/kg/day).
In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation days 7 to 17, azelastine hydrochloride caused structural abnormalities (oligo-and brachydactylia), delayed ossification, and skeletal variations, in the absence of maternal toxicity, at approximately 180 times the MRHDID in adults (on a mg/m2 basis at a maternal oral dose of 30 mg/kg/day). Azelastine hydrochloride caused embryo-fetal death and decreased fetal weight and severe maternal toxicity at approximately 410 times the MRHDID (on a mg/m2 basis at a maternal oral dose of 68.6 mg/kg/day). Neither fetal nor maternal effects occurred at approximately 10 times the MRHDID (on a mg/m2 basis at a maternal oral dose of 2 mg/kg/day).
In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6 to 18, azelastine hydrochloride caused abortion, delayed ossification and decreased fetal weight and severe maternal toxicity at approximately 360 times the MRHDID in adults (on a mg/m2 basis at a maternal oral dose of 30 mg/kg/day). Neither fetal nor maternal effects occurred at approximately 4 times the MRHDID (on a mg/m2 basis at a maternal oral dose of 0.3 mg/kg/day).
In a prenatal and postnatal development study in pregnant rats dosed from late in the gestation period and through the lactation period from gestation day 17 through lactation day 21, azelastine hydrochloride produced no adverse developmental effects on pups at maternal doses up to approximately 180 times the MRHDID (on mg/m2 basis at a maternal dose of 30 mg/kg/day.)
8.2 Lactation
Risk Summary
There are no data on the presence of azelastine hydrochloride in human milk, the effects on the breastfed infant, or the effects on milk production following use of azelastine hydrochloride. Because many drugs are excreted in human milk, caution should be exercised when azelastine HCl nasal spray, 0.15% is administered to a nursing woman.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for azelastine HCl nasal spray, 0.15% and any potential adverse effects on the breastfed infant from azelastine HCl nasal spray, 0.15% or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of azelastine HCl nasal spray, 0.15% have been established for seasonal allergic rhinitis in pediatric patients 6 to 17 years of age and perennial allergic rhinitis in pediatric patients 6 to 17 years of age [see Clinical Studies (14)]. The safety and effectiveness of azelastine HCl nasal spray, 0.15% in pediatric patients below 6 years of age have not been established.
8.5 Geriatric Use
Clinical trials of azelastine HCl nasal spray did not include sufficient numbers of patients 65 years of age and older to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
10 OVERDOSAGE
There have been no reported overdosages with azelastine HCl nasal spray. Acute overdosage by adults with this dosage form is unlikely to result in clinically significant adverse events, other than increased somnolence, since one 30-mL bottle of azelastine HCl nasal spray, 0.15% contains up to 45 mg of azelastine hydrochloride. Clinical trials in adults with single doses of the oral formulation of azelastine hydrochloride (up to 16 mg) have not resulted in increased incidence of serious adverse events. General supportive measures should be employed if overdosage occurs. There is no known antidote to azelastine HCl nasal spray. Oral ingestion of antihistamines has the potential to cause serious adverse effects in children. Accordingly, azelastine HCl nasal spray, 0.15% should be kept out of the reach of children.
-
11 DESCRIPTION
Azelastine HCl nasal spray, 0.15% is an antihistamine (H1 receptor antagonist) formulated as a metered-spray solution for intranasal administration.
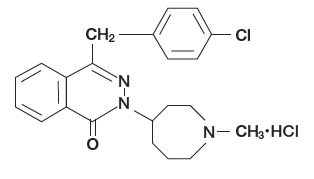
Azelastine hydrochloride, USP occurs as a white, almost odorless, crystalline powder with a bitter taste. It has a molecular weight of 418.37. It is sparingly soluble in water, methanol, and propylene glycol and slightly soluble in ethanol, octanol, and glycerine. It has a melting point of about 225°C and the pH of a saturated solution is between 5.0 and 5.4. Its chemical name is (±)-1-(2H)-phthalazinone,4-[(4-chlorophenyl) methyl]-2-(hexahydro-1-methyl-1H-azepin-4-yl)-, monohydrochloride.
Its molecular formula is C22H24ClN3O•HCl with the following chemical structure:
Azelastine HCl nasal spray, 0.15% contains 0.15% azelastine hydrochloride, USP in an isotonic aqueous solution containing sorbitol, sucralose, hypromellose, sodium citrate, edetate disodium, benzalkonium chloride (125 mcg/mL), and purified water (pH 6.4).
After priming [see Dosage and Administration (2.3)], each metered spray delivers a 0.137 mL mean volume containing 205.5 mcg of azelastine hydrochloride, USP (equivalent to 187.6 mcg of azelastine base). The 30-mL (net weight 30 gm of solution) bottle provides 200 metered sprays.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Azelastine hydrochloride, a phthalazinone derivative, exhibits histamine H1-receptor antagonist activity in isolated tissues, animal models, and humans. Azelastine HCl nasal spray, 0.15% is administered as a racemic mixture with no difference in pharmacologic activity noted between the enantiomers in in vitro studies. The major metabolite, desmethylazelastine, also possesses H1-receptor antagonist activity.
12.2 Pharmacodynamics
Cardiac Effects:
In a placebo-controlled trial (95 patients with allergic rhinitis), there was no evidence of an effect of azelastine hydrochloride nasal spray (2 sprays per nostril twice daily for 56 days) on cardiac repolarization as represented by the corrected QT interval (QTc) of the electrocardiogram. Following multiple dose oral administration of azelastine 4 mg or 8 mg twice daily, the mean change in QTc was 7.2 msec and 3.6 msec, respectively.
Interaction studies investigating the cardiac repolarization effects of concomitantly administered oral azelastine hydrochloride and erythromycin or ketoconazole were conducted. Oral erythromycin had no effect on azelastine pharmacokinetics or QTc based on analysis of serial electrocardiograms. Ketoconazole interfered with the measurement of azelastine plasma levels; however, no effects on QTc were observed [see Drug Interactions (7.2)].
12.3 Pharmacokinetics
Absorption:
After intranasal administration of 2 sprays per nostril (822 mcg total dose) of azelastine HCl nasal spray, 0.15%, the mean azelastine peak plasma concentration (Cmax) is 409 pg/mL, the mean extent of systemic exposure (AUC) is 9312 pg•hr/mL and the median time to reach Cmax (tmax) is 4 hours. The systemic bioavailability of azelastine hydrochloride is approximately 40% after intranasal administration.
Distribution:
Based on intravenous and oral administration, the steady-state volume of distribution of azelastine is 14.5 L/kg. In vitro studies with human plasma indicate that the plasma protein binding of azelastine and its metabolite, desmethylazelastine, are approximately 88% and 97%, respectively.
Metabolism:
Azelastine is oxidatively metabolized to the principal active metabolite, desmethylazelastine, by the cytochrome P450 enzyme system. The specific P450 isoforms responsible for the biotransformation of azelastine have not been identified. After a single-dose, intranasal administration of azelastine HCl nasal spray, 0.15% (822 mcg total dose), the mean desmethylazelastine Cmax is 38 pg/mL, the AUC is 3824 pg•hr/mL and the median tmax is 24 hours. After intranasal dosing of azelastine to steady-state, plasma concentrations of desmethylazelastine range from 20-50% of azelastine concentrations.
Elimination:
Following intranasal administration of azelastine HCl nasal spray, 0.15%, the elimination half-life of azelastine is 25 hours while that of desmethylazelastine is 57 hours. Approximately 75% of an oral dose of radiolabeled azelastine hydrochloride was excreted in the feces with less than 10% as unchanged azelastine.
Special Populations:
Hepatic Impairment: Following oral administration, pharmacokinetic parameters were not influenced by hepatic impairment.
Renal Impairment: Based on oral, single-dose studies, renal insufficiency (creatinine clearance <50 mL/min) resulted in a 70-75% higher Cmax and AUC compared to healthy subjects. Time to maximum concentration was unchanged.
Age: Following oral administration, pharmacokinetic parameters were not influenced by age.
Gender: Following oral administration, pharmacokinetic parameters were not influenced by gender.
Race: The effect of race has not been evaluated.
Drug-Drug Interactions:
Erythromycin: Co-administration of orally administered azelastine (4 mg twice daily) with erythromycin (500 mg three times daily for 7 days) resulted in Cmax of 5.36 ± 2.6 ng/mL and AUC of 49.7 ± 24 ng•h/mL for azelastine, whereas, administration of azelastine alone resulted in Cmax of 5.57 ± 2.7 ng/mL and AUC of 48.4 ± 24 ng•h/mL for azelastine [see Drug Interactions (7.2)].
Cimetidine and Ranitidine: In a multiple-dose, steady-state drug interaction trial in healthy subjects, cimetidine (400 mg twice daily) increased orally administered mean azelastine (4 mg twice daily) concentrations by approximately 65%. Co-administration of orally administered azelastine (4 mg twice daily) with ranitidine hydrochloride (150 mg twice daily) resulted in Cmax of 8.89 ±3.28 ng/mL and AUC of 88.22 ± 40.43 ng•h/mL for azelastine, whereas, administration of azelastine alone resulted in Cmax of 7.83 ± 4.06 ng/mL and AUC of 80.09 ± 43.55 ng•h/mL for azelastine [see Drug Interactions (7.3)].
Theophylline: No significant pharmacokinetic interaction was observed with the co-administration of an oral 4 mg dose of azelastine hydrochloride twice daily and theophylline 300 mg or 400 mg twice daily.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies in Crl:CD(SD)BR rats and NMRI mice were conducted to assess the carcinogenic potential of azelastine hydrochloride. No evidence of tumorigenicity was observed in rats at doses up to 30 mg/kg day (approximately 180 and 160 times the MRHDID for adults and children, respectively, on a mg/m2 basis). No evidence for tumorigenicity was observed in mice at doses up to 25 mg/kg (approximately 75 and 65 times the MRHDID for adults and children, respectively, on a mg/m2 basis).
Azelastine hydrochloride showed no genotoxic effects in the Ames test, DNA repair test, mouse lymphoma forward mutation assay, mouse micronucleus test, or chromosomal aberration test in rat bone marrow.
There were no effects on male or female fertility and reproductive performance in male and female rats at oral doses up to 30 mg/kg (approximately 180 times the MRHDID in adults on a mg/m2 basis). At 68.6 mg/kg (approximately 410 times the MRHDID on a mg/m2 basis), the duration of estrous cycles was prolonged and copulatory activity and the number of pregnancies were decreased. The numbers of corpora lutea and implantations were decreased; however, pre-implantation loss was not increased.
-
14 CLINICAL STUDIES
14.1 Seasonal Allergic Rhinitis
Azelastine HCl nasal spray, 0.15%
The efficacy and safety of azelastine HCl nasal spray, 0.15% in seasonal allergic rhinitis was evaluated in five randomized, multicenter, double-blind, placebo-controlled clinical trials in 2499 adult and adolescent patients 12 years and older with symptoms of seasonal allergic rhinitis (Trials 2, 3, 4, 5, and 6). The population of the trials was 12 to 83 years of age (64% female, 36% male; 81% white, 12% black, <2% Asian, 5% other; 23% Hispanic, 77% non-Hispanic). Assessment of efficacy was based on the rTNSS, iTNSS as described above, and other supportive secondary efficacy variables. The primary efficacy endpoint was the mean change from baseline in rTNSS over 2 weeks.
Two 2-week seasonal allergic rhinitis trials evaluated the efficacy of azelastine HCl nasal spray, 0.15% dosed at 2 sprays twice daily. The first trial (Trial 2) compared the efficacy of azelastine HCl nasal spray, 0.15% and azelastine HCl nasal spray without sweetener to vehicle placebo. The other trial (Trial 3) compared the efficacy of azelastine HCl nasal spray, 0.15% and azelastine HCl nasal spray, 0.1% to vehicle placebo. In these two trials, azelastine HCl nasal spray, 0.15% demonstrated greater decreases in rTNSS than placebo and the differences were statistically significant (Table 4).
Three 2-week seasonal allergic rhinitis trials evaluated the efficacy of azelastine HCl nasal spray, 0.15% dosed at 2 sprays once daily compared to the vehicle placebo. Trial 4 demonstrated a greater decrease in rTNSS than placebo and the difference was statistically significant (Table 4). Trial 5 and Trial 6 were conducted in patients with Texas mountain cedar allergy. In Trial 5 and Trial 6, azelastine HCl nasal spray, 0.15% demonstrated a greater decrease in rTNSS than placebo and the differences were statistically significant (Trials 5 and 6; Table 4). Instantaneous TNSS results for the once daily dosing regimen of azelastine HCl nasal spray, 0.15% are shown in Table 5. In Trials 5 and 6, azelastine HCl nasal spray, 0.15% demonstrated a greater decrease in iTNSS than placebo and the differences were statistically significant.
Table 4. Mean Change from Baseline in Reflective TNSS over 2 Weeks*
in Adults and Children ≥ 12 years with Seasonal Allergic Rhinitis
Treatment
(sprays per nostril)
n
Baseline
LS
Mean
Change
from
Baseline
Difference From Placebo
LS
Mean
95% CI
P
value
Trial 2
Two sprays twice daily
Azelastine HCl nasal spray, 0.15%
153
18.2
-4.3
-1.2
-2.1, -0.3
0.01
Azelastine HCl nasal spray without sweetener
153
17.9
-3.9
-0.9
-1.8, 0.1
0.07
Vehicle Placebo
153
18.1
-3.0
Trial 3
Two sprays twice daily
Azelastine HCl nasal spray, 0.15%
177
17.7
-5.1
-3.0
-3.9, -2.1
<0.001
Azelastine HCl nasal spray, 0.1%
169
18.2
-4.2
-2.1
-3.0, -1.2
<0.001
Vehicle Placebo
177
17.7
-2.1
Trial 4
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
238
17.4
-3.4
-1.0
-1.7, -0.3
0.008
Vehicle Placebo
242
17.4
-2.4
Trial 5
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
266
18.5
-3.3
-1.4
-2.1, -0.8
<0.001
Vehicle Placebo
266
18.0
-1.9
Trial 6
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
251
18.5
-3.4
-1.4
-2.1, -0.7
<0.001
Vehicle Placebo
254
18.8
-2.0
*Sum of AM and PM rTNSS for each day (Maximum score=24) and averaged over the 14 day treatment period
Table 5. Mean Change from Baseline AM Instantaneous TNSS over 2 Weeks*
in Adults and Children ≥ 12 years with Seasonal Allergic Rhinitis
Treatment
(sprays per nostril once daily)
n
Baseline
LS
Mean
Change
from
Baseline
Difference From Placebo
LS
Mean
95% CI
P
value
Trial 4
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
238
8.1
-1.3
-0.2
-0.6, 0.1
0.15
Vehicle Placebo
242
8.3
-1.1
Trial 5
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
266
8.7
-1.4
-0.7
-1.0, -0.4
<0.001
Vehicle Placebo
266
8.3
-0.7
Trial 6
Two sprays once daily
Azelastine HCl nasal spray, 0.15%
251
8.9
-1.4
-0.6
-0.9, -0.3
<0.001
Vehicle Placebo
254
8.9
-0.8
*AM iTNSS for each day (Maximum score=12) and averaged over the 14 day treatment period
Azelastine HCl nasal spray, 0.15% at a dose of 1 spray twice daily was not studied. The azelastine HCl nasal spray, 0.15% 1 spray twice daily dosing regimen is supported by previous findings of efficacy for azelastine HCl nasal spray without sweetener and a favorable comparison of azelastine HCl nasal spray, 0.15% to azelastine HCl nasal spray without sweetener and azelastine HCl nasal spray, 0.1% (Table 4).
The efficacy and safety of azelastine HCl nasal spray, 0.15% in children 6 to 11 years of age with seasonal allergic rhinitis was evaluated in a clinical study that enrolled pediatric patients with perennial allergic rhinitis, with or without concomitant seasonal allergic rhinitis (described below in Section 14.2).
14.2 Perennial Allergic Rhinitis
Azelastine HCl nasal spray, 0.15%
The efficacy and safety of azelastine HCl nasal spray, 0.15% in perennial allergic rhinitis was evaluated in one randomized, multicenter, double-blind, placebo-controlled clinical trial in 578 adult and adolescent patients 12 years and older with symptoms of perennial allergic rhinitis. The population of the trial was 12 to 84 years of age (68% female, 32% male; 85% white, 11% black, 1% Asian, 3% other; 17% Hispanic, 83% non-Hispanic).
Assessment of efficacy was based on the 12-hour reflective total nasal symptom score (rTNSS) assessed daily in the morning and evening, the instantaneous total nasal symptom score (iTNSS), and other supportive secondary efficacy variables. The primary efficacy endpoint was the mean change from baseline rTNSS over 4 weeks. The one 4-week perennial allergic rhinitis trial evaluated the efficacy of azelastine HCl nasal spray, 0.15%, azelastine HCl nasal spray, 0.1%, and vehicle placebo dosed at 2 sprays per nostril twice daily. In this trial, azelastine HCl nasal spray, 0.15% demonstrated a greater decrease in rTNSS than placebo and the difference was statistically significant (Table 6).
Table 6. Mean Change from Baseline in Reflective TNSS over 4 Weeks*
in Adults and Children ≥ 12 years with Perennial Allergic Rhinitis
Treatment
(sprays per nostril twice daily)
n
Baseline
LS
Mean
Change
from
Baseline
Difference From Placebo
LS
Mean
95% CI
P
value
Two sprays twice daily
Azelastine HCl nasal spray, 0.15%
192
15.8
-4.0
-0.9
-1.7, -0.1
0.03
Azelastine HCl nasal spray, 0.1%
194
15.5
-3.8
-0.7
-1.5, 0.1
0.08
Vehicle Placebo
192
14.7
-3.1
*Sum of AM and PM rTNSS for each day (Maximum score=24) and averaged over the 28 day treatment period
The efficacy and safety of azelastine HCl nasal spray, 0.1% and azelastine HCl nasal spray, 0.15% in pediatric patients 6 to 11 years of age with perennial allergic rhinitis, with or without concomitant seasonal allergic rhinitis, was evaluated in a randomized, double-blind, placebo-controlled clinical trial in 486 patients. All patients received one spray per nostril twice daily. The study population was 58% males and 42% females; 78% white, 13% black, 3% Asian, and 6% other.
Assessment of efficacy was based on the 12-hour reflective total nasal symptom score (rTNSS) assessed daily in the morning and evening. The primary efficacy endpoint was the mean change from baseline rTNSS over 4 weeks (Table 7). Both active treatments demonstrated statistically significant decreases in rTNSS compared to placebo. There was no statistically significant difference between the two active-treatment groups. There was also no difference in treatment effect between patients with perennial allergic rhinitis only compared to those with perennial allergic rhinitis and concomitant seasonal allergic rhinitis.
Table 7. Mean Change from Baseline in Reflective TNSS over 4 Weeks*
in Children 6 to 11 years with Perennial Allergic Rhinitis
Treatment
(sprays per nostril twice daily)
n
Baseline
LS
Mean
Change
from
Baseline
Difference From Placebo
LS
Mean
95% CI
P
value
One spray twice daily
Azelastine HCl nasal spray, 0.15%
159
16.6
-3.5
-1.0
-1.7, -0.3
0.005
Azelastine HCl nasal spray, 0.1%
166
16.4
-3.4
-0.9
-1.6, -0.2
0.015
Vehicle Placebo
161
16.1
-2.5
*Sum of AM and PM rTNSS for each day (Maximum score=24) and averaged over the 28 day treatment period
The efficacy of azelastine HCl nasal spray, 0.1% and azelastine HCl nasal spray, 0.15% in children 6 months to 5 years of age with allergic rhinitis was explored in a clinical study (described above in Section 14.1).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Azelastine HCl nasal spray, 0.15% is supplied as a 30-mL package (NDC 63629-2519-1) delivering 200 metered sprays in a high-density polyethylene (HDPE) bottle fitted with a metered-dose spray pump unit. The spray pump unit consists of a nasal spray pump fitted with a violet safety clip and a violet plastic dust cover. The net content of the bottle is 30 mL (net weight 30 gm of solution). The 30-mL bottle contains 45 mg (1.5 mg/mL) of azelastine hydrochloride, USP. After priming [see Dosage and Administration (2.3)], each spray delivers a fine mist containing a mean volume of 0.137 mL solution containing 205.5 mcg of azelastine hydrochloride, USP. The correct amount of medication in each spray cannot be assured before the initial priming and after 200 sprays for the 30-mL bottle have been used, even though the bottle is not completely empty. The bottle should be discarded after 200 sprays have been used.
Azelastine HCl nasal spray, 0.15% should not be used after the expiration date “EXP” printed on the medicine label and carton.
Storage:
Store upright at controlled room temperature 20° to 25°C (68° to 77°F). Protect from freezing.
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information and Instructions for Use).
Activities Requiring Mental Alertness
Somnolence has been reported in some patients taking azelastine HCl nasal spray.
Caution patients against engaging in hazardous occupations requiring complete mental alertness and motor coordination such as driving or operating machinery after administration of azelastine HCl nasal spray, 0.15% [see Warnings and Precautions (5.1)].
Concurrent Use of Alcohol and other Central Nervous System Depressants
Avoid concurrent use of azelastine HCl nasal spray, 0.15% with alcohol or other central nervous system depressants because additional reductions in alertness and additional impairment of central nervous system performance may occur [see Warnings and Precautions (5.1)].
Common Adverse Reactions
Inform patients that the treatment with azelastine HCl nasal spray, 0.15% may lead to adverse reactions, most common of which include pyrexia, dysgeusia, nasal discomfort, epistaxis, headache, sneezing, fatigue, somnolence, upper respiratory infection, cough, rhinalgia, vomiting, otitis media, contact dermatitis, and oropharyngeal pain. [see Adverse Reactions (6.1)].
Priming
Instruct patients to prime the pump before initial use and when azelastine HCl nasal spray, 0.15% has not been used for 3 or more days [see Dosage and Administration (2.3)].
Keep Spray Out of Eyes
Instruct patients to avoid spraying azelastine HCl nasal spray, 0.15% into their eyes.
Keep Out of Children’s Reach
Instruct patients to keep azelastine HCl nasal spray, 0.15% out of the reach of children. If a child accidentally ingests azelastine HCl nasal spray, 0.15% seek medical help or call a poison control center immediately.
- SPL UNCLASSIFIED SECTION
-
PATIENT INFORMATION
Azelastine (a-ZEL-uh-steen) HCl nasal spray, 0.15%
What is azelastine HCl nasal spray?
- •
- Azelastine HCl nasal spray is a prescription medicine used to treat symptoms of seasonal allergic rhinitis in patients 6 years of age and older and year-round allergic rhinitis in people age 6 years and older.
- •
- Azelastine HCl nasal spray may help to reduce your nasal symptoms including stuffy nose, runny nose, itching and sneezing.
It is not known if azelastine HCl nasal spray is safe and effective in children under 6 years of age.
What should I tell my healthcare provider before using azelastine HCl nasal spray?
Before using azelastine HCl nasal spray, tell your healthcare provider if you are:
- •
- allergic to any of the ingredients in azelastine HCl nasal spray. See the end of this leaflet for a complete list of ingredients in azelastine HCl nasal spray.
- •
- pregnant, or plan to become pregnant.
- •
- breastfeeding, or plan to breastfeed. It is not known if azelastine HCl nasal spray passes into your breast milk. You and your healthcare provider should decide if you will use azelastine HCl nasal spray if you plan to breastfeed.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Azelastine HCl nasal spray and other medicines may affect each other, causing side effects.
How should I use azelastine HCl nasal spray?
- •
- Read the Instructions for Use at the end of this leaflet for information about the right way to use azelastine HCl nasal spray.
- •
- An adult should help a young child use azelastine HCl nasal spray.
- •
- Spray azelastine HCl nasal spray in your nose only. Do not spray it into your eyes or mouth.
- •
- Use azelastine HCl nasal spray exactly as your healthcare provider tells you to use it.
- •
- Do not use more than your healthcare provider tells you.
- •
- Throw away your azelastine HCl nasal spray bottle after using 200 sprays. Even though the bottle may not be completely empty, you may not get the correct dose of medicine.
- •
- If you use too much or a child accidentally swallows azelastine HCl nasal spray, call your healthcare provider or go to the nearest hospital emergency room right away.
What should I avoid while using azelastine HCl nasal spray?
Azelastine HCl nasal spray can cause sleepiness:
- •
- Do not drive, operate machinery, or do other dangerous activities until you know how azelastine HCl nasal spray affects you.
- •
- Do not drink alcohol or take other medicines that may cause you to feel sleepy while using azelastine HCl nasal spray. It may make your sleepiness worse.
What are the possible side effects of azelastine HCl nasal spray?
The most common side effects of azelastine HCl nasal spray include:
- •
- fever
- •
- unusual taste
- •
- nose pain or discomfort
- •
- nosebleeds
- •
- headache
- •
- sneezing
- •
- fatigue
- •
- sleepiness
- •
- upper respiratory tract infections
- •
- cough
- •
- vomiting
- •
- middle ear infection
- •
- skin rash
- •
- sore throat
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of azelastine HCl nasal spray.
For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store azelastine HCl nasal spray?
- •
- Keep azelastine HCl nasal spray upright at 68°F to 77°F (20°C to 25°C).
- •
- Do not freeze azelastine HCl nasal spray.
- •
- Do not use azelastine HCl nasal spray after the expiration date “EXP” on the medicine label and box.
Keep azelastine HCl nasal spray and all medicines out of reach of children.
General information about the safe and effective use of azelastine HCl nasal spray.
Medicines are sometimes prescribed for conditions other than those listed in a Patient Information leaflet.
Do not use azelastine HCl nasal spray for a condition for which it was not prescribed. Do not give azelastine HCl nasal spray to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about azelastine HCl nasal spray. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about azelastine HCl nasal spray that is written for health professionals.
For more information, go to www.perrigorx.com or call 1-866-634-9120.
What are the ingredients in azelastine HCl nasal spray?
Active ingredient: azelastine hydrochloride, USP
Inactive ingredients: sorbitol, sucralose, hypromellose, sodium citrate, edetate disodium, benzalkonium chloride, and purified water.
-
INSTRUCTIONS FOR USE
Azelastine (a-ZEL-uh-steen) HCl nasal spray, 0.15%
Important: For use in your nose only.
For the correct dose of medicine:
- •
- Keep your head tilted downward when spraying into your nostril.
- •
- Change nostrils each time you use the spray.
- •
- Breathe gently and do not tip your head back after using the spray. This will keep the medicine from running down into your throat. You may get a bitter taste in your mouth.
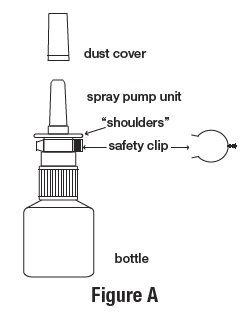
Figure A identifies the parts of your azelastine HCl nasal spray pump
Before you use azelastine HCl nasal spray for the first time, you will need to prime the bottle.
For use in young children: An adult should help a young child use azelastine HCl nasal spray. (See “Using your azelastine HCl nasal spray” Steps 1 through 8).
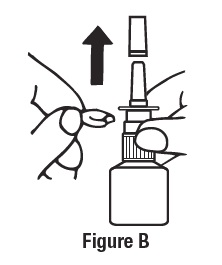
Priming your azelastine HCl nasal spray
Remove the violet dust cover over the tip of the bottle and the violet safety clip just under the “shoulders” of the bottle. (See Figure B).
- •
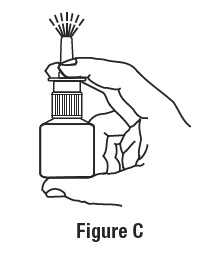
- Hold the bottle upright with 2 fingers on the shoulders of the spray pump unit and put your thumb on the bottom of the bottle. Press upward with your thumb and release for the pumping action. Repeat this until you see a fine mist. (See Figure C).
- •
- To get a fine mist you must pump the spray fast and use firm pressure against the bottom of the bottle. If you see a stream of liquid, the pump is not working correctly and you may have nasal discomfort.
- •
- This should happen in 6 sprays or less.
Now your pump is primed and ready to use.
- •
- Do not use azelastine HCl nasal spray unless you see a fine mist after you do the priming sprays. If you do not see a fine mist, clean the tip of the spray nozzle. See the “Cleaning the Spray Tip of your azelastine HCl nasal spray” section below.
- •
- If you do not use azelastine HCl nasal spray for 3 or more days, you will need to prime the pump with 2 sprays or until you see a fine mist.
Using your azelastine HCl nasal spray
For use in young children: An adult should help a young child use azelastine HCl nasal spray. (See Steps 1 through 8).
- Step 1. Blow your nose to clear your nostrils.
- Step 2. Keep your head tilted downward toward your toes.
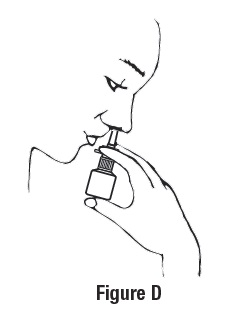
- Step 3. Place the spray tip about ¼ inch to ½ inch into 1 nostril.
- Hold bottle upright and aim the spray tip toward the back of your nose (See Figure D).
- Step 4. Close your other nostril with a finger. Press the pump 1 time and sniff gently at the same time, keeping your head tilted forward and down (See Figure E).
- Step 5. Repeat Step 3 and Step 4 in your other nostril.
- Step 6. If your healthcare provider tells you to use 2 sprays in each nostril, repeat Steps 2 through 4 above for the second spray in each nostril.
- Step 7. Breathe in gently, and do not tilt your head back after using azelastine HCl nasal spray. This will help to keep the medicine from going into your throat.
- Step 8. When you finish using your azelastine HCl nasal spray, wipe the spray tip with a clean tissue or cloth. Put the safety clip and dust cover back on the bottle.
- Cleaning the Spray Tip of your azelastine HCl nasal spray
- •
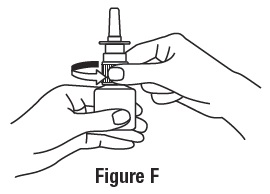
- If the spray tip opening is clogged, do not use a pin or pointed object to unclog the tip. Unscrew the spray pump unit from the bottle by turning it to the left (counter-clockwise) (See Figure F).
- •
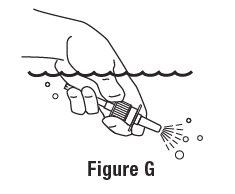
- Soak only the spray pump unit in warm water. Squirt the spray unit several times while holding it under water. Use the pumping action to clear the opening in the tip (See Figure G).
- •
- Let the spray pump unit air dry. Make sure it is dry before you put it back onto the bottle.
- •
- Put the spray pump unit back into the open bottle and tighten it by turning clockwise (to the right).
- •
- To keep the medicine from leaking out, use firm pressure when you put the pump back onto the bottle.
- •
- After cleaning, follow the instructions for priming.
This Patient Information and Instructions for Use has been approved by the U.S. Food and Drug Administration.
Made in Israel
Manufactured by Perrigo
Yeruham, Israel
Distributed By
Perrigo®
Allegan, MI 49010 • www.perrigorx.com
Rev 11-20
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
AZELASTINE HCL NASAL
azelastine hcl sprayProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63629-2519(NDC:45802-026) Route of Administration NASAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AZELASTINE HYDROCHLORIDE (UNII: 0L591QR10I) (AZELASTINE - UNII:ZQI909440X) AZELASTINE HYDROCHLORIDE 205.5 ug Inactive Ingredients Ingredient Name Strength SORBITOL (UNII: 506T60A25R) SUCRALOSE (UNII: 96K6UQ3ZD4) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) SODIUM CITRATE, UNSPECIFIED FORM (UNII: 1Q73Q2JULR) EDETATE DISODIUM (UNII: 7FLD91C86K) BENZALKONIUM CHLORIDE (UNII: F5UM2KM3W7) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63629-2519-1 1 in 1 CARTON 05/09/2014 1 200 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202743 05/09/2014 Labeler - Bryant Ranch Prepack (171714327) Registrant - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(63629-2519) , RELABEL(63629-2519)