Label: VAXELIS- diphtheria and tetanus toxoids and acellular pertussis, inactivated poliovirus, haemophilus b conjugate and hepatitis b vaccine injection, suspension
- NDC Code(s): 63361-243-10, 63361-243-15, 63361-243-58, 63361-243-88
- Packager: MSP Vaccine Company
- Category: VACCINE LABEL
Drug Label Information
Updated October 19, 2022
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VAXELIS safely and effectively. See full prescribing information for VAXELIS.
VAXELIS® (Diphtheria and Tetanus Toxoids and Acellular Pertussis, Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B Vaccine)
Suspension for Intramuscular Injection
Initial U.S. Approval: 2018INDICATIONS AND USAGE
VAXELIS is a vaccine indicated for active immunization to prevent diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease due to Haemophilus influenzae type b. VAXELIS is approved for use as a 3-dose series in children from 6 weeks through 4 years of age (prior to the 5th birthday). (1)
DOSAGE AND ADMINISTRATION
The 3-dose immunization series consists of a 0.5 mL intramuscular injection, administered at 2, 4, and 6 months of age. (2.1)
DOSAGE FORMS AND STRENGTHS
Suspension for injection (0.5 mL dose) available in single-dose vials and prefilled syringes. (3)
CONTRAINDICATIONS
- Severe allergic reaction (e.g., anaphylaxis) to a previous dose of VAXELIS, any ingredient of VAXELIS, or any other diphtheria toxoid, tetanus toxoid, pertussis-containing vaccine, inactivated poliovirus vaccine, hepatitis B vaccine, or Haemophilus influenzae type b vaccine. (4.1)
- Encephalopathy within 7 days of a previous pertussis-containing vaccine with no other identifiable cause. (4.2)
- Progressive neurologic disorder until a treatment regimen has been established and the condition has stabilized. (4.3)
WARNINGS AND PRECAUTIONS
- Carefully consider benefits and risks before administering VAXELIS to persons with a history of:
- If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome may be increased following VAXELIS. (5.3)
- Apnea following intramuscular vaccination has been observed in some infants born prematurely. The decision about when to administer an intramuscular vaccine, including VAXELIS, to an infant born prematurely should be based on consideration of the individual infant's medical status and the potential benefits and possible risks of vaccination. (5.5)
- Urine antigen detection may not have definitive diagnostic value in suspected H. influenzae type b disease following vaccination with VAXELIS. (5.7) (7.1)
ADVERSE REACTIONS
The solicited adverse reactions following any dose were irritability (≥55%), crying (≥45%), injection site pain (≥44%), somnolence (≥40%), injection site erythema (≥25%), decreased appetite (≥23%), fever ≥38.0°C (≥19%), injection site swelling (≥18%), and vomiting (≥9%). (6)
To report SUSPECTED ADVERSE REACTIONS, contact Sanofi Pasteur Inc., at 1-800-822-2463 (1-800-VACCINE) or VAERS at 1-800-822-7967 and http://vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Vaccination Schedule
2.2 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Encephalopathy
4.3 Progressive Neurologic Disorder
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
5.2 Adverse Reactions Following Prior Pertussis Vaccination
5.3 Guillain-Barré Syndrome and Brachial Neuritis
5.4 Altered Immunocompetence
5.5 Apnea in Premature Infants
5.6 Limitations of Vaccine Effectiveness
5.7 Interference with Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Interference with Laboratory Tests
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Effectiveness of VAXELIS
14.2 Immunogenicity
14.3 Concomitantly Administered Vaccines
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
VAXELIS® is a vaccine indicated for active immunization to prevent diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease due to Haemophilus influenzae (H. influenzae) type b. VAXELIS is approved for use as a 3-dose series in children 6 weeks through 4 years of age (prior to the 5th birthday).
-
2 DOSAGE AND ADMINISTRATION
For intramuscular use only.
2.1 Vaccination Schedule
VAXELIS is to be administered as a 3-dose series at 2, 4, and 6 months of age. The first dose may be given as early as 6 weeks of age. Three doses of VAXELIS constitute a primary immunization course against diphtheria, tetanus, H. influenzae type b invasive disease and poliomyelitis.
VAXELIS may be used to complete the hepatitis B immunization series.
A 3-dose series of VAXELIS does not constitute a primary immunization series against pertussis; an additional dose of pertussis-containing vaccine is needed to complete the primary series. [See Pertussis Vaccination Following VAXELIS.]
Pertussis Vaccination following VAXELIS
VAXELIS, Pentacel® [(Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Inactivated Poliovirus and Haemophilus b Conjugate (Tetanus Toxoid Conjugate) Vaccine): DTaP-IPV/Hib], Quadracel® [(Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed and Inactivated Poliovirus Vaccine): DTaP-IPV] and DAPTACEL® [(Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed): DTaP] contain the same pertussis antigens manufactured by the same process. Children who have received a 3-dose series of VAXELIS should complete the primary and pertussis vaccination series with Pentacel, Quadracel or DAPTACEL according to the respective prescribing information in the approved package inserts. [See ADVERSE REACTIONS (6.1) AND CLINICAL STUDIES (14).]
Administration of VAXELIS following previous doses of other DTaP-containing Vaccines
VAXELIS may be used to complete the first 3 doses of the 5-dose DTaP series in infants and children who have received 1 or 2 doses of Pentacel or DAPTACEL and are also scheduled to receive the other antigens in VAXELIS. Data are not available on the safety and immunogenicity of such mixed sequences.
Data are not available on the safety and effectiveness of using VAXELIS following 1 or 2 doses of a DTaP vaccine from a different manufacturer.
Administration of VAXELIS following previous doses of any Hepatitis B Vaccine
A 3-dose series of VAXELIS may be administered to infants born to HBsAg-negative mothers, and who have received a dose of any hepatitis B vaccine, prior to or at 1 month of age. [See ADVERSE REACTIONS (6.1) AND CLINICAL STUDIES (14).]
VAXELIS may be used to complete the hepatitis B vaccination series following 1 or 2 doses of other hepatitis B vaccines, in infants and children born of HBsAg-negative mothers and who are also scheduled to receive the other antigens in VAXELIS. However, data are not available on the safety and effectiveness of VAXELIS in such infants and children.
Administration of VAXELIS following previous doses of Inactivated Polio Vaccine (IPV)
VAXELIS may be administered to infants and children who have received 1 or 2 doses of IPV and are also scheduled to receive the other antigens in VAXELIS. However, data are not available on the safety and effectiveness of VAXELIS in such infants and children.
Administration of VAXELIS following previous doses of Haemophilus b Conjugate Vaccines
VAXELIS may be administered to infants and children who have received 1 or 2 doses of H. influenzae type b Conjugate Vaccine and are also scheduled to receive the other antigens in VAXELIS. However, data are not available on the safety and effectiveness of VAXELIS in such infants and children.
2.2 Administration
Just before use, shake the vial or syringe until a uniform, white, cloudy suspension results.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If either of these conditions exist, the product should not be administered.
Administer a single 0.5 mL dose of VAXELIS intramuscularly.
In infants younger than 1 year, the anterolateral aspect of the thigh is the preferred site of injection. The vaccine should not be injected into the gluteal area.
VAXELIS should not be combined through reconstitution or mixed with any other vaccine. Discard unused portion.
-
3 DOSAGE FORMS AND STRENGTHS
VAXELIS is a suspension for injection available in 0.5 mL single-dose vials and prefilled syringes. [See HOW SUPPLIED/STORAGE AND HANDLING (16).]
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Do not administer VAXELIS to anyone with a history of a severe allergic reaction (e.g., anaphylaxis) to a previous dose of VAXELIS, any ingredient of VAXELIS, or any other diphtheria toxoid, tetanus toxoid, pertussis-containing vaccine, inactivated poliovirus vaccine, hepatitis B vaccine, or H. influenzae type b vaccine [See DESCRIPTION (11).]
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Epinephrine hydrochloride solution (1:1,000) and other appropriate agents and equipment must be available for immediate use in case an anaphylactic or acute hypersensitivity reaction occurs.
5.2 Adverse Reactions Following Prior Pertussis Vaccination
If any of the following events occur after administration of a pertussis vaccine, the decision to administer VAXELIS should be based on careful consideration of potential benefits and possible risks.
- Temperature of ≥40.5°C (≥105°F) within 48 hours, not attributable to another identifiable cause.
- Collapse or shock-like state (hypotonic-hyporesponsive episode [HHE]) within 48 hours.
- Persistent, inconsolable crying lasting ≥3 hours within 48 hours.
- Seizures with or without fever within 3 days.
5.3 Guillain-Barré Syndrome and Brachial Neuritis
A review by the Institute of Medicine (IOM) found evidence for a causal relation between tetanus toxoid and both brachial neuritis and Guillain-Barré syndrome. If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome may be increased following VAXELIS. (1)
5.4 Altered Immunocompetence
If VAXELIS is administered to immunocompromised persons, including persons receiving immunosuppressive therapy, the expected immune response may not be obtained.
5.5 Apnea in Premature Infants
Apnea following intramuscular vaccination has been observed in some infants born prematurely. The decision about when to administer an intramuscular vaccine, including VAXELIS, to an infant born prematurely should be based on consideration of the infant's medical status and the potential benefits and possible risks of vaccination.
5.7 Interference with Laboratory Tests
Urine antigen detection may not have definitive diagnostic value in suspected H. influenzae type b disease following vaccination with VAXELIS. [See DRUG INTERACTIONS (7.1).]
-
6 ADVERSE REACTIONS
Rates of adverse reactions varied by number of doses of VAXELIS received. The solicited adverse reactions 0-5 days following any dose were irritability (≥55%), crying (≥45%), injection site pain (≥44%), somnolence (≥40%), injection site erythema (≥25%), decreased appetite (≥23%), fever ≥38.0°C (≥19%), injection site swelling (≥18%), and vomiting (≥9%).
6.1 Clinical Trials Experience
Because clinical trials are conducted under varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to vaccine use and for approximating rates of those events.
The safety of VAXELIS was evaluated in 6 clinical studies, in which a total of 5,251 infants 43 to 99 days of age at enrollment received at least 1 dose of VAXELIS. Two of these (study 005 and 006) were controlled clinical studies conducted in the US, in which a total of 3,380 infants 46 to 89 days of age at enrollment received at least 1 dose of VAXELIS. The vaccination schedules of VAXELIS, Control vaccines, and concomitantly administered vaccines used in these studies are provided in Table 1. At 15 months of age, participants in Study 005 received a dose of DAPTACEL and a H. influenzae type b conjugate vaccine, whereas participants in Study 006 received a dose of Pentacel. In a non-US study, 294 children received a dose of VAXELIS at 15 months of age.
Across the 2 studies conducted in the US, among all randomized participants (3,392 in the VAXELIS group and 889 in the Control group), 52.6% were male and 47.4% were female. The race distribution was as follows: 71.7% were White, 11.0% were Black, 4.5% were American Indian or Alaska Native, 3.5% were Asian, and 9.3% were of other racial groups. Most participants (81.8%) were of non-Hispanic or Latino ethnicity. The racial/ethnic distribution of participants who received VAXELIS and Control vaccines was similar.
Table 1: Clinical Safety Studies with VAXELIS in the US: Vaccination Schedules Study Vaccine Concomitantly Administered Vaccines Prevnar 13 (Pneumococcal 13-valent Conjugate Vaccine [Diphtheria CRM197 Protein]) RotaTeq (Rotavirus Vaccine, Live, Oral, Pentavalent) PedvaxHIB [Haemophilus b Conjugate Vaccine (Meningococcal Protein Conjugate)] RECOMBIVAX HB (Hepatitis B Vaccine [Recombinant]) - *
- The first dose of Hepatitis B vaccine was administered prior to study initiation (prior to or at 1 month of age).
005* VAXELIS at 2, 4, 6 months and DAPTACEL + PedvaxHIB® at 15 months RotaTeq® at 2, 4, and 6 months
Prevnar 13® at 2, 4, 6, and 15 monthsControl group vaccines:
Pentacel at 2, 4, 6 months and RECOMBIVAX HB® at 2 and 6 months
DAPTACEL+ ActHIB® at 15 monthsRotaTeq at 2, 4, and 6 months
Prevnar 13 at 2, 4, 6, and 15 months006* VAXELIS at 2, 4, 6 months and Pentacel at 15 months RotaTeq at 2, 4, and 6 months
Prevnar 13 at 2, 4, 6, and 15 monthsControl group vaccines:
Pentacel at 2, 4, 6, and 15 months
RECOMBIVAX HB at 2 and 6 monthsRotaTeq at 2, 4, and 6 months
Prevnar 13 at 2, 4, 6, and 15 monthsSolicited Adverse Reactions
Information on solicited adverse events was recorded daily by parents or guardians on vaccination report cards. The incidence and severity of solicited injection site and systemic adverse reactions (i.e., vaccine-related adverse events) that occurred within 5 days following each dose of VAXELIS or Control vaccines at 2, 4, and 6 months of age in studies 005 and 006 are shown in Table 2.
Table 2: Percentage of Infants with Solicited Adverse Reactions Occurring within 5 days Following VAXELIS or Control Vaccines Administered Concomitantly at Separate Sites with Prevnar 13 and RotaTeq in Studies 005 and 006 VAXELIS + Prevnar 13 + RotaTeq Pentacel + RECOMBIVAX HB + Prevnar 13 + RotaTeq Dose 1
(N=3,370)
(%)Dose 2
(N=3,221)
(%)Dose 3
(N=3,134)
(%)Dose 1
(N=880)
(%)Dose 2
(N=849)
(%)Dose 3
(N=825)
(%)Injection Site Adverse Reactions VAXELIS site Pentacel or RECOMBIVAX HB site N = Number of vaccinated participants with safety follow-up. - *
- Moderate: cries and protests when injection site is touched; Severe: cries when injected limb is moved or the movement of the injected limb is reduced.
- †
- Moderate: missed 1 or 2 feeds/meals completely; Severe: refuses ≥3 feeds or refuses most feeds.
- ‡
- Moderate: requiring increased attention; Severe: inconsolable.
- §
- Moderate: not interested in surroundings or did not wake up for a meal; Severe: Sleeping most of the time or difficult to wake up.
- ¶
- Moderate: 2–5 episodes per 24 hours; Severe: ≥6 episodes per 24 hours or requiring parenteral hydration.
A subject with the same adverse reactions at both the Pentacel and RECOMBIVAX HB injection site, was counted once and was classified according to the highest intensity grading.
Fever is based upon actual temperatures recorded with no adjustments due to the measurement route.
Following Doses 1–3 combined, the proportion of temperature measurements that were taken by rectal, axillary, or other routes were 91.7%, 8.1%, and 0% respectively, for VAXELIS group, and 90.3%, 9.7%, and 0%, respectively, for Pentacel + RECOMBIVAX HB vaccines group.
Injection site erythema Any 25.8 31.8 31.8 25.0 25.8 30.9 ≥2.5 cm 0.9 1.0 1.3 1.1 1.1 1.2 >5.0 cm 0.0 0.1 0.2 0.3 0.2 0.1 Injection site pain* Any 53.3 49.0 44.9 55.8 43.7 44.4 Moderate or severe 16.3 14.1 12.5 19.1 11.3 10.8 Severe 2.8 2.5 2.0 3.2 1.9 1.3 Injection site swelling Any 18.9 22.8 23.4 20.8 20.4 22.9 ≥2.5 cm 2.5 1.6 1.7 2.7 1.3 0.8 >5.0 cm 0.2 0.2 0.2 0.3 0.1 0.0 Systemic Adverse Reactions Fever ≥38°C 19.2 29.0 29.3 14.6 18.0 17.8 ≥38.5°C 5.3 11.5 13.2 3.4 6.5 8.1 ≥39.5°C 0.2 0.7 1.5 0.1 0.2 0.9 Crying Any 52.0 49.5 45.1 50.6 47.0 40.6 >1 hour 18.6 19.8 16.7 20.6 16.8 14.1 >3 hours 3.6 3.8 3.4 4.4 4.0 2.9 Decreased Appetite† Any 28.9 24.2 23.2 25.8 20.5 20.1 Moderate or severe 7.0 5.5 4.8 6.8 3.9 5.0 Severe 0.5 0.5 0.5 0.6 0.2 0.0 Irritability‡ Any 61.8 58.9 55.2 61.7 56.3 51.6 Moderate or severe 24.6 23.4 20.1 25.7 19.2 16.8 Severe 2.5 3.8 2.9 2.2 2.7 2.2 Somnolence§ Any 56.3 47.8 40.8 55.2 44.1 38.8 Moderate or severe 15.0 11.5 8.5 14.5 9.4 8.2 Severe 1.5 1.1 1.0 1.7 0.6 1.1 Vomiting¶ Any 13.1 11.5 9.5 11.3 9.7 6.9 Moderate or severe 3.5 2.6 2.1 2.8 3.1 1.0 Severe 0.4 0.2 0.1 0.5 0.6 0.1 Non-fatal Serious Adverse Events
Across Studies 005 and 006, within 30 days following any infant dose vaccination, 68 participants (2.0%) who received VAXELIS and concomitant vaccines versus 19 participants (2.2%) who received Control and concomitant vaccines experienced a serious adverse event. Of these, a vaccine-related SAE was reported for no participants in the Control vaccines group and for 4 participants (0.1%) in the VAXELIS group:
- 3 of these 4 experienced pyrexia 1 to 2 days following the first study vaccinations; and
- 1 of these 4 experienced an apparent life-threatening event (vomiting followed by pallor and lethargy) on the day of the first study vaccinations, and again 2 days later.
Deaths
In the 2 US studies, death was reported in 6 participants (0.2%) who received VAXELIS and in 1 participant (0.1%) who received Pentacel + RECOMBIVAX HB vaccines; none were assessed as vaccine related. Causes of death among infants who received VAXELIS were sepsis, 2 cases of Sudden Infant Death Syndrome, asphyxia, unknown cause, and hydrocephalus (occurring 2, 10 and 49, 42, 44 days, and 11 months post-vaccination, respectively). Across all 6 clinical studies, there were no deaths assessed as related to VAXELIS.
6.2 Postmarketing Experience
The following adverse events have been reported during post-marketing use of VAXELIS or other vaccines containing the antigens of VAXELIS. These adverse events are included based on a suspected causal connection to VAXELIS or the components of DAPTACEL® (Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed), IPOL® (Poliovirus Vaccine Inactivated), COMVAX® [Haemophilus b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine]. (COMVAX is no longer licensed in the US.)
Because these events are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to vaccination.
-
Immune System Disorders
Hypersensitivity (such as rash, urticaria, dyspnea, erythema multiforme), anaphylactic reaction (such as urticaria, angioedema, edema, face edema, shock). -
General Disorders and Administration Site Conditions
Extensive swelling of injected limb (including swelling that involves adjacent joints). -
Nervous System
Seizure, febrile seizure, hypotonic-hyporesponsive episode (HHE).
-
7 DRUG INTERACTIONS
7.1 Interference with Laboratory Tests
Sensitive tests (e.g., Latex Agglutination kits) have detected vaccine-derived polyribosylribitol phosphate (PRP) in the urine of vaccinees for at least 30 days following vaccination with PedvaxHIB [Haemophilus b Conjugate Vaccine (Meningococcal Protein Conjugate)]. (2) Therefore, urine antigen detection may not have definite diagnostic value in suspected H. influenzae type b disease following vaccination with VAXELIS. [See WARNINGS AND PRECAUTIONS (5.7).]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
VAXELIS is not approved for use in individuals 5 years of age and older. No human or animal data are available to assess vaccine-associated risks in pregnancy.
8.2 Lactation
VAXELIS is not approved for use in individuals 5 years of age and older. No human or animal data are available to assess the impact of VAXELIS on milk production, its presence in breast milk, or its effects on the breastfed infant.
8.4 Pediatric Use
The safety of VAXELIS has been established in the age group 6 weeks through 15 months, and the effectiveness of VAXELIS was established in the age group 6 weeks through 6 months on the basis of clinical studies. [See ADVERSE REACTIONS (6.1) AND CLINICAL STUDIES (14).]
The safety and effectiveness of VAXELIS in older children through 4 years of age are supported by evidence in younger children. The safety and effectiveness of VAXELIS in infants less than 6 weeks of age and in children and adolescents 5 through 17 years of age have not been established.
-
11 DESCRIPTION
VAXELIS (Diphtheria and Tetanus Toxoids and Acellular Pertussis, Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B Vaccine) is a sterile suspension for intramuscular injection.
Each 0.5 mL dose is formulated to contain 15 Lf diphtheria toxoid, 5 Lf tetanus toxoid, acellular pertussis antigens [20 mcg detoxified pertussis toxin (PT), 20 mcg filamentous hemagglutinin (FHA), 3 mcg pertactin (PRN), 5 mcg fimbriae types 2 and 3 (FIM)], inactivated polioviruses [29 D-antigen units (DU) Type 1 (Mahoney), 7 DU Type 2 (MEF-1), 26 DU Type 3 (Saukett)], 3 mcg polyribosylribitol phosphate (PRP) of H. influenzae type b covalently bound to 50 mcg of the outer membrane protein complex (OMPC) of Neisseria meningitidis serogroup B, and 10 mcg hepatitis B surface antigen (HBsAg). Each 0.5 mL dose contains 319 mcg aluminum from aluminum salts used as adjuvants.
Other ingredients per 0.5 mL dose include <0.0056% polysorbate 80 and the following residuals from the manufacturing process: ≤14 mcg formaldehyde, ≤50 ng glutaraldehyde, ≤50 ng bovine serum albumin, <5 ng of neomycin, <200 ng streptomycin sulfate, <25 ng polymyxin B sulfate, ≤0.125 μg ammonium thiocyanate and ≤0.1 mcg yeast protein (maximum 1% relative to HBsAg protein).
Corynebacterium diphtheriae is grown in modified Mueller's growth medium. (3) After purification by ammonium sulfate fractionation, the diphtheria toxin is detoxified with formaldehyde and diafiltered.
Clostridium tetani is grown in modified Mueller-Miller casamino acid medium without beef heart infusion. (4) Tetanus toxin is detoxified with formaldehyde and purified by ammonium sulfate fractionation and diafiltration. Diphtheria and tetanus toxoids are individually adsorbed onto aluminum phosphate.
The acellular pertussis vaccine antigens are produced from Bordetella pertussis cultures grown in Stainer-Scholte medium (5) modified by the addition of casamino acids and dimethyl-beta-cyclodextrin. PT, FHA and PRN are isolated separately from the supernatant culture medium. FIM are extracted and copurified from the bacterial cells. The pertussis antigens are purified by sequential filtration, salt-precipitation, ultrafiltration and chromatography. PT is detoxified with glutaraldehyde. FHA is treated with formaldehyde and the residual aldehydes are removed by ultrafiltration. The individual antigens are adsorbed separately onto aluminum phosphate.
The Type 1, Type 2, and Type 3 polioviruses are individually grown in Vero cells. The viral harvests are concentrated and purified, then inactivated with formaldehyde to produce monovalent suspensions of each serotype. Specified quantities of monovalent suspensions of each serotype are mixed to produce the trivalent poliovirus concentrate.
The HBsAg antigen is harvested and purified from fermentation cultures of a recombinant strain of the yeast Saccharomyces cerevisiae containing the gene for the adw subtype of HBsAg. The recombinant Saccharomyces cerevisiae is grown in a fermentation medium which consists of an extract of yeast, soy peptone, dextrose, amino acids, and mineral salts. The HBsAg protein is released from the yeast cells by cell disruption and purified by a series of physical and chemical methods which includes ion and hydrophobic chromatography, and diafiltration. The purified protein is treated in phosphate buffer with formaldehyde and then co-precipitated with alum (potassium aluminum sulfate) to form bulk vaccine adjuvanted with amorphous aluminum hydroxyphosphate sulfate.
The purified PRP of H. influenzae type b (Haemophilus b, Ross strain) is conjugated to an OMPC of the B11 strain of N. meningitidis serogroup B. H. influenzae type b is grown in a fermentation medium which includes an extract of yeast, nicotinamide adenine dinucleotide, hemin chloride, soy peptone, dextrose, and mineral salts. The PRP is purified from the culture broth by purification procedures which include ethanol fractionation, enzyme digestion, phenol extraction and diafiltration. N. meningitidis serogroup B is grown in a fermentation medium which includes an extract of yeast, amino acids and mineral salts. The OMPC is purified by detergent extraction, ultracentrifugation, diafiltration and sterile filtration. PRP is conjugated to OMPC by chemical coupling and the PRP-OMPC is then adsorbed onto an amorphous aluminum hydroxyphosphate sulfate adjuvant.
The adsorbed diphtheria, tetanus, and acellular pertussis antigens are combined with aluminum phosphate (as adjuvant) and water for injection into an intermediate concentrate. The individual HBsAg and PRP-OMPC adjuvanted bulks are added followed by the trivalent poliovirus concentrate, to produce VAXELIS.
Both diphtheria and tetanus toxoids induce at least 2 neutralizing units per mL of serum in the guinea pig potency test. The potency of the acellular pertussis antigens is evaluated by the antibody response of immunized mice to detoxified PT, FHA, PRN and FIM as measured by enzyme-linked immunosorbent assay (ELISA). The immunogenicity of the inactivated polioviruses is evaluated by the antibody response in rats measured by virus neutralization. The potency of the HBsAg component is measured relative to a standard by an in vitro immunoassay. The potency of the PRP-OMPC component is measured by quantitating the polysaccharide concentration using an HPLC method.
VAXELIS does not contain a preservative. The vial stopper, syringe plunger stopper, and syringe tip cap are not made with natural rubber latex.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Diphtheria
Diphtheria is an acute toxin-mediated disease caused by toxigenic strains of C. diphtheriae. Protection against disease is due to the development of neutralizing antibodies to diphtheria toxin. A serum diphtheria antitoxin level of 0.01 IU/mL is the lowest level giving some degree of protection. Antitoxin levels of ≥0.1 IU/mL are generally regarded as protective. (6) Levels of 1.0 IU/mL have been associated with long-term protection. (7)
Tetanus
Tetanus is an acute disease caused by an extremely potent neurotoxin produced by C. tetani. Protection against disease is due to the development of neutralizing antibodies to tetanus toxin. A serum tetanus antitoxin level of ≥0.01 IU/mL, measured by neutralization assay is considered the minimum protective level. (6) (8) A tetanus antitoxoid level ≥0.1 IU/mL as measured by the ELISA used in clinical studies of VAXELIS is considered protective.
Pertussis
Pertussis (whooping cough) is a respiratory disease caused by B. pertussis. This Gram-negative coccobacillus produces a variety of biologically active components, though their role in either the pathogenesis of, or immunity to, pertussis has not been clearly defined.
Poliomyelitis
Polioviruses, of which there are 3 serotypes (Types 1, 2, and 3), are enteroviruses. The presence of poliovirus type-specific neutralizing antibodies has been correlated with protection against poliomyelitis. (9)
Hepatitis B
Hepatitis B virus is one of several hepatitis viruses that cause systemic infection, with major pathology in the liver. Antibody concentrations of ≥10 mIU/mL against HBsAg correlate with protection against hepatitis B virus infection.
Haemophilus influenzae type b Invasive Disease
H. influenzae type b can cause invasive disease such as meningitis and sepsis. Anti-PRP antibody has been shown to correlate with protection against invasive disease due to H. influenzae type b.
Based on data from passive antibody studies (10) and an efficacy study with H. influenzae type b polysaccharide vaccine in Finland, (11) a post-vaccination anti-PRP level of ≥0.15 mcg/mL is considered a minimal protective level. Data from an efficacy study with H. influenzae type b polysaccharide vaccine in Finland indicate that an anti-PRP level of ≥1.0 mcg/mL 3 weeks after vaccination predicts protection through a subsequent 1-year period. (11) (12) These levels have been used to evaluate the effectiveness of H. influenzae type b conjugate vaccines, including the PRP-OMPC component of VAXELIS.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
14.1 Effectiveness of VAXELIS
The effectiveness of VAXELIS is based on the immunogenicity of the individual antigens compared to US licensed vaccines. Serological correlates of protection exist for diphtheria, tetanus, hepatitis B, poliomyelitis, and invasive disease due to H. influenzae type b. The effectiveness against pertussis is based upon the pertussis immune responses following 3 doses of VAXELIS compared to 3 doses of Pentacel, as well as the pertussis immune responses following a subsequent dose of DAPTACEL in the same 2 groups of children. VAXELIS, Pentacel and DAPTACEL contain the same pertussis antigens, manufactured by the same processes.
14.2 Immunogenicity
In the US Study 005 (Table 1), infants were randomized to receive 3 doses of VAXELIS at 2, 4, and 6 months of age and DAPTACEL and PedvaxHIB at 15 months of age, or Control group vaccines (3 doses of Pentacel vaccine at 2, 4, and 6 months of age + RECOMBIVAX HB at 2 and 6 months of age and DAPTACEL and ActHIB at 15 months of age). All subjects received concomitant vaccines: RotaTeq at 2, 4 and 6 months and Prevnar 13 at 2, 4, 6, and 15 months of age. [See ADVERSE REACTIONS (6.1).] All infants had received a dose of hepatitis B vaccine prior to study initiation, prior to or at one month of age. Among all randomized participants, 53.0% were male and 47.0% were female. Most (79.2%) participants were White, 14.1% were Black and 5.2% were multi-racial. Most (91.4%) participants were of non-Hispanic or non-Latin ethnicity.
Antibody responses to diphtheria, tetanus, pertussis (PT, FHA, PRN and FIM), poliovirus types 1, 2 and 3, hepatitis B and H. influenzae type b antigens were measured in sera obtained one month following the third dose of VAXELIS or Pentacel + RECOMBIVAX HB vaccines. VAXELIS was non-inferior to Pentacel + RECOMBIVAX HB administered concomitantly at separate sites, as demonstrated by the proportions of participants achieving seroprotective levels of antibodies to diphtheria, tetanus, poliovirus, hepatitis B and PRP antigens, and pertussis vaccine response rates and GMCs (except FHA), following 3 doses of the vaccine. See Table 3.
To complete the 4-dose pertussis primary vaccination series, participants in both groups received DAPTACEL at 15 months of age and were evaluated for immune responses to pertussis antigens one month later. The non-inferiority criteria for vaccine response rates and GMCs for all pertussis antigens were met following the fourth dose.
Table 3: Antibody Responses One Month Following Dose 3 of VAXELIS or Control Vaccines Administered Concomitantly with Prevnar 13 and RotaTeq in Study 005 VAXELIS + Prevnar 13 + RotaTeq
(N=688 – 810)Pentacel + RECOMBIVAX HB + Prevnar 13 + RotaTeq
(N=353 – 400)N = The number of participants with available data. - *
- Non-inferiority criterion met (lower bound of 2-sided 95% CI for the difference [VAXELIS group minus Control vaccines group] was >-10%).
- †
- Non-inferiority criterion met (lower bound of 2-sided 95% CI for the difference [VAXELIS group minus Control vaccines group] was >-5%).
- ‡
- Vaccine response = if pre-vaccination antibody concentration was <4 × lower limit of quantitation [LLOQ], then the post-vaccination antibody concentration was ≥4 × LLOQ; if pre-vaccination antibody concentration was ≥4 × LLOQ, then the post-vaccination antibody concentration was ≥pre-vaccination levels (pre-Dose 1).
- §
- Non-inferiority criterion met (lower bound of 2-sided 95% CI for the GMC ratio [VAXELIS group/Control vaccines group] was >0.67).
- ¶
- Non-inferiority criterion not met for anti-FHA GMC (lower bound of 2-sided 95% CI for the GMC ratio [VAXELIS group/Control vaccines group was 0.59 which is below the non-inferiority criterion >0.67).
Anti-Diphtheria Toxoid % ≥0.1 IU/mL 82.4* 86.3 Anti-Tetanus Toxoid % ≥0.1 IU/mL 99.9† 99.5 Anti-PT % vaccine response‡ 98.1* 98.5 GMC 109.6§ 85.4 Anti-FHA % vaccine response‡ 87.3* 92.0 GMC 46.6¶ 72.3 Anti-PRN % vaccine response‡ 79.3* 82.0 GMC 55.8§ 66.8 Anti-FIM % vaccine response‡ 90.2* 86.2 GMC 235.9§ 184.4 Anti-Poliovirus Type 1 % ≥1:8 dilution 100.0† 98.2 Anti-Poliovirus Type 2 % ≥1:8 dilution 100.0† 99.7 Anti-Poliovirus Type 3 % ≥1:8 dilution 100.0† 99.8 Anti-PRP % ≥0.15 μg/mL 97.3† 92.4 % ≥1.0 μg/mL 85.0* 75.3 Anti-HBsAg % ≥10 mIU/mL 99.4* 98.6 Study 006 (Table 1) was a lot consistency study conducted in the US, where infants were randomized to receive 3 doses of VAXELIS at 2, 4, and 6 months of age and Pentacel at 15 months of age (N=2,406), or control group vaccines (4 doses of Pentacel at 2, 4, 6, and 15 months of age + RECOMBIVAX HB at 2 and 6 months of age; N=402). All subjects received concomitant vaccines: RotaTeq at 2, 4 and 6 months and Prevnar 13 at 2, 4, 6, and 15 months of age. All infants had received a dose of hepatitis B vaccine prior to study initiation, from birth up to one month of age.
Antibody responses to diphtheria, tetanus, pertussis (PT, FHA, PRN and FIM), poliovirus types 1, 2 and 3, hepatitis B and H. influenzae type b antigens were measured in sera obtained one month following the third dose of VAXELIS or Pentacel + RECOMBIVAX HB. VAXELIS was non-inferior to Pentacel + RECOMBIVAX HB administered concomitantly at separate sites, as demonstrated by the proportions of participants achieving seroprotective levels of antibodies to diphtheria, tetanus, poliovirus, hepatitis B and PRP antigens, and pertussis vaccine response rates and GMCs, except for GMCs for FHA (lower bound of 2-sided 95% CI for GMC ratio [VAXELIS group/Control group vaccines] was 0.62, which was below the non-inferiority criterion >0.67).
To complete the 4-dose pertussis primary vaccination series, participants in both groups received Pentacel at 15 months of age and were evaluated for immune responses to pertussis antigens one month later. The non-inferiority criteria for antibody vaccine response rates and GMCs for all pertussis antigens were met following the fourth dose except for GMCs for PRN (lower bound of 2-sided 95% CI for GMC ratio [VAXELIS group/Control group vaccines] was 0.66, which was below the non-inferiority criterion >0.67).
14.3 Concomitantly Administered Vaccines
In Study 006 conducted in the US (Table 1), the immune responses to Prevnar 13 were measured one month after the third dose. Non-inferiority criteria were met for GMCs to 12 of the 13 serotype antigens in Prevnar 13 for participants who received VAXELIS relative to Control vaccines. For serotype 6B, the non-inferiority criterion was not met (lower bound of 2-sided 95% CI for GMC ratio [VAXELIS group/Control vaccines group] is 0.64, which is below the non-inferiority criterion >0.67).
-
15 REFERENCES
- 1
- Stratton K, Ford A, Rusch E, Clayton EW, eds. Institute of Medicine (IOM). Adverse Effects of Vaccines: Evidence and Causality. Washington, DC: The National Academies Press. 2011.
- 2
- Goepp JG, Hohenboken M, Almeido-Hill J, Santosham M. Persistent urinary antigen excretion in infants vaccinated with Haemophilus influenzae type b capsular polysaccharide conjugated with outer membrane protein from Neisseria meningitidis. Pediatr Infect Dis J 1992;11(1):2–5.
- 3
- Stainer DW. Production of diphtheria toxin. In: Manclark CR, editor. Proceedings of an informal consultation on the World Health Organization requirements for diphtheria, tetanus, pertussis and combined vaccines. United States Public Health Service, Bethesda, MD. DHHS 91-1174; 1991. p. 7–11.
- 4
- Mueller JH, Miller PA. Variable factors influencing the production of tetanus toxin. J Bacteriol 1954;67(3):271–7.
- 5
- Stainer DW, Scholte MJ. A simple chemically defined medium for the production of phase I Bordetella pertussis. J Gen Microbiol 1971;63:211–20.
- 6
- Department of Health and Human Services, Food and Drug Administration. Biological products; bacterial vaccines and toxoids; implementation of efficacy review; proposed rule. Federal Register 1985;50(240):51002–117.
- 7
- Tiwari TSP, Wharton M. Diphtheria toxoid. In: Plotkin SA, Orenstein WA, and Offit PA, editors. Vaccines. 6th ed. Philadelphia, PA: WB Saunders; 2013:153–66.
- 8
- Roper M, Wassilak SGF, Tiwari TSP, Orenstein WA. Tetanus toxoid. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 6th ed. Philadelphia, PA: WB Saunders; 2013. p. 746–72.
- 9
- Sutter RW, et al. Defining surrogate serologic tests with respect to predicting protective vaccine efficacy: Poliovirus vaccination. In: Williams JC, et al. eds. Combined vaccines and simultaneous administration. Current issues and perspectives. New York, NY: The New York Academy of Sciences. 1995:289–99.
- 10
- Robbins, J. B., et al: Quantitative measurement of 'natural' and immunization-induced Haemophilus influenzae type b capsular polysaccharide antibodies. Pediatr Res 1973;7(3):103–10.
- 11
- Kayhty H, et al. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis 1983;147:1100.
- 12
- Anderson P. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis 1984;149:1034.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
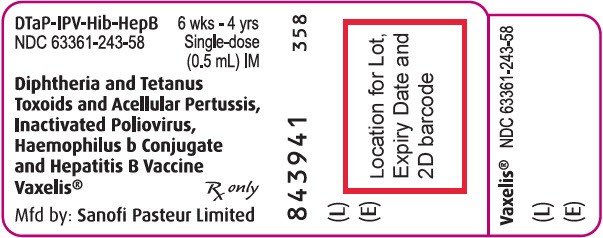
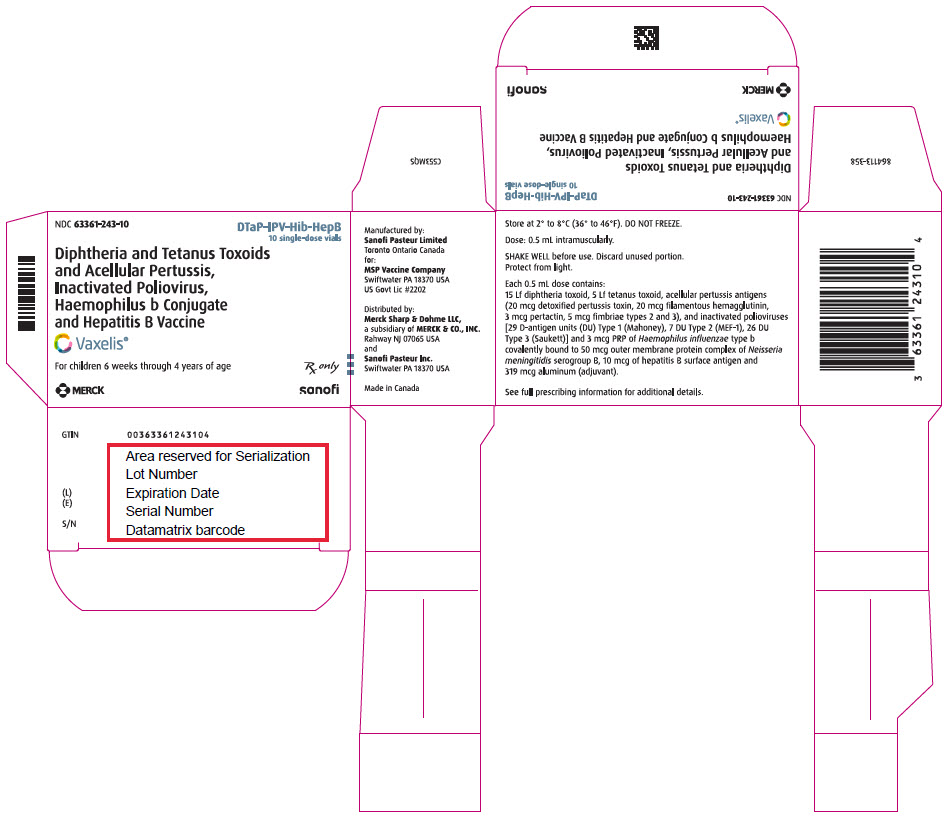
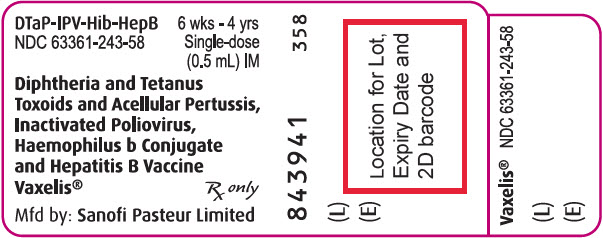
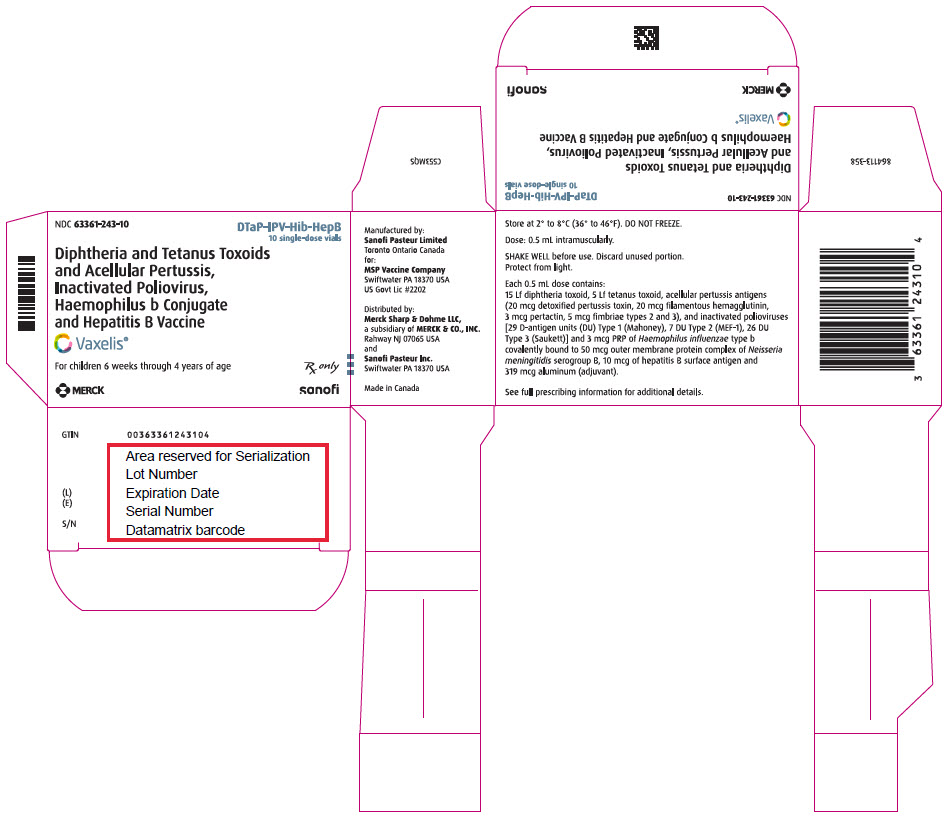
Single-dose vial (NDC 63361-243-58) in packages of 10 vials (NDC 63361-243-10).
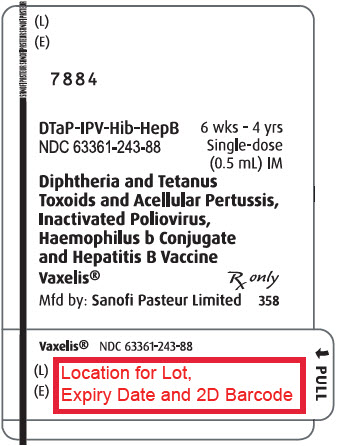
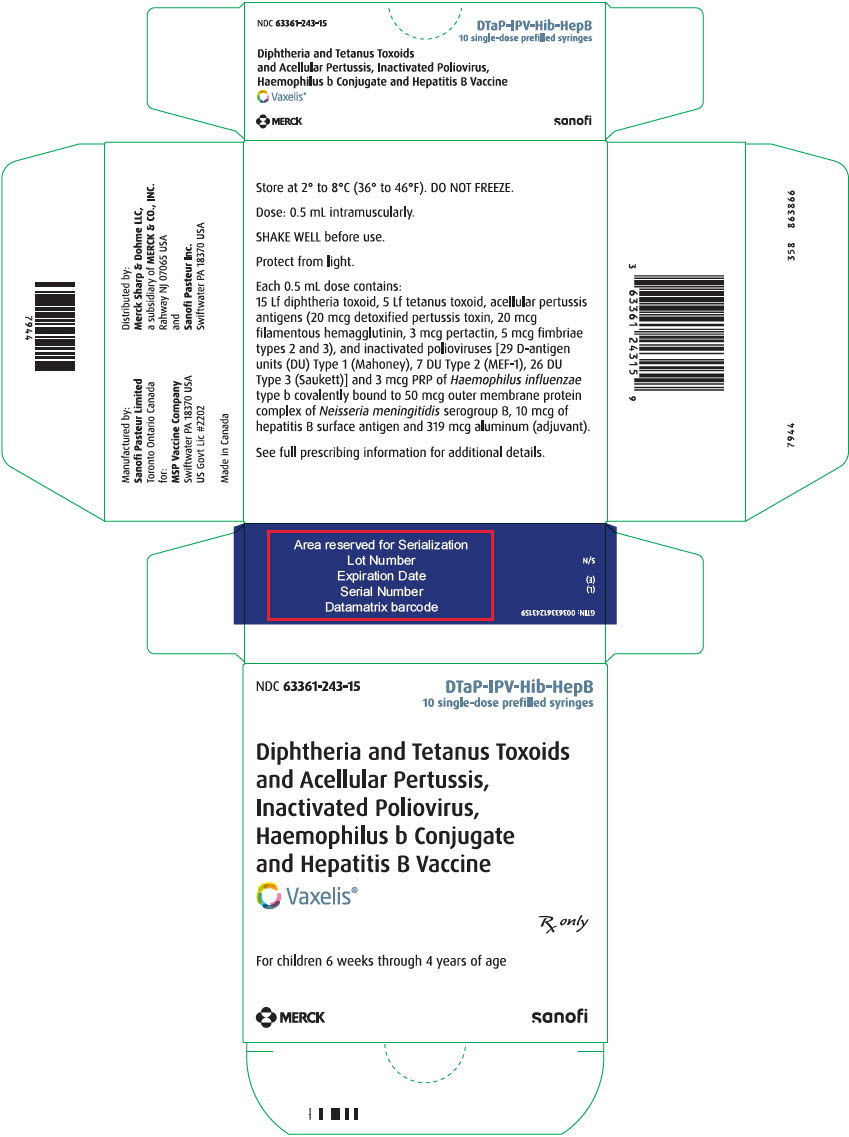
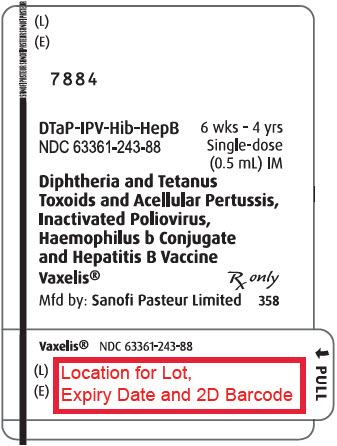
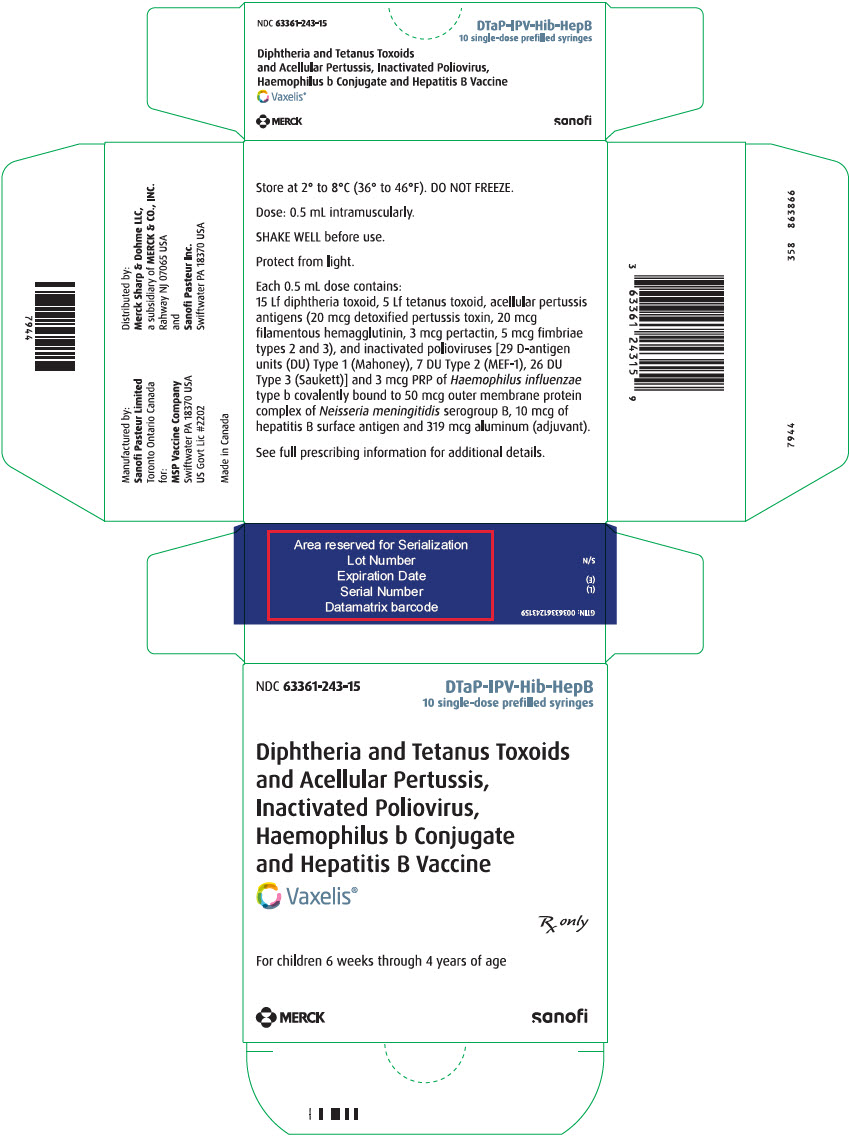
Single-dose, prefilled syringe with Luer lock connection and a tip cap, without needle, 0.5 mL (NDC 63361-243-88). Supplied as package of 10 (NDC 63361-243-15).
The vial stopper, syringe plunger stopper, and syringe tip cap are not made with natural rubber latex.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Inform the parent or guardian of the following:
- The potential benefits and risks of immunization with VAXELIS.
- The common adverse reactions that have occurred following administration of VAXELIS or other vaccines containing similar ingredients.
- Other adverse reactions can occur. Call healthcare provider with any adverse reactions of concern.
Provide the Vaccine Information Statements (VIS), which are required by the National Childhood Vaccine Injury Act of 1986.
-
SPL UNCLASSIFIED SECTION
Manufactured by:
Sanofi Pasteur Limited
Toronto Ontario Canada
for:
MSP Vaccine Company
Swiftwater PA 18370 USADistributed by:
Merck Sharp & Dohme LLC
A subsidiary of Merck & Co., Inc.
Rahway NJ 07065 USA
and Sanofi Pasteur Inc.
Swiftwater PA 18370 USAVAXELIS is a trademark of MSP Vaccine Company. The trademarks depicted herein are owned by their respective companies.
R9-1022 USA
-
PATIENT PACKAGE INSERT
Patient Information VAXELIS® (pronounced "vak-sel-lis")
(Diphtheria and Tetanus Toxoids and Acellular Pertussis, Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B Vaccine)Before your child gets VAXELIS, read this document and be sure you understand all of the information. Keep this document, you may need to read it again. If you have questions or side effects, ask your child's healthcare provider. This information does not take the place of talking about VAXELIS with your child's healthcare provider. What is VAXELIS? VAXELIS is a vaccine given to protect your child from getting diphtheria, tetanus (lockjaw), pertussis (whooping cough), polio, Hib (Haemophilus influenzae type b), and hepatitis B. Your child cannot get any of these diseases from VAXELIS. VAXELIS may not completely protect your child from these diseases. Who should not get VAXELIS? Your child should not get VAXELIS, if your child: - is allergic to any of the ingredients.
- had an allergic reaction to any prior shot for diphtheria, tetanus, pertussis, polio, Hib, or hepatitis B.
- had a serious reaction affecting their brain and nervous system after a whooping cough shot.
- has a brain and nerve illness that is getting worse.
Before your child gets VAXELIS, tell your healthcare provider if your child: - had problems with any shots for these diseases.
- is taking steroids, getting treatment for cancer, or has another problem that weakens the immune system.
How is VAXELIS given? - VAXELIS is given to children from 6 weeks through 4 years of age (up to 5th birthday).
- Your child will need 3 shots:
- one shot at 2 months old, and
- one shot at 4 months old, and
- one shot at 6 months old
- If your child misses a shot of VAXELIS, your healthcare provider may suggest a catch-up schedule.
- Your child may get VAXELIS at the same time they get other vaccines.
What are the most common side effects of VAXELIS? - pain, redness, or swelling where the shot was given
- fever (100.4°F or higher)
- crying more than usual
- eating less than usual
- fussy more than usual
- sleepy more than usual
- throwing up
There may be other side effects that are not listed. If your child has any side effects that worry you or seem to get worse, tell your child's healthcare provider right away. You may report any side effects directly to the Vaccine Adverse Event Reporting System (VAERS) at 1-800-822-7967 or http://vaers.hhs.gov, or contact Sanofi Pasteur Inc., at 1-800-822-2463 (1-800-VACCINE). To learn more about VAXELIS, ask your healthcare provider. You can also find the Full Prescribing Information written for doctors at www.fda.gov/media/119465/download. What is in VAXELIS? - Active ingredients: inactivated bacteria of diphtheria, tetanus, pertussis, Hib, and inactivated hepatitis B and polio viruses. The bacteria and viruses in VAXELIS are not alive and do not cause disease.
- Other ingredients: aluminum salts, polysorbate 80, glutaraldehyde, formaldehyde, bovine serum albumin, neomycin, streptomycin, polymyxin B, ammonium thiocyanate, yeast protein, and water.
- VAXELIS does not have any preservatives in it.
- VAXELIS vial stopper, syringe plunger stopper, and syringe tip cap do not contain natural rubber latex.
Manufactured by: Sanofi Pasteur Limited Toronto Ontario Canada for: MSP Vaccine Company Swiftwater PA 18370 USA.
Distributed by: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc. Rahway NJ 07065 USA, and by Sanofi Pasteur Inc. Swiftwater PA 18370 USA.
VAXELIS is a trademark of MSP Vaccine Company. The trademarks depicted herein are owned by their respective companies.
Initial Approval: 23 October 2020
R2-1022 - PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Package
- PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Label
- PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Package
-
INGREDIENTS AND APPEARANCE
VAXELIS
diphtheria and tetanus toxoids and acellular pertussis, inactivated poliovirus, haemophilus b conjugate and hepatitis b vaccine injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC:63361-243 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: IRH51QN26H) (CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:IRH51QN26H) CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 15 [Lf] in 0.5 mL CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: K3W1N8YP13) (CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:K3W1N8YP13) CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 5 [Lf] in 0.5 mL BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) (UNII: F4TN0IPY37) (BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) - UNII:F4TN0IPY37) BORDETELLA PERTUSSIS TOXOID ANTIGEN (GLUTARALDEHYDE INACTIVATED) 20 ug in 0.5 mL BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 8C367IY4EY) (BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:8C367IY4EY) BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) 20 ug in 0.5 mL BORDETELLA PERTUSSIS PERTACTIN ANTIGEN (UNII: 63GD90PP8X) (BORDETELLA PERTUSSIS PERTACTIN ANTIGEN - UNII:63GD90PP8X) BORDETELLA PERTUSSIS PERTACTIN ANTIGEN 3 ug in 0.5 mL BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN (UNII: 1O0600285A) (BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN - UNII:1O0600285A) BORDETELLA PERTUSSIS FIMBRIAE 2/3 ANTIGEN 5 ug in 0.5 mL POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 0LVY784C09) (POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:0LVY784C09) POLIOVIRUS TYPE 1 ANTIGEN (FORMALDEHYDE INACTIVATED) 29 [D'ag'U] in 0.5 mL POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 23JE9KDF4R) (POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:23JE9KDF4R) POLIOVIRUS TYPE 2 ANTIGEN (FORMALDEHYDE INACTIVATED) 7 [D'ag'U] in 0.5 mL POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 459ROM8M9M) (POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:459ROM8M9M) POLIOVIRUS TYPE 3 ANTIGEN (FORMALDEHYDE INACTIVATED) 26 [D'ag'U] in 0.5 mL HEPATITIS B VIRUS SUBTYPE ADW HBSAG SURFACE PROTEIN ANTIGEN (UNII: XL4HLC6JH6) (HEPATITIS B VIRUS SUBTYPE ADW HBSAG SURFACE PROTEIN ANTIGEN - UNII:XL4HLC6JH6) HEPATITIS B VIRUS SUBTYPE ADW HBSAG SURFACE PROTEIN ANTIGEN 10 ug in 0.5 mL HAEMOPHILUS INFLUENZAE TYPE B CAPSULAR POLYSACCHARIDE MENINGOCOCCAL OUTER MEMBRANE PROTEIN CONJUGATE ANTIGEN (UNII: LUY6P8763W) (HAEMOPHILUS INFLUENZAE TYPE B CAPSULAR POLYSACCHARIDE MENINGOCOCCAL OUTER MEMBRANE PROTEIN CONJUGATE ANTIGEN - UNII:LUY6P8763W) HAEMOPHILUS INFLUENZAE TYPE B CAPSULAR POLYSACCHARIDE MENINGOCOCCAL OUTER MEMBRANE PROTEIN CONJUGATE ANTIGEN 3 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength POLYSORBATE 80 (UNII: 6OZP39ZG8H) 28 ug in 0.5 mL FORMALDEHYDE (UNII: 1HG84L3525) 14 ug in 0.5 mL GLUTARAL (UNII: T3C89M417N) 50 ng in 0.5 mL ALBUMIN BOVINE (UNII: 27432CM55Q) 50 ng in 0.5 mL NEOMYCIN (UNII: I16QD7X297) 5 ng in 0.5 mL POLYMYXIN B SULFATE (UNII: 19371312D4) 25 ng in 0.5 mL STREPTOMYCIN (UNII: Y45QSO73OB) 200 ng in 0.5 mL AMMONIUM THIOCYANATE (UNII: YYL9152Z1Y) 0.125 ug in 0.5 mL GI-6207 (UNII: FIJ3OLQ3N8) 0.1 ug in 0.5 mL WATER (UNII: 059QF0KO0R) Other Ingredients Ingredient Kind Ingredient Name Quantity ADJV ALUMINUM PHOSPHATE (UNII: F92V3S521O) 319 ug in 0.5 mL ADJV ALUMINUM HYDROXYPHOSPHATE SULFATE (UNII: F41V936QZM) Product Characteristics Color WHITE (WHITE TO OFF-WHITE) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63361-243-10 10 in 1 PACKAGE 1 NDC:63361-243-58 0.5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC:63361-243-15 10 in 1 PACKAGE 2 NDC:63361-243-88 0.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125563 12/21/2018 Labeler - MSP Vaccine Company (079352454) Establishment Name Address ID/FEI Business Operations Sanofi Pasteur Limited 208206623 MANUFACTURE(63361-243) Establishment Name Address ID/FEI Business Operations Sanofi Pasteur SA 578763542 MANUFACTURE(63361-243) Establishment Name Address ID/FEI Business Operations Merck Sharp & Dohme LLC 002387926 MANUFACTURE(63361-243)