Label: BUPRENORPHINE HYDROCHLORIDE injection
- NDC Code(s): 42023-179-05
- Packager: Par Pharmaceutical, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: CIII
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated September 28, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
(What is this?)
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; NEONATAL OPIOID WITHDRAWAL SYNDROME and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Addiction, Abuse, and Misuse
Buprenorphine exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing buprenorphine, and monitor all patients regularly for the development of these behaviors and conditions (see WARNINGS).
Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression may occur with use of buprenorphine. Monitor for respiratory depression, especially during initiation of buprenorphine or following a dose increase (see WARNINGS).
Neonatal Opioid Withdrawal Syndrome
Prolonged use of buprenorphine during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available (see WARNINGS).
Risks From Concomitant Use With Benzodiazepines Or Other CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death (see WARNINGS, PRECAUTIONS).
- Reserve concomitant prescribing of buprenorphine and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
-
DESCRIPTION
Buprenorphine hydrochloride is a partial opioid agonist.
The chemical name of buprenorphine hydrochloride is 17-(cyclopropylmethyl)-α-(1,1-dimethylethyl)-4, 5-epoxy-18,19-dihydro-3-hydroxy-6-methoxy-α-methyl-6, 14-ethenomorphinan-7-methanol, hydrochloride [5α , 7α(S)].
Buprenorphine hydrochloride is a white powder, weakly acidic and with limited solubility in water.
Buprenorphine hydrochloride injection is a clear, sterile, injectable agonist-antagonist analgesic intended for intravenous or intramuscular administration. Each ml of Buprenorphine hydrochloride injection contains 0.324 mg buprenorphine hydrochloride (equivalent to 0.3 mg buprenorphine), 50 mg anhydrous dextrose, water for injection and HCl to adjust pH.
Buprenorphine hydrochloride has the molecular formula, C29H41NO4HCl, and the following structure:
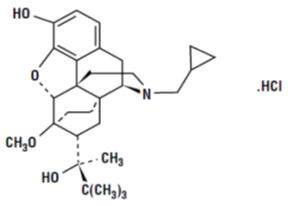
Molecular weight: 504.09 -
CLINICAL PHARMACOLOGY
Mechanism of Action
Buprenorphine is a partial agonist at the mu-opioid receptor and an antagonist at the kappa-opioid receptor. One unusual property of buprenorphine observed in in vitro studies is its very slow rate of dissociation from its receptor. This could account for its longer duration of action than morphine, the unpredictability of its reversal by opioid antagonists, and its low level of manifest physical dependence.
Pharmacodynamics
Buprenorphine hydrochloride is a parenteral opioid analgesic with 0.3 mg buprenorphine being approximately equivalent to 10 mg morphine sulfate in analgesic and respiratory depressant effects in adults. Pharmacological effects occur as soon as 15 minutes after intramuscular injection and persist for 6 hours or longer. Peak pharmacologic effects usually are observed at 1 hour. When used intravenously, the times to onset and peak effect are shortened.
Buprenorphine demonstrates narcotic antagonist activity and has been shown to be equipotent with naloxone as an antagonist of morphine in the mouse tail flick test.
Effects on the Central Nervous System
The principal action of therapeutic value of buprenorphine is analgesia and is thought to be due to buprenorphine binding with high affinity to opioid receptors on neurons in the brain and spinal cord.
Buprenorphine produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Under usual conditions of use in adults, both buprenorphine and morphine show similar dose-related respiratory depressant effects. At adult therapeutic doses, buprenorphine (0.3 mg buprenorphine) can decrease respiratory rate in an equivalent manner to an equianalgesic dose of morphine (10 mg). [see WARNINGS].
Buprenorphine causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Buprenorphine causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects on the Cardiovascular System
Buprenorphine produces peripheral vasodilation, which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
Buprenorphine may cause a decrease or, rarely, an increase in pulse rate and blood pressure in some patients.
Thorough QT studies with buprenorphine products have demonstrated QT prolongation ≤ 15 msec.
Effects on the Endocrine System
Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Chronic use of opioids may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date.
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships
The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with potent agonist opioids. The minimum effective analgesic concentration of buprenorphine for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome, and/or the development of analgesic tolerance.
Concentration–Adverse Reaction Relationships
There is a relationship between increasing buprenorphine plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions.
Pharmacokinetics
The limits of sensitivity of available analytical methodology precluded demonstration of bioequivalence between intramuscular and intravenous routes of administration.
Elimination
In postoperative adults, pharmacokinetic studies have shown elimination half-lives ranging from 1.2 to 7.2 hours (mean 2.2 hours) after intravenous administration of 0.3mg of buprenorphine. A single, ten-patient, pharmacokinetic study of doses of 3μg/kg in children (age 5 to 7 years) showed a high inter-patient variability, but suggests that the clearance of the drug may be higher in children than in adults. This is supported by at least one repeat-dose study in postoperative pain that showed an optimal inter-dose interval of 4 to 5 hours in pediatric patients as opposed to the recommended 6 to 8 hours in adults.
Metabolism
Buprenorphine undergoes both N-dealkylation to norbuprenorphine and glucuronidation. The N-dealkylation pathway is mediated primarily by CYP3A4. Norbuprenorphine, the major metabolite, can further undergo glucuronidation. Its clearance is related to hepatic blood flow. Studies in patients anesthetized with 0.5% halothane have shown that this anesthetic decreases hepatic blood flow by about 30%.
-
INDICATIONS AND USAGE
Buprenorphine hydrochloride injection is indicated for the management of pain severe enough to require an opioid analgesic and for which alternate treatments are inadequate.
Limitations of Use
Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses [see WARNINGS: Addiction, Abuse, and Misuse] reserve buprenorphine for use in patients for whom alternative treatment options [e.g., non-opioid analgesics or opioid combination products]:
-
Have not been tolerated, or are not expected to be tolerated,
- Have not provided adequate analgesia, or are not expected to provide adequate analgesia.
-
-
CONTRAINDICATIONS
Buprenorphine hydrochloride is contraindicated in patients with:
-
Significant respiratory depression [See WARNINGS].
-
Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [See WARNINGS].
-
Known or suspected gastrointestinal obstruction, including paralytic ileus [See WARNINGS].
- Hypersensitivity to buprenorphine (e.g., anaphylaxis) or any other ingredient in buprenorphine hydrochloride injection [See WARNINGS].
-
-
WARNINGS
Addiction, Abuse, and Misuse
Buprenorphine hydrochloride injection contains buprenorphine, a Schedule III controlled substance. As an opioid, buprenorphine exposes users to the risks of addiction, abuse, and misuse.
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed buprenorphine. Addiction can occur at recommended doses and if the drug is misused or abused.
Assess each patient's risk for opioid addiction, abuse, or misuse prior to prescribing buprenorphine, and monitor all patients receiving buprenorphine for the development of these behaviors and conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol addiction or abuse) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the prescribing of buprenorphine for the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as buprenorphine, but use in such patients necessitates intensive counseling about the risks and proper use of buprenorphine along with the intensive monitoring for signs of addiction, abuse, and misuse.
Opioids are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing buprenorphine. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug. Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory depression and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of buprenorphine, the risk is greatest during the initiation of therapy or following a dosage increase. Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with and following dosage increases of buprenorphine.
To reduce the risk of respiratory depression, proper dosing and titration of buprenorphine are essential. Overestimating the buprenorphine dosage when converting patients from another opioid product can result in a fatal overdose with the first dose.
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper [see Dosage and Administration].
Neonatal Opioid Withdrawal Syndrome
Prolonged use of buprenorphine during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see WARNINGS, PRECAUTIONS: Information for Patients, Pregnancy].
Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of buprenorphine with benzodiazepines or other CNS depressants (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions].
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Follow patients closely for signs and symptoms of respiratory depression and sedation.
Advise both patients and caregivers about the risks of respiratory depression and sedation when buprenorphine is used with benzodiazepines or other CNS depressants (including alcohol and illicit drugs). Advise patients not to drive or operate heavy machinery until the effects of concomitant use of the benzodiazepine or other CNS depressant have been determined. Screen patients for risk of substance use disorders, including opioid abuse and misuse, and warn them of the risk for overdose and death associated with the use of additional CNS depressants including alcohol and illicit drugs [see Drug Interactions, and Information for Patients].
Risk of Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of buprenorphine in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease: Buprenorphine-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive, including apnea, even at recommended dosages of buprenorphine [see WARNINGS].
Elderly, Cachectic, or Debilitated Patients: Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients.
Monitor such patients closely, particularly when initiating and titrating buprenorphine and when buprenorphine is given concomitantly with other drugs that depress respiration [see WARNINGS]. Alternatively, consider the use of non-opioid analgesics in these patients.
Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
Severe Hypotension
Buprenorphine may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume, or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics). Monitor these patients for signs of hypotension after initiating or titrating the dosage of buprenorphine. In patients with circulatory shock, buprenorphine may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of buprenorphine in patients with circulatory shock.
Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), buprenorphine may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with buprenorphine.
Opioids may also obscure the clinical course in a patient with a head injury.
Avoid the use of buprenorphine in patients with impaired consciousness or coma.
QTc Prolongation
Thorough QT studies with buprenorphine products have demonstrated QT prolongation ≤ 15 msec. This QTc prolongation effect does not appear to be mediated by hERG channels. Based on these two findings, buprenorphine is unlikely to be pro‐arrhythmic when used alone in patients without risk factors. The risk of combining buprenorphine with other QT‐prolonging agents is not known.
Consider these observations in clinical decisions when prescribing buprenorphine to patients with risk factors such as hypokalemia, bradycardia, recent conversion from atrial fibrillation, congestive heart failure, digitalis therapy, baseline QT prolongation, subclinical long‐QT syndrome, or severe hypomagnesemia.
Anaphylactic/Allergic Reactions
Cases of acute and chronic hypersensitivity to buprenorphine have been reported both in clinical trials and in post-marketing experience. The most common signs and symptoms include rashes, hives, and pruritus. Cases of bronchospasm, angioneurotic edema, and anaphylactic shock have been reported. Buprenorphine is contraindicated in patients with a history of hypersensitivity to buprenorphine.
Risks of Use in Patients with Gastrointestinal Conditions
Buprenorphine is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The buprenorphine in buprenorphine hydrochloride injection may cause spasm of the sphincter of Oddi. Opioids may cause increases in the serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
Increased Risk of Seizures in Patients with Seizure Disorders
The buprenorphine in buprenorphine hydrochloride injection may increase the frequency of seizures in patients with seizure disorders, and may increase the risk of seizures in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during buprenorphine therapy.
Risks Driving and Operating Machinery
Buprenorphine may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of buprenorphine and know how they will react to the medication [see PRECAUTIONS: Information for Patients].
-
PRECAUTIONS
General
Buprenorphine hydrochloride should be administered with caution in the elderly, debilitated patients, in children and those with severe impairment of hepatic, pulmonary, or renal function; myxedema or hypothyroidism; adrenal cortical insufficiency (e.g., Addison's disease); CNS depression or coma; toxic psychoses; prostatic hypertrophy or urethral stricture; acute alcoholism; delirium tremens; or kyphoscoliosis.
Because buprenorphine hydrochloride is metabolized by the liver, the activity of buprenorphine hydrochloride may be increased and/or extended in those individuals with impaired hepatic function or those receiving other agents known to decrease hepatic clearance.
Buprenorphine hydrochloride has been shown to increase intracholedochal pressure to a similar degree as other opioid analgesics, and thus should be administered with caution to patients with dysfunction of the biliary tract.
Information for Patients
Addiction, Abuse, and Misuse
Inform patients that the use of buprenorphine, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose or death [see WARNINGS]. Instruct patients not to share buprenorphine with others and to take steps to protect buprenorphine from theft or misuse.
Life-Threatening Respiratory Depression
Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when starting buprenorphine or when the dosage is increased, and that it can occur even at recommended dosages [see WARNINGS]. Advise patients how to recognize respiratory depression and to seek medical attention if breathing difficulties develop.
Serotonin Syndrome
Inform patients that opioids could cause a rare but potentially life-threatening condition resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their healthcare providers if they are taking, or plan to take serotonergic medications [see PRECAUTIONS; Drug Interactions].
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention [see CLINICAL PHARMACOLOGY: Pharmacodynamics, ADVERSE REACTIONS].
Drug Interactions
Clinically significant drug interactions with buprenorphine.
Benzodiazepines and Other Central Nervous System (CNS) Depressants
Clinical Impact:
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death.
Intervention:
Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients closely for signs of respiratory depression and sedation [see WARNINGS].
Examples:
Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, and other opioids, alcohol.
Inhibitors of CYP3A4
Clinical Impact:
The concomitant use of buprenorphine and CYP3A4 inhibitors can increase the plasma concentration of buprenorphine, resulting in increased or prolonged opioid effects, particularly when an inhibitor is added after a stable dose of buprenorphine is achieved.
After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the buprenorphine plasma concentration will decrease [see CLINICAL PHARMACOLOGY: Pharmacokinetics],potentially resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to buprenorphine.Intervention:
If concomitant use is necessary, consider dosage reduction of buprenorphine until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals.
If a CYP3A4 inhibitor is discontinued, consider increasing the buprenorphine dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal.Examples:
Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), protease inhibitors (e.g., ritonavir)
CYP3A4 Inducers
Clinical Impact:
The concomitant use of buprenorphine and CYP3A4 inducers can decrease the plasma concentration of buprenorphine [see CLINICAL PHARMACOLOGY: Pharmacokinetics], potentially resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to buprenorphine.
After stopping a CYP3A4 inducer, as the effects of the inducer decline, the buprenorphine plasma concentration will increase [see CLINICAL PHARMACOLOGY: Pharmacokinetics], which could increase or prolong both therapeutic effects and adverse reactions and may cause serious respiratory depression.Intervention:
If concomitant use is necessary, consider increasing the buprenorphine dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal.
If a CYP3A4 inducer is discontinued, consider buprenorphine dosage reduction and monitor for signs of respiratory depression.Examples:
Rifampin, carbamazepine, phenytoin
Serotonergic Drugs
Clinical Impact:
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome.
Intervention:
If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue buprenorphine if serotonin syndrome is suspected.
Examples:
Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Monoamine Oxidase Inhibitors (MAOIs)
Clinical Impact:
MAOI interactions with opioids may manifest as serotonin syndrome opioid toxicity (e.g., respiratory depression, coma).
Intervention:
The use of buprenorphine is not recommended for patients taking MAOIs or within 14 days of stopping such treatment.
Examples:
phenelzine, tranylcypromine, linezolid
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics
Clinical Impact:
May reduce the analgesic effect of buprenorphine and/or precipitate withdrawal symptoms.
Intervention:
Avoid concomitant use.
Examples:
butorphanol, nalbuphine, pentazocine
Muscle Relaxants
Clinical Impact:
Buprenorphine may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
Intervention:
Monitor patients receiving muscle relaxants and buprenorphine for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of buprenorphine and/or the muscle relaxant as necessary.
Diuretics
Clinical Impact:
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone.
Intervention:
Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed.
Anticholinergic Drugs
Clinical Impact:
The concomitant use of anticholinergic drugs may increase the risk of urinary retention and/or severe constipation, which may lead to paralytic ileus.
Intervention:
Monitor patients for signs of urinary retention or reduced gastric motility when buprenorphine is used concomitantly with anticholinergic drugs.
Antiretrovirals: Nucleoside reverse transcriptase inhibitors (NRTIs)
Clinical Impact:
Nucleoside reverse transcriptase inhibitors (NRTIs) do not appear to induce or inhibit the P450 enzyme pathway, thus no interactions with buprenorphine are expected.
Intervention:
None
Antiretrovirals: Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Clinical Impact:
Non-nucleoside reverse transcriptase inhibitors (NNRTIs) are metabolized principally by CYP3A4. Efavirenz, nevirapine, and etravirine are known CYP3A inducers, whereas delaviridine is a CYP3A inhibitor. Significant pharmacokinetic interactions between NNRTIs (e.g., efavirenz and delavirdine) and buprenorphine have been shown in clinical studies, but these pharmacokinetic interactions did not result in any significant pharmacodynamic effects.
Intervention:
Patients who are on chronic buprenorphine treatment should have their dose monitored if NNRTIs are added to their treatment regimen.
Examples:
efavirenz, nevirapine, etravirine, delavirdine
Antiretrovirals: Protease inhibitors (PIs)
Clinical Impact:
Studies have shown some antiretroviral protease inhibitors (PIs) with CYP3A4 inhibitory activity (nelfinavir, lopinavir/ritonavir, ritonavir) have little effect on buprenorphine pharmacokinetic and no significant pharmacodynamic effects. Other PIs with CYP3A4 inhibitory activity (atazanavir and atazanavir/ritonavir) resulted in elevated levels of buprenorphine and norbuprenorphine, and patients in one study reported increased sedation. Symptoms of opioid excess have been found in post-marketing reports of patients receiving buprenorphine and atazanavir with and without ritonavir concomitantly.
Intervention:
Monitor patients taking buprenorphine and atazanavir with and without ritonavir, and dose reduction of buprenorphine may be warranted.
Examples:
atazanavir, ritonavir
Carcinogenesis, Mutagenesis and Impairment of Fertility
Carcinogenesis
Carcinogenicity studies were conducted in Sprague-Dawley rats and CD-1 mice. Buprenorphine was administered in the diet at doses of 0.6, 5.5, and 56 mg/kg/day for 27 months in rats. These doses were approximately equivalent to 5.7, 52, and 534 times the recommended human dose (1.2 mg) on a mg/m2 body surface area basis. Statistically significant dose-related increases in testicular interstitial (Leydig's) cell tumors occurred, according to the trend test adjusted for survival. Pairwise comparison of the high dose against control failed to show statistical significance. In the mouse study, buprenorphine was administered in the diet at doses of 8, 50, and 100 mg/kg/day for 86 weeks.
The high dose was approximately equivalent to 477 times the recommended human dose (1.2 mg) on a mg/m2 basis. Buprenorphine was not carcinogenic in mice.
Mutagenesis
Buprenorphine was studied in a series of tests. Results were negative in Chinese hamster bone marrow and spermatogonia cells, and negative in mouse lymphoma L5178Y assay. Results were equivocal in the Ames test: negative in studies in two laboratories, but positive in frame shift mutation at high dose (5 mg/plate) in a third study.
Impairment of Fertility
Reproduction studies of buprenorphine in rats demonstrated no evidence of impaired fertility at daily oral doses up to 80 mg/kg (approximately 763 times the recommended human daily dose of 1.2 mg on a mg/m2 basis) or up to 5 mg/kg IM or SC (approximately 48 times the recommended human daily dose of 1.2 mg on a mg/m2 basis).
Pregnancy
Risk Summary
Prolonged use of opioid analgesics during pregnancy may cause neonatal opioid withdrawal syndrome [see WARNINGS: Neonatal Opioid Withdrawal Syndrome]. Available data with buprenorphine in pregnant women are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
Reproductive and developmental studies in rats and rabbits identified adverse events at approximately 2 times the maximum recommended human dose (MRHD) of 1.8 mg/day of buprenorphine. Embryofetal death was observed in both rats and rabbits administered buprenorphine during the period of organogenesis at doses approximately 54 and 2.2 times, respectively, the MRHD of 1.8 mg/day of buprenorphine. Pre-and postnatal development studies in rats demonstrated increased neonatal deaths at 2.7 times and above and dystocia at approximately 27 times the MRHD of 1.8 mg/day of buprenorphine. No clear teratogenic effects were seen when buprenorphine was administered during organogenesis with a range of doses 5 times or greater than the MRHD of 1.8 mg/day of buprenorphine. However, increases in skeletal abnormalities were noted in rats and rabbits administered buprenorphine daily during organogenesis at doses approximately 5.4 and 10.8 times the MRHD of 1.8 mg/day of buprenorphine, respectively. In a few studies, some events such as acephalus and omphalocele were also observed but these findings were not clearly treatment-related [see Data]. Based on animal data, advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Fetal/neonatal adverse reactions
Neonatal opioid withdrawal syndrome may occur in newborn infants of mothers who are receiving treatment with buprenorphine.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and/or failure to gain weight. Signs of neonatal withdrawal usually occur in the first days after birth. The duration and severity of neonatal opioid withdrawal syndrome may vary. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly [see WARNINGS: Neonatal Opioid Withdrawal Syndrome].
Labor and Delivery
The safety of buprenorphine hydrochloride given during labor and delivery has not been established. As with all opioids, use of buprenorphine hydrochloride prior to delivery may result in respiratory depression in the newborn.
Closely monitor neonates for signs of respiratory depression. An opioid antagonist such as naloxone should be available for reversal of opioid induced respiratory depression in the neonate.
Data
Human Data
Studies have been conducted to evaluate neonatal outcomes in women exposed to buprenorphine during pregnancy. Limited published data on malformations from trials, observational studies, case series, and case reports on buprenorphine use in pregnancy have not shown an increased risk of major malformations. Based on these studies the incidence of neonatal abstinence syndrome is not clear and there does not appear to be a dose-response relationship.
Animal Data
The exposure margins listed below are based on body surface area comparisons (mg/m2) to MRHD of 1.8 mg buprenorphine via buprenorphine hydrochloride injection.
Following oral administration to rats no teratogenic effects were observed at buprenorphine doses up to 250 mg/kg/day (estimated exposure approximately 1351 times the MRHD of 1.8 mg) in the presence of maternal toxicity (mortality). Following oral administration to rabbits, no teratogenic effects were observed at buprenorphine doses up to 40 mg/kg/day (estimated exposure approximately 432 times the MRHD of 1.8 mg) in the absence of clear maternal toxicity.
No definitive drug-related teratogenic effects were observed in rats and rabbits at IM doses up to 30 mg/kg/day (estimated exposure approximately 161 times and 324 times, respectively, the MRHD of 1.8 mg). Maternal toxicity resulting in mortality was noted in these studies in both rats and rabbits. Acephalus was observed in one rabbit fetus from the low-dose group and omphalocele was observed in two rabbit fetuses from the same litter in the mid-dose group; no findings were observed in fetuses from the high-dose group. Maternal toxicity was seen in the high-dose group but not at the lower doses where the findings were observed. Following oral administration of buprenorphine to rats, dose-related post-implantation losses, evidenced by increases in the numbers of early resorptions with consequent reductions in the numbers of fetuses, were observed at doses of 10 mg/kg/day or greater (estimated exposure approximately 54 times the MRHD of 1.8 mg).
In the rabbit, increased post-implantation losses occurred at an oral dose of 40 mg/kg/day. Following IM administration in the rat and the rabbit, post-implantation losses, as evidenced by decreases in live fetuses and increases in resorptions, occurred at 30 mg/kg/day.
Buprenorphine was not teratogenic in rats or rabbits after IM or subcutaneous (SC) doses up to 5 mg/kg/day (estimated exposure was approximately 27 and 54 times, respectively, the MRHD of 1.8 mg), after IV doses up to 0.8 mg/kg/day (estimated exposure was approximately 4.3 and 8.7 times, respectively, the MRHD of 1.8 mg), or after oral doses up to 160 mg/kg/day in rats (estimated exposure was approximately 865 times the MRHD of 1.8 mg) and 25 mg/kg/day in rabbits (estimated exposure was approximately 270 times the MRHD of 1.8 mg). Significant increases in skeletal abnormalities (e.g., extra thoracic vertebra or thoraco-lumbar ribs) were noted in rats after SC administration of 1 mg/kg/day and up (estimated exposure was approximately 5.4 times the MRHD of 1.8 mg), but were not observed at oral doses up to 160 mg/kg/day.
Increases in skeletal abnormalities in rabbits after IM administration of 5 mg/kg/day (estimated exposure was approximately 54 times the MRHD of 1.8 mg) in the absence of maternal toxicity or oral administration of 1 mg/kg/day or greater (estimated exposure was approximately 10.8 times the MRHD of 1.8 mg) were not statistically significant.
In rabbits, buprenorphine produced statistically significant pre-implantation losses at oral doses of 1 mg/kg/day or greater and post-implantation losses that were statistically significant at IV doses of 0.2 mg/kg/day or greater (estimated exposure approximately 2.2 times the MRHD of 1.8 mg). No maternal toxicity was noted at doses causing post-implantation loss in this study.
Dystocia was noted in pregnant rats treated intramuscularly with buprenorphine from Gestation Day 14 through Lactation Day 21 at 5 mg/kg/day (approximately 27 times the MRHD of 1.8 mg).
Fertility, pre-, and post-natal development studies with buprenorphine in rats indicated increases in neonatal mortality after oral doses of 0.8 mg/kg/day and up (approximately 4.3 times the MRHD of 1.8 mg), after IM doses of 0.5 mg/kg/day and up (approximately 2.7 times the MRHD of 1.8 mg), and after SC doses of 0.1 mg/kg/day and up (approximately 0.5 times the MRHD of 1.8 mg). An apparent lack of milk production during these studies likely contributed to the decreased pup viability and lactation indices. Delays in the occurrence of righting reflex and startle response were noted in rat pups at an oral dose of 80 mg/kg/day (approximately 432 times the MRHD of 1.8 mg).
Lactation
An apparent lack of milk production during general reproduction studies with buprenorphine in rats caused decreased viability and lactation indices. Use of high doses of sublingual buprenorphine in pregnant women showed that buprenorphine passes into the mother's milk. Breast-feeding is therefore not advised in nursing mothers treated with buprenorphine.
Females and Males of Reproductive Potential
Infertility
Chronic use of opioids may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see ADVERSE REACTIONS].
Pediatric Use
The safety and effectiveness of buprenorphine hydrochloride have been established for children between 2 and 12 years of age. Use of buprenorphine hydrochloride in children is supported by evidence from adequate and well controlled trials of buprenorphine hydrochloride in adults, with additional data from studies of 960 children ranging in age from 9 months to 18 years of age. Data is available from a pharmacokinetic study, several controlled clinical trials, and several large post-marketing studies and case series. The available information provides reasonable evidence that buprenorphine hydrochloride may be used safely in children ranging from 2 to 12 years of age, and that it is of similar effectiveness in children as in adults.
Geriatric Use
Elderly patients (aged 65 years or older) may have increased sensitivity to buprenorphine. In general, use caution when selecting a dosage for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of buprenorphine slowly in geriatric patients and monitor closely for signs of respiratory depression [see WARNINGS, PRECAUTIONS].
Buprenorphine is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
-
ADVERSE REACTIONS
The most frequent side effect in clinical studies involving 1,133 patients was sedation which occurred in approximately two-thirds of the patients. Although sedated, these patients could easily be aroused to an alert state.
Other less frequent adverse reactions occurring in 5 to 10% of the patients were:
Nausea
Dizziness/Vertigo
Occurring in 1 to 5% of the patients:
Sweating
Headache
Hypotension
Nausea/Vomiting
Vomiting
Hypoventilation
Miosis
The following adverse reactions were reported to have occurred in less than 1% of the patients:
CNS Effect:confusion, blurred vision, euphoria, weakness/fatigue, dry mouth, nervousness, depression, slurred speech, paresthesia.
Cardiovascular:hypertension, tachycardia, bradycardia.
Gastrointestinal:constipation.
Respiratory: dyspnea, cyanosis.
Dermatological: pruritus.
Ophthalmological: diplopia, visual abnormalities.
Miscellaneous:injection site reaction, urinary retention, dreaming, flushing/warmth, chills/cold, tinnitus, conjunctivitis, Wenckebach block, and psychosis.
Other effects observed infrequently include malaise, hallucinations, depersonalization, coma, dyspepsia, flatulence, apnea, rash, amblyopia, tremor, and pallor.
The following reactions have been reported to occur rarely: loss of appetite, dysphoria/agitation, diarrhea, urticaria, and convulsions/lack of muscle coordination.
Allergic Reactions: Cases of acute and chronic hypersensitivity to buprenorphine have been reported both in clinical trials and in the post-marketing experience of buprenorphine hydrochloride injection and other buprenorphine-containing products. The most common signs and symptoms include rashes, hives, and pruritus. Cases of bronchospasm, angioneurotic edema, and anaphylactic shock have been reported. A history of hypersensitivity to buprenorphine is a contraindication to buprenorphine hydrochloride.
In the United Kingdom, buprenorphine hydrochloride was made available under monitored release regulation during the first year of sale, and yielded data from 1,736 physicians on 9,123 patients (17,120 administrations). Data on 240 children under the age of 18 years were included in this monitored release program. No important new adverse effects attributable to buprenorphine hydrochloride were observed.
Postmarketing Experience
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Androgen deficiency: Cases of androgen deficiency have occurred with chronic use of opioids [see CLINICAL PHARMACOLOGY: Pharmacodynamics].
For medical advice about adverse reactions contact your medical professional. To report SUSPECTED ADVERSE REACTIONS, contact Par Pharmaceutical at 1-800-828-9393 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
DRUG ABUSE AND DEPENDENCE
Controlled Substance
Buprenorphine hydrochloride injection contains buprenorphine, a Schedule III controlled substance.
Abuse
Buprenorphine hydrochloride injection contains buprenorphine, a Schedule III controlled substance with an abuse potential similar to other Schedule III opioids. Buprenorphine can be abused and is subject to misuse, addiction and criminal diversion [see BOXED WARNING, WARNINGS, PRECAUTIONS].
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Prescription drug abuse is the intentional, non-therapeutic use of prescription drug, even once, for its rewarding psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and includes: a strong desire to take the drug, difficulties controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes physical withdrawal.
"Drug seeking" behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of the office hours, refusal to undergo appropriate examination, testing, or referral, repeated “loss” of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating healthcare providers. “Doctor shopping” (visiting multiple prescribers to obtain additional prescriptions) is common among drug abusers and people suffering from untreated addictions. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Healthcare providers should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
Buprenorphine, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity and frequency, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of Buprenorphine
Abuse of buprenorphine poses a risk of overdose and death. The risk is increased with concurrent abuse of buprenorphine with alcohol and other central nervous system depressants.
Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
Dependence
Both tolerance and physical dependence can develop during chronic therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dosage reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Buprenorphine should not be abruptly discontinued [see DOSAGE AND ADMINISTRATION]. If buprenorphine is abruptly discontinued in a physically-dependent patient, an abstinence a withdrawal syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including: irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy [see BOXED WARNING, WARNINGS: Neonatal Opioid Withdrawal Syndrome, PRECAUTIONS: Pregnancy].
-
OVERDOSAGE
Clinical Presentation
Acute overdose with buprenorphine can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations.
Treatment of Overdose
In the case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support techniques.
The opioid antagonists, naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to buprenorphine overdose, administer an opioid antagonist. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to buprenorphine overdose.
The healthcare provider must remember that buprenorphine is a long-acting depressant (36 to 48 hours), whereas the antagonists act for much shorter periods (one to three hours). Because the duration of opioid reversal is expected to be less than the duration of action of buprenorphine in buprenorphine hydrochloride injection, carefully monitor the patient until spontaneous respiration is reliably reestablished. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product's prescribing information.
In an individual physically dependent on opioids, the administration of the usual dose of an opioid antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be initiated with care and by titration with smaller than usual doses of the antagonist.
-
DOSAGE AND ADMINISTRATION
Use the lowest effective dosage for the shortest duration consistent with individual patients treatment goals [see WARNINGS].
Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see WARNINGS].
Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy and following dosage increases with buprenorphine and adjust the dosage accordingly [see WARNINGS].
Dosing
Adults and Pediatric Patients over 12 years of age
The initial starting dose is 1 mL buprenorphine hydrochloride (0.3 mg buprenorphine) given by deep intramuscular or slow (over at least 2 minutes) intravenous injection at up to 6-hour intervals, as needed.
Repeat once (up to 0.3 mg) if required, 30 to 60 minutes after initial dosage, giving consideration to previous dose pharmacokinetics, and thereafter only as needed. In high-risk patients (e.g., elderly, debilitated, presence of respiratory disease, etc.) and/or in patients where other CNS depressants are present, such as in the immediate postoperative period, the dose should be limited to the minimum required.
Extra caution should be exercised with the intravenous route of administration, particularly with the initial dose. Occasionally, it may be necessary to administer single doses of up to 0.6 mg to adults depending on the severity of the pain and the response of the patient. This dose should only be given IM and only to adult patients who are not in a high risk category [see WARNINGS and PRECAUTIONS]. At this time, there are insufficient data to recommend single doses greater than 0.6 mg for long-term use.
Pediatric Patients
Buprenorphine hydrochloride injection has been used in pediatric patients 2 to 12 years of age at doses between 2 to 6 micrograms/kg of body weight given every 4 to 6 hours. There is insufficient experience to recommend a dose in infants below the age of two years, single doses greater than 6 micrograms/kg of body weight, or the use of a repeat or second dose at 30 to 60 minutes (such as is used in adults). Since there is some evidence that not all pediatric patients clear buprenorphine faster than adults, fixed interval or "round-the-clock" dosing should not be undertaken until the proper inter-dose interval has been established by clinical observation of the child. Healthcare providers should recognize that, as with adults, some pediatric patients may not need to be remedicated for 6 to 8 hours.
Safety and Handling
Buprenorphine hydrochloride injection is supplied in sealed vials and poses no known environmental risk to healthcare providers. Accidental dermal exposure should be treated by removal of any contaminated clothing and rinsing the affected area with water.
Buprenorphine is a potent opioid and, like all drugs of this class, has been associated with abuse and dependence among healthcare providers. To control the risk of diversion, it is recommended that measures appropriate to the healthcare setting be taken to provide rigid accounting, control of wastage, and restriction of access.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- HOW SUPPLIED
- SPL UNCLASSIFIED SECTION
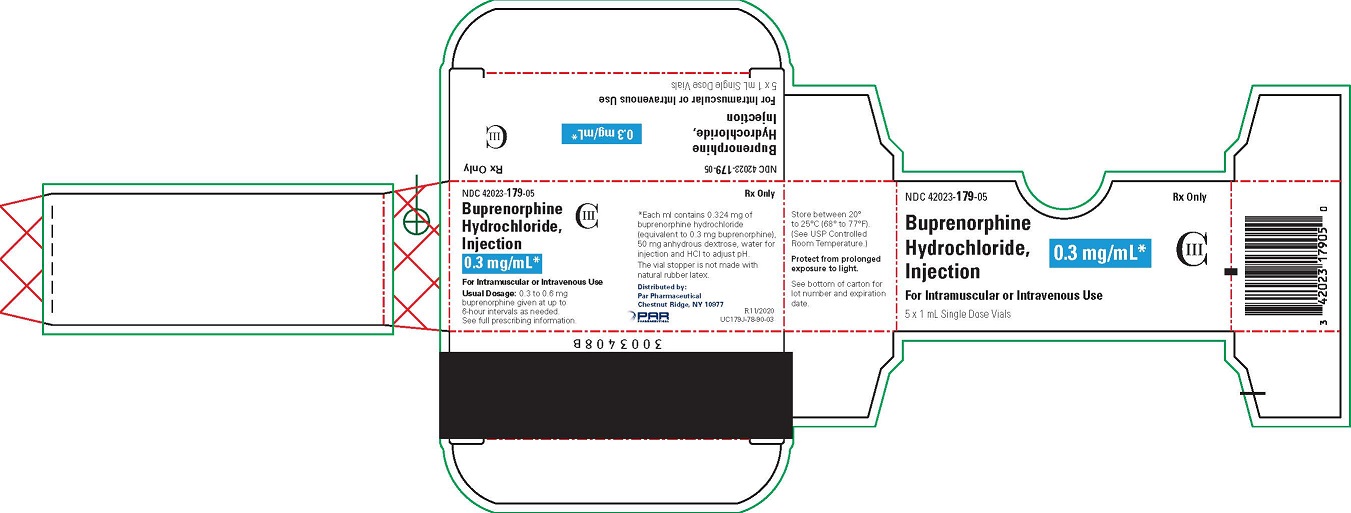
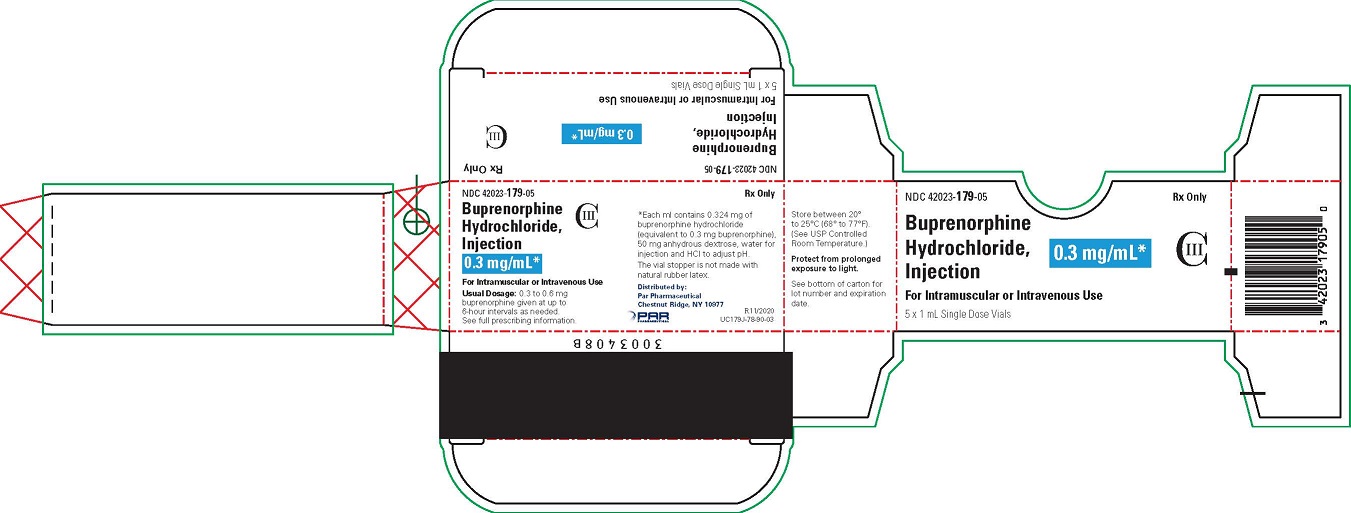
- PRINCIPAL DISPLAY PANEL - 0.3 mg/mL Vial Carton
-
INGREDIENTS AND APPEARANCE
BUPRENORPHINE HYDROCHLORIDE
buprenorphine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:42023-179 Route of Administration INTRAMUSCULAR, INTRAVENOUS DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BUPRENORPHINE HYDROCHLORIDE (UNII: 56W8MW3EN1) (BUPRENORPHINE - UNII:40D3SCR4GZ) BUPRENORPHINE 0.324 mg in 1 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS DEXTROSE (UNII: 5SL0G7R0OK) 50 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:42023-179-05 5 in 1 CARTON 07/30/2015 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA206586 07/30/2015 Labeler - Par Pharmaceutical, Inc. (092733690)