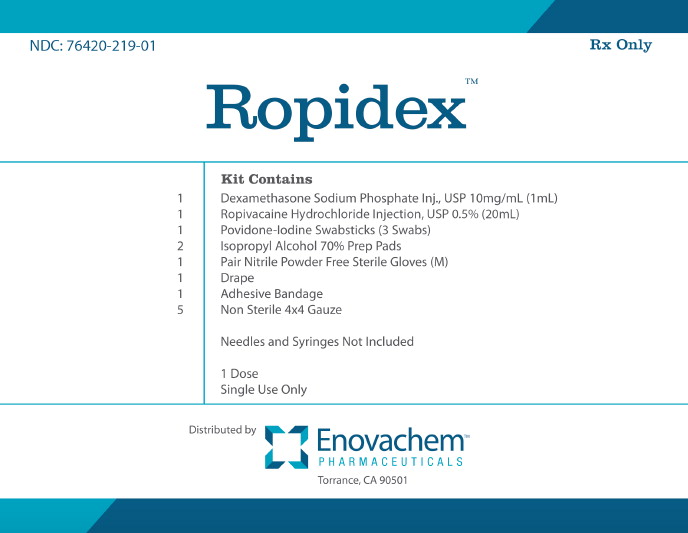
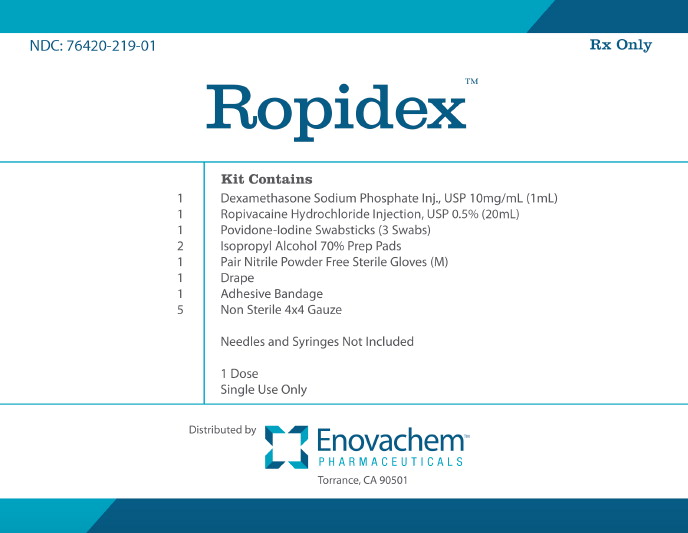
Label: ROPIDEX- dexamethasone sodium phosphate, ropivacaine hydrochloride, povidine iodine kit
- NDC Code(s): 55150-197-20, 63323-506-01, 67777-419-02, 76420-219-01
- Packager: Asclemed USA, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
DISCLAIMER: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here.
Drug Label Information
Updated September 22, 2020
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Dexamethasone Sodium Phosphate Injection, USP, is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly.
Dexamethasone Sodium Phosphate, USP chemically is Pregna-1,4-diene-3,20-dione, 9-fluoro- 11,17-dihydroxy-16-methyl-21-(phosphonooxy)-, disodium salt, (11ß, 16α).
It occurs as a white to creamy white powder, is exceedingly hygroscopic, is soluble in water and its solutions have a pH between 7.0 and 8.5. It has the following structural formula:
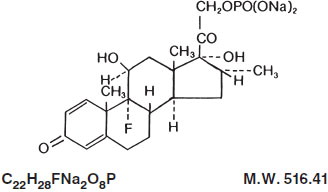
Each mL of Dexamethasone Sodium Phosphate Injection, USP (Preservative Free) contains dexamethasone sodium phosphate, USP equivalent to 10 mg dexamethasone phosphate; 24.75 mg sodium citrate, dihydrate; and Water for Injection, q.s. pH adjusted with citric acid or sodium hydroxide, if necessary. pH: 7.0 to 8.5.
-
CLINICAL PHARMACOLOGY
Dexamethasone sodium phosphate injection has a rapid onset but short duration of action when compared with less soluble preparations. Because of this, it is suitable for the treatment of acute disorders responsive to adrenocortical steroid therapy.
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, including dexamethasone, are primarily used for their potent anti-inflammatory effects in disorders of many organ systems.
Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli.
At equipotent anti-inflammatory doses, dexamethasone almost completely lacks the sodium-retaining property of hydrocortisone and closely related derivatives of hydrocortisone.
-
INDICATIONS AND USAGE
By intravenous or intramuscular injection when oral therapy is not feasible:
1. Endocrine Disorders
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; synthetic analogs may be used in conjunction with mineralocorticoids
where applicable; in infancy, mineralocorticoid supplementation is of particular importance).
Acute adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; mineralocorticoid supplementation may be necessary, particularly when synthetic analogs
are used).
Preoperatively, and in the event of serious trauma or illness, in patients with known adrenal insufficiency or when adrenocortical reserve is doubtful.
Shock unresponsive to conventional therapy if adrenocortical insufficiency exists or is suspected.
Congenital adrenal hyperplasia
Nonsuppurative thyroiditis
Hypercalcemia associated with cancer
2. Rheumatic Disorders
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Post-traumatic osteoarthritis
Synovitis of osteoarthritis
Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy).
Acute and subacute bursitis
Epicondylitis
Acute nonspecific tenosynovitis
Acute gouty arthritis
Psoriatic arthritis
Ankylosing spondylitis
3. Collagen Diseases
During an exacerbation or as maintenance therapy in selected cases of:
Systemic lupus erythematosus
Acute rheumatic carditis
4. Dermatologic Diseases
Pemphigus
Severe erythema multiforme (Stevens-Johnson syndrome)
Exfoliative dermatitis
Bullous dermatitis herpetiformis
Severe seborrheic dermatitis
Severe psoriasis
Mycosis fungoides
5. Allergic States
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in:
Bronchial asthma
Contact dermatitis
Atopic dermatitis
Serum sickness
Seasonal or perennial allergic rhinitis
Drug hypersensitivity reactions
Urticarial transfusion reactions
Acute noninfectious laryngeal edema (epinephrine is the drug of first choice).
6. Ophthalmic Diseases
Severe acute and chronic allergic and inflammatory processes involving the eye, such as:
Herpes zoster ophthalmicus
Iritis, iridocyclitis
Chorioretinitis
Diffuse posterior uveitis and choroiditis
Optic neuritis
Sympathetic ophthalmia
Anterior segment inflammation
Allergic conjunctivitis
Keratitis
Allergic corneal marginal ulcers
7. Gastrointestinal Diseases
To tide the patient over a critical period of the disease in:
Ulcerative colitis (systemic therapy)
Regional enteritis (systemic therapy)
8. Respiratory Diseases
Symptomatic sarcoidosis
Berylliosis
Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy.
Loeffler’s syndrome not manageable by other means.
Aspiration pneumonitis
9. Hematologic Disorders
Acquired (autoimmune) hemolytic anemia.
Idiopathic thrombocytopenic purpura in adults
(IV only; IM administration is contraindicated).
Secondary thrombocytopenia in adults
Erythroblastopenia (RBC anemia)
Congenital (erythroid) hypoplastic anemia
10. Neoplastic Diseases
For palliative management of:
Leukemias and lymphomas in adults
Acute leukemia of childhood
11. Edematous States
To induce diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
12. Miscellaneous
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy.
Trichinosis with neurologic or myocardial involvement.
13. Diagnostic testing of adrenocortical hyperfunction.
14. Cerebral Edema associated with primary or metastatic brain tumor, craniotomy, or head injury. Use in cerebral edema is not a substitute for careful neurosurgical evaluation
and definitive management such as neurosurgery or other specific therapy.
- CONTRAINDICATIONS
-
WARNINGS
Because rare instances of anaphylactoid reactions have occurred in patients receiving parenteral corticosteroid therapy, appropriate precautionary measures should be taken prior to administration, especially when the patient has a history of allergy to any drug. Anaphylactoid and hypersensitivity reactions have been reported for dexamethasone sodium phosphate injection (see ADVERSE REACTIONS).
Corticosteroids may exacerbate systemic fungal infections and, therefore, should not be used in the presence of such infections unless they are needed to control drug reactions due to amphotericin B. Moreover, there have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive failure.
In patients on corticosteroid therapy subjected to any unusual stress, increased dosage of rapidly acting corticosteroids before, during, and after the stressful situation is indicated.
Drug-induced secondary adrenocortical insufficiency may result from too rapid withdrawal of corticosteroids and may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. If the patient is receiving steroids already, dosage may have to be increased. Since mineralocorticoid secretion may be impaired, salt and/or a mineralocorticoid should be administered concurrently.
Corticosteroids may mask some signs of infection, and new infections may appear during their use. There may be decreased resistance and inability to localize infection when corticosteroids are used. Moreover, corticosteroids may affect the nitroblue-tetrazolium test for bacterial infection and produce false negative results.
In cerebral malaria, a double-blind trial has shown that the use of corticosteroids is associated with prolongation of coma and a higher incidence of pneumonia and gastrointestinal bleeding.
Corticosteroids may activate latent amebiasis. Therefore, it is recommended that latent or active amebiasis be ruled out before initiating corticosteroid therapy in any patient who has spent time in the tropics or in any patient with unexplained diarrhea.
Prolonged use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to fungi or viruses.
Average and large doses of cortisone or hydrocortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Administration of live virus vaccines, including smallpox, is contraindicated in individuals receiving immunosuppressive doses of corticosteroids. If inactivated viral or bacterial vaccines are administered to individuals receiving immunosuppressive doses of corticosteroids, the expected serum antibody response may not be obtained. However, immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy, e.g., for Addison’s disease.
Patients who are on drugs which suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in non-immune children or adults on corticosteroids. In such children or adults who have not had these diseases, particular care should be taken to avoid exposure. The risk of developing a disseminated infection varies among individuals and can be related to the dose, route and duration of corticosteroid administration as well as to the underlying disease. If exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If chickenpox develops, treatment with antiviral agents may be considered. If exposed to measles, prophylaxis with immune globulin (IG) may be indicated. (See the respective package inserts for VZIG and IG for complete prescribing information).
The use of dexamethasone sodium phosphate injection in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate antituberculous regimen.
If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary as reactivation of the disease may occur. During prolonged corticosteroid therapy, these patients should receive chemoprophylaxis.
Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
Serious Neurologic Adverse Reactions with Epidural Administration
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids has not been established, and corticosteroids are not approved for this use.
Usage in Pregnancy
Since adequate human reproduction studies have not been done with corticosteroids, use of these drugs in pregnancy or in women of childbearing potential requires that the anticipated benefits be weighed against the possible hazards to the mother and embryo or fetus. Infants born of mothers who have received substantial doses of corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Corticosteroids appear in breast milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other unwanted effects. Mothers taking pharmacologic doses of corticosteroids should be advised not to nurse.
-
PRECAUTIONS
This product, like many other steroid formulations, is sensitive to heat. Therefore, it should not be autoclaved when it is desirable to sterilize the exterior of the vial.
Following prolonged therapy, withdrawal of corticosteroids may result in symptoms of the corticosteroid withdrawal syndrome including fever, myalgia, arthralgia, and malaise. This may occur in patients even without evidence of adrenal insufficiency.
There is an enhanced effect of corticosteroids in patients with hypothyroidism and in those with cirrhosis.
Corticosteroids should be used cautiously in patients with ocular herpes simplex for fear of corneal perforation.
The lowest possible dose of corticosteroid should be used to control the condition under treatment, and when reduction in dosage is possible, the reduction must be gradual.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Aspirin should be used within caution in conjunction with corticosteroids in hypoprothrombinemia.
Steroids should be used with caution in nonspecific ulcerative colitis, if there is a probability of impending perforation, abscess, or other pyogenic infection, also in diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, renal insufficiency, hypertension, osteoporosis, and myasthenia gravis. Signs of peritoneal irritation following gastrointestinal perforation in patients receiving large doses of corticosteroids may be minimal or absent. Fat embolism has been reported as a possible complication of hypercortisonism.
When large doses are given, some authorities advise that antacids be administered between meals to help prevent peptic ulcer.
Steroids may increase or decrease motility and number of spermatozoa in some patients.
Phenytoin, phenobarbital, ephedrine, and rifampin may enhance the metabolic clearance of corticosteroids resulting in decreased blood levels and lessened physiologic activity, thus requiring adjustment in corticosteroid dosage. These interactions may interfere with dexamethasone suppression tests which should be interpreted with caution during administration of these drugs.
False negative results in the dexamethasone suppression test (DST) in patients being treated with indomethacin have been reported. Thus, results of the DST should be interpreted with caution in these patients.
The prothrombin time should be checked frequently in patients who are receiving corticosteroids and coumarin anticoagulants at the same time because of reports that corticosteroids have altered the response to these anticoagulants. Studies have shown that the usual effect produced by adding corticosteroids is inhibition of response to coumarins, although there have been some conflicting reports of potentiation not substantiated by studies.
When corticosteroids are administered concomitantly with potassium-depleting diuretics, patients should be observed closely for development of hypokalemia.
The slower rate of absorption by intramuscular administration should be recognized.
-
ADVERSE REACTIONS
Fluid and electrolyte disturbances:
Sodium retention
Fluid retention
Congestive heart failure in susceptible patients
Potassium loss
Hypokalemic alkalosis
Hypertension
Musculoskeletal:
Muscle weakness
Steroid myopathy
Loss of muscle mass
Osteoporosis
Vertebral compression fractures
Aseptic necrosis of femoral and humeral heads
Tendon rupture
Pathologic fracture of long bones
Gastrointestinal:
Peptic ulcer with possible subsequent perforation and hemorrhage
Perforation of the small and large bowel; particularly in patients with inflammatory
bowel disease
Pancreatitis
Abdominal distention
Ulcerative esophagitis
Dermatologic:
Impaired wound healing
Thin fragile skin
Petechiae and ecchymoses
Erythema
Increased sweating
May suppress reactions to skin tests
Burning or tingling, especially in the perineal area (after IV injection)
Other cutaneous reactions, such as allergic dermatitis, urticaria, angioneurotic edema
Neurologic:
Convulsions
Increased intracranial pressure with papilledema (pseudotumor cerebri) usually after
treatment
Vertigo
Headache
Psychic disturbances
Endocrine:
Menstrual irregularities
Development of cushingoid state
Suppression of growth in pediatric patients
Secondary adrenocortical and pituitary unresponsiveness, particularly in times of
stress, as in trauma, surgery, or illness
Decreased carbohydrate tolerance
Manifestations of latent diabetes mellitus
Increased requirements for insulin or oral hypoglycemic agents in diabetics
Hirsutism
Ophthalmic:
Posterior subcapsular cataracts
Increased intraocular pressure
Glaucoma
Exophthalmos
Retinopathy of prematurity
Metabolic:
Negative nitrogen balance due to protein catabolism
Cardiovascular:
Myocardial rupture following recent myocardial infarction (see WARNINGS)
Hypertrophic cardiomyopathy in low birth weight infants
Other:
Anaphylactoid or hypersensitivity reactions
Thromboembolism
Weight gain
Increased appetite
Nausea
Malaise
Hiccups
The following additional adverse reactions are related to parenteral corticosteroid therapy:
Hyperpigmentation or hypopigmentation
Subcutaneous and cutaneous atrophy
Sterile abscess
Charcot-like arthropathy
-
OVERDOSAGE
Reports of acute toxicity and/or death following overdosage of glucocorticoids are rare. In the event of overdosage, no specific antidote is available; treatment is supportive and symptomatic.
The oral LD 50 of dexamethasone in female mice was 6.5 g/kg. The intravenous LD 50 of dexamethasone sodium phosphate in female mice was 794 mg/kg.
-
DOSAGE AND ADMINISTRATION
Dexamethasone sodium phosphate injection, 10 mg/mL– For intravenous and intramuscular injection only.
Dexamethasone sodium phosphate injection can be given directly from the vial, or it can be added to Sodium Chloride Injection or Dextrose Injection and administered by intravenous drip.
Solutions used for intravenous administration or further dilution of this product should be preservative free when used in the neonate, especially the premature infant.
When it is mixed with an infusion solution, sterile precautions should be observed. Since infusion solutions generally do not contain preservatives, mixtures should be used within 24 hours.
DOSAGE REQUIREMENTS ARE VARIABLE AND MUST BE INDIVIDUALIZED ON THE BASIS OF THE DISEASE AND THE RESPONSE OF THE PATIENT.
Intravenous and Intramuscular Injection
The initial dosage of dexamethasone sodium phosphate injection varies from 0.5 to 9 mg a day depending on the disease being treated. In less severe diseases doses lower than 0.5 mg may suffice, while in severe diseases doses higher than 9 mg may be required.
The initial dosage should be maintained or adjusted until the patient’s response is satisfactory. If a satisfactory clinical response does not occur after a reasonable period of time, discontinue dexamethasone sodium phosphate injection and transfer the patient to other therapy.
After a favorable initial response, the proper maintenance dosage should be determined by decreasing the initial dosage in small amounts to the lowest dosage that maintains an adequate clinical response.
Patients should be observed closely for signs that might require dosage adjustment, including changes in clinical status resulting from remissions or exacerbations of the disease, individual drug responsiveness, and the effect of stress (e.g., surgery, infection, trauma). During stress it may be necessary to increase dosage temporarily.
If the drug is to be stopped after more than a few days of treatment, it usually should be withdrawn gradually.
When the intravenous route of administration is used, dosage usually should be the same as the oral dosage. In certain overwhelming, acute, life-threatening situations, however, administration in dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages. The slower rate of absorption by intramuscular administration should be recognized.
Shock
There is a tendency in current medical practice to use high (pharmacologic) doses of corticosteroids for the treatment of unresponsive shock. The following dosages of dexamethasone sodium phosphate injection have been suggested by various authors:
Author
Dosage
Cavanagh 1
3 mg/kg of body weight per 24 hours by constant intravenous infusion after an initial intravenous injection of 20 mg
Dietzman 2
2 to 6 mg/kg of body weight as a single intravenous injection
Frank 3
40 mg initially followed by repeat intravenous injection every 4 to 6 hours while shock persists
Oaks 4
40 mg initially followed by repeat intravenous injection every 2 to 6 hours while shock persists
Schumer 5
1 mg/kg of body weight as a single intravenous injection
Administration of high dose corticosteroid therapy should be continued only until the patient’s condition has stabilized and usually not longer than 48 to 72 hours.
Although adverse reactions associated with high dose, short-term corticosteroid therapy are uncommon, peptic ulceration may occur.
Cerebral Edema
Dexamethasone sodium phosphate injection is generally administered initially in a dosage of 10 mg intravenously followed by four mg every six hours intramuscularly until the symptoms of cerebral edema subside. Response is usually noted within 12 to 24 hours and dosage may be reduced after two to four days and gradually discontinued over a period of five to seven days. For palliative management of patients with recurrent or inoperable brain tumors, maintenance therapy with 2 mg two or three times a day may be effective.
Acute Allergic Disorders
In acute, self-limited allergic disorders or acute exacerbations of chronic allergic disorders, the following dosage schedule combining parenteral and oral therapy is suggested:
Dexamethasone sodium phosphate injection, first day, 4 or 8 mg intramuscularly.
Dexamethasone tablets, 0.75 mg: second and third days, 4 tablets in two divided doses each day; fourth day, 2 tablets in two divided doses; fifth and sixth days, 1 tablet each day; seventh day, no treatment; eighth day, follow-up visit.
This schedule is designed to ensure adequate therapy during acute episodes, while minimizing the risk of overdosage in chronic cases.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever the solution and container permit.
-
HOW SUPPLIED
Dexamethasone Sodium Phosphate Injection, USP (Preservative Free) equivalent to 10 mg dexamethasone phosphate, is supplied in a single dose vial as follows:
Product
No.
NDC
No.
Strength
Vial Size
500601
63323-506-01
10 mg per mL
1 mL vial, packaged in twenty-fives.
This container closure is not made with natural rubber latex.
-
REFERENCES
- Cavanagh, D.; Singh, K.B.: Endotoxin shock in pregnancy and abortion, in: “Corticosteroids in the Treatment of Shock”, Schumer, W.; Nyhus, L.M., Editors, Urbana, University of Illinois Press, 1970, pp. 86-96.
- Dietzman, R.H.; Ersek, R.A.; Bloch, J.M.; Lilleheir, R.C.: High-output, low-resistance gram-negative septic shock in man, Angiology 20: 691-700, Dec. 1969.
- Frank, E.: Clinical observations in shock and management (in: Shields, T.F., ed.: Symposium on current concepts and management of shock), J. Maine Med. Ass. 59: 195-200, Oct. 1968.
- Oaks, W. W.; Cohen, H.E.: Endotoxin shock in the geriatric patient, Geriat. 22: 120-130, Mar. 1967.
- Schumer, W.; Nyhus, L.M.: Corticosteroid effect on biochemical parameters of human oligemic shock, Arch. Surg. 100: 405-408, Apr. 1970.
- SPL UNCLASSIFIED SECTION
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Ropivacaine hydrochloride injection, USP contains ropivacaine hydrochloride which is a member of the amino amide class of local anesthetics. Ropivacaine hydrochloride injection, USP is a clear, colorless, sterile, isotonic solution free from visible particles that contains the enantiomerically pure drug substance, sodium chloride for isotonicity and water for injection. Sodium hydroxide and/or hydrochloric acid may be used for pH adjustment. It is administered parenterally.
Ropivacaine hydrochloride USP is chemically described as S-(-)-1-propyl-2’,6’-pipecoloxylidide hydrochloride monohydrate. The drug substance is a white crystalline powder, with the following structural formula:
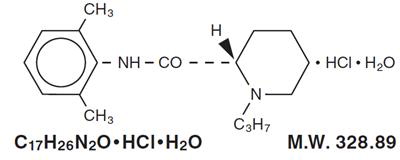
At 25°C ropivacaine hydrochloride has a solubility of 53.8 mg/mL in water, a distribution ratio between n-octanol and phosphate buffer at pH 7.4 of 14:1 and a pKa of 8.07 in 0.1 M KCl solution. The pKa of ropivacaine is approximately the same as bupivacaine (8.1) and is similar to that of mepivacaine (7.7). However, ropivacaine has an intermediate degree of lipid solubility compared to bupivacaine and mepivacaine.
Ropivacaine hydrochloride injection, USP is preservative-free and is available in single dose containers in 5 mg/mL (0.5%) concentrations. The specific gravity of ropivacaine hydrochloride injection, USP solutions range from 1.002 to 1.005 at 25°C.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Ropivacaine is a member of the amino amide class of local anesthetics and is supplied as the pure S-(-)-enantiomer. Local anesthetics block the generation and the conduction of nerve impulses, presumably by increasing the threshold for electrical excitation in the nerve, by slowing the propagation of the nerve impulse, and by reducing the rate of rise of the action potential. In general, the progression of anesthesia is related to the diameter, myelination and conduction velocity of affected nerve fibers. Clinically, the order of loss of nerve function is as follows: (1) pain, (2) temperature, (3) touch, (4) proprioception, and (5) skeletal muscle tone.
PHARMACOKINETICS
Absorption
The systemic concentration of ropivacaine is dependent on the total dose and concentration of drug administered, the route of administration, the patient’s hemodynamic/circulatory condition, and the vascularity of the administration site.
From the epidural space, ropivacaine shows complete and biphasic absorption. The half-lives of the 2 phases, (mean ± SD) are 14 ± 7 minutes and 4.2 ± 0.9 h, respectively. The slow absorption is the rate limiting factor in the elimination of ropivacaine that explains why the terminal half-life is longer after epidural than after intravenous administration. Ropivacaine shows dose-proportionality up to the highest intravenous dose studied, 80 mg, corresponding to a mean ± SD peak plasma concentration of 1.9 ± 0.3 mcg/mL.
Table 1 Pharmacokinetic (plasma concentration-time) data from clinical trials * Continuous 72 hour epidural infusion after an epidural block with 5 or 10 mg/mL.
† Epidural anesthesia with 7.5 mg/mL (0.75%) for cesarean delivery.
‡ Brachial plexus block with 7.5 mg/mL (0.75%) ropivacaine.
§ 20 minute IV infusion to volunteers (40 mg).
¶ Cmax measured at the end of infusion (i.e., at 72 hr).
# Cmax measured at the end of infusion (i.e., at 20 minutes).
♠ n/a=not applicable
♥ t1/2 is the true terminal elimination half-life. On the other hand, t1/2 follows absorption-dependent elimination (flip-flop) after non-intravenous administration.Route
Epidural Infusion *
Epidural Infusion *
Epidural Block †
Epidural Block †
Plexus Block ‡
IV Infusion §
Dose (mg)
1493±10
2075±206
1217±277
150
187.5
300
40
N
12
12
11
8
8
10
12
C max (mg/L)
2.4±1 ¶
2.8±0.5 ¶
2.3±1.1 ¶
1.1±0.2
1.6±0.6
2.3±0.8
1.2±0.2 #
T max (min)
n/a ♠
n/a
n/a
43±14
34±9
54±22
n/a
AUC 0-(mg.h/L)
135.5±50
145±34
161±90
7.2±2
11.3±4
13±3.3
1.8±0.6
CL (L/h)
11.03
13.7
n/a
5.5±2
5±2.6
n/a
21.2±7
t 1/2 (hr) ♥
5±2.5
5.7±3
6±3
5.7±2
7.1±3
6.8±3.2
1.9±0.5
In some patients after a 300 mg dose for brachial plexus block, free plasma concentrations of ropivacaine may approach the threshold for CNS toxicity (see PRECAUTIONS). At a dose of greater than 300 mg, for local infiltration, the terminal half-life may be longer (>30 hours).
Distribution
After intravascular infusion, ropivacaine has a steady-state volume of distribution of 41 ± 7 liters. Ropivacaine is 94% protein bound, mainly to α 1-acid glycoprotein. An increase in total plasma concentrations during continuous epidural infusion has been observed, related to a postoperative increase of α 1-acid glycoprotein. Variations in unbound, i.e., pharmacologically active, concentrations have been less than in total plasma concentration. Ropivacaine readily crosses the placenta and equilibrium in regard to unbound concentration will be rapidly reached (see PRECAUTIONS, Labor and Delivery).
Metabolism
Ropivacaine is extensively metabolized in the liver, predominantly by aromatic hydroxylation mediated by cytochrome P450 1A to 3-hydroxy ropivacaine. After a single IV dose approximately 37% of the total dose is excreted in the urine as both free and conjugated 3-hydroxy ropivacaine. Low concentrations of 3-hydroxy ropivacaine have been found in the plasma. Urinary excretion of the 4-hydroxy ropivacaine, and both the 3-hydroxy N-de-alkylated (3-OH-PPX) and 4-hydroxy N-de-alkylated (4-OH-PPX) metabolites account for less than 3% of the dose. An additional metabolite, 2-hydroxy-methyl-ropivacaine, has been identified but not quantified in the urine. The N-de-alkylated metabolite of ropivacaine (PPX) and 3-OH-ropivacaine are the major metabolites excreted in the urine during epidural infusion. Total PPX concentration in the plasma was about half as that of total ropivacaine; however, mean unbound concentrations of PPX were about 7 to 9 times higher than that of unbound ropivacaine following continuous epidural infusion up to 72 hours. Unbound PPX, 3-hydroxy and 4-hydroxy ropivacaine, have a pharmacological activity in animal models less than that of ropivacaine. There is no evidence of in vivo racemization in urine of ropivacaine.
Elimination
The kidney is the main excretory organ for most local anesthetic metabolites. In total, 86% of the ropivacaine dose is excreted in the urine after intravenous administration of which only 1% relates to unchanged drug. After intravenous administration ropivacaine has a mean ± SD total plasma clearance of 387 ± 107 mL/min, an unbound plasma clearance of 7.2 ± 1.6 L/min, and a renal clearance of 1 mL/min. The mean ± SD terminal half-life is 1.8 ± 0.7 h after intravascular administration and 4.2 ± 1 h after epidural administration (see Absorption).
Pharmacodynamics
Studies in humans have demonstrated that, unlike most other local anesthetics, the presence of epinephrine has no major effect on either the time of onset or the duration of action of ropivacaine. Likewise, addition of epinephrine to ropivacaine has no effect on limiting systemic absorption of ropivacaine.Systemic absorption of local anesthetics can produce effects on the central nervous and cardiovascular systems. At blood concentrations achieved with therapeutic doses, changes in cardiac conduction, excitability, refractoriness, contractility, and peripheral vascular resistance have been reported. Toxic blood concentrations depress cardiac conduction and excitability, which may lead to atrioventricular block, ventricular arrhythmias and to cardiac arrest, sometimes resulting in fatalities. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure.
Following systemic absorption, local anesthetics can produce central nervous system stimulation, depression or both. Apparent central stimulation is usually manifested as restlessness, tremors and shivering, progressing to convulsions, followed by depression and coma, progressing ultimately to respiratory arrest. However, the local anesthetics have a primary depressant effect on the medulla and on higher centers. The depressed stage may occur without a prior excited stage.
In 2 clinical pharmacology studies (total n=24) ropivacaine and bupivacaine were infused (10 mg/min) in human volunteers until the appearance of CNS symptoms, e.g., visual or hearing disturbances, perioral numbness, tingling and others. Similar symptoms were seen with both drugs. In 1 study, the mean ± SD maximum tolerated intravenous dose of ropivacaine infused (124 ± 38 mg) was significantly higher than that of bupivacaine (99 ± 30 mg) while in the other study the doses were not different (115 ± 29 mg of ropivacaine and 103 ± 30 mg of bupivacaine). In the latter study, the number of subjects reporting each symptom was similar for both drugs with the exception of muscle twitching which was reported by more subjects with bupivacaine than ropivacaine at comparable intravenous doses. At the end of the infusion, ropivacaine in both studies caused significantly less depression of cardiac conductivity (less QRS widening) than bupivacaine. Ropivacaine and bupivacaine caused evidence of depression of cardiac contractility, but there were no changes in cardiac output.
Clinical data in one published article indicate that differences in various pharmacodynamic measures were observed with increasing age. In one study, the upper level of analgesia increased with age, the maximum decrease of mean arterial pressure (MAP) declined with age during the first hour after epidural administration, and the intensity of motor blockade increased with age. However, no pharmacokinetic differences were observed between elderly and younger patients.
In non-clinical pharmacology studies comparing ropivacaine and bupivacaine in several animal species, the cardiac toxicity of ropivacaine was less than that of bupivacaine, although both were considerably more toxic than lidocaine. Arrhythmogenic and cardio-depressant effects were seen in animals at significantly higher doses of ropivacaine than bupivacaine. The incidence of successful resuscitation was not significantly different between the ropivacaine and bupivacaine groups.
Clinical Trials
Ropivacaine was studied as a local anesthetic both for surgical anesthesia and for acute pain management (see DOSAGE AND ADMINISTRATION). The onset, depth and duration of sensory block are, in general, similar to bupivacaine. However, the depth and duration of motor block, in general, are less than that with bupivacaine.
Epidural Administration In Surgery
There were 25 clinical studies performed in 900 patients to evaluate ropivacaine hydrochloride epidural injection for general surgery. Ropivacaine hydrochloride was used in doses ranging from 75 to 250 mg. In doses of 100 to 200 mg, the median (1st to 3rd quartile) onset time to achieve a T10 sensory block was 10 (5 to 13) minutes and the median (1st to 3rd quartile) duration at the T10 level was 4 (3 to 5) hours (see DOSAGE AND ADMINISTRATION). Higher doses produced a more profound block with a greater duration of effect.
Epidural Administration In Cesarean Section
A total of 12 studies were performed with epidural administration of ropivacaine hydrochloride for cesarean section. Eight of these studies involved 218 patients using the concentration of 5 mg/mL (0.5%) in doses up to 150 mg. Median onset measured at T6 ranged from 11 to 26 minutes. Median duration of sensory block at T6 ranged from 1.7 to 3.2 h, and duration of motor block ranged from 1.4 to 2.9 h. Ropivacaine hydrochloride provided adequate muscle relaxation for surgery in all cases.
In addition, 4 active controlled studies for cesarean section were performed in 264 patients at a concentration of 7.5 mg/mL (0.75%) in doses up to 187.5 mg. Median onset measured at T6 ranged from 4 to 15 minutes. Seventy-seven to 96% of ropivacaine hydrochloride-exposed patients reported no pain at delivery. Some patients received other anesthetic, analgesic, or sedative modalities during the course of the operative procedure.
Epidural Administration In Labor And Delivery
A total of 9 double-blind clinical studies, involving 240 patients were performed to evaluate ropivacaine hydrochloride for epidural block for management of labor pain. When administered in doses up to 278 mg as intermittent injections or as a continuous infusion, ropivacaine hydrochloride produced adequate pain relief.
A prospective meta-analysis on 6 of these studies provided detailed evaluation of the delivered newborns and showed no difference in clinical outcomes compared to bupivacaine. There were significantly fewer instrumental deliveries in mothers receiving ropivacaine as compared to bupivacaine.Table 2 LABOR AND DELIVERY META-ANALYSIS: MODE OF DELIVERY * p=0.004 versus bupivacaine Delivery Mode
Ropivacaine Hydrochloride
n=199
Bupivacaine
n=188
n
%
n
%
Spontaneous Vertex
116
58
92
49
Vacuum Extractor
26
33
}27*
}40
Forceps
28
42
Cesarean Section
29
15
21
11
Epidural Administration In Postoperative Pain Management
There were 8 clinical studies performed in 382 patients to evaluate ropivacaine hydrochloride 2 mg/mL (0.2%) for postoperative pain management after upper and lower abdominal surgery and after orthopedic surgery. The studies utilized intravascular morphine via PCA as a rescue medication and quantified as an efficacy variable.
Epidural anesthesia with ropivacaine hydrochloride 5 mg/mL, (0.5%) was used intraoperatively for each of these procedures prior to initiation of postoperative ropivacaine hydrochloride. The incidence and intensity of the motor block were dependent on the dose rate of ropivacaine hydrochloride and the site of injection. Cumulative doses of up to 770 mg of ropivacaine were administered over 24 hours (intraoperative block plus postoperative continuous infusion). The overall quality of pain relief, as judged by the patients, in the ropivacaine groups was rated as good or excellent (73% to 100%). The frequency of motor block was greatest at 4 hours and decreased during the infusion period in all groups. At least 80% of patients in the upper and lower abdominal studies and 42% in the orthopedic studies had no motor block at the end of the 21-hour infusion period. Sensory block was also dose rate-dependent and a decrease in spread was observed during the infusion period.
A double-blind, randomized, clinical trial compared lumbar epidural infusion of ropivacaine hydrochloride (n=26) and bupivacaine (n=26) at 2 mg/mL (8 mL/h), for 24 hours after knee replacement. In this study, the pain scores were higher in the ropivacaine hydrochloride group, but the incidence and the intensity of motor block were lower.
Continuous epidural infusion of ropivacaine hydrochloride 2 mg/mL (0.2%) during up to 72 hours for postoperative pain management after major abdominal surgery was studied in 2 multicenter, double-blind studies. A total of 391 patients received a low thoracic epidural catheter, and ropivacaine hydrochloride 7.5 mg/L (0.75%) was given for surgery, in combination with GA. Postoperatively, ropivacaine hydrochloride 2 mg/mL (0.2%), 4 to 14 mL/h, alone or with fentanyl 1, 2, or 4 mcg/mL was infused through the epidural catheter and adjusted according to the patient’s needs. These studies support the use of ropivacaine hydrochloride 2 mg/mL (0.2%) for epidural infusion at 6 to 14 mL/h (12 to 28 mg) for up to 72 hours and demonstrated adequate analgesia with only slight and nonprogressive motor block in cases of moderate to severe postoperative pain.
Clinical studies with 2 mg/mL (0.2%) ropivacaine hydrochloride have demonstrated that infusion rates of 6 to 14 mL (12 to 28 mg) per hour provide adequate analgesia with nonprogressive motor block in cases of moderate to severe postoperative pain. In these studies, this technique resulted in a significant reduction in patients’ morphine rescue dose requirement. Clinical experience supports the use of ropivacaine hydrochloride epidural infusions for up to 72 hours.
Peripheral Nerve Block
Ropivacaine hydrochloride, 5 mg/mL (0.5%), was evaluated for its ability to provide anesthesia for surgery using the techniques of Peripheral Nerve Block. There were 13 studies performed including a series of 4 pharmacodynamic and pharmacokinetic studies performed on minor nerve blocks. From these, 235 ropivacaine hydrochloride-treated patients were evaluable for efficacy. Ropivacaine hydrochloride was used in doses up to 275 mg. When used for brachial plexus block, onset depended on technique used. Supraclavicular blocks were consistently more successful than axillary blocks. The median onset of sensory block (anesthesia) produced by ropivacaine 0.5% via axillary block ranged from 10 minutes (medial brachial cutaneous nerve) to 45 minutes (musculocutaneous nerve). Median duration ranged from 3.7 hours (medial brachial cutaneous nerve) to 8.7 hours (ulnar nerve). The 5 mg/mL (0.5%) ropivacaine hydrochloride solution gave success rates from 56% to 86% for axillary blocks, compared with 92% for supraclavicular blocks.
In addition, ropivacaine hydrochloride, 7.5 mg/mL (0.75%), was evaluated in 99 ropivacaine hydrochloride-treated patients, in 2 double-blind studies, performed to provide anesthesia for surgery using the techniques of Brachial Plexus Block. Ropivacaine hydrochloride 7.5 mg/mL was compared to bupivacaine 5 mg/mL. In 1 study, patients underwent axillary brachial plexus block using injections of 40 mL (300 mg) of ropivacaine hydrochloride, 7.5 mg/mL (0.75%) or 40 mL injections of bupivacaine, 5 mg/mL (200 mg). In a second study, patients underwent subclavian perivascular brachial plexus block using 30 mL (225 mg) of ropivacaine hydrochloride, 7.5 mg/mL (0.75%) or 30 mL of bupivacaine 5 mg/mL (150 mg). There was no significant difference between the ropivacaine hydrochloride and bupivacaine groups in either study with regard to onset of anesthesia, duration of sensory blockade, or duration of anesthesia.
The median duration of anesthesia varied between 11.4 and 14.4 hours with both techniques. In one study, using the axillary technique, the quality of analgesia and muscle relaxation in the ropivacaine hydrochloride group was judged to be significantly superior to bupivacaine by both investigator and surgeon. However, using the subclavian perivascular technique, no statistically significant difference was found in the quality of analgesia and muscle relaxation as judged by both the investigator and surgeon. The use of ropivacaine hydrochloride 7.5 mg/mL for block of the brachial plexus via either the subclavian perivascular approach using 30 mL (225 mg) or via the axillary approach using 40 mL (300 mg) both provided effective and reliable anesthesia.
Local Infiltration
A total of 7 clinical studies were performed to evaluate the local infiltration of ropivacaine hydrochloride to produce anesthesia for surgery and analgesia in postoperative pain management. In these studies 297 patients who received ropivacaine hydrochloride in doses up to 200 mg (concentrations up to 5 mg/mL, 0.5%) were evaluable for efficacy. With infiltration of 100 to 200 mg ropivacaine hydrochloride, the time to first request for analgesic was 2 to 6 hours. When compared to placebo, ropivacaine hydrochloride produced lower pain scores and a reduction of analgesic consumption. -
INDICATIONS AND USAGE
Ropivacaine hydrochloride injection, USP is indicated for the production of local or regional anesthesia for surgery and for acute pain management.
Surgical Anesthesia: epidural block for surgery including cesarean section; major nerve block; local infiltration
Acute Pain Management: epidural continuous infusion or intermittent bolus, e.g., postoperative or labor; local infiltration - CONTRAINDICATIONS
-
WARNINGS
In performing ropivacaine hydrochloride blocks, unintended intravenous injection is possible and may result in cardiac arrhythmia or cardiac arrest. The potential for successful resuscitation has not been studied in humans. There have been rare reports of cardiac arrest during the use of ropivacaine hydrochloride for epidural anesthesia or peripheral nerve blockade, the majority of which occurred after unintentional accidental intravascular administration in elderly patients and in patients with concomitant heart disease. In some instances, resuscitation has been difficult. Should cardiac arrest occur, prolonged resuscitative efforts may be required to improve the probability of a successful outcome.
Ropivacaine hydrochloride should be administered in incremental doses. It is not recommended for emergency situations, where a fast onset of surgical anesthesia is necessary. Historically, pregnant patients were reported to have a high risk for cardiac arrhythmias, cardiac/circulatory arrest and death when 0.75% bupivacaine (another member of the amino amide class of local anesthetics) was inadvertently rapidly injected intravenously.
Prior to receiving major blocks the general condition of the patient should be optimized and the patient should have an IV line inserted. All necessary precautions should be taken to avoid intravascular injection. Local anesthetics should only be administered by clinicians who are well versed in the diagnosis and management of dose-related toxicity and other acute emergencies which might arise from the block to be employed, and then only after insuring the immediate (without delay) availability of oxygen, other resuscitative drugs, cardiopulmonary resuscitative equipment, and the personnel resources needed for proper management of toxic reactions and related emergencies (see also ADVERSE REACTIONS, PRECAUTIONS and MANAGEMENT OF LOCAL ANESTHETIC EMERGENCIES). Delay in proper management of dose-related toxicity, underventilation from any cause, and/or altered sensitivity may lead to the development of acidosis, cardiac arrest and, possibly, death. Solutions of ropivacaine hydrochloride should not be used for the production of obstetrical paracervical block anesthesia, retrobulbar block, or spinal anesthesia (subarachnoid block) due to insufficient data to support such use. Intravenous regional anesthesia (bier block) should not be performed due to a lack of clinical experience and the risk of attaining toxic blood levels of ropivacaine.
Intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric and adult patients following intra-articular infusions of local anesthetics with and without epinephrine for periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are not associated with these findings. The time of onset of symptoms, such as joint pain, stiffness and loss of motion can be variable, but may begin as early as the 2 nd month after surgery. Currently, there is no effective treatment for chondrolysis; patients who experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
It is essential that aspiration for blood, or cerebrospinal fluid (where applicable), be done prior to injecting any local anesthetic, both the original dose and all subsequent doses, to avoid intravascular or subarachnoid injection. However, a negative aspiration does not ensure against an intravascular or subarachnoid injection.
A well-known risk of epidural anesthesia may be an unintentional subarachnoid injection of local anesthetic. Two clinical studies have been performed to verify the safety of ropivacaine hydrochloride at a volume of 3 mL injected into the subarachnoid space since this dose represents an incremental epidural volume that could be unintentionally injected. The 15 and 22.5 mg doses injected resulted in sensory levels as high as T5 and T4, respectively. Anesthesia to pinprick started in the sacral dermatomes in 2 to 3 minutes, extended to the T10 level in 10 to 13 minutes and lasted for approximately 2 hours. The results of these two clinical studies showed that a 3 mL dose did not produce any serious adverse events when spinal anesthesia blockade was achieved.
Ropivacaine hydrochloride should be used with caution in patients receiving other local anesthetics or agents structurally related to amide-type local anesthetics, since the toxic effects of these drugs are additive.
Patients treated with class III antiarrhythmic drugs (e.g., amiodarone) should be under close surveillance and ECG monitoring considered, since cardiac effects may be additive.
Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure, and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue ropivacaine hydrochloride and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. -
PRECAUTIONS
General
The safe and effective use of local anesthetics depends on proper dosage, correct technique, adequate precautions and readiness for emergencies.
Resuscitative equipment, oxygen and other resuscitative drugs should be available for immediate use (see WARNINGS and ADVERSE REACTIONS). The lowest dosage that results in effective anesthesia should be used to avoid high plasma levels and serious adverse events. Injections should be made slowly and incrementally, with frequent aspirations before and during the injection to avoid intravascular injection. When a continuous catheter technique is used, syringe aspirations should also be performed before and during each supplemental injection. During the administration of epidural anesthesia, it is recommended that a test dose of a local anesthetic with a fast onset be administered initially and that the patient be monitored for central nervous system and cardiovascular toxicity, as well as for signs of unintended intrathecal administration before proceeding. When clinical conditions permit, consideration should be given to employing local anesthetic solutions, which contain epinephrine for the test dose because circulatory changes compatible with epinephrine may also serve as a warning sign of unintended intravascular injection. An intravascular injection is still possible even if aspirations for blood are negative. Administration of higher than recommended doses of ropivacaine hydrochloride to achieve greater motor blockade or increased duration of sensory blockade may result in cardiovascular depression, particularly in the event of inadvertent intravascular injection. Tolerance to elevated blood levels varies with the physical condition of the patient. Debilitated, elderly patients and acutely ill patients should be given reduced doses commensurate with their age and physical condition. Local anesthetics should also be used with caution in patients with hypotension, hypovolemia or heart block.
Careful and constant monitoring of cardiovascular and respiratory vital signs (adequacy of ventilation) and the patient’s state of consciousness should be performed after each local anesthetic injection. It should be kept in mind at such times that restlessness, anxiety, incoherent speech, light-headedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, depression, or drowsiness may be early warning signs of central nervous system toxicity. Because amide-type local anesthetics such as ropivacaine are metabolized by the liver, these drugs, especially repeat doses, should be used cautiously in patients with hepatic disease. Patients with severe hepatic disease, because of their inability to metabolize local anesthetics normally, are at a greater risk of developing toxic plasma concentrations. Local anesthetics should also be used with caution in patients with impaired cardiovascular function because they may be less able to compensate for functional changes associated with the prolongation of A-V conduction produced by these drugs.
Many drugs used during the conduct of anesthesia are considered potential triggering agents for malignant hyperthermia (MH). Amide-type local anesthetics are not known to trigger this reaction. However, since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for MH management should be available.
Epidural Anesthesia
During epidural administration, ropivacaine hydrochloride should be administered in incremental doses of 3 to 5 mL with sufficient time between doses to detect toxic manifestations of unintentional intravascular or intrathecal injection. Syringe aspirations should also be performed before and during each supplemental injection in continuous (intermittent) catheter techniques. An intravascular injection is still possible even if aspirations for blood are negative. During the administration of epidural anesthesia, it is recommended that a test dose be administered initially and the effects monitored before the full dose is given. When clinical conditions permit, the test dose should contain an appropriate dose of epinephrine to serve as a warning of unintentional intravascular injection. If injected into a blood vessel, this amount of epinephrine is likely to produce a transient “epinephrine response” within 45 seconds, consisting of an increase in heart rate and systolic blood pressure, circumoral pallor, palpitations and nervousness in the unsedated patient. The sedated patient may exhibit only a pulse rate increase of 20 or more beats per minute for 15 or more seconds. Therefore, following the test dose, the heart should be continuously monitored for a heart rate increase. Patients on beta-blockers may not manifest changes in heart rate, but blood pressure monitoring can detect a rise in systolic blood pressure. A test dose of a short-acting amide anesthetic such as lidocaine is recommended to detect an unintentional intrathecal administration. This will be manifested within a few minutes by signs of spinal block (e.g., decreased sensation of the buttocks, paresis of the legs, or, in the sedated patient, absent knee jerk). An intravascular or subarachnoid injection is still possible even if results of the test dose are negative. The test dose itself may produce a systemic toxic reaction, high spinal or epinephrine-induced cardiovascular effects.
Use in Brachial Plexus Block
Ropivacaine plasma concentrations may approach the threshold for central nervous system toxicity after the administration of 300 mg of ropivacaine for brachial plexus block. Caution should be exercised when using the 300 mg dose (see OVERDOSAGE).
The dose for a major nerve block must be adjusted according to the site of administration and patient status. Supraclavicular brachial plexus blocks may be associated with a higher frequency of serious adverse reactions, regardless of the local anesthetic used.
Use in Peripheral Nerve Block
Major peripheral nerve blocks may result in the administration of a large volume of local anesthetic in highly vascularized areas, often close to large vessels where there is an increased risk of intravascular injection and/or rapid systemic absorption, which can lead to high plasma concentrations.
Use in Head and Neck Area
Small doses of local anesthetics injected into the head and neck area may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. The injection procedures require the utmost care. Confusion, convulsions, respiratory depression, and/or respiratory arrest, and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded (see DOSAGE AND ADMINISTRATION).
Use in Ophthalmic Surgery
The use of ropivacaine hydrochloride in retrobulbar blocks for ophthalmic surgery has not been studied. Until appropriate experience is gained, the use of ropivacaine hydrochloride for such surgery is not recommended.Information for Patients
When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity in the anesthetized part of the body following proper administration of lumbar epidural anesthesia. Also, when appropriate, the physician should discuss other information including adverse reactions in the ropivacaine hydrochloride package insert.
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.Drug Interactions
Specific trials studying the interaction between ropivacaine and class III antiarrhythmic drugs (e.g., amiodarone) have not been performed, but caution is advised (see WARNINGS).
Ropivacaine hydrochloride should be used with caution in patients receiving other local anesthetics or agents structurally related to amide-type local anesthetics, since the toxic effects of these drugs are additive. Cytochrome P4501A2 is involved in the formation of 3-hydroxy ropivacaine, the major metabolite. In vivo, the plasma clearance of ropivacaine was reduced by 70% during coadministration of fluvoxamine (25 mg bid for 2 days), a selective and potent CYP1A2 inhibitor. Thus strong inhibitors of cytochrome P4501A2, such as fluvoxamine, given concomitantly during administration of ropivacaine hydrochloride, can interact with ropivacaine hydrochloride leading to increased ropivacaine plasma levels. Caution should be exercised when CYP1A2 inhibitors are coadministered. Possible interactions with drugs known to be metabolized by CYP1A2 via competitive inhibition such as theophylline and imipramine may also occur. Coadministration of a selective and potent inhibitor of CYP3A4, ketoconazole (100 mg bid for 2 days with ropivacaine infusion administered 1 hour after ketoconazole) caused a 15% reduction in in vivo plasma clearance of ropivacaine.
Patients who are administered local anesthetics are at increased risk of developing methemoglobinemia when concurrently exposed to the following drugs, which could include other local anesthetics:
Examples of Drugs Associated with Methemoglobinemia:Class
Examples
Nitrates/Nitrites
nitric oxide, nitroglycerin, nitroprusside, nitrous oxide
Local anesthetics
articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine
Antineoplastic agents
cyclophosphamide, flutamide, hydroxyurea, ifosfamide, rasburicase
Antibiotics
dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides
Antimalarials
chloroquine, primaquine
Anticonvulsants
Phenobarbital, phenytoin, sodium valproate
Other drugs
acetaminophen, metoclopramide, quinine, sulfasalazine
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals of most local anesthetics, including ropivacaine, to evaluate the carcinogenic potential have not been conducted.
Weak mutagenic activity was seen in the mouse lymphoma test. Mutagenicity was not noted in the other assays, demonstrating that the weak signs of in vitro activity in the mouse lymphoma test were not manifest under diverse in vivo conditions.
Studies performed with ropivacaine in rats did not demonstrate an effect on fertility or general reproductive performance over 2 generations.Pregnancy Category B
Reproduction toxicity studies have been performed in pregnant New Zealand white rabbits and Sprague-Dawley rats. During gestation days 6 to 18, rabbits received 1.3, 4.2, or 13 mg/kg/day subcutaneously. In rats, subcutaneous doses of 5.3, 11 and 26 mg/kg/day were administered during gestation days 6 to 15. No teratogenic effects were observed in rats and rabbits at the highest doses tested. The highest doses of 13 mg/kg/day (rabbits) and 26 mg/kg/day (rats) are approximately 1/3 of the maximum recommended human dose (epidural, 770 mg/24 hours) based on a mg/m 2 basis. In 2 prenatal and postnatal studies, the female rats were dosed daily from day 15 of gestation to day 20 postpartum. The doses were 5.3, 11 and 26 mg/kg/day subcutaneously. There were no treatment-related effects on late fetal development, parturition, lactation, neonatal viability, or growth of the offspring.
In another study with rats, the males were dosed daily for 9 weeks before mating and during mating. The females were dosed daily for 2 weeks before mating and then during the mating, pregnancy, and lactation, up to day 42 post coitus. At 23 mg/kg/day, an increased loss of pups was observed during the first 3 days postpartum. The effect was considered secondary to impaired maternal care due to maternal toxicity.
There are no adequate or well-controlled studies in pregnant women of the effects of ropivacaine hydrochloride on the developing fetus. Ropivacaine hydrochloride should only be used during pregnancy if the benefits outweigh the risk.
Teratogenicity studies in rats and rabbits did not show evidence of any adverse effects on organogenesis or early fetal development in rats (26 mg/kg sc) or rabbits (13 mg/kg). The doses used were approximately equal to total daily dose based on body surface area. There were no treatment-related effects on late fetal development, parturition, lactation, neonatal viability, or growth of the offspring in 2 perinatal and postnatal studies in rats, at dose levels equivalent to the maximum recommended human dose based on body surface area. In another study at 23 mg/kg, an increased pup loss was seen during the first 3 days postpartum, which was considered secondary to impaired maternal care due to maternal toxicity.Labor and Delivery
Local anesthetics, including ropivacaine, rapidly cross the placenta, and when used for epidural block can cause varying degrees of maternal, fetal and neonatal toxicity (see CLINICAL PHARMACOLOGY and PHARMACOKINETICS). The incidence and degree of toxicity depend upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus and neonate involve alterations of the central nervous system, peripheral vascular tone and cardiac function.
Maternal hypotension has resulted from regional anesthesia with ropivacaine hydrochloride for obstetrical pain relief. Local anesthetics produce vasodilation by blocking sympathetic nerves. Elevating the patient’s legs and positioning her on her left side will help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously, and electronic fetal monitoring is highly advisable. Epidural anesthesia has been reported to prolong the second stage of labor by removing the patient’s reflex urge to bear down or by interfering with motor function. Spontaneous vertex delivery occurred more frequently in patients receiving ropivacaine hydrochloride than in those receiving bupivacaine.Nursing Mothers
Some local anesthetic drugs are excreted in human milk and caution should be exercised when they are administered to a nursing woman. The excretion of ropivacaine or its metabolites in human milk has not been studied. Based on the milk/plasma concentration ratio in rats, the estimated daily dose to a pup will be about 4% of the dose given to the mother. Assuming that the milk/plasma concentration in humans is of the same order, the total ropivacaine hydrochloride dose to which the baby is exposed by breast-feeding is far lower than by exposure in utero in pregnant women at term (see PRECAUTIONS).
Pediatric Use
The safety and efficacy of ropivacaine hydrochloride in pediatric patients have not been established.
Geriatric Use
Of the 2,978 subjects that were administered ropivacaine hydrochloride injection in 71 controlled and uncontrolled clinical studies, 803 patients (27%) were 65 years of age or older which includes 127 patients (4%) 75 years of age and over. Ropivacaine hydrochloride injection was found to be safe and effective in the patients in these studies. Clinical data in one published article indicate that differences in various pharmacodynamic measures were observed with increasing age. In one study, the upper level of analgesia increased with age, the maximum decrease of mean arterial pressure (MAP) declined with age during the first hour after epidural administration, and the intensity of motor blockade increased with age.
This drug and its metabolites are known to be excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Elderly patients are more likely to have decreased hepatic, renal, or cardiac function, as well as concomitant disease. Therefore, care should be taken in dose selection, starting at the low end of the dosage range, and it may be useful to monitor renal function (see PHARMACOKINETICS, Elimination). -
ADVERSE REACTIONS
Reactions to ropivacaine are characteristic of those associated with other amide-type local anesthetics. A major cause of adverse reactions to this group of drugs may be associated with excessive plasma levels, which may be due to overdosage, unintentional intravascular injection or slow metabolic degradation.
The reported adverse events are derived from clinical studies conducted in the U.S. and other countries. The reference drug was usually bupivacaine. The studies used a variety of premedications, sedatives, and surgical procedures of varying length. A total of 3,988 patients have been exposed to ropivacaine hydrochloride at concentrations up to 1% in clinical trials. Each patient was counted once for each type of adverse event.
Incidence ≥ 5%
For the indications of epidural administration in surgery, cesarean section, postoperative pain management, peripheral nerve block, and local infiltration, the following treatment-emergent adverse events were reported with an incidence of ≥5% in all clinical studies (N=3988): hypotension (37%), nausea (24.8%), vomiting (11.6%), bradycardia (9.3%), fever (9.2%), pain (8%), postoperative complications (7.1%), anemia (6.1%), paresthesia (5.6%), headache (5.1%), pruritus (5.1%), and back pain (5%).
Incidence 1 to 5%
Urinary retention, dizziness, rigors, hypertension, tachycardia, anxiety, oliguria, hypoesthesia, chest pain, hypokalemia, dyspnea, cramps, and urinary tract infection.
Incidence in Controlled Clinical Trials
The reported adverse events are derived from controlled clinical studies with ropivacaine hydrochloride (concentrations ranged from 0.125% to 1% for ropivacaine hydrochloride and 0.25% to 0.75% for bupivacaine) in the U.S. and other countries involving 3,094 patients. Table 3A and 3B list adverse events (number and percentage) that occurred in at least 1% of ropivacaine hydrochloride-treated patients in these studies. The majority of patients receiving concentrations higher than 5 mg/mL (0.5%) were treated with ropivacaine hydrochloride.
Table 3A
Adverse Events Reported in ≥1% of Adult Patients Receiving Regional or Local Anesthesia (Surgery, Labor, Cesarean Section, Postoperative Pain Management, Peripheral Nerve Block and Local Infiltration) Adverse Reaction
Ropivacaine Hydrochloride
total N=1661
Bupivacaine
total N=1433
N
(%)
N
(%)
Hypotension
536
(32.3)
408
(28.5)
Nausea
283
(17)
207
(14.4)
Vomiting
117
(7)
88
(6.1)
Bradycardia
96
(5.8)
73
(5.1)
Headache
84
(5.1)
68
(4.7)
Paresthesia
82
(4.9)
57
(4)
Back pain
73
(4.4)
75
(5.2)
Pain
71
(4.3)
71
(5)
Pruritus
63
(3.8)
40
(2.8)
Fever
61
(3.7)
37
(2.6)
Dizziness
42
(2.5)
23
(1.6)
Rigors (Chills)
42
(2.5)
24
(1.7)
Postoperative complications
41
(2.5)
44
(3.1)
Hypoesthesia
27
(1.6)
24
(1.7)
Urinary retention
23
(1.4)
20
(1.4)
Progression of labor poor/failed
23
(1.4)
22
(1.5)
Anxiety
21
(1.3)
11
(0.8)
Breast disorder, breast-feeding
21
(1.3)
12
(0.8)
Rhinitis
18
(1.1)
13
(0.9)
Table 3B
Adverse Events Reported in ≥1% of Fetuses or Neonates of Mothers Who Received Regional Anesthesia (Cesarean Section and Labor Studies) Adverse Reaction
Ropivacaine Hydrochloride
total N=639
Bupivacaine
total N=573
N
(%)
N
(%)
Fetal bradycardia
77
(12.1)
68
(11.9)
Neonatal jaundice
49
(7.7)
47
(8.2)
Neonatal complication-NOS
42
(6.6)
38
(6.6)
Apgar score low
18
(2.8)
14
(2.4)
Neonatal respiratory disorder
17
(2.7)
18
(3.1)
Neonatal tachypnea
14
(2.2)
15
(2.6)
Neonatal fever
13
(2)
14
(2.4)
Fetal tachycardia
13
(2)
12
(2.1)
Fetal distress
11
(1.7)
10
(1.7)
Neonatal infection
10
(1.6)
8
(1.4)
Neonatal hypoglycemia
8
(1.3)
16
(2.8)
Incidence <1%
The following adverse events were reported during the ropivacaine hydrochloride clinical program in more than one patient (N=3988), occurred at an overall incidence of <1%, and were considered relevant:
Application Site Reactions – injection site pain
Cardiovascular System – vasovagal reaction, syncope, postural hypotension, non-specific ECG abnormalities
Female Reproductive – poor progression of labor, uterine atony
Gastrointestinal System – fecal incontinence, tenesmus, neonatal vomiting
General and Other Disorders – hypothermia, malaise, asthenia, accident and/or injury
Hearing and Vestibular – tinnitus, hearing abnormalities
Heart Rate and Rhythm – extrasystoles, non-specific arrhythmias, atrial fibrillation
Liver and Biliary System – jaundice
Metabolic Disorders – hypomagnesemia
Musculoskeletal System – myalgia
Myo/Endo/Pericardium – ST segment changes, myocardial infarction
Nervous System – tremor, Horner’s syndrome, paresis, dyskinesia, neuropathy, vertigo, coma, convulsion, hypokinesia, hypotonia, ptosis, stupor
Psychiatric Disorders – agitation, confusion, somnolence, nervousness, amnesia, hallucination, emotional lability, insomnia, nightmares
Respiratory System – bronchospasm, coughing
Skin Disorders – rash, urticaria
Urinary System Disorders – urinary incontinence, micturition disorder
Vascular – deep vein thrombosis, phlebitis, pulmonary embolism
Vision – vision abnormalities
For the indication epidural anesthesia for surgery, the 15 most common adverse events were compared between different concentrations of ropivacaine hydrochloride and bupivacaine. Table 4 is based on data from trials in the U.S. and other countries where ropivacaine hydrochloride was administered as an epidural anesthetic for surgery.
Table 4
Common Events (Epidural Administration) Adverse Reaction
Ropivacaine Hydrochloride
Bupivacaine
5 mg/mL
total N=256
7.5 mg/mL
total N=297
10 mg/mL
total N=207
5 mg/mL
total N=236
7.5 mg/mL
total N=174
N
(%)
N
(%)
N
(%)
N
(%)
N
(%)
hypotension
99
(38.7)
146
(49.2)
113
(54.6)
91
(38.6)
89
(51.1)
nausea
34
(13.3)
68
(22.9)
41
(17.4)
36
(20.7)
bradycardia
29
(11.3)
58
(19.5)
40
(19.3)
32
(13.6)
25
(14.4)
back pain
18
(7)
23
(7.7)
34
(16.4)
21
(8.9)
23
(13.2)
vomiting
18
(7)
33
(11.1)
23
(11.1)
19
(8.1)
14
(8)
headache
12
(4.7)
20
(6.7)
16
(7.7)
13
(5.5)
9
(5.2)
fever
8
(3.1)
5
(1.7)
18
(8.7)
11
(4.7)
chills
6
(2.3)
7
(2.4)
6
(2.9)
4
(1.7)
3
(1.7)
urinary retention
5
(2)
8
(2.7)
10
(4.8)
10
(4.2)
paresthesia
5
(2)
10
(3.4)
5
(2.4)
7
(3)
pruritus
14
(4.7)
3
(1.4)
7
(4)
Using data from the same studies, the number (%) of patients experiencing hypotension is displayed by patient age, drug and concentration in Table 5. In Table 6, the adverse events for ropivacaine hydrochloride are broken down by gender.
Table 5
Effects of Age on Hypotension (Epidural Administration) Total N: Ropivacaine Hydrochloride = 760, Bupivacaine = 410 AGE
Ropivacaine Hydrochloride
Bupivacaine
5 mg/mL
7.5 mg/mL
10 mg/mL
5 mg/mL
7.5 mg/mL
N
(%)
N
(%)
N
(%)
N
(%)
N
(%)
<65
68
(32.2)
99
(43.2)
87
(51.5)
64
(33.5)
73
(48.3)
≥65
31
(68.9)
47
(69.1)
26
(68.4)
27
(60)
16
(69.6)
Table 6
Most Common Adverse Events by Gender (Epidural Administration) Total N: Females = 405, Males = 355 Adverse Reaction
Female
Male
N
(%)
N
(%)
hypotension
220
(54.3)
138
(38.9)
nausea
119
(29.4)
23
(6.5)
bradycardia
65
(16)
56
(15.8)
vomiting
59
(14.6)
8
(2.3)
back pain
41
(10.1)
23
(6.5)
headache
33
(8.1)
17
(4.8)
chills
18
(4.4)
5
(1.4)
fever
16
(4)
3
(0.8)
pruritus
16
(4)
1
(0.3)
pain
12
(3)
4
(1.1)
urinary retention
11
(2.7)
7
(2)
dizziness
9
(2.2)
4
(1.1)
hypoesthesia
8
(2)
2
(0.6)
paresthesia
8
(2)
10
(2.8)
Systemic Reactions
The most commonly encountered acute adverse experiences that demand immediate countermeasures are related to the central nervous system and the cardiovascular system. These adverse experiences are generally dose-related and due to high plasma levels that may result from overdosage, rapid absorption from the injection site, diminished tolerance or from unintentional intravascular injection of the local anesthetic solution. In addition to systemic dose-related toxicity, unintentional subarachnoid injection of drug during the intended performance of lumbar epidural block or nerve blocks near the vertebral column (especially in the head and neck region) may result in underventilation or apnea (“Total or High Spinal”). Also, hypotension due to loss of sympathetic tone and respiratory paralysis or underventilation due to cephalad extension of the motor level of anesthesia may occur. This may lead to secondary cardiac arrest if untreated. Factors influencing plasma protein binding, such as acidosis, systemic diseases that alter protein production or competition with other drugs for protein binding sites, may diminish individual tolerance.
Epidural administration of ropivacaine hydrochloride has, in some cases, as with other local anesthetics, been associated with transient increases in temperature to >38.5°C. This occurred more frequently at doses of ropivacaine hydrochloride >16 mg/h.
Neurologic Reactions
These are characterized by excitation and/or depression. Restlessness, anxiety, dizziness, tinnitus, blurred vision or tremors may occur, possibly proceeding to convulsions. However, excitement may be transient or absent, with depression being the first manifestation of an adverse reaction. This may quickly be followed by drowsiness merging into unconsciousness and respiratory arrest. Other central nervous system effects may be nausea, vomiting, chills, and constriction of the pupils.
The incidence of convulsions associated with the use of local anesthetics varies with the route of administration and the total dose administered. In a survey of studies of epidural anesthesia, overt toxicity progressing to convulsions occurred in approximately 0.1% of local anesthetic administrations.
The incidence of adverse neurological reactions associated with the use of local anesthetics may be related to the total dose and concentration of local anesthetic administered and are also dependent upon the particular drug used, the route of administration, and the physical status of the patient. Many of these observations may be related to local anesthetic techniques, with or without a contribution from the drug. During lumbar epidural block, occasional unintentional penetration of the subarachnoid space by the catheter or needle may occur. Subsequent adverse effects may depend partially on the amount of drug administered intrathecally as well as the physiological and physical effects of a dural puncture. These observations may include spinal block of varying magnitude (including high or total spinal block), hypotension secondary to spinal block, urinary retention, loss of bladder and bowel control (fecal and urinary incontinence), and loss of perineal sensation and sexual function. Signs and symptoms of subarachnoid block typically start within 2 to 3 minutes of injection. Doses of 15 and 22.5 mg of ropivacaine hydrochloride resulted in sensory levels as high as T5 and T4, respectively. Analgesia started in the sacral dermatomes in 2 to 3 minutes and extended to the T10 level in 10 to 13 minutes and lasted for approximately 2 hours. Other neurological effects following unintentional subarachnoid administration during epidural anesthesia may include persistent anesthesia, paresthesia, weakness, paralysis of the lower extremities, and loss of sphincter control; all of which may have slow, incomplete or no recovery. Headache, septic meningitis, meningismus, slowing of labor, increased incidence of forceps delivery, or cranial nerve palsies due to traction on nerves from loss of cerebrospinal fluid have been reported (see DOSAGE AND ADMINISTRATION discussion of Lumbar Epidural Block). A high spinal is characterized by paralysis of the arms, loss of consciousness, respiratory paralysis and bradycardia.
Cardiovascular System Reactions
High doses or unintentional intravascular injection may lead to high plasma levels and related depression of the myocardium, decreased cardiac output, heart block, hypotension, bradycardia, ventricular arrhythmias, including ventricular tachycardia and ventricular fibrillation, and possibly cardiac arrest (see WARNINGS, PRECAUTIONS, and OVERDOSAGE).
Allergic Reactions
Allergic type reactions are rare and may occur as a result of sensitivity to the local anesthetic (see WARNINGS). These reactions are characterized by signs such as urticaria, pruritus, erythema, angioneurotic edema (including laryngeal edema), tachycardia, sneezing, nausea, vomiting, dizziness, syncope, excessive sweating, elevated temperature, and possibly, anaphylactoid symptomatology (including severe hypotension). Cross-sensitivity among members of the amide-type local anesthetic group has been reported. The usefulness of screening for sensitivity has not been definitively established. -
OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered, or large doses administered, during therapeutic use of local anesthetics or to unintended subarachnoid or intravascular injection of local anesthetic solution (see ADVERSE REACTIONS, WARNINGS, and PRECAUTIONS).
MANAGEMENT OF LOCAL ANESTHETIC EMERGENCIES
Therapy with ropivacaine hydrochloride should be discontinued at the first sign of toxicity. No specific information is available for the treatment of toxicity with ropivacaine hydrochloride; therefore, treatment should be symptomatic and supportive. The first consideration is prevention, best accomplished by incremental injection of ropivacaine hydrochloride, careful and constant monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic and during continuous infusion. At the first sign of change in mental status, oxygen should be administered.
The first step in the management of systemic toxic reactions, as well as underventilation or apnea due to unintentional subarachnoid injection of drug solution, consists of immediate attention to the establishment and maintenance of a patent airway and effective assisted or controlled ventilation with 100% oxygen with a delivery system capable of permitting immediate positive airway pressure by mask. Circulation should be assisted as necessary. This may prevent convulsions if they have not already occurred.
If necessary, use drugs to control convulsions. Intravenous barbiturates, anticonvulsant agents, or muscle relaxants should only be administered by those familiar with their use. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated. Supportive treatment of circulatory depression may require administration of intravenous fluids, and, when appropriate, a vasopressor dictated by the clinical situation (such as ephedrine or epinephrine to enhance myocardial contractile force).
Should cardiac arrest occur, prolonged resuscitative efforts may be required to improve the probability of a successful outcome.
The mean dosages of ropivacaine producing seizures, after intravenous infusion in dogs, nonpregnant and pregnant sheep were 4.9, 6.1 and 5.9 mg/kg, respectively. These doses were associated with peak arterial total plasma concentrations of 11.4, 4.3 and 5 mcg/mL, respectively.
In human volunteers given intravenous ropivacaine hydrochloride, the mean (min-max) maximum tolerated total and free arterial plasma concentrations were 4.3 (3.4 to 5.3) and 0.6 (0.3 to 0.9) mcg/mL respectively, at which time moderate CNS symptoms (muscle twitching) were noted.
Clinical data from patients experiencing local anesthetic induced convulsions demonstrated rapid development of hypoxia, hypercarbia and acidosis within a minute of the onset of convulsions. These observations suggest that oxygen consumption and carbon dioxide production are greatly increased during local anesthetic convulsions and emphasize the importance of immediate and effective ventilation with oxygen which may avoid cardiac arrest.
If difficulty is encountered in the maintenance of a patent airway or if prolonged ventilatory support (assisted or controlled) is indicated, endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated after initial administration of oxygen by mask.
The supine position is dangerous in pregnant women at term because of aortocaval compression by the gravid uterus. Therefore, during treatment of systemic toxicity, maternal hypotension or fetal bradycardia following regional block, the parturient should be maintained in the left lateral decubitus position if possible, or manual displacement of the uterus off the great vessels should be accomplished. Resuscitation of obstetrical patients may take longer than resuscitation of non-pregnant patients and closed-chest cardiac compression may be ineffective. Rapid delivery of the fetus may improve the response to resuscitative efforts. -
DOSAGE AND ADMINISTRATION
The rapid injection of a large volume of local anesthetic solution should be avoided and fractional (incremental) doses should always be used. The smallest dose and concentration required to produce the desired result should be administered.
There have been adverse event reports of chondrolysis in patients receiving intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures. Ropivacaine hydrochloride injection is not approved for this use (see WARNINGS and DOSAGE AND ADMINISTRATION).
The dose of any local anesthetic administered varies with the anesthetic procedure, the area to be anesthetized, the vascularity of the tissues, the number of neuronal segments to be blocked, the depth of anesthesia and degree of muscle relaxation required, the duration of anesthesia desired, individual tolerance, and the physical condition of the patient. Patients in poor general condition due to aging or other compromising factors such as partial or complete heart conduction block, advanced liver disease or severe renal dysfunction require special attention although regional anesthesia is frequently indicated in these patients. To reduce the risk of potentially serious adverse reactions, attempts should be made to optimize the patient’s condition before major blocks are performed, and the dosage should be adjusted accordingly.
Use an adequate test dose (3 mL to 5 mL of a short acting local anesthetic solution containing epinephrine) prior to induction of complete block. This test dose should be repeated if the patient is moved in such a fashion as to have displaced the epidural catheter. Allow adequate time for onset of anesthesia following administration of each test dose.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Solutions which are discolored or which contain particulate matter should not be administered.Table 7 Dosage Recommendations * = Not Applicable
† = The dose for a major nerve block must be adjusted according to site of administration and patient status. Supraclavicular brachial plexus blocks may be associated with a higher frequency of serious adverse reactions, regardless of the local anesthetic used (see PRECAUTIONS).
‡ = Median dose of 21 mg per hour was administered by continuous infusion or by incremental injections (top-ups) over a median delivery time of 5.5 hours.
§ = Cumulative doses up to 770 mg of ropivacaine hydrochloride over 24 hours (intraoperative block plus postoperative infusion); Continuous epidural infusion at rates up to 28 mg per hour for 72 hours have been well tolerated in adults, i.e., 2016 mg plus surgical dose of approximately 100 mg to 150 mg as top-up.
Conc.
Volume
mL
Dose
mg
Onset
min
Duration
hours
mg/mL
(%)
SURGICAL ANESTHESIA
Lumbar Epidural
5
(0.5%)
15 to 30
75 to 150
15 to 30
2 to 4
Administration
7.5
(0.75%)
15 to 25
113 to 188
10 to 20
3 to 5
Surgery
10
(1%)
15 to 20
150 to 200
10 to 20
4 to 6
Lumbar Epidural
5
(0.5%)
20 to 30
100 to 150
15 to 25
2 to 4
Administration
7.5
(0.75%)
15 to 20
113 to 150
10 to 20
3 to 5
Cesarean Section
Thoracic Epidural
5
(0.5%)
5 to 15
25 to 75
10 to 20
n/a *
Administration
7.5
(0.75%)
5 to 15
38 to 113
10 to 20
n/a *
Surgery
Major Nerve Block †
5
(0.5%)
35 to 50
175 to 250
15 to 30
5 to 8
(e.g., brachial plexus block)
7.5
(0.75%)
10 to 40
75 to 300
10 to 25
6 to 10
Field Block
5
(0.5%)
1 to 40
5 to 200
1 to 15
2 to 6
(e.g., minor nerve blocks and infiltration)
LABOR PAIN MANAGEMENT
Lumbar Epidural Administration
Initial Dose
2
(0.2%)
10 to 20
20 to 40
10 to 15
0.5 to 1.5
Continuous infusion ‡
2
(0.2%)
6 to 14 mL/h
12 to 28 mg/h
n/a *
n/a *
Incremental injections (top-up) ‡
2
(0.2%)
10 to 15 mL/h
20 to 30 mg/h
n/a *
n/a *
POSTOPERATIVE PAIN MANAGEMENT
Lumbar Epidural Administration
Continuous infusion §
2
(0.2%)
6 to 14 mL/h
12 to 28 mg/h
n/a*
n/a*
Thoracic Epidural Administration
2
(0.2%)
6 to 14 mL/h
12 to 28 mg/h
n/a*
n/a*
Continuous infusion §
Infiltration
2
(0.2%)
1 to 100
2 to 200
1 to 5
2 to 6
(e.g., minor nerve block)
5
(0.5%)
1 to 40
5 to 200
1 to 5
2 to 6
The doses in the table are those considered to be necessary to produce a successful block and should be regarded as guidelines for use in adults. Individual variations in onset and duration occur. The figures reflect the expected average dose range needed. For other local anesthetic techniques standard current textbooks should be consulted.
When prolonged blocks are used, either through continuous infusion or through repeated bolus administration, the risks of reaching a toxic plasma concentration or inducing local neural injury must be considered. Experience to date indicates that a cumulative dose of up to 770 mg ropivacaine hydrochloride injection administered over 24 hours is well tolerated in adults when used for postoperative pain management: i.e., 2016 mg. Caution should be exercised when administering ropivacaine hydrochloride injection for prolonged periods of time, e.g., >70 hours in debilitated patients.
For treatment of postoperative pain, the following technique can be recommended: If regional anesthesia was not used intraoperatively, then an initial epidural block with 5 mL to 7 mL ropivacaine hydrochloride injection is induced via an epidural catheter. Analgesia is maintained with an infusion of ropivacaine hydrochloride injection, 2 mg/mL (0.2%). Clinical studies have demonstrated that infusion rates of 6 mL to 14 mL (12 mg to 28 mg) per hour provide adequate analgesia with nonprogressive motor block. With this technique a significant reduction in the need for opioids was demonstrated. Clinical experience supports the use of ropivacaine hydrochloride epidural infusions for up to 72 hours.
-
HOW SUPPLIED
Ropivacaine hydrochloride injection, USP is a clear, colorless, sterile, isotonic solution free from visible particles and is supplied as follows:
Ropivacaine hydrochloride injection USP, 0.5 %
100 mg/20 mL (5 mg/mL): 20 mL Single Dose Vials
in a Carton of 25 NDC 55150-197-20
The solubility of ropivacaine is limited at pH above 6. Thus, care must be taken as precipitation may occur if ropivacaine hydrochloride injection, USP is mixed with alkaline solutions.
Disinfecting agents containing heavy metals, which cause release of respective ions (mercury, zinc, copper, etc.) should not be used for skin or mucous membrane disinfection since they have been related to incidents of swelling and edema.
When chemical disinfection of the container surface is desired, either isopropyl alcohol (91%) or ethyl alcohol (70%) is recommended. It is recommended that chemical disinfection be accomplished by wiping the vial stopper thoroughly with cotton or gauze that has been moistened with the recommended alcohol just prior to use. Glass containers may, as an alternative, be autoclaved once. Stability has been demonstrated using a targeted F 0 of 7 minutes at 121°C.
Solutions should be stored at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
The vial stoppers are not made with natural rubber latex.
These products are intended for single dose and are free from preservatives. Any solution remaining from an opened container should be discarded promptly. In addition, continuous infusion bottles should not be left in place for more than 24 hours.
Distributed by:
AuroMedics Pharma LLC
279 Princeton-Hightstown Rd.
E. Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma LimitedHyderabad - 500038
India
Revised: March 2019 - SPL UNCLASSIFIED SECTION
- Povidone Iodine Swabsticks
- ACTIVE INGREDIENT
- Purpose:
- Warnings:
- Do not use:
- Ask a doctor before use if you have:
- Stop Use:
- Keep Out Of Reach Of Children
- Directions Povidone iodine:
- Other information:
- INDICATIONS & USAGE
- Inactive Ingredients
-
Principal Display Panel - Ropidex Kit Label
NDC: 76420-219-01 RX Only
Ropidex™
Kit Contains
1 Dexamethasone Sodium Phosphate Inj., USP 10mg/mL (1mL)
1 Ropivacaine Hydrochloride Injection, USP 0.5% (20mL)
1 Povidone-Iodine Swabsticks (3 Swabs)
2 Isopropyl Alcohol 70% Prep Pads
1 Pair Nitrile Powder Free Sterile Gloves (M)
1 Drape
1 Adhesive Bandage
5 Non Sterile 4x4 Gauze
Needles and Syringes Not Included
1 Dose
Single Use Only
Distributed by
Enovachem™
PHARMACEUTICALS
Torrance, CA 90501
-
INGREDIENTS AND APPEARANCE
ROPIDEX
dexamethasone sodium phosphate, ropivacaine hydrochloride, povidine iodine kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:76420-219 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:76420-219-01 1 in 1 CARTON; Type 1: Convenience Kit of Co-Package 06/10/2019 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 VIAL 1 mL Part 2 1 VIAL, SINGLE-DOSE 20 mL Part 3 1 PACKET 0.9 mL Part 1 of 3 DEXAMETHASONE SODIUM PHOSPHATE
dexamethasone sodium phosphate injection, solutionProduct Information Item Code (Source) NDC:63323-506 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DEXAMETHASONE SODIUM PHOSPHATE (UNII: AI9376Y64P) (DEXAMETHASONE - UNII:7S5I7G3JQL) DEXAMETHASONE PHOSPHATE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CITRATE (UNII: 1Q73Q2JULR) 24.75 mg in 1 mL CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63323-506-01 25 in 1 TRAY 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040491 05/29/2003 Part 2 of 3 ROPIVACAINE HYDROCHLORIDE
ropivacaine hydrochloride injection, solutionProduct Information Item Code (Source) NDC:55150-197 Route of Administration INFILTRATION, PERINEURAL, EPIDURAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ROPIVACAINE HYDROCHLORIDE (UNII: V910P86109) (ROPIVACAINE - UNII:7IO5LYA57N) ROPIVACAINE HYDROCHLORIDE 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55150-197-20 25 in 1 CARTON 1 20 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205612 09/15/2016 Part 3 of 3 POVIDINE IODINE
povidine iodine swabProduct Information Item Code (Source) NDC:67777-419 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength POVIDONE-IODINE (UNII: 85H0HZU99M) (IODINE - UNII:9679TC07X4) IODINE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) POLYSORBATE 80 (UNII: 6OZP39ZG8H) SODIUM CITRATE (UNII: 1Q73Q2JULR) SODIUM PHOSPHATE, DIBASIC, ANHYDROUS (UNII: 22ADO53M6F) CITRIC ACID ACETATE (UNII: DSO12WL7AU) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:67777-419-02 0.9 mL in 1 PACKET; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date OTC monograph final part333C 09/13/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 06/10/2019 Labeler - Asclemed USA, Inc. (059888437)