Label: OXCARBAZEPINE tablet, extended release
- NDC Code(s): 27241-237-01, 27241-238-01, 27241-239-01
- Packager: Ajanta Pharma USA Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 17, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OXCARBAZEPINE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for OXCARBAZEPINE EXTENDED-RELEASE TABLETS.
OXCARBAZEPINE extended-release tablets, for oral use
Initial U.S. Approval: 2000
INDICATIONS AND USAGE
Oxcarbazepine extended-release tablets are indicated for the treatment of partial-onset seizures in patients 6 years of age and older (1)
DOSAGE AND ADMINISTRATION
- Adult Patients: The recommended initial dosage is 600 mg once per day. Increase the dosage in weekly increments of 600 mg once per day, based on clinical response and tolerability, to a recommended maintenance dosage of 1,200 mg to 2,400 mg once per day. (2.2)
- In adult patients with a creatinine clearance < 30 mL/min, initiate at one-half the usual starting dosage and increase slowly (2.3)
- Pediatric Patients: The recommended dosage is based on body weight and is administered orally once per day. Increase the dosage in weekly intervals based on clinical response and tolerability, to the recommended dosage (2.2).
- Geriatric Patients: Start at lower dosage (300 mg or 450 mg/day) and increase slowly (2.4)
- In conversion of oxcarbazepine immediate-release to oxcarbazepine extended-release tablets, higher dosages of oxcarbazepine extended-release tablets may be necessary (2.7, 12.3)
DOSAGE FORMS AND STRENGTHS
Extended-release tablets: 150 mg, 300 mg and 600 mg (3)
CONTRAINDICATIONS
Known hypersensitivity to oxcarbazepine, any of the components of oxcarbazepine extended-release tablets, or to eslicarbazepine acetate (4)
WARNINGS AND PRECAUTIONS
- Hyponatremia: Monitor sodium as recommended. (5.1)
- Cross Hypersensitivity Reaction to Carbamazepine: Discontinue immediately if hypersensitivity occurs (5.3)
- Serious Dermatological Reactions: Discontinue if observed (5.4)
- Suicidal Behavior and Ideation: Monitor for symptoms (5.5)
- Withdrawal of Oxcarbazepine Extended-Release Tablets: Withdrawal gradually (5.6)
- Drug Reaction with Eosinophilia and Systemic symptoms (DRESS)/Multi-Organ Hypersensitivity: Discontinue if suspected (5.7)
- Hematologic Reactions: Discontinue if suspected (5.8)
- Risk of Seizure Aggravation: Discontinue if occurs (5.10)
ADVERSE REACTIONS
Most commonly observed (≥ 5% and more frequent than placebo) adverse reactions in adults were dizziness, somnolence, headache, balance disorder, tremor, vomiting, diplopia, asthenia, and fatigue (6.1).
Adverse reactions in pediatric patients are similar to those seen in adult patients.
To report SUSPECTED ADVERSE REACTIONS, contact Ajanta Pharma USA Inc. at 855-664-7744 or contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
-
Phenytoin, Carbamazepine, and Phenobarbital:
Coadministration decreased blood levels of an active metabolite of oxcarbazepine extended-release tablets: Greater dosage of oxcarbazepine extended-release tablets may be required (2.5, 7.2). - Oral Contraceptives: Advise patients that oxcarbazepine extended-release tablets may decrease the effectiveness of hormonal contraceptives. Additional non-hormonal forms of contraception are recommended. (7.3)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 General Dosing Recommendations
2.3 Dosage Modifications in Adult Patients with Renal Impairment
2.4 Dosage Modifications in Geriatric Patients
2.5 Dosage Modification with Concomitant Use of Strong CYP3A4 Enzyme Inducers or UGT Enzyme Inducers
2.6 Withdrawal of AEDs
2.7 Conversion from Immediate-Release Oxcarbazepine to Oxcarbazepine Extended-Release Tablets
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hyponatremia
5.2 Anaphylactic Reactions and Angioedema
5.3 Cross Hypersensitivity Reaction to Carbamazepine
5.4 Serious Dermatological Reactions
5.5 Suicidal Behavior and Ideation
5.6 Withdrawal of AEDs
5.7 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity
5.8 Hematologic Reactions
5.9 Risk of Seizures in the Pregnant Patient
5.10 Risk of Seizure Aggravation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing and Other Experience
7 DRUG INTERACTIONS
7.1 Effect of Oxcarbazepine Extended-Release Tablets on Other Drugs
7.2 Effect of Other Drugs on Oxcarbazepine Extended-Release Tablets
7.3 Hormonal Contraceptives
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
10.1 Human Overdose Experience
10.2 Treatment and Management
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Oxcarbazepine Extended-Release Tablets Primary Trial
14.2 Immediate-Release Oxcarbazepine Adjunctive Therapy Trials
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Dosage Form Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Administer oxcarbazepine extended-release tablets as a single daily dose taken on an empty stomach (at least 1 hour before or at least 2 hours after meals) [see Clinical Pharmacology (12.3)]. If oxcarbazepine extended-release tablets are taken with food, adverse reactions are more likely to occur because of increased peak levels [see Clinical Pharmacology (12.3)].
Swallow oxcarbazepine extended-release tablets whole. Do not cut, crush, or chew the tablets. For ease of swallowing in pediatric patients or patients with difficulty swallowing, achieve daily dosages with multiples of appropriate lower strength tablets (e.g., 150 mg tablets).
2.2 General Dosing Recommendations
Monotherapy or Adjunctive Therapy
Adult Patients
Initiate treatment at a dosage of 600 mg/day given orally once daily for one week. Subsequent dosage increases can be made at weekly intervals in 600 mg/day increments to achieve the recommended daily dosage.
The recommended daily dosage of oxcarbazepine extended-release tablets are 1,200 mg to 2,400 mg/day, given once daily. The dosage of 2,400 mg/day showed slightly greater efficacy than 1,200 mg/day, but was associated with an increase in adverse reactions [see Adverse Reactions (6.1) and Clinical Studies (14.1)].
Dosage adjustment is recommended with concomitant use of strong CYP3A4 enzyme inducers or UGT inducers, which include certain antiepileptic drugs (AEDs) [see Drug Interactions (7.1, 7.2)].
Pediatric Patients (6 to Less than 17 Years of Age)
In pediatric patients 6 to less than 17 years of age, initiate treatment at a daily dosage of 8 mg/kg to 10 mg/kg orally once daily, not to exceed 600 mg per day in the first week.
Subsequent dosage increases can be made at weekly intervals in 8 mg/kg to 10 mg/kg increments once daily, not to exceed 600 mg, to achieve the target daily dosage. The target maintenance dosage, achieved over two to three weeks, is displayed in Table 1.
Table 1: Target Daily Dosage in Pediatric Patients (6 to Less Than 17 Years of Age) Weight
Target Daily Dosage
20 kg to 29 kg
900 mg/day
29.1 kg to 39 kg
1,200 mg/day
Greater than 39 kg
1,800 mg/day
Dosage adjustment is recommended with concomitant use of strong CYP3A4 enzyme inducers or UGT inducers, which include certain antiepileptic drugs (AEDs) [see Drug Interactions (7.1, 7.2)].
2.3 Dosage Modifications in Adult Patients with Renal Impairment
In adult patients with severe renal impairment (creatinine clearance less than 30 mL/minute), initiate oxcarbazepine extended-release tablets at one-half the usual starting dosage (300 mg/day). Subsequent dosage increases can be made at weekly intervals in increments of 300 mg to 450 mg/day to achieve the desired clinical response [see Use in Specific Populations (8.6)].
2.4 Dosage Modifications in Geriatric Patients
In geriatric patients, consider starting at a lower dosage (300 mg or 450 mg/day). Subsequent dosage increases can be made at weekly intervals in increments of 300 mg to 450 mg/day to achieve the desired clinical effect [see Use in Specific Populations (8.5)].
2.5 Dosage Modification with Concomitant Use of Strong CYP3A4 Enzyme Inducers or UGT Enzyme Inducers
Strong CYP3A4 inducers, including enzyme-inducing antiepileptic drugs such as carbamazepine, phenobarbital, and phenytoin, and UGT inducers (e.g., rifampin) decrease exposure to 10-monohydroxy derivative (MHD), the active metabolite [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)]. Dosage adjustment of oxcarbazepine extended-release tablets may be required after initiation, dosage modification, or discontinuation of such inducers. Dosage increases of oxcarbazepine extended-release tablets may be necessary with concomitant use. Consider initiating at 900 mg once daily for adults and 12 mg/kg to 15 mg/kg orally once daily (not to exceed 900 mg per day in the first week) in pediatric patients.
2.6 Withdrawal of AEDs
As with most antiepileptic drugs, oxcarbazepine extended-release tablets should be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus [see Warnings and Precautions (5.6)].
2.7 Conversion from Immediate-Release Oxcarbazepine to Oxcarbazepine Extended-Release Tablets
In conversion of oxcarbazepine immediate-release to oxcarbazepine extended-release tablets, higher dosages of oxcarbazepine extended-release tablets may be necessary [see Clinical Pharmacology (12.3)].
-
3 DOSAGE FORMS AND STRENGTHS
Extended-release tablets:
- 150 mg: yellow oval shaped, biconvex, tablet debossed with “XC1” on one side and plain on other side
- 300 mg: brown oval shaped, biconvex, tablet debossed with “XC2” on one side and plain on other side
- 600 mg: brownish red oval shaped, biconvex, tablet debossed with “XC3” on one side and plain on other side
-
4 CONTRAINDICATIONS
Oxcarbazepine extended-release tablets are contraindicated in patients with a known hypersensitivity to oxcarbazepine, to any of the components of oxcarbazepine extended-release tablets, or to eslicarbazepine acetate. Reactions have included anaphylaxis and angioedema [see Warnings and Precautions (5.2, 5.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hyponatremia
Clinically significant hyponatremia (sodium < 125 mmol/L) may develop during oxcarbazepine extended-release tablets use. Serum sodium levels less than 125 mmol/L have occurred in immediate-release oxcarbazepine-treated patients generally in the first three months of treatment. However, clinically significant hyponatremia may develop more than a year after initiating therapy.
Most immediate-release oxcarbazepine-treated patients who developed hyponatremia were asymptomatic in clinical trials. However, some of these patients had their dosage reduced, discontinued, or had their fluid intake restricted for hyponatremia. Serum sodium levels returned toward normal when the dosage was reduced or discontinued, or when the patient was treated conservatively (e.g., fluid restriction). Cases of symptomatic hyponatremia and syndrome of inappropriate antidiuretic hormone secretion (SIADH) have been reported during post-marketing use of immediate-release oxcarbazepine.
Among treated patients in a controlled trial of adjunctive therapy with oxcarbazepine extended-release tablets in 366 adults with complex partial seizures, 1 patient receiving 2,400 mg experienced a severe reduction in serum sodium (117 mEq/L) requiring discontinuation from treatment, while 2 other patients receiving 1,200 mg experienced serum sodium concentrations low enough (125 mEq/L and 126 mEq/L) to require discontinuation from treatment. The overall incidence of clinically significant hyponatremia in patients treated with oxcarbazepine extended-release tablets was 1.2%, although slight shifts in serum sodium concentrations from Normal to Low (< 135 mEq/L) were observed for the 2,400 mg (6.5%) and 1,200 mg (9.8%) groups compared to placebo (1.7%).
Measure serum sodium concentrations if patients develop symptoms of hyponatremia (e.g., nausea, malaise, headache, lethargy, confusion, obtunded consciousness, or increase in seizure frequency or severity). Consider measurement of serum sodium concentrations during treatment with oxcarbazepine extended-release tablets, particularly if the patient receives concomitant medications known to decrease serum sodium levels (for example, drugs associated with inappropriate ADH secretion).
5.2 Anaphylactic Reactions and Angioedema
Rare cases of anaphylaxis and angioedema involving the larynx, glottis, lips and eyelids have been reported in patients after taking the first or subsequent doses of immediate-release oxcarbazepine. Angioedema associated with laryngeal edema can be fatal. If a patient develops any of these reactions after treatment with oxcarbazepine extended-release tablets, discontinue the drug and initiate an alternative treatment. Do not rechallenge these patients with oxcarbazepine extended-release tablets.
5.3 Cross Hypersensitivity Reaction to Carbamazepine
Approximately 25% to 30% of patients who have had hypersensitivity reactions to carbamazepine will experience hypersensitivity reactions with oxcarbazepine extended-release tablets. For this reason, patients should be specifically questioned about any prior experience with carbamazepine, and patients with a history of hypersensitivity reactions to carbamazepine should ordinarily be treated with oxcarbazepine extended-release tablets only if the potential benefit justifies the potential risk. Discontinue oxcarbazepine extended-release tablets immediately if signs or symptoms of hypersensitivity develop [see Warnings and Precautions (5.2, 5.7)].
5.4 Serious Dermatological Reactions
Serious dermatological reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have occurred in both children and adults treated with immediate-release oxcarbazepine use. The median time of onset for reported cases was 19 days. Such serious skin reactions may be life threatening, and some patients have required hospitalization with very rare reports of fatal outcome. Recurrence of the serious skin reactions following rechallenge with immediate-release oxcarbazepine has also been reported.
The reporting rate of TEN and SJS associated with immediate-release oxcarbazepine use, which is generally accepted to be an underestimate due to underreporting, exceeds the background incidence rate estimates by a factor of 3- to 10-fold. Estimates of the background incidence rate for these serious skin reactions in the general population range between 0.5 to 6 cases per million-person years. Therefore, if a patient develops a skin reaction while taking oxcarbazepine extended-release tablets, consider discontinuing oxcarbazepine extended-release tablets use and prescribing another AED.
Association with HLA-B*1502
Patients carrying the HLA-B*1502 allele may be at increased risk for SJS/TEN with oxcarbazepine extended-release tablets treatment.
Human Leukocyte Antigen (HLA) allele B*1502 increases the risk for developing SJS/TEN in patients treated with carbamazepine. The chemical structures of immediate-release oxcarbazepine and oxcarbazepine extended-release tablets are similar to that of carbamazepine. Available clinical evidence, and data from nonclinical studies showing a direct interaction between immediate-release oxcarbazepine and HLA-B*1502 protein, suggest that the HLA-B*1502 allele may also increase the risk for SJS/TEN with oxcarbazepine extended-release tablets.
The frequency of HLA-B*1502 allele ranges from 2% to 12% in Han Chinese populations, is about 8% in Thai populations, and above 15% in the Philippines and in some Malaysian populations. Allele frequencies up to about 2% and 6% have been reported in Korea and India, respectively.
The frequency of the HLA-B*1502 allele is negligible in people from European descent, several African populations, indigenous peoples of the Americas, Hispanic populations, and in Japanese (< 1%).
Testing for the presence of the HLA-B*1502 allele should be considered in patients with ancestry in genetically at-risk populations, prior to initiating treatment with oxcarbazepine extended-release tablets. The use of oxcarbazepine extended-release tablets should be avoided in patients positive for HLA-B*1502 unless the benefits clearly outweigh the risks. Consideration should also be given to avoid the use of other drugs associated with SJS/TEN in HLA-B*1502 positive patients, when alternative therapies are otherwise equally acceptable. Screening is not generally recommended in patients from populations in which the prevalence of HLA-B*1502 is low, or in current oxcarbazepine extended-release tablets users, as the risk of SJS/TEN is largely confined to the first few months of therapy, regardless of HLA-B*1502 status.
The use of HLA-B*1502 genotyping has important limitations and must never substitute for appropriate clinical vigilance and patient management. The role of other possible factors in the development of, and morbidity from, SJS/TEN, such as antiepileptic drug (AED) dosage, compliance, concomitant medications, comorbidities, and the level of dermatologic monitoring have not been well characterized.
5.5 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including oxcarbazepine extended-release tablets, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Monitor patients treated with any AED for any indication for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 years to 100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
Table 2: Risk by Indication for Antiepileptic Drugs in the Pooled Analysis Indication
Placebo Patients with Events per 1,000 Patients
Drug Patients with Events per 1,000 Patients
Relative Risk:
Incidence of
Events in Drug
Patients/Incidence
in Placebo
Patients
Risk
Difference:
Additional
Drug Patients
with Events per
1,000 Patients
Epilepsy
1.0
3.4
3.5
2.4
Psychiatric
5.7
8.5
1.5
2.9
Other
1.0
1.8
1.9
0.9
Total
2.4
4.3
1.8
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing oxcarbazepine extended-release tablets or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during oxcarbazepine extended-release tablets treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
5.6 Withdrawal of AEDs
As with most AEDs, oxcarbazepine extended-release tablets should be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. But if withdrawal is needed because of a serious adverse event, rapid discontinuation can be considered.
5.7 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multi-organ hypersensitivity, has occurred with immediate-release oxcarbazepine. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling, in associated with other organ system involvement, such as hepatitis, nephritis, hematologic abnormalities, myocaraditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present even though rash is not evident. Oxcarbazepine extended-release tablets should be discontinued if an alternative etiology for the signs and symptoms cannot be established.
5.8 Hematologic Reactions
Rare reports of pancytopenia, agranulocytosis, and leukopenia have been seen in patients treated with immediate-release oxcarbazepine during post-marketing experience. Discontinuation of oxcarbazepine extended-release tablets should be considered if any evidence of these hematologic reactions develops.
5.9 Risk of Seizures in the Pregnant Patient
Due to physiological changes during pregnancy, plasma concentrations of the active metabolite of oxcarbazepine, the 10-monohydroxy derivative (MHD), may gradually decrease throughout pregnancy. Monitor patients carefully during pregnancy and through the postpartum period because MHD concentrations may increase after delivery.
5.10 Risk of Seizure Aggravation
Exacerbation of or new onset primary generalized seizures has been reported with immediate-release oxcarbazepine. The risk of aggravation of primary generalized seizures is seen especially in children but may also occur in adults. In case of seizure aggravation, oxcarbazepine extended-release tablets should be discontinued.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described in other sections of the labeling:
- Hyponatremia [see Warnings and Precautions (5.1)]
- Anaphylactic Reactions and Angioedema [see Warnings and Precautions (5.2)]
- Cross Hypersensitivity Reaction to Carbamazepine [see Warnings and Precautions (5.3)]
- Serious Dermatological Reactions [see Warnings and Precautions (5.4)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.5)]
- Withdrawal of AEDs [see Warnings and Precautions (5.6)]
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity [see Warnings and Precautions (5.7)]
- Hematologic Reactions [see Warnings and Precautions (5.8)]
- Risk of Seizures in the Pregnant Patient[see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety data presented below are from 384 patients with partial-onset seizures who received oxcarbazepine extended-release tablets (366 adults and 18 pediatric patients) with concomitant AEDs.
In addition, safety data presented below are from a total of 2,288 patients with seizure disorders treated with immediate-release oxcarbazepine; 1,832 were adults and 456 were pediatric patients.
Most Common Adverse Reactions Reported by Adult Patients Receiving Concomitant AEDs in Oxcarbazepine Extended-Release Tablets Clinical Studies
Table 3 lists adverse reactions that occurred in at least 2% of adult patients with epilepsy treated with oxcarbazepine extended-release tablets or placebo and concomitant AEDs and that were numerically more common in the patients treated with any dosage of oxcarbazepine extended-release tablets than in patients receiving placebo.
The overall incidence of adverse reactions appeared to be dose related, particularly during the titration period. The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine extended-release tablets and more frequent than in placebo-treated patients were: dizziness, somnolence, headache, balance disorder, tremor, vomiting, diplopia, and asthenia.
Table 3: Adverse Reaction Incidence in a Controlled Clinical Study of Oxcarbazepine Extended-Release Tablets with Concomitant AEDs in Adults*
Oxcarbazepine Extended-Release Tablets
2,400 mg/day
N=123
%
Oxcarbazepine Extended-Release Tablets
1,200 mg/day
N=122
%
Placebo
N=121
%
Any System / Any Term
69
57
55
Nervous System Disorders
Dizziness
41
20
15
Somnolence
14
12
9
Headache
15
8
7
Balance Disorder
7
5
5
Tremor
1
5
2
Nystagmus
3
3
1
Ataxia
1
3
1
Gastrointestinal Disorders
Vomiting
15
6
9
Abdominal Pain Upper
0
3
1
Dyspepsia
0
3
1
Gastritis
0
3
2
Eye Disorders
Diplopia
13
10
4
Vision Blurred
1
4
3
Visual Impairment
1
3
0
General Disorders and Administration
Site Conditions
Asthenia
7
3
1
Fatigue
3
6
1
Gait Disturbance
0
3
1
Drug Intolerance
2
0
0
Infections and Infestations
Nasopharyngitis
0
3
0
Sinusitis
0
3
2
* Reported by ≥ 2% of patients treated with oxcarbazepine extended-release tablets and numerically more frequent than in the placebo group
Adverse Reactions Associated with Discontinuation of Oxcarbazepine Extended-Release Tablets Treatment: Approximately 23.3% of the 366 adult patients receiving oxcarbazepine extended-release tablets in clinical studies discontinued treatment because of an adverse reaction. The adverse reactions most commonly associated with discontinuation of oxcarbazepine extended-release tablets (reported by ≥ 2%) were: dizziness (9.8%), vomiting (5.3%), nausea (3.7%), diplopia (3.2%), and somnolence (2.4%).
Adjunctive Therapy with Oxcarbazepine Extended-Release Tablets in Pediatric Patients 6 to Less than 17 Years of Age Previously Treated with other AEDs
In a pharmacokinetic study in 18 pediatric patients (including patients 6 to less than 17 years of age) with partial-onset seizures treated with different dosages of oxcarbazepine extended-release tablets, the observed adverse reactions seen in association with oxcarbazepine extended-release tablets were similar to those seen in adults.
Most Common Adverse Reactions in Immediate-Release Oxcarbazepine Controlled Clinical Studies
Controlled Clinical Studies of Adjunctive Therapy with Immediate-Release Oxcarbazepine in Adults Previously Treated with other AEDs: Table 4 lists adverse reactions that occurred in at least 2% of adult patients with epilepsy treated with immediate-release oxcarbazepine or placebo with concomitant AEDs and that were numerically more common in the patients treated with any dosage of immediate-release oxcarbazepine than in placebo. As immediate-release oxcarbazepine and oxcarbazepine extended-release tablets were not examined in the same trial, adverse event frequencies cannot be directly compared between the two formulations.
Table 4: Adverse Reaction Incidence in a Controlled Clinical Study of Immediate Release Oxcarbazepine with Concomitant AEDs in Adults* * Events in at least 2% of patients treated with 2,400 mg/day of immediate-release oxcarbazepine and numerically more frequent than in the placebo group
Immediate-Release Oxcarbazepine Dosage
(mg/day)
Placebo
N = 166
%
OXC 600
N = 163
%
OXC 1,200
N = 171
%
OXC 2,400
N = 126
%
Body as a Whole
Fatigue
15
12
15
7
Asthenia
6
3
6
5
Edema Legs
2
1
2
1
Weight Increase
1
2
2
1
Feeling Abnormal
0
1
2
0
Cardiovascular System
Hypotension
0
1
2
0
Digestive System
Nausea
15
25
29
10
Vomiting
13
25
36
5
Pain Abdominal
10
13
11
5
Diarrhea
5
6
7
6
Dyspepsia
5
5
6
2
Constipation
2
2
6
4
Gastritis
2
1
2
1
Metabolic and Nutritional Disorders
Hyponatremia
3
1
2
1
Musculoskeletal System
Muscle Weakness
1
2
2
0
Sprains and Strains
0
2
2
1
Nervous System
Headache
32
28
26
23
Dizziness
36
32
49
13
Somnolence
20
28
36
12
Ataxia
9
17
31
5
Nystagmus
7
20
26
5
Gait Abnormal
5
10
17
1
Insomnia
4
2
3
1
Tremor
3
8
16
5
Nervousness
2
4
2
1
Agitation
1
1
2
1
Coordination Abnormal
1
3
2
1
EEG Abnormal
0
0
2
0
Speech Disorder
1
1
3
0
Confusion
1
1
2
1
Cranial Injury NOS
1
0
2
1
Dysmetria
1
2
3
0
Thinking Abnormal
0
2
4
0
Respiratory System
Rhinitis
2
4
5
4
Skin and Appendages
Acne
1
2
2
0
Special Senses
Diplopia
14
30
40
5
Vertigo
6
12
15
2
Vision Abnormal
6
14
13
4
Accommodation Abnormal
0
0
2
0
Other Reactions Observed in Association with the Administration of Immediate-Release Oxcarbazepine
In the paragraphs that follow, the adverse reactions, other than those in the preceding tables or text, that occurred in a total of 565 children and 1,574 adults exposed to immediate-release oxcarbazepine and that are reasonably likely to be related to drug use are presented. Events common in the population, events reflecting chronic illness and events likely to reflect concomitant illness are omitted particularly if minor. They are listed in order of decreasing frequency. Because the reports cite reactions observed in open-label and uncontrolled trials, the role of immediate-release oxcarbazepine in their causation cannot be reliably determined.
Body as a Whole: fever, malaise, pain chest precordial, rigors, weight decrease.
Cardiovascular System: bradycardia, cardiac failure, cerebral hemorrhage, hypertension, hypotension postural, palpitation, syncope, tachycardia.
Digestive System: appetite increased, blood in stool, cholelithiasis, colitis, duodenal ulcer, dysphagia, enteritis, eructation, esophagitis, flatulence, gastric ulcer, gingival bleeding, gum hyperplasia, hematemesis, hemorrhage rectum, hemorrhoids, hiccup, mouth dry, pain biliary, pain right hypochondrium, retching, sialoadenitis, stomatitis, stomatitis ulcerative.
Hematologic and Lymphatic System: thrombocytopenia.
Laboratory Abnormality: gamma-GT increased, hyperglycemia, hypocalcemia, hypoglycemia, hypokalemia, liver enzymes elevated, serum transaminase increased.
Musculoskeletal System: hypertonia muscle.
Nervous System: aggressive reaction, amnesia, anguish, anxiety, apathy, aphasia, aura, convulsions aggravated, delirium, delusion, depressed level of consciousness, dysphonia, dystonia, emotional lability, euphoria, extrapyramidal disorder, feeling drunk, hemiplegia, hyperkinesia, hyperreflexia, hypoesthesia, hypokinesia, hyporeflexia, hypotonia, hysteria, libido decreased, libido increased, manic reaction, migraine, muscle contractions involuntary, nervousness, neuralgia, oculogyric crisis, panic disorder, paralysis, paroniria, personality disorder, psychosis, ptosis, stupor, tetany.
Respiratory System: asthma, bronchitis, coughing, dyspnea, epistaxis, laryngismus, pleurisy.
Skin and Appendages: acne, alopecia, angioedema, bruising, dermatitis contact, eczema, facial rash, flushing, folliculitis, heat rash, hot flushes, photosensitivity reaction, pruritus genital, psoriasis, purpura, rash erythematous, rash maculopapular, vitiligo, urticaria.
Special Senses: accommodation abnormal, cataract, conjunctival hemorrhage, edema eye, hemianopia, mydriasis, otitis externa, photophobia, scotoma, taste perversion, tinnitus, xerophthalmia.
Urogenital and Reproductive System: dysuria, hematuria, intermenstrual bleeding, leukorrhea, menorrhagia, micturition frequency, pain renal, pain urinary tract, polyuria, priapism, renal calculus, urinary tract infection.
Other: Systemic lupus erythematosus.
Laboratory Tests
Serum sodium levels below 125 mmol/L have been observed in patients treated with immediate-release oxcarbazepine [see Warnings and Precautions (5.1)]. Experience from clinical trials with immediate-release oxcarbazepine indicates that serum sodium levels return toward normal when the dosage is reduced or discontinued, or when the patient was treated conservatively (e.g., fluid restriction).
Laboratory data from clinical trials suggest that immediate-release oxcarbazepine use was associated with decreases in T4, without changes in T3 or TSH.
6.2 Postmarketing and Other Experience
The following adverse reactions have been observed in named patient programs or post-marketing experience with immediate-release oxcarbazepine or oxcarbazepine extended-release tablets. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole: multi-organ hypersensitivity disorders characterized by features such as rash, fever, lymphadenopathy, abnormal liver function tests, eosinophilia, and arthralgia [see Warnings and Precautions (5.7)]
Cardiovascular System: atrioventricular block
Digestive System: pancreatitis and/or lipase and/or amylase increase
Hematologic and Lymphatic Systems: aplastic anemia [see Warnings and Precautions (5.8)]
Immune System Disorders: anaphylaxis [see Warnings and Precautions (5.2)]
Metabolism and Nutrition Disorders: hypothyroidism and syndrome of inappropriate antidiuretic hormone secretion (SIADH)
Skin and Subcutaneous Tissue Disorders: erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis [see Warnings and Precautions (5.4)], Acute Generalized Exanthematous Pustulosis (AGEP)
Musculoskeletal, Connective Tissue and Bone Disorders: There have been reports of decreased bone mineral density, osteoporosis and fractures in patients on long-term therapy with immediate-release oxcarbazepine.
-
7 DRUG INTERACTIONS
7.1 Effect of Oxcarbazepine Extended-Release Tablets on Other Drugs
It is recommended that the plasma levels of phenytoin be monitored during the period of oxcarbazepine extended-release tablets titration and dosage modification [see Clinical Pharmacology (12.3)]. A decrease in the dosage of phenytoin may be required.
7.2 Effect of Other Drugs on Oxcarbazepine Extended-Release Tablets
If oxcarbazepine extended-release tablets and strong CYP3A4 inducers or UGT inducers (e.g., rifampin, carbamazepine, phenytoin and phenobarbital) are administered concurrently, it is recommended that the plasma levels of MHD be monitored during the period of oxcarbazepine extended-release tablets titration [see Clinical Pharmacology (12.3)]. Dosage adjustment of oxcarbazepine extended-release tablets may be required after initiation, dosage modification, or discontinuation of such inducers [see Dosage and Administration (2.5)].
7.3 Hormonal Contraceptives
Concurrent use of immediate-release oxcarbazepine with hormonal contraceptives may render these contraceptives less effective [see Clinical Pharmacology (12.3)]. Studies with other oral or implant contraceptives have not been conducted.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate data on the developmental risks associated with the use of oxcarbazepine extended-release tablets in pregnant women; however, oxcarbazepine extended-release tablets is closely related structurally to carbamazepine, which is considered to be teratogenic in humans. Data on a limited number of pregnancies from pregnancy registries suggest that oxcarbazepine monotherapy use is associated with congenital malformations (e.g., craniofacial defects such as oral clefts, and cardiac malformations such as ventricular septal defects). Increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity (embryolethality, growth retardation) were observed in the offspring of animals treated with either oxcarbazepine or its active 10-hydroxy metabolite (MHD) during pregnancy at doses similar to the maximum recommended human dose (MRHD).
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Clinical Considerations
An increase in seizure frequency may occur during pregnancy because of altered levels of the active metabolite of oxcarbazepine. Monitor patients carefully during pregnancy and through the postpartum period [see Warnings and Precautions (5.9)]
Data
Human Data
Data from published registries have reported craniofacial defects such as oral clefts and cardiac malformations such as ventricular septal defects in children with prenatal oxcarbazepine exposure.
Animal Data
When pregnant rats were given oxcarbazepine (30 mg/kg/day, 300 mg/kg/day, or 1,000 mg/kg/day) orally throughout the period of organogenesis, increased incidences of fetal malformations (craniofacial, cardiovascular, and skeletal) and variations were observed at the intermediate and high doses (approximately 1.2 and 4 times, respectively, the MRHD on a mg/m2 basis). Increased embryofetal death and decreased fetal body weights were seen at the high dose. Doses ≥ 300 mg/kg were also maternally toxic (decreased body weight gain, clinical signs), but there is no evidence to suggest that teratogenicity was secondary to the maternal effects.
In a study in which pregnant rabbits were orally administered MHD (20 mg/kg/day, 100 mg/kg/day, or 200 mg/kg/day) during organogenesis, embryofetal mortality was increased at the highest dose (1.5 times the MRHD on a mg/m2 basis). This dose produced only minimal maternal toxicity.
In a study in which female rats were dosed orally with oxcarbazepine (25 mg/kg/day, 50 mg/kg/day, or 150 mg/kg/day) during the latter part of gestation and throughout the lactation period, a persistent reduction in body weights and altered behavior (decreased activity) were observed in offspring exposed to the highest dose (0.6 times the MRHD on a mg/m2 basis). Oral administration of MHD (25 mg/kg/day, 75 mg/kg/day, or 250 mg/kg/day) to rats during gestation and lactation resulted in a persistent reduction in offspring weights at the highest dose (equivalent to the MRHD on a mg/m2 basis).
8.2 Lactation
Risk Summary
Oxcarbazepine and its active metabolite (MHD) are present in human milk after oxcarbazepine administration. The effects of oxcarbazepine and its active metabolite (MHD) on the breastfed infant or on milk production are unknown. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for oxcarbazepine extended-release tablets and any potential adverse effects on the breastfed infant from oxcarbazepine extended-release tablets or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Contraception
Use of oxcarbazepine extended-release tablets with hormonal contraceptives containing ethinylestradiol or levonorgestrel is associated with decreased plasma concentrations of these hormones and may result in a failure of the therapeutic effect of the oral contraceptive drug. Advise women of reproductive potential taking oxcarbazepine extended-release tablets who are using a contraceptive containing ethinylestradiol or levonorgestrel to use additional or alternative non-hormonal birth control [see Drug Interactions (7.3) and Clinical Pharmacology (12.3)].
8.4 Pediatric Use
The safety and effectiveness of oxcarbazepine extended-release tablets in pediatric patients 6 years of age and older for the treatment of partial-onset seizures is supported by:
1) An adequate and well-controlled safety and efficacy study of oxcarbazepine extended-release tablets in adults that included pharmacokinetic sampling [see Clinical Studies (14.1)],
2) A pharmacokinetic study of oxcarbazepine extended-release tablets in pediatric patients, which included patients 6 to less than 17 years of age [see Clinical Pharmacology (12.3)],
3) Safety and efficacy studies with the immediate-release formulation in adults and pediatric patients [see Clinical Studies (14.2) and Adverse Reactions (6.1)].
Oxcarbazepine extended-release tablets is not approved for pediatric patients less than 6 years of age because the size of the tablets are inappropriate for younger children.
8.5 Geriatric Use
Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 years to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 years to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance. Consider starting at a lower dosage and lower titration [see Dosage and Administration (2.4)]. Close monitoring of sodium levels is required in elderly patients at risk for hyponatremia [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
There is a linear correlation between creatinine clearance and the renal clearance of MHD [see Clinical Pharmacology (12.3) and Dosage and Administration (2.3)].
The pharmacokinetics of oxcarbazepine extended-release tablets has not been evaluated in patients with renal impairment. In patients with severe renal impairment (creatinine clearance < 30 mL/min) given immediate-release oxcarbazepine, the elimination half-life of MHD was prolonged with a corresponding two-fold increase in AUC [see Clinical Pharmacology (12.3)]. In these patients initiate oxcarbazepine extended-release tablets at a lower starting dosage and increase, if necessary, at a slower than usual rate until the desired clinical response is achieved [see Dosage and Administration (2.3)].
In patients with end-stage renal disease on dialysis, it is recommended that immediate-release oxcarbazepine be used instead of oxcarbazepine extended-release tablets.
8.7 Hepatic Impairment
The pharmacokinetics of oxcarbazepine and MHD has not been evaluated in severe hepatic impairment, and therefore is not recommended in these patients [see Clinical Pharmacology (12.3)].
- 9 DRUG ABUSE AND DEPENDENCE
-
10 OVERDOSAGE
10.1 Human Overdose Experience
Isolated cases of overdose with immediate-release oxcarbazepine have been reported. The maximum dose taken was approximately 48,000 mg. All patients recovered with symptomatic treatment. Nausea, vomiting, somnolence, aggression, agitation, hypotension, and tremor each occurred in more than one patient. Coma, confusional state, convulsion, dyscoordination, depressed level of consciousness, diplopia, dizziness, dyskinesia, dyspnea, QT prolongation, headache, miosis, nystagmus, overdose, decreased urine output, and blurred vision also occurred.
-
11 DESCRIPTION
Oxcarbazepine is an antiepileptic drug (AED). Oxcarbazepine extended-release tablets contain oxcarbazepine for once-a-day oral administration. Oxcarbazepine is 10,11-Dihydro-10-oxo-5H-dibenz[b,f]-azepine-5-carboxamide, and its structural formula is
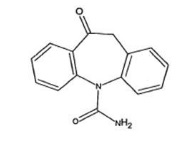
Oxcarbazepine is white or faintly orange, crystalline powder.
Oxcarbazepine USP is sparingly soluble in chloroform (30 g/L to 100 g/L). In aqueous media over pH range 1 to 8, oxcarbazepine is practically insoluble and its solubility is 40 mg/L (0.04 g/L) at pH 7.0, 25°C. The molecular formula is C15H12N2O2 and its molecular weight is 252.27.
Oxcarbazepine extended-release tablets contain the following inactive ingredients: colloidal silicon dioxide, hypromellose, hydroxypropyl cellulose, yellow iron oxide, red iron oxide (300 mg, 600 mg tablets only), black iron oxide (150 mg, 300 mg tablets only), magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, sodium lauryl sulfate, talc, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The pharmacological activity of oxcarbazepine extended-release tablets are primarily exerted through the 10-monohydroxy metabolite (MHD) of oxcarbazepine [see Clinical Pharmacology (12.3)]. The precise mechanism by which oxcarbazepine and MHD exert their antiseizure effect is unknown; however, in vitro electrophysiological studies indicate that they produce blockade of voltage-sensitive sodium channels, resulting in stabilization of hyperexcited neural membranes, inhibition of repetitive neuronal firing, and diminution of propagation of synaptic impulses. These actions are thought to be important in the prevention of seizure spread in the intact brain. In addition, increased potassium conductance and modulation of high-voltage activated calcium channels may contribute to the anticonvulsant effects of the drug. No significant interactions of oxcarbazepine or MHD with brain neurotransmitter or modulator receptor sites have been demonstrated.
12.2 Pharmacodynamics
Oxcarbazepine and its active metabolite (MHD) exhibit anticonvulsant properties in animal seizure models. They protected rodents against electrically induced tonic extension seizures and, to a lesser degree, chemically induced clonic seizures, and abolished or reduced the frequency of chronically recurring focal seizures in Rhesus monkeys with aluminum implants. No development of tolerance (i.e., attenuation of anticonvulsive activity) was observed in the maximal electroshock test when mice and rats were treated daily for five days and four weeks, respectively, with oxcarbazepine or MHD.
12.3 Pharmacokinetics
Following oral administration, oxcarbazepine is absorbed and extensively metabolized to its pharmacologically active 10-monohydroxy metabolite (MHD), which is responsible for most antiepileptic activity.
In clinical studies of oxcarbazepine extended-release tablets, the elimination half-life of oxcarbazepine was between 7 hours and 11 hours; the elimination half-life of MHD is between 9 hours and 11 hours.
In a mass balance study in humans, only 2% of total radioactivity in plasma after administration of immediate-release oxcarbazepine was due to unchanged oxcarbazepine, with approximately 70% present as MHD, and the remainder attributable to minor metabolites.
Absorption
Oxcarbazepine extended-release tablets administered as a once daily dosage is not bioequivalent to the same total dosage of the immediate-release formulation given twice daily at steady state. Steady state plasma concentrations of MHD are reached within 5 days when oxcarbazepine extended-release tablets is given once daily. At steady state, when 1,200 mg oxcarbazepine extended-release tablets was given once daily, MHD Cmax occurred 7 hours post-dose. At steady state, oxcarbazepine extended-release tablets given once daily produced MHD exposures (AUC and Cmax) about 19% lower and MHD minimum concentrations (Cmin) about 16% lower than the immediate-release oxcarbazepine given twice daily when administered at the same 1,200 mg total daily dosage. When oxcarbazepine extended-release tablets was administered at an equivalent 600 mg single dose (4 × 150 mg tablets, 2 × 300 mg tablets, or 1 × 600 mg tablet), equivalent MHD exposures (AUC) were observed.
Following a single dose of oxcarbazepine extended-release tablets (1 × 150 mg tablets, 1 × 300 mg tablets, or 1 × 600 mg tablet), the pharmacokinetics of MHD are not linear and show greater than dose proportional increase in AUC and less than proportional increase in Cmax: AUC increases 2.4-fold and Cmax increases 1.9-fold with a 2-fold increase in dose.
Effect of Food:
Single dose administration of 600 mg oxcarbazepine extended-release tablets following a high fat meal (800 calories to 1,000 calories) produced MHD exposure (AUC) equivalent to that produced under fasting conditions. Peak MHD concentration (Cmax) was about 60% higher and occurred 2 hours earlier under fed conditions than under fasting conditions.
The increase in Cmax, even without a significant change in the overall exposure, should be considered by the prescriber especially during the titration phase, when some adverse reactions are most likely to occur coincidentally with peak levels.
Distribution
The apparent volume of distribution of MHD is 49 L. Approximately 40% of MHD is bound to serum proteins, predominantly to albumin. Binding is independent of the serum concentration within the therapeutically relevant range. Oxcarbazepine and MHD do not bind to alpha-1-acid glycoprotein.
Elimination
Metabolism
Oxcarbazepine is rapidly reduced by cytosolic enzymes in the liver to MHD, which is primarily responsible for the pharmacological effect of oxcarbazepine extended-release tablets. MHD is metabolized further by conjugation with glucuronic acid. Minor amounts (4% of the dose) are oxidized to the pharmacologically inactive 10,11-dihydroxy metabolite (DHD).
Excretion
Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. More than 95% of a dose of immediate-release oxcarbazepine appears in the urine, with less than 1% as unchanged oxcarbazepine. Fecal excretion accounts for less than 4% of an administered dose. Approximately 80% of the dose is excreted in the urine either as glucuronides of MHD (49%) or as unchanged MHD (27%); the inactive DHD accounts for approximately 3% and conjugates of MHD and oxcarbazepine account for 13% of the dose.
The half-life of the parent was about two hours, while the half-life of MHD was about nine hours after the immediate-release formulation. A population pharmacokinetic model for oxcarbazepine extended-release tablets was developed in healthy normal adults and applied to pharmacokinetic data in patients with epilepsy. For oxcarbazepine, systemic parameters were scaled allometrically, suggesting that steady state oxcarbazepine exposure will vary inversely with weight.
Specific Populations
Geriatric Patients
No studies with oxcarbazepine extended-release tablets in elderly patients have been completed [see Use in Specific Populations (8.5)].
Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 years to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 years to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance.
Pediatric Patients
A pharmacokinetic study of oxcarbazepine extended-release tablets was performed in 18 pediatric patients with epilepsy, which included patients 6 to less than 17 years of age, after multiple doses. The population pharmacokinetic model suggested that dosing of pediatric patients with oxcarbazepine extended-release tablets can be determined based on body weight. Weight-normalized doses in pediatric patients should produce MHD exposures (AUC) comparable to that in typical adults, with oxcarbazepine exposures ~40% higher in children than in adults [see Use in Specific Populations (8.4)]. The pharmacokinetics of oxcarbazepine extended-release tablets in pediatric patients are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures.
Male and Female Patients
The effects of gender have not been studied for oxcarbazepine extended-release tablets.
No gender-related pharmacokinetic differences have been observed in children, adults, or the elderly with immediate-release oxcarbazepine.
Racial or Ethnic Groups
The effects of race have not been studied for oxcarbazepine extended-release tablets.
Patients with Renal or Hepatic Impairment
The effects of renal or hepatic impairment have not been studied for oxcarbazepine extended-release tablets [see Use in Specific Populations (8.6, 8.7)].
Based on investigations with immediate-release oxcarbazepine, there is a linear correlation between creatinine clearance and the renal clearance of MHD. When immediate-release oxcarbazepine is administered as a single 300 mg dose in renally-impaired patients (creatinine clearance < 30 mL/min), the elimination half-life of MHD is prolonged to 19 hours, with a two-fold increase in AUC. Dosage adjustment is recommended in these patients [see Dosage and Administration (2.3) and Use in Special Populations (8.6)].
The pharmacokinetics and metabolism of immediate-release oxcarbazepine and MHD were evaluated in healthy volunteers and hepatically impaired subjects after a single 900 mg oral dose. Mild-to-moderate hepatic impairment did not affect the pharmacokinetics of immediate-release oxcarbazepine and MHD. The pharmacokinetics of oxcarbazepine and MHD have not been evaluated in severe hepatic impairment, and therefore it is not recommended in these patients [see Use in Specific Populations (8.7)].
Pregnant Women
Due to physiological changes during pregnancy, MHD plasma levels may gradually decrease throughout pregnancy [see Use in Specific Populations (8.1)].
Drug Interaction Studies
In Vitro:
Oxcarbazepine can inhibit CYP2C19 and induce CYP3A4/5 with potentially important effects on plasma concentrations of other drugs. In addition, several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD.
Oxcarbazepine was evaluated in human liver microsomes to determine its capacity to inhibit the major cytochrome P450 enzymes responsible for the metabolism of other drugs. Results demonstrate that oxcarbazepine and its pharmacologically active 10-monohydroxy metabolite (MHD) have little or no capacity to function as inhibitors for most of the human cytochrome P450 enzymes evaluated (CYP1A2, CYP2A6, CYP2C9, CYP2D6, CYP2E1, CYP4A9 and CYP4A11) with the exception of CYP2C19 and CYP3A4/5.
Although inhibition of CYP3A4/5 by oxcarbazepine and MHD did occur at high concentrations, it is not likely to be of clinical significance. The inhibition of CYP2C19 by oxcarbazepine and MHD, is clinically relevant.
In vitro, the UDP-glucuronyl transferase level was increased, indicating induction of this enzyme. Increases of 22% with MHD and 47% with oxcarbazepine were observed. As MHD, the predominant plasma substrate, is only a weak inducer of UDP-glucuronyl transferase, it is unlikely to have an effect on drugs that are mainly eliminated by conjugation through UDP-glucuronyl transferase (e.g., valproic acid, lamotrigine).
In addition, oxcarbazepine and MHD induce a subgroup of the cytochrome P450 3A family (CYP3A4 and CYP3A5) responsible for the metabolism of dihydropyridine calcium antagonists, oral contraceptives and cyclosporine resulting in a lower plasma concentration of these drugs.
Several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. No autoinduction has been observed with immediate-release oxcarbazepine.
As binding of MHD to plasma proteins is low (40%), clinically significant interactions with other drugs through competition for protein binding sites are unlikely.
In Vivo:
Other Antiepileptic Drugs
Potential interactions between immediate-release oxcarbazepine and other AEDs were assessed in clinical studies. The effect of these interactions on mean AUCs and Cmin are summarized in Table 5 [see Drug Interactions (7.1, 7.2)].
Table 5: AED Drug Interactions with Immediate-Release (IR) Oxcarbazepine 1nc denotes a mean change of less than 10%
2Pediatrics
3Mean increase in adults at high doses of immediate-release oxcarbazepine
AED
Coadministered (daily dosage)
Immediate–Release-
Oxcarbazepine (daily dosage)
Influence of Immediate–Release - Oxcarbazepine on AED Concentration Mean Change [90% Confidence Interval]
Influence of AED on MHD Concentration (Mean Change, 90% Confidence Interval)
Carbamazepine
(400 mg to 2,000 mg)
900 mg
nc1
40% decrease
[CI: 17% decrease,
57% decrease]
Phenobarbital
(100 mg to 150 mg)
600 mg to 1,800 mg
14% increase
[CI: 2% increase,
24% increase]
25% decrease
[CI: 12% decrease,
51% decrease]
Phenytoin
(250 mg to 500 mg)
600 mg to 1,800 mg
> 1,200 mg to 2,400 mg
nc1,2
up to 40% increase3
[CI: 12% increase,
60% increase]
30% decrease
[CI: 3% decrease,
48% decrease]
Valproic Acid
(400 mg to 2,800 mg)
600 mg to 1,800 mg
nc1
18% decrease
[CI: 13% decrease,
40% decrease]
Lamotrigine
(200 mg)
1,200 mg
nc1
nc1
Hormonal Contraceptives
Coadministration of immediate-release oxcarbazepine with an oral contraceptive has been shown to influence the plasma concentrations of two components of hormonal contraceptives, ethinylestradiol (EE) and levonorgestrel (LNG). The mean AUC values of EE were decreased by 48% [90% CI: 22-65] in one study and 52% [90% CI: 38-52] in another study. The mean AUC values of LNG were decreased by 32% [90% CI: 20-45] in one study and 52% [90% CI: 42-52] in another study.
Other Drug Interactions
Calcium Antagonists: After repeated coadministration of immediate-release oxcarbazepine, the AUC of felodipine was lowered by 28% [90% CI: 20-33]. Verapamil produced a decrease of 20% [90% CI: 18-27] of the plasma levels of MHD after coadministration with immediate-release oxcarbazepine.
Cimetidine, erythromycin and dextropropoxyphene had no effect on the pharmacokinetics of MHD after coadministration with immediate-release oxcarbazepine. Results with warfarin show no evidence of interaction with either single or repeated doses of immediate-release oxcarbazepine.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In two-year carcinogenicity studies, oxcarbazepine was administered in the diet at doses of up to 100 mg/kg/day to mice and by gavage at doses of up to 250 mg/kg/day to rats, and the pharmacologically active 10-hydroxy metabolite (MHD) was administered orally at doses of up to 600 mg/kg/day to rats. In mice, a dose-related increase in the incidence of hepatocellular adenomas was observed at oxcarbazepine doses ≥ 70 mg/kg/day or approximately 0.1 times the maximum recommended human dose (MRHD) on a mg/m2 basis. In rats, the incidence of hepatocellular carcinomas was increased in females treated with oxcarbazepine at doses ≥ 25 mg/kg/day (0.1 times the MRHD on a mg/m2 basis), and incidences of hepatocellular adenomas and/or carcinomas were increased in males and females treated with MHD at doses of 600 mg/kg/day (2.4 times the MRHD on a mg/m2 basis) and ≥ 250 mg/kg/day (equivalent to the MRHD on a mg/m2 basis), respectively. There was an increase in the incidence of benign testicular interstitial cell tumors in rats at 250 mg oxcarbazepine/kg/day and at ≥ 250 mg MHD/kg/day, and an increase in the incidence of granular cell tumors in the cervix and vagina in rats at 600 mg MHD/kg/day.
Mutagenesis
Oxcarbazepine increased mutation frequencies in the Ames test in vitro in the absence of metabolic activation in one of five bacterial strains. Both oxcarbazepine and MHD produced increases in chromosomal aberrations and polyploidy in the Chinese hamster ovary assay in vitro in the absence of metabolic activation. MHD was negative in the Ames test, and no mutagenic or clastogenic activity was found with either oxcarbazepine or MHD in V79 Chinese hamster cells in vitro. Oxcarbazepine and MHD were both negative for clastogenic or aneugenic effects (micronucleus formation) in an in vivo rat bone marrow assay.
Impairment of Fertility
In a fertility study in which rats were administered MHD (50 mg/kg, 150 mg/kg, or 450 mg/kg) orally prior to and during mating and early gestation, estrous cyclicity was disrupted and numbers of corpora lutea, implantations, and live embryos were reduced in females receiving the highest dose (approximately two times the MRHD on a mg/m2 basis).
-
14 CLINICAL STUDIES
Oxcarbazepine extended-release tablets has been evaluated as adjunctive therapy for partial-onset seizures in adults. The use of oxcarbazepine extended-release tablets for the treatment of partial-onset seizures in pediatric patients 6 years of age and older is based on adequate and well-controlled studies of oxcarbazepine extended-release tablets in adults, along with clinical trials of immediate-release oxcarbazepine in pediatric patients, and on pharmacokinetic evaluations of the use of oxcarbazepine extended-release tablets in pediatric patients.
14.1 Oxcarbazepine Extended-Release Tablets Primary Trial
A multicenter, randomized, double-blind, placebo-controlled, three-arm, parallel-group study (Study 1) in male and female adults with refractory partial-onset seizures (18 years to 65 years of age, inclusive) was performed to examine the safety and efficacy of oxcarbazepine extended-release tablets.
Patients had at least three partial-onset seizures per 28 days during an 8 week Baseline Period. Subjects were receiving treatment with at least one to three antiepileptic drugs and were on stable treatment for a minimum of 4 weeks. Subjects with a diagnosis other than partial-onset seizures were excluded.
The study included an 8 week Baseline Period, followed by a Treatment Period, which included a 4 week Titration Phase followed by a 12 week Maintenance Phase. The primary endpoint of the study was median percentage change from baseline in seizure frequency per 28 days during the treatment period relative to the baseline period. The criterion for statistical significance was p < 0.05. A total of 366 patients were enrolled at 88 sites in North America and Eastern Europe. Subjects were randomized to one of three treatment groups and took oxcarbazepine extended-release tablets (1,200 mg/day or 2,400 mg/day) or placebo.
Table 6 presents the primary efficacy results by treatment group.
Table 6: Primary Efficacy Results in Study 1: Percent Change from Baseline in Partial-Onset Seizure Frequency in the 16-week Treatment Period *Wilcoxon rank-sum test of the median percentage change in partial-onset seizure frequency per 28 days during the 16-week Treatment Phase (Titration + Maintenance Periods) relative to the 8-week Baseline Phase.
Median seizure frequency during 8-week baseline period (per 28 days)
Median seizure frequency during 16-week treatment period (per 28 days)
Median percent change in seizure frequency
Seizure frequency percent change effect size
P value vs placebo*
Placebo (N=121)
7.0
5.0
-28.7 %
Oxcarbazepine Extended-Release Tablets
1,200 mg/day
(N=122)
6.0
4.3
-38.2 %
9.5%
0.078
Oxcarbazepine Extended-Release Tablets
2,400 mg/day
(N=123)
6.0
3.7
-42.9 %
14.2%
0.003
Although the 1,200 mg/day-placebo contrast did not reach statistical significance, concentration-response analyses reveal that the 1,200 mg/day dosage is an effective dosage.
14.2 Immediate-Release Oxcarbazepine Adjunctive Therapy Trials
The effectiveness of immediate-release oxcarbazepine as an adjunctive therapy for partial-onset seizures in adults was demonstrated at dosages of 600 mg/day, 1,200 mg/day, and 2,400 mg/day (divided twice daily) in a randomized, double-blind, placebo-controlled trial. All dosages resulted in a statistically significant reduction in seizure frequency when compared to placebo (p < 0.05).
The effectiveness of immediate-release oxcarbazepine in dosages of 30 mg/kg/day to 46 mg/kg/day, depending on baseline weight, as an adjunctive therapy for partial-onset seizures in pediatric patients, including patients 6 to less than 17 years of age, was studied in a randomized, double-blind, placebo-controlled trial. Oxcarbazepine in the single weight-based dosage group resulted in a statistically significant reduction in seizure frequency when compared to placebo (p < 0.05).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
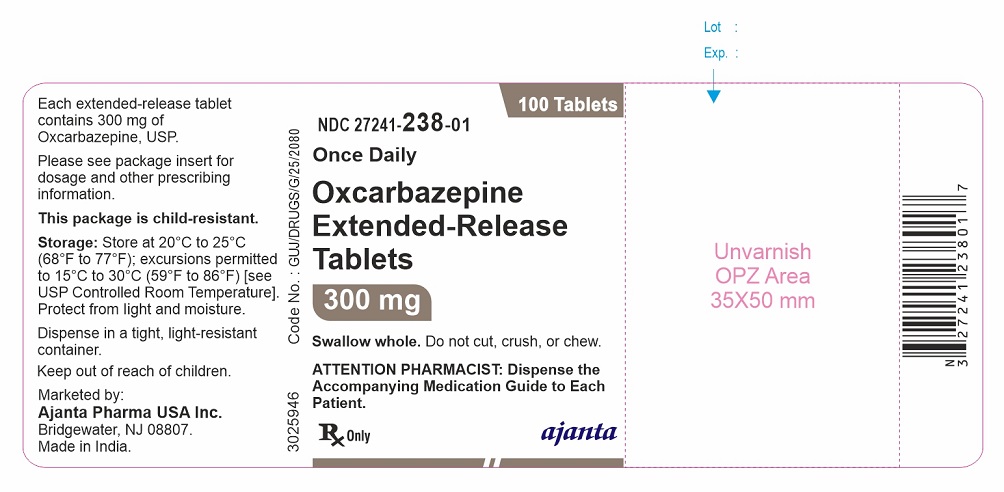
16.1 Dosage Form Supplied
150 mg (yellow oval shaped, biconvex tablet debossed with "XC1" on one side and plain on other side).
Bottles of 100 tablets with child-resistant closure………………………...…...NDC 27241-237-01
300 mg (brown oval shaped, biconvex tablet debossed with "XC2" on one side and plain on other side).
Bottles of 100 tablets with child-resistant closure………………………...…...NDC 27241-238-01
600 mg (brownish red oval shaped, biconvex tablet debossed with "XC3" on one side and plain on other side).
Bottles of 100 tablets with child-resistant closure……………………...……...NDC 27241-239-01
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-Approved patient labeling (Medication Guide).
Administration Information
Advise patients to take the tablet whole. Do not cut, chew, or crush the tablet. Advise patients to take oxcarbazepine extended-release tablets on an empty stomach. This means they should take oxcarbazepine extended-release tablets at least one hour before food or at least two hours after food [see Dosage and Administration (2.1) and Clinical Pharmacology (12.3)].
Hyponatremia
Advise patients that oxcarbazepine extended-release tablets may reduce serum sodium concentrations especially if they are taking other medications that can lower sodium. Advise patients to report symptoms of low sodium like nausea, tiredness, lack of energy, confusion, and more frequent or more severe seizures [see Warnings and Precautions (5.1)].
Anaphylactic Reactions and Angioedema
Anaphylactic reactions and angioedema may occur during treatment with oxcarbazepine extended-release tablets. Advise patients to immediately report signs and symptoms suggesting angioedema (swelling of the face, eyes, lips, tongue, or difficulty in swallowing or breathing) and to stop taking the drug until they have consulted with their physician [see Warnings and Precautions (5.2)].
Cross Hypersensitivity Reaction to Carbamazepine
Inform patients who have exhibited hypersensitivity reactions to carbamazepine that approximately 25% to 30% of these patients may also experience hypersensitivity reactions with oxcarbazepine extended-release tablets. If patients experience a hypersensitivity reaction while taking oxcarbazepine extended-release tablets, advise them to consult with their physician immediately [see Warnings and Precautions (5.3)].
Serious Dermatological Reactions
Advise patients that serious skin reactions have been reported in association with immediate-release oxcarbazepine. If patients experience a skin reaction while taking oxcarbazepine extended-release tablets, advise patients to consult with their physician immediately [see Warnings and Precautions (5.4)].
Suicidal Behavior and Ideation
Counsel patients, their caregivers, and families that AEDs, including oxcarbazepine extended-release tablets, may increase the risk of suicidal thoughts and behavior and that they need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Advise them to immediately report behaviors of concern to healthcare providers [see Warnings and Precautions (5.5)].
DRESS/Multi-Organ Hypersensitivity
Instruct patients that a fever associated with signs of other organ system involvement (e.g., rash, lymphadenopathy, hepatic dysfunction, etc.) occurring during treatment with oxcarbazepine extended-release tablets may be drug-related, and advise them to consult their physician immediately [see Warnings and Precautions (5.7)].
Hematologic Reactions
Advise patients that there have been rare reports of blood disorders reported in patients treated with immediate-release oxcarbazepine. Instruct patients to immediately consult with their physician if they experience symptoms suggestive of blood disorders during treatment with oxcarbazepine extended-release tablets [see Warnings and Precautions (5.8)].
Drug Interactions
Warn female patients of childbearing age that the concurrent use of oxcarbazepine extended-release tablets with hormonal contraceptives may render this method of contraception less effective [see Drug Interactions (7.3) and Use in Specific Populations (8.1)]. Additional non-hormonal forms of contraception are recommended when using oxcarbazepine extended-release tablets.
Oxcarbazepine Extended-Release Tablets are marketed by:
Ajanta Pharma USA Inc.
Bridgewater, NJ 08807.
Made in India.
All other trademark names are the property of their respective owners.
-
MEDICATION GUIDE
Oxcarbazepine (ox kar bay’ ze peen)
extended-release tablets, for oral useWhat is the most important information I should know about oxcarbazepine extended-release tablets?
Do not stop taking oxcarbazepine extended-release tablets without first talking to your healthcare provider. Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems.
Oxcarbazepine extended-release tablets can cause serious side effects, including:
1. Oxcarbazepine extended-release tablets may cause the level of sodium in your blood to be low. Symptoms of low blood sodium include:• nausea
• tiredness, lack of energy
• headache
• confusion
• more frequent or more severe seizures
Similar symptoms that are not related to low sodium may occur from taking oxcarbazepine extended-release tablets. You should tell your healthcare provider if you have any of these side effects and if they bother you or they do not go away.
Some other medicines can also cause low sodium in your blood. Be sure to tell your healthcare provider about all the other medicines that you are taking.
Your healthcare provider may do blood tests to check your sodium levels during your treatment with oxcarbazepine extended-release tablets.
2. Oxcarbazepine extended-release tablets may also cause allergic reactions or serious problems which may affect organs and other parts of your body like the liver or blood cells. You may or may not have a rash with these types of reactions.
Call your healthcare provider right away if you have any of the following:• swelling of your face, eyes, lips, or tongue
• trouble swallowing or breathing
• a skin rash
• hives
• fever, swollen glands, or sore throat that does not go away or comes and goes
• painful sores in the mouth or around your eyes
• yellowing of your skin or eyes
• unusual bruising or bleeding
• severe fatigue or weakness
• severe muscle pain
• frequent infections that do not go away
Many people who are allergic to carbamazepine are also allergic to oxcarbazepine extended-release tablets. Tell your healthcare provider if you are allergic to carbamazepine.
3. Like other antiepileptic drugs, oxcarbazepine extended-release tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call your healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
• thoughts about suicide or dying
• attempts to commit suicide
• new or worse depression
• new or worse anxiety
• feeling agitated or restless
• panic attacks
• trouble sleeping (insomnia)
• new or worse irritability
• acting aggressive, being angry, or violent
• acting on dangerous impulses
• an extreme increase in activity and talking (mania)
• other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Do not stop taking oxcarbazepine extended-release tablets without first talking to a healthcare provider.- Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems.
- Stopping a seizure medicine suddenly in a patient who has epilepsy may cause seizures that will not stop (status epilepticus).
Suicidal thoughts or actions may be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
What are oxcarbazepine extended-release tablets?
Oxcarbazepine extended-release tablets are a prescription medicine used to treat partial onset seizures in adults and children 6 years of age and older.
Oxcarbazepine extended-release tablets is not for use in children under 6 years of age.
It is not known if oxcarbazepine extended-release tablets is safe and effective in children under 6 years of age.Who should not take oxcarbazepine extended-release tablets?
Do not take oxcarbazepine extended-release tablets if you are allergic to oxcarbazepine or any of the other ingredients in oxcarbazepine extended-release tablets, or to eslicarbazepine acetate. See the end of this Medication Guide for a complete list of ingredients in oxcarbazepine extended-release tablets.What should I tell my healthcare provider before taking oxcarbazepine extended-release tablets?
Before taking oxcarbazepine extended-release tablets, tell your healthcare provider about all your medical conditions, including if you:- have or have had suicidal thoughts or actions, depression or mood problems.
- have liver problems.
- have kidney problems.
- are allergic to carbamazepine. Many people who are allergic to carbamazepine are also allergic to oxcarbazepine extended-release tablets.
- use birth control medicine. Oxcarbazepine extended-release tablets may cause your birth control medicine to be less effective. Talk to your healthcare provider about the best birth control method to use.
- are pregnant or plan to become pregnant. Oxcarbazepine extended-release tablets may harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking oxcarbazepine extended-release tablets. You and your healthcare provider will decide if you should take oxcarbazepine extended-release tablets while you are pregnant.
- are breastfeeding or plan to breastfeed. Oxcarbazepine passes into breast milk. Talk with your healthcare provider about the best way to feed your baby if you take oxcarbazepine extended-release tablets.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking oxcarbazepine extended-release tablets with certain other medicines may cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider.
Especially tell your healthcare provider if you take: carbamazepine, phenobarbital, phenytoin, or birth control medicine.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.How should I take oxcarbazepine extended-release tablets?
- Do not stop taking oxcarbazepine extended-release tablets without talking to your healthcare provider. Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems, including seizures that will not stop (status epilepticus).
- Take oxcarbazepine extended-release tablets exactly as prescribed. Your healthcare provider may change your dose. Your healthcare provider will tell you how much oxcarbazepine extended-release tablets to take.
- Take oxcarbazepine extended-release tablets 1 time each day.
- Take oxcarbazepine extended-release tablets on an empty stomach. This means you should take oxcarbazepine extended-release tablets at least 1 hour before or at least 2 hours after a meal.
- Take oxcarbazepine extended-release tablets whole with water or other liquid.
- Do not cut, crush, or chew the tablets before swallowing.
- If you take too much oxcarbazepine extended-release tablets call your healthcare provider right away.
What are the possible side effects of oxcarbazepine extended-release tablets?
See “What is the most important information I should know about oxcarbazepine extended-release tablets?”
Oxcarbazepine extended-release tablets may cause other serious side effects including: seizures that can happen more often or become worse, especially in children.
The most common side effects of oxcarbazepine extended-release tablets include:
• dizziness
• sleepiness
• headache
• balance problems
• tremors
• vomiting
• double vision
• weakness or lack of energy (asthenia)
These are not all the possible side effects of oxcarbazepine extended-release tablets. For more information, ask your healthcare provider or pharmacist.
Tell your healthcare provider if you have any side effect that bothers you or does not go away.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1- 800-FDA-1088.How should I store oxcarbazepine extended-release tablets?
- Oxcarbazepine extended-release tablets comes in a child-resistant package.
- Store oxcarbazepine extended-release tablets at room temperature between 68°F to 77°F (20°C and 25°C).
- Keep oxcarbazepine extended-release tablets in a tightly closed container and out of the light.
- Keep oxcarbazepine extended-release tablets dry.
Keep oxcarbazepine extended-release tablets and all medicines out of the reach of children.
General Information about the safe and effective use of oxcarbazepine extended-release tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use oxcarbazepine extended-release tablets for a condition for which it was not prescribed. Do not give oxcarbazepine extended-release tablets to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your healthcare provider or pharmacist for information about oxcarbazepine extended-release tablets that is written for health professionals.What are the ingredients in oxcarbazepine extended-release tablets?
Active ingredient: oxcarbazepine
Inactive ingredients:
150 mg tablets: colloidal silicon dioxide, hypromellose, hydroxypropyl cellulose, yellow iron oxide, black iron oxide, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, sodium lauryl sulfate, talc, and titanium dioxide.
300 mg tablets: colloidal silicon dioxide, hypromellose, hydroxypropyl cellulose, yellow iron oxide, red iron oxide, black iron oxide, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, sodium lauryl sulfate, talc, and titanium dioxide.
600 mg tablets: colloidal silicon dioxide, hypromellose, hydroxypropyl cellulose, yellow iron oxide, red iron oxide, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, sodium lauryl sulfate, talc, and titanium dioxide.Marketed by:
Ajanta Pharma USA Inc.
Bridgewater, NJ 08807.Made in India.
All other trademark names are the property of their respective owners.
This Medication Guide has been approved by the U.S. Food and Drug Administration
Revised: 01/2023
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 27241-237-01
Once Daily
100 Tablets
Oxcarbazepine Extended-Release Tablets
150 mg
Swallow whole. Do not cut, crush, or chew.
ATTENTION PHARMACIST: Dispense the Accompanying Medication Guide to Each Patient.
Rx Only
ajanta
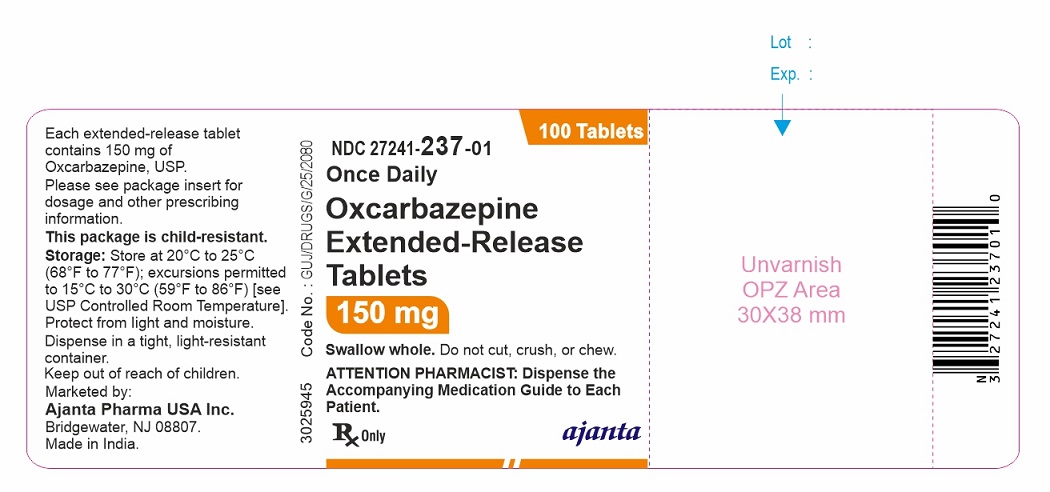
NDC 27241-238-01
Once Daily
100 Tablets
Oxcarbazepine Extended-Release Tablets
300 mg
Swallow whole. Do not cut, crush, or chew.
ATTENTION PHARMACIST: Dispense the Accompanying Medication Guide to Each Patient.
Rx Only
ajanta
NDC 27241-239-01
Once Daily
100 Tablets
Oxcarbazepine Extended-Release Tablets
600 mg
Swallow whole. Do not cut, crush, or chew.
ATTENTION PHARMACIST: Dispense the Accompanying Medication Guide to Each Patient.
Rx Only
ajanta
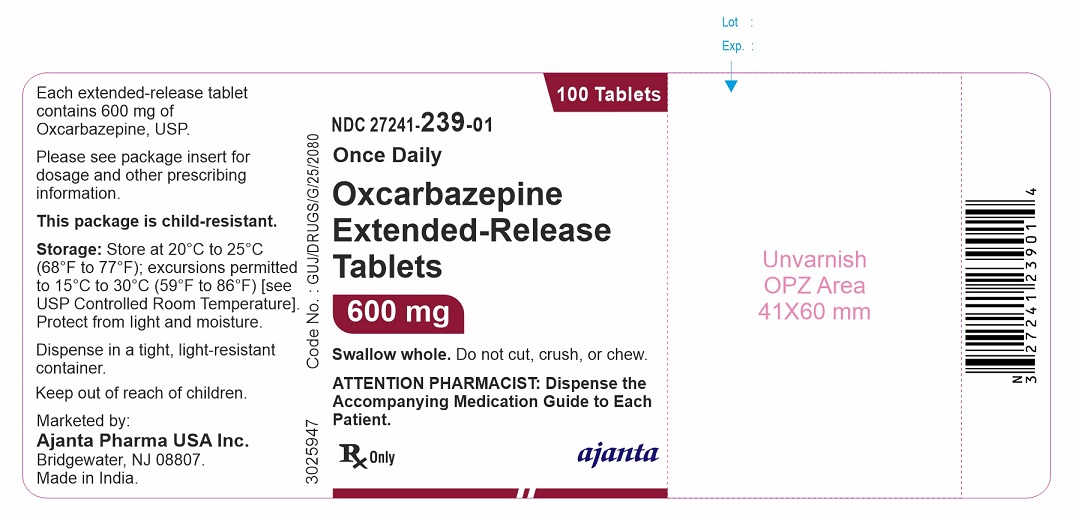
-
INGREDIENTS AND APPEARANCE
OXCARBAZEPINE
oxcarbazepine tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:27241-237 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXCARBAZEPINE (UNII: VZI5B1W380) (OXCARBAZEPINE - UNII:VZI5B1W380) OXCARBAZEPINE 150 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 9XZ8H6N6OH) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color YELLOW Score no score Shape OVAL Size 13mm Flavor Imprint Code XC1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:27241-237-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/22/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA217659 02/22/2024 OXCARBAZEPINE
oxcarbazepine tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:27241-238 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXCARBAZEPINE (UNII: VZI5B1W380) (OXCARBAZEPINE - UNII:VZI5B1W380) OXCARBAZEPINE 300 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 9XZ8H6N6OH) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERROSOFERRIC OXIDE (UNII: XM0M87F357) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE RED (UNII: 1K09F3G675) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color BROWN Score no score Shape OVAL Size 16mm Flavor Imprint Code XC2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:27241-238-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/22/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA217659 02/22/2024 OXCARBAZEPINE
oxcarbazepine tablet, extended releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:27241-239 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXCARBAZEPINE (UNII: VZI5B1W380) (OXCARBAZEPINE - UNII:VZI5B1W380) OXCARBAZEPINE 600 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) HYDROXYPROPYL CELLULOSE, UNSPECIFIED (UNII: 9XZ8H6N6OH) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) FERRIC OXIDE RED (UNII: 1K09F3G675) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color BROWN (Brownish red) Score no score Shape OVAL Size 19mm Flavor Imprint Code XC3 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:27241-239-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/22/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA217659 02/22/2024 Labeler - Ajanta Pharma USA Inc. (557554156) Registrant - Ajanta Pharma Limited, Paithan (918594859) Establishment Name Address ID/FEI Business Operations Ajanta Pharma Ltd., Dahej 862199968 MANUFACTURE(27241-237, 27241-238, 27241-239)