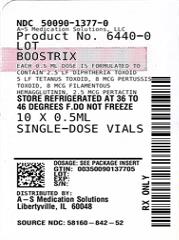
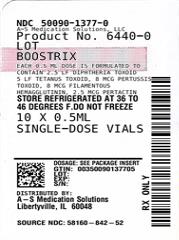
Label: BOOSTRIX- tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine, adsorbed suspension
- NDC Code(s): 50090-1377-0, 50090-1377-1, 50090-1377-2
- Packager: A-S Medication Solutions
- This is a repackaged label.
- Source NDC Code(s): 58160-842
- Category: VACCINE LABEL
- DEA Schedule: None
- Marketing Status: Biologic Licensing Application
Drug Label Information
Updated March 27, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use BOOSTRIX safely and effectively. See full prescribing information for BOOSTRIX.
BOOSTRIX (Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed) injectable suspension, for intramuscular use
Initial U.S. Approval: 2005INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
For intramuscular use only.
- •
- Each dose of BOOSTRIX is administered as a 0.5-mL injection. (2.2)
- •
- An initial dose of BOOSTRIX is administered 5 years or more after the last dose of the Diphtheria and Tetanus Toxoids and Acellular Pertussis (DTaP) series or 5 years or more after a dose of Tetanus and Diphtheria Toxoids Adsorbed (Td). BOOSTRIX may be administered as an additional dose 9 years or more after the initial dose of Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed (Tdap). (2.2)
- •
- BOOSTRIX may be administered for tetanus prophylaxis for wound management. For management of a tetanus-prone wound, a dose of BOOSTRIX may be administered if at least 5 years have elapsed since previous receipt of a tetanus toxoid-containing vaccine. (2.2)
- •
- To provide protection against pertussis in infants younger than 2 months of age, administer BOOSTRIX during the third trimester of pregnancy. (2.2)
DOSAGE FORMS AND STRENGTHS
Single-dose vials and single-dose prefilled syringes containing a 0.5-mL suspension for injection. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- •
- The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions. (5.2)
- •
- If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk of Guillain-Barré syndrome may be increased following a subsequent dose of tetanus toxoid-containing vaccine, including BOOSTRIX. (5.3)
- •
- Progressive or unstable neurologic conditions are reasons to defer vaccination with a pertussis-containing vaccine, including BOOSTRIX. (5.4)
- •
- Persons who experienced an Arthus-type hypersensitivity reaction following a prior dose of a tetanus toxoid-containing vaccine should not receive BOOSTRIX unless at least 10 years have elapsed since the last dose of a tetanus toxoid-containing vaccine. (5.5)
ADVERSE REACTIONS
- •
- Common solicited adverse reactions (≥15%) in adolescents (aged 10 to 18 years) were pain, redness, and swelling at the injection site; increase in arm circumference of the injected arm; headache; fatigue; and gastrointestinal symptoms. (6.1)
- •
- Common solicited adverse reactions (≥15%) in adults (aged 19 to 64 years) were pain, redness, and swelling at the injection site; headache; fatigue; and gastrointestinal symptoms. (6.1)
- •
- The most common solicited adverse reaction (≥15%) in the elderly (aged 65 years and older) was pain at the injection site. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
2.2 Administration, Dose, and Schedule
2.3 Additional Dosing Information
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Severe Allergic Reaction
4.2 Encephalopathy
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
5.2 Latex
5.3 Guillain-Barré Syndrome and Brachial Neuritis
5.4 Progressive or Unstable Neurologic Disorders
5.5 Arthus-Type Hypersensitivity
5.6 Altered Immunocompetence
5.7 Syncope
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Concomitant Vaccine Administration
7.2 Immunosuppressive Therapies
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Effectiveness of BOOSTRIX, INFANRIX, and PEDIARIX
14.2 Immunological Evaluation following an Initial Dose of BOOSTRIX
14.3 Study in Pregnant Women
14.4 Immune Responses to Vaccination in Infants Born to Mothers Who Received BOOSTRIX During Pregnancy
14.5 Immunological Evaluation following Revaccination with BOOSTRIX
14.6 Concomitant Administration with Meningococcal Conjugate Vaccine
14.7 Concomitant Administration with FLUARIX (Inactivated Influenza Vaccine)
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For intramuscular use only.
2.1 Preparation for Administration
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use the vaccine if either of these conditions exist. Shake vigorously to obtain a homogeneous, turbid, white suspension before administration. Do not use if resuspension does not occur with vigorous shaking.
For the prefilled syringes, attach a sterile needle and administer intramuscularly.
For the vials, use a sterile needle and sterile syringe to withdraw the 0.5-mL dose and administer intramuscularly. Changing needles between drawing vaccine from a vial and injecting it into a recipient is not necessary unless the needle has been damaged or contaminated.
2.2 Administration, Dose, and Schedule
BOOSTRIX is administered as a 0.5-mL intramuscular injection into the deltoid muscle of the upper arm.
Active Booster Immunization
An initial dose of BOOSTRIX is administered 5 years or more after the last dose of the Diphtheria and Tetanus Toxoids and Acellular Pertussis (DTaP) series or 5 years or more after a dose of Tetanus and Diphtheria Toxoids Adsorbed (Td).
BOOSTRIX may be administered as an additional dose 9 years or more after the initial dose of Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed (Tdap).
BOOSTRIX may be administered for tetanus prophylaxis for wound management. For management of a tetanus-prone wound, a dose of BOOSTRIX may be administered if at least 5 years have elapsed since previous receipt of a tetanus toxoid-containing vaccine.
Immunization During the Third Trimester of Pregnancy
To prevent pertussis in infants younger than 2 months of age, administer BOOSTRIX to pregnant individuals during the third trimester of pregnancy.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
4.1 Severe Allergic Reaction
Do not administer BOOSTRIX to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of BOOSTRIX or after a previous dose of any tetanus toxoid-, diphtheria toxoid-, or pertussis antigen-containing vaccine [see Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment to manage allergic reactions must be immediately available in the event an acute allergic reaction occurs following administration of BOOSTRIX.
5.2 Latex
The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions.
5.3 Guillain-Barré Syndrome and Brachial Neuritis
If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk of Guillain-Barré syndrome may be increased following a subsequent dose of tetanus toxoid-containing vaccine, including BOOSTRIX. A review by the Institute of Medicine (IOM) found evidence for a causal relationship between receipt of tetanus toxoid and both Guillain-Barré syndrome and brachial neuritis.1
5.4 Progressive or Unstable Neurologic Disorders
Progressive or unstable neurologic conditions (e.g., cerebrovascular events, acute encephalopathic conditions) are reasons to defer vaccination with a pertussis-containing vaccine, including BOOSTRIX. It is not known whether administration of BOOSTRIX to persons with an unstable or progressive neurologic disorder might hasten manifestations of the disorder or affect the prognosis. Administration of BOOSTRIX to persons with an unstable or progressive neurologic disorder may result in diagnostic confusion between manifestations of the underlying illness and possible adverse effects of vaccination.
5.5 Arthus-Type Hypersensitivity
Persons who experienced an Arthus-type hypersensitivity reaction following a prior dose of a tetanus toxoid-containing vaccine usually have a high serum tetanus antitoxin level and should not receive BOOSTRIX or other tetanus toxoid-containing vaccines unless at least 10 years have elapsed since the last dose of tetanus toxoid-containing vaccine.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Table 1 provides an overview of the studies that evaluated the safety of BOOSTRIX in various populations.
Table 1. Studies Conducted with BOOSTRIX and the Non-U.S. Formulation of BOOSTRIX a Non-U.S. formulation of BOOSTRIX contains the same antigens and in the same quantities as BOOSTRIX. The non-U.S. formulation is manufactured to contain 0.5 mg aluminum per dose. The U.S. formulation is manufactured to contain 0.3 mg aluminum per dose. Clinical Studies
Age
Trial Arms (Number of Subjects Vaccinated)
Initial-Dose Studies
U.S. Adolescent Study (NCT00109330)
10 to 18
YearsBOOSTRIX (3,080)
Td (1,034)
German Adolescent Study (NCT00263679)
10 to 12
YearsBOOSTRIX (319)
U.S. Adult Study (NCT00346073)
19 to 64
YearsBOOSTRIX (1,522)
Tdap (762)
U.S Elderly Study (NCT00835237)
≥65
YearsBOOSTRIX (887)
Td (445)
Revaccination Studies (all subjects were vaccinated with BOOSTRIX and trial arms were defined based on initial-dose vaccination; subjects in the Control trial arm received a first dose of BOOSTRIX)
U.S. Revaccination Study – 10 Years after Initial Td or BOOSTRIX Dose (NCT01738477)
20 to 29
YearsBOOSTRIX (128)
Td (37)
U.S. Revaccination Study – 9 Years after Initial BOOSTRIX or Tdap Dose (NCT00489970)
28 to 73
YearsBOOSTRIX (309)
Tdap (138)
Control (362)
Concomitant Vaccine Studies
Concomitant Vaccination with Meningococcal Conjugate Vaccine (MCV4) (NCT00282295)
11 to 18
YearsBOOSTRIX+MCV4 (446)
BOOSTRIX→MCV4 (446)
MCV4→BOOSTRIX (449)
Concomitant Vaccination with Inactivated Trivalent Influenza Vaccine (TIV) (NCT00385255)
19 to 64
YearsBOOSTRIX+TIV (748)
TIV→BOOSTRIX (749)
Study in Pregnant Women
Vaccination During the Third Trimester of Pregnancy (NCT02377349)
18 to 45
YearsNon-U.S. formulation of BOOSTRIX/Tdapa (341)
Placebo (346)In these studies, subjects were monitored for solicited adverse events using standardized diary cards during the 4 days (Days 0 to 3), 8 days (Days 0 to 7), or 15 days (Days 0 to 14) following vaccination. Unsolicited adverse events were monitored for the 31-day period following vaccination (Days 0 to 30).
Serious adverse events were monitored for 6 months post-vaccination in the initial-dose studies (NCT00109330, NCT00263679, NCT00346073, NCT00835237), for the 31-day (Days 0 to 30) period post-vaccination in the revaccination (NCT01738477, NCT00489970) and the concomitant-vaccine administration studies (NCT00282295, NCT00385255), and from vaccination through 2 months after delivery in the study of pregnant individuals (NCT02377349).
Initial-Dose Studies
In clinical studies, 4,949 adolescents (aged 10 to 18 years) and 4,076 adults (aged 19 years and older) were vaccinated with a single dose of BOOSTRIX. Of these adolescents, 1,341 were vaccinated with BOOSTRIX in a coadministration study with meningococcal conjugate vaccine [see Drug Interactions (7.1), Clinical Studies (14.5)]. Of these adults, 1,104 were aged 65 years and older [see Clinical Studies (14.2)]. A total of 860 adults aged 19 years and older received concomitant vaccination with BOOSTRIX and influenza vaccines in a coadministration study [see Drug Interactions (7.1), Clinical Studies (14.6)].
Solicited Adverse Events in the U.S. Adolescent Study: Table 2 presents the solicited local adverse reactions and general adverse events within 15 days of vaccination with BOOSTRIX or Td vaccine for the total vaccinated cohort.
The primary safety endpoint was the incidence of Grade 3 pain (spontaneously painful and/or prevented normal activity) at the injection site within 15 days of vaccination. Grade 3 pain was reported in 4.6% of those who received BOOSTRIX compared with 4.0% of those who received the Td vaccine. The difference in rate of Grade 3 pain was within the pre-defined clinical limit for non-inferiority (upper limit of the 95% CI for the difference [BOOSTRIX minus Td] ≤4%).
Table 2. Rates of Solicited Local Adverse Reactions or General Adverse Events within the 15-Daya Post-Vaccination Period in Adolescents Aged 10 to 18 Years (Total Vaccinated Cohort) Td = Tetanus and Diphtheria Toxoids Adsorbed manufactured by MassBiologics.
n = Number of subjects in the total vaccinated cohort with local/general symptoms sheets completed.
Grade 2 = Local: painful when limb moved; General: interfered with normal activity.
Grade 3 = Local: spontaneously painful and/or prevented normal activity; General: prevented normal activity.
a Day of vaccination and the next 14 days.
b Statistically significantly higher (P <0.05) following BOOSTRIX as compared with Td vaccine.
c Grade 3 injection site pain following BOOSTRIX was not inferior to Td vaccine (upper limit of 2-sided 95% CI for the difference [BOOSTRIX minus Td] in the percentage of subjects ≤4%).
d Mid-upper region of the vaccinated arm.
e Gastrointestinal symptoms included nausea, vomiting, diarrhea, and/or abdominal pain.
f Oral temperatures or axillary temperatures.Adverse Reactions/Adverse Events
BOOSTRIX
(n = 3,032)
%
Td
(n = 1,013)
%
Local
Pain, anyb
75
72
Pain, Grade 2 or 3b
51
43
Pain, Grade 3c
5
4
Redness, any
23
20
Redness, >20 mm
4
4
Redness, ≥50 mm
2
2
Swelling, any
21
20
Swelling, >20 mm
5
5
Swelling, ≥50 mm
3
3
Arm circumference increase, >5 mmd
28
30
Arm circumference increase, >20 mmd
2
2
Arm circumference increase, >40 mmd
1
0.3
General
Headache, any
43
42
Headache, Grade 2 or 3b
16
13
Headache, Grade 3
4
3
Fatigue, any
37
37
Fatigue, Grade 2 or 3
14
13
Fatigue, Grade 3
4
3
Gastrointestinal symptoms, anye
26
26
Gastrointestinal symptoms, Grade 2 or 3e
10
10
Gastrointestinal symptoms, Grade 3e
3
3
Fever, ≥99.5°F (37.5°C)f
14
13
Fever, >100.4°F (38.0°C)f
5
5
Fever, >102.2°F (39.0°C)f
1
1
Unsolicited Adverse Events in the U.S. Adolescent Study: The incidence of unsolicited adverse events reported in the 31 days after vaccination was comparable between the 2 groups (25.4% and 24.5% for BOOSTRIX and Td vaccine, respectively).
Solicited Adverse Events in the German Adolescent Study: BOOSTRIX was administered to 319 children aged 10 to 12 years previously vaccinated with 5 doses of acellular pertussis antigen-containing vaccines; 193 of these subjects received 5 doses of INFANRIX (Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed). Table 3 presents the rates of solicited local adverse reactions and fever within 15 days of vaccination for those subjects who had previously been vaccinated with 5 doses of INFANRIX. No cases of whole arm swelling were reported. Two individuals (2/193) reported large injection site swelling (range: 110 to 200 mm diameter), in 1 case associated with Grade 3 pain. Neither individual sought medical attention. These episodes were reported to resolve without sequelae within 5 days.
Table 3. Rates of Solicited Local Adverse Reactions and Fever Reported within the 15-Daya Post-Vaccination Period following Administration of BOOSTRIX in Adolescents Aged 10 to 12 Years Who Had Previously Received 5 Doses of INFANRIX INFANRIX = Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed manufactured by GlaxoSmithKline Biologics.
n = Number of subjects with local/general symptoms sheets completed.
Grade 2 = Painful when limb moved.
Grade 3 = Spontaneously painful and/or prevented normal activity.
a Day of vaccination and the next 14 days.
b Oral temperatures or axillary temperatures.Adverse Reactions and Fever
BOOSTRIX
(n = 193)
%
Pain, any
62
Pain, Grade 2 or 3
33
Pain, Grade 3
6
Redness, any
48
Redness, >20 mm
15
Redness, ≥50 mm
11
Swelling, any
39
Swelling, >20 mm
18
Swelling, ≥50 mm
14
Fever, ≥99.5°F (37.5°C)b
9
Fever, >100.4°F (38.0°C)b
4
Fever, >102.2°F (39.0°C)b
1
Solicited Adverse Events in the U.S. Adult (Aged 19 to 64 Years) Study: Table 4 presents solicited local adverse reactions and general adverse events within 15 days of vaccination with BOOSTRIX or the comparator Tdap vaccine for the total vaccinated cohort.
Table 4. Rates of Solicited Local Adverse Reactions or General Adverse Events within the 15-Daya Post-Vaccination Period in Adults Aged 19 to 64 Years (Total Vaccinated Cohort) Tdap = ADACEL (Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed, a Tdap vaccine manufactured by Sanofi Pasteur).
n = Number of subjects in the total vaccinated cohort with local/general symptoms sheets completed.
Grade 2 = Local: painful when limb moved; General: interfered with normal activity.
Grade 3 = Local/General: prevented normal activity.
a Day of vaccination and the next 14 days.
b Gastrointestinal symptoms included nausea, vomiting, diarrhea, and/or abdominal pain.
c Oral temperatures.Adverse Reactions/Adverse Events
BOOSTRIX
(n = 1,480)
%
Tdap
(n = 741)
%
Local
Pain, any
61
69
Pain, Grade 2 or 3
35
44
Pain, Grade 3
2
2
Redness, any
21
27
Redness, >20 mm
4
6
Redness, ≥50 mm
2
2
Swelling, any
18
26
Swelling, >20 mm
4
6
Swelling, ≥50 mm
1
3
General
Headache, any
30
31
Headache, Grade 2 or 3
11
11
Headache, Grade 3
2
2
Fatigue, any
28
29
Fatigue, Grade 2 or 3
9
9
Fatigue, Grade 3
3
1
Gastrointestinal symptoms, anyb
16
18
Gastrointestinal symptoms, Grade 2 or 3b
4
6
Gastrointestinal symptoms, Grade 3b
1
1
Fever, ≥99.5°F (37.5°C)c
6
8
Fever, >100.4°F (38.0°C)c
1
2
Fever, >102.2°F (39.0°C)c
0.1
0.4
Unsolicited Adverse Events in the U.S. Adult (Aged 19 to 64 Years) Study: The incidence of unsolicited adverse events reported in the 31 days after vaccination was comparable between the 2 groups (17.8% and 22.2% for BOOSTRIX and Tdap vaccine, respectively).
Solicited Adverse Events in the U.S. Elderly (Aged 65 Years and Older) Study: Table 5 presents solicited local adverse reactions and general adverse events within 4 days of vaccination with BOOSTRIX or the comparator Td vaccine for the total vaccinated cohort.
Table 5. Rates of Solicited Local Adverse Reactions or General Adverse Events within 4 Daysa of Vaccination in the Elderly Aged 65 Years and Older (Total Vaccinated Cohort) Td = DECAVAC (Tetanus and Diphtheria Toxoids Adsorbed, a U.S.-licensed Td vaccine, manufactured by Sanofi Pasteur).
n = Number of subjects with a documented dose.
Grade 2 = Local: painful when limb moved; General: interfered with normal activity.
Grade 3 = Local/General: prevented normal activity.
a Day of vaccination and the next 3 days.
b Gastrointestinal symptoms included nausea, vomiting, diarrhea, and/or abdominal pain.
c Oral temperatures.Adverse Reactions/Adverse Events
BOOSTRIX
%
Td
%
Local
(n = 882)
(n = 444)
Pain, any
22
28
Pain, Grade 2 or 3
8
10
Pain, Grade 3
0.2
1
Redness, any
11
13
Redness, >20 mm
1
3
Redness, ≥50 mm
1
1
Swelling, any
8
12
Swelling, >20 mm
2
3
Swelling, ≥50 mm
1
1
General
(n = 882)
(n = 445)
Fatigue, any
13
15
Fatigue, Grade 2 or 3
3
3
Fatigue, Grade 3
1
1
Headache, any
12
12
Headache, Grade 2 or 3
2
2
Headache, Grade 3
1
0
Gastrointestinal symptoms, anyb
8
9
Gastrointestinal symptoms, Grade 2 or 3b
2
2
Gastrointestinal symptoms, Grade 3b
0.3
0.4
Fever, ≥99.5°F (37.5°C)c
2
3
Fever, >100.4°F (38.0°C)c
0.2
0.2
Fever, >102.2°F (39.0°C)c
0
0
Unsolicited Adverse Events in the U.S. Elderly (Aged 65 Years and Older) Study: The incidence of unsolicited adverse events reported in the 31 days after vaccination was comparable between the 2 groups (17.1% and 14.4% for BOOSTRIX and Td vaccine, respectively).
Serious Adverse Events (SAEs): In the U.S. and German adolescent safety studies, no serious adverse events were reported to occur within 31 days of vaccination. During the 6-month extended safety evaluation period, no serious adverse events that were of potential autoimmune origin or new onset and chronic in nature were reported to occur. In non-U.S. adolescent studies in which serious adverse events were monitored for up to 37 days, 1 subject was diagnosed with insulin-dependent diabetes 20 days following administration of BOOSTRIX. No other serious adverse events of potential autoimmune origin or that were new onset and chronic in nature were reported to occur in these studies. In the U.S. adult (aged 19 to 64 years) study, serious adverse events were reported to occur during the entire study period (0-6 months) by 1.4% and 1.7% of subjects who received BOOSTRIX and the comparator Tdap vaccine, respectively. During the 6-month extended safety evaluation period, no serious adverse events of a neuroinflammatory nature or with information suggesting an autoimmune etiology were reported in subjects who received BOOSTRIX. In the U.S. elderly (aged 65 years and older) study, serious adverse events were reported to occur by 0.7% and 0.9% of subjects who received BOOSTRIX and the comparator Td vaccine, respectively, during the 31-day period after vaccination. Serious adverse events were reported to occur by 4.2% and 2.2% of subjects who received BOOSTRIX and the comparator Td vaccine, respectively, during the 6-month period after vaccination.
Revaccination Studies
U.S. Revaccination Studies in Adults: In 2 clinical studies, 974 adults (aged 20 years and older) were vaccinated with a dose of BOOSTRIX [see Clinical Studies (14.4)].
Solicited Adverse Events in the U.S. Revaccination Studies: Table 6 presents solicited local adverse reactions and general adverse events within 4 days of vaccination with BOOSTRIX for the total vaccinated cohort in both studies.
Table 6. Rates of Solicited Local Adverse Reactions or General Adverse Events within 4 Daysa of Vaccination in Adults Aged 20 to 73 Years (Total Vaccinated Cohort) Td = Tetanus and Diphtheria Toxoids Adsorbed for Adult Use manufactured by MassBiologics.
Tdap = ADACEL (Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed, a Tdap vaccine manufactured by Sanofi Pasteur).
n = Number of subjects with a documented dose.
Grade 2 = Local: painful when limb moved and interfered with normal activities; General: interfered with normal activity.
Grade 3 = Local: significant pain at rest and/or prevented normal activity; General: prevented normal activity.
a Day of vaccination and the next 3 days.
b Subjects who were revaccinated with BOOSTRIX 10 years after initial vaccination with BOOSTRIX.
c Subjects who received a dose of BOOSTRIX 10 years after initial vaccination with Td vaccine.
d Subjects who were revaccinated with BOOSTRIX 9 years after initial vaccination with BOOSTRIX.
e Subjects who received a dose of BOOSTRIX 9 years after initial vaccination with Tdap vaccine.
f Control Group = Newly enrolled subjects who received an initial dose of BOOSTRIX.
g In the study of adults aged 20 to 29 years, redness >50 mm was recorded.
h In the study of adults aged 20 to 29 years, swelling >50 mm was recorded.
i Gastrointestinal symptoms included nausea, vomiting, diarrhea, and/or abdominal pain.
j Oral temperatures.Adverse Reactions/
Adverse EventsAdults Aged 20 to 29 Years
Adults Aged 28 to 73 Years
BOOSTRIXb
(n = 125)
%
Tdc
(n = 36)
%
BOOSTRIXd
(n = 306)
%
Tdape
(n = 137)
%
Controlf
(n = 358)
%
Local
Pain, any
78
58
59
61
37
Pain, Grade 2 or 3
33
19
17
15
9
Pain, Grade 3
5
6
1
1
1
Redness, any
38
42
24
23
15
Redness, >20 mm
4
0
6
4
1
Redness, ≥50 mmg
1
0
2
2
0
Swelling, any
24
19
19
19
12
Swelling, >20 mm
2
3
3
3
3
Swelling, ≥50 mmh
0
0
1
2
1
General
Headache, any
32
22
17
18
15
Headache, Grade 2 or 3
10
3
4
4
2
Headache, Grade 3
2
0
0
1
0.3
Fatigue, any
30
22
23
17
14
Fatigue, Grade 2 or 3
14
3
8
7
3
Fatigue, Grade 3
2
0
1
1
0
Gastrointestinal symptoms, anyi
9
3
9
3
8
Gastrointestinal symptoms, Grade 2 or 3i
2
0
2
0
3
Gastrointestinal symptoms, Grade 3i
2
0
0
0
0
Fever, ≥100.4°F (38.0°C)j
1
0
1
0
1
Fever, >102.2°F (39.0°C)j
0
0
0.3
0
0
Concomitant Vaccination with Meningococcal Conjugate Vaccine in Adolescents
Table 7 presents the percentages of subjects experiencing local reactions at the injection site for BOOSTRIX and solicited general events following BOOSTRIX. The incidence of unsolicited adverse events reported in the 31 days after any vaccination was similar following each dose of BOOSTRIX in all cohorts.
Table 7. Rates of Solicited Local Adverse Reactions or General Adverse Events Reported within the 4-Day Post-Vaccination Period following Administration of BOOSTRIX in Individuals Aged 11 to 18 Years (Total Vaccinated Cohort) MCV4 = MENACTRA (Meningococcal [Groups A, C, Y, and W-135] Polysaccharide Diphtheria Toxoid Conjugate Vaccine), Sanofi Pasteur.
n = Number of subjects in the total vaccinated cohort with local/general symptoms sheets completed.
a BOOSTRIX+MCV4 = Concomitant vaccination with BOOSTRIX and MENACTRA.
b BOOSTRIX→MCV4 = BOOSTRIX followed by MCV4 1 month later.
c MCV4→BOOSTRIX = MCV4 followed by BOOSTRIX 1 month later.
d Gastrointestinal symptoms included nausea, vomiting, diarrhea, and/or abdominal pain.
e Oral temperatures.Adverse Reactions/Adverse Events
BOOSTRIX+MCV4a
(n = 441)
%
BOOSTRIX→MCV4b
(n = 432-433)
%
MCV4→BOOSTRIXc
(n = 441)
%
Local (at injection site for BOOSTRIX)
Pain, any
70
70
48
Redness, any
23
26
18
Swelling, any
18
18
12
General (following administration of BOOSTRIX)
Fatigue
34
32
20
Headache
34
31
17
Gastrointestinal symptomsd
15
15
8
Fever, ≥99.5°F (37.5°C)e
5
4
2
Vaccination During Pregnancy
Safety of non-U.S. formulation BOOSTRIX (0.5 mg aluminum/per dose) during the third trimester of pregnancy was evaluated in study NCT02377349. The safety data with the non-U.S. formulation are relevant because the non-U.S. formulation of BOOSTRIX contains the same antigens and in the same quantities as BOOSTRIX. However, the non-U.S. formulation contains more aluminum per dose (see Table 1).
In the randomized, controlled study NCT02377349, 687 pregnant individuals received the non-U.S. formulation of BOOSTRIX or placebo during the third trimester (341 non-U.S. formulation of BOOSTRIX, 346 placebo [saline]). The placebo recipients received the non-U.S. formulation of BOOSTRIX postpartum. The rates of reported solicited adverse reactions following receipt of the non-U.S. formulation of BOOSTRIX administered during pregnancy were consistent with the rates following receipt of the non-U.S. formulation of BOOSTRIX administered to study participants postpartum. For further information about pregnancy outcomes [see Use in Specific Populations (8.1)].
6.2 Postmarketing Experience
In addition to reports in clinical trials for BOOSTRIX, the following adverse events have been identified in persons aged 10 years and older during postapproval use of BOOSTRIX worldwide. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the vaccine.
Blood and Lymphatic System Disorders
Lymphadenitis, lymphadenopathy.
Immune System Disorders
Allergic reactions, including anaphylactic and anaphylactoid reactions.
Cardiac Disorders
Myocarditis.
General Disorders and Administration Site Conditions
Extensive swelling of the injected limb, injection site induration, injection site inflammation, injection site mass, injection site pruritus, injection site nodule, injection site warmth, injection site reaction.
Musculoskeletal and Connective Tissue Disorders
Arthralgia, back pain, myalgia.
Nervous System Disorders
Convulsions (with and without fever), encephalitis, facial palsy, loss of consciousness, paresthesia, syncope.
Skin and Subcutaneous Tissue Disorders
Angioedema, exanthem, Henoch-Schönlein purpura, rash, urticaria.
-
7 DRUG INTERACTIONS
7.1 Concomitant Vaccine Administration
In a clinical study of participants 11 to 18 years of age, BOOSTRIX was administered concomitantly with MENACTRA [see Clinical Studies (14.5)]. Post-vaccination geometric mean antibody concentrations (GMCs) to pertactin (PRN) were lower following BOOSTRIX administered concomitantly with meningococcal conjugate vaccine compared with BOOSTRIX administered first. It is not known if the efficacy of BOOSTRIX is affected by the reduced response to PRN.
In a clinical study of adults 19 to 64 years of age, BOOSTRIX was administered concomitantly with FLUARIX (Influenza Virus Vaccine) [see Clinical Studies (14.6)]. Lower GMCs for antibodies to the pertussis antigens filamentous hemagglutinin (FHA) and PRN were observed when BOOSTRIX was administered concomitantly with FLUARIX as compared with BOOSTRIX alone. It is not known if the efficacy of BOOSTRIX is affected by the reduced response to FHA and PRN.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to BOOSTRIX during pregnancy. Healthcare providers are encouraged to register women by calling 1-888-452-9622 or visiting http://pregnancyregistry.gsk.com/boostrix.html.
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
In a randomized, controlled clinical study (NCT02377349), in which the non-U.S. formulation of BOOSTRIX was administered during the third trimester of pregnancy, there were no identified vaccine-related adverse effects on pregnancy or on the fetus/newborn child (see Data).
Available data from the pregnancy registry and from spontaneous and postmarketing reports suggest that the rates of major birth defects and miscarriage in women who received BOOSTRIX within 28 days prior to conception or during pregnancy are consistent with estimated background rates (see Data).
A developmental toxicity study was performed in female rats administered INFANRIX prior to mating and BOOSTRIX during gestation, 0.1 mL at each occasion (a single human dose is 0.5 mL). In a second study, female rats were administered 0.2 mL of BOOSTRIX prior to mating and during the gestation and lactation period. In a third study, female New Zealand White rabbits were given 0.5 mL (full human dose) of BOOSTRIX (non-U.S. formulation) prior to mating and during gestation. These studies revealed no evidence of harm to the fetus due to BOOSTRIX (see Data).
Data
Human Data: Safety data from a randomized (1:1), controlled clinical study (NCT02377349) (341 non-U.S. formulation of BOOSTRIX, 346 placebo pregnancy outcomes) in which the non-U.S. formulation of BOOSTRIX was administered to pregnant women during the third trimester did not reveal any vaccine-related adverse effects on pregnancy or on the fetus/newborn child. Safety data from prospective clinical studies on the use of BOOSTRIX during the first and second trimester of pregnancy are not available.
An assessment of data from the U.S. pregnancy exposure registry over approximately 17 years (2005-2022) included 1,523 prospective reports of exposure to BOOSTRIX within 28 days prior to conception or during pregnancy. Among the 256 reports with known pregnancy outcomes, 19 women were exposed to BOOSTRIX in the first trimester with no major birth defects reported and 3 spontaneous abortions with no apparent birth defect; 28 women were exposed to BOOSTRIX in the second trimester, and 199 women were exposed to BOOSTRIX in the third trimester with no major birth defects reported; 10 women were exposed to BOOSTRIX at an unknown timing in pregnancy with no major birth defects reported.
An assessment of U.S. spontaneous reports and postmarketing data included 810 prospective reports of exposure to BOOSTRIX during pregnancy since May 2005 through 31 August 2022. Among the 138 reports with known pregnancy outcomes, 17 women were exposed to BOOSTRIX in the first trimester with no major birth defects reported and 2 spontaneous abortions with no apparent birth defect; 26 women were exposed to BOOSTRIX in the second trimester, and 92 women were exposed to BOOSTRIX in the third trimester with no major birth defects reported; 3 women were exposed to BOOSTRIX at an unknown timing in pregnancy with no major birth defects reported.
Animal Data: Developmental toxicity studies were performed in female rats and New Zealand White rabbits. In one study, female rats were administered 0.1 mL of INFANRIX (a single human dose is 0.5 mL) by intramuscular injection 30 days prior to mating and 0.1 mL of BOOSTRIX (a single human dose is 0.5 mL) by intramuscular injection on Gestation Days 6, 8, 11, and 15. The antigens in INFANRIX are the same as those in BOOSTRIX, but INFANRIX is formulated with higher quantities of these antigens. In a second study, female rats were administered 0.2 mL of BOOSTRIX by intramuscular injection 28 days and 14 days prior to mating, on Gestation Days 3, 8, 11, and 15, and on Lactation Day 7. In these studies, no adverse effects on embryo-fetal or pre-weaning development up to Postnatal Day 25 were observed; there were no fetal malformations or variations observed. In a third study, female New Zealand White rabbits were administered 0.5 mL (full human dose) of BOOSTRIX (non-U.S. formulation) by intramuscular injection on Premating Days -28 and -14 and on Gestation Days 3, 8, 11, 15, and 24. In this study, no adverse effects on embryo-fetal development related to BOOSTRIX were observed; postnatal development was not evaluated.
8.2 Lactation
Risk Summary
It is not known whether the vaccine components of BOOSTRIX are excreted in human milk. Data are not available to assess the effect of administration of BOOSTRIX on breastfed infants or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for BOOSTRIX and any potential adverse effects on the breastfed child from BOOSTRIX or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
BOOSTRIX is not indicated for use in children aged younger than 10 years. Safety and effectiveness of BOOSTRIX in this age group have not been established.
8.5 Geriatric Use
In the initial-dose clinical trials, 1,104 subjects aged 65 years and older received BOOSTRIX; of these subjects, 299 were aged 75 years and older. Adverse events following BOOSTRIX were similar in frequency to those reported with the comparator Td vaccine [see Adverse Reactions (6.1)].
A revaccination study of BOOSTRIX in adults aged 28 to 73 years [see Clinical Studies (14.4)] did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects.
-
11 DESCRIPTION
BOOSTRIX (Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed) is a noninfectious, sterile, vaccine for intramuscular administration. It contains tetanus toxoid, diphtheria toxoid, and pertussis antigens (inactivated pertussis toxin [PT] and formaldehyde-treated FHA and PRN). The antigens are the same as those in INFANRIX, but BOOSTRIX is formulated with reduced quantities of these antigens.
Tetanus toxin is produced by growing Clostridium tetani (C. tetani) in a modified Latham medium derived from bovine casein. The diphtheria toxin is produced by growing Corynebacterium diphtheriae (C. diphtheriae) in Fenton medium containing a bovine extract. The bovine materials used in these extracts are sourced from countries which the United States Department of Agriculture (USDA) has determined neither have nor are at risk of bovine spongiform encephalopathy (BSE). Both toxins are detoxified with formaldehyde, concentrated by ultrafiltration, and purified by precipitation, dialysis, and sterile filtration.
The acellular pertussis antigens (PT, FHA, and PRN) are isolated from Bordetella pertussis (B. pertussis) culture grown in modified Stainer-Scholte liquid medium. PT and FHA are isolated from the fermentation broth; PRN is extracted from the cells by heat treatment and flocculation. The antigens are purified in successive chromatographic and precipitation steps. PT is detoxified using glutaraldehyde and formaldehyde. FHA and PRN are treated with formaldehyde.
Each antigen is individually adsorbed onto aluminum hydroxide. Each 0.5-mL dose is formulated to contain 5 Lf of tetanus toxoid, 2.5 Lf of diphtheria toxoid, 8 mcg of inactivated PT, 8 mcg of FHA, and 2.5 mcg of PRN (69 kiloDalton outer membrane protein).
Tetanus and diphtheria toxoid potency is determined by measuring the amount of neutralizing antitoxin in previously immunized guinea pigs. The potency of the acellular pertussis components (inactivated PT and formaldehyde-treated FHA and PRN) is determined by enzyme-linked immunosorbent assay (ELISA) on sera from previously immunized mice.
Each 0.5-mL dose contains aluminum hydroxide as adjuvant (formulated to contain 0.3 mg aluminum) and 4.4 mg of sodium chloride. The aluminum content is measured by assay. Each dose also contains ≤100 mcg of residual formaldehyde and ≤100 mcg of polysorbate 80 (Tween 80).
BOOSTRIX is available in vials and prefilled syringes. The tip caps of the prefilled syringes contain natural rubber latex; the plungers are not made with natural rubber latex. The vial stoppers are not made with natural rubber latex.
BOOSTRIX is formulated without preservatives.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Active Immunization
Tetanus is a condition manifested primarily by neuromuscular dysfunction caused by a potent exotoxin released by C. tetani. Protection against disease is due to the development of neutralizing antibodies to the tetanus toxin. A serum tetanus antitoxin level of at least 0.01 IU/mL, measured by neutralization assays, is considered the minimum protective level.2 A level ≥0.1 IU/mL by ELISA has been considered as protective.
Diphtheria is an acute toxin-mediated infectious disease caused by toxigenic strains of C. diphtheriae. Protection against disease is due to the development of neutralizing antibodies to the diphtheria toxin. A serum diphtheria antitoxin level of 0.01 IU/mL, measured by neutralization assays, is the lowest level giving some degree of protection; a level of 0.1 IU/mL by ELISA is regarded as protective. Diphtheria antitoxin levels ≥1.0 IU/mL by ELISA have been associated with long-term protection.3
Pertussis (whooping cough) is a disease of the respiratory tract caused by B. pertussis. The role of the different components produced by B. pertussis in either the pathogenesis of, or the immunity to, pertussis is not well understood.
Passive Immunization to Prevent Pertussis in Infants
Antibodies to pertussis antigens from individuals vaccinated during the third trimester of pregnancy are transferred transplacentally to prevent pertussis in infants younger than 2 months of age.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
BOOSTRIX has not been evaluated for carcinogenic or mutagenic potential, or for impairment of male fertility in animals. Vaccination of female rabbits and rats with BOOSTRIX had no effect on fertility. [See Use in Specific Populations (8.1).]
-
14 CLINICAL STUDIES
14.1 Effectiveness of BOOSTRIX, INFANRIX, and PEDIARIX
Effectiveness of BOOSTRIX
The effectiveness of the tetanus and diphtheria toxoid components of BOOSTRIX is based on the immunogenicity of the individual antigens compared with U.S.-licensed vaccines using established serologic correlates of protection. The effectiveness of the pertussis components of BOOSTRIX was evaluated by comparison of the immune response of adolescents and adults following an initial dose of BOOSTRIX to the immune response of infants following a 3-dose primary series of INFANRIX or by comparison of the immune response of adults following an additional dose of BOOSTRIX to the immune response of infants following a 3-dose primary series of PEDIARIX. In addition, the ability of BOOSTRIX to induce a booster response to each of the antigens was evaluated.
Efficacy of INFANRIX Against Pertussis
The efficacy of a 3-dose primary series of INFANRIX in infants has been assessed in 2 clinical studies: A prospective efficacy trial conducted in Germany employing a household contact study design and a double-blind, randomized, active Diphtheria and Tetanus Toxoids (DT)-controlled trial conducted in Italy sponsored by the National Institutes of Health (NIH) (for details see INFANRIX prescribing information). In the household contact study, the protective efficacy of INFANRIX in infants against WHO-defined pertussis (21 days or more of paroxysmal cough with infection confirmed by culture and/or serologic testing) was calculated to be 89% (95% CI: 77%, 95%). When the definition of pertussis was expanded to include clinically milder disease, with infection confirmed by culture and/or serologic testing, the efficacy of INFANRIX against ≥7 days of any cough was 67% (95% CI: 52%, 78%) and against ≥7 days of paroxysmal cough was 81% (95% CI: 68%, 89%) (for details see INFANRIX prescribing information).
Immune Responses to Pertussis Antigens of PEDIARIX Compared with INFANRIX
The diphtheria, tetanus, and pertussis components in PEDIARIX are the same as those in INFANRIX. The effectiveness of the pertussis component of PEDIARIX was determined in clinical trials by comparison to antibody responses to INFANRIX (for details see PEDIARIX prescribing information).
Immune Responses to Pertussis Antigens of BOOSTRIX Compared with INFANRIX or PEDIARIX
Although a serologic correlate of protection for pertussis has not been established, serological data from a subset of infants immunized with a 3-dose primary series of INFANRIX in the German household contact study were compared with the sera of adolescents and adults immunized with an initial dose of BOOSTRIX [see Clinical Studies (14.2)]. Serological data from infants immunized with a 3-dose primary series of PEDIARIX in an additional pediatric study were compared with the sera of adults immunized with an additional dose of BOOSTRIX [see Clinical Studies (14.4)]. The GMCs to each of the pertussis antigens 1 month following a dose of BOOSTRIX were compared with the GMCs of infants following INFANRIX administered at 3, 4, and 5 months of age or were compared with the GMCs of infants following PEDIARIX administered at 2, 4, and 6 months of age. The majority of subjects in the study of INFANRIX had only anti-PT serology data.
14.2 Immunological Evaluation following an Initial Dose of BOOSTRIX
Adolescents (Aged 10 to 18 years)
In a multicenter, randomized, observer-blinded, controlled study conducted in the United States (NCT00109330), the immune responses to each of the antigens contained in BOOSTRIX were evaluated in sera obtained approximately 1 month after administration of a single dose of vaccine to adolescent subjects (aged 10 to 18 years). Of the subjects enrolled in this study, approximately 76% were aged 10 to 14 years and 24% were aged 15 to 18 years. Approximately 98% of participants in this study had received the recommended series of 4 or 5 doses of either DTwP or a combination of DTwP and DTaP in childhood. The racial/ethnic demographics were as follows: White 85.8%, Black 5.7%, Hispanic 5.6%, Oriental 0.8%, and other 2.1%.
Response to Tetanus and Diphtheria Toxoids: The antibody responses to the tetanus and diphtheria toxoids of BOOSTRIX compared with Td vaccine are shown in Table 8. One month after a single dose, anti-tetanus and anti-diphtheria seroprotective rates (≥0.1 IU/mL by ELISA) and booster response rates were comparable between BOOSTRIX and the comparator Td vaccine.
Table 8. Antibody Responses to Tetanus and Diphtheria Toxoids following BOOSTRIX Compared with Td Vaccine in Adolescents Aged 10 to 18 Years (ATP Cohort for Immunogenicity) Td = Tetanus and Diphtheria Toxoids, Adsorbed manufactured by MassBiologics.
ATP = According-to-protocol; CI = Confidence Interval.
a Measured by ELISA.
b Booster response: In subjects with pre-vaccination <0.1 IU/mL, post-vaccination concentration ≥0.4 IU/mL. In subjects with pre-vaccination concentration ≥0.1 IU/mL, an increase of at least 4 times the pre-vaccination concentration.
c Seroprotection rate or booster response rate to BOOSTRIX was non-inferior to Td (upper limit of 2-sided 95% CI on the difference for Td minus BOOSTRIX ≤10%).
d Non-inferiority criteria not prospectively defined for this endpoint.Antibodies
n
% ≥0.1 IU/mLa
(95% CI)
% ≥1.0 IU/mLa
(95% CI)
% Booster
Responseb(95% CI)
Anti-tetanus
BOOSTRIX
2,469-2,516
Pre-vaccination
97.7 (97.1, 98.3)
36.8 (34.9, 38.7)
–
Post-vaccination
100 (99.8, 100)c
99.5 (99.1, 99.7)d
89.7 (88.4, 90.8)c
Td
817-834
Pre-vaccination
96.8 (95.4, 97.9)
39.9 (36.5, 43.4)
–
Post-vaccination
100 (99.6, 100)
99.8 (99.1, 100)
92.5 (90.5, 94.2)
Anti-diphtheria
BOOSTRIX
2,463-2,515
Pre-vaccination
85.8 (84.3, 87.1)
17.1 (15.6, 18.6)
–
Post-vaccination
99.9 (99.7, 100)c
97.3 (96.6, 97.9)d
90.6 (89.4, 91.7)c
Td
814-834
Pre-vaccination
84.8 (82.1, 87.2)
19.5 (16.9, 22.4)
–
Post-vaccination
99.9 (99.3, 100)
99.3 (98.4, 99.7)
95.9 (94.4, 97.2)
Response to Pertussis Antigens: The booster response rates of adolescents to the pertussis antigens are shown in Table 9. For each of the pertussis antigens the lower limit of the 2-sided 95% CI for the percentage of subjects with a booster response exceeded the pre-defined lower limit of 80% for demonstration of an acceptable booster response.
Table 9. Booster Responses to the Pertussis Antigens following BOOSTRIX in Adolescents Aged 10 to 18 Years (ATP Cohort for Immunogenicity) ATP = According-to-protocol; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
a Booster response: In initially seronegative subjects (<5 EL.U./mL), post-vaccination antibody concentrations ≥20 EL.U./mL. In initially seropositive subjects with pre-vaccination antibody concentrations ≥5 EL.U./mL and <20 EL.U./mL, an increase of at least 4 times the pre-vaccination antibody concentration. In initially seropositive subjects with pre-vaccination antibody concentrations ≥20 EL.U./mL, an increase of at least 2 times the pre-vaccination antibody concentration.Pertussis Antibodies
n
BOOSTRIX
% Booster Responsea (95% CI)
Anti-PT
2,677
84.5 (83.0, 85.9)
Anti-FHA
2,744
95.1 (94.2, 95.9)
Anti-PRN
2,752
95.4 (94.5, 96.1)
The GMCs to each of the pertussis antigens 1 month following a single dose of BOOSTRIX were compared with the GMCs of a subset of infants following a 3-dose primary series of INFANRIX in the German household contact study [see Clinical Studies (14.1)]. Table 10 presents the results for the total immunogenicity cohort in both studies (vaccinated subjects with serology data available for at least 1 pertussis antigen). Anti-PT, anti-FHA, and anti-PRN antibody concentrations observed in adolescents 1 month after a single dose of BOOSTRIX were non-inferior to those infants following a primary vaccination series with INFANRIX.
Table 10. Ratio of GMCs to Pertussis Antigens following 1 Dose of BOOSTRIX in Adolescents Aged 10 to 18 Years Compared with 3 Doses of INFANRIX in Infants (Total Immunogenicity Cohort) GMC = Geometric mean antibody concentration, measured in ELISA units; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects for GMC evaluation.
a GMC following BOOSTRIX was non-inferior to GMC following INFANRIX (lower limit of 95% CI for the GMC ratio of BOOSTRIX/INFANRIX >0.67).Pertussis Antibodies
BOOSTRIX
(n)
INFANRIX
(n)
GMC Ratio: BOOSTRIX/INFANRIX
(95% CI)
Anti-PT
2,941
2,884
1.90 (1.82, 1.99)a
Anti-FHA
2,979
685
7.35 (6.85, 7.89)a
Anti-PRN
2,978
631
4.19 (3.73, 4.71)a
Adults (Aged 19 to 64 Years)
A multicenter, randomized, observer-blinded study, conducted in the United States (NCT00346073), evaluated the immunogenicity of BOOSTRIX compared with the licensed comparator Tdap vaccine (Sanofi Pasteur). Vaccines were administered as a single dose to subjects (N = 2,284) who had not received a tetanus-diphtheria booster within 5 years. The immune responses to each of the antigens contained in BOOSTRIX were evaluated in sera obtained approximately 1 month after administration. Approximately 33% of subjects were aged 19 to 29 years, 33% were aged 30 to 49 years, and 34% were aged 50 to 64 years. Among subjects in the combined vaccine groups, 62% were female; 84% of subjects were White, 8% Black, 1% Asian, and 7% were of other racial/ethnic groups.
Response to Tetanus and Diphtheria Toxoids: The antibody responses to the tetanus and diphtheria toxoids of BOOSTRIX compared with the comparator Tdap vaccine are shown in Table 11. One month after a single dose, anti-tetanus and anti-diphtheria seroprotective rates (≥0.1 IU/mL by ELISA) were comparable between BOOSTRIX and the comparator Tdap vaccine.
Table 11. Antibody Responses to Tetanus and Diphtheria Toxoids following 1 Dose of BOOSTRIX Compared with the Comparator Tdap Vaccine in Adults Aged 19 to 64 Years (ATP Cohort for Immunogenicity) Tdap = Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed manufactured by Sanofi Pasteur.
ATP = According-to-protocol; CI = Confidence Interval.
a Measured by ELISA.
b Seroprotection rates for BOOSTRIX were non-inferior to the comparator Tdap vaccine (lower limit of 95% CI on the difference of BOOSTRIX minus Tdap ≥-10%).
c Non-inferiority criteria not prospectively defined for this endpoint.Antibodies
% ≥0.1 IU/mLa
% ≥1.0 IU/mLa
n
(95% CI)
(95% CI)
Anti-tetanus
BOOSTRIX
1,445-1,447
Pre-vaccination
95.9 (94.8, 96.9)
71.9 (69.5, 74.2)
Post-vaccination
99.6 (99.1, 99.8)b
98.3 (97.5, 98.9)b
Tdap
727-728
Pre-vaccination
97.2 (95.8, 98.3)
74.7 (71.4, 77.8)
Post-vaccination
100 (95.5, 100)
99.3 (98.4, 99.8)
Anti-diphtheria
BOOSTRIX
1,440-1,444
Pre-vaccination
85.2 (83.3, 87.0)
23.7 (21.5, 26.0)
Post-vaccination
98.2 (97.4, 98.8)b
87.9 (86.1, 89.5)c
Tdap
720-727
Pre-vaccination
89.2 (86.7, 91.3)
26.5 (23.3, 29.9)
Post-vaccination
98.6 (97.5, 99.3)
92.0 (89.8, 93.9)
Response to Pertussis Antigens: Booster response rates to the pertussis antigens are shown in Table 12. For the FHA and PRN antigens, the lower limit of the 95% CI for the booster responses exceeded the pre-defined limit of 80% demonstrating an acceptable booster response following BOOSTRIX. The PT antigen booster response lower limit of the 95% CI (74.9%) did not exceed the pre-defined limit of 80%.
Table 12. Booster Responses to the Pertussis Antigens following 1 Dose of BOOSTRIX in Adults Aged 19 to 64 Years (ATP Cohort for Immunogenicity) ATP = According-to-protocol; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
a Booster response: In initially seronegative subjects (<5 EL.U./mL), post-vaccination antibody concentrations ≥20 EL.U./mL. In initially seropositive subjects with pre-vaccination antibody concentrations ≥5 EL.U./mL and <20 EL.U./mL, an increase of at least 4 times the pre-vaccination antibody concentration. In initially seropositive subjects with pre-vaccination antibody concentrations ≥20 EL.U./mL, an increase of at least 2 times the pre-vaccination antibody concentration.
b The PT antigen booster response lower limit of the 95% CI did not exceed the pre-defined limit of 80%.
c The FHA and PRN antigens booster response lower limit of the 95% CI exceeded the pre-defined limit of 80%.Pertussis Antibodies
BOOSTRIX
% Booster Responsea
n
(95% CI)
Anti-PT
1,419
77.2 (74.9, 79.3)b
Anti-FHA
1,433
96.9 (95.8, 97.7)c
Anti-PRN
1,441
93.2 (91.8, 94.4)c
The GMCs to each of the pertussis antigens 1 month following a single dose of BOOSTRIX were compared with the GMCs of a subset of infants following a 3-dose primary series of INFANRIX in the German household contact study [see Clinical Studies (14.1)]. Table 13 presents the results for the total immunogenicity cohort in both studies (vaccinated subjects with serology data available for at least 1 pertussis antigen). Anti-PT, anti-FHA, and anti-PRN antibody concentrations observed in adults 1 month after a single dose of BOOSTRIX were non-inferior to those infants following a primary vaccination series with INFANRIX.
Table 13. Ratio of GMCs to Pertussis Antigens following 1 Dose of BOOSTRIX in Adults Aged 19 to 64 Years Compared with 3 Doses of INFANRIX in Infants (Total Immunogenicity Cohort) GMC = Geometric mean antibody concentration; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects for GMC evaluation.
a BOOSTRIX was non-inferior to INFANRIX (lower limit of 95% CI for the GMC ratio of BOOSTRIX/INFANRIX ≥0.67).Pertussis Antibodies
BOOSTRIX
INFANRIX
GMC Ratio: BOOSTRIX/INFANRIX
(n)
(n)
(95% CI)
Anti-PT
1,460
2,884
1.39 (1.32, 1.47)a
Anti-FHA
1,472
685
7.46 (6.86, 8.12)a
Anti-PRN
1,473
631
3.56 (3.10, 4.08)a
Elderly (Aged 65 Years and Older)
The U.S. elderly (aged 65 years and older) study, a randomized, observer-blinded study (NCT00835237), evaluated the immunogenicity of BOOSTRIX (n = 887) compared with a U.S.-licensed comparator Td vaccine (n = 445) (Sanofi Pasteur). Vaccines were administered as a single dose to subjects who had not received a tetanus-diphtheria booster within 5 years. Among all vaccine recipients, the mean age was approximately 72 years; 54% were female and 95% were White. The immune responses to each of the antigens contained in BOOSTRIX were evaluated in sera obtained approximately 1 month after administration.
Response to Tetanus and Diphtheria Toxoids: Immune responses to tetanus and diphtheria toxoids were measured 1 month after administration of a single dose of BOOSTRIX or a comparator Td vaccine. Anti-tetanus and anti-diphtheria seroprotective rates (≥0.1 IU/mL) were comparable between BOOSTRIX and the comparator Td vaccine (Table 14).
Table 14. Immune Responses to Tetanus and Diphtheria Toxoids following BOOSTRIX or Comparator Td Vaccine in the Elderly Aged 65 Years and Older (ATP Cohort for Immunogenicity) Td = Tetanus and Diphtheria Toxoids Adsorbed, a U.S.-licensed Td vaccine, manufactured by Sanofi Pasteur.
ATP = According-to-protocol; CI = Confidence Interval.
a Seroprotection rates for BOOSTRIX were non-inferior to the comparator Td vaccine (lower limit of 95% CI on the difference of BOOSTRIX minus Td ≥-10%).
b Non-inferiority criteria not prospectively defined for this endpoint.Anti-Tetanus and Anti-Diphtheria Titers
BOOSTRIX
Td
(n = 844-864)
(n = 430-439)
Anti-tetanus
% ≥0.1 IU/mL (95% CI)
96.8 (95.4, 97.8)a
97.5 (95.6, 98.7)
% ≥1.0 IU/mL (95% CI)
88.8 (86.5, 90.8)a
90.0 (86.8, 92.6)
Anti-diphtheria
% ≥0.1 IU/mL (95% CI)
84.9 (82.3, 87.2)a
86.6 (83.0, 89.6)
% ≥1.0 IU/mL (95% CI)
52.0 (48.6, 55.4)b
51.2 (46.3, 56.0)
Response to Pertussis Antigens: The GMCs to each of the pertussis antigens 1 month following a single dose of BOOSTRIX were compared with the GMCs of a subset of infants following a 3-dose primary series of INFANRIX in the German household contact study [see Clinical Studies (14.1)]. Table 15 presents the results for the total immunogenicity cohort in both studies (vaccinated subjects with serology data available for at least 1 pertussis antigen). Anti-PT, anti-FHA, and anti-PRN antibody concentrations in the elderly 1 month after a single dose of BOOSTRIX were non-inferior to those of infants following a primary vaccination series with INFANRIX.
Table 15. Ratio of GMCs to Pertussis Antigens following 1 Dose of BOOSTRIX in the Elderly Aged 65 Years and Older Compared with 3 Doses of INFANRIX in Infants (Total Immunogenicity Cohort) GMC = Geometric mean antibody concentration; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects for GMC evaluation.
a BOOSTRIX was non-inferior to INFANRIX (lower limit of 95% CI for the GMC ratio of BOOSTRIX/INFANRIX ≥0.67).Pertussis Antibodies
BOOSTRIX
INFANRIX
GMC Ratio: BOOSTRIX/INFANRIX
(n)
(n)
(95% CI)
Anti-PT
865
2,884
1.07 (1.00, 1.15)a
Anti-FHA
847
685
8.24 (7.45, 9.12)a
Anti-PRN
878
631
0.93 (0.79, 1.10)a
14.3 Study in Pregnant Women
The effectiveness of BOOSTRIX immunization during the third trimester of pregnancy to prevent pertussis among infants younger than 2 months of age was based on a re-analysis within a Bayesian meta-analysis framework of the BOOSTRIX-relevant data from an observational case-control study of Tdap vaccine effectiveness.4 In this re-analysis, a conditional logistic regression model controlling for age, maternal education, and family size was fit to data from 108 cases (including 4 cases whose mothers received BOOSTRIX during the third trimester) and 183 controls (including 18 whose mothers received BOOSTRIX during the third trimester) matched by age group (<2 weeks old, ≥2 weeks old) and birth hospital. This yielded a preliminary vaccine effectiveness estimate of 78.0% (95% CI: -38.0, 96.5) for vaccination during the third trimester of pregnancy. This preliminary effectiveness estimate was updated using a Bayesian meta-analysis with an informative prior constructed from four observational studies that provided estimates of the vaccine effectiveness of the non-U.S. formulation of BOOSTRIX against pertussis in infants whose mothers were immunized during pregnancy.5, 6, 7, 8 To account for potential publication bias, this informative prior was downweighted by combining it with an uninformative prior. When the informative prior has 20% weight, the Bayesian update resulted in estimates of effectiveness of vaccination during the third trimester of pregnancy of 81.5% (95% credible interval:12.9, 94.5). When the informative prior has 90% weight, the Bayesian update resulted in estimates of effectiveness of vaccination during the third trimester of pregnancy of 83.4% (95% credible interval: 55.7, 92.5). The vaccine effectiveness point estimates were consistent, regardless of the weight applied to the informative prior.
14.4 Immune Responses to Vaccination in Infants Born to Mothers Who Received BOOSTRIX During Pregnancy
Data are not available on immune responses to US licensed vaccines administered on the US schedule among infants born to mothers who received BOOSTRIX during pregnancy.
In infants whose mothers received BOOSTRIX (non-US formulation) during the third trimester of pregnancy, antibody responses to a non-US licensed DTaP-containing vaccine were diminished for anti-PT, anti-FHA and anti-PRN following the primary series (NCT 02422264), and for anti-PT and anti-FHA following a booster dose (NCT 02853929) compared to infants who received the same vaccine but whose mothers received placebo during pregnancy. Whether the diminished immune responses observed in vaccinated infants whose mothers received BOOSTRIX (non-US formulation) during pregnancy result in diminished effectiveness of pertussis vaccination in infants is unknown.
14.5 Immunological Evaluation following Revaccination with BOOSTRIX
Adults (Aged 20 to 29 Years)
A multicenter, open-label, controlled study conducted in the United States evaluated the immunogenicity of BOOSTRIX in adults aged 20 to 29 years who received an initial dose of BOOSTRIX (n = 128) or the comparator Td vaccine (MassBiologics) (n = 37) in the U.S. adolescent (aged 10 to 18 years) study (NCT01738477). BOOSTRIX was administered to all subjects 10 years after initial vaccination. The immune responses to each of the antigens contained in BOOSTRIX were evaluated in sera obtained approximately 1 month after vaccine administration. Among all vaccine recipients, the mean age was 23.5 years; 45.5% were female, and 87.9% were White.
Response to Tetanus and Diphtheria Toxoids: The antibody responses to the tetanus and diphtheria toxoids of BOOSTRIX are shown in Table 16. One month after vaccination, anti-tetanus and anti-diphtheria seroprotective rates (≥0.1 IU/mL by ELISA) were comparable between groups.
Table 16. Antibody Responses to Tetanus and Diphtheria Toxoids following BOOSTRIX in Adults Aged 20 to 29 Years (ATP Cohort for Immunogenicity) Td manufactured by MassBiologics.
ATP = According-to-protocol; CI = Confidence Interval.
n = Number of subjects with available results.
a Measured by ELISA.
b Subjects who were revaccinated with BOOSTRIX 10 years after initial vaccination with BOOSTRIX.
c Seroprotection rates following revaccination with BOOSTRIX were non-inferior to an initial dose of BOOSTRIX (Td group) (lower limit of 2-sided 95% CI on the difference for second dose of BOOSTRIX minus first dose of BOOSTRIX ≥-10%).
d Non-inferiority criteria not prospectively defined for this endpoint.
e Subjects who received a dose of BOOSTRIX 10 years after initial vaccination with Td vaccine.% ≥0.1 IU/mLa
% ≥1.0 IU/mLa
Antibodies
n
(95% CI)
(95% CI)
Anti-tetanus
BOOSTRIXb
115
Pre-vaccination
100 (96.8, 100)
74.8 (65.8, 82.4)
Post-vaccination
100 (96.8, 100)c
100 (96.8, 100)d
Tde
35
Pre-vaccination
100 (90, 100)
77.1 (59.9, 89.6)
Post-vaccination
100 (90, 100)
100 (90, 100)
Anti-diphtheria
BOOSTRIXb
115
Pre-vaccination
100 (96.8, 100)
60.9 (51.3, 69.8)
Post-vaccination
100 (96.8, 100)c
100 (96.8, 100)d
Tde
35
Pre-vaccination
100 (90, 100)
65.7 (47.8, 80.9)
Post-vaccination
100 (90,100)
97.1 (85.1, 99.9)
Response to Pertussis Antigens: The GMCs to each of the pertussis antigens 1 month following revaccination with BOOSTRIX in subjects who had received an initial dose of BOOSTRIX 10 years earlier were compared with the GMCs of infants following a 3-dose primary series of PEDIARIX [see Clinical Studies (14.1)]. Table 17 presents the results for the ATP cohort for immunogenicity in both studies. Anti-PT, anti-FHA, and anti-PRN antibody concentrations observed in adults 1 month after revaccination with BOOSTRIX were non-inferior to those of infants following a primary vaccination series with PEDIARIX.
Table 17. Ratio of GMCs to Pertussis Antigens following BOOSTRIX in Adults Aged 20 to 29 Years Compared with 3 Doses of PEDIARIX in Infants (ATP Cohort for Immunogenicity) GMC = Geometric mean antibody concentration; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects for GMC evaluation.
a Subjects who were revaccinated with BOOSTRIX 10 years after initial vaccination with BOOSTRIX.
b BOOSTRIX was non-inferior to PEDIARIX (lower limit of 95% CI for the GMC ratio of BOOSTRIX/PEDIARIX ≥0.67).BOOSTRIXa
PEDIARIX
GMC Ratio: BOOSTRIX/PEDIARIX
Pertussis Antibodies
(n)
(n)
(95% CI)
Anti-PT
115
149
1.81 (1.48, 2.21)b
Anti-FHA
115
149
2.37 (1.98, 2.83)b
Anti-PRN
115
149
9.87 (7.80, 12.49)b
Adults (Aged 28 to 73 Years)
A multicenter, open-label, controlled study conducted in the United States evaluated the immunogenicity of BOOSTRIX in adults aged 28 to 73 years who received an initial dose of BOOSTRIX (n = 309) or the licensed comparator Tdap vaccine (Sanofi Pasteur) (n = 138) in the U.S. adult (aged 19 to 64 years) study (NCT00489970). BOOSTRIX was administered to all subjects 9 years after initial vaccination. A control group of newly enrolled adult subjects received an initial dose of BOOSTRIX (n = 362). The immune responses to each of the antigens contained in BOOSTRIX were evaluated in sera obtained approximately 1 month after vaccine administration. Of the subjects enrolled in this study, the mean age was 52.1 years; 62.6% were female, and 86.6% were White.
Response to Tetanus and Diphtheria Toxoids: The antibody responses to the tetanus and diphtheria toxoids of BOOSTRIX are shown in Table 18. One month after vaccination, anti-tetanus and anti-diphtheria seroprotective rates (≥0.1 IU/mL by ELISA) were comparable between groups.
Table 18. Antibody Responses to Tetanus and Diphtheria Toxoids following BOOSTRIX in Adults Aged 28 to 73 Years (ATP Cohort for Immunogenicity) Tdap = Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed manufactured by Sanofi Pasteur.
ATP = According-to-protocol; CI = Confidence Interval.
n = Number of subjects with available results.
a Measured by ELISA.
b Booster response: In subjects with pre-vaccination <0.1 IU/mL, post-vaccination concentration ≥0.4 IU/mL. In subjects with pre-vaccination concentration ≥0.1 IU/mL, an increase of at least 4 times the pre-vaccination concentration.
c Subjects who were revaccinated with BOOSTRIX 9 years after initial vaccination with BOOSTRIX.
d Seroprotection rates following a dose of BOOSTRIX in subjects who had received an initial dose of BOOSTRIX or the licensed comparator Tdap vaccine were non-inferior to an initial dose of BOOSTRIX (Control Group) (lower limit of 97.5% CI on the difference of BOOSTRIX minus Control Group ≥-10%).
e Non-inferiority criteria not prospectively defined for this endpoint.
f The booster response rates following a dose of BOOSTRIX in subjects who had received an initial dose of BOOSTRIX or the licensed comparator Tdap vaccine did not meet the pre-defined non-inferiority criteria (lower limit of the 97.5% CIs ≥-10% [BOOSTRIX minus Control Group] and [Tdap minus Control Group]).
g Subjects who received a dose of BOOSTRIX 9 years after initial vaccination with Tdap vaccine.
h Control Group = Newly enrolled subjects who received an initial dose of BOOSTRIX.Antibodies
n
% ≥0.1 IU/mLa
(95% CI)
% ≥1.0 IU/mLa
(95% CI)
% Booster Responseb
(95% CI)
Anti-tetanus
BOOSTRIXc
268-271
Pre-vaccination
98.1 (95.7, 99.4)
78.7 (73.3, 83.5)
Post-vaccination
100 (98.6, 100)d
99.3 (97.4, 99.9)e
47.0 (40.9, 53.2)f
Tdapg
120-121
Pre-vaccination
100 (97.0, 100)
84.2 (76.4, 90.2)
Post-vaccination
100 (97.0, 100)d
100 (97.0, 100)e
36.7 (28.1, 45.9)f
Controlh
324-327
Pre-vaccination
93.8 (90.6, 96.2)
71.3 (66.0, 76.2)
Post-vaccination
99.7 (98.3, 100)
97.6 (95.2, 98.9)
48.5 (42.9, 54.0)
Anti-diphtheria
BOOSTRIXc
269-271
Pre-vaccination
91.1 (87.0, 94.2)
42.4 (36.4, 48.5)
Post-vaccination
99.3 (97.4, 99.9)d
91.9 (88.0, 94.8)e
62.8 (56.7, 68.6)f
Tdapg
118-121
Pre-vaccination
95.8 (90.4, 98.6)
45.8 (36.6, 55.2)
Post-vaccination
99.2 (95.5, 100)d
93.4 (87.4, 97.1)e
60.2 (50.7, 69.1)f
Controlh
324-326
Pre-vaccination
81.8 (77.1, 85.8)
28.4 (23.5, 33.6)
Post-vaccination
97.9 (95.6, 99.1)
86.5 (82.3, 90.0)
68.7 (63.4, 73.7)
Response to Pertussis Antigens: The GMCs to each of the pertussis antigens 1 month following a dose of BOOSTRIX in subjects who had received an initial dose of BOOSTRIX or the licensed comparator Tdap vaccine (Sanofi Pasteur) 9 years earlier were compared with the GMCs of infants following a 3-dose primary series of PEDIARIX [see Clinical Studies (14.1)].Table 19 presents the results for the ATP cohort for immunogenicity in both studies. Anti-PT, anti-FHA, and anti-PRN antibody concentrations observed in adults 1 month after a dose of BOOSTRIX were non-inferior to those of infants following a primary vaccination series with PEDIARIX.
Table 19. Ratio of GMCs to Pertussis Antigens following BOOSTRIX in Adults Aged 28 to 73 Years Compared with 3 Doses of PEDIARIX in Infants (ATP Cohort for Immunogenicity) Tdap = Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed manufactured by Sanofi Pasteur.
GMC = Geometric mean antibody concentration; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects for GMC evaluation.
a BOOSTRIX was non-inferior to PEDIARIX (lower limit of 97.5% CI for the GMC ratio of BOOSTRIX/PEDIARIX ≥0.67).Pertussis Antibodies
Vaccinated with BOOSTRIX 9 Years after Initial Vaccination with:
PEDIARIX
(n)
GMC Ratio:
BOOSTRIX
(n)
Tdap
(n)
BOOSTRIX/
PEDIARIX
(97.5% CI)
Tdap/
PEDIARIX
(97.5% CI)
Anti-PT
271
121
149
1.33
(1.09, 1.61)a
1.46
(1.14, 1.87)a
Anti-FHA
271
121
149
2.02
(1.72, 2.37)a
2.07
(1.68, 2.57)a
Anti-PRN
271
121
149
8.64
(6.85, 10.89)a
10.90
(8.27, 14.38)a
Compared with the Control Group, non-inferiority of booster response rates to the pertussis antigens following a dose of BOOSTRIX in subjects who had received an initial dose of BOOSTRIX or another licensed Tdap vaccine (Sanofi Pasteur) was achieved for the PT antigen [BOOSTRIX minus Control Group] and the FHA antigen [Tdap minus Control Group], respectively (Table 20). Non-inferiority was not achieved for FHA and PRN booster response rates [BOOSTRIX minus Control Group] or for PT and PRN booster response rates [Tdap minus Control Group].
Table 20. Booster Responses to the Pertussis Antigens following BOOSTRIX in Adults Aged 28 to 73 Years (ATP Cohort for Immunogenicity) Tdap = Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed manufactured by Sanofi Pasteur.
ATP = According-to-protocol; CI = Confidence Interval; PT = Pertussis toxin; FHA = Filamentous hemagglutinin; PRN = Pertactin.
n = Number of subjects with available results.
a Booster response: In initially seronegative subjects (pre-vaccination antibody concentration below the assay cut-off), post-vaccination antibody concentrations ≥4 times the assay cut-off. In initially seropositive subjects with pre-vaccination antibody concentrations <4 times the assay cut-off, an increase of at least 4 times the pre-vaccination antibody concentration. In initially seropositive subjects with pre-vaccination antibody concentrations ≥4 times the assay cut-off, an increase of at least 2 times the pre-vaccination antibody concentration. Assay cut-offs: anti-PT = 2.693 IU/mL; anti-FHA = 2.046 IU/mL; anti-PRN = 2.187 IU/mL.
b Subjects who were revaccinated with BOOSTRIX 9 years after initial vaccination with BOOSTRIX.
c Non-inferiority of the booster response rate for each pertussis antigen was demonstrated if the lower limit of the 97.5% CI [BOOSTRIX minus Control Group] or [Tdap minus Control Group] was above the pre-defined limit of -10%.
d Subjects who received a dose of BOOSTRIX 9 years after initial vaccination with Tdap vaccine.
e Control Group = Newly enrolled subjects who received an initial dose of BOOSTRIX.Pertussis Antibodies
n
% Booster Responsea
(95% CI)
Difference in Booster Response Rates
BOOSTRIX minus
Control Group
(97.5 % CI)
Tdap minus Control Group (97.5% CI)
Anti-PT
BOOSTRIXb
271
86.7 (82.1, 90.5)
-2.85 (-9.09, 3.08)c
Tdapd
120
88.3 (81.2, 93.5)
-1.24 (-10.03, 5.57)
Controle
326
89.6 (85.7, 92.7)
Anti-FHA
BOOSTRIXb
271
85.6 (80.9, 89.6)
-7.05 (-13.16, -1.40)
Tdapd
120
96.7 (91.7, 99.1)
4.01 (-2.38, 8.66)c
Controle
327
92.7 (89.3, 95.2)
Anti-PRN
BOOSTRIXb
271
77.5 (72.0, 82.3)
-10.32 (-17.50, -3.38)
Tdapd
118
83.1 (75.0, 89.3)
-4.76 (-14.53, 3.18)
Controle
320
87.8 (83.7, 91.2)
14.6 Concomitant Administration with Meningococcal Conjugate Vaccine
The concomitant use of BOOSTRIX and a tetravalent meningococcal (groups A, C, Y, and W-135) conjugate vaccine (Sanofi Pasteur) was evaluated in a randomized study in healthy adolescents aged 11 to 18 years (NCT00282295). A total of 1,341 adolescents were vaccinated with BOOSTRIX. Of these, 446 subjects received BOOSTRIX administered concomitantly with meningococcal conjugate vaccine at different injection sites, 446 subjects received BOOSTRIX followed by meningococcal conjugate vaccine 1 month later, and 449 subjects received meningococcal conjugate vaccine followed by BOOSTRIX 1 month later.
Immune responses to diphtheria and tetanus toxoids (% of subjects with anti-tetanus and anti-diphtheria antibodies ≥1.0 IU/mL by ELISA), pertussis antigens (booster responses and GMCs), and meningococcal antigens (vaccine responses) were measured 1 month (range: 30 to 48 days) after concomitant or separate administration of BOOSTRIX and meningococcal conjugate vaccine. For BOOSTRIX given concomitantly with meningococcal conjugate vaccine compared with BOOSTRIX administered first, non-inferiority was demonstrated for all antigens, with the exception of the anti-PRN GMC. The lower limit of the 95% CI for the GMC ratio was 0.54 for anti-PRN (pre-specified limit ≥0.67). For the anti-PRN booster response, non-inferiority was demonstrated. It is not known if the efficacy of BOOSTRIX is affected by the reduced response to PRN.
There was no evidence that BOOSTRIX interfered with the antibody responses to the meningococcal antigens when measured by rabbit serum bactericidal assays (rSBA) when given concomitantly or sequentially (meningococcal conjugate vaccine followed by BOOSTRIX or BOOSTRIX followed by meningococcal conjugate vaccine).
14.7 Concomitant Administration with FLUARIX (Inactivated Influenza Vaccine)
The concomitant use of BOOSTRIX and FLUARIX was evaluated in a multicenter, open-label, randomized, controlled study (NCT00385255) of 1,497 adults aged 19 to 64 years. In one group, subjects received BOOSTRIX and FLUARIX concurrently (n = 748). The other group received FLUARIX at the first visit, then 1 month later received BOOSTRIX (n = 749). Sera was obtained prior to and 1 month following concomitant or separate administration of BOOSTRIX and/or FLUARIX, as well as 1 month after the separate administration of FLUARIX.
Immune responses following concurrent administration of BOOSTRIX and FLUARIX were non-inferior to separate administration for diphtheria (seroprotection defined as ≥0.1 IU/mL), tetanus (seroprotection defined as ≥0.1 IU/mL and based on concentrations ≥1.0 IU/mL), PT antigen (anti-PT GMC), and influenza antigens (percent of subjects with hemagglutination-inhibition [HI] antibody titer ≥1:40 and ≥4-fold rise in HI titer). Non-inferiority criteria were not met for the anti-pertussis antigens FHA and PRN. The lower limit of the 95% CI of the GMC ratio was 0.64 for anti-FHA and 0.60 for anti-PRN and the pre-specified limit was ≥0.67. It is not known if the efficacy of BOOSTRIX is affected by the reduced response to FHA and PRN.
-
15 REFERENCES
- 1.
- Institute of Medicine (IOM). Stratton KR, Howe CJ, Johnston RB, eds. Adverse events associated with childhood vaccines. Evidence bearing on causality. Washington, DC: National Academy Press; 1994.
- 2.
- Wassilak SGF, Roper MH, Kretsinger K, and Orenstein WA. Tetanus Toxoid. In: Plotkin SA, Orenstein WA, and Offit PA, eds. Vaccines. 5th ed. Saunders; 2008:805-839.
- 3.
- Vitek CR and Wharton M. Diphtheria Toxoid. In: Plotkin SA, Orenstein WA, and Offit PA, eds. Vaccines. 5th ed. Saunders; 2008:139-156.
- 4.
- Skoff TH, Blain AE, Watt J, et al. Impact of the US maternal tetanus, diphtheria, and acellular pertussis vaccination program on preventing pertussis in infants <2 months of age: a case-control evaluation. Clin Infect Dis. 2017; 65 (12): 1977-83.
- 5.
- Bellido-Blasco J, Guiral-Rodrigo S, Míguez-Santiyán A, Salazar-Cifre A, González-Morán F. A case-control study to assess the effectiveness of pertussis vaccination during pregnancy on newborns, Valencian community, Spain, 1 March 2015 to 29 February 2016. Euro Surveill. 2017;22(22).
- 6.
- Saul N, Wang K, Bag S, Baldwin H, Alexander K, Chandra M, et al. Effectiveness of maternal pertussis vaccination in preventing infection and disease in infants: The NSW Public Health Network case-control study. Vaccine. 2018;36(14):1887-1892.
- 7.
- Uriarte PS, Rodríguez SSJ, Sancristobal IG, Agirre NM. Effectiveness of dTpa vaccination during pregnancy in preventing whooping cough in infants under 3 months of age. Bizkaia, Basque Country, Spain. Heliyon. 2019;5(2):e01207.
- 8.
- Andrews A, Campbell H, Riberio S, Fry N, Amirthalingham G. Boostrix-IPV Report: Effectiveness of Maternal Pertussis Vaccination in Prevention of Confirmed Pertussis in Children in England Using the Screening Method Report to 30 September 2018. Public Health England. Unpublished. 2020.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Provide the following information to the vaccine recipient, parent, or guardian:
- •
- Inform of the potential benefits and risks of immunization with BOOSTRIX.
- •
- Inform about the potential for adverse reactions that have been temporally associated with administration of BOOSTRIX or other vaccines containing similar components.
- •
- Instruct vaccine recipient to report any adverse events to their healthcare provider.
- •
- Advise women who receive BOOSTRIX during pregnancy to enroll in the pregnancy registry [see Use in Specific Populations (8.1)].
- •
- Give the Vaccine Information Statements, which are required by the National Childhood Vaccine Injury Act of 1986 prior to immunization. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
-
SPL UNCLASSIFIED SECTION
BOOSTRIX, FLUARIX, INFANRIX, PEDIARIX, and TIP‑LOK are trademarks owned by or licensed to the GSK group of companies. The other brands listed are trademarks owned by or licensed to their respective owners and are not owned by or licensed to the GSK group of companies. The makers of these brands are not affiliated with and do not endorse the GSK group of companies or its products.
Manufactured by GlaxoSmithKline BiologicalsRixensart, Belgium, U.S. License 1617, and
GSK Vaccines GmbH
Marburg, Germany, U.S. License 1617
Distributed by GlaxoSmithKline
Durham, NC 27701
©2022 GSK group of companies or its licensor.
BTX:35PI
- Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed
-
INGREDIENTS AND APPEARANCE
BOOSTRIX
tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine, adsorbed suspensionProduct Information Product Type VACCINE Item Code (Source) NDC:50090-1377(NDC:58160-842) Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: K3W1N8YP13) (CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:K3W1N8YP13) CLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 5 [iU] in 0.5 mL CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: IRH51QN26H) (CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:IRH51QN26H) CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) 2.5 [iU] in 0.5 mL BORDETELLA PERTUSSIS TOXOID ANTIGEN (FORMALDEHYDE, GLUTARALDEHYDE INACTIVATED) (UNII: QSN5XO8ZSU) (BORDETELLA PERTUSSIS TOXOID ANTIGEN (FORMALDEHYDE, GLUTARALDEHYDE INACTIVATED) - UNII:QSN5XO8ZSU) BORDETELLA PERTUSSIS TOXOID ANTIGEN (FORMALDEHYDE, GLUTARALDEHYDE INACTIVATED) 8 ug in 0.5 mL BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: 8C367IY4EY) (BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:8C367IY4EY) BORDETELLA PERTUSSIS FILAMENTOUS HEMAGGLUTININ ANTIGEN (FORMALDEHYDE INACTIVATED) 8 ug in 0.5 mL BORDETELLA PERTUSSIS PERTACTIN ANTIGEN (FORMALDEHYDE INACTIVATED) (UNII: I05O535NV6) (BORDETELLA PERTUSSIS PERTACTIN ANTIGEN (FORMALDEHYDE INACTIVATED) - UNII:I05O535NV6) BORDETELLA PERTUSSIS PERTACTIN ANTIGEN (FORMALDEHYDE INACTIVATED) 2.5 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength ALUMINUM HYDROXIDE (UNII: 5QB0T2IUN0) FORMALDEHYDE (UNII: 1HG84L3525) SODIUM CHLORIDE (UNII: 451W47IQ8X) POLYSORBATE 80 (UNII: 6OZP39ZG8H) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:50090-1377-1 1 in 1 POUCH 1 .5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 2 NDC:50090-1377-0 10 in 1 CARTON 2 NDC:50090-1377-2 .5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125106 07/24/2009 Labeler - A-S Medication Solutions (830016429) Establishment Name Address ID/FEI Business Operations A-S Medication Solutions 830016429 RELABEL(50090-1377)