Label: FLUMAZENIL injection, solution
- NDC Code(s): 63323-424-05, 63323-424-10
- Packager: Fresenius Kabi USA, LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 22, 2020
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION:
Flumazenil Injection, USP is a benzodiazepine receptor antagonist. Chemically, flumazenil is ethyl 8-fluoro-5,6-dihydro-5-methyl-6-oxo-4H-imidazo [1,5-a](1,4)benzodiazepine-3-carboxylate. Flumazenil has an imidazobenzodiazepine structure and the following structural formula:
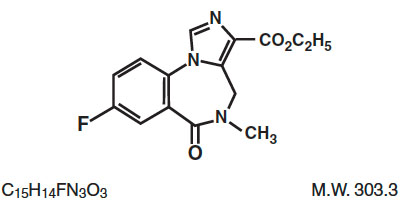
Flumazenil is a white to off-white crystalline compound with an octanol:buffer partition coefficient of 14 to 1 at pH 7.4. It is insoluble in water but slightly soluble in acidic aqueous solutions. Flumazenil Injection, USP is available as a sterile parenteral dosage form for intravenous administration. Each mL contains 0.1 mg of flumazenil compounded with 1.8 mg of methylparaben, 0.2 mg of propylparaben, 0.9% sodium chloride, 0.01% edetate disodium, and 0.01% acetic acid; the pH is adjusted to approximately 3.8 to 4.3 with hydrochloric acid and/or, if necessary, sodium hydroxide.
-
CLINICAL PHARMACOLOGY:
Flumazenil, an imidazobenzodiazepine derivative, antagonizes the actions of benzodiazepines on the central nervous system. Flumazenil competitively inhibits the activity at the benzodiazepine recognition site on the GABA/benzodiazepine receptor complex. Flumazenil is a weak partial agonist in some animal models of activity, but has little or no agonist activity in man.
Flumazenil does not antagonize the central nervous system effects of drugs affecting GABA-ergic neurons by means other than the benzodiazepine receptor (including ethanol, barbiturates, or general anesthetics) and does not reverse the effects of opioids.
In animals pretreated with high doses of benzodiazepines over several weeks, flumazenil elicited symptoms of benzodiazepine withdrawal, including seizures. A similar effect was seen in adult human subjects.
Pharmacodynamics
Intravenous flumazenil has been shown to antagonize sedation, impairment of recall, psychomotor impairment and ventilatory depression produced by benzodiazepines in healthy human volunteers.
The duration and degree of reversal of benzodiazepine effects are related to the dose and plasma concentrations of flumazenil as shown in the following data from a study in normal volunteers.
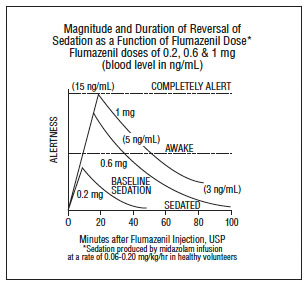
Generally, doses of approximately 0.1 mg to 0.2 mg (corresponding to peak plasma levels of 3 to 6 ng/mL) produce partial antagonism, whereas higher doses of 0.4 to 1 mg (peak plasma levels of 12 to 28 ng/mL) usually produce complete antagonism in patients who have received the usual sedating doses of benzodiazepines. The onset of reversal is usually evident within 1 to 2 minutes after the injection is completed. Eighty percent response will be reached within 3 minutes, with the peak effect occurring at 6 to 10 minutes. The duration and degree of reversal are related to the plasma concentration of the sedating benzodiazepine as well as the dose of flumazenil given.
In healthy volunteers, flumazenil did not alter intraocular pressure when given alone and reversed the decrease in intraocular pressure seen after administration of midazolam.
Pharmacokinetics
After IV administration, plasma concentrations of flumazenil follow a two-exponential decay model. The pharmacokinetics of flumazenil are dose-proportional up to 100 mg.
Distribution
Flumazenil is extensively distributed in the extravascular space with an initial distribution half-life of 4 to 11 minutes and a terminal half-life of 40 to 80 minutes. Peak concentrations of flumazenil are proportional to dose, with an apparent initial volume of distribution of 0.5 L/kg. The volume of distribution at steady-state is 0.9 to 1.1 L/kg. Flumazenil is a weak lipophilic base. Protein binding is approximately 50% and the drug shows no preferential partitioning into red blood cells. Albumin accounts for two thirds of plasma protein binding.
Metabolism
Flumazenil is completely (99%) metabolized. Very little unchanged flumazenil (<1%) is found in the urine. The major metabolites of flumazenil identified in urine are the de-ethylated free acid and its glucuronide conjugate. In preclinical studies there was no evidence of pharmacologic activity exhibited by the de-ethylated free acid.
Elimination
Elimination of radiolabeled drug is essentially complete within 72 hours, with 90% to 95% of the radioactivity appearing in urine and 5% to 10% in the feces. Clearance of flumazenil occurs primarily by hepatic metabolism and is dependent on hepatic blood flow. In pharmacokinetic studies of normal volunteers, total clearance ranged from 0.8 to 1 L/hr/kg.
Pharmacokinetic parameters following a 5-minute infusion of a total of 1 mg of flumazenil mean (coefficient of variation, range):
Cmax (ng/mL)
24 (38%, 11 to 43)
AUC (ng•hr/mL)
15 (22%, 10 to 22)
Vss (L/kg)
1 (24%, 0.8 to 1.6)
Cl (L/hr/kg)
1 (20%, 0.7 to 1.4)
Half-life (min)
54 (21%, 41 to 79)
Food Effects
Ingestion of food during an intravenous infusion of the drug results in a 50% increase in clearance, most likely due to the increased hepatic blood flow that accompanies a meal.
Special Populations
The Elderly
The pharmacokinetics of flumazenil are not significantly altered in the elderly.
Gender
The pharmacokinetics of flumazenil are not different in male and female subjects.
Renal Failure (creatinine clearance <10 mL/min) and Hemodialysis
The pharmacokinetics of flumazenil are not significantly affected.
Patients With Liver Dysfunction
For patients with moderate liver dysfunction, their mean total clearance is decreased to 40% to 60% and in patients with severe liver dysfunction, it is decreased to 25% of normal value, compared with age-matched healthy subjects. This results in a prolongation of the half-life to 1.3 hours in patients with moderate hepatic impairment and 2.4 hours in severely impaired patients. Caution should be exercised with initial and/or repeated dosing to patients with liver disease.
Drug-Drug Interaction
The pharmacokinetic profile of flumazenil is unaltered in the presence of benzodiazepine agonists and the kinetic profiles of those benzodiazepines studied (i.e., diazepam, flunitrazepam, lormetazepam, and midazolam) are unaltered by flumazenil. During the 4-hour steady-state and post infusion of ethanol, there were no pharmacokinetic interactions on ethanol mean plasma levels as compared to placebo when flumazenil doses were given intravenously (at 2.5 hours and 6 hours) nor were interactions of ethanol on the flumazenil elimination half-life found.
Pharmacokinetics in Pediatric Patients
The pharmacokinetics of flumazenil have been evaluated in 29 pediatric patients ranging in age from 1 to 17 years who had undergone minor surgical procedures. The average doses administered were 0.53 mg (0.044 mg/kg) in patients aged 1 to 5 years, 0.63 mg (0.020 mg/kg) in patients aged 6 to 12 years, and 0.8 mg (0.014 mg/kg) in patients aged 13 to 17 years. Compared to adults, the half-life was somewhat shorter and more variable in these patients, averaging 40 minutes and generally ranging from 20 to 75 minutes. Clearance and volume of distribution, normalized for body weight, were in the same range as those seen in adults, although more variability was seen in the pediatric patients.
-
CLINICAL TRIALS:
Flumazenil has been administered in adults to reverse the effects of benzodiazepines in conscious sedation, general anesthesia, and the management of suspected benzodiazepine overdose. Limited information from uncontrolled studies in pediatric patients is available regarding the use of flumazenil to reverse the effects of benzodiazepines in conscious sedation only.
Conscious Sedation in Adults
Flumazenil was studied in four trials in 970 patients who received an average of 30 mg diazepam or 10 mg midazolam for sedation (with or without a narcotic) in conjunction with both inpatient and outpatient diagnostic or surgical procedures. Flumazenil was effective in reversing the sedating and psychomotor effects of the benzodiazepine; however, amnesia was less completely and less consistently reversed. In these studies, flumazenil was administered as an initial dose of 0.4 mg IV (two doses of 0.2 mg) with additional 0.2 mg doses as needed to achieve complete awakening, up to a maximum total dose of 1 mg.
Seventy-eight percent of patients receiving flumazenil responded by becoming completely alert. Of those patients, approximately half responded to doses of 0.4 mg to 0.6 mg, while the other half responded to doses of 0.8 mg to 1 mg. Adverse effects were infrequent in patients who received 1 mg of flumazenil or less, although injection site pain, agitation and anxiety did occur. Reversal of sedation was not associated with any increase in the frequency of inadequate analgesia or increase in narcotic demand in these studies. While most patients remained alert throughout the 3-hour postprocedure observation period, resedation was observed to occur in 3% to 9% of the patients, and was most common in patients who had received high doses of benzodiazepines (see PRECAUTIONS).
General Anesthesia in Adults
Flumazenil was studied in four trials in 644 patients who received midazolam as an induction and/or maintenance agent in both balanced and inhalational anesthesia. Midazolam was generally administered in doses ranging from 5 mg to 80 mg, alone and/or in conjunction with muscle relaxants, nitrous oxide, regional or local anesthetics, narcotics and/or inhalational anesthetics. Flumazenil was given as an initial dose of 0.2 mg IV, with additional 0.2 mg doses as needed to reach a complete response, up to a maximum total dose of 1 mg. These doses were effective in reversing sedation and restoring psychomotor function, but did not completely restore memory as tested by picture recall. Flumazenil was not as effective in the reversal of sedation in patients who had received multiple anesthetic agents in addition to benzodiazepines.
Eighty-one percent of patients sedated with midazolam responded to flumazenil by becoming completely alert or just slightly drowsy. Of those patients, 36% responded to doses of 0.4 mg to 0.6 mg, while 64% responded to doses of 0.8 mg to 1 mg.
Resedation in patients who responded to flumazenil occurred in 10% to 15% of patients studied and was more common with larger doses of midazolam (>20 mg), long procedures (>60 minutes) and use of neuromuscular blocking agents (see PRECAUTIONS).
Management of Suspected Benzodiazepine Overdose in Adults
Flumazenil was studied in two trials in 497 patients who were presumed to have taken an overdose of a benzodiazepine, either alone or in combination with a variety of other agents. In these trials, 299 patients were proven to have taken a benzodiazepine as part of the overdose, and 80% of the 148 who received flumazenil responded by an improvement in level of consciousness. Of the patients who responded to flumazenil, 75% responded to a total dose of 1 mg to 3 mg.
Reversal of sedation was associated with an increased frequency of symptoms of CNS excitation. Of the patients treated with flumazenil, 1% to 3% were treated for agitation or anxiety. Serious side effects were uncommon, but six seizures were observed in 446 patients treated with flumazenil in these studies. Four of these 6 patients had ingested a large dose of cyclic antidepressants, which increased the risk of seizures (see WARNINGS).
Individualization of Dosage
General Principles
The serious adverse effects of flumazenil are related to the reversal of benzodiazepine effects. Using more than the minimally effective dose of flumazenil is tolerated by most patients but may complicate the management of patients who are physically dependent on benzodiazepines or patients who are depending on benzodiazepines for therapeutic effect (such as suppression of seizures in cyclic antidepressant overdose).
In high-risk patients, it is important to administer the smallest amount of flumazenil that is effective. The 1-minute wait between individual doses in the dose-titration recommended for general clinical populations may be too short for high-risk patients. This is because it takes 6 to 10 minutes for any single dose of flumazenil to reach full effects. Practitioners should slow the rate of administration of flumazenil administered to high-risk patients as recommended below.
Anesthesia and Conscious Sedation in Adult Patients
Flumazenil is well tolerated at the recommended doses in individuals who have no tolerance to (or dependence on) benzodiazepines. The recommended doses and titration rates in anesthesia and conscious sedation (0.2 mg to 1 mg given at 0.2 mg/min) are well tolerated in patients receiving the drug for reversal of a single benzodiazepine exposure in most clinical settings (see ADVERSE REACTIONS). The major risk will be resedation because the duration of effect of a long-acting (or large dose of a short-acting) benzodiazepine may exceed that of flumazenil. Resedation may be treated by giving a repeat dose at no less than 20-minute intervals. For repeat treatment, no more than 1 mg (at 0.2 mg/min doses) should be given at any one time and no more than 3 mg should be given in any one hour.
Overdose in Adult Patients
The risk of confusion, agitation, emotional lability and perceptual distortion with the doses recommended in patients with benzodiazepine overdose (3 mg to 5 mg administered as 0.5 mg/min) may be greater than that expected with lower doses and slower administration. The recommended doses represent a compromise between a desirable slow awakening and the need for prompt response and a persistent effect in the overdose situation. If circumstances permit, the physician may elect to use the 0.2 mg/minute titration rate to slowly awaken the patient over 5 to 10 minutes, which may help to reduce signs and symptoms on emergence.
Flumazenil has no effect in cases where benzodiazepines are not responsible for sedation. Once doses of 3 mg to 5 mg have been reached without clinical response, additional flumazenil is likely to have no effect.
Patients Tolerant to Benzodiazepines
Flumazenil may cause benzodiazepine withdrawal symptoms in individuals who have been taking benzodiazepines long enough to have some degree of tolerance. Patients who had been taking benzodiazepines prior to entry into the flumazenil trials, who were given flumazenil in doses over 1 mg, experienced withdrawal-like events 2 to 5 times more frequently than patients who received less than 1 mg.
In patients who may have tolerance to benzodiazepines, as indicated by clinical history or by the need for larger than usual doses of benzodiazepines, slower titration rates of 0.1 mg/min and lower total doses may help reduce the frequency of emergent confusion and agitation. In such cases, special care must be taken to monitor the patients for resedation because of the lower doses of flumazenil used.
Patients Physically Dependent on Benzodiazepines
Flumazenil is known to precipitate withdrawal seizures in patients who are physically dependent on benzodiazepines, even if such dependence was established in a relatively few days of high dose sedation in Intensive Care Unit (ICU) environments. The risk of either seizures or resedation in such cases is high and patients have experienced seizures before regaining consciousness. Flumazenil should be used in such settings with extreme caution, since the use of flumazenil in this situation has not been studied and no information as to dose and rate of titration is available. Flumazenil should be used in such patients only if the potential benefits of using the drug outweigh the risks of precipitated seizures. Physicians are directed to the scientific literature for the most current information in this area.
-
INDICATIONS AND USAGE:
Adult Patients
Flumazenil Injection, USP is indicated for the complete or partial reversal of the sedative effects of benzodiazepines in cases where general anesthesia has been induced and/or maintained with benzodiazepines, where sedation has been produced with benzodiazepines for diagnostic and therapeutic procedures, and for the management of benzodiazepine overdose.
Pediatric Patients (aged 1 to 17)
Flumazenil Injection, USP is indicated for the reversal of conscious sedation induced with benzodiazepines (see PRECAUTIONS, Pediatric Use).
-
CONTRAINDICATIONS:
Flumazenil Injection, USP is contraindicated:
• in patients with a known hypersensitivity to flumazenil or benzodiazepines.
• in patients who have been given a benzodiazepine for control of a potentially life-threatening condition (e.g., control of intracranial pressure or status epilepticus).
• in patients who are showing signs of serious cyclic antidepressant overdose (see WARNINGS).
-
WARNINGS:
THE USE OF FLUMAZENIL HAS BEEN ASSOCIATED WITH THE OCCURRENCE OF SEIZURES.
THESE ARE MOST FREQUENT IN PATIENTS WHO HAVE BEEN ON BENZODIAZEPINES FOR LONG-TERM SEDATION OR IN OVERDOSE CASES WHERE PATIENTS ARE SHOWING SIGNS OF SERIOUS CYCLIC ANTIDEPRESSANT OVERDOSE.
PRACTITIONERS SHOULD INDIVIDUALIZE THE DOSAGE OF FLUMAZENIL AND BE PREPARED TO MANAGE SEIZURES.
Risk of Seizures
The reversal of benzodiazepine effects may be associated with the onset of seizures in certain high-risk populations. Possible risk factors for seizures include: concurrent major sedative-hypnotic drug withdrawal, recent therapy with repeated doses of parenteral benzodiazepines, myoclonic jerking or seizure activity prior to flumazenil administration in overdose cases, or concurrent cyclic antidepressant poisoning.
Flumazenil is not recommended in cases of serious cyclic antidepressant poisoning, as manifested by motor abnormalities (twitching, rigidity, focal seizure), dysrhythmia (wide QRS, ventricular dysrhythmia, heart block), anticholinergic signs (mydriasis, dry mucosa, hypoperistalsis), and cardiovascular collapse at presentation. In such cases flumazenil should be withheld and the patient should be allowed to remain sedated (with ventilatory and circulatory support as needed) until the signs of antidepressant toxicity have subsided. Treatment with flumazenil has no known benefit to the seriously ill mixed-overdose patient other than reversing sedation and should not be used in cases where seizures (from any cause) are likely.
Most convulsions associated with flumazenil administration require treatment and have been successfully managed with benzodiazepines, phenytoin or barbiturates. Because of the presence of flumazenil, higher than usual doses of benzodiazepines may be required.
Hypoventilation
Patients who have received flumazenil for the reversal of benzodiazepine effects (after conscious sedation or general anesthesia) should be monitored for resedation, respiratory depression, or other residual benzodiazepine effects for an appropriate period (up to 120 minutes) based on the dose and duration of effect of the benzodiazepine employed.
This is because flumazenil has not been established in patients as an effective treatment for hypoventilation due to benzodiazepine administration. In healthy male volunteers, flumazenil is capable of reversing benzodiazepine-induced depression of the ventilatory responses to hypercapnia and hypoxia after a benzodiazepine alone. However, such depression may recur because the ventilatory effects of typical doses of flumazenil (1 mg or less) may wear off before the effects of many benzodiazepines. The effects of flumazenil on ventilatory response following sedation with a benzodiazepine in combination with an opioid are inconsistent and have not been adequately studied. The availability of flumazenil does not diminish the need for prompt detection of hypoventilation and the ability to effectively intervene by establishing an airway and assisting ventilation.
Overdose cases should always be monitored for resedation until the patients are stable and resedation is unlikely.
-
PRECAUTIONS:
Return of Sedation
Flumazenil may be expected to improve the alertness of patients recovering from a procedure involving sedation or anesthesia with benzodiazepines, but should not be substituted for an adequate period of postprocedure monitoring. The availability of flumazenil does not reduce the risks associated with the use of large doses of benzodiazepines for sedation.
Patients should be monitored for resedation, respiratory depression (see WARNINGS) or other persistent or recurrent agonist effects for an adequate period of time after administration of flumazenil.
Resedation is least likely in cases where flumazenil is administered to reverse a low dose of a short-acting benzodiazepine (<10 mg midazolam). It is most likely in cases where a large single or cumulative dose of a benzodiazepine has been given in the course of a long procedure along with neuromuscular blocking agents and multiple anesthetic agents.
Profound resedation was observed in 1% to 3% of adult patients in the clinical studies. In clinical situations where resedation must be prevented in adult patients, physicians may wish to repeat the initial dose (up to 1 mg of flumazenil given at 0.2 mg/min) at 30 minutes and possibly again at 60 minutes. This dosage schedule, although not studied in clinical trials, was effective in preventing resedation in a pharmacologic study in normal volunteers.
The use of flumazenil to reverse the effects of benzodiazepines used for conscious sedation has been evaluated in one open-label clinical trial involving 107 pediatric patients between the ages of 1 and 17 years. This study suggested that pediatric patients who have become fully awake following treatment with flumazenil may experience a recurrence of sedation, especially younger patients (ages 1 to 5). Resedation was experienced in 7 of 60 patients who were fully alert 10 minutes after the start of flumazenil administration. No patient experienced a return to the baseline level of sedation. Mean time to resedation was 25 minutes (range: 19 to 50 minutes) (see PRECAUTIONS, Pediatric Use). The safety and effectiveness of repeated flumazenil administration in pediatric patients experiencing resedation have not been established.
Use in the ICU
Flumazenil should be used with caution in the ICU because of the increased risk of unrecognized benzodiazepine dependence in such settings. Flumazenil may produce convulsions in patients physically dependent on benzodiazepines (see Individualization of Dosage and WARNINGS).
Administration of flumazenil to diagnose benzodiazepine-induced sedation in the ICU is not recommended due to the risk of adverse events as described above. In addition, the prognostic significance of a patient’s failure to respond to flumazenil in cases confounded by metabolic disorder, traumatic injury, drugs other than benzodiazepines, or any other reasons not associated with benzodiazepine receptor occupancy is unknown.
Use in Overdosage
Flumazenil is intended as an adjunct to, not as a substitute for, proper management of airway, assisted breathing, circulatory access and support, internal decontamination by lavage and charcoal, and adequate clinical evaluation.
Necessary measures should be instituted to secure airway, ventilation and intravenous access prior to administering flumazenil. Upon arousal, patients may attempt to withdraw endotracheal tubes and/or intravenous lines as the result of confusion and agitation following awakening.
Head Injury
Flumazenil should be used with caution in patients with head injury as it may be capable of precipitating convulsions or altering cerebral blood flow in patients receiving benzodiazepines. It should be used only by practitioners prepared to manage such complications should they occur.
Use With Neuromuscular Blocking Agents
Flumazenil should not be used until the effects of neuromuscular blockade have been fully reversed.
Use in Psychiatric Patients
Flumazenil has been reported to provoke panic attacks in patients with a history of panic disorder.
Pain on Injection
To minimize the likelihood of pain or inflammation at the injection site, flumazenil should be administered through a freely flowing intravenous infusion into a large vein. Local irritation may occur following extravasation into perivascular tissues.
Use in Respiratory Disease
The primary treatment of patients with serious lung disease who experience serious respiratory depression due to benzodiazepines should be appropriate ventilatory support (see PRECAUTIONS) rather than the administration of flumazenil. Flumazenil is capable of partially reversing benzodiazepine-induced alterations in ventilatory drive in healthy volunteers, but has not been shown to be clinically effective.
Use in Cardiovascular Disease
Flumazenil did not increase the work of the heart when used to reverse benzodiazepines in cardiac patients when given at a rate of 0.1 mg/min in total doses of less than 0.5 mg in studies reported in the clinical literature. Flumazenil alone had no significant effects on cardiovascular parameters when administered to patients with stable ischemic heart disease.
Use in Liver Disease
The clearance of flumazenil is reduced to 40% to 60% of normal in patients with mild to moderate hepatic disease and to 25% of normal in patients with severe hepatic dysfunction (see Pharmacokinetics). While the dose of flumazenil used for initial reversal of benzodiazepine effects is not affected, repeat doses of the drug in liver disease should be reduced in size or frequency.
Use in Drug and Alcohol Dependent Patients
Flumazenil should be used with caution in patients with alcoholism and other drug dependencies due to the increased frequency of benzodiazepine tolerance and dependence observed in these patient populations.
Flumazenil is not recommended either as a treatment for benzodiazepine dependence or for the management of protracted benzodiazepine abstinence syndromes, as such use has not been studied.
The administration of flumazenil can precipitate benzodiazepine withdrawal in animals and man. This has been seen in healthy volunteers treated with therapeutic doses of oral lorazepam for up to 2 weeks who exhibited effects such as hot flushes, agitation and tremor when treated with cumulative doses of up to 3 mg doses of flumazenil.
Similar adverse experiences suggestive of flumazenil precipitation of benzodiazepine withdrawal have occurred in some adult patients in clinical trials. Such patients had a short-lived syndrome characterized by dizziness, mild confusion, emotional lability, agitation (with signs and symptoms of anxiety), and mild sensory distortions. This response was dose-related, most common at doses above 1 mg, rarely required treatment other than reassurance and was usually short-lived. When required (5 to 10 cases), these patients were successfully treated with usual doses of a barbiturate, a benzodiazepine, or other sedative drug.
Practitioners should assume that flumazenil administration may trigger dose-dependent withdrawal syndromes in patients with established physical dependence on benzodiazepines and may complicate the management of withdrawal syndromes for alcohol, barbiturates and cross-tolerant sedatives.
Drug Interactions
Interaction with central nervous system depressants other than benzodiazepines has not been specifically studied; however, no deleterious interactions were seen when flumazenil was administered after narcotics, inhalational anesthetics, muscle relaxants and muscle relaxant antagonists administered in conjunction with sedation or anesthesia.
Particular caution is necessary when using flumazenil in cases of mixed drug overdosage since the toxic effects (such as convulsions and cardiac dysrhythmias) of other drugs taken in overdose (especially cyclic antidepressants) may emerge with the reversal of the benzodiazepine effect by flumazenil (see WARNINGS).
The use of flumazenil is not recommended in epileptic patients who have been receiving benzodiazepine treatment for a prolonged period. Although flumazenil exerts a slight intrinsic anticonvulsant effect, its abrupt suppression of the protective effect of a benzodiazepine agonist can give rise to convulsions in epileptic patients.
Flumazenil blocks the central effects of benzodiazepines by competitive interaction at the receptor level. The effects of non-benzodiazepine agonists at benzodiazepine receptors, such as zopiclone, triazolopyridazines and others, are also blocked by flumazenil.
The pharmacokinetics of benzodiazepines are unaltered in the presence of flumazenil and vice versa.
There is no pharmacokinetic interaction between ethanol and flumazenil.
Use in Ambulatory Patients
The effects of flumazenil may wear off before a long-acting benzodiazepine is completely cleared from the body. In general, if a patient shows no signs of sedation within 2 hours after a 1 mg dose of flumazenil, serious resedation at a later time is unlikely. An adequate period of observation must be provided for any patient in whom either long-acting benzodiazepines (such as diazepam) or large doses of short-acting benzodiazepines (such as >10 mg of midazolam) have been used (see Individualization of Dosage).
Because of the increased risk of adverse reactions in patients who have been taking benzodiazepines on a regular basis, it is particularly important that physicians query patients or their guardians carefully about benzodiazepine, alcohol and sedative use as part of the history prior to any procedure in which the use of flumazenil is planned (see PRECAUTIONS, Use in Drug and Alcohol Dependent Patients).
Information for Patients
Flumazenil does not consistently reverse amnesia. Patients cannot be expected to remember information told to them in the postprocedure period and instructions given to patients should be reinforced in writing or given to a responsible family member. Physicians are advised to discuss with patients or their guardians, both before surgery and at discharge, that although the patient may feel alert at the time of discharge, the effects of the benzodiazepine (e.g., sedation) may recur. As a result, the patient should be instructed, preferably in writing, that their memory and judgment may be impaired and specifically advised:
- Not to engage in any activities requiring complete alertness, and not to operate hazardous machinery or a motor vehicle during the first 24 hours after discharge, and it is certain no residual sedative effects of the benzodiazepine remain.
- Not to take any alcohol or non-prescription drugs during the first 24 hours after flumazenil administration or if the effects of the benzodiazepine persist.
Laboratory Tests
No specific laboratory tests are recommended to follow the patient’s response or to identify possible adverse reactions.
Drug/Laboratory Test Interactions
The possible interaction of flumazenil with commonly used laboratory tests has not been evaluated.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No studies in animals to evaluate the carcinogenic potential of flumazenil have been conducted.
Mutagenesis
No evidence for mutagenicity was noted in the Ames test using five different tester strains. Assays for mutagenic potential in S. cerevisiae D7 and in Chinese hamster cells were considered to be negative as were blastogenesis assays in vitro in peripheral human lymphocytes and in vivo in a mouse micronucleus assay. Flumazenil caused a slight increase in unscheduled DNA synthesis in rat hepatocyte culture at concentrations which were also cytotoxic; no increase in DNA repair was observed in male mouse germ cells in an in vivo DNA repair assay.
Impairment of Fertility
A reproduction study in male and female rats did not show any impairment of fertility at oral dosages of 125 mg/kg/day. From the available data on the area under the curve (AUC) in animals and man the dose represented 120x the human exposure from a maximum recommended intravenous dose of 5 mg.
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of the use of flumazenil in pregnant women. Flumazenil should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Teratogenic Effects
Flumazenil has been studied for teratogenicity in rats and rabbits following oral treatments of up to 150 mg/kg/day. The treatments during the major organogenesis were on days 6 to 15 of gestation in the rat and days 6 to 18 of gestation in the rabbit. No teratogenic effects were observed in rats or rabbits at 150 mg/kg; the dose, based on the available data on the area under the plasma concentration-time curve (AUC) represented 120x to 600x the human exposure from a maximum recommended intravenous dose of 5 mg in humans. In rabbits, embryocidal effects (as evidenced by increased preimplantation and postimplantation losses) were observed at 50 mg/kg or 200x the human exposure from a maximum recommended intravenous dose of 5 mg. The no-effect dose of 15 mg/kg in rabbits represents 60x the human exposure.
Nonteratogenic Effects
An animal reproduction study was conducted in rats at oral dosages of 5, 25 and 125 mg/kg/day of flumazenil. Pup survival was decreased during the lactating period, pup liver weight at weaning was increased for the high-dose group (125 mg/kg/day) and incisor eruption and ear opening in the offspring were delayed; the delay in ear opening was associated with a delay in the appearance of the auditory startle response. No treatment-related adverse effects were noted for the other dose groups. Based on the available data from AUC, the effect level (125 mg/kg) represents 120x the human exposure from 5 mg, the maximum recommended intravenous dose in humans. The no-effect level represents 24x the human exposure from an intravenous dose of 5mg.
Labor and Delivery
The use of flumazenil to reverse the effects of benzodiazepines used during labor and delivery is not recommended because the effects of the drug in the newborn are unknown.
Nursing Mothers
Caution should be exercised when deciding to administer flumazenil to a nursing woman because it is not known whether flumazenil is excreted in human milk.
Pediatric Use
The safety and effectiveness of flumazenil have been established in pediatric patients 1 year of age and older. Use of flumazenil in this age group is supported by evidence from adequate and well-controlled studies of flumazenil in adults with additional data from uncontrolled pediatric studies including one open-label trial.
The use of flumazenil to reverse the effects of benzodiazepines used for conscious sedation was evaluated in one uncontrolled clinical trial involving 107 pediatric patients between the ages of 1 and 17 years. At the doses used, flumazenil’s safety was established in this population. Patients received up to 5 injections of 0.01 mg/kg flumazenil up to a maximum total dose of 1 mg at a rate not exceeding 0.2 mg/min.
Of 60 patients who were fully alert at 10 minutes, 7 experienced resedation. Resedation occurred between 19 and 50 minutes after the start of flumazenil administration. None of the patients experienced a return to the baseline level of sedation. All 7 patients were between the ages of 1 and 5 years. The types and frequency of adverse events noted in these pediatric patients were similar to those previously documented in clinical trials with flumazenil to reverse conscious sedation in adults. No patient experienced a serious adverse event attributable to flumazenil.
The safety and efficacy of flumazenil in the reversal of conscious sedation in pediatric patients below the age of 1 year have not been established (see CLINICAL PHARMACOLOGY, Pharmacokinetics in Pediatric Patients).
The safety and efficacy of flumazenil have not been established in pediatric patients for reversal of the sedative effects of benzodiazepines used for induction of general anesthesia, for the management of overdose, or for the resuscitation of the newborn, as no well-controlled clinical studies have been performed to determine the risks, benefits and dosages to be used. However, published anecdotal reports discussing the use of flumazenil in pediatric patients for these indications have reported similar safety profiles and dosing guidelines to those described for the reversal of conscious sedation.
The risks identified in the adult population with flumazenil use also apply to pediatric patients. Therefore, consult the CONTRAINDICATIONS, WARNINGS, PRECAUTIONS, and ADVERSE REACTIONS sections when using flumazenil in pediatric patients.
Geriatric Use
Of the total number of subjects in clinical studies of flumazenil, 248 were 65 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
The pharmacokinetics of flumazenil have been studied in the elderly and are not significantly different from younger patients. Several studies of flumazenil in subjects over the age of 65 and one study in subjects over the age of 80 suggest that while the doses of benzodiazepine used to induce sedation should be reduced, ordinary doses of flumazenil may be used for reversal.
-
ADVERSE REACTIONS:
Serious Adverse Reactions
Deaths have occurred in patients who received flumazenil in a variety of clinical settings. The majority of deaths occurred in patients with serious underlying disease or in patients who had ingested large amounts of non-benzodiazepine drugs (usually cyclic antidepressants), as part of an overdose.
Serious adverse events have occurred in all clinical settings, and convulsions are the most common serious adverse events reported. Flumazenil administration has been associated with the onset of convulsions in patients with severe hepatic impairment and in patients who are relying on benzodiazepine effects to control seizures, are physically dependent on benzodiazepines, or who have ingested large doses of other drugs (mixed-drug overdose) (see WARNINGS).
Two of the 446 patients who received flumazenil in controlled clinical trials for the management of a benzodiazepine overdose had cardiac dysrhythmias (1 ventricular tachycardia, 1 junctional tachycardia).
Adverse Events in Clinical Studies
The following adverse reactions were considered to be related to flumazenil administration (both alone and for the reversal of benzodiazepine effects) and were reported in studies involving 1875 individuals who received flumazenil in controlled trials. Adverse events most frequently associated with flumazenil alone were limited to dizziness, injection site pain, increased sweating, headache, and abnormal or blurred vision (3% to 9%).
Body as a Whole: fatigue (asthenia, malaise), headache, injection site pain* and injection site reaction (thrombophlebitis, skin abnormality, rash)
Cardiovascular System: cutaneous vasodilation (sweating, flushing, hot flushes)
Digestive System: nausea and vomiting (11%)
Nervous System: agitation (anxiety, nervousness, dry mouth, tremor, palpitations, insomnia, dyspnea, hyperventilation)*, dizziness (vertigo, ataxia) (10%) and emotional lability (crying abnormal, depersonalization, euphoria, increased tears, depression, dysphoria, paranoia)
Special Senses: abnormal vision (visual field defect, diplopia) and paresthesia (sensation abnormal, hypoesthesia)
All adverse reactions occurred in 1% to 3% of cases unless otherwise marked.
*indicates reaction in 3% to 9% of cases.
Observed percentage reported if greater than 9%.
The following adverse events were observed infrequently (less than 1%) in the clinical studies, but were judged as probably related to flumazenil administration and/or reversal of benzodiazepine effects:
Nervous System: confusion (difficulty concentrating, delirium), convulsions (see WARNINGS) and somnolence (stupor)
Special Senses: abnormal hearing (transient hearing impairment, hyperacusis, tinnitus)
The following adverse events occurred with frequencies less than 1% in the clinical trials. Their relationship to flumazenil administration is unknown, but they are included as alerting information for the physician.
Body as a Whole: rigors, shivering
Cardiovascular System: arrhythmia (atrial, nodal, ventricular extrasystoles), bradycardia, tachycardia, hypertension and chest pain
Digestive System: hiccup
Nervous System: speech disorder (dysphonia, thick tongue)
Not included in this list is operative site pain that occurred with the same frequency in patients receiving placebo as in patients receiving flumazenil for reversal of sedation following a surgical procedure.
Additional Adverse Reactions Reported During Postmarketing Experience
The following events have been reported during postapproval use of flumazenil.
Nervous System: Fear, panic attacks in patients with a history of panic disorders.
Withdrawal symptoms may occur following rapid injection of flumazenil in patients with long-term exposure to benzodiazepines.
-
DRUG ABUSE AND DEPENDENCE:
Flumazenil acts as a benzodiazepine antagonist, blocks the effects of benzodiazepines in animals and man, antagonizes benzodiazepine reinforcement in animal models, produces dysphoria in normal subjects, and has had no reported abuse in foreign marketing.
Although flumazenil has a benzodiazepine-like structure it does not act as a benzodiazepine agonist in man and is not a controlled substance.
-
OVERDOSAGE:
Large intravenous doses (exceeding those recommended) of flumazenil, when administered to healthy normal volunteers in the absence of a benzodiazepine agonist, produced no serious adverse reactions, severe signs or symptoms, or clinically significant laboratory test abnormalities. In clinical studies, most adverse reactions to flumazenil were an extension of the pharmacologic effects of the drug in reversing benzodiazepine effects.
Reversal with an excessively high dose of flumazenil may produce anxiety, agitation, increased muscle tone, hyperesthesia and possibly convulsions. Convulsions have been treated with barbiturates, benzodiazepines and phenytoin, generally with prompt resolution of the seizures (see WARNINGS).
-
DOSAGE AND ADMINISTRATION:
Flumazenil Injection, USP is recommended for intravenous use only. It is compatible with 5% dextrose in water, lactated Ringer’s and normal saline solutions. If Flumazenil Injection, USP is drawn into a syringe or mixed with any of these solutions, it should be discarded after 24 hours. For optimum sterility, Flumazenil Injection, USP should remain in the vial until just before use. As with all parenteral drug products, Flumazenil Injection, USP should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
To minimize the likelihood of pain at the injection site, Flumazenil Injection, USP should be administered through a freely running intravenous infusion into a large vein.
Reversal of Conscious Sedation
Adult Patients
For the reversal of the sedative effects of benzodiazepines administered for conscious sedation, the recommended initial dose of Flumazenil Injection, USP is 0.2 mg (2 mL) administered intravenously over 15 seconds. If the desired level of consciousness is not obtained after waiting an additional 45 seconds, a further dose of 0.2 mg (2 mL) can be injected and repeated at 60-second intervals where necessary (up to a maximum of 4 additional times) to a maximum total dose of 1 mg (10 mL). The dosage should be individualized based on the patient’s response, with most patients responding to doses of 0.6 mg to 1 mg (see Individualization of Dosage).
In the event of resedation, repeated doses may be administered at 20-minute intervals as needed. For repeat treatment, no more than 1 mg (given as 0.2 mg/min) should be administered at any one time, and no more than 3 mg should be given in any one hour.
It is recommended that Flumazenil Injection, USP be administered as the series of small injections described (not as a single bolus injection) to allow the practitioner to control the reversal of sedation to the approximate endpoint desired and to minimize the possibility of adverse effects (see Individualization of Dosage).
Pediatric Patients
For the reversal of the sedative effects of benzodiazepines administered for conscious sedation in pediatric patients greater than 1 year of age, the recommended initial dose is 0.01 mg/kg (up to 0.2 mg) administered intravenously over 15 seconds. If the desired level of consciousness is not obtained after waiting an additional 45 seconds, further injections of 0.01 mg/kg (up to 0.2 mg) can be administered and repeated at 60-second intervals where necessary (up to a maximum of 4 additional times) to a maximum total dose of 0.05 mg/kg or 1 mg, whichever is lower. The dose should be individualized based on the patient’s response. The mean total dose administered in the pediatric clinical trial of flumazenil was 0.65 mg (range: 0.08 mg to 1 mg). Approximately one-half of patients required the maximum of five injections.
Resedation occurred in 7 of 60 patients who were fully alert 10 minutes after the start of Flumazenil Injection, USP administration (see PRECAUTIONS, Pediatric Use). The safety and efficacy of repeated flumazenil administration in pediatric patients experiencing resedation have not been established.
It is recommended that Flumazenil Injection, USP be administered as the series of small injections described (not as a single bolus injection) to allow the practitioner to control the reversal of sedation to the approximate endpoint desired and to minimize the possibility of adverse effects (see Individualization of Dosage).
The safety and efficacy of Flumazenil Injection, USP in the reversal of conscious sedation in pediatric patients below the age of 1 year have not been established.
Reversal of General Anesthesia in Adult Patients
For the reversal of the sedative effects of benzodiazepines administered for general anesthesia, the recommended initial dose of Flumazenil Injection, USP is 0.2 mg (2 mL) administered intravenously over 15 seconds. If the desired level of consciousness is not obtained after waiting an additional 45 seconds, a further dose of 0.2 mg (2 mL) can be injected and repeated at 60-second intervals where necessary (up to a maximum of 4 additional times) to a maximum total dose of 1 mg (10 mL). The dosage should be individualized based on the patient’s response, with most patients responding to doses of 0.6 mg to 1 mg (see Individualization of Dosage).
In the event of resedation, repeated doses may be administered at 20-minute intervals as needed. For repeat treatment, no more than 1 mg (given as 0.2 mg/min) should be administered at any one time, and no more than 3 mg should be given in any one hour.
It is recommended that Flumazenil Injection, USP be administered as the series of small injections described (not as a single bolus injection) to allow the practitioner to control the reversal of sedation to the approximate endpoint desired and to minimize the possibility of adverse effects (see Individualization of Dosage).
Management of Suspected Benzodiazepine Overdose in Adult Patients
For initial management of a known or suspected benzodiazepine overdose, the recommended initial dose of Flumazenil Injection, USP is 0.2 mg (2 mL) administered intravenously over 30 seconds. If the desired level of consciousness is not obtained after waiting 30 seconds, a further dose of 0.3 mg (3 mL) can be administered over another 30 seconds. Further doses of 0.5 mg (5 mL) can be administered over 30 seconds at 1-minute intervals up to a cumulative dose of 3 mg.
Do not rush the administration of Flumazenil Injection, USP. Patients should have a secure airway and intravenous access before administration of the drug and be awakened gradually (see PRECAUTIONS).
Most patients with a benzodiazepine overdose will respond to a cumulative dose of 1 mg to 3 mg of Flumazenil Injection, USP, and doses beyond 3 mg do not reliably produce additional effects. On rare occasions, patients with a partial response at 3 mg may require additional titration up to a total dose of 5 mg (administered slowly in the same manner).
If a patient has not responded 5 minutes after receiving a cumulative dose of 5 mg of Flumazenil Injection, USP, the major cause of sedation is likely not to be due to benzodiazepines, and additional Flumazenil Injection, USP is likely to have no effect.
In the event of resedation, repeated doses may be given at 20-minute intervals if needed. For repeat treatment, no more than 1 mg (given as 0.5 mg/min) should be given at any one time and no more than 3 mg should be given in any one hour.
-
HOW SUPPLIED:
Product
No.
NDC
No.
402405
63323-424-05
Flumazenil Injection, USP 0.5 mg per 5 mL (0.1 mg per mL), in a 5 mL multiple dose vial, packaged in trays of 10.
402410
63323-424-10
Flumazenil Injection, USP 1 mg per 10 mL (0.1 mg per mL), in a 10 mL multiple dose vial, packaged individually.
The container closure is not made with natural rubber latex.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
- SPL UNCLASSIFIED SECTION
-
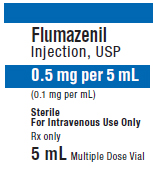
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY - Flumazenil 5 mL Multiple Dose Vial Label
Flumazenil
Injection, USP0.5 mg per 5 mL
(0.1 mg per mL)Sterile
For Intravenous Use Only
Rx only
5 mL
Multiple Dose Vial
PACKAGE LABEL - PRINCIPAL DISPLAY - Flumazenil 5 mL Multiple Dose Vial Tray Label
Flumazenil
Injection, USP0.5 mg per 5 mL
(0.1 mg per mL)Sterile
For Intravenous Use Only
Rx only
5 mL Multiple Dose Vial
-
INGREDIENTS AND APPEARANCE
FLUMAZENIL
flumazenil injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63323-424 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUMAZENIL (UNII: 40P7XK9392) (FLUMAZENIL - UNII:40P7XK9392) FLUMAZENIL 0.1 mg in 1 mL Inactive Ingredients Ingredient Name Strength METHYLPARABEN (UNII: A2I8C7HI9T) 1.8 mg in 1 mL PROPYLPARABEN (UNII: Z8IX2SC1OH) 0.2 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) EDETATE DISODIUM (UNII: 7FLD91C86K) ACETIC ACID (UNII: Q40Q9N063P) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63323-424-05 10 in 1 TRAY 04/05/2005 1 5 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 2 NDC:63323-424-10 1 in 1 CARTON 04/05/2005 2 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076955 04/05/2005 Labeler - Fresenius Kabi USA, LLC (608775388) Establishment Name Address ID/FEI Business Operations Fresenius Kabi USA, LLC 023648251 MANUFACTURE(63323-424)