Label: TETRACAINE- tetracaine hydrochloride injection
-
Contains inactivated NDC Code(s)
NDC Code(s): 42494-437-10 - Packager: Cameron Pharmaceuticals
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: unapproved drug other
DISCLAIMER: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here.
Drug Label Information
Updated July 28, 2021
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
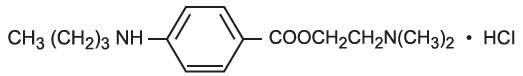
Tetracaine hydrochloride is 2-(Dimethylamino)ethyl p-(butylamino)benzoate monohydrochloride. It is a white crystalline, odorless powder that is readily soluble in water, physiologic saline solution, and dextrose solution. It has the following structural formula:
Tetracaine hydrochloride is a local anesthetic of the ester-linkage type, related to procaine.
1% Solution: A sterile, isotonic, isobaric solution.
Each mL contains:
Active: 10 mg Tetracaine Hydrochloride
Inactives: 7.5 mg Sodium Chloride, Hydrochloric Acid may be added to adjust pH (3.2 to 6.0) and Water for Injection, USP.
Nitrogen gas has been used to displace the air in the vials.
This formulation does not contain preservatives.
-
CLINICAL PHARMACOLOGY
Parenteral administration of tetracaine hydrochloride stabilizes the neuronal membrane and prevents initiation and transmission of nerve impulses thereby effecting local anesthesia. The onset of action is rapid, and the duration is prolonged (up to two or three hours or longer of surgical anesthesia).
Tetracaine hydrochloride is detoxified by plasma esterases to aminobenzoic acid and diethylaminoethanol.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Spinal anesthesia with tetracaine hydrochloride is contraindicated in patients with known hypersensitivity to tetracaine hydrochloride or to drugs of a similar chemical configuration (ester-type local anesthetics), or aminobenzoic acid or its derivatives; and in patients for whom spinal anesthesia as a technique is contraindicated.
The decision as to whether or not spinal anesthesia should be used for an individual patient should be made by the physician after weighing the advantages with the risks and possible complications. Contraindications to spinal anesthesia as a technique can be found in standard reference texts, and usually include generalized septicemia, infection at the site of injection, certain diseases of the cerebrospinal system, uncontrolled hypotension, etc.
-
WARNINGS
RESUSCITATIVE EQUIPMENT AND DRUGS SHOULD BE IMMEDIATELY AVAILABLE WHENEVER ANY LOCAL ANESTHETIC DRUG IS USED.
Large doses of local anesthetics should not be used in patients with heartblock.
Reactions resulting in fatality have occurred on rare occasions with the use of local anesthetics, even in the absence of a history of hypersensitivity.
Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs and symptoms of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death.
Discontinue tetracaine hydrochloride and any other oxidizing agents. Depending on the severity of the symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. More severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
-
PRECAUTIONS
The safety and effectiveness of any spinal anesthetic depend upon proper dosage, correct technique, adequate precautions, and readiness for emergencies. The lowest dosage that results in effective anesthesia should be used to avoid high plasma levels and serious systemic side effects. Tolerance varies with the status of the patient; debilitated, elderly patients or acutely ill patients should be given reduced doses commensurate with their weight, age, and physical status. Reduced doses are also indicated for obstetric patients and those with increased intra-abdominal pressure.
Caution should be used in administering tetracaine hydrochloride to patients with abnormal or reduced levels of plasma esterases.
Blood pressure should be frequently monitored during spinal anesthesia and hypotension immediately corrected.
Spinal anesthetics should be used with caution in patients with severe disturbances of cardiac rhythm, shock, and heartblock.
Drug Interactions
Tetracaine hydrochloride should not be used if the patient is being treated with a sulfonamide because aminobenzoic acid inhibits the action of sulfonamides. Patients that are administered local anesthetics may be at increased risk of developing methemoglobinemia when concurrently exposed to the following oxidizing agents:
Class Examples Nitrates/Nitrites nitroglycerin, nitroprusside, nitric oxide, nitrous oxide Local anesthetics benzocaine, lidocaine, bupivacaine, mepivacaine, tetracine, prilocaine, procaine, articaine, ropivacaine Antineoplastic agents cyclophosphamide, flutamide, rasburicase, ifosfamide, hydroxyurea Antibiotics dapsone, sulfonamides, nitrofurantoin, para-aminosalicylic acid Antimalarials chloroquine, primaquine Anticonvulsants phenytoin, sodium valproate, phenobarbital Other drugs Acetaminophen, metoclopramide, sulfa drugs (i.e., sulfasalazine), quinine Carcinogenesis, Mutagenesis, Impairment of Fertility
There have been no long-term animal studies to evaluate carcinogenic potential and reproduction studies in animals. There is no evidence from human data that tetracaine hydrochloride may be carcinogenic or that it impairs fertility.
Pregnancy Category C
There have been no animal reproduction studies conducted with tetracaine hydrochloride. It is not known whether tetracaine hydrochloride can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Tetracaine hydrochloride should be given to a pregnant woman only if clearly needed and the potential benefits outweigh the risk.
Labor and Delivery
Vasopressor agents administered for the treatment of hypotension resulting from spinal anesthesia may result in severe persistent hypertension and/or rupture of cerebral blood vessels if oxytocic drugs have also been administered; therefore, vasopressors should be used with extreme caution in the presence of oxytocic drugs.
Tetracaine hydrochloride has a recognized use during labor and delivery; the effect of the drug on duration of labor, incidence of forceps delivery, status of the newborn, and later growth and development of the child have not been studied.
Nursing Mothers
It is not known whether tetracaine hydrochloride is excreted in human milk; however, it is rapidly metabolized following absorption into the plasma. Because many drugs are excreted in human milk, caution should be exercised when tetracaine hydrochloride is administered to a nursing woman.
Pediatric Use: Safety and effectiveness of tetracaine hydrochloride in pediatric patients have not been established.
-
ADVERSE REACTIONS
Systemic adverse reactions to tetracaine hydrochloride are characteristic of those associated with other local anesthetics and can involve the central nervous system and the cardiovascular system. Systemic reactions usually result from high plasma levels due to excessive dosage, rapid adsorption, or inadvertent intravascular injection.
A small number of reactions to tetracaine hydrochloride may result from hypersensitivity, idiosyncrasy or diminished tolerance to normal dosage.
Central nervous system effects are characterized by excitation or depression. The first manifestation may be nervousness, dizziness, blurred vision, or tremors, followed by drowsiness, convulsions, unconsciousness and possibly respiratory and cardiac arrest. Since excitement may be transient or absent, the first manifestation may be drowsiness, sometimes merging into unconsciousness and respiratory and cardiac arrest. Other central nervous system effects may be nausea, vomiting, chills, constriction of the pupils, or tinnitus.
Cardiovascular system reactions include depression of the myocardium, blood pressure changes (usually hypotension), and cardiac arrest.
Allergic reactions, which may be due to hypersensitivity, idiosyncrasy, or diminished tolerance, are characterized by cutaneous lesions (eg. urticaria), edema, and other manifestations of allergy. Detection of sensitivity by skin testing is of limited value. Severe allergic reactions including anaphylaxis have rarely occurred and are not usually dose-related.
Reactions Associated with Spinal Anesthesia Techniques: Central Nervous System: post-spinal headache, meningismus, arachnoiditis, palsies, or spinal nerve paralysis. Cardiovascular: hypotension due to vasomotor paralysis and pooling of the blood in the venous bed. Respiratory: respiratory impairment or paralysis due to the level of anesthesia extending to the upper thoracic and cervical segments.
Gastrointestinal: nausea and vomiting.
Treatment of Reactions: Toxic effects of local anesthetics require symptomatic treatment; there is no specific cure. The most important measure is oxygenation of the patient by maintaining an airway and supporting ventilation. Supportive treatment of the cardiovascular system includes intravenous fluids and, when appropriate, vasopressors (preferably those that stimulate the myocardium). Convulsions are usually controlled with adequate oxygenation alone but intravenous administration in small increments of a barbiturate (preferably an ultrashort-acting barbiturate such as thiopental and thiamylal), or diazepam can be utilized. Intravenous barbiturates or anticonvulsant agents should only be administered by those familiar with their use and only if ventilation and oxygenation have first been assured. In spinal anesthesia, sympathetic blockade also occurs as a pharmacological action, resulting in peripheral vasodilation and often hypotension. The extent of the hypotension will usually depend on the number of dermatomes blocked. The blood pressure should therefore be monitored in the early phases of anesthesia. If hypotension occurs, it is readily controlled by vasoconstrictors administered either by the intramuscular or the intravenous route, the dosage of which would depend on the severity of the hypotension and the response to treatment.
-
Dosage and Administration
As with all anesthetics, the dosage varies and depends upon the area to be anesthetized, the number of neuronal segments to be blocked, individual tolerance, and the technique of anesthesia. The lowest dosage needed to provide effective anesthesia should be administered. For specific techniques and procedures, refer to standard textbooks.
Suggested Dosage for Spinal Anesthesia Using 1% Tetracaine HCl Injection, USP Extent of Anesthesia Dose of solution (mL) Volume of spinal fluid (mL) Site of injection (lumbar interspace) Perineum 0.5 (= 5 mg)* 0.5 4th Perineum and lower extremities 1.0 (= 10 mg) 1.0 3rd or 4th Up to costal margin (= 15 mg to 20 mg)† 1.5 to 2.0 1.5 to 2.0 2nd, 3rd, or 4th Inject solution at rate of about 1 mL per 5 seconds.
The extent and degree of spinal anesthesia depend upon dosage, specific gravity of the anesthetic solution, volume of solution used, force of the injection, level of puncture, position of the patient during and immediately after injection, etc.
Then spinal fluid is added to 1% tetracaine hydrochloride injection, some turbidity results, the degree depending on the pH of the spinal fluid, the temperature of the solution during mixing, as well as the amount of drug and diluent employed.
Liberation of base (which is completed within the spinal canal) is held to be essential for satisfactory results with any spinal anesthetic.
The specific gravity of spinal fluid at 25°C/25°C varies under normal conditions from 1.0063 to 1.0075. The 1% concentration in saline solution has a specific gravity of 1.0060 to 1.0074 at 25°C/25°C.
A hyperbaric solution may be prepared by mixing equal volumes of the 1% solution and Dextrose Solution 10%.
Examine vials carefully before use. Do not use solution if crystals, cloudiness, or discoloration is observed.
This formulation of tetracaine hydrochloride does not contain antimicrobial or bacteriostatic agents; therefore, unused portions should be discarded.
-
Sterilization of Vials
The tetracaine hydrochloride injection is sterile within an undamaged vial. To destroy bacteria on the exterior of vials use heat sterilization (autoclaving) before opening. Immersion in antiseptic solution is not recommended.
Autoclave at 15-pounds pressure, at 121°C (250°F), for 15 minutes.
Autoclaving increases likelihood of crystal formation. Unused autoclaved vials should be discarded. Under no circumstances should unused vials which have been autoclaved be returned to stock.
To report SUSPECTED ADVERSE REACTIONS, contact:
Cameron Pharmaceuticals, LLC at 1-888-296-9383
(or FDA 1-800-FDA-1088) or www.fda.gov/medwatch.
- HOW SUPPLIED
-
PATIENT COUNSELING INFORMATION
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); rapid heart rate; shortness of breath; lightheadedness; or fatigue.
- SPL UNCLASSIFIED SECTION
-
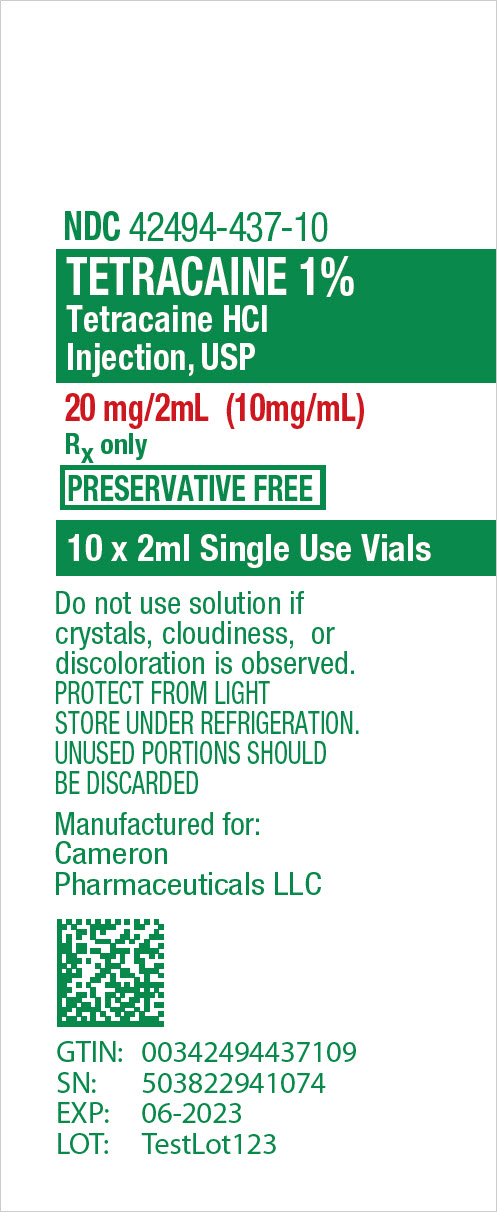
PRINCIPAL DISPLAY PANEL - 2 mL Vial Label
NDC 42494-437-10
TETRACAINE 1%
Tetracaine HCl
Injection, USP20 mg/2mL (10mg/mL)
Rx onlyPRESERVATIVE FREE
10 x 2ml Single Use Vials
Do not use solution if
crystals, cloudiness, or
discoloration is observed.
PROTECT FROM LIGHT
STORE UNDER REFRIGERATION.
UNUSED PORTIONS SHOULD
BE DISCARDEDManufactured for:
Cameron
Pharmaceuticals LLCGTIN: 00342494437109
SN: 503822941074
EXP: 06-2023
LOT: TestLot123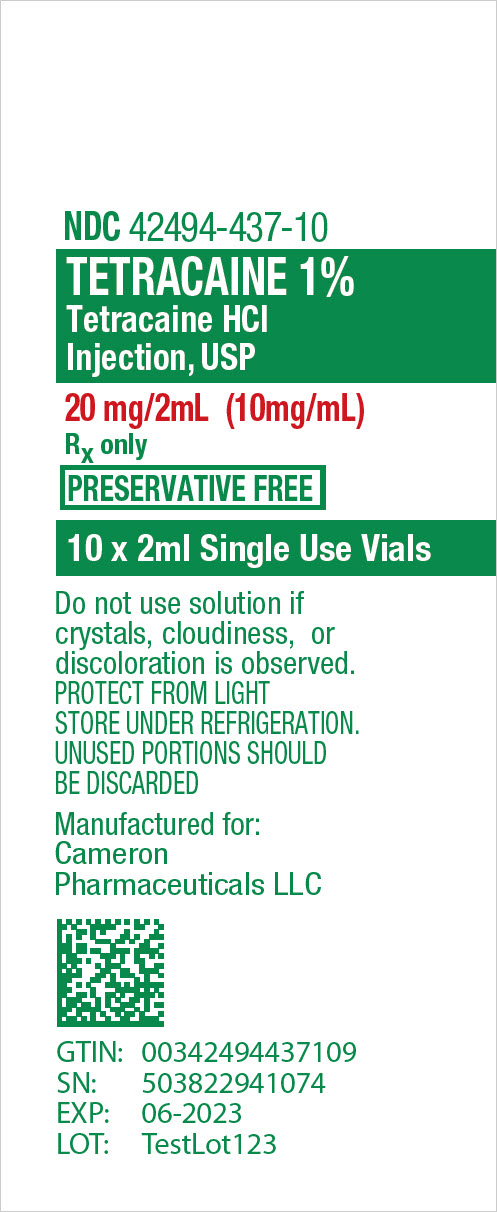
-
INGREDIENTS AND APPEARANCE
TETRACAINE
tetracaine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:42494-437 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TETRACAINE HYDROCHLORIDE (UNII: 5NF5D4OPCI) (Tetracaine - UNII:0619F35CGV) TETRACAINE HYDROCHLORIDE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength sodium chloride (UNII: 451W47IQ8X) hydrochloric acid (UNII: QTT17582CB) sodium hydroxide (UNII: 55X04QC32I) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:42494-437-10 2 mL in 1 VIAL; Type 0: Not a Combination Product 07/20/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved drug other 07/20/2021 Labeler - Cameron Pharmaceuticals (078371442) Establishment Name Address ID/FEI Business Operations Vitae Enim Vitae Scientific, Inc. 080492645 MANUFACTURE(42494-437)