Label: I 123 MIBG META IODOBENZYLGUANIDINE- i 123 mibg injection, powder, lyophilized, for solution
-
Contains inactivated NDC Code(s)
NDC Code(s): 51808-103-01 - Packager: AnazaoHealth Corporation
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: unapproved drug other
DISCLAIMER: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here.
Drug Label Information
Updated May 23, 2012
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
Description
I-123 MIBG is provided as a freeze-dried, radio-labeled sterile powder. The powder is reconstituted with 2 mL of sterile normal saline. The dose should be measured using a dose calibrator prior to administration. Caution: Radioactive Material. A commonly used name for iobenguane is meta-iodobenzylguanidine or MIBG.
-
Clinical Pharmacology
Iobenguane or meta-iodobenzylguanidine (MIBG) is a physiological analog of the guanidines, such as guanethidine and phenethylguanidine. In adrenergic nerves, guanidines are believed to share the same transport pathway as norepinephrine and to accumulate in, and displace norepinephrine from, intraneuronal storage granules. Similarly, I-123 MIBG is concentrated in, stored in, and released from chromaffin granules. The retention of I-123 MIBG in the adrenal medulla may be a result of their uptake in adrenergic neurons and subsequent sequestration into chromaffin storage granules. Due to their selective uptake mechanism, I-123 MIBG allows specific detection and localization of neuroendocrine tumors and adrenal medullary hyperplasia. The gamma emissions given off by I-123 MIBG allow detection of adrenergic tumors by scintigraphy. Medullary thyroid carcinoma: Although the mechanism of I-123 MIBG uptake by medullary thyroid carcinoma (MTC) is not completely understood, it has been found that MTC can produce catecholamines (epinephrine and norepinephrine). Therefore, I-123 MIBG could be taken up and stored in catecholamine vesicles of MTC.
-
Indications and Usage
Iobenguane is indicated as a radioactive isotope diagnosing for adrenomedullary disorders and neuroendocrine tumors.
Tumors, adrenal medulla (diagnosis): I-123 MIBG is used for diagnostic imaging of the adrenal medulla, for the evaluation and localization of intra- and extra-adrenal pheochromocytomas, paragangliomas, and neuroblastomas, as well as for localization of metastatic lesions from these tumors. I-123 MIBG can also be used for confirmation of diagnosis of pheochromocytoma when catecholamine determination tests are unclear.
Tumors, carcinoid (diagnosis): I-123 MIBG scintigraphy is used as screening procedures for suspected carcinoid tumors, especially those of intestinal origin.
Hyperplasia, adrenal medulla (diagnosis): I-123 MIBG is used in the evaluation of the adrenal medulla for disorders such as medullary hyperplasia in patients at risk of developing medullary disease (e.g., multiple endocrine neoplasia [MEN type 2, MEN type 3]).
Carcinoma, thyroid (diagnosis): I-123 MIBG is used for diagnostic imaging of medullary thyroid carcinoma.
DISTRIBUTION
After intravenous administration, there is rapid uptake of MIBG mainly in the liver, and in lesser amounts in the lungs, heart, and salivary glands. A limited number of patients may show activity in normal adrenals, lung, skeletal, muscle, and blocked thyroid glands. Although the uptake in normal adrenal glands is very low, hyperplastic adrenals and tumors such as pheochromocytoma, neuroblastoma, and other tumors with neurosecretory granules have a relatively higher uptake. Significant clearance of I-123 MIBG from the liver and the spleen occurs within 72 hours. I-123 MIBG—In adrenal medullary tumors: Initial images may be obtained 2 to 3 hours after injection. Images may also be obtained at 18 to 24 hours, and as late as 48 hours post injection. Most pheochromocytomas are visualized at 24 hours. However, due to the short half-life of I-123 MIBG, images may not be possible at times when background (e.g., liver) activity is low and imaging would be optimal. Small amounts of radioactivity used in diagnosis; radiation received is low and considered safe.
ELIMINATION
Renal; about 40 to 50% of the injected activity is eliminated within 24 hours and about 70 to 90% within 4 days (mainly as unchanged drug with small amounts of I-123 m-iodohippuric acid [I-123 MIHA], I-123 iodide, and I-123 m-iodobenzoic acid [I-123 MIBA]).
-
PRECAUTIONS TO CONSIDER
Pregnancy:
The possibility of pregnancy should be assessed in women of child-bearing potential. Clinical situations exist where the benefit to the patient and fetus, based on information derived from radiopharmaceutical use, outweighs the risks from fetal exposure to radiation. In these situations, the physician should use discretion and reduce the administered activity to the lowest possible amount.
Breast-feeding:
It is not known whether I-123 MIBG is distributed into breast milk. However, this preparation may be contaminated with free radioiodide, which may be distributed into breast milk. It has been recommended that, after administration of a radiopharmaceutical, nursing be resumed only after the infant's ingested effective dose equivalent (EDE) is below 1 mSv (100 mrem). A method to calculate the EDE has been proposed based on the effective half-life of the radionuclide, the activity administered to the mother, the fraction of administered activity ingested by the infant, and the total body effective dose to the newborn infant per unit of activity ingested. According to this method, it has been estimated that, for sodium iodide I-123, the time period required is 3 days with administration of an uncontaminated preparation, 40 days with a preparation contaminated with I-124, and 340 days for a preparation contaminated with I-125. Because of the difficulty of maintaining the maternal milk supply for such an extended period of time, complete cessation of nursing is usually recommended for all radioiodines, except for uncontaminated I-123.
Pediatrics:
When I-123MIBG is used in children, the diagnostic benefit should be judged to outweigh the potential risk of radiation.
DRUG INTERACTIONS AND/OR RELATED PROBLEMS
The following drug interactions and/or related problems have been selected on the basis of their potential clinical significance (possible mechanism in parentheses where appropriate)—not necessarily inclusive ( » = major clinical significance):
» Amphetamines or
» Antidepressants, tricyclic or
» Bretylium or
» Calcium channel blocking agents or
» Cocaine or
» Guanethidine or
» Haloperidol or
» Labetalol or
» Loxapine or
» Metaraminol or
» Phenothiazines or
» Reserpine or
» Sympathomimetics or
» Thiothixene (these medications may interfere with the uptake of I-123 or I-131 MIBG; although the ideal time to stop treatment with potential interacting medicines is 1 week prior to administration of I-123 or I-131 MIBG, the following withdrawal periods are usually recommended based on the individual half-life of each medication: 24 hours for bretylium, cocaine, and metaraminol; 48 hours for amphetamines, calcium channel blocking agents, guanethidine, haloperidol, loxapine, tricyclic antidepressants, phenothiazines, sympathomimetics, and thiothixene; 72 hours for labetalol and reserpine) Phenoxybenzamine (although usual doses of phenoxybenzamine do not interfere with I-123 or I-131MIBG uptake, when given in high doses necessary to control blood pressure in patients with pheochromocytomas or paragangliomas preparing for surgery, tumor uptake of I-123 or I-131 MIBG may be suppressed resulting in false-negative studies)
-
SIDE/ADVERSE EFFECTS
At present, there are no known side/adverse effects associated with the use of diagnostic dosages of I-123 MIBG.
PREPARATION FOR THIS TEST
Special preparatory instructions may apply; patient should inquire in advance.
Administration of potassium iodide or Lugol’s solution one day before administration of I-123MIBG and for 6 days after administration to prevent or reduce thyroid uptake of radioiodide contaminant.
GENERAL DOSAGE INFORMATION
Radiopharmaceuticals are to be administered only by or under the supervision of physicians who have had extensive training in the safe use and handling of radioactive materials and who are authorized by the Nuclear Regulatory Commission (NRC) or the appropriate State agency, if required, or, outside the U.S., the appropriate authority. To minimize uptake of radioactive iodine by the thyroid, potassium iodide (SSKI, 60 mg twice a day) or Lugol's solution (1 drop three times a day) may be used, beginning at least 24 hours before and continuing for 6 days after administration of I-123 MIBG.
Safety considerations for handling this radiopharmaceutical:
Improper handling of this radiopharmaceutical may cause radioactive contamination. Guidelines for handling radioactive material have been prepared by scientific, professional, state, federal, and international bodies and are available to the specially qualified and authorized users who have access to radiopharmaceuticals.
IOBENGUANE I-123 INJECTION
Usual adult administered activity for diagnosis of tumors or medullary disease:
Intravenous, 370 megabecquerels (10 millicuries) of I-123 mIBG, with a minimum specific activity of 740 megabecquerels to 1.3 gigabecquerels (20 to 35.6 millicuries) per mg (at time of calibration), administered over a period of fifteen to thirty seconds.
Usual pediatric administered activity for diagnosis of tumors or medullary disease:
In children up to 18 years of age, dosage must be individualized by physician.
Usual geriatric administered activity:
See usual adult administered activity.
Thank you,
AnazaoHealth Corporation
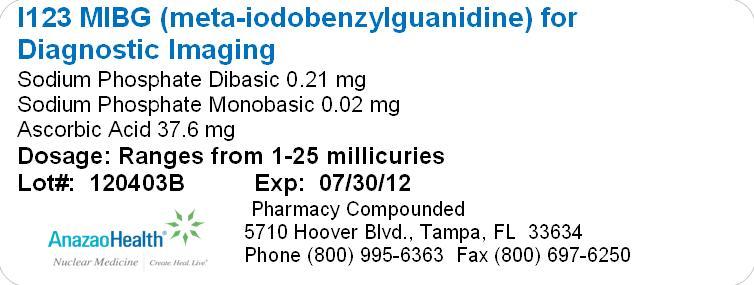
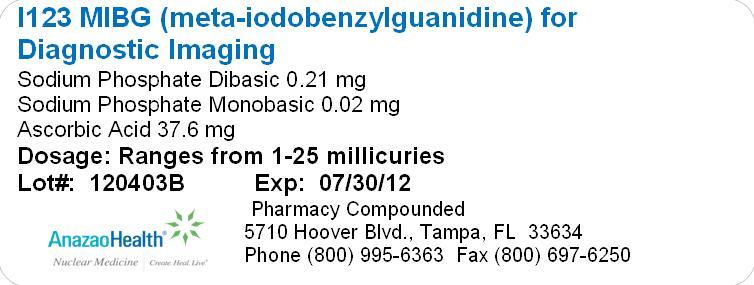
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
I 123 MIBG META IODOBENZYLGUANIDINE
i 123 mibg injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:51808-103 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IOBENGUANE SULFATE I-123 (UNII: 23X1185WBO) (IOBENGUANE I-123 - UNII:P2TH1XYZ84) IOBENGUANE SULFATE I-123 25 mCi Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) 0.21 mg SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) 0.02 mg ASCORBIC ACID (UNII: PQ6CK8PD0R) 37.6 mg Product Characteristics Color WHITE (White Powder) Score no score Shape Size Flavor Imprint Code Contains preservative free Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:51808-103-01 1 in 1 CONTAINER Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved drug other 05/23/2012 Labeler - AnazaoHealth Corporation (011038762) Establishment Name Address ID/FEI Business Operations AnazaoHealth Corporation 011038762 MANUFACTURE