Label: DOXYCYCLINE capsule
-
NDC Code(s):
63187-712-14,
63187-712-20,
63187-712-30,
63187-712-60, view more63187-712-90
- Packager: Proficient Rx LP
- This is a repackaged label.
- Source NDC Code(s): 68382-707
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated November 1, 2019
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
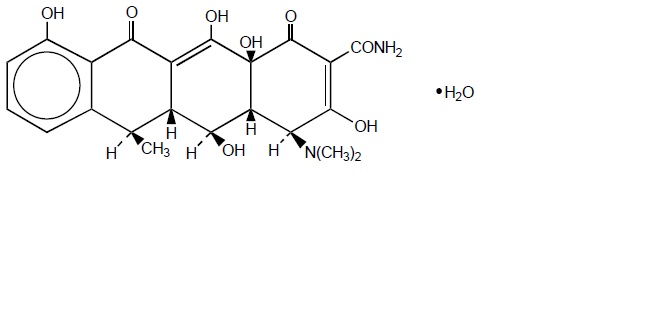
DESCRIPTION
Doxycycline is a broad-spectrum antibacterial synthetically derived from oxytetracycline. Doxycycline capsules 100 mg, 75 mg, and 50 mg capsules contain doxycycline monohydrate, USP equivalent to 100 mg, 75 mg, or 50 mg of doxycycline for oral administration. The chemical designation of the light-yellow to pale yellow powder is alpha-6-deoxy-5-oxytetracycline.
Structural formula:
C22H24N2O8 • H2O M.W. = 462.45
Doxycycline has a high degree of lipid solubility and a low affinity for calcium binding. It is highly stable in normal human serum. Doxycycline will not degrade into an epianhydro form.
Each doxycycline capsule, USP intended for oral administration contains 50 mg or 75 mg or 100 mg of doxycycline. In addition, each capsule contains the following inactive ingredients: colloidal silicon dioxide, gelatin, magnesium stearate, microcrystalline cellulose, sodium lauryl sulfate, sodium starch glycolate and titanium dioxide. Additionally, each 50 and 100 mg capsule shell contains iron oxide yellow, each 75 mg and 100 mg capsule shell contains: D & C yellow # 10, FD & C blue # 1, FD & C red # 3 and FD & C yellow # 6 and each 100 mg capsule shell contains iron oxide red. The capsule is printed with black pharmaceutical ink which contains following ingredients: black iron oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
USP Dissolution Test pending.
-
CLINICAL PHARMACOLOGY
Tetracyclines are readily absorbed and are bound to plasma proteins in varying degrees. They are concentrated by the liver in the bile and excreted in the urine and feces at high concentrations in a biologically active form. Doxycycline is virtually completely absorbed after oral administration.
Following a 200 mg dose of doxycycline monohydrate, 24 normal adult volunteers averaged the following serum concentration values:
Time (hr):
0.5
1
1.5
2
3
4
8
12
24
48
72
Conc.
1.02
2.26
2.67
3.01
3.16
3.03
2.03
1.62
0.95
0.37
0.15 (mcg/ mL)
Average Observed Values
Maximum Concentration
3.61 mcg/mL (± 0.9 sd)
Time of Maximum Concentration
2.60 hr (± 1.10 sd)
Elimination Rate Constant
0.049 per hr (± 0.030 sd)
Halflife
16.33 hr (± 4.53 sd)
Excretion of doxycycline by the kidney is about 40%/72 hours in individuals with normal function (creatinine clearance about 75 mL/min). This percentage excretion may fall as low as 1 to 5%/72 hours in individuals with severe renal insufficiency (creatinine clearance below 10 mL/min). Studies have shown no significant difference in serum half-life of doxycycline (range 18 to 22 hours) in individuals with normal and severely impaired renal functioHemodialysis does not alter serum half- life.
Microbiology
Mechanism of Action
Doxycycline inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit. Doxycycline has bacteriostatic activity against a broad range of Gram-positive and Gram-negative bacteria. Cross resistance with other tetracyclines is common. Doxycycline has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section of the package insert for doxycycline capsules.
Gram-Negative Bacteria
Acinetobacter species
Bartonella bacilliformis
Brucella species
Calymmatobacterium granulomatis
Campylobacter fetus
Enterobacter aerogenes
Escherichia coli
Francisella tularensis
Haemophilus ducreyi
Haemophilus influenzae
Klebsiella species
Neisseria gonorrhoeae
Shigella species
Vibrio cholerae
Yersinia pestis
Gram-Positive Bacteria
Bacillus anthracis
Streptococcus pneumoniae
Anaerobic Bacteria
Clostridium species
Fusobacterium fusiforme
Propionibacterium acnes
Other Bacteria
Nocardiae and other Actinomyces species
Borrelia recurrentis
Chlamydophila psittaci
Chlamydia trachomatis
Mycoplasma pneumoniae
Rickettsiae
Treponema pallidum
Treponema pertenue
Ureaplasma urealyticum
Parasites
Balantidium coli
Entamoeba species
Susceptibility Testing Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drugs used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized test method (broth and/or agar).1,2,4 The MIC values should be interpreted according to criteria provided in Table 1.
Diffusion techniques
Quantitative methods that require measurement of zone diameters can also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size provides an estimate of the susceptibility of bacteria to antimicrobial compounds.
The zone size should be determined using a standardized test method.1,3,4 This procedure uses paper disks impregnated with 30 mcg doxycycline to test the susceptibility of microorganisms to doxycycline. The disk diffusion interpretive criteria are provided in Table 1.
Anaerobic Techniques
For anaerobic bacteria, the susceptibility to doxycycline can be determined by a standardized test method.5The MIC values obtained should be interpreted according to the criteria provided in Table 1
Table 1Susceptibility Test Interpretive Criteria for Doxycycline and Tetracycline *Organisms susceptible to tetracycline are also considered susceptible to doxycycline. However, some organisms that are intermediate or resistant to tetracycline may be susceptible to doxycycline.
†The current absence of resistance isolates precludes defining any results other than "Susceptible". If isolates yielding MIC results other than susceptible, they should be submitted to a reference laboratory for further testing.
‡Gonococci with 30 mcg tetracycline disk zone diameters of less than 19 mm usually indicate a plasmid-mediated tetracycline resistant Neisseria gonorrhoeae isolate. Resistance in these strains should be confirmed by a dilution test (MIC ≥ 16 mcg per mL).
Bacteria*
Minimal Inhibitory Concentration
(mcg per mL)
Zone Diameter
(mm)
Agar Dilution
(mcg per mL)
S
I
R
S
I
R
S
I
R
Acinetobacter spp.
Doxycycline
Tetracycline
≤ 4
≤ 4
8
8
≥16
≥16
≥13
≥15
10 to 12
12 to 14
≤9
≤11
-
-
-
-
-
-
Anaerobes
Tetracycline
-
-
-
-
-
-
≤4
8
≥16
Bacillus anthracis†
Doxycycline
Tetracycline
≤1
≤1
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Brucella species†
Doxycycline
Tetracycline
≤1
≤1
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Enterobacteriaceae
Doxycycline
Tetracycline
≤4
≤4
8
8
≥16
≥16
≥14
≥15
11 to 13
12 to 14
≤10
≤11
-
-
-
-
-
-
Franciscella tularensis†
Doxycycline
Tetracycline
≤4
≤4
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Haemophilus influenzae
Tetracycline
≤2
4
≥8
≥29
26 to 28
≤25
-
-
-
Mycoplasma pneumoniae†
Tetracycline
-
-
-
-
-
-
≤2
-
-
Neisseria gonorrhoeae‡
Tetracycline
-
-
-
≥38
31 to 37
≤30
≤0.25
0.5 to 1
≥2
Norcardiae and other aerobic Actinomyces species†
Doxycycline
≤1
2 to 4
≥8
-
-
-
-
-
-
Streptococcus pneumoniae
Tetracycline
≤2
4
≥8
≥23
19 to 22
≤18
-
-
-
Vibrio cholerae
Doxycycline
Tetracycline
≤4
≤4
8
8
≥16
≥16
-
-
-
-
-
-
-
-
-
-
-
-
Yersinia pestis Doxycycline
Tetracycline
≤4
≤4
8
8
≥16
≥16
-
-
-
-
-
-
-
-
-
-
-
-
Ureaplasma urealyticum
Tetracycline
-
-
-
-
-
-
≤1
-
≥2
A report of Susceptible (S) indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations at the infection site necessary to inhibit growth of the pathogen. A report of Intermediate (I) indicates that the result should be considered equivocal, and, if the bacteria is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug product is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant (R) indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of the supplies and reagents used in the assay, and the techniques of the individuals performing the test.1,2,3,4,5,6,7Standard doxycycline and tetracycline powders should provide the following range of MIC values noted in Table 2. For the diffusion technique using the 30 mcg doxycycline disk the criteria noted in Table 2 should be achieved.
Table 2Acceptable Quality Control Ranges for Susceptibility Testing for Doxycycline and Tetracycline
QC Strain
Minimal Inhibitory
Concentration
(mcg per mL)
Zone Diameter
(mm)
Agar Dilution
(mcg per mL)
Enterococcus faecalis ATCC 29212
Doxycycline
Tetracycline
2 to 8
8 to 32
-
-
-
-
Escherichia coli ATCC 25922
Doxycycline
Tetracycline
0.5 to 2
0.5 to 2
18 to 24
18 to 25
-
-
Haemophilus influenzae ATCC 49247
Tetracycline
4 to 32
14 to 22
-
Neisseria gonorrhoeae ATCC 49226
Tetracycline
-
30 to 42
0.25 to 1
Staphylococcus aureus ATCC 25923
Doxycycline
Tetracycline
-
-
23 to 29
24 to 30
-
-
Staphylococcus aureus ATCC 29213
Doxycycline
Tetracycline
0.12 to 0.5
0.12 to 1
-
-
-
-
Streptococcus pneumoniae ATCC 49619
Doxycycline
Tetracycline
0.015 to 0.12
0.06 to 0.5
25 to 34
27 to 31
-
-
Bacteroides fragilis ATCC 25285
Tetracycline
-
-
0.125 to 0.5
Bacteroides thetaiotaomicron ATCC 29741
Tetracycline
-
-
8 to 32
Mycoplasma pneumoniae ATCC 29342
Tetracycline
0.06 to 0.5
-
0.06 to 0.5
Ureaplasma urealyticum ATCC 33175
Tetracycline
-
-
≥8
-
INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain effectiveness of doxycycline capsules, USP and other antibacterial drugs, doxycycline capsules, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Doxycycline capsules, USP are indicated for the treatment of the following infections:
Rocky mountain spotted fever, typhus fever and the typhus group, Q fever, rickettsialpox, and tick fevers caused by Rickettsiae.
Respiratory tract infections caused by Mycoplasma pneumoniae.
Lymphogranuloma venereum caused by Chlamydia trachomatis.
Psittacosis (ornithosis) caused by Chlamydophila psittaci.
Trachoma caused by Chlamydia trachomatis, although the infectious agent is not always eliminated as judged by immunofluorescence.
Inclusion conjunctivitis caused by Chlamydia trachomatis.
Uncomplicated urethral, endocervical or rectal infections in adults caused by Chlamydia trachomatis.
Nongonococcal urethritis caused by Ureaplasma urealyticum.
Relapsing fever due to Borrelia recurrentis.
Doxycycline capsules, USP are also indicated for the treatment of infections caused by the following gram-negative microorganisms:
Chancroid caused by Haemophilus ducreyi.
Plague due to Yersinia pestis.
Tularemia due to Francisella tularensis.
Cholera caused by Vibrio cholerae.
Campylobacter fetus infections caused by Campylobacter fetus.
Brucellosis due to Brucella species (in conjunction with streptomycin).
Bartonellosis due to Bartonella bacilliformis.
Granuloma inguinale caused by Calymmatobacterium granulomatis.
Because many strains of the following groups of microorganisms have been shown to be resistant to doxycycline, culture and susceptibility testing are recommended.
Doxycycline capsules, USP are indicated for treatment of infections caused by the following gram-negative microorganisms, when bacteriologic testing indicates appropriate susceptibility to the drug:
Escherichia coli
Enterobacter aerogenes
Shigella species
Acinetobacter species
Respiratory tract infections caused by Haemophilus influenzae.
Respiratory tract and urinary tract infections caused by Klebsiella species.
Doxycycline capsules, USP are indicated for treatment of infections caused by the following gram-positive microorganisms when bacteriologic testing indicates appropriate susceptibility to the drug:
Upper respiratory infections caused by Streptococcus pneumoniae.
Anthrax due to Bacillus anthracis, including inhalational anthrax (post-exposure): to reduce the incidence or progression of disease following exposure to aerosolized Bacillus anthracis.
When penicillin is contraindicated, doxycycline is an alternative drug in the treatment of the following infections:
Uncomplicated gonorrhea caused by Neisseria gonorrhoeae.
Syphilis caused by Treponema pallidum.
Yaws caused by Treponema pertenue.
Listeriosis due to Listeria monocytogenes.
Vincent's infection caused by Fusobacterium fusiforme.
Actinomycosis caused by Actinomyces israelii.
Infections caused by Clostridium species.
In acute intestinal amebiasis, doxycycline may be a useful adjunct to amebicides.
In severe acne, doxycycline may be useful adjunctive therapy.
- CONTRAINDICATIONS
-
WARNINGS
THE USE OF DRUGS OF THE TETRACYCLINE CLASS DURING TOOTH DEVELOPMENT (LAST HALF OF PREGNANCY, INFANCY, AND CHILDHOOD TO THE AGE OF 8 YEARS) MAY CAUSE PERMANENT DISCOLORATION OF THE TEETH (YELLOW-GRAY-BROWN). This adverse reaction is more common during long- term use of the drugs but has been observed following repeated short-term courses. Enamel hypoplasia has also been reported. TETRACYCLINE DRUGS, THEREFORE, SHOULD NOT BE USED IN THIS AGE GROUP, EXCEPT FOR ANTHRAX, INCLUDING INHALATIONAL ANTHRAX (POST-EXPOSURE), UNLESS OTHER DRUGS ARE NOT LIKELY TO BE EFFECTIVE OR ARE CONTRAINDICATED.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including doxycycline capsules, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
All tetracyclines form a stable calcium complex in any bone-forming tissue. A decrease in the fibula growth rate has been observed in prematures given oral tetracycline in doses of 25 mg/kg every six hours. This reaction was shown to be reversible when the drug was discontinued.
Results of animal studies indicate that tetracyclines cross the placenta, are found in fetal tissues, and can have toxic effects on the developing fetus (often related to retardation of skeletal development). Evidence of embryo toxicity has been noted in animals treated early in pregnancy. If any tetracycline is used during pregnancy or if the patient becomes pregnant while taking these drugs, the patient should be apprised of the potential hazard to the fetus.
The antianabolic action of the tetracyclines may cause an increase in BUN. Studies to date indicate that this does not occur with the use of doxycycline in patients with impaired renal function.
Photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines. Patients apt to be exposed to direct sunlight or ultraviolet light should be advised that this reaction can occur with tetracycline drugs, and treatment should be discontinued at the first evidence of skin erythema.
-
PRECAUTIONS
General
As with other antibacterial preparations, use of this drug may result in overgrowth of non-susceptible organisms, including fungi. If superinfection occurs, doxycycline capsules should be discontinued and appropriate therapy instituted.
Intracranial hypertension (IH, pseudotumor cerebri) has been associated with the use of tetracyclines including doxycycline capsules. Clinical manifestations of IH include headache, blurred vision, diplopia, and vision loss; papilledema can be found on fundoscopy. Women of childbearing age who are overweight or have a history of IH are at greater risk for developing tetracycline associated IH. Concomitant use of isotretinoin and doxycycline capsules should be avoided because isotretinoin is also known to cause pseudotumor cerebri.
Although IH typically resolves after discontinuation of treatment, the possibility for permanent visual loss exists. If visual disturbance occurs during treatment, prompt ophthalmologic evaluation is warranted. Since intracranial pressure can remain elevated for weeks after drug cessation patients should be monitored until they stabilize.
Incision and drainage or other surgical procedures should be performed in conjunction with antibacterial therapy when indicated.
Prescribing doxycycline capsules in the absence of proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
All patients taking doxycycline should be advised:
- to avoid excessive sunlight or artificial ultraviolet light while receiving doxycycline and to discontinue therapy if phototoxicity (e.g., skin eruptions, etc.) occurs. Sunscreen or sunblock should be considered. (See WARNINGS.)
- to drink fluids liberally along with doxycycline to reduce the risk of esophageal irritation and ulceration. (See ADVERSE REACTIONS.)
- that the absorption of tetracyclines is reduced when taken with foods, especially those which contain calcium. However, the absorption of doxycycline is not markedly influenced by simultaneous ingestion of food or milk. (See Drug Interactions.)
- that the absorption of tetracyclines is reduced when taking bismuth subsalicylate. (See Drug Interactions.)
- not to use outdated or poorly stored doxycycline.
- that the use of doxycycline might increase the incidence of vaginal candidiasis.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Patients should be counseled that antibacterial drugs including doxycycline capsules should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When doxycycline capsules are prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by doxycycline capsules or other antibacterial drugs in the future.
Laboratory Tests:
In venereal disease when coexistent syphilis is suspected, a dark-field examination should be done before treatment is started and the blood serology repeated monthly for at least four months.
In long-term therapy, periodic laboratory evaluations of organ systems, including hematopoietic, renal, and hepatic studies should be performed.
Drug Interactions:
Because tetracyclines have been shown to depress plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage.
Since bacteriostatic drugs may interfere with the bactericidal action of penicillin, it is advisable to avoid giving tetracyclines in conjunction with penicillin.
Absorption of tetracyclines is impaired by antacids containing aluminum, calcium, or magnesium, and iron-containing preparations.
Barbiturates, carbamazepine, and phenytoin decrease the half-life of doxycycline.
The concurrent use of tetracycline and methoxyflurane has been reported to result in fatal renal toxicity.
Concurrent use of tetracycline may render oral contraceptives less effective.
Drug/Laboratory Test Interactions:
False elevations of urinary catecholamine levels may occur due to interference with the fluorescence test.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Long-term studies in animals to evaluate the carcinogenic potential of doxycycline have not been conducted. However, there has been evidence of oncogenic activity in rats in studies with related antibacterial, oxytetracycline (adrenal and pituitary tumors) and minocycline (thyroid tumors). Likewise, although mutagenicity studies of doxycycline have not been conducted, positive results in in vitro mammalian cell assays have been reported for related antibacterial (tetracycline, oxytetracycline). Doxycycline administered orally at dosage levels as high as 250 mg/kg/day had no apparent effect on the fertility of female rats. Effect on male fertility has not been studied.
Pregnancy
Teratogenic Effects
Pregnancy Category D
There are no adequate and well-controlled studies on the use of doxycycline in pregnant short-term, first trimester exposure. There are no human data available to assess the effects of long-term therapy of doxycycline in pregnant women such as that proposed for treatment of anthrax exposure. An expert review of published data on experiences with doxycycline use during pregnancy by TERIS - the Teratogen Information System - concluded that therapeutic doses during pregnancy are unlikely to pose a substantial teratogenic risk (the quantity and quality of data were assessed as limited to fair), but the data are insufficient to state that there is no risk.8
A case-control study (18,515 mothers of infants with congenital anomalies and 32,804 mothers of infants with no congenital anomalies) shows a weak but marginally statistically significant association with total malformations and use of doxycycline anytime during pregnancy. (Sixty-three [0.19%] of the controls and 56 [0.30%] of the cases were treated with doxycycline.) This association was not seen when the analysis was confined to maternal treatment during the period of organogenesis (i.e., in the second and third months of gestation) with the exception of a marginal relationship with neural tube defect based on only two exposed cases.9
A small prospective study of 81 pregnancies describes 43 pregnant women treated for 10 days with doxycycline during early first trimester. All mothers reported their exposed infants were normal at 1 year of age.10
Labor and Delivery
The effect of tetracyclines on labor and delivery is unknown.
Nursing Mothers
Tetracyclines are excreted in human milk, however, the extent of absorption of tetracyclines, including doxycycline, by the breastfed infant is not known. Short-term use by lactating women is not necessarily contraindicated; however, the effects of prolonged exposure to doxycycline in breast milk are unknown.11 Because of the potential for adverse reactions in nursing infants from doxycycline, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. (See WARNINGS.)
Pediatric Use
See WARNINGS and DOSAGE AND ADMINISTRATION sections.
-
ADVERSE REACTIONS
Due to oral doxycycline's virtually complete absorption, side effects to the lower bowel, particularly diarrhea, have been infrequent. The following adverse reactions have been observed in patients receiving tetracyclines.
Gastrointestinal
Anorexia, nausea, vomiting, diarrhea, glossitis, dysphagia, enterocolitis, and inflammatory lesions (with monilial overgrowth) in the anogenital region. Hepatotoxicity has been reported. These reactions have been caused by both the oral and parenteral administration of tetracyclines. Rare instances of esophagitis and esophageal ulcerations have been reported in patients receiving capsule and tablet forms of drugs in the tetracycline class. Most of these patients took medications immediately before going to bed. (See DOSAGE AND ADMINISTRATION.)
Skin
Maculopapular and erythematous rashes, Stevens-Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme have been reported. Exfoliative dermatitis has been reported but is uncommon. Photosensitivity is discussed above. (See WARNINGS.)
Renal Toxicity
Rise in BUN has been reported and is apparently dose related. (See WARNINGS.)
Hypersensitivity Reactions
Urticaria, angioneurotic edema, anaphylaxis, anaphylactoid purpura, serum sickness, pericarditis, and exacerbation of systemic lupus erythematosus.
Blood
Hemolytic anemia, thrombocytopenia, neutropenia, and eosinophilia have been reported with tetracyclines.
Other
Intracranial hypertension (IH, pseudotumor cerebri) has been associated with the use of tetracyclines. (See PRECAUTIONS-General.)
When given over prolonged periods, tetracyclines have been reported to produce brown-black microscopic discoloration of the thyroid gland. No abnormalities of thyroid function are known to occur.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
THE USUAL DOSAGE AND FREQUENCY OF ADMINISTRATION OF DOXYCYCLINE DIFFERS FROM THAT OF THE OTHER TETRACYCLINES. EXCEEDING THE RECOMMENDED DOSAGE MAY RESULT IN AN INCREASED INCIDENCE OF SIDE EFFECTS.
Adults
The usual dose of oral doxycycline is 200 mg on the first day of treatment (administered 100 mg every 12 hours or 50 mg every 6 hours) followed by a maintenance dose of 100 mg/day. The maintenance dose may be administered as a single dose or as 50 mg every 12 hours. In the management of more severe infections (particularly chronic infections of the urinary tract), 100 mg every 12 hours is recommended.
For pediatric patients above eight years of age
The recommended dosage schedule for pediatric patients weighing 100 pounds or less is 2 mg/lb of body weight divided into two doses on the first day of treatment, followed by 1 mg/lb of body weight given as a single daily dose or divided into two doses, on subsequent days. For more severe infections up to 2 mg/lb of body weight may be used. For pediatric patients over 100 pounds the usual adult dose should be used.
Uncomplicated gonococcal infections in adults (except anorectal infections in men)
100 mg, by mouth, twice a day for 7 days. As an alternate single visit dose, administer 300 mg stat followed in one hour by a second 300 mg dose.
Acute epididymo-orchitis caused by N. gonorrhoeae
100 mg, by mouth, twice a day for at least 10 days.
Primary and secondary syphilis
300 mg a day in divided doses for at least 10 days.
Uncomplicated urethral, endocervical, or rectal infection in adults caused by Chlamydia trachomatis
100 mg, by mouth, twice a day for at least 7 days.
Nongonococcal urethritis caused by C. trachomatis and U. urealyticum: 100 mg, by mouth, twice a day for at least 7 days.
Acute epididymo-orchitis caused by C. trachomatis
100 mg, by mouth, twice a day for at least 10 days.
Inhalational anthrax (post-exposure)
ADULTS: 100 mg of doxycycline, by mouth, twice a day for 60 days. CHILDREN: weighing less than 100 pounds (45 kg); 1 mg/lb (2.2 mg/kg) of body weight, by mouth, twice a day for 60 days. Children weighing 100 pounds or more should receive the adult dose.
When used in streptococcal infections, therapy should be continued for 10 days.
Administration of adequate amounts of fluid along with capsule and tablet forms of drugs in the tetracycline class is recommended to wash down the drugs and reduce the risk of esophageal irritation and ulceration. (See ADVERSE REACTIONS.) If gastric irritation occurs, doxycycline may be given with food. Ingestion of a high fat meal has been shown to delay the time to peak plasma concentrations by an average of one hour and 20 minutes. However, in the same study, food enhanced the average peak concentration by 7.5% and the area under the curve by 5.7%.
-
HOW SUPPLIED
Doxycycline Capsules USP, 100 mg are light yellow to yellow powder filled in hard gelatin capsule shells having an opaque yellow cap and an opaque orange body printed with 707 on cap in black ink and are supplied as follows:
NDC 63187-712-14 in bottle of 14 capsules
NDC 63187-712-20 in bottle of 20 capsules
NDC 63187-712-30 in bottle of 30 capsules
NDC 63187-712-60 in bottle of 60 capsules
Storage
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP.
ANIMAL PHARMACOLOGY AND ANIMAL TOXICOLOGY
Hyperpigmentation of the thyroid has been produced by members of the tetracycline class in the following species: in rats by oxytetracycline, doxycycline, tetracycline PO4, and methacycline; in minipigs by doxycycline, minocycline, tetracycline PO4, and methacycline; in dogs by doxycycline and minocycline; in monkeys by minocycline.
Minocycline, tetracycline PO4, methacycline, doxycycline, tetracycline base, oxytetracycline HCl and tetracycline HCl were goitrogenic in rats fed a low iodine diet. This goitrogenic effect was accompanied by high radioactive iodine uptake. Administration of minocycline also produced a large goiter with high radioiodine uptake in rats fed a relatively high iodine diet.
Treatment of various animal species with this class of drugs has also resulted in the induction of thyroid hyperplasia in the following: in rats and dogs (minocycline), in chickens (chlortetracycline) and in rats and mice (oxytetracycline). Adrenal gland hyperplasia has been observed in goats and rats treated with oxytetracycline.
-
REFERENCES
- 1.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-third Informational Supplement, CLSI document M100-S23. CLSI document M100S23, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2013.
- 2.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically; Approved Standard – Ninth Edition. CLSI document M07-A9, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2012.
- 3.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Disk Diffusion Susceptibility Tests; Approved Standard – Eleventh Edition. CLSI document M02-A11, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2012.
- 4.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria; Approved Guideline – Second Edition. CLSI document M45 A2, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2010.
- 5.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard – Eighth Edition. CLSI document M11-A8, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2012.
- 6.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Mycobacteria, Nocardiae, and Other Aerobic Actinomycetes; Approved Standard – Second Edition. CLSI document M24-A2, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2011.
- 7.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Susceptibility Testing for Human Mycoplasmas; Approved Guideline. CLSI document M43-A, Clinical Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne Pennsylvania 19087, USA, 2011.
- 8.
- Friedman JM and Polifka JE. Teratogenic Effects of Drugs. A Resource for Clinicians (TERIS). Baltimore, MD: The Johns Hopkins University Press: 2000: 149-195.
- 9.
- Cziezel AE and Rockenbauer M. Teratogenic study of doxycycline. Obstet Gynecol 1997;89:524-528.
- 10.
- Horne HW Jr. and Kundsin RB. The role of mycoplasma among 81 consecutive pregnancies: a prospective study. Int J Fertil 1980; 25:315-317.
- 11.
- Hale T. Medications and Mothers Milk. 9th edition. Amarillo, TX: Pharmasoft Publishing 2000; 225-226.
Please address medical inquiries to, (MedicalAffairs@zydususa.com) Tel.: 1-877-993-8779.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
- SPL UNCLASSIFIED SECTION
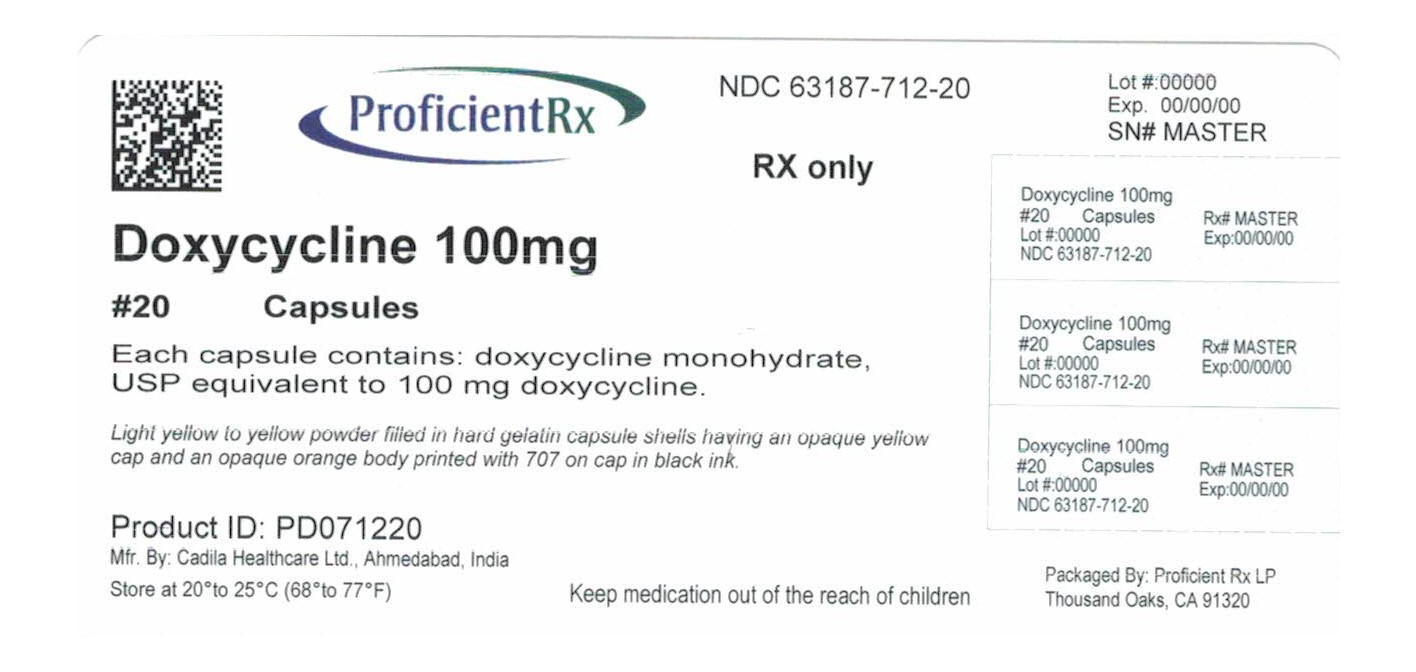
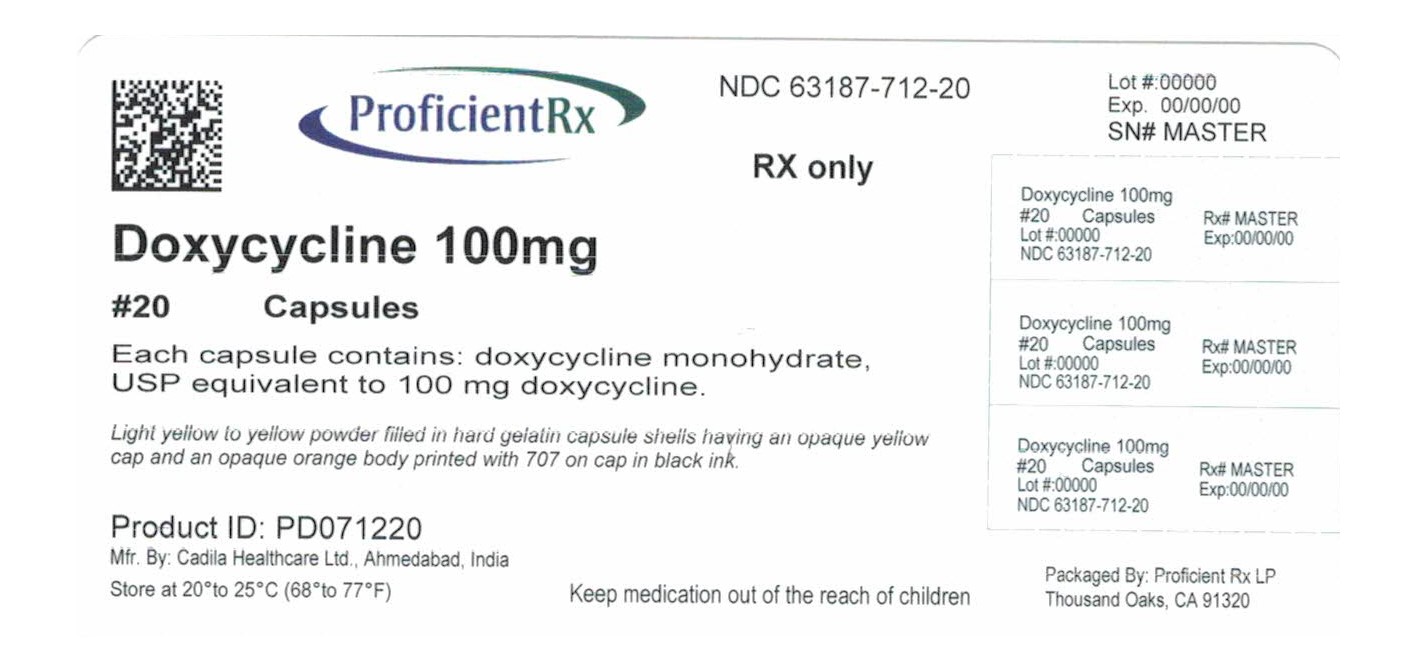
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
DOXYCYCLINE
doxycycline capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63187-712(NDC:68382-707) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DOXYCYCLINE (UNII: N12000U13O) (DOXYCYCLINE ANHYDROUS - UNII:334895S862) DOXYCYCLINE ANHYDROUS 100 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C RED NO. 3 (UNII: PN2ZH5LOQY) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) FERRIC OXIDE RED (UNII: 1K09F3G675) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) Product Characteristics Color YELLOW (OPAQUE YELLOW) , ORANGE (OPAQUE ORANGE) Score no score Shape CAPSULE (CAPSULE) Size 19mm Flavor Imprint Code 707 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63187-712-14 14 in 1 BOTTLE; Type 0: Not a Combination Product 06/01/2016 2 NDC:63187-712-20 20 in 1 BOTTLE; Type 0: Not a Combination Product 06/01/2016 3 NDC:63187-712-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/01/2016 4 NDC:63187-712-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 06/01/2016 5 NDC:63187-712-90 90 in 1 BOTTLE; Type 0: Not a Combination Product 06/01/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205115 03/14/2016 Labeler - Proficient Rx LP (079196022) Establishment Name Address ID/FEI Business Operations Proficient Rx LP 079196022 REPACK(63187-712) , RELABEL(63187-712)