Label: CONJUPRI- levamlodipine tablet
-
Contains inactivated NDC Code(s)
NDC Code(s): 66992-425-30, 66992-430-30 - Packager: WraSer LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated May 3, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CONJUPRI ® safely and effectively. See full prescribing information for CONJUPRI ®.
CONJUPRI ® (levamlodipine) tablets, for oral use.
Initial U.S. Approval: 2019INDICATIONS AND USAGE
CONJUPRI ® is calcium channel blocker and may be used alone or in combination with other antihypertensive agents for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. (1)
DOSAGE AND ADMINISTRATION
- Adult recommended starting dose: 2.5 mg orally once daily with maximum dose 5 mg once daily. (
2.1)
- Small, fragile, or elderly patients, or patients with hepatic insufficiency may be started on 1.25 mg once daily. ( 2.1)
- Pediatric starting dose: 1.25 mg to 2.5 mg once daily. ( 2.2)
Important Limitation: Doses in excess of 2.5 mg daily have not been studied in pediatric patients. ( 2.2)
DOSAGE FORMS AND STRENGTHS
- Tablets: 2.5 mg (functionally scored), and 5 mg, 2.5 mg tablets can be split for 1.25 mg dose. ( 3)
CONTRAINDICATIONS
- Known sensitivity to amlodipine. ( 4)
WARNINGS AND PRECAUTIONS
- Symptomatic hypotension is possible, particularly in patients with severe aortic stenosis. However, acute hypotension is unlikely. ( 5.1)
- Worsening angina and acute myocardial infarction can develop after starting or increasing the dose of amlodipine, particularly in patients with severe obstructive coronary artery disease. ( 5.2)
- Titrate slowly in patients with severe hepatic impairment. ( 5.3)
ADVERSE REACTIONS
Most common adverse reactions to amlodipine is edema which occurred in a dose related manner. Other adverse experiences not dose related but reported with an incidence >1.0% are fatigue, nausea, abdominal pain and somnolence. ( 6)
To report SUSPECTED ADVERSE REACTIONS, call WraSer Pharmaceuticals LLC at 1-888-252-3901 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for FDA-approved patient labeling.
Revised: 8/2021
- Adult recommended starting dose: 2.5 mg orally once daily with maximum dose 5 mg once daily. (
2.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1. INDICATIONS AND USAGE
1.1 Hypertension
2 DOSAGE AND ADMINISTRATION
2.1 Adults
2.2 Children
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension
5.2 Increased Angina or Myocardial Infarction
5.3 Patients with Hepatic Failure
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Impact of Other Drugs on Amlodipine
7.2 Impact of Amlodipine on Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Pediatric Patients
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Effects in Hypertension
16 HOW SUPPLIED/STORAGE AND HANDLING
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1. INDICATIONS AND USAGE
1.1 Hypertension
CONJUPRI ® is indicated for the treatment of hypertension in adults and pediatric patients 6 years and older, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including levamlodipine.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program's Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Levamlodipine may be used alone or in combination with other antihypertensive agents.
-
2 DOSAGE AND ADMINISTRATION
2.1 Adults
The usual initial antihypertensive oral dose of levamlodipine is 2.5 mg once daily, and the maximum dose is 5 mg once daily.
Small, fragile, or elderly patients, or patients with hepatic insufficiency may be started on 1.25 mg once daily and this dose may be used when adding levamlodipine to other antihypertensive therapy.
Adjust dosage according to blood pressure goals. In general, wait 7 to 14 days between titration steps. Titrate more rapidly, however, if clinically warranted, provided the patient is assessed frequently.
2.2 Children
The effective antihypertensive oral dose in pediatric patients ages 6–17 years is 1.25 mg to 2.5 mg once daily. Doses in excess of 2.5 mg daily have not been studied in pediatric patients [see Clinical Pharmacology (12.4), Clinical Studies (14.1)] .
-
3 DOSAGE FORMS AND STRENGTHS
Tablet, 2.5 mg is white to off-white, capsule shaped, flat-faced tablet with functional score on each side, engraved with "OE" on one side and "B47" on the other side.
Tablet of 2.5 mg can be split for 1.25 mg dose for medical conditions that need 1.25 mg dose.
Tablet, 5 mg is white to off-white, soap shaped, flat-faced tablet, engraved with “OE” on one side and “B48” on the other side.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension
Symptomatic hypotension is possible, particularly in patients with severe aortic stenosis. Because of the gradual onset of action, acute hypotension is unlikely.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Amlodipine has been evaluated for safety in more than 11,000 patients in U.S. and foreign clinical trials. In general, treatment with amlodipine besylate was well-tolerated at doses up to 10 mg daily. Most adverse reactions reported during therapy with amlodipine were of mild or moderate severity. In controlled clinical trials directly comparing amlodipine besylate (N = 1730) at doses up to 10 mg to placebo (N = 1250), discontinuation of amlodipine besylate because of adverse reactions was required in only about 1.5% of patients and was not significantly different from placebo (about 1%). The most commonly reported side effects more frequent than placebo are reflected in the table below. The incidence (%) of side effects that occurred in a dose related manner are as follows:
Amlodipine Placebo 2.5mg 5mg 10mg N=275 N=296 N=268 N=520 Edema 1.8 3.0 10.8 0.6 Dizziness 1.1 3.4 3.4 1.5 Flushing 0.7 1.4 2.6 0.0 Palpitation 0.7 1.4 4.5 0.6 Other adverse reactions that were not clearly dose related but were reported with an incidence greater than 1.0% in placebo-controlled clinical trials include the following:
Amlodipine (%)
(N=1730)Placebo (%)
(N=1250)Fatigue 4.5 2.8 Nausea 2.9 1.9 Abdominal Pain 1.6 0.3 Somnolence 1.4 0.6 For several adverse experiences that appear to be drug and dose related, there was a greater incidence in women than men associated with amlodipine treatment as shown in the following table:
Amlodipine (%) Placebo (%) Male = %
(N=1218)Female = %
(N=512)Male = %
(N=914)Female = %
(N=336)Edema 5.6 14.6 1.4 5.1 Flushing 1.5 4.5 0.3 0.9 Palpitations 1.4 3.3 0.9 0.9 Somnolence 1.3 1.6 0.8 0.3 The following events occurred in <1% but >0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain; they are listed to alert the physician to a possible relationship:
Cardiovascular: arrhythmia (including ventricular tachycardia and atrial fibrillation), bradycardia, chest pain, peripheral ischemia, syncope, tachycardia, vasculitis.
Central and Peripheral Nervous System: hypoesthesia, neuropathy peripheral, paresthesia, tremor, vertigo.
Gastrointestinal: anorexia, constipation, dysphagia, diarrhea, flatulence, pancreatitis, vomiting, gingival hyperplasia.
General: allergic reaction, asthenia, 1 back pain, hot flushes, malaise, pain, rigors, weight gain, weight decrease.
Musculoskeletal System: arthralgia, arthrosis, muscle cramps, 1 myalgia.
Psychiatric: sexual dysfunction (male 1 and female), insomnia, nervousness, depression, abnormal dreams, anxiety, depersonalization.
Respiratory System: dyspnea, 1 epistaxis.
Skin and Appendages: angioedema, erythema multiforme, pruritus, 1 rash, 1 rash erythematous, rash maculopapular.
Special Senses: abnormal vision, conjunctivitis, diplopia, eye pain, tinnitus.
Urinary System: micturition frequency, micturition disorder, nocturia.
Autonomic Nervous System: dry mouth, sweating increased.
Metabolic and Nutritional: hyperglycemia, thirst.
Hemopoietic: leukopenia, purpura, thrombocytopenia.
Amlodipine therapy has not been associated with clinically significant changes in routine laboratory tests. No clinically relevant changes were noted in serum potassium, serum glucose, total triglycerides, total cholesterol, HDL cholesterol, uric acid, blood urea nitrogen, or creatinine.
In the CAMELOT and PREVENT studies of amlodipine in coronary artery disease, the adverse event profile was similar to that reported previously (see above), with the most common adverse event being peripheral edema.
- 1
- These events occurred in less than 1% in placebo-controlled trials, but the incidence of these side effects was between 1% and 2% in all multiple dose studies.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following postmarketing event has been reported infrequently where a causal relationship is uncertain: gynecomastia. In postmarketing experience, jaundice and hepatic enzyme elevations (mostly consistent with cholestasis or hepatitis), in some cases severe enough to require hospitalization, have been reported in association with use of amlodipine.
Postmarketing reporting has also revealed a possible association between extrapyramidal disorder and amlodipine.
Amlodipine has been used safely in patients with chronic obstructive pulmonary disease, well-compensated congestive heart failure, coronary artery disease, peripheral vascular disease, diabetes mellitus, and abnormal lipid profiles.
-
7 DRUG INTERACTIONS
7.1 Impact of Other Drugs on Amlodipine
CYP3A Inhibitors
Co-administration with CYP3A inhibitors (moderate and strong) results in increased systemic exposure to amlodipine and may require dose reduction. Monitor for symptoms of hypotension and edema when amlodipine is co-administered with CYP3A inhibitors to determine the need for dose adjustment [see Clinical Pharmacology (12.3)]
CYP3A Inducers
No information is available on the quantitative effects of CYP3A inducers on amlodipine. Blood pressure should be closely monitored when amlodipine is co-administered with CYP3A inducers.
Sildenafil
Monitor for hypotension when sildenafil is co-administered with amlodipine [see Clinical Pharmacology (12.2)] .
7.2 Impact of Amlodipine on Other Drugs
Simvastatin
Co-administration of simvastatin with amlodipine increases the systemic exposure of simvastatin. Limit the dose of simvastatin in patients on amlodipine to 20 mg daily [see Clinical Pharmacology (12.3)] .
Immunosuppressants
Amlodipine may increase the systemic exposure of cyclosporine or tacrolimus when co-administered. Frequent monitoring of trough blood levels of cyclosporine and tacrolimus is recommended and adjust the dose when appropriate [see Clinical Pharmacology (12.3)] .
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The limited available data based on post-marketing reports with amlodipine use in pregnant women are not sufficient to inform a drug-associated risk for major birth defects and miscarriage. There are risks to the mother and fetus associated with poorly controlled hypertension in pregnancy [see Clinical Considerations] . In animal reproduction studies, there was no evidence of adverse developmental effects when pregnant rats and rabbits were treated orally with amlodipine during organogenesis at doses approximately 10 and 20-times the maximum recommended human dose (MRHD), respectively. However for rats, litter size was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly increased (about 5-fold). Amlodipine has been shown to prolong both the gestation period and the duration of labor in rats at this dose [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Hypertension in pregnancy increases the maternal risk for pre-eclampsia, gestational diabetes, premature delivery, and delivery complications (e.g., need for cesarean section and post-partum hemorrhage). Hypertension increases the fetal risk for intrauterine growth restriction and intrauterine death. Pregnant women with hypertension should be carefully monitored and managed accordingly.
Data
Animal Data
No evidence of teratogenicity or other embryo/fetal toxicity was found when pregnant rats and rabbits were treated orally with amlodipine at doses up to 10 mg amlodipine/kg/day (approximately 10 and 20 times the MRHD based on body surface area, respectively) during their respective periods of major organogenesis. However for rats, litter size was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly increased (about 5-fold) in rats receiving amlodipine at a dose equivalent to 10 mg amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine has been shown to prolong both the gestation period and the duration of labor in rats at this dose.
8.2 Lactation
Risk Summary
Limited available data from a published clinical lactation study reports that amlodipine is present in human milk at an estimated median relative infant dose of 4.2%. No adverse effects of amlodipine on the breastfed infant have been observed. There is no available information on the effects of amlodipine on milk production.
8.4 Pediatric Use
Levamlodipine (1.25 to 2.5 mg daily) is effective in lowering blood pressure in patients 6 to 17 years [see Clinical Studies (14.1)] . Effect of levamlodipine on blood pressure in patients less than 6 years of age is not known.
8.5 Geriatric Use
Clinical studies of amlodipine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40–60%, and a lower initial dose may be required [see Dosage and Administration (2.1)] .
-
10 OVERDOSAGE
Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension and possibly a reflex tachycardia. In humans, experience with intentional overdosage of amlodipine is limited.
Single oral doses of amlodipine equivalent to 40 mg amlodipine/kg and 100 mg amlodipine/kg in mice and rats, respectively, caused deaths. Single oral amlodipine doses equivalent to 4 or more mg amlodipine/kg or higher in dogs (11 or more times the maximum recommended human dose on a mg/m 2 basis) caused a marked peripheral vasodilation and hypotension.
If massive overdose should occur, initiate active cardiac and respiratory monitoring. Frequent blood pressure measurements are essential. Should hypotension occur, provide cardiovascular support including elevation of the extremities and the judicious administration of fluids. If hypotension remains unresponsive to these conservative measures, consider administration of vasopressors (such as phenylephrine) with attention to circulating volume and urine output. As amlodipine is highly protein bound, hemodialysis is not likely to be of benefit.
-
11 DESCRIPTION
The active ingredient levamlodipine maleate is the maleate salt of levamlodipine, the pharmacologically active isomer of amlodipine, a long-acting calcium channel blocker.
Levamlodipine maleate is chemically described as (S)3-ethyl-5-methyl-2-(2-aminoethoxymethyl)-4-(2-chlorophenyl)-1,4-dihydro-6-methyl-3,5-pyridinedicarboxylate maleate, and its structural formula is:
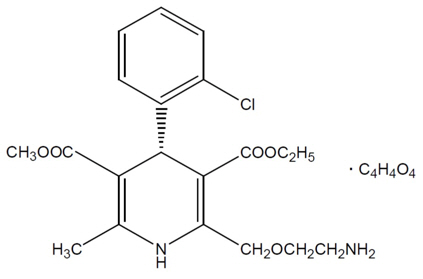
Levamlodipine maleate is an off-white to light yellow crystalline powder with a molecular weight of 524.95. It is slightly soluble in water and sparingly soluble in ethanol. CONJUPRI ® (levamlodipine) tablets are formulated as white to off-white tablets containing 2.5, and 5 mg of levamlodipine (equivalent to 3.2, and 6.4 mg of levamlodipine maleate respectively), for oral administration. In addition to the active ingredient, levamlodipine maleate, each tablet contains the following inactive ingredients: betadex, colloidal silicon dioxide, magnesium stearate, microcrystalline cellulose, and pregelatinized starch .
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Amlodipine is a dihydropyridine calcium antagonist (calcium ion antagonist or slow-channel blocker) that inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle. Experimental data suggest that amlodipine binds to both dihydropyridine and nondihydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure.
Amlodipine is a 1:1 racemic mixture of levamlodipine and dextro amlodipine, it has been demonstrated that levamlodipine is the pharmacologically active, anti-hypertensive isomer.
12.2 Pharmacodynamics
Hemodynamics: Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing. Although the acute intravenous administration of amlodipine decreases arterial blood pressure and increases heart rate in hemodynamic studies of patients with chronic stable angina, chronic oral administration of amlodipine in clinical trials did not lead to clinically significant changes in heart rate or blood pressures in normotensive patients with angina.
With chronic once daily oral administration, antihypertensive effectiveness is maintained for at least 24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The magnitude of reduction in blood pressure with amlodipine is also correlated with the height of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105–114 mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure 90–104 mmHg). Normotensive subjects experienced no clinically significant change in blood pressures (+1/–2 mmHg).
In hypertensive patients with normal renal function, therapeutic doses of amlodipine resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and effective renal plasma flow without change in filtration fraction or proteinuria.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and man, even when co-administered with beta-blockers to man. Similar findings, however, have been observed in normal or well-compensated patients with heart failure with agents possessing significant negative inotropic effects.
Electrophysiologic Effects: amlodipine does not change sinoatrial nodal function or atrioventricular conduction in intact animals or man. In patients with chronic stable angina, intravenous administration of 10 mg did not significantly alter A-H and H-V conduction and sinus node recovery time after pacing. Similar results were obtained in patients receiving amlodipine and concomitant beta-blockers. In clinical studies in which amlodipine was administered in combination with beta-blockers to patients with either hypertension or angina, no adverse effects on electrocardiographic parameters were observed. In clinical trials with angina patients alone, amlodipine therapy did not alter electrocardiographic intervals or produce higher degrees of AV blocks.
Drug Interactions
Sildenafil: When amlodipine and sildenafil were used in combination, each agent independently exerted its own blood pressure lowering effect [see Drug Interactions (7.1)] .
12.3 Pharmacokinetics
The exposure (C max and AUC) of levamlodipine is similar between CONJUPRI ® 5 mg and Norvasc ® (amlodipine besylate) 10 mg under fasting condition.
Absorption
After oral administration of CONJUPRI ®, absorption produces peak plasma concentrations between 6 and 12 hours. Absolute bioavailability has been estimated to be between 64 and 90%. The bioavailability of CONJUPRI ® is not altered by the presence of food.
Distribution
Ex vivo studies have shown that approximately 93% of the circulating drug is bound to plasma proteins in hypertensive patients.
Metabolism
Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism with 10% of the parent compound and 60% of the metabolites excreted in the urine.
Excretion
Elimination from the plasma is biphasic with a terminal elimination half-life of about 30–50 hours. Steady-state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily dosing.
Specific Populations
Renal Impairment
The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose.
Hepatic Impairment
Elderly patients and patients with hepatic insufficiency have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40–60%, and a lower initial dose may be required. A similar increase in AUC was observed in patients with moderate to severe heart failure.
12.4 Pediatric Patients
Sixty-two hypertensive patients aged 6 to 17 years received doses of amlodipine between 1.25 mg and 20 mg. Weight-adjusted clearance and volume of distribution were similar to values in adults.
Drug Interactions
In vitro data indicate that amlodipine has no effect on the human plasma protein binding of digoxin, phenytoin, warfarin, and indomethacin.
Impact of other drugs on amlodipine
Co-administered cimetidine, magnesium-and aluminum hydroxide antacids, sildenafil, and grapefruit juice have no impact on the exposure to amlodipine.
CYP3A inhibitors: Co-administration of a 180 mg daily dose of diltiazem with 5 mg amlodipine in elderly hypertensive patients resulted in a 60% increase in amlodipine systemic exposure. Erythromycin co-administration in healthy volunteers did not significantly change amlodipine systemic exposure. However, strong inhibitors of CYP3A (e.g., itraconazole, clarithromycin) may increase the plasma concentrations of amlodipine to a greater extent [see Drug Interactions (7.1)] .
Impact of amlodipine on other drugs
Amlodipine is a weak inhibitor of CYP3A and may increase exposure to CYP3A substrates.
Co-administered amlodipine does not affect the exposure to atorvastatin, digoxin, ethanol and the warfarin prothrombin response time.
Simvastatin: Co-administration of multiple doses of 10 mg of amlodipine with 80 mg simvastatin resulted in a 77% increase in exposure to simvastatin compared to simvastatin alone [see Drug Interactions (7.2)] .
Cyclosporine: A prospective study in renal transplant patients (N=11) showed on an average of 40% increase in trough cyclosporine levels when concomitantly treated with amlodipine [see Drug Interactions (7.2)] .
Tacrolimus: A prospective study in healthy Chinese volunteers (N=9) with CYP3A5 expressers showed a 2.5- to 4-fold increase in tacrolimus exposure when concomitantly administered with amlodipine compared to tacrolimus alone. This finding was not observed in CYP3A5 non-expressers (N= 6). However, a 3-fold increase in plasma exposure to tacrolimus in a renal transplant patient (CYP3A5 non-expresser) upon initiation of amlodipine for the treatment of post-transplant hypertension resulting in reduction of tacrolimus dose has been reported. Irrespective of the CYP3A5 genotype status, the possibility of an interaction cannot be excluded with these drugs [see Drug Interactions (7.2)] .
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Rats and mice treated with amlodipine in the diet for up to two years, at concentrations calculated to provide daily dosage levels of 0.5, 1.25, and 2.5 amlodipine mg/kg/day, showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on a mg/m 2 basis, similar to the maximum recommended human dose of 10 mg amlodipine/day. 2 For the rat, the highest dose was, on a mg/m 2 basis, about twice the maximum recommended human dose. 2
Mutagenicity studies conducted with amlodipine revealed no drug related effects at either the gene or chromosome level.
There was no effect on the fertility of rats treated orally with amlodipine (males for 64 days and females for 14 days prior to mating) at doses up to 10 mg amlodipine/kg/day (8 times the maximum recommended human dose 2 of 10 mg/day on a mg/m 2 basis).
- 2
- Based on patient weight of 50 kg
-
14 CLINICAL STUDIES
14.1 Effects in Hypertension
Adult Patients
The antihypertensive efficacy of amlodipine has been demonstrated in a total of 15 double-blind, placebo-controlled, randomized studies involving 800 patients on amlodipine and 538 on placebo. Once daily administration produced statistically significant placebo-corrected reductions in supine and standing blood pressures at 24 hours postdose, averaging about 12/6 mmHg in the standing position and 13/7 mmHg in the supine position in patients with mild to moderate hypertension. Maintenance of the blood pressure effect over the 24-hour dosing interval was observed, with little difference in peak and trough effect. Tolerance was not demonstrated in patients studied for up to 1 year. The 3 parallel, fixed dose, dose response studies showed that the reduction in supine and standing blood pressures was dose-related within the recommended dosing range. Effects on diastolic pressure were similar in young and older patients. The effect on systolic pressure was greater in older patients, perhaps because of greater baseline systolic pressure. Effects were similar in black patients and in white patients.
Pediatric Patients
Two hundred sixty-eight hypertensive patients aged 6 to 17 years were randomized first to amlodipine 2.5 or 5 mg once daily for 4 weeks and then randomized again to the same dose or to placebo for another 4 weeks. Patients receiving 2.5 mg or 5 mg at the end of 8 weeks had significantly lower systolic blood pressure than those secondarily randomized to placebo. The magnitude of the treatment effect is difficult to interpret, but it is probably less than 5 mmHg systolic on the 5 mg dose and 3.3 mmHg systolic on the 2.5 mg dose. Adverse events were similar to those seen in adults.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
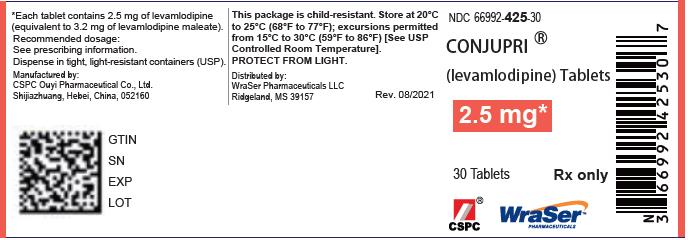
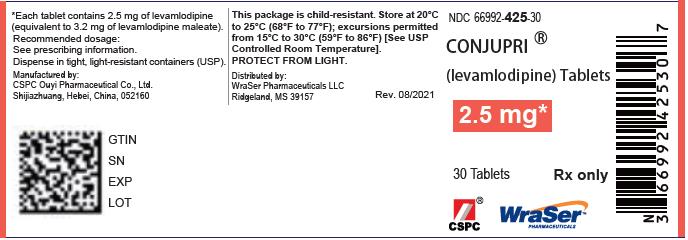
2.5 mg Tablets
Levamlodipine – 2.5 mg tablets are supplied as white to off-white, capsule shaped, flat-faced tablet with functional score on each side, engraved with "OE" on one side and "B47" on the other side and supplied as follows:
NDC 66992-425-30 Bottle of 30 tablets with child-resistant closure
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration Issued: 08/2021 PATIENT INFORMATION
CONJUPRI ® ('kon-ju-pri)
(levamlodipine)
tabletsWhat is CONJUPRI ®?
CONJUPRI ® is a prescription medicine used to treat high blood pressure (hypertension) in adults and pediatric patients 6 years and older. CONJUPRI ® can be used by itself or with other high blood pressure medicines.
It is not known if CONJUPRI ® is safe and effective in children less than 6 years of age.Do not take CONJUPRI ® if you are allergic to amlodipine or to any of the ingredients in CONJUPRI ®. See the end of this Patient Information for a complete list of ingredients in CONJUPRI ®. Before taking CONJUPRI ®, tell your healthcare provider about all of your medical conditions, including if you: - have heart problems
- have liver problems
- are pregnant or plan to become pregnant. It is not known if CONJUPRI ® can harm your unborn baby. Tell your healthcare provider if you become pregnant during treatment with CONJUPRI ®.
- are breastfeeding or plan to breastfeed. CONJUPRI ® can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with CONJUPRI ®.
How should I take CONJUPRI ®? - Take CONJUPRI ® exactly as your healthcare provider tell you to.
- Take CONJUPRI ® 1 time a day.
- If you take too much CONJUPRI ®, contact your local poison control center or go to the nearest hospital emergency room right away.
What are the possible side effects of CONJUPRI ®?
CONJUPRI ® may cause serious side effects, including :- Low blood pressure (hypotension). CONJUPRI ® may cause low blood pressure, especially in people that have a condition called severe aortic stenosis. Tell your healthcare provider if you feel faint or lightheaded.
- Worsening chest pain (angina) or heart attack. CONJUPRI ® may cause worsening chest pain or heart attack after starting or increasing your dose, especially in people with a condition called severe obstructive coronary artery disease. If that happens, call your healthcare provider right away or go directly to a hospital emergency room.
- swelling of your legs or ankles
- tiredness
- nausea
- stomach pain
- sleepiness
- dizziness
- flushing (hot or warm feeling in your face)
- heart palpitations (very fast heartbeat)
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store CONJUPRI ®? - Store CONJUPRI ® at 68°F to 77°F (20°C to 25°C).
- Keep CONJUPRI ® out of the light.
General information about the safe and effective use of CONJUPRI ®.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use CONJUPRI ® for a condition for which it was not prescribed. Do not give CONJUPRI ® to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about CONJUPRI ® that is written for health professionals.What are the ingredients in CONJUPRI ®?
Active ingredient: levamlodipine maleate
Inactive ingredients: betadex, colloidal silicon dioxide, magnesium stearate, microcrystalline cellulose, and pregelatinized starch
Manufactured by:
CSPC Ouyi Pharmaceutical Co., Ltd.
Shijiazhuang, Hebei, China, 052160
Distributed by:
WraSer Pharmaceuticals LLC
Ridgeland, MS 39157
CONJUPRI ® is a registered trademark of CSPC Ouyi Pharmaceutical Co., Ltd.
© 2021 CSPC Ouyi Pharmaceutical Co., Ltd.
For more information, call Toll Free number 1-888-252-3901 - PRINCIPAL DISPLAY PANEL - 2.5 mg Tablet Bottle Label
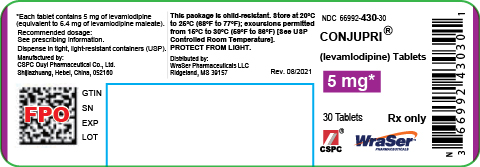
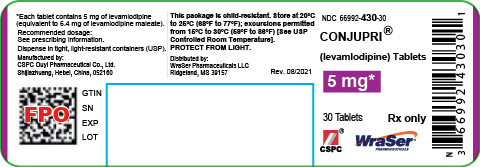
- PRINCIPAL DISPLAY PANEL - 5 mg Tablet Bottle Label
-
INGREDIENTS AND APPEARANCE
CONJUPRI
levamlodipine tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:66992-425 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVAMLODIPINE MALEATE (UNII: 12WW9T2ITA) (LEVAMLODIPINE - UNII:0P6NLP6806) LEVAMLODIPINE MALEATE 2.5 mg Inactive Ingredients Ingredient Name Strength BETADEX (UNII: JV039JZZ3A) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color white (white to off-white) Score 2 pieces Shape OVAL Size 12mm Flavor Imprint Code OE;B47 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:66992-425-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/15/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA212895 08/15/2021 CONJUPRI
levamlodipine tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:66992-430 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVAMLODIPINE MALEATE (UNII: 12WW9T2ITA) (LEVAMLODIPINE - UNII:0P6NLP6806) LEVAMLODIPINE MALEATE 5 mg Inactive Ingredients Ingredient Name Strength BETADEX (UNII: JV039JZZ3A) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color white (white to off-white) Score no score Shape OVAL (Soap Shaped) Size 11mm Flavor Imprint Code OE;B48 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:66992-430-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/15/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA212895 08/15/2021 Labeler - WraSer LLC (121828334) Establishment Name Address ID/FEI Business Operations CSPC OUYI PHARMACEUTICAL CO., LTD 421303775 manufacture(66992-425, 66992-430)