MODERNA COVID-19 VACCINE- cx-024414 injection, suspension
Moderna US, Inc.
----------
FACT SHEET FOR HEALTHCARE PROVIDERS ADMINISTERING VACCINE (VACCINATION PROVIDERS)
EMERGENCY USE AUTHORIZATION (EUA) OF THE MODERNA COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19)
The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, MODERNA COVID-19 VACCINE, for active immunization to prevent COVID-19 in individuals 18 years of age and older.
SUMMARY OF INSTRUCTIONS FOR COVID-19 VACCINATION PROVIDERS
Vaccination providers enrolled in the federal COVID-19 Vaccination Program must report all vaccine administration errors, all serious adverse events, cases of Multisystem Inflammatory Syndrome (MIS) in adults, and cases of COVID-19 that result in hospitalization or death following administration of the Moderna COVID-19 Vaccine. See “MANDATORY REQUIREMENTS FOR MODERNA COVID-19 VACCINE ADMINISTRATION UNDER EMERGENCY USE AUTHORIZATION” for reporting requirements.
The Moderna COVID-19 Vaccine is a suspension for intramuscular injection.
Primary Series:
Each primary series dose of the Moderna COVID-19 Vaccine is 0.5 mL.
The Moderna COVID-19 Vaccine is administered as a primary series of two doses (0.5 mL each) 1 month apart to individuals 18 years of age or older.
A third primary series dose of the Moderna COVID-19 Vaccine (0.5 mL) at least 1 month following the second dose is authorized for administration to individuals at least 18 years of age who have undergone solid organ transplantation, or who are diagnosed with conditions that are considered to have an equivalent level of immunocompromise.
Booster Dose:
The booster dose of the Moderna COVID-19 Vaccine is 0.25 mL.
A single Moderna COVID-19 Vaccine booster dose (0.25 mL) may be administered intramuscularly at least 6 months after completing a primary series of the Moderna COVID-19 Vaccine to individuals 18 years of age or older.
A single booster dose of the Moderna COVID-19 Vaccine (0.25 mL) may be administered as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
See this Fact Sheet for instructions for preparation and administration. This Fact Sheet may have been updated. For the most recent Fact Sheet, please see www.modernatx.com/covid19vaccine-eua.
For information on clinical trials that are testing the use of the Moderna COVID-19 Vaccine for active immunization against COVID-19, please see www.clinicaltrials.gov.
DESCRIPTION OF COVID-19
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the novel coronavirus, SARS-CoV-2, that appeared in late 2019. It is predominantly a respiratory illness that can affect other organs. People with COVID-19 have reported a wide range of symptoms, ranging from mild symptoms to severe illness. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle and body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; diarrhea.
DOSAGE AND ADMINISTRATION
Storage and Handling
The information in this Fact Sheet supersedes the information on the vial and carton labels.
During storage, minimize exposure to room light.
The Moderna COVID-19 Vaccine multiple-dose vials are stored frozen between -50º to -15ºC (-58º to 5ºF). Store in the original carton to protect from light.
Do not store on dry ice or below -50ºC (-58ºF). Use of dry ice may subject vials to temperatures colder than -50°C (-58°F).
Vials may be stored refrigerated between 2° to 8°C (36° to 46°F) for up to 30 days prior to first use.
Vials may be stored between 8° to 25°C (46° to 77°F) for a total of 24 hours.
After the first dose has been withdrawn, the vial should be held between 2° to 25°C (36° to 77°F). Vials should be discarded 12 hours after the first puncture.
Thawed vials can be handled in room light conditions.
Do not refreeze once thawed.
Transportation of Thawed Vials at 2° to 8°C (36° to 46°F)
If transport at -50° to -15°C (-58° to 5°F) is not feasible, available data support transportation of one or more thawed vials for up to 12 hours at 2° to 8°C (36° to 46°F) when shipped using shipping containers which have been qualified to maintain 2° to 8°C (36° to 46°F) and under routine road and air transport conditions with shaking and vibration minimized. Once thawed and transported at 2° to 8°C (36° to 46°F), vials should not be refrozen and should be stored at 2° to 8°C (36° to 46°F) until use.
Dosing and Schedule
Primary Series:
Each primary series dose of the Moderna COVID-19 Vaccine is 0.5 mL.
The Moderna COVID-19 Vaccine is administered as a primary series of two doses (0.5 mL each) 1 month apart to individuals 18 years of age or older.
A third primary series dose of the Moderna COVID-19 Vaccine (0.5 mL) at least 1 month following the second dose is authorized for administration to individuals at least 18 years of age who have undergone solid organ transplantation, or who are diagnosed with conditions that are considered to have an equivalent level of immunocompromise.
Booster Dose:
The booster dose of the Moderna COVID-19 Vaccine is 0.25 mL.
A single Moderna COVID-19 Vaccine booster dose (0.25 mL) may be administered intramuscularly at least 6 months after completing a primary series of the Moderna COVID-19 Vaccine to individuals 18 years of age or older.
A single booster dose of the Moderna COVID-19 Vaccine (0.25 mL) may be administered as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
Dose Preparation
- The Moderna COVID-19 Vaccine multiple-dose vials contain a frozen suspension that does not contain a preservative and must be thawed prior to administration.
- Remove the required number of vial(s) from storage and thaw each vial before use following the instructions below.
|
Multiple-dose Vials Containing |
Thaw in Refrigerator |
Thaw at Room Temperature |
|
5.5 mL |
Thaw in refrigerated conditions between 2° to 8°C (36° to 46°F) for 2 hours and 30 minutes. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw at room temperature between 15° to 25°C (59° to 77°F) for 1 hour. |
|
7.5 mL |
Thaw in refrigerated conditions between 2° to 8°C (36° to 46°F) for 3 hours. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw at room temperature between 15° to 25°C (59° to 77°F) for 1 hour and 30 minutes. |
- After thawing, do not refreeze.
- Swirl vial gently after thawing and between each withdrawal. Do not shake. Do not dilute the vaccine.
- The Moderna COVID-19 Vaccine is a white to off-white suspension. It may contain white or translucent product-related particulates. Visually inspect the Moderna COVID-19 Vaccine vials for other particulate matter and/or discoloration prior to administration. If either of these conditions exists, the vaccine should not be administered.
- The Moderna COVID-19 Vaccine is supplied in two multiple-dose vial presentations:
- A multiple-dose vial containing 5.5 mL
- A multiple-dose vial containing 7.5 mL
- Primary series doses of 0.5 mL and booster doses of 0.25 mL may be extracted from either vial presentation, preferentially using low dead-volume syringes and/or needles.
- When extracting only primary series doses, depending on the syringes and needles used, a maximum of 11 doses (range: 10-11 doses) may be extracted from the vial containing 5.5 mL or a maximum of 15 doses (range: 13-15 doses) may be extracted from the vial containing 7.5 mL.
- When extracting only booster doses or a combination of primary series and booster doses, the maximum number of doses that may be extracted from either vial presentation should not exceed 20 doses. Do not puncture the vial stopper more than 20 times.
- Irrespective of the type of syringe and needle:
- Each primary series dose must contain 0.5 mL of vaccine.
- Each booster dose must contain 0.25 mL of vaccine.
- If the vial stopper has been punctured 20 times, discard the vial and contents.
- If the amount of vaccine remaining in the vial cannot provide a full dose of 0.5 mL or 0.25 mL, discard the vial and contents. Do not pool excess vaccine from multiple vials.
- After the first dose has been withdrawn, the vial should be held between 2° to 25°C (36° to 77°F). Record the date and time of first use on the Moderna COVID-19 Vaccine vial label. Discard vial after 12 hours. Do not refreeze.
Administration
Visually inspect each dose of the Moderna COVID-19 Vaccine in the dosing syringe prior to administration. The white to off-white suspension may contain white or translucent product-related particulates. During the visual inspection,
- verify the final dosing volume of 0.5 mL for a primary series dose or 0.25 mL for a booster dose.
- confirm there are no other particulates and that no discoloration is observed.
- do not administer if vaccine is discolored or contains other particulate matter.
Administer the Moderna COVID-19 Vaccine intramuscularly.
CONTRAINDICATION
Do not administer the Moderna COVID-19 Vaccine to individuals with a known history of a severe allergic reaction (e.g., anaphylaxis) to any component of the Moderna COVID-19 Vaccine (see Full EUA Prescribing Information) .
WARNINGS
Management of Acute Allergic Reactions
Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the Moderna COVID-19 Vaccine.
Monitor Moderna COVID-19 Vaccine recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention (CDC) guidelines ( https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html).
Myocarditis and Pericarditis
Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose. The observed risk is higher among males under 40 years of age than among females and older males. The observed risk is highest in males 18 through 24 years of age. Although some cases required intensive care support, available data from short-term follow-up suggest that most individuals have had resolution of symptoms with conservative management. Information is not yet available about potential long-term sequelae.
Some, but not all, observational analyses of postmarketing data suggest that there may be an increased risk of myocarditis and pericarditis in males under 40 years of age following the second dose of the Moderna COVID-19 Vaccine relative to other authorized or approved mRNA COVID-19 vaccines. Although postmarketing data following a booster dose of mRNA vaccines are limited, available evidence suggests a lower myocarditis risk following a booster dose relative to the risk following the primary series second dose.
The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis ( https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
Altered Immunocompetence
Immunocompromised persons, including individuals receiving immunosuppressant therapy, may have a diminished immune response to the Moderna COVID-19 Vaccine.
Limitations of Vaccine Effectiveness
The Moderna COVID-19 Vaccine may not protect all vaccine recipients.
ADVERSE REACTIONS
Adverse Reactions in Clinical Trials
Adverse reactions reported in clinical trials following administration of the Moderna COVID-19 Vaccine include pain at the injection site, fatigue, headache, myalgia, arthralgia, chills, nausea/vomiting, axillary swelling/tenderness, fever, swelling at the injection site, erythema at the injection site, and rash. (See Full EUA Prescribing Information)
Adverse Reactions in Post-Authorization Experience
Anaphylaxis and other severe allergic reactions, myocarditis, pericarditis, and syncope have been reported following administration of the Moderna COVID-19 Vaccine during mass vaccination outside of clinical trials.
Additional adverse reactions, some of which may be serious, may become apparent with more widespread use of the Moderna COVID-19 Vaccine.
USE WITH OTHER VACCINES
There is no information on the co-administration of the Moderna COVID-19 Vaccine with other vaccines.
INFORMATION TO PROVIDE TO VACCINE RECIPIENTS/CAREGIVERS
As the vaccination provider, you must communicate to the recipient or their caregiver, information consistent with the “Fact Sheet for Recipients and Caregivers” (and provide a copy or direct the individual to the website www.modernatx.com/covid19vaccine-eua to obtain the Fact Sheet) prior to the individual receiving each dose of the Moderna COVID-19 Vaccine, including:
- FDA has authorized the emergency use of the Moderna COVID-19 Vaccine, which is not an FDA-approved vaccine.
- The recipient or their caregiver has the option to accept or refuse the Moderna COVID-19 Vaccine.
- The significant known and potential risks and benefits of the Moderna COVID-19 Vaccine, and the extent to which such risks and benefits are unknown.
- Information about available alternative vaccines and the risks and benefits of those alternatives.
For information on clinical trials that are evaluating the use of the Moderna COVID-19 Vaccine to prevent COVID-19, please see www.clinicaltrials.gov.
Provide a vaccination card to the recipient or their caregiver with the date when the recipient needs to return for the second dose of Moderna COVID-19 Vaccine.
Provide the v-safe information sheet to vaccine recipients/caregivers and encourage vaccine recipients to participate in v-safe. V-safe is a new voluntary smartphone-based tool that uses text messaging and web surveys to check in with people who have been vaccinated to identify potential side effects after COVID-19 vaccination. V-safe asks questions that help CDC monitor the safety of COVID-19 vaccines. V-safe also provides second-dose reminders if needed and live telephone follow-up by CDC if participants report a significant health impact following COVID-19 vaccination. For more information, visit: www.cdc.gov/vsafe.
MANDATORY REQUIREMENTS FOR MODERNA COVID-19 VACCINE ADMINISTRATION UNDER EMERGENCY USE AUTHORIZATION
In order to mitigate the risks of using this unapproved product under EUA and to optimize the potential benefit of the Moderna COVID-19 Vaccine, the following items are required. Use of unapproved Moderna COVID-19 Vaccine for active immunization to prevent COVID-19 under this EUA is limited to the following (all requirements must be met):
- The Moderna COVID-19 Vaccine is authorized for use in individuals 18 years of age and older.
- The vaccination provider must communicate to the individual receiving the Moderna COVID-19 Vaccine or their caregiver information consistent with the “Fact Sheet for Recipients and Caregivers” prior to the individual receiving the Moderna COVID-19 Vaccine.
- The vaccination provider must include vaccination information in the state/local jurisdiction’s Immunization Information System (IIS) or other designated system.
- The vaccination provider is responsible for mandatory reporting of the following to the Vaccine Adverse Event Reporting System (VAERS):
- vaccine administration errors whether or not associated with an adverse event,
- serious adverse events* (irrespective of attribution to vaccination),
- cases of Multisystem Inflammatory Syndrome (MIS) in adults, and
- cases of COVID-19 that result in hospitalization or death.
- Complete and submit reports to VAERS online at https://vaers.hhs.gov/reportevent.html. For further assistance with reporting to VAERS, call 1-800-822-7967. The reports should include the words “Moderna COVID- 19 Vaccine EUA” in the description section of the report.
- The vaccination provider is responsible for responding to FDA requests for information about vaccine administration errors, adverse events, cases of MIS in adults, and cases of COVID-19 that result in hospitalization or death following administration of the Moderna COVID-19 Vaccine to recipients.
*Serious adverse events are defined as:- Death;
- A life-threatening adverse event;
- Inpatient hospitalization or prolongation of existing hospitalization;
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions;
- A congenital anomaly/birth defect;
- An important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed above.
OTHER ADVERSE EVENT REPORTING TO VAERS AND MODERNATX, INC.
Vaccination providers may report to VAERS other adverse events that are not required to be reported using the contact information above.
To the extent feasible, report adverse events to ModernaTX, Inc. using the contact information below or by providing a copy of the VAERS form to ModernaTX, Inc.
|
|
Fax number |
Telephone number |
|
1-866-599-1342 |
1-866-MODERNA
|
ADDITIONAL INFORMATION
For general questions, visit the website or call the telephone number provided below.
To access the most recent Moderna COVID-19 Vaccine Fact Sheets, please scan the QR code or visit the website provided below.
|
Website |
Telephone number |
|
www.modernatx.com/covid19vaccine-eua 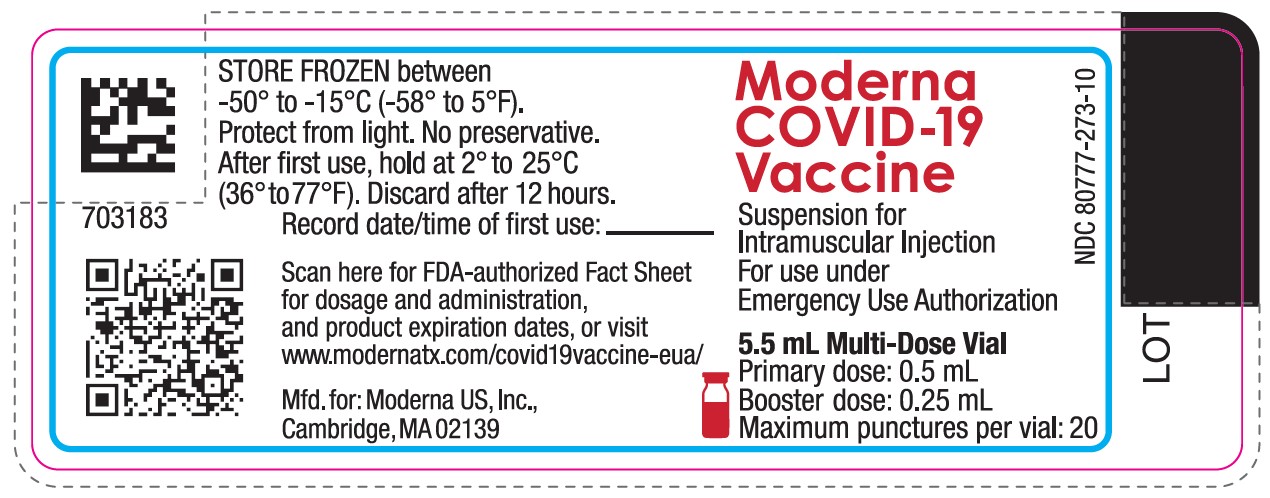 |
1-866-MODERNA
|
AVAILABLE ALTERNATIVES
Comirnaty (COVID-19 Vaccine, mRNA) is an FDA-approved vaccine to prevent COVID-19 caused by SARS-CoV-2. There may be clinical trials or availability under EUA of other COVID-19 vaccines.
FEDERAL COVID-19 VACCINATION PROGRAM
This vaccine is being made available for emergency use exclusively through the CDC COVID-19 Vaccination Program (the Vaccination Program). Healthcare providers must enroll as providers in the Vaccination Program and comply with the provider requirements. Vaccination providers may not charge any fee for the vaccine and may not charge the vaccine recipient any out-of-pocket charge for administration. However, vaccination providers may seek appropriate reimbursement from a program or plan that covers COVID-19 vaccine administration fees for the vaccine recipient (private insurance, Medicare, Medicaid, HRSA COVID-19 Uninsured Program for non-insured recipients). For information regarding provider requirements and enrollment in the CDC COVID-19 Vaccination Program, see https://www.cdc.gov/vaccines/covid-19/provider-enrollment.html.
Individuals becoming aware of any potential violations of the CDC COVID-19 Vaccination Program requirements are encouraged to report them to the Office of the Inspector General, U.S. Department of Health and Human Services, at 1-800-HHS-TIPS or TIPS.HHS.GOV.
AUTHORITY FOR ISSUANCE OF THE EUA
The Secretary of the Department of Health and Human Services (HHS) has declared a public health emergency that justifies the emergency use of drugs and biological products during the COVID-19 Pandemic. In response, the FDA has issued an EUA for the unapproved product, Moderna COVID-19 Vaccine, for active immunization to prevent COVID-19 in individuals 18 years of age and older.
FDA issued this EUA, based on ModernaTX, Inc.’s request and submitted data.
Although limited scientific information is available, based on the totality of the scientific evidence available to date, it is reasonable to believe that the Moderna COVID-19 Vaccine may be effective for the prevention of COVID-19 in individuals as specified in the Full EUA Prescribing Information.
This EUA for the Moderna COVID-19 Vaccine will end when the Secretary of HHS determines that the circumstances justifying the EUA no longer exist or when there is a change in the approval status of the product such that an EUA is no longer needed.
For additional information about Emergency Use Authorization, visit FDA at: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy- framework/emergency-use-authorization.
COUNTERMEASURES INJURY COMPENSATION PROGRAM
The Countermeasures Injury Compensation Program (CICP) is a federal program that has been created to help pay for related costs of medical care and other specific expenses to compensate people injured after use of certain medical countermeasures. Medical countermeasures are specific vaccines, medications, devices, or other items used to prevent, diagnose, or treat the public during a public health emergency or a security threat. For more information about CICP regarding the vaccines to prevent COVID-19, visit http://www.hrsa.gov/cicp, email cicp@hrsa.gov, or call: 1-855-266-2427.
Moderna US, Inc.
Cambridge, MA 02139
©2021 ModernaTX, Inc. All rights reserved.
Patent(s):
www.modernatx.com/patents
Revised: Nov/19/2021
END SHORT VERSION FACT SHEET
Long Version (Full EUA Prescribing Information) Begins On Next Page
FULL EMERGENCY USE AUTHORIZATION (EUA)
PRESCRIBING INFORMATION
MODERNA COVID-19 VACCINE
|
FULL EUA PRESCRIBING INFORMATION: CONTENTS* |
11 USE IN SPECIFIC POPULATIONS |
|
1 AUTHORIZED USE |
11.1 Pregnancy |
|
2 DOSAGE AND ADMINISTRATION |
11.2 Lactation |
|
2.1 Preparation for Administration |
11.3 Pediatric Use |
|
2.2 Administration |
11.4 Geriatric Use |
|
2.3 Dosing and Schedule |
11.5 Use in Immunocompromised |
|
3 DOSAGE FORMS AND STRENGTHS |
13 DESCRIPTION |
|
4 CONTRAINDICATIONS |
14 CLINICAL PHARMACOLOGY |
|
5 WARNINGS AND PRECAUTIONS |
14.1 Mechanism of Action |
|
5.1 Management of Acute Allergic Reactions |
18 CLINICAL TRIAL RESULTS AND SUPPORTING DATA FOR EUA 18.1 Efficacy of Two-Dose Primary Series 18.2 Immunogenicity in Solid Organ Transplant Recipients 18.3 Immunogenicity of a Booster Dose Following a Moderna COVID-19 Vaccine Primary Series 18.4 Immunogenicity of a Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine 19 HOW SUPPLIED/STORAGE AND HANDLING 20 PATIENT COUNSELING INFORMATION 21 CONTACT INFORMATION *Sections or subsections omitted from the full prescribing information are not listed |
|
5.2 Myocarditis and Pericarditis |
|
|
5.3 Syncope |
|
|
5.4 Altered Immunocompetence |
|
|
5.5 Limitations of Vaccine Effectiveness |
|
|
6 OVERALL SAFETY SUMMARY |
|
|
6.1 Clinical Trials Experience |
|
|
6.2 Post-Authorization Experience |
|
|
8 REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS |
|
|
10 DRUG INTERACTIONS |
1 AUTHORIZED USE
Moderna COVID-19 Vaccine is authorized for use under an Emergency Use Authorization (EUA) for active immunization to prevent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in individuals 18 years of age and older.
2 DOSAGE AND ADMINISTRATION
For intramuscular injection only.
2.1 Preparation for Administration
- The Moderna COVID-19 Vaccine multiple-dose vials contain a frozen suspension that does not contain a preservative and must be thawed prior to administration.
- Remove the required number of vial(s) from storage and thaw each vial before use following the instructions below.
|
Multiple-dose Vials Containing |
Thaw in Refrigerator |
Thaw at Room Temperature |
|
5.5 mL |
Thaw in refrigerated conditions between 2° to 8°C (36° to 46°F) for 2 hours and 30 minutes. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw at room temperature between 15° to 25°C (59° to 77°F) for 1 hour. |
|
7.5 mL |
Thaw in refrigerated conditions between 2° to 8°C (36° to 46°F) for 3 hours. Let each vial stand at room temperature for 15 minutes before administering. |
Alternatively, thaw at room temperature between 15° to 25°C (59° to 77°F) for 1 hour and 30 minutes. |
- After thawing, do not refreeze.
- Swirl vial gently after thawing and between each withdrawal. Do not shake. Do not dilute the vaccine.
- The Moderna COVID-19 Vaccine is a white to off-white suspension. It may contain white or translucent product-related particulates. Visually inspect the Moderna COVID-19 Vaccine vials for other particulate matter and/or discoloration prior to administration. If either of these conditions exists, the vaccine should not be administered.
- The Moderna COVID-19 Vaccine is supplied in two multiple-dose vial presentations:
- A multiple-dose vial containing 5.5 mL
- A multiple-dose vial containing 7.5 mL
- Primary series doses of 0.5 mL and booster doses of 0.25 mL may be extracted from either vial presentation, preferentially using low dead-volume syringes and/or needles.
- When extracting only primary series doses, depending on the syringes and needles used, a maximum of 11 doses (range: 10-11 doses) may be extracted from the vial containing 5.5 mL or a maximum of 15 doses (range: 13-15 doses) may be extracted from the vial containing 7.5 mL.
- When extracting only booster doses or a combination of primary series and booster doses, the maximum number of doses that may be extracted from either vial presentation should not exceed 20 doses. Do not puncture the vial stopper more than 20 times.
- Irrespective of the type of syringe and needle:
- Each primary series dose must contain 0.5 mL of vaccine.
- Each booster dose must contain 0.25 mL of vaccine.
- If the vial stopper has been punctured 20 times, discard the vial and contents.
- If the amount of vaccine remaining in the vial cannot provide a full dose of 0.5 mL or 0.25 mL, discard the vial and contents. Do not pool excess vaccine from multiple vials.
- After the first dose has been withdrawn, the vial should be held between 2° to 25°C (36° to 77°F). Record the date and time of first use on the Moderna COVID-19 Vaccine vial label. Discard vial after 12 hours. Do not refreeze.
2.2 Administration
Visually inspect each dose of the Moderna COVID-19 Vaccine in the dosing syringe prior to administration. The white to off-white suspension may contain white or translucent product-related particulates. During the visual inspection,
- verify the final dosing volume of 0.5 mL for a primary series dose or 0.25 mL for a booster dose.
- confirm there are no other particulates and that no discoloration is observed.
- do not administer if vaccine is discolored or contains other particulate matter.
Administer the Moderna COVID-19 Vaccine intramuscularly.
2.3 Dosing and Schedule
Primary Series:
Each primary series dose of the Moderna COVID-19 Vaccine is 0.5 mL.
The Moderna COVID-19 Vaccine is administered as a primary series of two doses (0.5 mL each) 1 month apart to individuals 18 years of age or older.
A third primary series dose of the Moderna COVID-19 Vaccine (0.5 mL) at least 1 month following the second dose is authorized for administration to individuals at least 18 years of age who have undergone solid organ transplantation, or who are diagnosed with conditions that are considered to have an equivalent level of immunocompromise.
Booster Dose:
The booster dose of the Moderna COVID-19 Vaccine is 0.25 mL.
A single Moderna COVID-19 Vaccine booster dose (0.25 mL) may be administered intramuscularly at least 6 months after completing a primary series of the Moderna COVID-19 Vaccine to individuals 18 years of age or older.
A single booster dose of the Moderna COVID-19 Vaccine (0.25 mL) may be administered as a heterologous booster dose following completion of primary vaccination with another authorized or approved COVID-19 vaccine. The dosing interval for the heterologous booster dose is the same as that authorized for a booster dose of the vaccine used for primary vaccination.
3 DOSAGE FORMS AND STRENGTHS
Moderna COVID-19 Vaccine is a suspension for intramuscular injection.
- Each primary series dose is 0.5 mL.
- The booster dose is 0.25 mL.
4 CONTRAINDICATIONS
Do not administer the Moderna COVID-19 Vaccine to individuals with a known history of severe allergic reaction (e.g., anaphylaxis) to any component of the Moderna COVID-19 Vaccine [see Description ( 13)] .
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment to manage immediate allergic reactions must be immediately available in the event an acute anaphylactic reaction occurs following administration of the Moderna COVID-19 Vaccine.
Monitor Moderna COVID-19 Vaccine recipients for the occurrence of immediate adverse reactions according to the Centers for Disease Control and Prevention (CDC) guidelines ( https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html).
5.2 Myocarditis and Pericarditis
Postmarketing data demonstrate increased risks of myocarditis and pericarditis, particularly within 7 days following the second dose. The observed risk is higher among males under 40 years of age than among females and older males. The observed risk is highest in males 18 through 24 years of age. Although some cases required intensive care support, available data from short-term follow-up suggest that most individuals have had resolution of symptoms with conservative management. Information is not yet available about potential long-term sequelae.
Some, but not all, observational analyses of postmarketing data suggest that there may be an increased risk of myocarditis and pericarditis in males under 40 years of age following the second dose of the Moderna COVID-19 Vaccine relative to other authorized or approved mRNA COVID-19 vaccines. Although postmarketing data following a booster dose of mRNA vaccines are limited, available evidence suggests a lower myocarditis risk following a booster dose relative to the risk following the primary series second dose.
The CDC has published considerations related to myocarditis and pericarditis after vaccination, including for vaccination of individuals with a history of myocarditis or pericarditis ( https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html).
5.3 Syncope
Syncope (fainting) may occur in association with administration of injectable vaccines. Procedures should be in place to avoid injury from fainting.
6 OVERALL SAFETY SUMMARY
It is MANDATORY for vaccination providers to report to the Vaccine Adverse Event Reporting System (VAERS) all vaccine administration errors, all serious adverse events, cases of Multisystem Inflammatory Syndrome (MIS) in adults, and hospitalized or fatal cases of COVID-19 following vaccination with the Moderna COVID-19 Vaccine. To the extent feasible, provide a copy of the VAERS form to ModernaTX, Inc. Please see the REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS section for details on reporting to VAERS and ModernaTX, Inc.
In a clinical study, the adverse reactions in participants 18 years of age and older following administration of the primary series included pain at the injection site (92.0%), fatigue (70.0%), headache (64.7%), myalgia (61.5%), arthralgia (46.4%), chills (45.4%), nausea/vomiting (23.0%), axillary swelling/tenderness (19.8%), fever (15.5%), swelling at the injection site (14.7%), and erythema at the injection site (10.0%).
In a clinical study, the adverse reactions in participants 18 years of age and older following administration of a booster dose included pain at the injection site (83.8%), fatigue (58.7%), headache (55.1%), myalgia (49.1%), arthralgia (41.3%), chills (35.3%), axillary swelling/tenderness (20.4%), nausea/vomiting (11.4%), fever (6.6%), swelling at the injection site (5.4%), erythema at the injection site (4.8%), and rash (1.8%).
Anaphylaxis and other severe allergic reactions, myocarditis, pericarditis, and syncope have been reported following administration of the Moderna COVID-19 Vaccine outside of clinical trials.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Overall, 15,419 participants aged 18 years and older received at least one dose of Moderna COVID- 19 Vaccine in three clinical trials (NCT04283461, NCT04405076, and NCT04470427). In a fourth clinical trial (NCT04885907), 60 solid organ transplant recipients received a third dose of Moderna COVID-19 Vaccine.
Two-Dose Primary Series
The safety of Moderna COVID-19 Vaccine was evaluated in an ongoing Phase 3 randomized, placebo-controlled, observer-blind clinical trial conducted in the United States involving 30,351 participants 18 years of age and older who received at least one dose (0.5 mL) of Moderna COVID-19 Vaccine (n=15,185) or placebo (n=15,166) (Study 1, NCT04470427). At the time of vaccination, the mean age of the population was 52 years (range 18-95); 22,831 (75.2%) of participants were 18 to 64 years of age and 7,520 (24.8%) of participants were 65 years of age and older. Overall, 52.7% were male, 47.3% were female, 20.5% were Hispanic or Latino, 79.2% were White, 10.2% were African American, 4.6% were Asian, 0.8% were American Indian or Alaska Native, 0.2% were Native Hawaiian or Pacific Islander, 2.1% were other races, and 2.1% were Multiracial. Demographic characteristics were similar among participants who received Moderna COVID-19 Vaccine and those who received placebo.
Solicited Adverse Reactions
Local and systemic adverse reactions and use of antipyretic medication were solicited in an electronic diary for 7 days following each injection (i.e., day of vaccination and the next 6 days) among participants receiving Moderna COVID-19 Vaccine (n=15,179) and participants receiving placebo (n=15,163) with at least 1 documented dose. Events that persisted for more than 7 days were followed until resolution. Solicited adverse reactions were reported more frequently among vaccine participants than placebo participants.
The reported number and percentage of the solicited local and systemic adverse reactions by age group and dose are presented in Table 1 and Table 2, respectively.
| Moderna COVID-19 Vaccine | Placebo a | |||
|---|---|---|---|---|
| Dose 1
(N=11,406) n (%) | Dose 2
(N=10,985) n (%) | Dose 1
(N=11,407) n (%) | Dose 2
(N=10,918) n (%) |
|
| * 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Placebo was a saline solution. b Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity. c Grade 3 swelling and erythema: Defined as >100 mm / >10 cm. d Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity. e Grade 4 fatigue, arthralgia: Defined as requires emergency room visit or hospitalization. f Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity. g Grade 3 chills: Defined as prevents daily activity and requires medical intervention. h Grade 3 nausea/vomiting: Defined as prevents daily activity, requires outpatient intravenous hydration. i Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F. j Grade 4 fever: Defined as >40.0°C / >104.0°F. |
||||
|
Local Adverse Reactions | ||||
|
Pain |
9,908 (86.9) |
9,873 (89.9) |
2,177 (19.1) |
2,040 (18.7) |
|
Pain, Grade 3 b |
366 (3.2) |
506 (4.6) |
23 (0.2) |
22 (0.2) |
|
Axillary swelling/tenderness |
1,322 (11.6) |
1,775 (16.2) |
567 (5.0) |
470 (4.3) |
|
Axillary swelling/tenderness, Grade 3 b |
37 (0.3) |
46 (0.4) |
13 (0.1) |
11 (0.1) |
|
Swelling (hardness) ≥25 mm |
767 (6.7) |
1,389 (12.6) |
34 (0.3) |
36 (0.3) |
|
Swelling (hardness), Grade 3 c |
62 (0.5) |
182 (1.7) |
3 (<0.1) |
4 (<0.1) |
|
Erythema (redness) ≥25 mm |
344 (3.0) |
982 (8.9) |
47 (0.4) |
43 (0.4) |
|
Erythema (redness), Grade 3 c |
34 (0.3) |
210 (1.9) |
11 (<0.1) |
12 (0.1) |
|
Systemic Adverse Reactions | ||||
|
Fatigue |
4,384 (38.4) |
7,430 (67.6) |
3,282 (28.8) |
2,687 (24.6) |
|
Fatigue, Grade 3 d |
120 (1.1) |
1,174 (10.7) |
83 (0.7) |
86 (0.8) |
|
Fatigue, Grade 4 e |
1 (<0.1) |
0 (0) |
0 (0) |
0 (0) |
|
Headache |
4,030 (35.3) |
6,898 (62.8) |
3,304 (29.0) |
2,760 (25.3) |
|
Headache, Grade 3 f |
219 (1.9) |
553 (5.0) |
162 (1.4) |
129 (1.2) |
|
Myalgia |
2,699 (23.7) |
6,769 (61.6) |
1,628 (14.3) |
1,411 (12.9) |
|
Myalgia, Grade 3 d |
73 (0.6) |
1,113 (10.1) |
38 (0.3) |
42 (0.4) |
|
Arthralgia |
1,893 (16.6) |
4,993 (45.5) |
1,327 (11.6) |
1,172 (10.7) |
|
Arthralgia, Grade 3 d |
47 (0.4) |
647 (5.9) |
29 (0.3) |
37 (0.3) |
|
Arthralgia, Grade 4 e |
1 (<0.1) |
0 (0) |
0 (0) |
0 (0) |
|
Chills |
1,051 (9.2) |
5,341 (48.6) |
730 (6.4) |
658 (6.0) |
|
Chills, Grade 3 g |
17 (0.1) |
164 (1.5) |
8 (<0.1) |
15 (0.1) |
|
Nausea/vomiting |
1,068 (9.4) |
2,348 (21.4) |
908 (8.0) |
801 (7.3) |
|
Nausea/vomiting, Grade 3 h |
6 (<0.1) |
10 (<0.1) |
8 (<0.1) |
8 (<0.1) |
|
Fever |
105 (0.9) |
1,908 (17.4) |
37 (0.3) |
39 (0.4) |
|
Fever, Grade 3 i |
10 (<0.1) |
184 (1.7) |
1 (<0.1) |
2 (<0.1) |
|
Fever, Grade 4 j |
4 (<0.1) |
12 (0.1) |
4 (<0.1) |
2 (<0.1) |
|
Use of antipyretic or pain medication |
2,656 (23.3) |
6,292 (57.3) |
1,523 (13.4) |
1,248 (11.4) |
| Moderna COVID-19 Vaccine | Placebo a | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Dose 1
(N=3,762) n (%) | Dose 2
(N=3,692) n (%) | Dose 1
(N=3,748) n (%) | Dose 2
(N=3,648) n (%) |
||||||
| * 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Placebo was a saline solution. b Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity. c Grade 3 swelling and erythema: Defined as >100 mm / >10 cm. d Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity. e Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity. f Grade 3 chills: Defined as prevents daily activity and requires medical intervention. g Grade 3 nausea/vomiting: Defined as prevents daily activity, requires outpatient intravenous hydration. h Grade 4 nausea/vomiting: Defined as requires emergency room visit or hospitalization for hypotensive shock. i Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F. j Grade 4 fever: Defined as >40.0°C / >104.0°F. |
|||||||||
|
Local Adverse Reactions | |||||||||
|
Pain |
2,782 (74.0) |
3,070 (83.2) |
481 (12.8) |
437 (12.0) |
|||||
|
Pain, Grade 3 b |
50 (1.3) |
98 (2.7) |
32 (0.9) |
18 (0.5) |
|||||
|
Axillary swelling/tenderness |
231 (6.1) |
315 (8.5) |
155 (4.1) |
97 (2.7) |
|||||
|
Axillary swelling/tenderness, Grade 3 b |
12 (0.3) |
21 (0.6) |
14 (0.4) |
8 (0.2) |
|||||
|
Swelling (hardness) ≥25 mm |
165 (4.4) |
400 (10.8) |
18 (0.5) |
13 (0.4) |
|||||
|
Swelling (hardness), Grade 3 c |
20 (0.5) |
72 (2.0) |
3 (<0.1) |
7 (0.2) |
|||||
|
Erythema (redness) ≥25 mm |
86 (2.3) |
275 (7.5) |
20 (0.5) |
13 (0.4) |
|||||
|
Erythema (redness), Grade 3 c |
8 (0.2) |
77 (2.1) |
2 (<0.1) |
3 (<0.1) |
|||||
|
Systemic Adverse Reactions | |||||||||
|
Fatigue |
1,251 (33.3) |
2,152 (58.3) |
851 (22.7) |
716 (19.6) |
|||||
|
Fatigue, Grade 3 d |
30 (0.8) |
254 (6.9) |
22 (0.6) |
20 (0.5) |
|||||
|
Headache |
921 (24.5) |
1,704 (46.2) |
723 (19.3) |
650 (17.8) |
|||||
|
Headache, Grade 3 e |
52 (1.4) |
106 (2.9) |
34 (0.9) |
33 (0.9) |
|||||
|
Myalgia |
742 (19.7) |
1,739 (47.1) |
443 (11.8) |
398 (10.9) |
|||||
|
Myalgia, Grade 3 d |
17 (0.5) |
205 (5.6) |
9 (0.2) |
10 (0.3) |
|||||
|
Arthralgia |
618 (16.4) |
1,291 (35.0) |
456 (12.2) |
397 (10.9) |
|||||
|
Arthralgia, Grade 3 d |
13 (0.3) |
123 (3.3) |
8 (0.2) |
7 (0.2) |
|||||
|
Chills |
202 (5.4) |
1,141 (30.9) |
148 (4.0) |
151 (4.1) |
|||||
|
Chills, Grade 3 f |
7 (0.2) |
27 (0.7) |
6 (0.2) |
2 (<0.1) |
|||||
|
Nausea/vomiting |
194 (5.2) |
437 (11.8) |
166 (4.4) |
133 (3.6) |
|||||
|
Nausea/vomiting, Grade 3 g |
4 (0.1) |
10 (0.3) |
4 (0.1) |
3 (<0.1) |
|||||
|
Nausea/vomiting, Grade 4 h |
0 (0) |
1 (<0.1) |
0 (0) |
0 (0) |
|||||
|
Fever |
10 (0.3) |
370 (10.0) |
7 (0.2) |
4 (0.1) |
|||||
|
Fever, Grade 3 i |
1 (<0.1) |
18 (0.5) |
1 (<0.1) |
0 (0) |
|||||
|
Fever, Grade 4 j |
0 (0) |
1 (<0.1) |
2 (<0.1) |
1 (<0.1) |
|||||
|
Use of antipyretic or pain medication |
673 (17.9) |
1,546 (41.9) |
477 (12.7) |
329 (9.0) |
|||||
Solicited local and systemic adverse reactions reported following administration of Moderna COVID-19 Vaccine had a median duration of 1 to 3 days.
Grade 3 solicited local adverse reactions were more frequently reported after Dose 2 than after Dose 1. Solicited systemic adverse reactions were more frequently reported by vaccine recipients after Dose 2 than after Dose 1.
Unsolicited Adverse Events
Participants were monitored for unsolicited adverse events for up to 28 days following each dose and follow-up is ongoing. Serious adverse events and medically attended adverse events will be recorded for the entire study duration of 2 years. As of November 25, 2020, among participants who had received at least 1 dose of vaccine or placebo (vaccine=15,185, placebo=15,166), unsolicited adverse events that occurred within 28 days following each vaccination were reported by 23.9% of participants (n=3,632) who received Moderna COVID-19 Vaccine and 21.6% of participants (n=3,277) who received placebo. In these analyses, 87.9% of study participants had at least 28 days of follow-up after Dose 2.
Lymphadenopathy-related events that were not necessarily captured in the 7-day e-diary were reported by 1.1% of vaccine recipients and 0.6% of placebo recipients. These events included lymphadenopathy, lymphadenitis, lymph node pain, vaccination-site lymphadenopathy, injection-site lymphadenopathy, and axillary mass, which were plausibly related to vaccination. This imbalance is consistent with the imbalance observed for solicited axillary swelling/tenderness in the injected arm.
Hypersensitivity adverse events were reported in 1.5% of vaccine recipients and 1.1% of placebo recipients. Hypersensitivity events in the vaccine group included injection site rash and injection site urticaria, which are likely related to vaccination. Delayed injection site reactions that began >7 days after vaccination were reported in 1.2% of vaccine recipients and 0.4% of placebo recipients. Delayed injection site reactions included pain, erythema, and swelling and are likely related to vaccination.
Throughout the same period, there were three reports of Bell’s palsy in the Moderna COVID-19 Vaccine group (one of which was a serious adverse event), which occurred 22, 28, and 32 days after vaccination, and one in the placebo group which occurred 17 days after vaccination. Currently available information on Bell’s palsy is insufficient to determine a causal relationship with the vaccine.
There were no other notable patterns or numerical imbalances between treatment groups for specific categories of adverse events (including other neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Moderna COVID-19 Vaccine.
Serious Adverse Events
As of November 25, 2020, serious adverse events were reported by 1.0% (n=147) of participants who received Moderna COVID-19 Vaccine and 1.0% (n=153) of participants who received placebo, one of which was the case of Bell’s palsy which occurred 32 days following receipt of vaccine.
In these analyses, 87.9% of study participants had at least 28 days of follow-up after Dose 2, and the median follow-up time for all participants was 9 weeks after Dose 2.
There were two serious adverse events of facial swelling in vaccine recipients with a history of injection of dermatological fillers. The onset of swelling was reported 1 and 2 days, respectively, after vaccination and was likely related to vaccination.
There was one serious adverse event of intractable nausea and vomiting in a participant with prior history of severe headache and nausea requiring hospitalization. This event occurred 1 day after vaccination and was likely related to vaccination.
There were no other notable patterns or imbalances between treatment groups for specific categories of serious adverse events (including neurologic, neuro-inflammatory, and thrombotic events) that would suggest a causal relationship to Moderna COVID-19 Vaccine.
Solid Organ Transplant Recipients
From an independent study (NCT04885907), in 60 participants who had undergone various solid organ transplant procedures (heart, kidney, kidney-pancreas, liver, lung, pancreas) a median of 3.57 years previously (range 1.99-6.75 years) who received a third vaccine dose (0.5 mL), the adverse event profile was similar to that after the second dose and no Grade 3 or Grade 4 events were reported.
Booster Dose Following a Primary Series of Moderna COVID-19 Vaccine
Study 2 is an ongoing Phase 2, randomized, observer-blind, placebo-controlled, dose-confirmation study to evaluate the safety, reactogenicity, and immunogenicity of the Moderna COVID-19 Vaccine in participants 18 years of age and older (NCT04405076). In this study, 198 participants received two doses (0.5 mL 1 month apart) of the Moderna COVID-19 Vaccine primary series. In an open label-phase, 171 of those participants received a single booster dose (0.25 mL) at least 6 months (range of 5.8 to 8.5 months) after receiving the second dose of the primary series. Safety monitoring after the booster dose was the same as that described for Study 1 participants who received the primary series.
Among the 171 booster dose recipients, the median age was 55 years (range 18-87), 39.2% were male and 60.8% were female, 95.9% were White, 5.8% were Hispanic or Latino, 2.9% were Black or African American, 0.6% were Asian, and 0.6% were American Indian or Alaska Native. Following the booster dose, the median follow-up time was 5.7 months (range of 3.1 to 6.4 months).
Solicited Adverse Reactions
Tables 3 and 4 present the frequency and severity of reported solicited local and systemic adverse reactions among Study 2 Moderna COVID-19 Vaccine booster dose recipients 18 to <65 years of age and ≥65 years of age, respectively, within 7 days of a booster vaccination.
| Study 2
Second Dose of Primary Series (N=155) n (%) | Study 2
Booster Dose (N=129) n (%) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| * 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Grade 3 pain and axillary swelling/tenderness: Defined as any use of prescription pain reliever; prevents daily activity. b Grade 3 erythema: Defined as >100 mm / >10 cm. c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity. d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity. e Grade 3 chills: Defined as prevents daily activity and requires medical intervention. f Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F. |
||||||||||||
|
Local Adverse Reactions | ||||||||||||
|
Pain |
137 (88.4) |
111 (86.0) |
||||||||||
|
Pain, Grade 3 a |
1 (0.6) |
4 (3.1) |
||||||||||
|
Axillary swelling/tenderness |
18 (11.6) |
32 (24.8) |
||||||||||
|
Axillary swelling/tenderness, Grade 3 a |
0 (0) |
1 (0.8) |
||||||||||
|
Swelling (hardness) ≥25 mm |
16 (10.3) |
8 (6.2) |
||||||||||
|
Erythema (redness) ≥25 mm |
12 (7.7) |
7 (5.4) |
||||||||||
|
Erythema (redness), Grade 3 b |
2 (1.3) |
1 (0.8) |
||||||||||
|
Systemic Adverse Reactions | ||||||||||||
|
Fatigue |
105 (67.7) |
80 (62.0) |
||||||||||
|
Fatigue, Grade 3 c |
16 (10.3) |
4 (3.1) |
||||||||||
|
Headache |
87 (56.1) |
76 (58.9) |
||||||||||
|
Headache, Grade 3 d |
8 (5.2) |
1 (0.8) |
||||||||||
|
Myalgia |
89 (57.4) |
64 (49.6) |
||||||||||
|
Myalgia, Grade 3 c |
15 (9.7) |
4 (3.1) |
||||||||||
|
Arthralgia |
66 (42.6) |
54 (41.9) |
||||||||||
|
Arthralgia, Grade 3 c |
8 (5.2) |
4 (3.1) |
||||||||||
|
Chills |
71 (45.8) |
52 (40.3) |
||||||||||
|
Chills, Grade 3 e |
1 (0.6) |
0 (0) |
||||||||||
|
Nausea/vomiting |
36 (23.2) |
16 (12.4) |
||||||||||
|
Fever |
24 (15.5) |
9 (7.0) |
||||||||||
|
Fever, Grade 3 f |
3 (1.9) |
2 (1.6) |
||||||||||
|
Rash |
5 (3.2) |
3 (2.3) |
||||||||||
|
Use of antipyretic or pain medication |
86 (55.5) |
64 (49.6) |
||||||||||
| Study 2
Second Dose of Primary Series (N=43) n (%) | Study 2
Booster Dose (N=38) n (%) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| * 7 days included day of vaccination and the subsequent 6 days. Events and use of antipyretic or pain medication were collected in the electronic diary (e-diary).
a Grade 3 pain: Defined as any use of prescription pain reliever; prevents daily activity. b Grade 3 swelling and erythema: Defined as >100 mm / >10 cm. c Grade 3 fatigue, myalgia, arthralgia: Defined as significant; prevents daily activity. d Grade 3 headache: Defined as significant; any use of prescription pain reliever or prevents daily activity. e Grade 3 fever: Defined as ≥39.0° – ≤40.0°C / ≥102.1° – ≤104.0°F. |
|||||||||||||||
|
Local Adverse Reactions | |||||||||||||||
|
Pain |
32 (74.4) |
29 (76.3) |
|||||||||||||
|
Pain, Grade 3 a |
0 (0.0) |
2 (5.3) |
|||||||||||||
|
Axillary swelling/tenderness |
2 (4.7) |
2 (5.3) |
|||||||||||||
|
Swelling (hardness) ≥25 mm |
5 (11.6) |
1 (2.6) |
|||||||||||||
|
Swelling (hardness), Grade 3 b |
1 (2.3) |
1 (2.6) |
|||||||||||||
|
Erythema (redness) ≥25 mm |
3 (7.0) |
1 (2.6) |
|||||||||||||
|
Erythema (redness), Grade 3 b |
3 (7.0) |
0 (0.0) |
|||||||||||||
|
Systemic Adverse Reactions | |||||||||||||||
|
Fatigue |
23 (53.5) |
18 (47.4) |
|||||||||||||
|
Fatigue, Grade 3 c |
2 (4.7) |
3 (7.9) |
|||||||||||||
|
Myalgia |
15 (34.9) |
18 (47.4) |
|||||||||||||
|
Myalgia, Grade 3 c |
0 (0) |
1 (2.6) |
|||||||||||||
|
Headache |
17 (39.5) |
16 (42.1) |
|||||||||||||
|
Headache, Grade 3 d |
1 (2.3) |
1 (2.6) |
|||||||||||||
|
Arthralgia |
11 (25.6) |
15 (39.5) |
|||||||||||||
|
Arthralgia, Grade 3 c |
0 (0) |
1 (2.6) |
|||||||||||||
|
Chills |
7 (16.3) |
7 (18.4) |
|||||||||||||
|
Nausea/vomiting |
5 (11.6) |
3 (7.9) |
|||||||||||||
|
Fever |
2 (4.7) |
2 (5.4) |
|||||||||||||
|
Fever, Grade 3 e |
1 (2.3) |
0 (0) |
|||||||||||||
|
Rash |
1 (2.3) |
0 (0.0) |
|||||||||||||
|
Use of antipyretic or pain medication |
11 (25.6) |
11 (28.9) |
|||||||||||||
In participants who received a booster dose, the median duration of solicited local and systemic adverse reactions was 2 to 3 days.
Unsolicited Adverse Events
Overall, the 171 participants who received a booster dose had a median follow-up time of 5.7 months after the booster dose to the cut-off date (August 16, 2021). Through the cut-off date, there were no unsolicited adverse events not already captured as solicited local and systemic reactions that were considered causally related to the Moderna COVID-19 Vaccine.
Serious Adverse Events
Of the 171 participants who received a booster dose of Moderna COVID-19 Vaccine, there were no serious adverse events reported from the booster dose through 28 days after the booster dose. Through the cut-off date of August 16, 2021, there were no serious adverse events following the booster dose considered causally related to the Moderna COVID-19 Vaccine.
Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine
The safety of a Moderna COVID-19 Vaccine (0.25 mL) booster dose in individuals who completed primary vaccination with another authorized or approved COVID-19 Vaccine (heterologous booster dose) is inferred from the safety of a Moderna COVID-19 Vaccine (0.25 mL) booster dose administered following completion of a Moderna COVID-19 Vaccine primary series (homologous booster dose) and from data from an independent Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a heterologous booster dose (0.5 mL) of the Moderna COVID-19 Vaccine. In this study, adults who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of one of three vaccines: Moderna COVID-19 Vaccine (0.5 mL), Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine. Adverse events were assessed through 28 days after the booster dose. An overall review of adverse reactions reported following the Moderna COVID-19 Vaccine heterologous booster dose (0.5 mL) did not identify any new safety concerns, as compared with adverse reactions reported following Moderna COVID-19 Vaccine primary series doses or homologous booster dose (0.25 mL).
6.2 Post-Authorization Experience
The following adverse reactions have been identified during post-authorization use of the Moderna COVID-19 Vaccine. Because these reactions are reported voluntarily, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac Disorders: myocarditis, pericarditis
Immune System Disorders: anaphylaxis
Nervous System Disorders: syncope
8 REQUIREMENTS AND INSTRUCTIONS FOR REPORTING ADVERSE EVENTS AND VACCINE ADMINISTRATION ERRORS
See Overall Safety Summary ( Section 6) for additional information.
The vaccination provider enrolled in the federal COVID-19 Vaccination Program is responsible for the MANDATORY reporting of the listed events following Moderna COVID-19 Vaccine to the Vaccine Adverse Event Reporting System (VAERS)
- Vaccine administration errors whether or not associated with an adverse event
- Serious adverse events* (irrespective of attribution to vaccination)
- Cases of Multisystem Inflammatory Syndrome (MIS) in adults
- Cases of COVID-19 that results in hospitalization or death
*Serious Adverse Events are defined as:
- Death;
- A life-threatening adverse event;
- Inpatient hospitalization or prolongation of existing hospitalization;
- A persistent or significant incapacity or substantial disruption of the ability to conduct normal life functions;
- A congenital anomaly/birth defect;
- An important medical event that based on appropriate medical judgement may jeopardize the individual and may require medical or surgical intervention to prevent one of the outcomes listed above.
Instructions for Reporting to VAERS
The vaccination provider enrolled in the federal COVID-19 Vaccination Program should complete and submit a VAERS form to FDA using one of the following methods:
- Complete and submit the report online: https://vaers.hhs.gov/reportevent.html, or
- If you are unable to submit this form electronically, you may fax it to VAERS at 1-877- 721-0366. If you need additional help submitting a report, you may call the VAERS toll- free information line at 1-800-822-7967 or send an email to info@vaers.org.
IMPORTANT: When reporting adverse events or vaccine administration errors to VAERS, please complete the entire form with detailed information. It is important that the information reported to FDA be as detailed and complete as possible. Information to include:
- Patient demographics (e.g., patient name, date of birth)
- Pertinent medical history
- Pertinent details regarding admission and course of illness
- Concomitant medications
- Timing of adverse event(s) in relationship to administration of Moderna COVID-19 Vaccine
- Pertinent laboratory and virology information
- Outcome of the event and any additional follow-up information if it is available at the time of the VAERS report. Subsequent reporting of follow-up information should be completed if additional details become available.
The following steps are highlighted to provide the necessary information for safety tracking:
- In Box 17, provide information on Moderna COVID-19 Vaccine and any other vaccines administered on the same day; and in Box 22, provide information on any other vaccines received within one month prior.
- In Box 18, description of the event:
- Write “Moderna COVID-19 Vaccine EUA” as the first line
- Provide a detailed report of vaccine administration error and/or adverse event. It is important to provide detailed information regarding the patient and adverse event/medication error for ongoing safety evaluation of this unapproved vaccine. Please see information to include listed above.
- Contact information:
- In Box 13, provide the name and contact information of the prescribing healthcare provider or institutional designee who is responsible for the report.
- In Box 14, provide the name and contact information of the best doctor/healthcare professional to contact about the adverse event.
- In Box 15, provide the address of the facility where vaccine was given (NOT the healthcare provider’s office address).
Other Reporting Instructions
Vaccination providers may report to VAERS other adverse events that are not required to be reported using the contact information above.
To the extent feasible, report adverse events to ModernaTX, Inc. using the contact information below or by providing a copy of the VAERS form to ModernaTX, Inc.
|
|
Fax number |
Telephone number |
|
ModernaPV@modernatx.com |
1-866-599-1342 |
1-866-MODERNA (1-866-663-3762) |
10 DRUG INTERACTIONS
There are no data to assess the concomitant administration of the Moderna COVID-19 Vaccine with other vaccines.
11 USE IN SPECIFIC POPULATIONS
11.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Moderna COVID-19 Vaccine during pregnancy. Women who are vaccinated with Moderna COVID-19 Vaccine during pregnancy are encouraged to enroll in the registry by calling 1-866- MODERNA (1-866-663-3762).
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Available data on Moderna COVID-19 Vaccine administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
In a developmental toxicity study, 0.2 mL of a vaccine formulation containing the same quantity of nucleoside-modified messenger ribonucleic acid (mRNA) (100 mcg) and other ingredients included in a single human dose of Moderna COVID-19 Vaccine was administered to female rats by the intramuscular route on four occasions: 28 and 14 days prior to mating, and on gestation days 1 and 13. No vaccine-related adverse effects on female fertility, fetal development, or postnatal development were reported in the study.
11.2 Lactation
Risk Summary
Data are not available to assess the effects of Moderna COVID-19 Vaccine on the breastfed infant or on milk production/excretion.
11.3 Pediatric Use
Safety and effectiveness have not been assessed in persons less than 18 years of age. Emergency Use Authorization of Moderna COVID-19 Vaccine does not include use in individuals younger than 18 years of age.
11.4 Geriatric Use
Clinical studies of Moderna COVID-19 Vaccine included participants 65 years of age and older receiving vaccine or placebo, and their data contribute to the overall assessment of safety and efficacy. In an ongoing Phase 3 clinical study (Study 1) of primary series dosing (0.5 mL), 24.8% (n=7,520) of participants were 65 years of age and older and 4.6% (n=1,399) of participants were 75 years of age and older. Vaccine efficacy in participants 65 years of age and older was 86.4% (95% CI 61.4, 95.2) compared to 95.6% (95% CI 90.6, 97.9) in participants 18 to <65 years of age [see Clinical Trial Results and Supporting Data for EUA ( 18)] . Overall, there were no notable differences in the safety profiles observed in participants 65 years of age and older and younger participants [see Overall Safety Summary ( 6.1)] .
In an ongoing Phase 2 clinical study (Study 2) of a single booster dose (0.25 mL), 22.2% (n=38) of participants were 65 years of age and older. This study did not include sufficient numbers of participants 65 years of age and older to determine whether they respond differently than younger participants. Some local and systemic adverse reactions were reported in a lower proportion of participants 65 years of age and older compared to participants 18 through 64 years of age [see Overall Safety Summary ( 6.1)] .
11.5 Use in Immunocompromised
In an independent study, safety and effectiveness of a third 0.5 mL primary series dose of the Moderna COVID-19 Vaccine have been evaluated in participants who received solid organ transplants [seeOverall Safety Summary ( 6.1) and Clinical Trial Results and Supporting Data for EUA ( 18.2)] . The administration of a third primary series vaccine dose appears to be only moderately effective in increasing antibody titers. Patients should be counseled to maintain physical precautions to help prevent COVID-19. In addition, close contacts of immunocompromised persons should be vaccinated, as appropriate for their health status.
13 DESCRIPTION
Moderna COVID-19 Vaccine is provided as a white to off-white suspension for intramuscular injection.
Each 0.5 mL dose of Moderna COVID-19 Vaccine contains 100 mcg of nucleoside-modified messenger RNA (mRNA) encoding the pre-fusion stabilized Spike glycoprotein (S) of SARS-CoV-2 virus. Each 0.5 mL dose of the Moderna COVID-19 Vaccine contains the following ingredients: a total lipid content of 1.93 mg (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), 0.31 mg tromethamine, 1.18 mg tromethamine hydrochloride, 0.043 mg acetic acid, 0.20 mg sodium acetate trihydrate, and 43.5 mg sucrose. Each 0.25 mL dose of Moderna COVID-19 Vaccine contains half of these ingredients.
Moderna COVID-19 Vaccine does not contain a preservative.
The vial stoppers are not made with natural rubber latex.
14 CLINICAL PHARMACOLOGY
14.1 Mechanism of Action
The nucleoside-modified mRNA in the Moderna COVID-19 Vaccine is formulated in lipid particles, which enable delivery of the nucleoside-modified mRNA into host cells to allow expression of the SARS-CoV-2 S antigen. The vaccine elicits an immune response to the S antigen, which protects against COVID-19.
18 CLINICAL TRIAL RESULTS AND SUPPORTING DATA FOR EUA
18.1 Efficacy of Two-Dose Primary Series
Study 1 is an ongoing Phase 3 randomized, placebo-controlled, observer-blind clinical trial to evaluate the efficacy, safety, and immunogenicity of the Moderna COVID-19 Vaccine in participants 18 years of age and older in the United States (NCT04470427). Randomization was stratified by age and health risk: 18 to <65 years of age without comorbidities (not at risk for progression to severe COVID-19), 18 to <65 years of age with comorbidities (at risk for progression to severe COVID-19), and 65 years of age and older with or without comorbidities. Participants who were immunocompromised and those with a known history of SARS-CoV-2 infection were excluded from the study. Participants with no known history of SARS-CoV-2 infection but with positive laboratory results indicative of infection at study entry were included. The study allowed for the inclusion of participants with stable pre-existing medical conditions, defined as disease not requiring significant change in therapy or hospitalization for worsening disease during the 3 months before enrollment, as well as participants with stable human immunodeficiency virus (HIV) infection. A total of 30,420 participants were randomized equally to receive 2 doses of the Moderna COVID-19 Vaccine or saline placebo 1 month apart. Participants will be followed for efficacy and safety until 24 months after the second dose.
The primary efficacy analysis population (referred to as the Per-Protocol Set) included 28,207 participants who received two doses (0.5 mL at 0 and 1 month) of either Moderna COVID-19 Vaccine (n=14,134) or placebo (n=14,073), and had a negative baseline SARS-CoV-2 status. In the Per-Protocol Set, 47.4% were female, 19.7% were Hispanic or Latino; 79.5% were White, 9.7% were African American, 4.6% were Asian, and 2.1% other races. The median age of participants was 53 years (range 18-95) and 25.3% of participants were 65 years of age and older. Of the study participants in the Per-Protocol Set, 18.5% were at increased risk of severe COVID-19 due to at least one pre-existing medical condition (chronic lung disease, significant cardiac disease, severe obesity, diabetes, liver disease, or HIV infection) regardless of age. Between participants who received Moderna COVID-19 Vaccine and those who received placebo, there were no notable differences in demographics or pre-existing medical conditions.
Efficacy Against COVID-19
COVID-19 was defined based on the following criteria: The participant must have experienced at least two of the following systemic symptoms: fever (≥38ºC / ≥100.4°F), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s); or the participant must have experienced at least one of the following respiratory signs/symptoms: cough, shortness of breath or difficulty breathing, or clinical or radiographical evidence of pneumonia; and the participant must have at least one NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS- CoV-2 by RT-PCR. COVID-19 cases were adjudicated by a Clinical Adjudication Committee.
The median length of follow-up for efficacy for participants in the study was 9 weeks post Dose 2. There were 11 COVID-19 cases in the Moderna COVID-19 Vaccine group and 185 cases in the placebo group, with a vaccine efficacy of 94.1% (95% confidence interval of 89.3% to 96.8%).
| * COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms or one respiratory symptom. Cases starting 14 days after Dose 2.
† VE and 95% CI from the stratified Cox proportional hazard model. |
||||||
|
Moderna COVID-19 Vaccine |
Placebo |
|
||||
|
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
|
|
14,134 |
11 |
3.328 |
14,073 |
185 |
56.510 |
94.1 (89.3, 96.8) |
The subgroup analyses of vaccine efficacy are presented in Table 6.
| * COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least two systemic symptoms or one respiratory symptom. Cases starting 14 days after Dose 2.
† VE and 95% CI from the stratified Cox proportional hazard model. |
||||||||||||||
|
Age Subgroup (Years) |
Moderna COVID-19 Vaccine |
Placebo |
|
|||||||||||
|
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
Participants (N) |
COVID-19 Cases (n) |
Incidence Rate of COVID-19 per 1,000 Person-Years |
|||||||||
|
18 to <65 |
10,551 |
7 |
2.875 |
10,521 |
156 |
64.625 |
95.6 (90.6, 97.9) |
|||||||
|
≥65 |
3,583 |
4 |
4.595 |
3,552 |
29 |
33.728 |
86.4 (61.4, 95.2) |
|||||||
Severe COVID-19 was defined based on confirmed COVID-19 as per the primary efficacy endpoint case definition, plus any of the following: Clinical signs indicative of severe systemic illness, respiratory rate ≥30 per minute, heart rate ≥125 beats per minute, SpO2 ≤93% on room air at sea level or PaO2/FIO2 <300 mm Hg; or respiratory failure or ARDS (defined as needing high-flow oxygen, non-invasive or mechanical ventilation, or ECMO), evidence of shock (systolic blood pressure <90 mmHg, diastolic BP <60 mmHg or requiring vasopressors); or significant acute renal, hepatic, or neurologic dysfunction; or admission to an intensive care unit or death.
Among all participants in the Per-Protocol Set analysis, which included COVID-19 cases confirmed by an adjudication committee, no cases of severe COVID-19 were reported in the Moderna COVID-19 Vaccine group compared with 30 cases reported in the placebo group (incidence rate 9.138 per 1,000 person-years). One PCR-positive case of severe COVID-19 in a vaccine recipient was awaiting adjudication at the time of the analysis.
18.2 Immunogenicity in Solid Organ Transplant Recipients
An independent randomized-controlled study has been conducted in 120 participants who had undergone various solid organ transplant procedures (heart, kidney, kidney-pancreas, liver, lung, pancreas) a median of 3.57 years previously (range 1.99-6.75 years). A third 0.5 mL primary series dose of the Moderna COVID-19 Vaccine was administered to 60 participants approximately 2 months after they had received a second dose; saline placebo was given to 60 individuals for comparison. Significant increases in levels of SARS-CoV-2 antibodies occurred four weeks after the third dose in 55.0% of participants in the Moderna COVID-19 Vaccine group (33 of 60) and 17.5% of participants in the placebo group (10 of 57).
18.3 Immunogenicity of a Booster Dose Following a Moderna COVID-19 Vaccine Primary Series
Effectiveness of a booster dose of the Moderna COVID-19 Vaccine was based on assessment of neutralizing antibody titers (ID50) against a pseudovirus expressing the SARS-CoV-2 Spike protein from a USA_WA1/2020 isolate carrying the D614G mutation. Immunogenicity analyses compared the ID50 following the booster dose to the ID50 following the primary series.
In an open-label phase of Study 2, participants 18 years of age and older received a single booster dose (0.25 mL) at least 6 months after completion of the primary series (two doses of 0.5 mL 1 month apart). The primary immunogenicity analysis population included 149 booster dose participants in Study 2 (including one individual who had only received a single dose of the primary series) and a random subset of 1,055 participants from Study 1 who received two doses (0.5 mL 1 month apart) of Moderna COVID-19 Vaccine. Study 1 and 2 participants included in the analysis population had no serologic or virologic evidence of SARS-CoV-2 infection prior to the first primary series dose and prior to the booster dose, respectively. Among participants assessed for immunogenicity, 60.4% were female, 6.7% were Hispanic or Latino; 95.3% were White, 3.4% were Black or African American, 0.7% were Asian, and 0.7% were American Indian or Alaskan Native; 9.4% were obese (body mass index ≥30 kg/m 2). The median age of Study 2 participants was 56 years of age (range 18-82) and 24.8% of participants were 65 years of age and older. Study 2 participants included in the primary immunogenicity analysis population did not have pre-existing medical conditions that would place them at risk of severe COVID-19. Study 1 participants included in the primary immunogenicity analysis population were a stratified random sample which reflected the overall primary efficacy analysis population with regards to demographics and pre-existing medical conditions with a higher percentage of those ≥65 years of age (33.6%), with risk factors for severe COVID-19 (39.4%), and communities of color (53.5%).
Immunogenicity analyses included an assessment of ID50 geometric mean titer (GMT) ratio and difference in seroresponse rates. The analysis of the GMT ratio of ID50 following the booster dose compared to the primary series met the immunobridging criteria for a booster response. Seroresponse for a participant was defined as achieving a ≥4-fold rise in ID50 from baseline (before the booster dose in Study 2 and before the first dose of the primary series in Study 1). The lower limit of the 2-sided 95% CI for the difference in seroresponse rates between Study 1 and Study 2 was -16.7%, which did not meet the immunobridging criterion for a booster response (lower limit of 2-sided 95% CI for the percentage difference of ≥ -10%). These analyses are summarized in Tables 7 and 8.
| * Per-Protocol Immunogenicity Set included all subjects who had both baseline (or Study 2 Day 1 for Study 2) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline (or Study 2 Day 1 for Study 2), did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (Day 29 for Study 2 and Day 57 for Study 1).
a Number of subjects with non-missing data at the corresponding timepoint. b Given the lack of randomization in Study 2, the statistical analysis plan pre-specified an analysis of covariance model for estimating the geometric mean titer that adjusts for differences in age groups (<65 years, ≥65 years). c Immunobridging is declared if the lower limit of the 2-sided 95% CI for the GMR is >0.67 and the point estimate of the GLSM ratio is ≥1.0. Note: Antibody values < the lower limit of quantitation (LLOQ) are replaced by 0.5 × LLOQ. Values > the upper limit of quantitation (ULOQ) are replaced by the ULOQ if actual values are not available. GLSM = Geometric least squares mean GMR = Geometric mean ratio |
|||
|
Study 2 Booster Dose N a=149 GMT b (95% CI) |
Study 1 Primary Series N a=1053 GMT b (95% CI) |
GMT Ratio (Study 2/Study 1) |
Met Success Criteria c |
|
1802 (1548, 2099) |
1027 (968, 1089) |
1.8 (1.5, 2.1) |
Lower limit of 95% CI ≥0.67 Criterion: Yes Point Estimate ≥1.0 Criterion: Yes |
| * Per-Protocol Immunogenicity Set included all subjects who had both baseline (or Study 2 Day 1 for Study 2) and post-vaccination immunogenicity samples, did not have SARS-CoV-2 infection at baseline (or Study 2 Day 1 for Study 2), did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest (Day 29 for Study 2 and Day 57 for Study 1).
a Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody titers (ID50) from baseline (pre-booster dose in Study 2 and pre-Dose 1 in Study 1), where baseline titers < LLOQ are set to LLOQ for the analysis. b Number of subjects with non-missing data at both baseline and the post-baseline timepoint of interest. c 95% CI is calculated using the Clopper-Pearson method. d 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits. e Immunobridging is declared if the lower limit of the 2-sided 95% CI for the percentage difference is > -10%. |
|||||||
|
Study 2 Booster Seroresponse a N b=149 n (%) (95% CI) c |
Study 1 Primary Series Seroresponse a N b=1050 n (%) (95% CI) c |
Difference in Seroresponse Rate (Study 2-Study 1) % (95% CI) d |
Met Success Criterion e |
||||
|
131 (87.9) (81.6, 92.7) |
1033 (98.4) (97.4, 99.1) |
-10.5 (-16.7, -6.1) |
Lower limit of 95% CI ≥-10% Criterion: No |
||||
Study 2 participants who met the ≥4-fold increase in titer post-booster dose (87.9%) had a lower baseline GMT of 109 (range of individual titers 9, 4393), whereas Study 2 participants who did not meet the ≥4-fold increase in titers post-booster had a higher baseline GMT of 492 (range of individual titers 162, 2239).
An additional descriptive analysis evaluated seroresponse rates using baseline neutralizing antibody titers prior to Dose 1 of the primary series. As shown in Table 9 below, the booster dose seroresponse rate, with seroresponse defined as at least a 4-fold rise relative to the pre-Dose 1 titer, was 100%. The difference in seroresponse rates in this post-hoc analysis was 1.6% (95% CI -0.9, 2.6).
| * Per-Protocol Immunogenicity Set included all subjects who had non-missing data at baseline (before Dose 1) and 28 days post-booster in Study 2 or 28 days post-Dose 2 in the primary series in Study 1, respectively, did not have SARS-CoV-2 infection at pre-booster in Study 2 or baseline in Study 1, did not have a major protocol deviation that impacted immune response, and had post-injection immunogenicity assessment at timepoint of primary interest.
a Seroresponse is defined as ≥4-fold rise of pseudovirus neutralizing antibody titers (ID50) from pre-Dose 1, where baseline titers < LLOQ are set to LLOQ for the analysis. b Number of subjects with non-missing data at baseline (before Dose 1) and 28 days post-booster in Study 2. c Number of subjects with non-missing data at baseline (before Dose 1) and 28 days post-Dose 2 in the primary series in Study 1. d 95% CI is calculated using the Clopper-Pearson method. e 95% CI is calculated using the Miettinen-Nurminen (score) confidence limits. |
||||||||||
|
Study 2 Booster Seroresponse a N b=148 n (%) (95% CI) d |
Study 1 Primary Series Seroresponse a N c=1050 n (%) (95% CI) d |
Difference in Seroresponse Rate (After Booster-After Primary Series) % (95% CI) e |
||||||||
|
148 (100) (97.5, 100) |
1033 (98.4) (97.4, 99.1) |
1.6 (-0.9, 2.6) |
||||||||
18.4 Immunogenicity of a Booster Dose Following Primary Vaccination with Another Authorized or Approved COVID-19 Vaccine
Effectiveness of a Moderna COVID-19 Vaccine (0.25 mL) booster dose in individuals who completed primary vaccination with another authorized or approved COVID-19 Vaccine (heterologous booster dose) is inferred from immunogenicity data supporting effectiveness of a Moderna COVID-19 Vaccine (0.25 mL) booster dose administered following completion of a Moderna COVID-19 Vaccine primary series and from immunogenicity data from an independent Phase 1/2 open-label clinical trial (NCT04889209) conducted in the United States that evaluated a heterologous booster dose (0.5 mL) of the Moderna COVID-19 Vaccine. In this study, adults who had completed primary vaccination with a Moderna COVID-19 Vaccine 2-dose series (N=151), a Janssen COVID-19 Vaccine single dose (N=156), or a Pfizer-BioNTech COVID-19 Vaccine 2-dose series (N=151) at least 12 weeks prior to enrollment and who reported no history of SARS-CoV-2 infection were randomized 1:1:1 to receive a booster dose of one of three vaccines: Moderna COVID-19 Vaccine, Janssen COVID-19 Vaccine, or Pfizer-BioNTech COVID-19 Vaccine. Neutralizing antibody titers, as measured by a pseudovirus neutralization assay using a lentivirus expressing the SARS-CoV-2 Spike protein with D614G mutation, were assessed on Day 1 prior to administration of the booster dose and on Day 15 after the booster dose. A booster response to the Moderna COVID-19 Vaccine (0.5 mL) was demonstrated regardless of primary vaccination.
19 HOW SUPPLIED/STORAGE AND HANDLING
Moderna COVID-19 Vaccine Suspension for Intramuscular Injection Multiple-Dose Vials are supplied as follows:
NDC 80777-273-99 Carton of 10 multiple-dose vials, each vial containing 5.5 mL
NDC 80777-273-98 Carton of 10 multiple-dose vials, each vial containing 7.5 mL
During storage, minimize exposure to room light.
Store frozen between -50º to -15ºC (-58º to 5ºF). Store in the original carton to protect from light.
Do not store on dry ice or below -50ºC (-58ºF). Use of dry ice may subject vials to temperatures colder than -50°C (-58°F).
Vials may be stored refrigerated between 2° to 8°C (36° to 46°F) for up to 30 days prior to first use. Do not refreeze.
Vials may be stored between 8° to 25°C (46° to 77°F) for a total of 24 hours.
After the first dose has been withdrawn, the vial should be held between 2° to 25°C (36° to 77°F). Vials should be discarded 12 hours after the first puncture.
Thawed vials can be handled in room light conditions.
Do not refreeze once thawed.
Transportation of Thawed Vials at 2° to 8°C (36° to 46°F)
If transport at -50° to -15°C (-58° to 5°F) is not feasible, available data support transportation of one or more thawed vials for up to 12 hours at 2° to 8°C (36° to 46°F) when shipped using shipping containers which have been qualified to maintain 2° to 8°C (36° to 46°F) and under routine road and air transport conditions with shaking and vibration minimized. Once thawed and transported at 2° to 8°C (36° to 46°F), vials should not be refrozen and should be stored at 2° to 8°C (36° to 46°F) until use.
20 PATIENT COUNSELING INFORMATION
Advise the recipient or caregiver to read the Fact Sheet for Recipients and Caregivers.
The vaccination provider must include vaccination information in the state/local jurisdiction’s Immunization Information System (IIS) or other designated system. Advise recipient or caregiver that more information about IISs can be found at: https://www.cdc.gov/vaccines/programs/iis/about.html.
21 CONTACT INFORMATION
For general questions, send an email or call the telephone number provided below.
|
|
Telephone number |
|
medinfo@modernatx.com |
1-866-MODERNA (1-866-663-3762) |
This EUA Prescribing Information may have been updated. For the most recent Full EUA Prescribing Information, please visit www.modernatx.com/covid19vaccine-eua.
Moderna US, Inc.
Cambridge, MA 02139
©2021 ModernaTX, Inc. All rights reserved.
Patent(s):
www.modernatx.com/patents
Revised: Nov/19/2021
FACT SHEET FOR RECIPIENTS AND CAREGIVERS
EMERGENCY USE AUTHORIZATION (EUA) OF THE MODERNA COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19) IN INDIVIDUALS 18 YEARS OF AGE AND OLDER
You are being offered the Moderna COVID-19 Vaccine to prevent Coronavirus Disease 2019 (COVID-19) caused by SARS-CoV-2. This Fact Sheet contains information to help you understand the risks and benefits of the Moderna COVID-19 Vaccine, which you may receive because there is currently a pandemic of COVID-19.
The Moderna COVID-19 Vaccine is a vaccine and may prevent you from getting COVID-19.
Read this Fact Sheet for information about the Moderna COVID-19 Vaccine. Talk to the vaccination provider if you have questions. It is your choice to receive the Moderna COVID-19 Vaccine .
The Moderna COVID-19 Vaccine has received EUA from FDA to provide:
- a two-dose primary series to individuals 18 years of age and older;
- a third primary series dose to individuals 18 years of age and older who have been determined to have certain kinds of immunocompromise;
- a single booster dose to the individuals 18 years of age and older who have completed a primary series with the Moderna COVID-19 Vaccine; and
- a single booster dose to individuals 18 years of age and older who have completed primary vaccination with a different authorized or approved COVID-19 vaccine.
The Moderna COVID-19 Vaccine may not protect everyone.
This Fact Sheet may have been updated. For the most recent Fact Sheet, please visit www.modernatx.com/covid19vaccine-eua.
WHAT YOU NEED TO KNOW BEFORE YOU GET THIS VACCINE
WHAT IS COVID-19?
COVID-19 is caused by a coronavirus called SARS-CoV-2. This type of coronavirus has not been seen before. You can get COVID-19 through contact with another person who has the virus. It is predominantly a respiratory illness that can affect other organs. People with COVID-19 have had a wide range of symptoms reported, ranging from mild symptoms to severe illness. Symptoms may appear 2 to 14 days after exposure to the virus. Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle or body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; diarrhea.
WHAT IS THE MODERNA COVID-19 VACCINE?
The Moderna COVID-19 Vaccine is an unapproved vaccine that may prevent COVID-19.
The FDA has authorized the emergency use of the Moderna COVID-19 Vaccine to prevent COVID-19 in individuals 18 years of age and older under an Emergency Use Authorization (EUA).
For more information on EUA, see the “ What is an Emergency Use Authorization (EUA)?” section at the end of this Fact Sheet.
WHAT SHOULD YOU MENTION TO YOUR VACCINATION PROVIDER BEFORE YOU GET THE MODERNA COVID-19 VACCINE?
Tell your vaccination provider about all of your medical conditions, including if you:
- have any allergies
- have had myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the lining outside the heart)
- have a fever
- have a bleeding disorder or are on a blood thinner
- are immunocompromised or are on a medicine that affects your immune system
- are pregnant or plan to become pregnant
- are breastfeeding
- have received another COVID-19 vaccine
- have ever fainted in association with an injection
WHO SHOULD GET THE MODERNA COVID-19 VACCINE?
FDA has authorized the emergency use of the Moderna COVID-19 Vaccine in individuals 18 years of age and older.
WHO SHOULD NOT GET THE MODERNA COVID-19 VACCINE?
You should not get the Moderna COVID-19 Vaccine if you:
- had a severe allergic reaction after a previous dose of this vaccine
- had a severe allergic reaction to any ingredient of this vaccine
WHAT ARE THE INGREDIENTS IN THE MODERNA COVID-19 VACCINE?
The Moderna COVID-19 Vaccine contains the following ingredients: messenger ribonucleic acid (mRNA), lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), tromethamine, tromethamine hydrochloride, acetic acid, sodium acetate trihydrate, and sucrose.
HOW IS THE MODERNA COVID-19 VACCINE GIVEN?
The Moderna COVID-19 Vaccine will be given to you as an injection into the muscle.
Primary Series: The Moderna COVID-19 Vaccine is administered as a 2-dose series, one month apart. A third primary series dose may be administered at least one month after the second dose to individuals who are determined to have certain kinds of immunocompromise.
Booster Dose:
- A single booster dose of the Moderna COVID-19 Vaccine may be administered at least 6 months after completion of a primary series.
- A single booster dose of the Moderna COVID-19 Vaccine may be administered to individuals 18 years of age and older who have completed primary vaccination with a different authorized or approved COVID-19 vaccine. Please check with your healthcare provider regarding timing of the booster dose.
HAS THE MODERNA COVID-19 VACCINE BEEN USED BEFORE?
The Moderna COVID-19 Vaccine is an unapproved vaccine. In clinical trials, approximately 15,400 individuals 18 years of age and older have received at least 1 dose of the Moderna COVID-19 Vaccine. Millions of individuals have received the vaccine under EUA since December 18, 2020.
WHAT ARE THE BENEFITS OF THE MODERNA COVID-19 VACCINE?
In an ongoing clinical trial, the Moderna COVID-19 Vaccine has been shown to prevent COVID-19 following 2 doses given 1 month apart. The duration of protection against COVID-19 is currently unknown.
WHAT ARE THE RISKS OF THE MODERNA COVID-19 VACCINE ?
There is a remote chance that the Moderna COVID-19 Vaccine could cause a severe allergic reaction. A severe allergic reaction would usually occur within a few minutes to one hour after getting a dose of the Moderna COVID-19 Vaccine. For this reason, your vaccination provider may ask you to stay at the place where you received your vaccine for monitoring after vaccination. Signs of a severe allergic reaction can include:
- Difficulty breathing
- Swelling of your face and throat
- A fast heartbeat
- A bad rash all over your body
- Dizziness and weakness
Myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining outside the heart) have occurred in some people who have received the Moderna COVID-19 Vaccine, more commonly in males under 40 years of age than among females and older males. In most of these people, symptoms began within a few days following receipt of the second dose of the Moderna COVID-19 Vaccine. The chance of having this occur is very low. You should seek medical attention right away if you have any of the following symptoms after receiving the Moderna COVID-19 Vaccine:
- Chest pain
- Shortness of breath
- Feelings of having a fast-beating, fluttering, or pounding heart
Side effects that have been reported in clinical trials with the Moderna COVID-19 Vaccine include:
- Injection site reactions: pain, tenderness and swelling of the lymph nodes in the same arm of the injection, swelling (hardness), and redness
- General side effects: fatigue, headache, muscle pain, joint pain, chills, nausea and vomiting, fever, and rash
Side effects that have been reported during post-authorization use of the Moderna COVID-19 Vaccine include:
- Severe allergic reactions
- Myocarditis (inflammation of the heart muscle)
- Pericarditis (inflammation of the lining outside the heart)
- Fainting in association with injection of the vaccine
These may not be all the possible side effects of the Moderna COVID-19 Vaccine. Serious and unexpected side effects may occur. The Moderna COVID-19 Vaccine is still being studied in clinical trials.
WHAT SHOULD I DO ABOUT SIDE EFFECTS?
If you experience a severe allergic reaction, call 9-1-1, or go to the nearest hospital.
Call the vaccination provider or your healthcare provider if you have any side effects that bother you or do not go away.
Report vaccine side effects to FDA/CDC Vaccine Adverse Event Reporting System (VAERS). The VAERS toll-free number is 1-800-822-7967 or report online to https://vaers.hhs.gov/reportevent.html. Please include “Moderna COVID-19 Vaccine EUA” in the first line of box #18 of the report form.
In addition, you can report side effects to ModernaTX, Inc. at 1-866-MODERNA (1-866-663-3762).
You may also be given an option to enroll in v-safe. V-safe is a new voluntary smartphone-based tool that uses text messaging and web surveys to check in with people who have been vaccinated to identify potential side effects after COVID-19 vaccination. V-safe asks questions that help CDC monitor the safety of COVID-19 vaccines. V-safe also provides second-dose reminders if needed and live telephone follow-up by CDC if participants report a significant health impact following COVID-19 vaccination. For more information on how to sign up, visit: www.cdc.gov/vsafe.
WHAT IF I DECIDE NOT TO GET THE MODERNA COVID-19 VACCINE?
It is your choice to receive or not receive the Moderna COVID-19 Vaccine. Should you decide not to receive it, it will not change your standard medical care.
ARE OTHER CHOICES AVAILABLE FOR PREVENTING COVID-19 BESIDES MODERNA COVID-19 VACCINE?
Another choice for preventing COVID-19 is Comirnaty, an FDA-approved COVID-19 vaccine. Other vaccines to prevent COVID-19 may be available under Emergency Use Authorization.
CAN I RECEIVE THE MODERNA COVID-19 VACCINE AT THE SAME TIME AS OTHER VACCINES?
Data have not yet been submitted to FDA on administration of Moderna COVID-19 Vaccine at the same time as other vaccines. If you are considering receiving Moderna COVID-19 Vaccine with other vaccines, discuss your options with your healthcare provider.
WHAT IF I AM IMMUNOCOMPROMISED?
If you are immunocompromised, you may receive a third primary series dose of the Moderna COVID-19 Vaccine. The third dose may still not provide full immunity to COVID-19 in people who are immunocompromised, and you should continue to maintain physical precautions to help prevent COVID-19. In addition, your close contacts should be vaccinated as appropriate.
WHAT IF I AM PREGNANT OR BREASTFEEDING?
If you are pregnant or breastfeeding, discuss your options with your healthcare provider.
WILL THE MODERNA COVID-19 VACCINE GIVE ME COVID-19?
No. The Moderna COVID-19 Vaccine does not contain SARS-CoV-2 and cannot give you COVID-19.
KEEP YOUR VACCINATION CARD
When you receive your first dose, you will get a vaccination card to show you when to return for your second dose of the Moderna COVID-19 Vaccine. Remember to bring your card when you return.
ADDITIONAL INFORMATION
If you have questions, visit the website or call the telephone number provided below.
To access the most recent Fact Sheets, please scan the QR code provided below.
|
Moderna COVID-19 Vaccine website |
Telephone number |
|
www.modernatx.com/covid19vaccine-eua 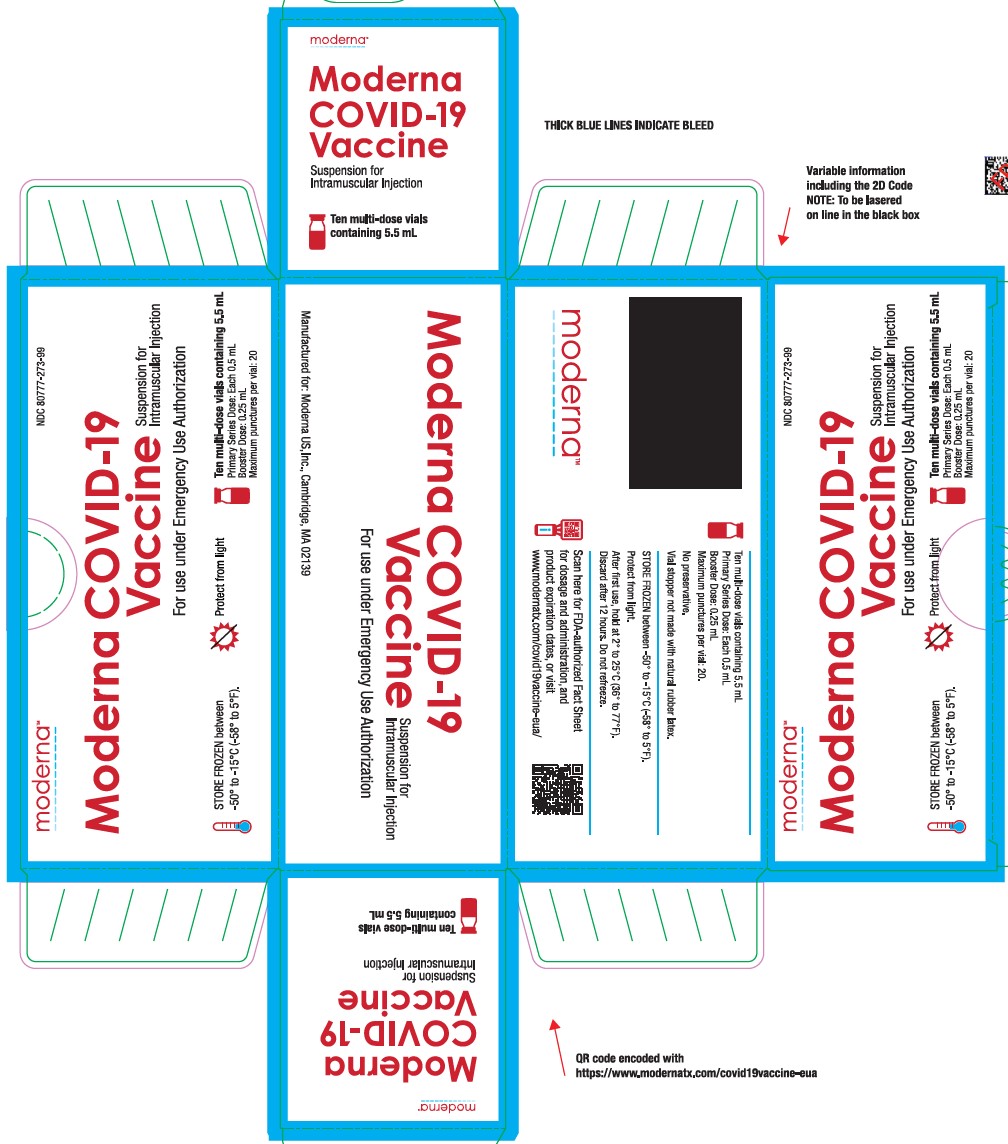 |
1-866-MODERNA (1-866-663-3762) |
HOW CAN I LEARN MORE?
- Ask the vaccination provider
- Visit CDC at https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Visit FDA at https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization
- Contact your state or local public health department
WHERE WILL MY VACCINATION INFORMATION BE RECORDED?
The vaccination provider may include your vaccination information in your state/local jurisdiction’s Immunization Information System (IIS) or other designated system. This will ensure that you receive the same vaccine when you return for the second dose. For more information about IISs, visit: https://www.cdc.gov/vaccines/programs/iis/about.html.
CAN I BE CHARGED AN ADMINISTRATION FEE FOR RECEIPT OF THE COVID-19 VACCINE?
No. At this time, the provider cannot charge you for a vaccine dose and you cannot be charged an out-of-pocket vaccine administration fee or any other fee if only receiving a COVID-19 vaccination. However, vaccination providers may seek appropriate reimbursement from a program or plan that covers COVID-19 vaccine administration fees for the vaccine recipient (private insurance, Medicare, Medicaid, HRSA COVID-19 Uninsured Program for non-insured recipients).
WHERE CAN I REPORT CASES OF SUSPECTED FRAUD?
Individuals becoming aware of any potential violations of the CDC COVID-19 Vaccination Program requirements are encouraged to report them to the Office of the Inspector General, U.S. Department of Health and Human Services, at 1-800-HHS-TIPS or TIPS.HHS.GOV.
WHAT IS THE COUNTERMEASURES INJURY COMPENSATION PROGRAM?
The Countermeasures Injury Compensation Program (CICP) is a federal program that may help pay for costs of medical care and other specific expenses of certain people who have been seriously injured by certain medicines or vaccines, including this vaccine. Generally, a claim must be submitted to the CICP within one (1) year from the date of receiving the vaccine. To learn more about this program, visit www.hrsa.gov/cicp/ or call 1-855-266-2427.
WHAT IS AN EMERGENCY USE AUTHORIZATION (EUA)?
The United States FDA has made the Moderna COVID-19 Vaccine available under an emergency access mechanism called an EUA. The EUA is supported by a Secretary of Health and Human Services (HHS) declaration that circumstances exist to justify the emergency use of drugs and biological products during the COVID-19 pandemic.
The Moderna COVID-19 Vaccine has not undergone the same type of review as an FDA- approved or cleared product. FDA may issue an EUA when certain criteria are met, which includes that there are no adequate, approved, and available alternatives. In addition, the FDA decision is based on the totality of the scientific evidence available showing that the product may be effective to prevent COVID-19 during the COVID-19 pandemic and that the known and potential benefits of the product outweigh the known and potential risks of the product. All of these criteria must be met to allow for the product to be used during the COVID-19 pandemic.
The EUA for the Moderna COVID-19 Vaccine is in effect for the duration of the COVID-19 EUA declaration justifying emergency use of these products, unless terminated or revoked (after which the products may no longer be used).
Moderna US, Inc.
Cambridge, MA 02139
©2021 ModernaTX, Inc. All rights reserved.
Patent(s):
www.modernatx.com/patents
Revised: Nov/19/2021
Package/Label Display Panel
NDC 80777-273-10
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
5.5 mL Multi-Dose Vial
Primary dose: 0.5 mL
Booster dose: 0.25 mL
Maximum punctures per vial: 20
Package/Label Display Panel
NDC 80777-273-99
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
STORE FROZEN between -50° to -15°C (-58° to 5°F).
Protect from light
Ten multi-dose vials containing 5.5 mL
Primary Series Dose: Each 0.5 mL
Booster Dose: 0.25 mL
Maximum punctures per vial: 20
Package/Label Display Panel
NDC 80777-273-15
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
7.5 mL Multi-Dose Vial
Primary dose: 0.5 mL
Booster dose: 0.25 mL
Maximum punctures per vial: 20
Package/Label Display Panel
NDC 80777-273-98
Moderna COVID-19 Vaccine
Suspension for Intramuscular Injection
For use under Emergency Use Authorization
STORE FROZEN between -50° to -15°C (-58° to 5°F).
Protect from light
Ten multi-dose vials containing 7.5 mL
Primary Series Dose: Each 0.5 mL
Booster Dose: 0.25 mL
Maximum punctures per vial: 20
| MODERNA COVID-19 VACCINE
cx-024414 injection, suspension |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Moderna US, Inc. (117626450) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Lonza Biologics, Inc. | 093149750 | analysis(80777-273) , api manufacture(80777-273) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| ModernaTX, Inc. | 116912313 | analysis(80777-273) , api manufacture(80777-273) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Catalent Indiana, LLC | 172209277 | manufacture(80777-273) , label(80777-273) , pack(80777-273) | |