NEXIUM I.V.- esomeprazole sodium injection
Cardinal Health
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use NEXIUM I.V. safely and effectively. See full prescribing information for NEXIUM I.V.
NEXIUM® I.V. (esomeprazole sodium) for Injection, for intravenous use Initial U.S. Approval: 2005 RECENT MAJOR CHANGESDosage and Administration, GERD, with EE (2.1) 04/2011 Dosage and Administration, Preparations for Use (2.2) 04/2011 Warnings and Precautions, Hypomagnesemia (5.4) 06/2011 St John's Wort or Rifampin (5.5) 06/2011 Warnings and Precautions, Interactions with Investigations for Neuroendocrine Tumors (5.6) 06/2011 Warnings and Precautions, Concomitant use of NEXIUM with Methotrexate (5.7) 01/2012 INDICATIONS AND USAGENEXIUM I.V. is a proton pump inhibitor indicated for the treatment of Gastroesophageal Reflux Disease (GERD) with erosive esophagitis (EE) in adults and pediatric patients greater than one month of age, when oral therapy is not possible or appropriate. (1.1) (1) DOSAGE AND ADMINISTRATIONGERD –with Erosive Esophagitis (2) • Adults: Dose is either 20 mg or 40 mg esomeprazole given once daily by intravenous injection (no less than 3 minutes) or intravenous infusion (10 minutes to 30 minutes). (2.1) (2) • Pediatric: Give the following doses once daily as an intravenous infusion over 10 minutes to 30 minutes. (2)
DOSAGE FORMS AND STRENGTHSNEXIUM I.V. for Injection is supplied as a freeze-dried powder containing 20 mg or 40 mg of esomeprazole per single-use vial. (3) (3) CONTRAINDICATIONSPatients with known hypersensitivity to any component of the formulation or to substituted benzimidazoles (angioedema and anaphylaxis have occurred). (4) (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (>1%): (6)
To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6) DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 7/2018 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Treatment of Gastroesophageal Reflux Disease (GERD) with Erosive Esophagitis
NEXIUM I.V. for Injection is indicated for the short-term treatment of GERD with erosive esophagitis in adults and pediatric patients 1 month to 17 years, inclusively as an alternative to oral therapy when oral NEXIUM is not possible or appropriate.
2 DOSAGE AND ADMINISTRATION
NEXIUM I.V. for Injection should not be administered concomitantly with any other medications through the same intravenous site and or tubing. The intravenous line should always be flushed with either 0.9% Sodium Chloride Injection, USP, Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP both prior to and after administration of NEXIUM I.V. for Injection.
The admixture should be stored at room temperature up to 30°C (86°F) and should be administered within the designated time period as listed in the Table 1 below. No refrigeration is required.
Table 1
| Diluent | Administer within: |
|---|---|
|
0.9% Sodium Chloride Injection, USP |
12 hours |
|
Lactated Ringer’s Injection, USP |
12 hours |
|
5% Dextrose Injection, USP |
6 hours |
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
As soon as oral therapy is possible or appropriate, intravenous therapy with NEXIUM I.V. for Injection should be discontinued and the therapy should be continued orally.
Special Populations
Hepatic Insufficiency: No dosage adjustment is necessary in patients with mild to moderate liver impairment (Child Pugh Classes A and B). For patients with severe liver impairment (Child Pugh Class C), a dose of 20 mg of NEXIUM should not be exceeded [see Use in Specific Populations (8.6) and Clinical Pharmacology, Pharmacokinetics (12.3)].
2.1 GERD with Erosive Esophagitis
Adults
The recommended adult dose is either 20 mg or 40 mg esomeprazole given once daily by intravenous injection (no less than 3 minutes) or intravenous infusion (10 minutes to 30 minutes).
Safety and efficacy of NEXIUM I.V. for Injection as a treatment of GERD patients with erosive esophagitis for more than 10 days have not been demonstrated.
Pediatric
The recommended doses for children ages 1 month to 17 years, inclusive, are provided below. Dose should be infused over 10 minutes to 30 minutes.
1 year to 17 years:
Body weight less than 55 kg: 10 mg
Body weight 55 kg or greater: 20 mg
1 month to less than 1 year of age: 0.5 mg/kg
2.2 Preparations for Use and Administration
Adults
Intravenous Injection (20 mg or 40 mg vial) over no less than 3 minutes
The freeze-dried powder should be reconstituted with 5 mL of 0.9% Sodium Chloride Injection, USP. Withdraw 5 mL of the reconstituted solution and administer an intravenous injection over no less than 3 minutes.
Intravenous Infusion (20 mg or 40 mg) over 10 minutes to 30 minutes
A solution for intravenous infusion is prepared by first reconstituting the contents of one vial with 5 mL of 0.9% Sodium Chloride Injection, USP, Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP and further diluting the resulting solution to a final volume of 50 mL. The solution (admixture) should be administered as an intravenous infusion over a period of 10 minutes to 30 minutes.
The reconstituted solution should be stored at room temperature up to 30°C (86°F) and administered within 12 hours after reconstitution. No refrigeration is required.
Pediatric Population
Intravenous Infusion over 10 minutes to 30 minutes (0.5 mg/kg) for patients ages 1 month to less than 1 year of age
A solution for intravenous infusion is prepared by first reconstituting the contents of one vial with 5 mL of 0.9% Sodium Chloride Injection, USP and further diluting the resulting solution to a final volume of 50 mL. The resultant concentration after diluting to a final volume of 50 mL is as follows:
40 mg vial: 0.8 mg/mL
20 mg vial: 0.4 mg/mL
Withdraw appropriate amount of volume for desired dose (0.5 mg/kg) and administer as an intravenous infusion over 10 minutes to 30 minutes
Intravenous Infusion (10 mg and 20 mg) over 10 minutes to 30 minutes for Pediatric Patients, ages 1 year to 17 years of age
40 mg vial
A solution for intravenous infusion is prepared by first reconstituting the contents of one vial with 5 mL of 0.9% Sodium Chloride Injection, USP and further diluting the resulting solution to a final volume of 50 ml. The resultant concentration after diluting to a final volume of 50 mL is 0.8 mg/mL.
20 mg dose: Withdraw 25 mL of the final solution and administer as an intravenous infusion over 10 minutes to 30 minutes
10 mg dose: Withdraw 12.5 mL of the final solution and administer as an intravenous infusion over 10 minutes to 30 minutes
20 mg vial
A solution for intravenous infusion is prepared by first reconstituting the contents of one vial with 5 mL of 0.9% Sodium Chloride Injection, USP and further diluting the resulting solution to a final volume of 50 mL The resultant concentration after diluting to a final volume of 50 mL is 0.4 mg/mL.
20 mg dose: Administer the final solution (50 mL) as an intravenous infusion over 10 minutes to 30 minutes
10 mg dose: Withdraw 25 mL of the final solution and administer as an intravenous infusion over 10 minutes to 30 minutes
3 DOSAGE FORMS AND STRENGTHS
NEXIUM I.V. for Injection is supplied as a freeze-dried white to off-white powder containing 20 mg or 40 mg of esomeprazole per single-use vial.
4 CONTRAINDICATIONS
Patients with known hypersensitivity to any component of the formulation or to substituted benzimidazoles (angioedema and anaphylaxis have occurred).
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Concomitant Gastric Malignancy
Symptomatic response to therapy with NEXIUM does not preclude the presence of gastric malignancy.
5.2 Atrophic Gastritis
Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with omeprazole, of which esomeprazole is an enantiomer.
5.3 Bone Fracture
Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines. [see Dosage and Administration (2) and Adverse Reactions (6.3)]
5.4 Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically. [See Adverse Reactions (6.3)]
5.5 Concomitant use of NEXIUM with St John’s Wort or Rifampin
Drugs which induce CYP2C19 or CYP3A4 (such as St John’s Wort or rifampin) can substantially decrease esomeprazole concentrations [see Drug Interactions (7)]. Avoid concomitant use of NEXIUM with St John’s Wort or rifampin.
5.6 Interactions with Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Providers should temporarily stop esomeprazole treatment before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g. for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary.
5.7 Concomitant use of NEXIUM with Methotrexate
Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration a temporary withdrawal of the PPI may be considered in some patients. [see Drug Interactions (7.3)]
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience with Intravenous NEXIUM
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
The safety of intravenous esomeprazole is based on results from clinical trials conducted in three different populations including patients having symptomatic GERD with or without a history of erosive esophagitis (n=199), patients with erosive esophagitis (n=160), and healthy subjects (n=204). Adverse experiences occurring in >1% of patients treated with intravenous esomeprazole (n=359) in trials are listed below by body system:
Symptomatic GERD and Erosive Esophagitis Trials
The data described below reflect exposure to NEXIUM I.V for Injection in 359 patients. NEXIUM I.V. for Injection was studied only in actively-controlled trials. The population was 18 to 77 years of age; 45% Male, 52% Caucasian, 17% Black, 3% Asian, 28% Other, and had either erosive reflux esophagitis (44%) or GERD (56%). Most patients received doses of either 20 or 40 mg either as an infusion or an injection.
Table 2
| Adverse Reactions | % of patients
Esomeprazole Intravenous (n=359) |
|---|---|
|
Headache |
10.9 |
|
Flatulence |
10.3 |
|
Nausea |
6.4 |
|
Abdominal pain |
5.8 |
|
Diarrhea |
3.9 |
|
Mouth dry |
3.9 |
|
Dizziness/vertigo |
2.8 |
|
Constipation |
2.5 |
|
Injection site reaction |
1.7 |
|
Pruritus |
1.1 |
Intravenous treatment with esomeprazole 20 and 40 mg administered as an injection or as an infusion was found to have a safety profile similar to that of oral administration of esomeprazole.
Pediatric
In a randomized, open-label, multi-national study to evaluate the pharmacokinetics of repeated intravenous doses of once daily esomeprazole, esomeprazole was well tolerated in pediatric patients 1 month to 17 years old, inclusive. The safety results are consistent with the known safety profile of esomeprazole and no unexpected safety signals were identified. [See Clinical Pharmacology (12.3)]
6.2 Clinical Trials Experience with Oral NEXIUM
Adult
The safety of oral NEXIUM was evaluated in over 15,000 patients (aged 18 to 84 years) in clinical trials worldwide including over 8,500 patients in the United States and over 6,500 patients in Europe and Canada. Over 2,900 patients were treated in long-term studies for up to 6-12 months. In general, NEXIUM was well tolerated in both short and long-term clinical trials.
The safety in the treatment of healing of erosive esophagitis was assessed in four randomized comparative clinical trials, which included 1,240 patients on NEXIUM 20 mg, 2,434 patients on NEXIUM 40 mg, and 3,008 patients on omeprazole 20 mg daily. The most frequently occurring adverse events (≥1%) in all three groups were headache (5.5, 5.0, and 3.8, respectively) and diarrhea (no difference among the three groups). Nausea, flatulence, abdominal pain, constipation, and dry mouth occurred at similar rates among patients taking NEXIUM or omeprazole.
Additional adverse events that were reported as possibly or probably related to NEXIUM with an incidence <1% are listed below by body system:
Body as a Whole: abdomen enlarged, allergic reaction, asthenia, back pain, chest pain, chest pain substernal, facial edema, peripheral edema, hot flushes, fatigue, fever, flu-like disorder, generalized edema, leg edema, malaise, pain, rigors;Cardiovascular: flushing, hypertension, tachycardia; Endocrine: goiter; Gastrointestinal: bowel irregularity, constipation aggravated, dyspepsia, dysphagia, dysplasia GI, epigastric pain, eructation, esophageal disorder, frequent stools, gastroenteritis, GI hemorrhage, GI symptoms not otherwise specified, hiccup, melena, mouth disorder, pharynx disorder, rectal disorder, serum gastrin increased, tongue disorder, tongue edema, ulcerative stomatitis, vomiting; Hearing: earache, tinnitus; Hematologic: anemia, anemia hypochromic, cervical lymphadenopathy, epistaxis, leukocytosis, leukopenia, thrombocytopenia; Hepatic: bilirubinemia, hepatic function abnormal, SGOT increased, SGPT increased; Metabolic/Nutritional: glycosuria, hyperuricemia, hyponatremia, increased alkaline phosphatase, thirst, vitamin B12 deficiency, weight increase, weight decrease; Musculoskeletal: arthralgia, arthritis aggravated, arthropathy, cramps, fibromyalgia syndrome, hernia, polymyalgia rheumatica; Nervous System/Psychiatric: anorexia, apathy, appetite increased, confusion, depression aggravated, dizziness, hypertonia, nervousness, hypoesthesia, impotence, insomnia, migraine, migraine aggravated, paresthesia, sleep disorder, somnolence, tremor, vertigo, visual field defect; Reproductive: dysmenorrhea, menstrual disorder, vaginitis; Respiratory: asthma aggravated, coughing, dyspnea, larynx edema, pharyngitis, rhinitis, sinusitis; Skin and Appendages: acne, angioedema, dermatitis, pruritus, pruritus ani, rash, rash erythematous, rash maculo-papular, skin inflammation, sweating increased, urticaria; Special Senses: otitis media, parosmia, taste loss, taste perversion; Urogenital: abnormal urine, albuminuria, cystitis, dysuria, fungal infection, hematuria, micturition frequency, moniliasis, genital moniliasis, polyuria; Visual: conjunctivitis, vision abnormal.
Endoscopic findings that were reported as adverse events include: duodenitis, esophagitis, esophageal stricture, esophageal ulceration, esophageal varices, gastric ulcer, gastritis, hernia, benign polyps or nodules, Barrett’s esophagus, and mucosal discoloration.
The incidence of treatment-related adverse events during 6- month maintenance treatment was similar to placebo. There were no differences in types of related adverse events seen during maintenance treatment up to 12 months compared to short-term treatment.
Two placebo-controlled studies were conducted in 710 patients for the treatment of symptomatic gastroesophageal reflux disease. The most common adverse events that were reported as possibly or probably related to NEXIUM were diarrhea (4.3%), headache (3.8%), and abdominal pain (3.8%).
The following potentially clinically significant laboratory changes in clinical trials, irrespective of relationship to NEXIUM, were reported in ≤ 1% of patients: increased creatinine, uric acid, total bilirubin, alkaline phosphatase, ALT, AST, hemoglobin, white blood cell count, platelets, serum gastrin, potassium, sodium, thyroxine and thyroid stimulating hormone [see Clinical Pharmacology, Endocrine Effects (12.2) for further information on thyroid effects]. Decreases were seen in hemoglobin, white blood cell count,platelets, potassium, sodium, and thyroxine.
Pediatric
The safety of oral NEXIUM was evaluated in 316 pediatric and adolescent patients aged 1 to 17 years in four clinical trials for the treatment of symptomatic GERD [see Clinical Studies (14.2) ]. In 109 pediatric patients aged 1 to 11 years, the most frequently reported (at least 1%) treatment-related adverse reactions in these patients were diarrhea (2.8%), headache (1.9%) and somnolence (1.9%). In 149 pediatric patients aged 12 to 17 years the most frequently reported (at least 2%) treatment-related adverse reactions in these patients were headache (8.1%), abdominal pain (2.7%), diarrhea (2%), and nausea (2%). No new safety concerns were identified in pediatric patients.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of NEXIUM. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Postmarketing Reports - There have been spontaneous reports of adverse events with postmarketing use of esomeprazole. These reports occurred rarely and are listed below by body system:
Blood And Lymphatic System Disorders: agranulocytosis, pancytopenia; Eye Disorders: blurred vision; Gastrointestinal Disorders: pancreatitis; stomatitis; microscopic colitis; Hepatobiliary Disorders: hepatic failure, hepatitis with or without jaundice; Immune System Disorders: anaphylactic reaction/shock; Infections and Infestations: GI candidiasis; Metabolism and nutritional disorders: hypomagnesemia; Musculoskeletal And Connective Tissue Disorders: muscular weakness, myalgia, bone fracture; Nervous System Disorders: hepatic encephalopathy, taste disturbance; Psychiatric Disorders: aggression, agitation, depression, hallucination; Renal and Urinary Disorders: interstitial nephritis; Reproductive System and Breast Disorders: gynecomastia; Respiratory, Thoracic and Mediastinal Disorders: bronchospasm; Skin and Subcutaneous Tissue Disorders: alopecia, erythema multiforme, hyperhidrosis, photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis (TEN, some fatal).
Other adverse events not observed with NEXIUM, but occurring with omeprazole can be found in the omeprazole package insert, ADVERSE REACTIONS section.
7 DRUG INTERACTIONS
Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4.
In vitro and in vivo studies have shown that esomeprazole is not likely to inhibit CYPs 1A2, 2A6, 2C9, 2D6, 2E1 and 3A4. No clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Drug interaction studies have shown that esomeprazole does not have any clinically significant interactions with phenytoin, warfarin, quinidine, clarithromycin or amoxicillin. Post-marketing reports of changes in prothrombin measures have been received among patients on concomitant warfarin and esomeprazole therapy. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Esomeprazole may potentially interfere with CYP2C19, the major esomeprazole metabolizing enzyme. Coadministration of esomeprazole 30 mg and diazepam, a CYP2C19 substrate, resulted in a 45% decrease in clearance of diazepam. Increased plasma levels of diazepam were observed 12 hours after dosing and onwards. However, at that time, the plasma levels of diazepam were below the therapeutic interval, and thus this interaction is unlikely to be of clinical relevance.
Omeprazole acts as an inhibitor of CYP 2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in cross-over study, increased Cmax and AUC of cilostazol by 18% and 26%, respectively. Cmax and AUC of one of its active metabolites, 3,4-dihydro-cilostazol, which has 4-7 times the activity of cilostazol, were increased by 29% and 69%, respectively. Co-administration of cilostazol with esomeprazole is expected to increase concentrations of cilostazol and its above mentioned active metabolite. Therefore, a dose reduction of cilostazol from 100 mg twice daily to 50 mg twice daily should be considered.
Concomitant administration of esomeprazole and a combined inhibitor of CYP2C19 and CYP3A4, such as voriconazole, may result in more than doubling of the esomeprazole exposure. Dose adjustment of esomeprazole is not normally required for the recommended doses. However, in patients who may require higher doses, dose adjustment may be considered.
Drugs known to induce CYP2C19 or CYP3A4 (such as rifampin) may lead to decreased esomeprazole serum levels. Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with St. John’s wort, an inducer of CYP3A4. In a cross-over study in 12 healthy male subjects, St John’s wort (300 mg three times daily for 14 days) significantly decreased the systemic exposure of omeprazole in CYP2C19 poor metabolizers (Cmax and AUC decreased by 37.5% and 37.9%, respectively) and extensive metabolizers (Cmax and AUC decreased by 49.6% and 43.9%, respectively). Avoid concomitant use of St. John’s Wort or rifampin with NEXIUM.
Coadministration of oral contraceptives, diazepam, phenytoin, or quinidine did not seem to change the pharmacokinetic profile of esomeprazole.
Concomitant use of atazanavir and proton pump inhibitors is not recommended. Co-administration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and thereby reduce its therapeutic effect.
Omeprazole has been reported to interact with some antiretroviral drugs. The clinical importance and the mechanisms behind these interactions are not always known. Increased gastric pH during omeprazole treatment may change the absorption of the antiretroviral drug. Other possible interaction mechanisms are via CYP2C19. For some antiretroviral drugs, such as atazanavir and nelfinavir, decreased serum levels have been reported when given together with omeprazole. Following multiple doses of nelfinavir (1250 mg, twice daily) and omeprazole (40 mg daily), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75%, respectively, for nelfinavir and M8. Following multiple doses of atazanavir (400 mg daily) and omeprazole (40 mg daily, 2 hr before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95%. Concomitant administration with omeprazole and drugs such as atazanavir and nelfinavir is therefore not recommended. For other antiretroviral drugs, such as saquinavir, elevated serum levels have been reported with an increase in AUC by 82%, in Cmax by 75% and in Cmin by 106% following multiple dosing of saquinavir/ritonavir (1000/100 mg) twice daily for 15 days with omeprazole 40 mg daily co-administered days 11 to 15. Dose reduction of saquinavir should be considered from the safety perspective for individual patients. There are also some antiretroviral drugs of which unchanged serum levels have been reported when given with omeprazole.
Studies evaluating concomitant administration of esomeprazole and either naproxen (non-selective NSAID) or rofecoxib (COX-2 selective NSAID) did not identify any clinically relevant changes in the pharmacokinetic profiles of esomeprazole or these NSAIDs.
Esomeprazole inhibits gastric acid secretion. Therefore, esomeprazole may interfere with the absorption of drugs where gastric pH is an important determinant of bioavailability. Like with other drugs that decrease the intragastric acidity, the absorption of drugs such as ketoconazole, atazanavir, iron salts, and erlotinib can decrease, while the absorption of drugs such as digoxin can increase during treatment with esomeprazole. Concomitant treatment with omeprazole (20 mg daily) and digoxin in healthy subjects increased the bioavailability of digoxin by 10% (30% in two subjects). Esomeprazole is an enantiomer of omeprazole. Coadministration of digoxin with esomeprazole is expected to increase the systemic exposure of digoxin. Therefore, patients may need to be monitored when digoxin is taken concomitantly with esomeprazole.
7.1 Interactions with Investigations of Neuroendocrine Tumors
Drug-induced decrease in gastric acidity results in enterochromaffin-like cell hyperplasia and increased Chromogranin A levels which may interfere with investigations for neuroendocrine tumors [see Warnings and Precautions (5.5) and Clinical Pharmacology (12.2)].
7.2 Tacrolimus
Concomitant administration of esomeprazole and tacrolimus may increase the serum levels of tacrolimus.
7.3 Methotrexate
Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of methotrexate with PPIs have been conducted [see Warnings and Precautions (5.7)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects. Pregnancy Category B
Teratology studies have been performed in rats at oral doses up to 280 mg/kg/day (about 57 times the human dose on a body surface area basis) and in rabbits at oral doses up to 86 mg/kg/day (about 35 times the human dose on a body surface area basis) and have revealed no evidence of impaired fertility or harm to the fetus due to esomeprazole. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Teratology studies conducted with omeprazole in rats at oral doses up to 138 mg/kg/day (about 56 times the human dose on a body surface area basis) and in rabbits at doses up to 69 mg/kg/day (about 56 times the human dose on a body surface area basis) did not disclose any evidence for a teratogenic potential of omeprazole. In rabbits, omeprazole in a dose range of 6.9 to 69.1 mg/kg/day (about 5.5 to 56 times the human dose on a body surface area basis) produced dose-related increases in embryo-lethality, fetal resorptions, and pregnancy disruptions. In rats, dose-related embryo/fetal toxicity and postnatal developmental toxicity were observed in offspring resulting from parents treated with omeprazole at 13.8 to 138 mg/kg/day (about 5.6 to 56 times the human doses on a body surface area basis). There are no adequate and well-controlled studies in pregnant women. Sporadic reports have been received of congenital abnormalities occurring in infants born to women who have received omeprazole during pregnancy.
8.3 Nursing Mothers
The excretion of esomeprazole in milk has not been studied. However, omeprazole concentrations have been measured in breast milk of a woman following oral administration of 20 mg. Because esomeprazole is likely to be excreted in human milk, because of the potential for serious adverse reactions in nursing infants from esomeprazole, and because of the potential for tumorigenicity shown for omeprazole in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of NEXIUM I.V. for Injection have been established in pediatric patients 1 month to 17 years of age for short-term treatment of GERD with Erosive Esophagitis [see Clinical Pharmacology, Pharmacokinetics (12.3)]. However, effectiveness has not been established in patients less than 1 month of age.
1 month to 17 years of age
Use of NEXIUM I.V. for Injection in pediatric patients 1 month to 17 years of age for short-term treatment of GERD with Erosive Esophagitis is supported by: a) results observed from a pharmacokinetic (PK) study on NEXIUM I.V. for Injection performed in pediatric patients, b) predictions from a population PK model comparing I.V. PK data between adult and pediatric patients, and c) relationship between exposure and pharmacodynamic results obtained from adult I.V. and pediatric oral data and d) PK results already included in the current approved labeling and from adequate and well-controlled studies that supported the approval of NEXIUM I.V. for Injection for adults.
Neonates 0 to 1 month of age
Following administration of NEXIUM I.V. in neonates the geometric mean (range) for CL was 0.17 L/h/kg (0.04 L/h/kg- 0.32 L/h/kg).
8.5 Geriatric Use
Of the total number of patients who received oral NEXIUM in clinical trials, 1,459 were 65 to 74 years of age and 354 patients were ≥ 75 years of age.
No overall differences in safety and efficacy were observed between the elderly and younger individuals, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
No dosage adjustment is necessary in patients with mild to moderate hepatic insufficiency (Child Pugh Classes A and B). For patients with severe hepatic insufficiency (Child Pugh Class C) a dose of 20 mg once daily should not be exceeded [see Dosage and Administration (2) and Clinical Pharmacology, Pharmacokinetics (12.3)].
10 OVERDOSAGE
The minimum lethal dose of esomeprazole sodium in rats after bolus administration was 310 mg/kg (about 62 times the human dose on a body surface area basis). The major signs of acute toxicity were reduced motor activity, changes in respiratory frequency, tremor, ataxia and intermittent clonic convulsions.
The symptoms described in connection with deliberate NEXIUM overdose (limited experience of doses in excess of 240 mg/day) are transient. Single doses of 80 mg of esomeprazole were uneventful. Reports of overdosage with omeprazole in humans may also be relevant. Doses ranged up to 2,400 mg (120 times the usual recommended clinical dose). Manifestations were variable, but included confusion, drowsiness, blurred vision, tachycardia, nausea, diaphoresis, flushing, headache, dry mouth, and other adverse reactions similar to those seen in normal clinical experience (see omeprazole package insert - ADVERSE REACTIONS). No specific antidote for esomeprazole is known. Since esomeprazole is extensively protein bound, it is not expected to be removed by dialysis. In the event of overdosage, treatment should be symptomatic and supportive.
As with the management of any overdose, the possibility of multiple drug ingestion should be considered. For current information on treatment of any drug overdose, a certified Regional Poison Control Center should be contacted. Telephone numbers are listed in the Physicians’ Desk Reference (PDR) or local telephone book.
11 DESCRIPTION
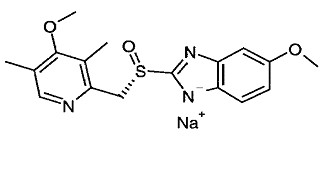
The active ingredient in NEXIUM® I.V. (esomeprazole sodium) for Injection is (S)-5-methoxy-2[[(4-methoxy-3,5- dimethyl-2-pyridinyl)-methyl]sulfinyl]-1 H-benzimidazole sodium, a proton pump inhibitor that inhibits gastric acid secretion. Esomeprazole is the S-isomer of omeprazole, which is a mixture of the S- and R- isomers. Its empirical formula is C17H18N3O3SNa with molecular weight of 367.4 g/mol (sodium salt) and 345.4 g/mol (parent compound). Esomeprazole sodium is very soluble in water and freely soluble in ethanol (95%). The structural formula is:
NEXIUM I.V. for Injection is supplied as a sterile, freeze-dried, white to off-white, porous cake or powder in a 5 mL vial, intended for intravenous administration after reconstitution with 0.9% Sodium Chloride Injection, USP; Lactated Ringer’s Injection, USP or 5% Dextrose Injection, USP. NEXIUM I.V. for Injection contains esomeprazole sodium 21.3 mg or 42.5 mg equivalent to esomeprazole 20 mg or 40 mg, edetate disodium 1.5 mg and sodium hydroxide q.s. for pH adjustment. The pH of reconstituted solution of NEXIUM I.V. for Injection depends on the reconstitution volume and is in the pH range of 9 to 11. The stability of esomeprazole sodium in aqueous solution is strongly pH dependent. The rate of degradation increases with decreasing pH.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Esomeprazole is a proton pump inhibitor that suppresses gastric acid secretion by specific inhibition of the H+/K+- ATPase in the gastric parietal cell. The S- and R-isomers of omeprazole are protonated and converted in the acidic compartment of the parietal cell forming the active inhibitor, the achiral sulphenamide. By acting specifically on the proton pump, esomeprazole blocks the final step in acid production, thus reducing gastric acidity. This effect is dose-related up to a daily dose of 20 to 40 mg and leads to inhibition of gastric acid secretion.
12.2 Pharmacodynamics
Antisecretory Activity
The effect of intravenous esomeprazole on intragastric pH was determined in two separate studies. In the first study, 20 mg of NEXIUM I.V. for Injection was administered intravenously once daily at constant rate over 30 minutes for 5 days. Twenty-two healthy subjects were included in the study. In the second study, 40 mg of NEXIUM I.V. for Injection was administered intravenously once daily at constant rate over 30 minutes for 5 days. Thirty-eight healthy subjects were included in the study.
Table 3
|
Esomeprazole 20 mg (n=22) |
Esomeprazole 40 mg (n=38) |
|
|
% Time Gastric pH>4 (95% CI) |
49.5 41.9–57.2 |
66.2 62.4–70.0 |
Gastric pH was measured over a 24-hour period
Serum Gastrin Effects
In oral studies, the effect of NEXIUM on serum gastrin concentrations was evaluated in approximately 2,700 patients in clinical trials up to 8 weeks and in over 1,300 patients for up to 6-12 months. The mean fasting gastrin level increased in a dose-related manner. This increase reached a plateau within two to three months of therapy and returned to baseline levels within four weeks after discontinuation of therapy.
Increased gastrin causes enterochromaffin-like cell hyperplasia and increased serum Chromogranin A (CgA) levels. The increased CgA levels may cause false positive results in diagnostic investigations for neuroendocrine tumors.
Enterochromaffin-like (ECL) Cell Effects
There are no data available on the effects of intravenous esomeprazole on ECL cells.
In 24-month carcinogenicity studies of oral omeprazole in rats, a dose-related significant occurrence of gastric ECL cell carcinoid tumors and ECL cell hyperplasia was observed in both male and female animals [see Nonclinical Toxicology, (13.1)]. Carcinoid tumors have also been observed in rats subjected to fundectomy or long-term treatment with other proton pump inhibitors or high doses of H2-receptor antagonists.
Human gastric biopsy specimens have been obtained from more than 3,000 patients treated orally with omeprazole in long-term clinical trials. The incidence of ECL cell hyperplasia in these studies increased with time; however, no case of ECL cell carcinoids, dysplasia, or neoplasia has been found in these patients.
In over 1,000 patients treated with NEXIUM (10, 20 or 40 mg/day) up to 6-12 months, the prevalence of ECL cell hyperplasia increased with time and dose. No patient developed ECL cell carcinoids, dysplasia, or neoplasia in the gastric mucosa.
Endocrine Effects
NEXIUM had no effect on thyroid function when given in oral doses of 20 or 40 mg for 4 weeks. Other effects of NEXIUM on the endocrine system were assessed using omeprazole studies. Omeprazole given in oral doses of 30 or 40 mg for 2 to 4 weeks had no effect on carbohydrate metabolism, circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin or secretin.
12.3 Pharmacokinetics
Absorption
The pharmacokinetic profile of NEXIUM I.V. for Injection 20 mg and 40 mg was determined in 24 healthy volunteers for the 20 mg dose and 38 healthy volunteers for the 40 mg dose following once daily administration of 20 mg and 40 mg of NEXIUM I.V. for Injection by constant rate over 30 minutes for five days. The results are shown in the following table:
Table 4
|
Parameter |
NEXIUM I.V. 20 mg |
NEXIUM I.V. 40 mg |
|
AUC (μmol*h/L) |
5.11 (3.96:6.61) |
16.21 (14.46:18.16) |
|
Cmax (μmol/L) |
3.86 (3.16:4.72) |
7.51 (6.93:8.13) |
|
t1/2 (h) |
1.05 (0.90:1.22) |
1.41 (1.30:1.52) |
Values represent the geometric mean (95% CI)
Distribution
Esomeprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 2- 20 μmol/L. The apparent volume of distribution at steady state in healthy volunteers is approximately 16 L.
Metabolism
Esomeprazole is extensively metabolized in the liver by the cytochrome P450 (CYP) enzyme system. The metabolites of esomeprazole lack antisecretory activity. The major part of esomeprazole’s metabolism is dependent upon the CYP2C19 isoenzyme, which forms the hydroxy and desmethyl metabolites. The remaining amount is dependent on CYP3A4 which forms the sulphone metabolite. CYP2C19 isoenzyme exhibits polymorphism in the metabolism of esomeprazole, since some 3% of Caucasians and 15-20% of Asians lack CYP2C19 and are termed Poor Metabolizers. At steady state, the ratio of AUC in Poor Metabolizers to AUC in the rest of the population (Extensive metabolizers) is approximately 2.
Following administration of equimolar doses, the S- and R-isomers are metabolized differently by the liver, resulting in higher plasma levels of the S- than of the R-isomer.
Excretion
Esomeprazole is excreted as metabolites primarily in urine but also in feces. Less than 1% of parent drug is excreted in the urine. Esomeprazole is completely eliminated from plasma, and there is no accumulation during once daily administration. The plasma elimination half-life of intravenous esomeprazole is approximately 1.1 to 1.4 hours and is prolonged with increasing dose of intravenous esomeprazole.
Special Populations
Investigation of age, gender, race, renal, and hepatic impairment and metabolizer status has been made previously with oral esomeprazole. The pharmacokinetics of esomeprazole is not expected to be affected differently by intrinsic or extrinsic factors after intravenous administration compared to oral administration. The same recommendations for dose adjustment in special populations are suggested for intravenous esomeprazole as for oral esomeprazole.
Geriatric
In oral studies, the AUC and Cmax values were slightly higher (25% and 18%, respectively) in the elderly as compared to younger subjects at steady state. Dosage adjustment based on age is not necessary.
Pediatric
In a randomized, open-label, multi-national, repeated dose study, esomeprazole PK was evaluated following a once-daily 3-minute injection in a total of 50 pediatric patients 0 to 17 years old, inclusive. Esomeprazole plasma AUC values for 20 mg NEXIUM IV were 183% and 60% higher in pediatric patients aged 6 – 11 years and 12 –17 years respectively compared to adults given 20 mg. Subsequent pharmacokinetic analyses predicted that a dosage regimen of 0.5 mg/kg once-daily for pediatric patients 1-11 months of age, 10 mg for pediatric patients 1-17 years with body weight <55 kg, and 20 mg for pediatric patients 1-17 years with body >55 kg would achieve comparable steady-state plasma exposures (AUC0-24) to those observed in adult patients administered 20 mg of NEXIUM I.V. once every 24 hours. Further, increasing the infusion duration from 3 minutes to 10 minutes or 30 minutes was predicted to produce steady-state Cmax values that were comparable to those observed in adult patients at the 40 mg and 20 mg NEXIUM I.V. doses.
Gender
In oral studies, the AUC and Cmax values were slightly higher (13%) in females than in males at steady state. Similar differences have been seen for intravenous administration of esomeprazole. Dosage adjustment based on gender is not necessary.
Hepatic Insufficiency
In oral studies, the steady state pharmacokinetics of esomeprazole obtained after administration of 40 mg once daily to 4 patients each with mild (Child Pugh Class A), moderate (Child Pugh Class B), and severe (Child Pugh Class C) liver insufficiency were compared to those obtained in 36 male and female GERD patients with normal liver function. In patients with mild and moderate hepatic insufficiency, the AUCs were within the range that could be expected in patients with normal liver function. In patients with severe hepatic insufficiency the AUCs were 2 to 3 times higher than in the patients with normal liver function. No dosage adjustment is recommended for patients with mild to moderate hepatic insufficiency (Child Pugh Classes A and B). However, in patients with severe hepatic insufficiency (Child Pugh Class C) a dose of 20 mg once daily should not be exceeded [see Dosage and Administration (2) and Use in Specific Populations (8.6)].
Renal Insufficiency
The pharmacokinetics of esomeprazole in patients with renal impairment are not expected to be altered relative to healthy volunteers as less than 1% of esomeprazole is excreted unchanged in urine.
12.4 Microbiology
Effects on Gastrointestinal Microbial Ecology
Decreased gastric acidity due to any means including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and, in hospitalized patients, possibly also Clostridium difficile.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of esomeprazole was assessed using omeprazole studies. In two 24-month oral carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44.0, and 140.8 mg/kg/day (about 0.7 to 57 times the human dose of 20 mg/day expressed on a body surface area basis) produced gastric ECL cell carcinoids in a dose-related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8 mg omeprazole/kg/day (about 5.6 times the human dose on a body surface area basis) for 1 year, then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of 1 year (94% treated vs 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs 26%) but still showed more hyperplasia in the treated group. Gastric adenocarcinoma was seen in one rat (2%). No similar tumor was seen in male or female rats treated for 2 years. For this strain of rat no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. A 78-week oral mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive.
Esomeprazole was negative in the Ames mutation test, in the in vivo rat bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test. Esomeprazole, however, was positive in the in vitro human lymphocyte chromosome aberration test. Omeprazole was positive in the in vitro human lymphocyte chromosome aberration test, the in vivo mouse bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test.
The potential effects of esomeprazole on fertility and reproductive performance were assessed using omeprazole studies. Omeprazole at oral doses up to 138 mg/kg/day in rats (about 56 times the human dose on a body surface area basis) was found to have no effect on reproductive performance of parental animals.
14 CLINICAL STUDIES
14.1 Acid Suppression in Gastroesophageal Reflux Disease (GERD)
Four multicenter, open-label, two-period crossover studies were conducted to compare the pharmacodynamic efficacy of the intravenous formulation of esomeprazole (20 mg and 40 mg) to that of NEXIUM delayed-release capsules at corresponding doses in patients with symptoms of GERD, with or without erosive esophagitis. The patients (n=206, 18 to 72 years old; 112 female; 110 Caucasian, 50 Black, 10 Asian, and 36 Other Race) were randomized to receive either 20 or 40 mg of intravenous or oral esomeprazole once daily for 10 days (Period 1), and then were switched in Period 2 to the other formulation for 10 days, matching their respective dose level from Period 1. The intravenous formulation was administered as a 3-minute injection in two of the studies, and as a 15-minute infusion in the other two studies. Basal acid output (BAO) and maximal acid output (MAO) were determined 22-24 hours post-dose on Period 1, Day 11; on Period 2, Day 3; and on Period 2, Day 11. BAO and MAO were estimated from 1-hour continuous collections of gastric contents prior to and following (respectively) subcutaneous injection of 6.0 mcg/kg of pentagastrin.
In these studies, after 10 days of once daily administration, the intravenous dosage forms of NEXIUM 20 mg and 40 mg were similar to the corresponding oral dosage forms in their ability to suppress BAO and MAO in these GERD patients (see table below).
There were no major changes in acid suppression when switching between intravenous and oral dosage forms.
Table 5
|
BAO in mmol H+/h |
MAO in mmol H+/h |
|||||
|
Study |
Dose in mg |
Intravenous Administration Method |
Intravenous |
Oral |
Intravenous |
Oral |
|
1 (N=42) |
20 |
3-minute injection |
0.71 (1.24) |
0.69 (1.24) |
5.96 (5.41) |
5.27 (5.39) |
|
2 (N=44) |
20 |
15-minute infusion |
0.78 (1.38) |
0.82 (1.34) |
5.95 (4.00) |
5.26 (4.12) |
|
3 (N=50) |
40 |
3-minute injection |
0.36 (0.61) |
0.31 (0.55) |
5.06 (3.90) |
4.41 (3.11) |
|
4 (N=47) |
40 |
15-minute infusion |
0.36 (0.79) |
0.22 (0.39) |
4.74 (3.65) |
3.52 (2.86) |
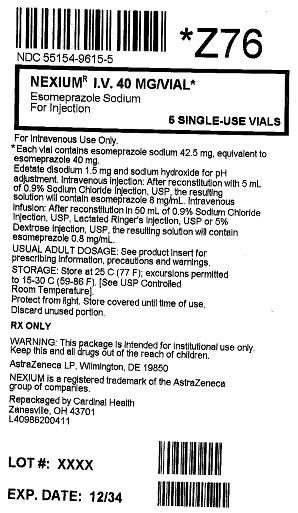
16 HOW SUPPLIED/STORAGE AND HANDLING
NEXIUM I.V. for Injection is supplied as a freeze-dried powder containing 20 mg or 40 mg of esomeprazole per single-use vial.
NDC 0186-6020-01 one carton containing 10 vials of NEXIUM I.V. for Injection (each vial contains 20 mg of esomeprazole).
NDC 0186-6040-01 one carton containing 10 vials of NEXIUM I.V. for Injection (each vial contains 40 mg of esomeprazole).
Storage
Store at 25°C (77°F); excursions permitted to 15°-30°C (59°- 86°F). [See USP Controlled Room Temperature]. Protect from light. Store in carton until time of use.
Following reconstitution and administration, discard any unused portion of esomeprazole solution.
17 PATIENT COUNSELING INFORMATION
- Advise patients to let their healthcare provider know if they are taking, or begin taking other medications, because NEXIUM can interfere with antiretroviral drugs and drugs that are affected by gastric pH changes [see Drug Interactions (7)].
- Let patients know that antacids may be used while taking NEXIUM.
Advise patients to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia [see Warnings and Precautions (5.4)].
NEXIUM is a registered trademark of the AstraZeneca group of companies.
© AstraZeneca 2012
Manufactured for:
AstraZeneca LP
Wilmington, DE 19850
Revised: 01/2012
| NEXIUM
I.V.
esomeprazole sodium injection |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Cardinal Health (188557102) |
| Registrant - AstraZeneca PLC (230790719) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Cardinal Health | 188557102 | REPACK(55154-9615) | |