FINACEA- azelaic acid gel
Bayer HealthCare Pharmaceuticals Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use FINACEA® Gel safely and effectively. See full prescribing information for FINACEA Gel.
FINACEA® (azelaic acid) Gel, 15% for topical use Initial U.S. Approval: 1995 RECENT MAJOR CHANGES
Warnings and Precautions:
INDICATIONS AND USAGEFINACEA® (azelaic acid) Gel, 15% is indicated for topical treatment of the inflammatory papules and pustules of mild to moderate rosacea. Efficacy for treatment of erythema in rosacea in the absence of papules and pustules has not been evaluated. (1) (1) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSGel, 15% (3) CONTRAINDICATIONSNone. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe most common adverse reactions are burning/stinging/tingling (29%), pruritus (11%), scaling/dry skin/xerosis (8%) and erythema/irritation (4%). (6) To report SUSPECTED ADVERSE REACTIONS, contact Bayer HealthCare at 1-866-463-3634 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. See 17 for PATIENT COUNSELING INFORMATION. Revised: 8/2016 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
FINACEA® (azelaic acid) Gel, 15% is indicated for topical treatment of the inflammatory papules and pustules of mild to moderate rosacea. Although some reduction of erythema which was present in patients with papules and pustules of rosacea occurred in clinical studies, efficacy for treatment of erythema in rosacea in the absence of papules and pustules has not been evaluated.
2 DOSAGE AND ADMINISTRATION
- •
- Apply and gently massage a thin layer of FINACEA Gel into the affected areas on the face twice daily (morning and evening).
- •
- Use only very mild soaps or soapless cleansing lotion before application of FINACEA Gel.
- •
- Cosmetics may be applied after the application of FINACEA Gel has dried.
- •
- Avoid the use of occlusive dressings or wrappings.
- •
- Instruct patients to avoid spicy foods, thermally hot foods and drinks, alcoholic beverages.
- •
- Patients should be reassessed if no improvement is observed upon completing 12 weeks of therapy.
- •
- Not for oral, ophthalmic or intravaginal use.
3 DOSAGE FORMS AND STRENGTHS
FINACEA (azelaic acid) Gel, 15% is a white to yellowish white opaque gel. Each gram of FINACEA Gel contains 0.15 gm of azelaic acid (15% w/w).
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Hypersensitivity reactions, including cases of angioedema, eye swelling, facial swelling, dyspnea, urticaria, and adverse skin reactions, have been reported during post marketing surveillance.
Avoid the use of FINACEA Gel in patients with known hypersensitivity to any component of the gel. If hypersensitivity develops during treatment, discontinue FINACEA Gel and institute appropriate therapy.
5.2 Skin Reactions
Skin irritation (i.e. pruritus, burning or stinging) may occur during use of FINACEA Gel, usually during the first few weeks of treatment. If sensitivity or severe irritation develops and persists, discontinue treatment and institute appropriate therapy.
There have been isolated reports of hypopigmentation after use of azelaic acid. Since azelaic acid has not been well studied in patients with dark complexion, monitor these patients for early signs of hypopigmentation.
5.3 Eye and Mucous Membranes Irritation
Avoid contact with the eyes, mouth and other mucous membranes. If FINACEA Gel does come in contact with the eyes, wash the eyes with large amounts of water and consult a physician if eye irritation persists [see Adverse Reactions (6.2)].
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In two vehicle-controlled and one active-controlled U.S. clinical trials, treatment safety was monitored in 788 subjects who used twice-daily FINACEA Gel for 12 weeks (N=333) or 15 weeks (N=124), or the gel vehicle (N=331) for 12 weeks. In all three trials, the most common treatment-related adverse events were: burning/stinging/tingling (29%), pruritus (11%), scaling/dry skin/xerosis (8%) and erythema/irritation (4%). In the active-controlled trial, overall adverse reactions (including burning, stinging/tingling, dryness/tightness/scaling, itching, and erythema/irritation/redness) were 19.4% (24/124) for FINACEA Gel compared to 7.1% (9/127) for the active comparator gel at 15 weeks.
|
FINACEA Gel, 15% N=457 (100%) |
Vehicle N=331 (100%) |
|||||
|
Mild N=99 (22%) |
Moderate N=61 (13%) |
Severe N=27 (6%) |
Mild N=46 (14%) |
Moderate N=30 (9%) |
Severe N=5 (2%) |
|
|
Burning/stinging/tingling |
71 (16%) |
42 (9%) |
17 (4%) |
8 (2%) |
6 (2%) |
2 (1%) |
|
Pruritus |
29 (6%) |
18 (4%) |
5 (1%) |
9 (3%) |
6 (2%) |
0 (0%) |
|
Scaling/dry skin/xerosis |
21 (5%) |
10 (2%) |
5 (1%) |
31 (9%) |
14 (4%) |
1 (<1%) |
|
Erythema/irritation |
6 (1%) |
7 (2%) |
2 (<1%) |
8 (2%) |
4 (1%) |
2 (1%) |
|
Contact dermatitis |
2 (<1%) |
3 (1%) |
0 (0%) |
1 (<1%) |
0 (0%) |
0 (0%) |
|
Edema |
3 (1%) |
2 (<1%) |
0 (0%) |
3 (1%) |
0 (0%) |
0 (0%) |
|
Acne |
3 (1%) |
1 (<1%) |
0 (0%) |
1 (<1%) |
0 (0%) |
0 (0%) |
|
||||||
In patients using azelaic acid formulations, the following adverse events have been reported: worsening of asthma, vitiligo, depigmentation, small depigmented spots, hypertrichosis, reddening (signs of keratosis pilaris) and exacerbation of recurrent herpes labialis.
Local Tolerability Studies
FINACEA Gel and its vehicle caused irritant reactions at the application site in human dermal safety studies. FINACEA Gel caused significantly more irritation than its vehicle in a cumulative irritation study. Some improvement in irritation was demonstrated over the course of the clinical trials, but this improvement might be attributed to subject dropouts. No phototoxicity or photoallergenicity were reported in human dermal safety studies.
6.2 Post-Marketing Experience
The following adverse reactions have been identified post approval of FINACEA Gel. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure:
Eyes: iridocyclitis upon accidental exposure of the eyes to FINACEA Gel
Hypersensitivity: angioedema, eye swelling, facial swelling, urticaria.
Respiratory: worsening of asthma, dyspnea, wheezing,
7 DRUG INTERACTIONS
There have been no formal studies of the interaction of FINACEA Gel with other drugs.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. Therefore, FINACEA Gel should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Dermal embryofetal developmental toxicology studies have not been performed with azelaic acid, 15% gel. Oral embryofetal developmental studies were conducted with azelaic acid in rats, rabbits, and cynomolgus monkeys. Azelaic acid was administered during the period of organogenesis in all three animal species. Embryotoxicity was observed in rats, rabbits, and monkeys at oral doses of azelaic acid that generated some maternal toxicity. Embryotoxicity was observed in rats given 2500 mg/kg/day [162 times the maximum recommended human dose (MRHD) based on body surface area (BSA)], rabbits given 150 or 500 mg/kg/day (19 or 65 times the MRHD based on BSA) and cynomolgus monkeys given 500 mg/kg/day (65 times the MRHD based on BSA) azelaic acid. No teratogenic effects were observed in the oral embryofetal developmental studies conducted in rats, rabbits and cynomolgus monkeys.
An oral peri- and post-natal developmental study was conducted in rats. Azelaic acid was administered from gestational day 15 through day 21 postpartum up to a dose level of 2500 mg/kg/day. Embryotoxicity was observed in rats at an oral dose of 2500 mg/kg/day (162 times the MRHD based on BSA) that generated some maternal toxicity. In addition, slight disturbances in the post-natal development of fetuses was noted in rats at oral doses that generated some maternal toxicity (500 and 2500 mg/kg/day; 32 and 162 times the MRHD based on BSA). No effects on sexual maturation of the fetuses were noted in this study.
8.3 Nursing Mothers
It is not known whether azelaic acid is excreted in human milk; however, in vitro studies using equilibrium dialysis were conducted to assess the potential for human milk partitioning. The studies demonstrated that, at an azelaic acid concentration of 25 µg/mL, the milk/plasma distribution coefficient was 0.7 and the milk/buffer distribution was 1.0. These data indicate that passage of drug into maternal milk may occur. Since less than 4% of a topically applied dose of 20% azelaic acid cream is systemically absorbed, the uptake of azelaic acid into maternal milk is not expected to cause a significant change from baseline azelaic acid levels in the milk. Nevertheless, a decision should be made to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
11 DESCRIPTION
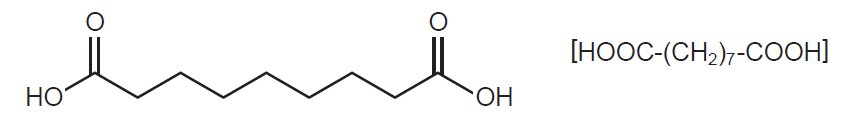
FINACEA (azelaic acid) Gel, 15%, is an aqueous gel which contains azelaic acid, a naturally-occurring saturated dicarboxylic acid. Chemically, azelaic acid is 1,7-heptanedicarboxylic acid. The molecular formula for azelaic acid is C9 H16 O4. It has the following structure:
Azelaic acid has a molecular weight of 188.22. It is a white, odorless crystalline solid. It is poorly soluble in water at 20°C (0.24%) but freely soluble in boiling water and in ethanol.
FINACEA Gel is a white to yellowish white opaque gel for topical use; each gram contains 0.15 gm azelaic acid (15%w/w) in an aqueous gel base containing benzoic acid (as a preservative), disodium EDTA, lecithin, medium-chain triglycerides, polyacrylic acid, polysorbate 80, propylene glycol, purified water, and sodium hydroxide to adjust pH.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism(s) by which azelaic acid interferes with the pathogenic events in rosacea are unknown.
12.2 Pharmacodynamics
The pharmacodynamics of azelaic acid in association with the treatment of rosacea is unknown.
12.3 Pharmacokinetics
The percutaneous absorption of azelaic acid after topical application of FINACEA Gel could not be reliably determined. Mean plasma azelaic acid concentrations in rosacea subjects treated with FINACEA Gel twice daily for at least 8 weeks are in the range of 42 to 63.1 ng/mL. These values are within the maximum concentration range of 24.0 to 90.5 ng/mL observed in rosacea subjects treated with vehicle only. This indicates that FINACEA Gel does not increase plasma azelaic acid concentration beyond the range derived from nutrition and endogenous metabolism.
In vitro and human data suggest negligible cutaneous metabolism of 3H-azelaic acid after topical application of 20% azelaic acid cream. Azelaic acid is mainly excreted unchanged in the urine, but undergoes some ß oxidation to shorter chain dicarboxylic acids.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Systemic long-term animal studies have not been performed to evaluate the carcinogenic potential of azelaic acid. In a 26-week dermal carcinogenicity study using transgenic (Tg.AC) mice, FINACEA Gel and the gel vehicle, when applied once or twice daily, did not increase the number of female Tg.AC animals with papillomas at the treatment site. No statistically significant increase in the number of animals with papillomas at the treatment site was observed in male Tg.AC animals after once daily application. After twice daily application, FINACEA Gel and the gel vehicle induced a statistically significant increase in the number of male animals with papillomas at the treatment site when compared to untreated males. This suggests that the positive effect may be associated with the vehicle application. The clinical relevance of the findings in animals to humans is not clear.
Azelaic acid was not mutagenic or clastogenic in a battery of in vitro [Ames assay, HGPRT in V79 cells (Chinese hamster lung cells), and chromosomal aberration assay in human lymphocytes] and in vivo (dominant lethal assay in mice and mouse micronucleus assay) genotoxicity tests.
Oral administration of azelaic acid at dose levels up to 2500 mg/kg/day (162 times the MRHD based on BSA) did not affect fertility or reproductive performance in male or female rats.
14 CLINICAL STUDIES
FINACEA Gel was evaluated for the treatment of mild to moderate papulopustular rosacea in two multicenter, randomized, double-blind, vehicle-controlled, 12-week clinical trials having identical protocols and involving a total of 664 (active: 333; vehicle: 331) subjects aged 21 to 86 years (mean age = 49). Overall, 92.5% of subjects were Caucasian and 73% of subjects were female. Enrolled subjects had mild to moderate rosacea with a mean lesion count of 18 (range 8 to 60) inflammatory papules and pustules. The following subjects were excluded: a) those without papules and pustules; b) those with nodules, rhinophyma, or ocular involvement and c) those with a history of hypersensitivity to propylene glycol or to any other ingredients of the study drug. FINACEA Gel or its vehicle were to be applied twice daily for 12 weeks; no other topical or systemic medication affecting the course of rosacea and/or evaluability was to be used during the studies. Subjects were instructed to avoid spicy foods, thermally hot food/drink and alcoholic beverages during the study. Subjects were also instructed to use only very mild soaps or soapless cleansing lotion for facial cleansing.
The primary efficacy endpoints included both 1) change from baseline in inflammatory lesion counts as well as 2) success defined as a score of “clear” or “minimal” with at least a 2-step reduction from baseline on the Investigator’s Global Assessment (IGA), defined as follows below:
CLEAR:
No papules and/or pustules; no or residual erythema; no or mild to moderate telangiectasia
MINIMAL:
Rare papules and/or pustules; residual to mild erythema; mild to moderate telangiectasia
MILD:
Few papules and/or pustules; mild erythema; mild to moderate telangiectasia
MILD TO MODERATE:
Distinct number of papules and/or pustules; mild to moderate erythema; mild to moderate telangiectasia
MODERATE:
Pronounced number of papules and/or pustules; moderate erythema; mild to moderate telangiectasia
MODERATE TO SEVERE:
Many papules and/or pustules, occasionally with large inflamed lesions; moderate erythema; moderate degree of telangiectasia
SEVERE:
Numerous papules and/or pustules, occasionally with confluent areas of inflamed lesions; moderate or severe erythema; moderate or severe telangiectasia
Primary efficacy assessment was based on the “intent-to-treat” (ITT) population with the “last observation carried forward” (LOCF).
Both trials demonstrated a statistically significant difference in favor of FINACEA Gel over its vehicle in both reducing the number of inflammatory papules and pustules associated with rosacea (Table 2) as well as demonstrating success on the IGA in the ITT-LOCF population at the end of treatment.
| *ITT population with last observation carried forward (LOCF) | ||||
|
Study One FINACEA Gel, 15% N=164 |
Study One VEHICLE N=165 |
Study Two FINACEA Gel, 15% N=167 |
Study Two VEHICLE N=166 |
|
|
Mean Lesion Count Baseline |
17.5 |
17.6 |
17.9 |
18.5 |
|
End of Treatment* |
6.8 |
10.5 |
9.0 |
12.1 |
|
Mean Percent Reduction End of Treatment* |
57.9% |
39.9% |
50.0% |
38.2% |
Although some reduction of erythema which was present in subjects with papules and pustules of rosacea occurred in clinical trials, efficacy for treatment of erythema in rosacea in the absence of papules and pustules has not been evaluated.
FINACEA Gel was superior to the vehicle with regard to success based on the IGA of rosacea on a 7-point static score at the end of treatment (ITT population; Table 3).
| *ITT population with last observation carried forward (LOCF) | |||||||||
|
Study One FINACEA Gel, 15% N=164 |
Study One VEHICLE N=165 |
Study Two FINACEA Gel, 15% N=167 |
Study Two VEHICLE N=166 |
||||||
|
Clear, Minimal or Mild at End of Treatment (% of Subjects) |
61% |
40% |
61% |
48% |
|||||
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
Inform patients using FINACEA Gel of the following information and instructions:
- •
- For external use only.
- •
- Before applying FINACEA Gel, cleanse affected area(s) with a very mild soap or a soapless cleansing lotion and pat dry with a soft towel.
- •
- Avoid use of alcoholic cleansers, tinctures and astringents, abrasives and peeling agents.
- •
- Avoid contact with the eyes, mouth and other mucous membranes. If FINACEA Gel does come in contact with the eyes, wash the eyes with large amounts of water and consult your physician if eye irritation persists.
- •
- Wash hands immediately following application of FINACEA Gel.
- •
- Cosmetics may be applied after the application of FINACEA Gel has dried.
- •
- Avoid the use of occlusive dressings or wrappings.
- •
- Skin irritation (e.g., pruritus, burning, or stinging) may occur during use of FINACEA Gel, usually during the first few weeks of treatment. If irritation is excessive or persists, or allergic reactions occur, discontinue use and consult your physician.
- •
- If allergic reactions occur, discontinue use and consult their healthcare providers.
- •
- Advise patients to report any worsening of asthma to their healthcare providers.
- •
- Report abnormal changes in skin color to their healthcare providers.
- •
- To help manage rosacea, avoid any triggers that may provoke erythema, flushing, and blushing. These triggers can include spicy and thermally hot food and drinks such as hot coffee, tea, or alcoholic beverages.
- •
- FINACEA Gel comes in a tube and a pump:
- o
- Tube instructions: Remove the cap before use. Squeeze the tube to dispense a small amount of FINACEA Gel.
- o
- Pump instructions:
- ▪
- Remove the cap before use. Depress the pump to dispense a small amount of FINACEA Gel. At first use, the pump may have to be depressed repeatedly until product is dispensed.
- ▪
- Discard the pump 8 weeks after opening.
© 2002, Bayer HealthCare Pharmaceuticals Inc. All rights reserved.
Manufactured for:
Bayer HealthCare Pharmaceuticals Inc.
Whippany, NJ 07981
Manufactured in Italy
| FINACEA
azelaic acid gel |
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
| Labeler - Bayer HealthCare Pharmaceuticals Inc. (005436809) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Leo Pharma Manufacturing Italy SRL | 439982002 | MANUFACTURE(50419-825) | |