OPTIPRANOLOL- metipranolol solution/ drops
Bausch & Lomb Incorporated
----------
OptiPranolol
metipranolol ophthalmic solution 0.3%
DESCRIPTION
OptiPranolol® (metipranolol ophthalmic solution) 0.3% contains metipranolol, a non-selective beta-adrenergic receptor blocking agent. Metipranolol is a white, odorless, crystalline powder.
The chemical name of metipranolol is (±)-1-(4-Hydroxy-2, 3, 5-trimethylphenoxy)-3-(isopropylamino)-2-propanol-4-acetate.
The chemical structure of metipranolol is:
C17H27NO4
Mol. Wt. 309.40
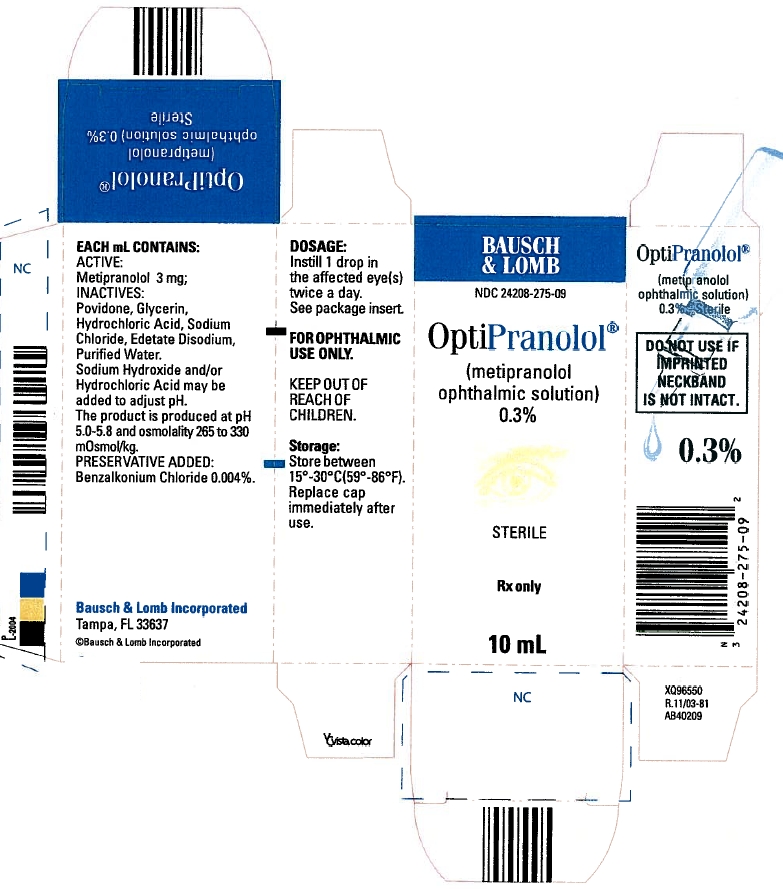
Each mL of OptiPranolol® contains 3 mg of metipranolol. INACTIVES: Povidone, Glycerin, Hydrochloric Acid, Sodium Chloride, Edetate Disodium, and Purified Water. Sodium Hydroxide and/or Hydrochloric Acid may be added to adjust pH. The product is produced at pH 5.0-5.8 and osmolality 265 to 330 mOsmol/kg. PRESERVATIVE ADDED: Benzalkonium Chloride 0.004%.
CLINICAL PHARMACOLOGY
Metipranolol blocks beta1 and beta2 (non-selective) adrenergic receptors. It does not have significant intrinsic sympathomimetic activity, and has only weak local anesthetic (membrane-stabilizing) and myocardial depressant activity.
Orally administered beta-adrenergic blocking agents reduce cardiac output in both healthy subjects and patients with heart disease. In patients with severe impairment of myocardial function, beta-adrenergic receptor antagonists may inhibit the sympathetic stimulatory effect necessary to maintain adequate cardiac output.
Beta-adrenergic receptor blockade in the bronchi and bronchioles may result in significantly increased airway resistance from unopposed parasympathetic activity. Such an effect is potentially dangerous in patients with asthma or other bronchospastic conditions (see CONTRAINDICATIONS and WARNINGS).
OptiPranolol Ophthalmic Solution, when applied topically in the eye, has the action of reducing elevated as well as normal intraocular pressure (IOP), whether or not accompanied by glaucoma. Elevated intraocular pressure is a major risk factor in the pathogenesis of glaucomatous visual field loss.
The higher the level of intraocular pressure, the greater the likelihood of glaucomatous visual field loss and optic nerve damage.
The primary mechanism of the ocular hypotensive action of metipranolol is most likely due to a reduction in aqueous humor production. A slight increase in outflow may be an additional mechanism. OptiPranolol Ophthalmic Solution reduces IOP with little or no effect on pupil size or accommodation.
In controlled studies of patients with intraocular pressure greater than 24 mmHg at baseline, OptiPranolol Ophthalmic Solution reduced the average intraocular pressure approximately 20-26%.
The onset of action of OptiPranolol Ophthalmic Solution, as measured by a reduction in intraocular pressure, occurs within 30 minutes after a single administration. The maximum effect occurs at about 2 hours. A reduction in intraocular pressure can be demonstrated 24 hours after a single dose.
Clinical studies in patients with glaucoma treated for up to two years indicate that an intraocular pressure lowering effect is maintained.
ANIMAL PHARMACOLOGY
In rabbits administered metipranolol in one eye at 2 to 4 fold increased concentrations, multi-focal interstitial nephritis was observed in male animals, and lympho-hystiocytic and heterophilic interstitial pneumonia was observed in female animals. The clinical relevance of these findings is unknown.
INDICATIONS AND USAGE
OptiPranolol Ophthalmic Solution is indicated in the treatment of elevated intraocular pressure in patients with ocular hypertension or open angle glaucoma.
CONTRAINDICATIONS
Hypersensitivity to any component of this product.
OptiPranolol Ophthalmic Solution is contraindicated in patients with bronchial asthma or a history of bronchial asthma, or severe chronic obstructive pulmonary disease; symptomatic sinus bradycardia; greater than a first degree atrioventricular block; cardiogenic shock; or overt cardiac failure.
WARNINGS
As with other topically applied ophthalmic drugs, this drug may be absorbed systemically. Thus, the same adverse reactions found with systemic administration of beta-adrenergic blocking agents may occur with topical administration. For example, severe respiratory reactions and cardiac reactions, including death due to bronchospasm in patients with asthma, and rarely, death in association with cardiac failure, have been reported following topical application of beta-adrenergic blocking agents (see CONTRAINDICATIONS).
Since OptiPranolol Ophthalmic Solution had a minor effect on heart rate and blood pressure in clinical studies, caution should be observed in treating patients with a history of cardiac failure. Treatment with OptiPranolol Ophthalmic Solution should be discontinued at the first evidence of cardiac failure.
OptiPranolol Ophthalmic Solution, or other beta-blockers, should not, in general, be administered to patients with chronic obstructive pulmonary disease (e.g., chronic bronchitis, emphysema) of mild or moderate severity (see CONTRAINDICATIONS). However, if the drug is necessary in such patients, then it should be administered with caution since it may block bronchodilation produced by endogenous and exogenous catecholamine stimulation of beta2 receptors.
PRECAUTIONS
General
Because of potential effects of beta-adrenergic receptor blocking agents relative to blood pressure and pulse, these agents should be used with caution in patients with cerebrovascular insufficiency. If signs or symptoms suggesting reduced cerebral blood flow develop following initiation of therapy with OptiPranolol Ophthalmic Solution, alternative therapy should be considered.
Some authorities recommend gradual withdrawal of beta-adrenergic receptor blocking agents in patients undergoing elective surgery. If necessary during surgery, the effects of beta-adrenergic receptor blocking agents may be reversed by sufficient doses of such agonists as isoproterenol, dopamine, dobutamine or levarterenol.
While OptiPranolol Ophthalmic Solution has demonstrated a low potential for systemic effect, it should be used with caution in patients with diabetes (especially labile diabetes) because of possible masking of signs and symptoms of acute hypoglycemia.
Beta-adrenergic receptor blocking agents may mask certain signs and symptoms of hyperthyroidism, and their abrupt withdrawal might precipitate a thyroid storm.
Beta-adrenergic blockade has been reported to potentiate muscle weakness consistent with certain myasthenic symptoms (e.g., diplopia, ptosis, and generalized weakness).
Risk of anaphylactic reaction: While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Information for patients
Patients should be instructed to avoid allowing the tip of the dispensing container to contact the eye or surrounding structures.
Patients should be advised that OptiPranolol contains benzalkonium chloride which may be absorbed by soft contact lenses. Contact lenses should be removed prior to administration of the solution. Lenses may be reinserted 15 minutes following OptiPranolol administration.
Drug interactions
OptiPranolol® Ophthalmic Solution should be used with caution in patients who are receiving a beta-adrenergic blocking agent orally, because of the potential for additive effects on systemic beta-blockade.
Close observation of the patient is recommended when a beta-blocker is administered to patients receiving catecholamine-depleting drugs such as reserpine, because of possible additive effects and the production of hypotension and/or bradycardia.
Caution should be used in the coadministration of beta-adrenergic receptor blocking agents, such as metipranolol, and oral or intravenous calcium channel antagonists, because of possible precipitation of left ventricular failure, and hypotension. In patients with impaired cardiac function, who are receiving calcium channel antagonists, coadministration should be avoided.
The concomitant use of beta-adrenergic receptor blocking agents with digitalis and calcium channel antagonists may have additive effects, prolonging atrioventricular conduction time.
Caution should be used in patients using concomitant adrenergic psychotropic drugs.
Ocular
In patients with angle-closure glaucoma, the immediate treatment objective is to re-open the angle by constriction of the pupil with a miotic agent.
OptiPranolol Ophthalmic Solution has little or no effect on the pupil, therefore, when it is used to reduce intraocular pressure in angle-closure glaucoma, it should be used only with concomitant administration of a miotic agent.
Carcinogenesis, mutagenesis, impairment of fertility
Lifetime studies with metipranolol have been conducted in mice at oral doses of 5, 50, and 100 mg/kg/day and in rats at oral doses of up to 70 mg/kg/day. Metipranolol demonstrated no carcinogenic effect. In the mouse study, female animals receiving the low, but not the intermediate or high dose, had an increased number of pulmonary adenomas. The significance of this observation is unknown. In a variety of in vitro and in vivo bacterial and mammalian cell assays, metipranolol was nonmutagenic.
Reproduction and fertility studies of metipranolol in rats and mice showed no adverse effect on male fertility at oral doses of up to 50 mg/kg/day, and female fertility at oral doses of up to 25 mg/kg/day.
Pregnancy
Teratogenic effects
Pregnancy Category C:
No drug related effects were reported for the segment II teratology study in fetal rats after administration, during organogenesis, to dams of up to 50 mg/kg/day. OptiPranolol Ophthalmic Solution has been shown to increase fetal resorption, fetal death, and delayed development when administered orally to rabbits at 50 mg/kg/day during organogenesis.
There are no adequate and well-controlled studies in pregnant women. OptiPranolol Ophthalmic Solution should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
ADVERSE REACTIONS
In clinical trials, the use of OptiPranolol Ophthalmic Solution has been associated with transient local discomfort.
Other ocular adverse reactions, such as abnormal vision, blepharitis, blurred vision, browache, conjunctivitis, edema, eyelid dermatitis, photophobia, tearing, and uveitis have been reported in small numbers of patients.
Other systemic adverse reactions, such as allergic reaction, angina, anxiety, arthritis, asthenia, atrial fibrillation, bradycardia, bronchitis, coughing, depression, dizziness, dyspnea, epistaxis, headache, hypertension, myalgia, myocardial infarct, nausea, nervousness, palpitation, rash, rhinitis, and somnolence have also been reported in small numbers of patients.
Overdosage
No information is available on overdosage of OptiPranolol Ophthalmic Solution in humans. The symptoms which might be expected with an overdose of a systemically administered beta-adrenergic receptor blocking agent are bradycardia, hypotension and acute cardiac failure.
DOSAGE AND ADMINISTRATION
The recommended dose is one drop of OptiPranolol Ophthalmic Solution in the affected eye(s) twice a day.
If the patient’s IOP is not at a satisfactory level on this regimen, use of more frequent administration or a larger dose of OptiPranolol Ophthalmic Solution is not known to be of benefit. Concomitant therapy to lower intraocular pressure can be instituted.
In clinical trials, OptiPranolol® Ophthalmic Solution was safely used during concomitant therapy with pilocarpine, epinephrine or acetazolamide.
HOW SUPPLIED
OptiPranolol® (metipranolol ophthalmic solution) 0.3% is supplied in a plastic bottle with a controlled drop tip and a yellow plastic screw-top cap as follows:
5 mL: NDC 24208-275-07 - AB40207
10 mL: NDC 24208-275-09 - AB40209
STORAGE
Store between 15° - 30°C (59° - 86°F). Replace cap immediately after use.
DO NOT USE IF IMPRINTED NECKBAND IS NOT INTACT.
FOR OPHTHALMIC USE ONLY.
Rx only
| OPTIPRANOLOL
metipranolol solution/ drops |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Bausch & Lomb Incorporated (196603781) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Bausch & Lomb Incorporated | 807927397 | MANUFACTURE(24208-275) | |