UDENYCA- pegfilgrastim-cbqv injection, solution
Coherus BioSciences Inc
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use UDENYCA safely and effectively. See full prescribing information for UDENYCA.
UDENYCA® (pegfilgrastim-cbqv) injection, for subcutaneous use INITIAL U.S. APPROVAL: 2018 UDENYCA (pegfilgrastim-cbqv) is biosimilar* to NEULASTA (pegfilgrastim). * Biosimilar means that the biological product is approved based on data demonstrating that it is highly similar to an FDA-approved biological product, known as a reference product, and that there are no clinically meaningful differences between the biosimilar product and the reference product. Biosimilarity of UDENYCA has been demonstrated for the condition(s) of use (e.g. indication(s), dosing regimen(s), strength(s), dosage form(s), and route(s) of administration) described in its Full Prescribing Information. RECENT MAJOR CHANGESINDICATIONS AND USAGEUDENYCA is a leukocyte growth factor indicated to
Limitations of Use UDENYCA is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation. DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSInjection: 6 mg/0.6 mL in a single-dose prefilled syringe for manual use only. (3) CONTRAINDICATIONSPatients with a history of serious allergic reaction to human granulocyte colony-stimulating factors such as pegfilgrastim products or filgrastim products. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (≥ 5% difference in incidence compared to placebo) are bone pain and pain in extremity. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Coherus BioSciences at 1-800-4UDENYCA (1-800-483-3692) or FDA at 1-800-FDA-1088 (1-800-332-1088) or www.fda.gov/medwatch See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 11/2022 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Patients with Cancer Receiving Myelosuppressive Chemotherapy
UDENYCA is indicated to decrease the incidence of infection, as manifested by febrile neutropenia, in patients with non-myeloid malignancies receiving myelosuppressive anti-cancer drugs associated with a clinically significant incidence of febrile neutropenia [see Clinical Studies (14.1)].
Limitations of Use
UDENYCA is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation.
2 DOSAGE AND ADMINISTRATION
2.1 Patients with Cancer Receiving Myelosuppressive Chemotherapy
The recommended dosage of UDENYCA is a single subcutaneous injection of 6 mg administered once per chemotherapy cycle. For dosing in pediatric patients weighing less than 45 kg, refer to Table 1. Do not administer UDENYCA between 14 days before and 24 hours after administration of cytotoxic chemotherapy.
2.2 Patients with Hematopoietic Subsyndrome of Acute Radiation Syndrome
The recommended dose of UDENYCA is two doses, 6 mg each, administered subcutaneously one week apart. For dosing in pediatric patients weighing less than 45 kg, refer to Table 1. Administer the first dose as soon as possible after suspected or confirmed exposure to radiation levels greater than 2 gray (Gy). Administer the second dose one week after the first dose.
Obtain a baseline complete blood count (CBC). Do not delay administration of UDENYCA if a CBC is not readily available. Estimate a patient’s absorbed radiation dose (i.e., level of radiation exposure) based on information from public health authorities, biodosimetry if available, or clinical findings such as time to onset of vomiting or lymphocyte depletion kinetics.
2.3 Administration
UDENYCA is administered subcutaneously via a single-dose prefilled syringe for manual use.
Prior to use‚ remove the carton from the refrigerator and allow the UDENYCA prefilled syringe to reach room temperature for a minimum of 30 minutes. Discard any prefilled syringe left at room temperature for greater than 48 hours.
Visually inspect parenteral drug products (prefilled syringe) for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not administer UDENYCA if discoloration or particulates are observed.
The needle cap on the prefilled syringe is not made with natural rubber latex.
Pediatric Patients Weighing Less than 45 kg
The UDENYCA prefilled syringe is not designed to allow for direct administration of doses less than 0.6 mL (6 mg). The syringe does not bear graduation marks which are necessary to accurately measure doses of UDENYCA less than 0.6 mL (6 mg) for direct administration to patients. Thus, the direct administration to patients requiring dosing of less than 0.6 mL (6 mg) is not recommended due to the potential for dosing errors. Refer to Table 1.
|
||
| Body Weight | UDENYCA Dose | Volume to Administer |
|---|---|---|
| Less than 10 kg* | See below* | See below* |
| 10 - 20 kg | 1.5 mg | 0.15 mL |
| 21 - 30 kg | 2.5 mg | 0.25 mL |
| 31 - 44 kg | 4 mg | 0.4 mL |
3 DOSAGE FORMS AND STRENGTHS
Injection: 6 mg/0.6 mL clear, colorless, preservative-free solution in a single-dose prefilled syringe for manual use only.
4 CONTRAINDICATIONS
UDENYCA is contraindicated in patients with a history of serious allergic reactions to pegfilgrastim products or filgrastim products. Reactions have included anaphylaxis [see Warnings and Precautions (5.3)].
5 WARNINGS AND PRECAUTIONS
5.1 Splenic Rupture
Splenic rupture, including fatal cases, can occur following the administration of pegfilgrastim products. Evaluate for an enlarged spleen or splenic rupture in patients who report left upper abdominal or shoulder pain after receiving UDENYCA.
5.2 Acute Respiratory Distress Syndrome
Acute respiratory distress syndrome (ARDS) can occur in patients receiving pegfilgrastim products. Evaluate patients who develop fever and lung infiltrates or respiratory distress after receiving UDENYCA for ARDS. Discontinue UDENYCA in patients with ARDS.
5.3 Serious Allergic Reactions
Serious allergic reactions, including anaphylaxis, can occur in patients receiving pegfilgrastim products. The majority of reported events occurred upon initial exposure. Allergic reactions, including anaphylaxis, can recur within days after the discontinuation of initial anti-allergic treatment. Permanently discontinue UDENYCA in patients with serious allergic reactions. Do not administer UDENYCA to patients with a history of serious allergic reactions to pegfilgrastim products or filgrastim products.
5.4 Use in Patients with Sickle Cell Disorders
Severe and sometimes fatal sickle cell crises can occur in patients with sickle cell disorders receiving pegfilgrastim products. Discontinue UDENYCA if sickle cell crisis occurs.
5.5 Glomerulonephritis
Glomerulonephritis has occurred in patients receiving pegfilgrastim products. The diagnoses were based upon azotemia, hematuria (microscopic and macroscopic), proteinuria, and renal biopsy. Generally, events of glomerulonephritis resolved after dose reduction or discontinuation of pegfilgrastim products. If glomerulonephritis is suspected, evaluate for cause. If causality is likely, consider dose-reduction or interruption of UDENYCA.
5.6 Leukocytosis
White blood cell (WBC) counts of 100 x 109/L or greater have been observed in patients receiving pegfilgrastim products. Monitoring of complete blood count (CBC) during UDENYCA therapy is recommended.
5.7 Thrombocytopenia
Thrombocytopenia has been reported in patients receiving pegfilgrastim products. Monitor platelet counts.
5.8 Capillary Leak Syndrome
Capillary leak syndrome has been reported after G-CSF administration, including pegfilgrastim products, and is characterized by hypotension, hypoalbuminemia, edema, and hemoconcentration. Episodes vary in frequency, severity and may be life-threatening if treatment is delayed. Patients who develop symptoms of capillary leak syndrome should be closely monitored and receive standard symptomatic treatment, which may include a need for intensive care.
5.9 Potential for Tumor Growth Stimulatory Effects on Malignant Cells
The granulocyte colony-stimulating factor (G-CSF) receptor through which pegfilgrastim products and filgrastim products act has been found on tumor cell lines. The possibility that pegfilgrastim products act as a growth factor for any tumor type, including myeloid malignancies and myelodysplasia, diseases for which pegfilgrastim products are not approved, cannot be excluded.
5.10 Myelodysplastic Syndrome (MDS) and Acute Myeloid Leukemia (AML) in Patients with Breast and Lung Cancer
MDS and AML have been associated with the use of pegfilgrastim products in conjunction with chemotherapy and/or radiotherapy in patients with breast and lung cancer. Monitor patients for signs and symptoms of MDS/AML in these settings.
5.11 Aortitis
Aortitis has been reported in patients receiving pegfilgrastim products. It may occur as early as the first week after start of therapy. Manifestations may include generalized signs and symptoms such as fever, abdominal pain, malaise, back pain, and increased inflammatory markers (e.g., c-reactive protein and white blood cell count). Consider aortitis in patients who develop these signs and symptoms without known etiology. Discontinue UDENYCA if aortitis is suspected.
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Splenic Rupture [see Warnings and Precautions (5.1)]
- Acute Respiratory Distress Syndrome [see Warnings and Precautions (5.2)]
- Serious Allergic Reactions [see Warnings and Precautions (5.3)]
- Use in Patients with Sickle Cell Disorders [see Warnings and Precautions (5.4)]
- Glomerulonephritis [see Warnings and Precautions (5.5)]
- Leukocytosis [see Warnings and Precautions (5.6)]
- Thrombocytopenia [see Warnings and Precautions (5.7)]
- Capillary Leak Syndrome [see Warnings and Precautions (5.8)]
- Potential for Tumor Growth Stimulatory Effects on Malignant Cells [see Warnings and Precautions (5.9)]
- Myelodysplastic syndrome [see Warnings and Precautions (5.10)]
- Acute myeloid leukemia [see Warnings and Precautions (5.10)]
- Aortitis [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Pegfilgrastim clinical trials safety data are based upon 932 patients receiving pegfilgrastim in seven randomized clinical trials. The population was 21 to 88 years of age and 92% female. The ethnicity was 75% Caucasian, 18% Hispanic, 5% Black, and 1% Asian. Patients with breast (n = 823), lung and thoracic tumors (n = 53) and lymphoma (n = 56) received pegfilgrastim after nonmyeloablative cytotoxic chemotherapy. Most patients received a single 100 mcg/kg (n = 259) or a single 6 mg (n = 546) dose per chemotherapy cycle over 4 cycles.
The following adverse reaction data in Table 2 are from a randomized, double-blind, placebo-controlled study in patients with metastatic or non-metastatic breast cancer receiving docetaxel 100 mg/m2 every 21 days (Study 3). A total of 928 patients were randomized to receive either 6 mg pegfilgrastim (n = 467) or placebo (n = 461). The patients were 21 to 88 years of age and 99% female. The ethnicity was 66% Caucasian, 31% Hispanic, 2% Black, and <1% Asian, Native American or other.
The most common adverse reactions occurring in ≥ 5% of patients and with a between-group difference of ≥ 5% higher in the pegfilgrastim arm in placebo controlled clinical trials are bone pain and pain in extremity.
| Body System Adverse Reaction | Placebo (N = 461) | pegfilgrastim 6 mg SC on Day 2 (N = 467) |
|---|---|---|
| Musculoskeletal and connective tissue disorders | ||
| Bone pain | 26% | 31% |
| Pain in extremity | 4% | 9% |
Leukocytosis
In clinical studies, leukocytosis (WBC counts > 100 x 109/L was observed in less than 1% of 932 patients with non-myeloid malignancies receiving pegfilgrastim. No complications attributable to leukocytosis were reported in clinical studies.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other pegfilgrastim products may be misleading.
Binding antibodies to pegfilgrastim were detected using a BIAcore assay. The approximate limit of detection for this assay is 500 ng/mL. Pre-existing binding antibodies were detected in approximately 6% (51/849) of patients with metastatic breast cancer. Four of 521 pegfilgrastim-treated subjects who were negative at baseline developed binding antibodies to pegfilgrastim following treatment. None of these 4 patients had evidence of neutralizing antibodies detected using a cell-based bioassay.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post approval use of pegfilgrastim products. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Splenic rupture and splenomegaly (enlarged spleen) [see Warnings and Precautions (5.1)]
- Acute respiratory distress syndrome (ARDS) [see Warnings and Precautions (5.2)]
- Allergic reactions/hypersensitivity, including anaphylaxis, skin rash, urticaria, generalized erythema and flushing [see Warnings and Precautions (5.3)]
- Sickle cell crisis [see Warnings and Precautions (5.4)]
- Glomerulonephritis [see Warnings and Precautions (5.5)]
- Leukocytosis [see Warnings and Precautions (5.6)]
- Thrombocytopenia [see Warnings and Precautions (5.7)]
- Capillary leak syndrome [see Warnings and Precautions (5.8)]
- Injection site reactions
- Sweet’s syndrome (acute febrile neutrophilic dermatosis), cutaneous vasculitis
- Myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) in patients with breast and lung cancer receiving chemotherapy and/or radiotherapy [see Warnings and Precautions (5.10)]
- Aortitis [see Warnings and Precautions (5.11)]
- Alveolar hemorrhage
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Although available data with UDENYCA or pegfilgrastim product use in pregnant women are insufficient to establish whether there is a drug associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes, there are available data from published studies in pregnant women exposed to filgrastim products. These studies have not established an association of filgrastim product use during pregnancy with major birth defects, miscarriage, or adverse maternal or fetal outcomes.
In animal studies, no evidence of reproductive/developmental toxicity occurred in the offspring of pregnant rats that received cumulative doses of pegfilgrastim approximately 10 times the recommended human dose (based on body surface area). In pregnant rabbits, increased embryolethality and spontaneous abortions occurred at 4 times the maximum recommended human dose simultaneously with signs of maternal toxicity (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Animal Data
Pregnant rabbits were dosed with pegfilgrastim subcutaneously every other day during the period of organogenesis. At cumulative doses ranging from the approximate human dose to approximately 4 times the recommended human dose (based on body surface area), treated rabbits exhibited decreased maternal food consumption, maternal weight loss, as well as reduced fetal body weights and delayed ossification of the fetal skull; however, no structural anomalies were observed in the offspring from either study. Increased incidences of post-implantation losses and spontaneous abortions (more than half the pregnancies) were observed at cumulative doses approximately 4 times the recommended human dose, which were not seen when pregnant rabbits were exposed to the recommended human dose.
Three studies were conducted in pregnant rats dosed with pegfilgrastim at cumulative doses up to approximately 10 times the recommended human dose at the following stages of gestation: during the period of organogenesis, from mating through the first half of pregnancy, and from the first trimester through delivery and lactation. No evidence of fetal loss or structural malformations was observed in any study. Cumulative doses equivalent to approximately 3 and 10 times the recommended human dose resulted in transient evidence of wavy ribs in fetuses of treated mothers (detected at the end of gestation but no longer present in pups evaluated at the end of lactation).
8.2 Lactation
Risk Summary
There are no data on the presence of pegfilgrastim products in human milk, the effects on the breastfed child, or the effects on milk production. Other filgrastim products are secreted poorly into breast milk, and filgrastim products are not orally absorbed by neonates. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for UDENYCA and any potential adverse effects on the breastfed child from UDENYCA or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of pegfilgrastim have been established in pediatric patients. No overall differences in safety were identified between adult and pediatric patients with pegfilgrastim based on postmarketing surveillance and review of the scientific literature.
Use of pegfilgrastim in pediatric patients for chemotherapy-induced neutropenia is based on adequate and well controlled studies in adults with additional pharmacokinetic and safety data in pediatric patients with sarcoma [see Clinical Pharmacology (12.3) and Clinical Studies (14)].
The use of pegfilgrastim to increase survival in pediatric patients acutely exposed to myelosuppressive doses of radiation is based on efficacy studies conducted in animals and clinical data supporting the use of pegfilgrastim in patients with cancer receiving myelosuppressive chemotherapy. Efficacy studies of pegfilgrastim products could not be conducted in humans with acute radiation syndrome for ethical and feasibility reasons. Results from population modeling and simulation indicate that two doses of pegfilgrastim (Table 1), administered one week apart provide pediatric patients with exposures comparable to that in adults receiving two 6 mg doses one week apart [see Dosage and Administration (2.3), Clinical Pharmacology (12.3) and Clinical Studies (14.2)].
10 OVERDOSAGE
Overdosage of pegfilgrastim products may result in leukocytosis and bone pain. Events of edema, dyspnea, and pleural effusion have been reported in a single patient who administered pegfilgrastim on 8 consecutive days in error. In the event of overdose, the patient should be monitored for adverse reactions [see Adverse Reactions (6)].
11 DESCRIPTION
Pegfilgrastim-cbqv is a covalent conjugate of recombinant methionyl human G-CSF and monomethoxypolyethylene glycol. Recombinant methionyl human G-CSF is a water-soluble, 175 amino acid protein with a molecular weight of approximately 19 kilodaltons (kDa). Recombinant methionyl human G-CSF is obtained from the bacterial fermentation of a strain of E coli transformed with a genetically engineered plasmid containing the human G-CSF gene. During the pegfilgrastim-cbqv manufacturing process, fermentation is carried out in nutrient medium containing the antibiotic kanamycin. However, kanamycin is cleared in the manufacturing process and is not detectable in the final product. To produce pegfilgrastim-cbqv, a 20 kDa monomethoxypolyethylene glycol molecule is covalently bound to the N-terminal methionyl residue of recombinant methionyl human G-CSF. The average molecular weight of pegfilgrastim-cbqv is approximately 39 kDa.
UDENYCA (pegfilgrastim-cbqv) injection is supplied in 0.6 mL prefilled syringes for manual subcutaneous injection. The prefilled syringe does not bear graduation marks and is designed to deliver the entire contents of the syringe (6 mg/0.6 mL).
Each syringe contains 6 mg pegfilgrastim-cbqv (based on protein weight) in a sterile, clear, colorless, preservative-free solution (pH 4.0) containing acetate (0.35 mg), polysorbate 20 (0.02 mg), sodium (0.02 mg), and sorbitol (30 mg) in Water for Injection, USP.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pegfilgrastim products are colony-stimulating factors that act on hematopoietic cells by binding to specific cell surface receptors, thereby stimulating proliferation, differentiation, commitment, and end cell functional activation.
12.2 Pharmacodynamics
Animal data and clinical data in humans suggest a correlation between pegfilgrastim products exposure and the duration of severe neutropenia as a predictor of efficacy. Selection of the dosing regimen of UDENYCA is based on reducing the duration of severe neutropenia.
12.3 Pharmacokinetics
The pharmacokinetics of pegfilgrastim were studied in 379 patients with cancer. The pharmacokinetics of pegfilgrastim were nonlinear, and clearance decreased with increases in dose. Neutrophil receptor binding is an important component of the clearance of pegfilgrastim, and serum clearance is directly related to the number of neutrophils. In addition to numbers of neutrophils, body weight appeared to be a factor. Patients with higher body weights experienced higher systemic exposure to pegfilgrastim after receiving a dose normalized for body weight. A large variability in the pharmacokinetics of pegfilgrastim was observed. The half-life of pegfilgrastim ranged from 15 to 80 hours after subcutaneous injection.
Specific Populations
No gender-related differences were observed in the pharmacokinetics of pegfilgrastim, and no differences were observed in the pharmacokinetics of geriatric patients (≥ 65 years of age) compared with younger patients (< 65 years of age) [see Use in Specific Populations (8.5)].
Renal Impairment
In a study of 30 subjects with varying degrees of renal dysfunction, including end stage renal disease, renal dysfunction had no effect on the pharmacokinetics of pegfilgrastim.
Pediatric Patients with Cancer Receiving Myelosuppressive Chemotherapy
The pharmacokinetics and safety of pegfilgrastim were studied in 37 pediatric patients with sarcoma in Study 4 [see Clinical Studies 14.1]. The mean (± standard deviation [SD]) systemic exposure (AUC0-inf) of pegfilgrastim after subcutaneous administration at 100 mcg/kg was 47.9 (± 22.5) mcg·hr/mL in the youngest age group (0 to 5 years, n = 11), 22.0 (± 13.1) mcg·hr/mL in the 6 to 11 years age group (n = 10), and 29.3 (± 23.2) mcg·hr/mL in the 12 to 21 years age group (n = 13). The terminal elimination half-lives of the corresponding age groups were 30.1 (± 38.2) hours, 20.2 (± 11.3) hours, and 21.2 (± 16.0) hours, respectively.
Patients Acutely Exposed to Myelosuppressive Doses of Radiation
The pharmacokinetics of pegfilgrastim products is not available in patients acutely exposed to myelosuppressive doses of radiation. Based on limited pharmacokinetic data in irradiated non-human primates, the area under the concentration-time curve (AUC), reflecting the exposure to pegfilgrastim in non-human primates following a 300 mcg/kg dose of pegfilgrastim, appears to be greater than in humans receiving a 6 mg dose. Results from population modeling and simulation indicate that two 6 mg doses of pegfilgrastim administered one week apart in adults result in clinically relevant effects on duration of grade 3 and 4 neutropenia. In addition, weight based dosing in pediatric patients weighing less than 45 kg [see Dosage and Administration, Section 2.3, Table 1] provides exposures comparable to those in adults receiving two 6 mg doses one week apart.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or mutagenesis studies have been performed with pegfilgrastim products.
Pegfilgrastim did not affect reproductive performance or fertility in male or female rats at cumulative weekly doses approximately 6 to 9 times higher than the recommended human dose (based on body surface area).
14 CLINICAL STUDIES
14.1 Patients with Cancer Receiving Myelosuppressive Chemotherapy
Pegfilgrastim was evaluated in three randomized, double-blind, controlled studies. Studies 1 and 2 were active- controlled studies that employed doxorubicin 60 mg/m2 and docetaxel 75 mg/m2 administered every 21 days for up to 4 cycles for the treatment of metastatic breast cancer. Study 1 investigated the utility of a fixed dose of pegfilgrastim. Study 2 employed a weight-adjusted dose. In the absence of growth factor support, similar chemotherapy regimens have been reported to result in a 100% incidence of severe neutropenia (ANC < 0.5 x 109/L) with a mean duration of 5 to 7 days and a 30% to 40% incidence of febrile neutropenia. Based on the correlation between the duration of severe neutropenia and the incidence of febrile neutropenia found in studies with filgrastim, duration of severe neutropenia was chosen as the primary endpoint in both studies, and the efficacy of pegfilgrastim was demonstrated by establishing comparability to filgrastim-treated patients in the mean days of severe neutropenia.
In Study 1, 157 patients were randomized to receive a single subcutaneous injection of pegfilgrastim (6 mg) on day 2 of each chemotherapy cycle or daily subcutaneous filgrastim (5 mcg/kg/day) beginning on day 2 of each chemotherapy cycle. In Study 2, 310 patients were randomized to receive a single subcutaneous injection of pegfilgrastim (100 mcg/kg) on day 2 or daily subcutaneous filgrastim (5 mcg/kg/day) beginning on day 2 of each chemotherapy cycle.
Both studies met the major efficacy outcome measure of demonstrating that the mean days of severe neutropenia of pegfilgrastim-treated patients did not exceed that of filgrastim-treated patients by more than 1 day in cycle 1 of chemotherapy. The mean days of cycle 1 severe neutropenia in Study 1 were 1.8 days in the pegfilgrastim arm compared to 1.6 days in the filgrastim arm [difference in means 0.2 (95% CI -0.2, 0.6)] and in Study 2 were 1.7 days in the pegfilgrastim arm compared to 1.6 days in the filgrastim arm [difference in means 0.1 (95% CI -0.2, 0.4)].
A secondary endpoint in both studies was days of severe neutropenia in cycles 2 through 4 with results similar to those for cycle 1.
Study 3 was a randomized, double-blind, placebo-controlled study that employed docetaxel 100 mg/m2 administered every 21 days for up to 4 cycles for the treatment of metastatic or non-metastatic breast cancer. In this study, 928 patients were randomized to receive a single subcutaneous injection of pegfilgrastim (6 mg) or placebo on day 2 of each chemotherapy cycle. Study 3 met the major trial outcome measure of demonstrating that the incidence of febrile neutropenia (defined as temperature ≥ 38.2°C and ANC ≤ 0.5 x109/L) was lower for pegfilgrastim-treated patients as compared to placebo-treated patients (1% versus 17%, respectively, p < 0.001). The incidence of hospitalizations (1% versus 14%) and IV anti-infective use (2% versus 10%) for the treatment of febrile neutropenia was also lower in the pegfilgrastim-treated patients compared to the placebo-treated patients.
Study 4 was a multicenter, randomized, open-label study to evaluate the efficacy, safety, and pharmacokinetics [see Clinical Pharmacology (12.3)] of pegfilgrastim in pediatric and young adult patients with sarcoma. Patients with sarcoma receiving chemotherapy age 0 to 21 years were eligible. Patients were randomized to receive subcutaneous pegfilgrastim as a single dose of 100 mcg/kg (n= 37) or subcutaneous filgrastim at a dose 5 mcg/kg/day (n=6) following myelosuppressive chemotherapy. Recovery of neutrophil counts was similar in the pegfilgrastim and filgrastim groups. The most common adverse reaction reported was bone pain.
14.2 Patients with Hematopoietic Subsyndrome of Acute Radiation Syndrome
Efficacy studies of pegfilgrastim products could not be conducted in humans with acute radiation syndrome for ethical and feasibility reasons. Approval of this indication was based on efficacy studies conducted in animals and data supporting pegfilgrastim's effect on severe neutropenia in patients with cancer receiving myelosuppressive chemotherapy [see Dosage and Administration (2.1)].
The recommended dose of UDENYCA is two doses, 6 mg each, administered one week apart for humans exposed to myelosuppressive doses of radiation. For pediatric patients weighing less than 45 kg, dosing of UDENYCA is weight based and is provided in Table 1 [see Dosage and Administration (2.3)]. This dosing regimen is based on population modeling and simulation analyses. The exposure associated with this dosing regimen is expected to provide sufficient pharmacodynamic activity to treat humans exposed to myelosuppressive doses of radiation [see Clinical Pharmacology (12.3)]. The safety of pegfilgrastim at a dose of 6 mg has been assessed on the basis of clinical experience in patients with cancer receiving myelosuppressive chemotherapy.
The efficacy of pegfilgrastim for the acute radiation syndrome setting was studied in a randomized, placebo- controlled non-human primate model of radiation injury. Rhesus macaques were randomized to either a control (n = 23) or treated (n = 23) cohort. On study day 0, animals (n = 6 to 8 per irradiation day) were exposed to total body irradiation (TBI) of 7.50 ± 0.15 Gy delivered at 0.8 ± 0.03 Gy/min, representing a dose that would be lethal in 50% of animals by 60 days of follow-up (LD50/60). Animals were administered subcutaneous injections of a blinded treatment (control article [5% dextrose in water] or pegfilgrastim [300-319 mcg/kg/day]) on study day 1 and on study day 8. The primary endpoint was survival. Animals received medical management consisting of intravenous fluids, antibiotics, blood transfusions, and other support as required.
Pegfilgrastim significantly (at 0.0014 level of significance) increased 60-day survival in irradiated non-human primates: 91% survival (21/23) in the pegfilgrastim group compared to 48% survival (11/23) in the control group.
16 HOW SUPPLIED/STORAGE AND HANDLING
UDENYCA (pegfilgrastim-cbqv) injection is a clear, colorless, preservative-free solution supplied in a prefilled single-dose syringe with an UltraSafe Passive™ Needle Guard, containing 6mg of pegfilgrastim-cbqv.
The needle cap of the prefilled syringe is not made with natural rubber latex.
UDENYCA is provided in a dispensing pack containing one 6 mg/0.6 mL prefilled syringe (NDC 70114-101-01).
UDENYCA prefilled syringe does not bear graduation marks and is intended only to deliver the entire contents of the syringe (6 mg/0.6 mL) for direct administration. Use of the prefilled syringe is not recommended for direct administration for pediatric patients weighing less than 45 kg who require doses that are less than the full contents of the syringe.
Store refrigerated between 2° to 8°C (36° to 46°F) in the carton to protect from light. Do not shake. Discard syringes stored at room temperature for more than 48 hours. Avoid freezing; if frozen, thaw in the refrigerator before administration. Discard syringe if frozen more than once.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use)
Advise patients of the following risks and potential risks with UDENYCA:
- Splenic rupture and splenomegaly
- Acute Respiratory Distress Syndrome
- Serious allergic reactions
- Sickle cell crisis
- Glomerulonephritis
- Increased risk of Myelodysplastic Syndrome and/or Acute Myeloid Leukemia in patients with breast and lung cancer who receive UDENYCA in conjunction with chemotherapy and/or radiation therapy
- Capillary Leak Syndrome
- Aortitis
Advise patients acutely exposed to myelosuppressive doses of radiation (Hematopoietic Subsyndrome of Acute Radiation Syndrome) that efficacy studies of pegfilgrastim products for this indication could not be conducted in humans for ethical and feasibility reasons and that, therefore, approval of this use was based on efficacy studies conducted in animals [see Clinical Studies (14.2)].
Instruct patients who self-administer UDENYCA using the single-dose prefilled syringe of the:
- Importance of following the Instructions for Use (see Instructions for Use).
- Dangers of reusing syringes.
- Importance of following local requirements for proper disposal of used syringes.
Coherus
BioSciences
UDENYCA® (pegfilgrastim-cbqv)
Manufactured by: Coherus BioSciences, Inc., Redwood City, California 94065-1442
U.S. License No. 2023
© 2021 Coherus BioSciences Inc. All rights reserved.
For more information, go to www.UDENYCA.com or call 1-800-4UDENYCA (1-800-483-3692)
PMD-0004, Rev. 06
| Instructions for Use UDENYCA® (yoo-den-i-kah) (pegfilgrastim-cbqv) Injection Single-Dose Prefilled Syringe |
|
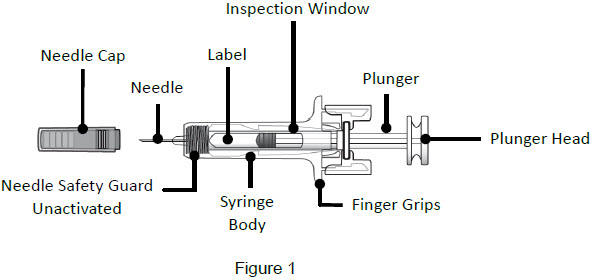
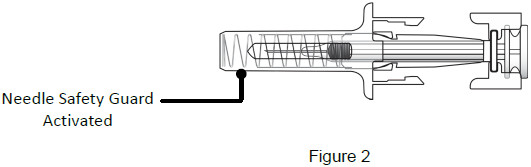
| Guide to Parts | |
| Before Use | |
 |
|
| Important: The needle is covered by a needle cap before use | |
| After Use | |
 |
|
| Important Read the Patient Information for important information you need to know about UDENYCA before using these Instructions for Use. |
|
| Storing the UDENYCA prefilled syringe | |
|  |
| Using the prefilled syringe | |
| |
| Call your healthcare provider if you have any questions. | |
| Prepare the injection | |
| 1 - Remove carton from refrigerator and check expiration date | |
| 1A: Remove the carton from the refrigerator and check the expiration date printed on the carton. (See Figure 3) Do not use if the expiration date has passed. | 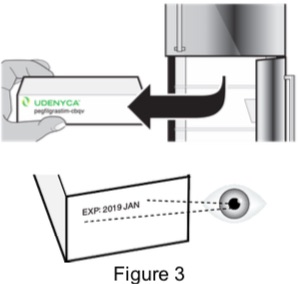 |
| 1B: Open the carton and remove the sealed syringe tray. (See Figure 4) | 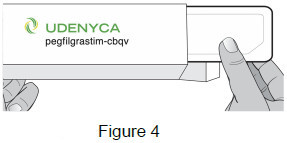 |
| 2 - Allow UDENYCA to reach room temperature and gather supplies | |
| 2A: Place the sealed syringe tray on a flat, clean work surface and allow it to sit at room temperature for at least 30 minutes. (See Figure 5) Do not attempt to warm up the syringe in any other way, such as a microwave, hot water, or direct sunlight. |  |
2B: Gather the following supplies: (See Figure 6)
| 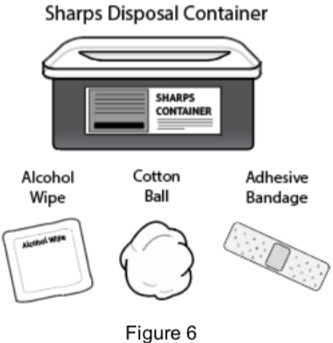 |
| 3 - Wash your hands and remove syringe from tray | |
| 3A: Wash your hands well with soap and warm water. (See Figure 7) | 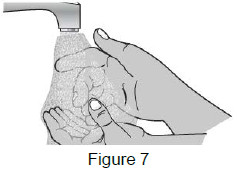 |
| 3B: Open the tray by peeling away the cover. Remove the prefilled syringe from the tray by grasping the middle of the syringe body and carefully pulling it out of the tray. (See Figure 8) For Safety reasons:
| 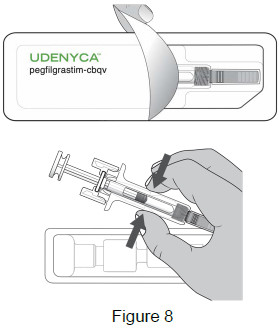 |
| 4 - Inspect the syringe and medicine | |
| Check the medicine through the Inspection Window. The medicine should be clear and colorless. It is normal to see 1 or more air bubbles in the syringe. Removal of the air is not needed. (See Figure 9) Do not use the prefilled syringe if:
| 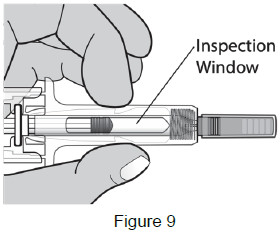 |
| Select and clean injection site | |
| 5 - Select and clean the injection site | |
5A: Select the injection site. The recommended injection sites for a subcutaneous injection are the: (See Figure 10)
If you want to use the same injection site, make sure it is not the same spot on the injection site you used for a previous injection. | 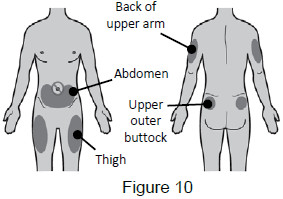 |
| 5B: Clean the injection site with an alcohol wipe.
(See Figure 11) Do not touch this area again before injection. | 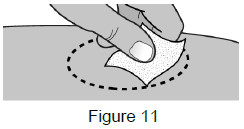 |
| Inject the dose | |
| 6 - Remove needle cap | |
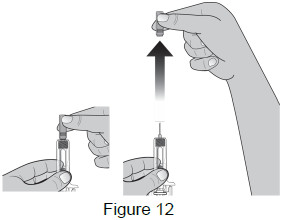
Remove the needle cap by pulling it straight off.
(See Figure 12)
|  |
| 7 – Position fingers | |
Grasp the body of the syringe like a dart (just under the finger grips) with your thumb and index fingers. (See Figure 13)
|  |
| 8 – Pinch the skin and insert the needle | |
| 8A: Use your free hand to gently pinch the cleaned injection site to create a firm surface. (See Figure 14) | 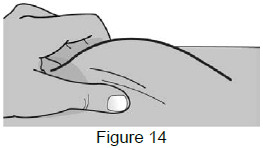 |
8B: Hold the pinch. Insert the needle into the skin at a 45 to 90-degree angle. (See Figure 15)
| 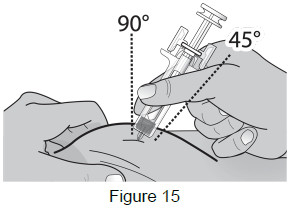 |
| 8C: After fully inserting the needle, release the
pinched skin and use your free hand to stabilize the bottom of the syringe. Then move your other hand into injection position with your thumb on the plunger head. (See Figure 16) | 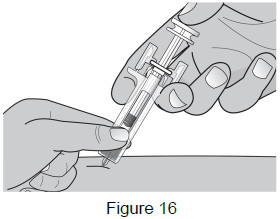 |
| 9 – Push plunger head down to deliver dose | |
| 9A: Using slow and constant pressure, push the plunger head down until it reaches the bottom. This will help to ensure that you receive the full dose. (See Figure 17) | 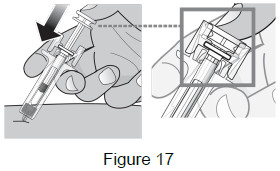 |
| 9B: While the needle is still inserted, slowly move your thumb back, allowing the plunger to rise. This will release the needle safety guard to safely cover the needle. Then remove the syringe from the injection site. (See Figure 18) Important: When you remove the syringe, if it looks like the medicine is still in the syringe, this means you have not received a full dose. Call your healthcare provider right away.
| 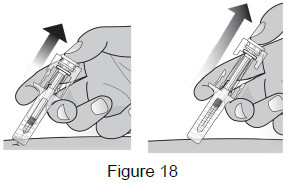 |
| Dispose | |
| 10 – Dispose of used prefilled syringes | |
| Put the used prefilled syringe into an FDA-cleared sharps disposal container right away after use. Do not throw away the syringe in the household trash. (See Figure 19) |  |
|
|
| This Instructions for Use has been approved by the U.S. Food and Drug Administration. | Issued: 09/2019 |
Coherus
BioSciences
UDENYCA® (pegfilgrastim-cbqv)
Manufactured by: Coherus BioSciences, Inc., Redwood City, California 94065-1442
U.S. License No. 2023
© 2019 Coherus BioSciences Inc. All rights reserved.
For more Information go to www.UDENYCA.com or call 1-800-4UDENYCA (1-800-483-3692)
PMD-0005, Rev. 02
| Patient Information
UDENYCA® (yoo-den-i-kah) (pegfilgrastim-cbqv) Injection Single-Dose Prefilled Syringe |
|
| What is UDENYCA?
UDENYCA is a man-made form of granulocyte colony-stimulating factor (G-CSF). G-CSF is a substance produced by the body. It stimulates the growth of neutrophils, a type of white blood cell important in the body’s fight against infection. Acute Radiation Syndrome: The effectiveness of pegfilgrastim for this use was only studied in animals, because it could not be studied in people. |
|
| Do not take UDENYCAif you have had a serious allergic reaction to pegfilgrastim products or filgrastim products. | |
Before you receive UDENYCA, tell your healthcare provider about all of your medical conditions, including if you:
|
|
How will I receive UDENYCA?
|
|
| What are possible side effects of UDENYCA? UDENYCA may cause serious side effects, including:
These are not all the possible side effects of UDENYCA. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store UDENYCA?
|
|
| General information about the safe and effective use of UDENYCA.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use UDENYCA for a condition for which it was not prescribed. Do not give UDENYCA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about UDENYCA that is written for health professionals. |
|
| What are the ingredients in UDENYCA?
Active ingredient: pegfilgrastim-cbqv Inactive ingredients: acetate, polysorbate 20, sodium, and sorbitol in Water for Injection. |
|
| |
|
| Manufactured by: Coherus BioSciences, Inc., Redwood City, California 94065-1442 U.S. License No. 2023 © 2021 Coherus BioSciences Inc. All rights reserved. For more Information go to www.UDENYCA.com or call 1-800-4UDENYCA (1-800-483-3692) PMD-0006 Rev. 05 | Coherus BioSciences |
| This Patient Information has been approved by the U.S. Food and Drug Administration | Revised: 11/2022 |
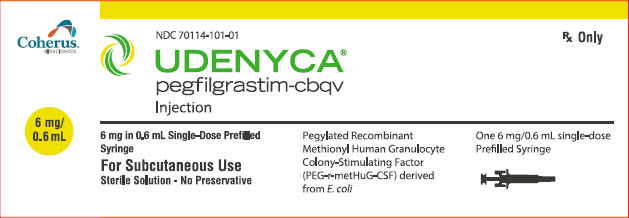
Carton Label - One 6 mg/0.6 mL Single-Dose Prefilled Syringe - UDENYCA
PRINCIPAL DISPLAY PANEL
Coherus
BioSciences
6 mg/
0.6 mL
NDC 70114-101-01
UDENYCA®
pegfilgrastim-cbqv
Injection
Rx Only
6 mg in 0.6 mL Single-Dose Prefilled
Syringe
For Subcutaneous Use
Sterile Solution - No Preservative
Pegylated Recombinant
Methionyl Human Granulocyte
Colony-Stimulating Factor
(PEG-r-metHuG-CSF) derived
from E. coli
One 6 mg/0.6 mL single-dose
Prefilled Syringe
| UDENYCA
pegfilgrastim-cbqv injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Coherus BioSciences Inc (078502849) |
| Registrant - Coherus BioSciences Inc (078502849) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| KBI Biopharma, Inc. | 079582679 | manufacture(70114-101) | |