INFERGEN- interferon alfacon-1 injection
Valeant Pharmaceuticals, Inc.
----------
INFERGEN®
(Interferon alfacon-1)
|
Alpha interferons, including Interferon alfacon-1, cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. |
|
|
Patients should be monitored closely with periodic clinical and laboratory evaluations. Patients with persistently severe or worsening symptoms of these conditions should be withdrawn from therapy. In many but not all cases, these disorders resolve after stopping Interferon alfacon-1 therapy. |
|
|
SeeWARNINGS andADVERSE REACTIONS. |
|
DESCRIPTION
Interferon alfacon-1 is a recombinant non-naturally occurring type-I interferon. The 166-amino acid sequence of Interferon alfacon-1 was derived by scanning the sequences of several natural interferon alpha subtypes and assigning the most frequently observed amino acid in each corresponding position.1 Four additional amino acid changes were made to facilitate the molecular construction, and a corresponding synthetic DNA sequence was constructed using chemical synthesis methodology. Interferon alfacon-1 differs from interferon alfa-2b at 20/166 amino acids (88% homology), and comparison with interferon-beta shows identity at over 30% of the amino acid positions. Interferon alfacon-1 is produced in Escherichia coli (E. coli) cells that have been genetically altered by insertion of a synthetically constructed sequence that codes for Interferon alfacon-1. Prior to final purification, Interferon alfacon-1 is allowed to oxidize to its native state, and its final purity is achieved by sequential passage over a series of chromatography columns. This protein has a molecular weight of 19,434 daltons.
INFERGEN is a sterile, clear, colorless, preservative-free liquid formulated with 100 mM sodium chloride and 27 mM sodium phosphate at pH 7.0 ± 0.2. The product is available in single-use vials containing 9 mcg and 15 mcg Interferon alfacon-1 at a fill volume of 0.3 mL and 0.5 mL, respectively. INFERGEN vials contain 0.03 mg/mL Interferon alfacon-1, 5.9 mg/mL sodium chloride, and 3.8 mg/mL sodium phosphate in Water for Injection, USP. INFERGEN is to be administered undiluted by subcutaneous (SC) injection.
CLINICAL PHARMACOLOGY
General
Interferons are a family of naturally occurring, small protein molecules with molecular weights of 15,000 to 21,000 daltons that are produced and secreted by cells in response to viral infections or to various synthetic and biological inducers. Two major classes of interferons have been identified (i.e., type-I and type-II). Type-I interferons include a family of more than 25 alpha interferons as well as beta interferon and omega interferon. While all alpha interferons have similar biological effects, not all the activities are shared by each alpha interferon and, in many cases, the extent of activity varies substantially for each interferon subtype.
All type-I interferons share common biological activities generated by binding of interferon to the cell-surface receptor, leading to the production of several interferon-stimulated gene products. Type-I interferons induce pleiotropic biologic responses which include antiviral, antiproliferative, and immunomodulatory effects, regulation of cell surface major histocompatibility antigen (HLA class I and class II) expression and regulation of cytokine expression. Examples of interferon-stimulated gene products include 2'5' oligoadenylate synthetase (2'5'OAS) and β-2 microglobulin.
The antiviral, antiproliferative, natural killer (NK) cell activation, and gene-induction activities of INFERGEN have been compared with other recombinant alpha interfereons in in vitro assays and have demonstrated similar ranges of activity. INFERGEN exhibited at least 5 times higher specific activity in vitro than Interferon alfa-2a and Interferon alfa-2b.2 Comparison of INFERGEN with a WHO international potency standard for recombinant alpha interferon (83/514) revealed that the specific activity of INFERGEN in both an in vitro antiviral cytopathic effect assay and an antiproliferative assay was 1 x 109 U/mg. However, correlation between in vitro activity and clinical activity of any interferon is unknown.
Pharmacokinetics and Pharmacodynamics
The pharmacokinetic properties of INFERGEN have not been evaluated in patients with chronic hepatitis C. Pharmacokinetic profiles were evaluated in normal, healthy volunteer subjects after SC injection of 1, 3, or 9 mcg INFERGEN. Plasma levels of INFERGEN after SC administration of any dose were too low to be detected by either enzyme-linked immunosorbent assay (ELISA) or by inhibition of viral cytopathic effect. However, analysis of INFERGEN-induced cellular products (induction of 2'5' OAS and β-2 microglobulin) after treatment in these subjects revealed a statistically significant, dose-related increase in the area under the curve (AUC) for the levels of 2'5' OAS or β-2 microglobulin induced over time (p < 0.001 for all comparisons). Concentrations of 2'5' OAS were maximal at 24 hours after dosing, while serum levels of β-2 microglobulin appeared to reach a maximum 24 to 36 hours after dosing. The dose-response relationships observed for 2'5' OAS and β-2 microglobulin were indicative of biological activity after SC administration of 1 to 9 mcg INFERGEN.
Preclinical Experience
All interferons have been shown to be highly species-specific. Antiviral activity of INFERGEN was observed in the rhesus monkey LLC cell line and golden Syrian hamster BHK cell line. Antiviral activity of INFERGEN in the golden Syrian hamster was confirmed further in vivo.3 Pharmacokinetic studies of INFERGEN in golden Syrian hamsters and rhesus monkeys demonstrated rapid absorption following SC injection. Peak serum concentrations of INFERGEN were observed at 1 hour and 4 hours in golden Syrian hamsters and in rhesus monkeys, respectively. Subcutaneous bioavailability was high in both species, averaging 99% in golden Syrian hamsters and 83% to 104% in rhesus monkeys. Clearance of INFERGEN, averaging 1.99 mL/minute/kg in golden Syrian hamsters and 0.71 to 0.92 mL/minute/kg in rhesus monkeys, was due predominantly to catabolism and excretion by the kidneys. The terminal half-life of INFERGEN following SC dosing was 1.3 hours in golden Syrian hamsters and 3.4 hours in rhesus monkeys. Upon 7-day multiple SC dosing, no accumulation of serum levels was observed in golden Syrian hamsters.
In preclinical toxicology studies in golden Syrian hamsters and rhesus monkeys, administration of INFERGEN at doses of up to 100 mcg/kg/day was associated with decreased body weight, decreased food consumption, and bone marrow suppression. High-dose chronic exposure at doses of 10 to 100 mcg/kg/day (50- to 500-fold higher than the maximum clinical dose given daily) in rhesus monkeys was not tolerated for greater than 1 month, due to the development of vascular leak syndrome.
Reproductive toxicity studies in pregnant rhesus monkeys and golden Syrian hamsters demonstrated an increase in fetal loss in hamsters treated with INFERGEN at doses of > 150 mcg/kg/day and in rhesus monkeys at doses of 3 and 10 mcg/kg/day. The INFERGEN toxicity profile described is consistent with the known toxicity profile of other alpha interferons.4
CLINICAL EXPERIENCE: RESPONSE TO INFERGEN
Initial Treatment
INFERGEN was studied in an open-label dose-escalation study using 3, 6, 9, 12, or 15 mcg administered three times per week (TIW) to patients with compensated liver disease secondary to chronic hepatitis C virus (HCV) infection. The 15 mcg dose was the maximum tolerated dose. All doses demonstrated an acceptable safety profile and preliminary evidence of efficacy.
The efficacy of 3 and 9 mcg doses of INFERGEN in the treatment of chronic HCV infection was examined in a randomized, double-blind clinical trial involving 704 patients previously untreated with alpha interferon.5 Patients were 18 years or older, had compensated liver disease, tested positive for HCV RNA, and had elevated serum alanine aminotransferase (ALT) averaging greater than 1.5 times the upper limit of normal. Staging of chronic liver disease was confirmed by a liver biopsy taken within 1 year prior to enrollment. Other causes of chronic liver disease were ruled out prior to randomization. Notable exclusion criteria were decompensated liver disease, thyroid abnormality, or history of depression.
Efficacy of INFERGEN therapy was assessed on an intent-to-treat basis and was determined by measurement of serum ALT at the end of therapy (24 weeks) and following 24 weeks of observation after the end of treatment (sustained response rate). Serum HCV RNA was also assessed using a research-based quantitative reverse transcriptase polymerase chain reaction (RT-PCR) assay with a lower limit of sensitivity of 100 copies/mL. Liver histology was assessed by comparing the histology activity index (HAI) score6 of a pretreatment biopsy specimen with the HAI score from a specimen obtained 24 weeks after cessation of interferon therapy.
Patients enrolled in the study were randomized to 1 of 3 treatment groups: INFERGEN at a dose of 3 mcg (n = 232), INFERGEN at a dose of 9 mcg (n = 232), or Interferon alfa-2b recombinant (IFN α-2b, Intron® A [Intron® is a registered trademark of the Schering Corporation]) at a dose of 3 million international units (MIU) (approximately 15 mcg) (n = 240). All patients were scheduled to receive their respective interferons SC TIW for 24 weeks (end of treatment). Following treatment, patients were observed for an additional 24 weeks to assess durability of ALT normalization (end of posttreatment observation). In all patients, a complete response was defined as a decrease in serum ALT to, at, or below the upper limit of normal (48 U/L) at the end of the posttreatment observation period, even if ALT normalization had not been observed at the end of treatment. Complete response was dependent on 2 consecutive normal serum ALT values determined 4 weeks apart. Reduction of HCV RNA to less than 100 copies/mL was measured as a secondary efficacy endpoint (2 consecutive measurements).
Sustained response rates by ALT normalization and HCV RNA reductions to below detectable limits for patients who received initial treatment are included in Table 1. Among the INFERGEN treatment groups in this study, the 9 mcg dosage arm demonstrated a similar efficacy profile when compared to the IFN α-2b dosage arm. The 3 mcg INFERGEN dosage arm had lesser efficacy; 3% of patients receiving 3 mcg INFERGEN had sustained reductions in their ALT to within the normal range and 3% had sustained reductions in HCV RNA to below detectable limits.
| End of 24-week | End of Observation | ||||
|---|---|---|---|---|---|
| Treatment | (Sustained Response Rate) | ||||
| INFERGEN | IFN α-2b | INFERGEN | IFN α-2b | ||
| 9 mcg | 3 MIUb | 9 mcg | 3 MIUb | ||
| n = 232 | n = 240 | n = 232 | n = 240 | ||
| a. Cl = Confidence Interval. | |||||
| b. 3 MIU IFN α-2b is equivalent to approximately 15 mcg IFN α-2b. | |||||
|
Normalized ALT |
39% |
35% |
17% |
17% |
|
|
(33%, 46%) |
(29%, 41%) |
(12%, 22%) |
(13%, 22%) |
||
|
HCV RNA |
33% |
25% |
9% |
8% |
|
|
Negative |
(27%, 39%) |
(19%, 31%) |
(6%, 14%) |
(5%, 13%) |
|
In this study, liver biopsies were taken at baseline and at the end of posttreatment observation. Similar improvement in liver histology, assessed by HAI score, was observed in the 9 mcg INFERGEN (68%), 3 mcg INFERGEN (63%), and IFN α-2b (65%) dosage arms.
Subsequent Treatment
Subsequent treatment with 15 mcg of INFERGEN for 24 and 48 weeks was evaluated in an open-label clinical trial in 208 patients who had failed initial therapy for 24 weeks with either 9 mcg INFERGEN or 3 MIU (approximately 15 mcg) IFN α-2b.7 Of these patients, 133/208 had failed to normalize ALT during the initial treatment period. Seventy-five of 208 achieved normal ALT during initial treatment, but experienced relapse (return of abnormal ALT) during posttreatment observation. Patients were assessed for normalization of ALT (ALT response rate) and HCV RNA reduction to less than 100 copies/mL (HCV response rate) at the end of 24 weeks of observation following discontinuation of therapy. Sustained response rates measured by ALT normalization and HCV RNA reductions to below detectable limits for patients who received subsequent treatment with 15 mcg of INFERGEN are included in Table 2.
Patients who received 48 weeks of interferon therapy were more likely to experience a sustained response than were those who received 24 weeks of therapy. Similarly, patients who normalized their serum ALT but subsequently relapsed following initial therapy were more likely to experience a sustained response than those who were refractory to initial therapy.
| All Patients | Prior Nonresponders | Prior Relapsers | |||
|---|---|---|---|---|---|
| 24 Weeks | 48 Weeks | 24 Weeks | 48 Weeks | 24 Weeks | 48 Weeks |
| n =107 | n =101 | n =74 | n =59 | n =33 | n =42 |
| a. Subsequent treatment data are presented for patients initially treated with 9 mcg INFERGEN or 3 MIU IFN α-2b in the initial treatment study; patients initially treated with 3 mcg INFERGEN were excluded from this analysis | |||||
| b. P value = 0.01. | |||||
|
End of Observation | |||||
|
Normalized ALT | |||||
|
13% |
19% |
7% |
7% |
27% |
36% |
|
(7.3%, 21.0%) |
(11.7%, 27.8%) |
(2.2%, 15.1%) |
(1.9%, 16.5%) |
(13.3%, 45.5%) |
(21.6%, 52.0%) |
|
End of Observation | |||||
|
HCV RNA Negative | |||||
|
9% |
22%b |
4% |
12% |
21% |
36% |
|
(4.6%, 16.7%) |
(13.4%, 30.0%) |
(0.9%, 11.5%) |
(4.9%, 22.9%) |
(9.0%, 38.9%) |
(21.6%, 52.0%) |
Serum antibody levels were measured in all patients using both an INFERGEN-binding radioimmunoassay and an IFN α-2b-binding ELISA. A patient was considered to have developed binding antibodies if, using serum samples from 2 consecutive time points, a positive response was detected in either assay. The number of patients developing positive binding antibody responses in either assay was similar in the 9 mcg INFERGEN (11%) and 3 MIU IFN α-2b groups (15%). The titer of neutralizing antibodies to interferon was not measured. Sustained ALT response rates in patients treated with INFERGEN who developed binding antibodies (4/25) were similar to sustained ALT response rates in patients who did not develop detectable antibody titers (40/195). The most frequently observed time to first antibody response was week 16 of interferon treatment. Following cessation of interferon therapy, the number of patients with a positive antibody response declined during posttreatment observation.
INDICATIONS AND USAGE
INFERGEN is indicated for the treatment of chronic HCV infection in patients 18 years of age or older with compensated liver disease who have anti-HCV serum antibodies and/or the presence of HCV RNA. Other causes of hepatitis, such as viral hepatitis B or autoimmune hepatitis, should be ruled out prior to initiation of therapy with INFERGEN. In some patients with chronic HCV infection, INFERGEN normalizes serum ALT, reduces serum HCV RNA concentrations to undetectable quantities (< 100 copies/mL), and improves liver histology.
CONTRAINDICATIONS
INFERGEN is contraindicated in patients with
- known hypersensitivity to alpha interferons or to any component of the product
- decompensated hepatic disease
- autoimmune hepatitis
WARNINGS
Treatment with INFERGEN should be administered under the guidance of a qualified physician, and may lead to moderate-to-severe adverse experiences requiring dose reduction, temporary dose cessation, or discontinuation of further therapy.
Withdrawal from study for adverse events occurred in 7% of patients initially treated with 9 mcg INFERGEN (including 4% due to psychiatric events). Withdrawal from study due to adverse events occurred in 5% of patients subsequently treated with 15 mcg INFERGEN for 24 weeks and 11% of patients subsequently treated with 15 mcg INFERGEN for 48 weeks.
Neuropsychiatric Disorders
Severe psychiatric adverse events may manifest in patients receiving therapy with alpha interferons, including INFERGEN. Depression, suicidal ideation, suicide attempt, and suicide may occur. Other prominent psychiatric adverse events may also occur, including psychosis, aggressive behavior, nervousness, anxiety, emotional lability, abnormal thinking, agitation, apathy and relapse of drug addiction. INFERGEN should be used with extreme caution in patients who report a history of depression. Physicians should monitor all patients for evidence of depression and other psychiatric symptoms. Prior to initiation of INFERGEN therapy, physicians should inform patients of the possible development of depression and patients should be advised to immediately report any sign or symptom of depression and/or suicidal ideation. In severe cases, therapy should be stopped immediately and psychiatric intervention instituted (SeeDOSAGE AND ADMINISTRATION: Dose Reduction).
Bone Marrow Toxicity
Alpha interferons suppress bone marrow function and may result in severe cytopenias including very rare events of aplastic anemia. It is advised that complete blood counts be obtained pretreatment and monitored routinely during therapy. Alpha interferon therapy should be discontinued in patients who develop severe decreases in neutrophil (<0.5 x 109/L) or platelet counts (<50 x 109/L).
Cardiovascular Disorders
Hypertension, tachycardia, palpitation, and tachyarrhythmias have been reported in patients treated with INFERGEN. INFERGEN should be administered with caution to patients with preexisting cardiac disease. Supraventricular arrhythmias, chest pain, and myocardial infarction have been associated with alpha interferon therapies.8
Hypersensitivity
Serious acute hypersensitivity reactions have been reported in rare instances following treatment with alpha interferons. If hypersensitivity reactions occur (e.g., urticaria, angioedema, bronchoconstriction, anaphylaxis), INFERGEN should be discontinued immediately and appropriate medical treatment instituted.
Endocrine Disorders
INFERGEN should be administered with caution to patients with a history of endocrine disorders. Occurrence or aggravation of hyperthyroidism or hypothyroidism have been reported with INFERGEN. Hyperglycemia and diabetes mellitus have also been observed in patients treated with INFERGEN. Patients who develop these conditions during treatment that cannot be controlled with medication should not continue INFERGEN therapy.
Autoimmune Disorders
Development of or exacerbation of autoimmune disorders (e.g., autoimmune thrombocytopenia, idiopathic thrombocytopenic purpura, psoriasis, rheumatoid arthritis) have been reported in patients receiving alpha interferon therapies, including INFERGEN. INFERGEN should not be used in patients with autoimmune hepatitis (seeCONTRAINDICATIONS) and should be used with caution in patients with other autoimmune disorders.
Pulmonary Disorder
Pneumonia and interstitial pneumonitis, some resulting in respiratory failure and/or patient deaths, have been induced or aggravated by alpha interferon therapy, including INFERGEN. Patients who develop persistent or unexplained pulmonary infiltrates or pulmonary function impairment should discontinue treatment with INFERGEN.
Colitis
Hemorrhagic/ischemic colitis, sometimes fatal, has been observed within 12 weeks of alpha interferon therapies and has been reported in patients treated with INFERGEN. INFERGEN treatment should be discontinued immediately in patients who develop signs and symptoms of colitis.
Pancreatitis
Pancreatitis, sometimes fatal, has been observed in patients treated with alpha interferons, including INFERGEN. INFERGEN should be suspended in patients with signs and symptoms suggestive of pancreatitis and discontinued in patients diagnosed with pancreatitis.
Hepatic Exacerbations and Decompensated Hepatic Disease
Chronic hepatitis C patients with cirrhosis may be at risk of hepatic decompensation when treated with alpha interferons, including INFERGEN. During treatment, patients’ clinical status and hepatic function should be closely monitored, and INFERGEN treatment should be immediately discontinued if symptoms of hepatic decompensation, such as jaundice, ascites, coagulopathy, or decreased serum albumin, are observed (seeCONTRAINDICATIONS).
Ophthalmologic Disorders
Decrease or loss of vision, retinopathy including macular edema, retinal artery or vein thrombosis, retinal hemorrhages and cotton wool spots; optic neuritis, and papilledema are induced or aggravated by treatment with INFERGEN or other alpha interferons. All patients should receive an eye examination at baseline. Patients with preexisting ophthalmologic disorders (e.g., diabetic or hypertensive retinopathy) should receive periodic ophthalmologic exams during interferon alpha treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. INFERGEN therapy should be discontinued in patients who develop new or worsening ophthalmologic disorders.
Cerebrovascular Disorders
Ischemic and hemorrhagic cerebrovascular events have been observed in patients treated with interferon alfa-based therapies, including INFERGEN. Events occurred in patients with few or no reported risk factors for stroke, including patients less than 45 years of age. Because these are spontaneous reports, estimates of frequency cannot be made and a causal relationship between interferon alfa-based therapies and these events is difficult to establish.
PRECAUTIONS
General
While fever may be related to the flu-like symptoms reported in patients treated with INFERGEN, when fever occurs, other possible causes of persistent fever should be ruled out.
Bone Marrow Toxicity
INFERGEN should be used cautiously in patients with abnormally low peripheral blood cell counts or who are receiving agents that are known to cause myelosuppression. Transplantation patients or other chronically immunosuppressed patients should receive alpha interferon therapy with caution.
Renal Impairment
Increases in serum creatinine levels, and rarely renal failure, have been observed in patients receiving INFERGEN. INFERGEN has not been studied in patients with renal insufficiency. Patients with impaired renal function should be closely monitored and INFERGEN should be used with caution in patients with renal insufficiency.
Information for Patients
If home use is determined to be desirable by the physician, instructions on appropriate use should be given by a healthcare professional. The patient must be instructed as to the proper dosage and administration. Information included in the MEDICATION GUIDE should be fully reviewed with the patient; it is not a disclosure of all, or possible, adverse effects. The most common adverse reactions occurring with INFERGEN therapy are flu-like symptoms including fatigue, fever, rigors, headache, arthralgia, myalgia, and increased sweating. Non-narcotic analgesics and bedtime administration of INFERGEN may be used to prevent or lessen some of these symptoms.
Additionally, patients must be thoroughly instructed in the importance of proper disposal procedures and cautioned against the reuse of needles, syringes, or re-entry of the drug product. A puncture-resistant container for the disposal of used syringes and needles should be used by the patient and should be disposed of according to the directions provided by the health care provider (seeMEDICATION GUIDE).
Laboratory Tests
Laboratory tests are recommended for all patients on INFERGEN therapy, prior to beginning treatment (baseline), 2 weeks after initiation of therapy, and periodically thereafter during the 24 or 48 weeks of therapy at the discretion of the physician. Following completion of INFERGEN therapy, any abnormal test values should be monitored periodically. The entrance criteria that were used for the clinical study of INFERGEN may be considered as a guideline to acceptable baseline values for initiation of treatment:
- Platelet count ≥ 75 x 109/L
- Hemoglobin concentration ≥ 100 g/L
- ANC ≥ 1500 x 106/L
- Serum creatinine concentration < 180 μmol/L (< 2.0 mg/dL) or creatinine clearance > 0.83 mL/second (> 50 mL/minute)
- Serum albumin concentration ≥ 25 g/L
- Bilirubin within normal limits
- TSH and T4 within normal limits
Neutropenia, thrombocytopenia, hypertriglyceridemia, and thyroid disorders have been reported with administration of INFERGEN (seeADVERSE REACTIONS). Therefore, these laboratory parameters should be monitored closely.
Drug Interactions
No formal drug interaction studies have been conducted with INFERGEN. INFERGEN should be used cautiously in patients who are receiving agents that are known to cause myelosuppression or with agents known to be metabolized via the cytochrome P-450 pathway.9 Patients taking drugs that are metabolized by this pathway should be monitored closely for changes in the therapeutic and/or toxic levels of concomitant drugs.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: No carcinogenicity data for INFERGEN are available in animals or humans.
Mutagenesis: INFERGEN was not mutagenic when tested in several in vitro assays, including the Ames bacterial mutagenicity assay and an in vitro cytogenetic assay in human lymphocytes, either in the presence or absence of metabolic activation.
Impairment of Fertility: INFERGEN at doses as high as 100 mcg/kg did not selectively affect reproductive performance or the development of the offspring when administered SC to male and female golden Syrian hamsters for 70 and 14 days before mating, respectively, and then through mating and to day 7 of pregnancy.
Pregnancy Category C
INFERGEN has been shown to have embryolethal or abortifacient effects in golden Syrian hamsters when given at 135 times the human dose and in cynomolgus and rhesus monkeys when given at 9 to 81 times (based on body surface area) the human dose. There are no adequate and well-controlled studies in pregnant women. INFERGEN should not be used during pregnancy. If a woman becomes pregnant or plans to become pregnant while taking INFERGEN, she should be informed of the potential hazards to the fetus. Males and females treated with INFERGEN should be advised to use effective contraception.
Nursing Mothers
It is not known whether INFERGEN is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised if INFERGEN is administered to a nursing woman. The effect on the nursing neonate of orallyingested INFERGEN in breast milk has not been evaluated.
Pediatric Use
The safety and effectiveness of INFERGEN have not been established in patients below the age of 18 years. INFERGEN therapy is not recommended in pediatric patients.
Geriatric Use
Clinical studies of INFERGEN did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. However, treatment with Interferons, including INFERGEN, is associated with psychiatric, cardiac, and systemic (flu-like) adverse effects. Since decreased hepatic, renal or cardiac function, concomitant disease and the use of other drug therapies in elderly patients may produce adverse reactions of greater severity, caution should be exercised in the use of INFERGEN in this population.
ADVERSE REACTIONS
Adverse experiences that were reported, regardless of attribution to treatment, in at least 5% of patients in the 9 mcg INFERGEN or 3 MIU IFN α-2b groups of the pivotal study are presented in Table 3, listed in decreasing order by the 9 mcg INFERGEN group. The incidence of adverse events is expressed based on the number of patients experiencing each event at least once during treatment or during posttreatment observation.
Most adverse events were mild-to-moderate in severity and abated with cessation of therapy. Flu-like symptoms (i.e., headache, fatigue, fever, rigors, myalgia, sweating increased, and arthralgia) were the most frequently reported treatment-related adverse reactions. Most were short-lived and could be treated symptomatically.
Depression, usually mild-to-moderate in severity, was reported in 26% of patients who received 9 mcg INFERGEN and was the most common adverse event resulting in study drug discontinuation.
In patients who had tolerated previous interferon therapy (9 mcg INFERGEN or 3 MIU IFN α-2b) and failed to normalize ALT, or who had achieved normalization of ALT during the treatment period but who relapsed during the posttreatment observation period, subsequent treatment with 15 mcg TIW of INFERGEN for 24 or 48 weeks was generally tolerated. Adverse experiences of patients receiving subsequent treatment, regardless of attribution to treatment, are reported in Table 3. The higher dose of INFERGEN used in these patients was associated with a greater incidence of leukopenia and granulocytopenia. One or more dose reductions for all causes were required in up to 36% of patients. Patients who do not tolerate initial standard interferon therapy should not receive therapy with 15 mcg TIW of INFERGEN.
| Initial Treatmentb | Subsequent Treatmentb | |||
|---|---|---|---|---|
| INFERGEN | IFN α-2b | INFERGEN | INFERGEN | |
| 9 mcg | 15 mcg | 15 mcg | ||
| (n = 231) | (n = 236) | 24 wks | 48 wks | |
| (n = 165) | (n = 168) | |||
| Body System/Preferred Term | % of Patients | % of Patients | ||
| a. Only events that occurred at a frequency of ≥ 5% in any treatment group are included. Patients can appear more than once in Table 3. Because the 2 studies were conducted at different times with nonidentical patient groups, the adverse events profile for the subsequent treatment study is not directly comparable to the initial treatment study. | ||||
| b. Adverse events reported in patients during treatment or posttreatment observation in the pivotal initial treatment and subsequent treatment studies are listed regardless of attribution to treatment. | ||||
| c. Influenza-like symptoms: presumed viral etiology. | ||||
|
APPLICATION SITE |
||||
|
Injection Site Erythema |
23 |
15 |
17 |
22 |
|
Injection Site Pain |
9 |
3 |
8 |
11 |
|
Injection Site Ecchymosis |
6 |
7 |
5 |
5 |
|
BODY AS A WHOLE |
||||
|
Fatigue |
69 |
67 |
65 |
71 |
|
Fever |
61 |
45 |
58 |
55 |
|
Rigors |
57 |
45 |
62 |
66 |
|
Body Pain |
54 |
45 |
39 |
51 |
|
Influenza-like Symptomsc |
15 |
11 |
8 |
8 |
|
Pain Chest |
13 |
14 |
5 |
9 |
|
Hot Flushes |
13 |
7 |
7 |
4 |
|
Malaise |
11 |
10 |
2 |
5 |
|
Asthenia |
9 |
11 |
10 |
7 |
|
Edema Peripheral |
9 |
8 |
4 |
3 |
|
Access Pain |
8 |
9 |
1 |
1 |
|
Allergic Reaction |
7 |
5 |
3 |
4 |
|
Weight Decrease |
5 |
7 |
5 |
2 |
|
CARDIOVASCULAR |
||||
|
Hypertension |
5 |
3 |
2 |
4 |
|
Palpitation |
3 |
6 |
5 |
2 |
|
CNS/PNS |
||||
|
Headache |
82 |
83 |
78 |
80 |
|
Insomnia |
39 |
30 |
24 |
28 |
|
Dizziness |
22 |
25 |
18 |
25 |
|
Paresthesia |
13 |
10 |
9 |
9 |
|
Hypoesthesia |
10 |
8 |
8 |
10 |
|
Amnesia |
10 |
6 |
2 |
5 |
|
Hypertonia |
7 |
10 |
6 |
6 |
|
Somnolence |
4 |
8 |
6 |
7 |
|
Confusion |
4 |
6 |
4 |
5 |
|
Hyperesthesia |
1 |
1 |
1 |
5 |
|
ENDOCRINE DISORDERS |
||||
|
Thyroid Test Abnormal |
9 |
5 |
4 |
6 |
|
GASTROINTESTINAL |
||||
|
Abdominal Pain |
41 |
40 |
24 |
32 |
|
Nausea |
40 |
36 |
30 |
36 |
|
Diarrhea |
29 |
24 |
24 |
22 |
|
Anorexia |
24 |
17 |
21 |
14 |
|
Dyspepsia |
21 |
18 |
12 |
10 |
|
Vomiting |
12 |
11 |
13 |
11 |
|
Constipation |
9 |
6 |
5 |
6 |
|
Flatulence |
8 |
9 |
6 |
5 |
|
Tooth Ache |
7 |
7 |
3 |
7 |
|
Saliva Decreased |
6 |
7 |
4 |
1 |
|
Hemorrhoids |
6 |
3 |
1 |
2 |
|
Stomatitis Ulcerative |
3 |
4 |
2 |
6 |
|
Gingivitis |
2 |
3 |
1 |
5 |
|
HEARING/VESTIBULAR |
||||
|
Tinnitus |
6 |
4 |
4 |
2 |
|
Earache |
5 |
7 |
5 |
5 |
|
Otitis |
2 |
5 |
1 |
3 |
|
HEMATOLOGIC |
||||
|
Granulocytopenia |
23 |
25 |
42 |
39 |
|
Thrombocytopenia |
19 |
16 |
18 |
18 |
|
Leukopenia |
15 |
13 |
19 |
28 |
|
Lymphadenopathy |
6 |
8 |
4 |
4 |
|
Ecchymosis |
6 |
4 |
4 |
2 |
|
Lymphocytosis |
5 |
7 |
11 |
5 |
|
PT Increased |
3 |
5 |
1 |
0 |
|
Anemia |
2 |
3 |
2 |
6 |
|
LIVER AND BILIARY |
||||
|
Liver Tender |
5 |
3 |
6 |
2 |
|
Hepatomegaly |
3 |
5 |
5 |
2 |
|
METABOLIC/NUTRITION |
||||
|
Hypertriglyceridemia |
6 |
7 |
5 |
5 |
|
MUSCULO-SKELETAL |
||||
|
Myalgia |
58 |
56 |
51 |
55 |
|
Arthralgia |
51 |
44 |
43 |
46 |
|
Back Pain |
42 |
37 |
29 |
23 |
|
Limb Pain |
26 |
25 |
13 |
23 |
|
Skeletal Pain |
14 |
14 |
10 |
12 |
|
Neck Pain |
14 |
13 |
8 |
5 |
|
Musculo-skeletal Disorder |
4 |
4 |
7 |
4 |
|
PSYCHIATRIC DISORDER |
||||
|
Nervousness |
31 |
29 |
16 |
22 |
|
Depression |
26 |
25 |
18 |
19 |
|
Anxiety |
19 |
18 |
9 |
14 |
|
Emotional Lability |
12 |
11 |
6 |
3 |
|
Thinking Abnormal |
8 |
12 |
10 |
20 |
|
Agitation |
6 |
6 |
4 |
4 |
|
Libido Decreased |
5 |
5 |
5 |
4 |
|
Apathy |
2 |
3 |
4 |
5 |
|
REPRODUCTIVE (FEMALE) |
||||
|
Dysmenorrhea |
9 |
9 |
2 |
7 |
|
Vaginitis |
8 |
2 |
5 |
5 |
|
Menstrual Disorder |
6 |
5 |
2 |
5 |
|
Menorrhagia |
3 |
0 |
2 |
5 |
|
Moniliasis Genital |
2 |
6 |
2 |
0 |
|
Breast Mass |
0 |
3 |
0 |
5 |
|
Breast Pain |
0 |
5 |
2 |
0 |
|
RESISTANCE MECHANISM |
||||
|
Infection |
3 |
5 |
2 |
6 |
|
RESPIRATORY |
||||
|
Pharyngitis |
34 |
31 |
17 |
21 |
|
Infection Upper Respiratory |
31 |
34 |
16 |
18 |
|
Cough |
22 |
17 |
12 |
11 |
|
Sinusitis |
17 |
22 |
12 |
16 |
|
Rhinitis |
13 |
16 |
7 |
9 |
|
Respiratory Tract Congestion |
12 |
7 |
4 |
9 |
|
Upper Resp. Tract Congestion |
10 |
14 |
7 |
9 |
|
Epistaxis |
8 |
12 |
6 |
6 |
|
Dyspnea |
7 |
12 |
8 |
7 |
|
Bronchitis |
6 |
6 |
2 |
1 |
|
SKIN AND APPENDAGES |
||||
|
Alopecia |
14 |
25 |
10 |
13 |
|
Pruritus |
14 |
14 |
11 |
10 |
|
Rash |
13 |
15 |
13 |
10 |
|
Sweating Increased |
12 |
11 |
13 |
11 |
|
Erythema |
6 |
6 |
7 |
9 |
|
Skin Dry |
6 |
5 |
2 |
5 |
|
Wound |
4 |
7 |
3 |
4 |
|
SPECIAL SENSES |
||||
|
Taste Perversion |
3 |
6 |
3 |
5 |
|
VISION DISORDERS |
||||
|
Conjunctivitis |
8 |
8 |
4 |
6 |
|
Eye Pain |
5 |
6 |
4 |
2 |
|
Vision Abnormal |
3 |
5 |
5 |
5 |
Laboratory Values
The following laboratory values were found to be affected by therapy with INFERGEN in the 231 patients who received treatment with 9 mcg INFERGEN.
Hemoglobin and Hematocrit: Treatment with INFERGEN was associated with gradual decreases in mean values for hemoglobin and hematocrit, which were 4% and 5% below baseline at the end of treatment. Decreases from baseline of 20% or more in hemoglobin or hematocrit were seen in 1% of patients or less.
White Blood Cells: INFERGEN treatment was associated with decreases in mean values for both total white blood cell (WBC) count and ANC within the first 2 weeks of treatment. By the end of treatment, mean decreases from baseline of 19% for WBCs and 23% for ANC were observed. These effects reversed during the posttreatment observation period. In 2 INFERGEN-treated patients in the phase 3 trial, decreases in ANC to levels below 500 x 106 cells/L were seen. In both cases, the ANC returned to clinically acceptable levels with reduction of the dose of INFERGEN, and these transient decreases in neutrophils were not associated with infections.
Platelets: INFERGEN treatment was associated with alterations in platelet count. Decreases in mean platelet count of 16% compared to baseline were seen by the end of treatment. These decreases were reversed during the posttreatment observation period. Values below normal were common during treatment with 3% of patients developing values less than 50 x 109 cells/L, usually necessitating dose reduction.
Triglycerides: Mean values for serum triglyceride increased shortly after the start of administration of INFERGEN, with increases of 41%, compared with baseline, at the end of the treatment period. Seven percent of the patients developed values which were at least 3 times above pretreatment levels during treatment. This effect was promptly reversed after discontinuation of treatment.
Thyroid Function: INFERGEN treatment was associated with biochemical changes consistent with hypothyroidism including increases in TSH and decreases in T4 mean values. Increases in TSH to greater than 7 mU/L were seen in 10% of 9 mcg INFERGEN-treated patients either during the treatment period or the 24-week posttreatment observation period. Thyroid supplements were instituted in approximately one-third of these patients.
Laboratory Values for Subsequent Treatment: From a database of 165 patients receiving subsequent treatment with 15 mcg of INFERGEN for 24 weeks, and 168 patients receiving subsequent treatment with 15 mcg of INFERGEN for 48 weeks after failing initial interferon therapy, similar changes in the laboratory values as outlined above were observed. Mean decreases from baseline up to 23% for WBCs and up to 27% for ANC were observed for patients subsequently treated with interferon, which was greater than during initial treatment. Two patients in the 24-week group experienced reversible reductions in ANC to less than 500 x 106 cells/L, which were not associated with infectious complications. No patients discontinued as a result of hematologic toxicity.
Postmarketing Experience
In addition, the following potential adverse reactions have been reported during post-approval use of INFERGEN. Because the reports of these adverse events are voluntary and the population of uncertain size, it is not possible to reliably estimate the frequency of the reaction or establish a causal relationship to drug exposure.
Application site: injection site reaction, including injection site necrosis ulcer, and bruising; Ear and Labyrinth: hearing loss, hearing impairment; Gastrointestinal: abdominal distention, gastrointestinal bleeding, gastritis; Hepatobiliary: hepatic enzyme elevations, including ALT and AST elevation, abnormal hepatic function, hyperbilirubinemia, jaundice, ascites, hepatic encephalopathy; Infections: sepsis; Metabolism and Nutritional: dehydration; Musculoskeletal: rhabdomyolysis, arthritis, bone pain; Nervous: speech disorder, ataxia, gait abnormal, convulsions, loss of consciousness, memory impairment, tremors, visual field defect; Psychiatric: delusions, hallucinations; Skin and Subcutaneous: bruising, pyoderma gangrenosum, toxic epidermal necrolysis; Vascular Disorders: hemorrhage
OVERDOSAGE
In INFERGEN trials, the maximum overdose reported was a dose of 150 mcg INFERGEN administered SC in a patient enrolled in a phase 1 advanced malignancy trial. The patient received 10 times the prescribed dosage for 3 days. The patient experienced a mild increase in anorexia, chills, fever, and myalgia. Increases in ALT (15 to 127 IU/L), aspartate transaminase (AST) (15 to 164 IU/L), and lactic dehydrogenase (LDH) (183 to 281 IU/L) were reported. These laboratory values returned to normal or to the patient’s baseline values within 30 days.
DOSAGE AND ADMINISTRATION
The recommended dose of INFERGEN for treatment of chronic HCV infection is 9 mcg TIW administered SC as a single injection for 24 weeks. At least 48 hours should elapse between doses of INFERGEN. (Seeillustrated MEDICATION GUIDE for instructions.)
Patients who tolerated previous interferon therapy and did not respond or relapsed following its discontinuation may be subsequently treated with 15 mcg of INFERGEN TIW administered SC as a single injection for up to 48 weeks. (Seeillustrated MEDICATION GUIDE for instructions.)
There are significant differences in specific activities among interferons. Healthcare providers should be aware that changes in interferon brand may require adjustments of dosage and/or change in route of administration. Patients should be warned not to change brands of interferon without medical consultation. Patients should also be instructed by their physician not to reduce the dosage of INFERGEN prior to medical consultation.
Dose Reduction
For patients who experience a severe adverse reaction on INFERGEN, dosage should be withheld temporarily. If the adverse reaction does not become tolerable, therapy should be discontinued. Dose reduction to 7.5 mcg may be necessary following an intolerable adverse event. In the pivotal study, 11% of patients (26/231) who initially received INFERGEN at a dose of 9 mcg (0.3 mL) were dose-reduced to 7.5 mcg (0.25 mL).
If adverse reactions continue to occur at the reduced dosage, the physician may discontinue treatment or reduce dosage further. However, decreased efficacy may result from continued treatment at dosages below 7.5 mcg.
During subsequent treatment for 48 weeks with 15 mcg of INFERGEN, up to 36% of patients required dose reductions in 3 mcg increments.
Administration of INFERGEN
If home use is determined to be desirable by the physician, instructions on appropriate use should be given by a healthcare professional. After administration of INFERGEN, it is essential to follow the procedure for proper disposal of syringes and needles. See theMEDICATION GUIDE for detailed instructions.
HOW SUPPLIED
Use only 1 dose per vial; do not re-enter the vial. Discard unused portions. Do not save unused drug for later administration.
Single-dose, preservative-free vials containing 9 mcg (0.3 mL) of Interferon alfacon-1 are available in dispensing packs of 6 vials (NDC 0187-2007-06).
Single-dose, preservative-free vials containing 15 mcg (0.5 mL) of Interferon alfacon-1 are available in dispensing packs of 6 vials (NDC 0187-2006-05).
INFERGEN should be stored in the refrigerator at 2° to 8°C (36° to 46°F). Do not freeze. Avoid vigorous shaking and exposure to direct sunlight.
REFERENCES
- Alton K, Stabinsky Y, Richards R, et al. Production, characterization and biological effects of recombinant DNA derived human IFN-α and IFN-γ analogs. In: De Maeyer E, Schellekens H, eds. The Biology of the Interferon System 1983. Elsevier Science Publishers: Amsterdam. 1983;119-128.
- Blatt LM, Davis J, Klein SB, Taylor MW. The biologic activity and molecular characterization of a novel synthetic interferon-alpha species, consensus interferon. J Interferon Cytokine Res. 1996;16:489-499.
- Fish EN, Banerjee K, Levine HL, Stebbing N. Antiherpetic effects of a human alpha interferon analog, IFN-alpha Con1, in hamsters. Antimicrob Agents Chemother. 1986;30:52-56.
- Trown PW, Willis RJ, Kamm JJ. The preclinical development of Roferon®-A. Cancer. 1986;57 (8 Suppl.):1648-1656.
- Tong MJ, Reddy KR, Lee WM, Consensus Interferon Study Group, et al. Treatment of chronic hepatitis C with consensus interferon: a multicenter, randomized, controlled trial. Hepatology. 1997;26:747-754.
- Knodell RG, Ishak KG, Black WC, et al. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981;1:431-435.
- Heathcote E, Keeffe E, Lee S, et al. Retreatment of chronic hepatitis C with consensus interferon. Hepatology. 1998;27:1136-1143.
- Vial T, Descotes J. Clinical toxicity of interferons. Drug Safety. 1994;10: 115-150.
- Horsmans Y, Brenard R, Geubel AP. Short report: interferon-α decreases 14C- aminopyrine breath test values in patients with chronic hepatitis C. Aliment Pharmacol Ther. 1994;8:353-355.
This product and its use are covered by the following US Patent Nos.: 5,372,808; 5,541,293; 5,980,884.
U.S. License number 1735
MEDICATION GUIDE
INFERGEN®
(Interferon alfacon-1)
Suspension for Injection
Read this Medication Guide carefully before you start taking Infergen (In'-fer-jen). Read the Medication Guide each time you refill your prescription because new information may have been added. You should also make sure that the pharmacist has given you the interferon your healthcare provider prescribed for you. The information in this Medication Guide does not take the place of talking with your healthcare provider about your medical condition or treatment.
What is the most important information I should know about Infergen?
Infergen is one of the treatments used for some people who are infected with the hepatitis C virus (HCV). Infergen can have serious side effects that, in a few people, may lead to death. Before starting treatment, talk to your healthcare provider about the possible benefits of Infergen and its possible side effects to decide if Infergen is right for you. While taking Infergen, you will need to see your healthcare provider regularly for medical exams and lab tests to make sure your treatment is working and to check for side effects.
The most serious possible side effects of Infergen include:
Mental health problems: Infergen may cause mood or behavior problems. Some of the signs of these problems include irritability (getting upset easily), depression (feeling hopeless or feeling bad about yourself), nervousness, anxiety, or aggressive behavior. Some patients may have thoughts of hurting or killing themselves or other people or may attempt to do so.
Tell your healthcare provider if you are being treated for a mental illness or had treatment in the past for any mental illness, including depression and suicidal thoughts. Former drug addicts may lapse back into drug addiction or overdose. You should tell your healthcare provider if you have ever been addicted to drugs or alcohol.
Blood problems (bone marrow toxicity): Infergen can cause a drop in the numbers of two types of blood cells (white blood cells and platelets). Infections and bleeding can happen if these blood counts fall to dangerously low levels.
Heart problems: Infergen may cause high blood pressure, a very fast heart beat, chest pains, and a heart attack. Patients who have heart problems may have a higher chance for heart problems with Infergen. Tell your healthcare provider if you have or have had any heart problems.
Autoimmune problems: These are diseases that happen when the body’s own immune system begins to attack itself Infergen may cause autoimmune disorders such as psoriasis or thyroid problems. Infergen may worsen an autoimmune disease that you already have.
Body organ problems: Infergen may cause problems with your lungs (such as trouble breathing or pneumonia), and stomach pains, nausea and vomiting, and eye problems that can cause blurred vision or cause you to lose your vision.
Call your healthcare provider right away if you develop any of the following:
- depression or have thoughts about hurting or killing yourself or others
- trouble breathing
- severe chest pain
- severe stomach or lower back pain, bloody diarrhea or bloody bowel movements
- poor eyesight
- skin turns yellow
- become pregnant
- a high fever
- unusual easy bruising, or bleeding
For other possible side effects, please read the section “What are the possible side effects of Infergen?” in this Medication Guide (below).
What is Infergen?
Infergen (Interferon alfacon-1) is a medicine used to treat adults with lasting (chronic) hepatitis C virus (HCV) infection. HCV is a liver disease that is caused by the hepatitis C virus and is spread by contact with the blood of a person carrying the hepatitis C virus. Most people who get HCV carry the virus in their blood for the rest of their lives. Most of these people will have some liver damage, but many do not feel sick from the disease. Some people will develop a badly damaged or scarred liver (cirrhosis). Cirrhosis can cause the liver to stop working.
Your healthcare provider will tell you if the hepatitis C virus you have is resistant (type 1 virus) or easier to treat (type 2 or 3 virus) and the chance of treatments working. Infergen may lower the amount of the hepatitis C virus in the body so that it cannot be measured by blood tests. Your healthcare provider should do regular blood tests to check for side effects and your response to treatment.
It is not known if Infergen can cure HCV (permanently get rid of the virus) or if it can prevent liver failure or liver cancer that is caused by HCV infection.
Infergen therapy alone or in combination with other treatments will not prevent a person with HCV from giving another person the HCV infection.
Who should not take Infergen?
Do not take Infergen if you:
- are pregnant or breast feeding or planning to become pregnant
- have autoimmune hepatitis (hepatitis caused by your immune system attacking your liver)
- had an allergic reaction to another alpha-interferon medicine or are allergic to any of the ingredients in Infergen (See the ingredient listing at the end of this Medication Guide)
Before starting Infergen, tell your healthcare provider if you have or ever had any of the following conditions or serious medical problems:
- depression or anxiety
- sleep problems
- drug or alcohol addiction or abuse
- high blood pressure
- heart problems
- liver problems (other than HCV)
- autoimmune disease such as psoriasis, systemic lupus erythematosus, or rheumatoid arthritis
- thyroid problems
- diabetes
- colitis (an inflammation of the bowels)
- cancer
- hepatitis B infection
- HIV infection
- kidney problems
- blood disorders
- taking a medication that suppresses your immune system
Tell your healthcare provider about all the medicines you take including prescription or non-prescription medicines, vitamin and mineral supplements and herbal medicines.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine.
How should I take Infergen?
See the instructions for injecting Infergen (“How do I prepare and inject the Infergen dose?”) later in this Medication Guide.
- Infergen is given as an injection under your skin. Your healthcare provider will inject your Infergen when you first start using it. Your healthcare provider will decide if you, a family member, or a friend is able to inject your Infergen at home. Your healthcare provider will teach you or the person that will be giving your injections, the right way to prepare and inject Infergen. Make sure you understand the instructions before you inject Infergen at home.
- Infergen comes in ready-to-use vials. There is one dose of medicine in each vial. Your healthcare provider will tell you the amount (your dose) to inject. Do not change your dose unless your healthcare provider tells you to change it. It is important that you take Infergen exactly as your healthcare provider tells you. Too little Infergen may not be effective in treating your HCV infection and too much Infergen may cause side effects.
- Inject your dose of Infergen three times a week, at the same time of day.
- If you miss a dose of Infergen, give yourself an injection as soon as you remember and then call your healthcare provider. Do not take your next scheduled dose until you have been told what you should do by your healthcare provider.
- If you take more than your prescribed amount of Infergen, call your healthcare provider right away. Your healthcare provider may want to examine you.
- Once you start treatment with Infergen, do not switch to another brand of interferon without talking to your healthcare provider. Other interferons may not have the same effect on the treatment of your disease. Switching brands will also require a change in your dose.
You must get regular blood tests to help your healthcare provider check to see how the treatment is working and to check for side effects.
What should I avoid while taking Infergen?
- Avoid becoming pregnant while taking Infergen. Infergen may cause harm to an unborn child or cause you to lose your baby (miscarry).
- Do not breastfeed your baby while taking Infergen.
What are the possible side effects of Infergen?
Infergen can cause serious side effects including:
- mental health problems
- blood problems
- heart problems
- autoimmune problems
See “What is the most important information I should know about Infergen?”
Infergen can cause serious allergic reactions. Stop Infergen and get medical treatment right away if you have:
- hives
- swelling around your eyes or lips
- swelling in your mouth or throat
- trouble breathing
Some of the common but less serious side effects with Infergen include:
- Flu-like symptoms. Infergen causes “flu-like” symptoms in most patients. Symptoms include headache, muscle aches, tiredness, chills and fever that usually lessen after the first few weeks of therapy. If you inject your Infergen dose at bedtime, you may be able to sleep through the symptoms. You may also take a fever and pain reducer such as acetaminophen or ibuprofen, to help relieve or reduce the flu-like symptoms.
- Tiredness (fatigue). Infergen causes extreme tiredness in many patients.
- Upset stomach. Nausea, loss of appetite, diarrhea and weight loss may happen.
- Blood sugar problems. Infergen may affect blood sugar levels and cause high blood sugar or diabetes.
- Skin reactions at the injection site. Redness, rash, itching, a lump, swelling, or bruising that does not go away may happen at the site of injection. Call your healthcare provider if these symptoms do not go away after several days.
- Hair thinning. Hair thinning may happen during Infergen treatment, but hair loss stops and hair growth returns after you stop taking Infergen.
These are not all of the side effects of Infergen. Your healthcare provider or pharmacist can give you a more complete list that has all the side effects.
If you are worried about side effects or find them troublesome, talk to your healthcare provider.
HOW DO I PREPARE AND INJECT THE INFERGEN DOSE?
Find a clean, comfortable, well-lit place and remove a vial of Infergen from the refrigerator and allow it to reach room temperature.
1. Assemble the supplies you will need for your injection:
- A vial of Infergen
- One sterile disposable syringe and needle
- Several alcohol swabs and
- A puncture-proof container to dispose of the needle and syringe when you are done
2. Make sure you have the right syringe to use with Infergen. It is important to use a syringe that is marked in tenths of millimeters (mLs), for example, 0.1 mL. Your healthcare provider may refer to a mL as a cc (1 mL = 1 cc). Failure to use the right syringe can lead to a mistake in dosage. You may receive too little or too much Infergen.
3. Check the date on the vial of Infergen and make sure that the date has not passed and look at the liquid inside the vial.
- Do not use the Infergen if:
- The liquid is cloudy
- The liquid is not clear and colorless
- The liquid has particles
- The expiration date has passed
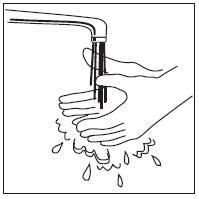
4. Wash your hands thoroughly with soap and water.
SELECT AND PREPARE THE INJECTION SITE ON YOUR BODY
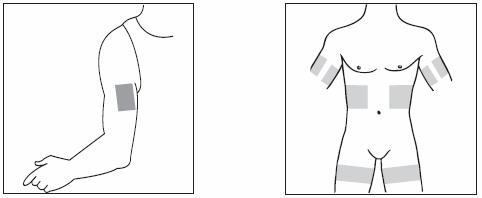
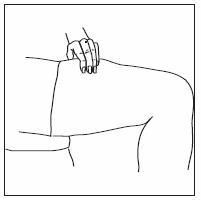
5. Pick a site for your injection.
- Back of the upper arms (if someone is giving you the injection)
- Upper stomach area (abdomen), except for the belly button (navel) and waist areas
- Upper thighs
You should change the site for injection each time you inject to avoid soreness at any one site.
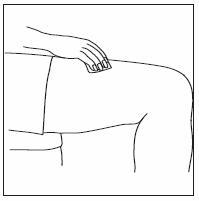
6. Clean the injection site with an alcohol swab. Use circular motions from the inside to the outside. Keep the used alcohol swab nearby.
PREPARING THE DOSE
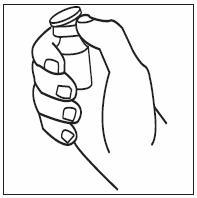
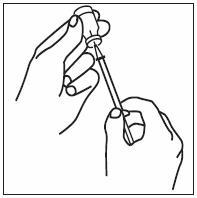
7. Remove the colored cap from the vial, exposing the rubber stopper.
8. Clean the rubber stopper with a new alcohol swab, and then cover the stopper with the swab.
9. Remove the syringe and needle from their packages. If either package looks like there have been opened or damaged, do not use the syringe or needle; dispose of it in the puncture-proof disposal container.
10. Remove the needle cover and pull the plunger back and draw air into the syringe. The amount of air you draw into the syringe should be the same amount as the dose of medicine your healthcare provider has prescribed.
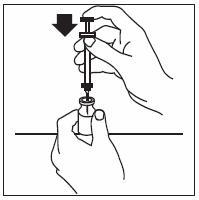
11. Remove the alcohol wipe from the top of the vial and insert the needle straight through the center of the rubber stopper.
12. Push the plunger of the syringe down to inject the air into the air space above the liquid in the vial. The air injected into the vial will allow Infergen to be easily withdrawn from the vial into the syringe.
13. Keeping the needle in the vial, turn the vial upside down and make sure that the tip of the needle is in the liquid.
14. Slowly pull the plunger back and let the medicine enter the syringe, filling it to the line that equals the dose your healthcare provider prescribed.
15. Keeping the needle in the vial, check for air bubbles in the syringe. Air bubbles are harmless but can reduce the dose you should be receiving. To remove the air bubbles, gently tap the syringe with your fingers until the bubbles rise to the needle-end of the syringe barrel. Then push the plunger in to force the air out of the syringe.
Make sure the tip of the needle is in the liquid and slowly pull back on the plunger until the liquid in the syringe reaches the mark that correctly matches the amount of your dose.
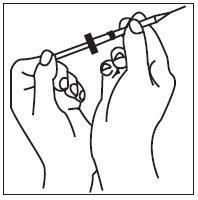
16. Take the needle out of the vial and hold the syringe needle facing up in the hand that you will use to inject yourself. Do not lay the syringe down or allow the needle to touch anything.
INJECTING THE DOSE
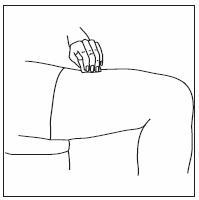
17. Use the other hand to pinch a fold of skin at the site you cleaned for an injection.
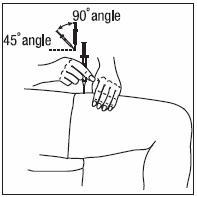
18. Hold the syringe the way you would hold a pencil and insert the needle either straight up and down (90 degree angle) or at a slight angle (45 degree angle) to the skin.
19. After the needle is in, let go of the skin. Pull the plunger back slightly. If blood appears, do not inject Infergen, because the needle has entered a blood vessel. Withdraw the syringe and discard it. Prepare a new syringe and inject at a new site. Repeat this procedure at the second site, checking for blood before injecting.
20. If no blood appears, slowly push down on the plunger all the way, until all the medicine is gone from the syringe.
21. Pull the needle out of the skin at the same angle you put it in and place an alcohol swab over the injection site, then press for several seconds.
22. Promptly place the needle and syringe in the puncture-proof disposal container. Never reuse the syringe or needle. Do not recap the needle.
Disposal
Dispose of syringes and needles as directed by your healthcare provider or pharmacist. There may be special state and local laws.
Place all used needles, needle covers, and syringes in a special container called a “Sharps Container” or a hard plastic container‚ or a metal container with a plastic lid. Do not use glass or clear plastic containers‚ or any container that will allow the needles to stick through them.
Always keep the container out of the reach of children.
Do not recycle containers or throw full containers into the household trash.
How should I store Infergen?
- Store Infergen in the refrigerator at 36° to 46°F (2° to 8°C)‚ but not in the freezer compartment.
- Do not let Infergen freeze or leave it in direct sunlight.
- Do not use a vial of Infergen that has been frozen or past the expiration date stamped on the label. If you think that the Infergen has been frozen or left in direct sunlight‚ do not use it‚ and call your healthcare provider or nurse for instructions.
- To transport Infergen‚ keep the vials cool and avoid extreme temperature changes.
- Do not shake Infergen. If Infergen is shaken too hard, it will not work properly.
- Keep Infergen and all medicines out of the reach of children.
General advice about prescription medicines
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. If you have any concerns about Infergen, ask your healthcare provider. Your healthcare provider or pharmacist can give you information about Infergen that was written for healthcare professionals. Do not use Infergen for a condition for which it was not prescribed. Do not share this medicine with other people.
Ingredients
Interferon alfacon-1 in a sterile, preservative-free solution of sodium chloride, sodium phosphate, and Water for Injection, USP.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Valeant Pharmaceuticals North America
One Enterprise, Aliso Viejo, CA 92656 U.S.A.
(800) 548-5100
3265704
08/02/07
| INFERGEN
interferon alfacon-1 injection |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Valeant Pharmaceuticals, Inc. (042230623) |