Label: LIDOCAINE HYDROCHLORIDE solution
- NDC Code(s): 63739-997-64
- Packager: McKesson Corporation dba SKY Packaging
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated December 10, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
DESCRIPTION
Lidocaine Hydrochloride Topical Solution USP, 4% contains a local anesthetic agent and is administered topically. See INDICATIONS for specific uses.
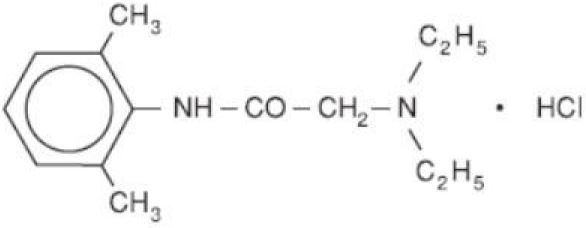
Lidocaine Hydrochloride Topical Solution USP, 4% contains lidocaine HCl, which is chemically designated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl)-, monohydrochloride and has the following structural formula:
The 50 mL screw-cap bottle should not be autoclaved, because the closure employed cannot withstand autoclaving temperatures and pressures. Composition of Lidocaine Hydrochloride Topical Solution USP, 4%: Each mL contains lidocaine HCl, 40 mg, methylparaben, purified water, and sodium hydroxide to adjust pH to 6.0-7.0.
An aqueous solution. NOT FOR INJECTION.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Lidocaine HCl stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action.
Hemodynamics
Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. These changes may be attributable to a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system.
Pharmacokinetics and Metabolism
Lidocaine HCl may be absorbed following topical administration to mucous membranes, its rate of absorption and percent of dose absorbed depending upon concentration and total dose administered, the specific site of application and duration of exposure. In general, the rate of absorption of local anesthetic agents following topical application occurs most rapidly after intratracheal administration. Lidocaine HCl is well-absorbed from the gastrointestinal tract, but little intact drug appears in the circulation because of biotransformation in the liver.
Lidocaine HCl is metabolized rapidly by the liver, and metabolites and unchanged drug are excreted by the kidney. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine HCl. Approximately 90% of lidocaine HCl administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged. The primary metabolite in urine is a conjugate of 4-hydroxy-2,6-dimethylaniline.
The plasma binding of lidocaine HCl is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg of free base per mL, 60 to 80 percent of lidocaine HCl is protein bound. Binding is also dependent on the plasma concentration of the alpha-1-acid glycoprotein.
Lidocaine HCl crosses the blood-brain and placental barriers, presumably by passive diffusion.
Studies of lidocaine HCl metabolism following intravenous bolus injections have shown that the elimination half-life of this agent is typically 1.5 to 2 hours. Because of the rapid rate at which lidocaine HCl is metabolized, any condition that affects liver function may alter lidocaine HCl kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction. Renal dysfunction does not affect lidocaine HCl kinetics but may increase the accumulation of metabolites.
Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine HCl required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6 mcg free base per mL. In the rhesus monkey arterial blood levels of 18 to 21 mcg/mL have been shown to be threshold for convulsive activity.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
-
WARNINGS
IN ORDER TO MANAGE POSSIBLE ADVERSE REACTIONS, RESUSCITATIVE EQUIPMENT, OXYGEN AND OTHER RESUSCITATIVE DRUGS MUST BE IMMEDIATELY AVAILABLE WHEN LOCAL ANESTHETIC AGENTS, SUCH AS LIDOCAINE HCl, ARE ADMINISTERED TO MUCOUS MEMBRANES.
Lidocaine Hydrochloride Topical Solution, 4% should be used with extreme caution if there is sepsis or severely traumatized mucosa in the area of application, since under such conditions there is the potential for rapid systemic absorption.
Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs and symptoms of methemoglobinemia may occur immediately or may be delayed some hours after exposure, and are characterized by a cyanotic skin discoloration and abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue Lidocaine Hydrochloride Topical Solution, 4% and any other oxidizing agents. Depending on the severity of the symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. More severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
-
PRECAUTIONS
General
The safety and effectiveness of lidocaine HCl depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Resuscitative equipment, oxygen, and other resuscitative drugs should be available for immediate use (see WARNINGS and ADVERSE REACTIONS). The lowest dosage that results in effective anesthesia should be used to avoid high plasma levels and serious adverse effects. Repeated doses of lidocaine HCl may cause significant increases in blood levels with each repeated dose because of slow accumulation of the drug or its metabolites. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients, acutely ill patients, and children should be given reduced doses commensurate with their age and physical status. Lidocaine HCl should also be used with caution in patients with severe shock or heart block.
Lidocaine Hydrochloride Topical Solution, 4% should be used with caution in patients with known drug sensitivities. Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine HCl.
Although it has been shown that the rate of absorption of lidocaine HCl after spraying the laryngotracheal mucosa with a solution of the local anesthetic agent is normally relatively slow, there is the attendant risk that occasionally some of the solution may gravitate into the lower respiratory tract where surface area for absorption and tissue blood flow are markedly greater. This can result in unexpectedly rapid and high blood levels, and this possibility must be kept in mind whenever Lidocaine Hydrochloride Topical Solution, 4% is administered.
Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Since it is not known whether amide-type local anesthetics may trigger this reaction and since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for management should be available. Early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the suspect triggering agent(s) and institution of treatment, including oxygen therapy, indicated supportive measures and dantrolene (consult dantrolene sodium intravenous package insert before using).
Information for Patients
When topical anesthetics are used in the mouth, the patient should be aware that the production of topical anesthesia may impair swallowing and thus enhance the danger of aspiration. For this reason, food should not be ingested for 60 minutes following use of local anesthetic preparations in the mouth or throat area. This is particularly important in children because of their frequency of eating.
Numbness of the tongue or buccal mucosa may enhance the danger of unintentional biting trauma. Food and chewing gum should not be taken while the mouth or throat area is anesthetized.
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.
Drug Interactions
Patients that are administered local anesthetics may be at increased risk of developing methemoglobinemia when concurrently exposed to the following oxidizing agents:
Nitrates/Nitrites nitroglycerin, nitroprusside, nitric oxide, nitrous oxide Local anesthetics benzocaine, lidocaine, bupivacaine, mepivacaine, tetracaine, prilocaine, procaine, articaine Antineoplastic agents cyclophosphamide, flutamide, rasburicase, ifosfamide, hydroxyurea Antibiotics dapsone, sulfonamides, nitrofurantoin, para-aminosalicylic acid Antimalarials chloroquine, primaquine Anticonvulsants phenytoin, sodium valproate, phenobarbital Other drugs acetaminophen, metoclopramide, sulfa drugs (i.e., sulfasalazine), quinine Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies of lidocaine HCl in animals to evaluate the carcinogenic and mutagenic potential or the effect on fertility have not been conducted.
Use in Pregnancy
Pregnancy Category B. Reproduction studies have been performed in rats at doses up to 6.6 times the human dose and have revealed no evidence of harm to the fetus caused by lidocaine HCl. There are, however, no adequate and well-controlled studies in pregnant women. Animal reproduction studies are not always predictive of human response. General consideration should be given to this fact before administering lidocaine HCl to women of childbearing potential, especially during early pregnancy when maximum organogenesis takes place.
Labor and Delivery
Lidocaine HCl is not contraindicated in labor and delivery. Should Lidocaine Hydrochloride Topical Solution, 4% be used concomitantly with other products containing lidocaine HCl, the total dose being administered must be kept in mind.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when lidocaine HCl is administered to a nursing woman.
Pediatric Use
Dosages in children should be reduced, commensurate with age, body weight and physical condition (see DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
Adverse experiences following the administration of lidocaine HCl are similar in nature to those observed with other amide local anesthetic agents. These adverse experiences are, in general, doserelated and may result from high plasma levels caused by excessive dosage or rapid absorption, or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported:
Central Nervous System
CNS manifestations are excitatory and/or depressant and may be characterized by lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory manifestations may be very brief or may not occur at all, in which case the first manifestation of toxicity may be drowsiness merging into unconsciousness and respiratory arrest.
Drowsiness following the administration of lidocaine HCl is usually an early sign of a high blood level of the drug and may occur as a consequence of rapid absorption.
Cardiovascular System
Cardiovascular manifestations are usually depressant and are characterized by bradycardia, hypotension, and cardiovascular collapse, which may lead to cardiac arrest.
Allergic
Allergic reactions are characterized by cutaneous lesions, urticaria, edema or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to the local anesthetic agent or to other ingredients in the formulation. Allergic reactions as a result of sensitivity to lidocaine HCl are extremely rare and, if they occur, should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
To report SUSPECTED ADVERSE REACTIONS, contact PAI Pharma 1-800-845-8210, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics (see ADVERSE REACTIONS, WARNINGS, and PRECAUTIONS).
Management of Local Anesthetic Emergencies
The first consideration is prevention, best accomplished by careful and constant monitoring of cardiovascular and respiratory vital signs and the patient's state of consciousness after each local anesthetic administration. At the first sign of change, oxygen should be administered.
The first step in the management of convulsions consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, small increments of an ultra-short acting barbiturate (such as thiopental or thiamylal) or a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (eg, ephedrine).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias and cardiac arrest. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted.
Dialysis is of negligible value in the treatment of acute overdosage with lidocaine HCl.
The intravenous LD50 of lidocaine HCl in female mice is 26 (21 to 31) mg/kg and the subcutaneous LD50 is 264 (203 to 304) mg/kg.
-
DOSAGE AND ADMINISTRATION
When Lidocaine Hydrochloride Topical Solution, 4% is used concomitantly with other products containing lidocaine HCl, the total dose contributed by all formulations must be kept in mind.
The dosage varies and depends upon the area to be anesthetized, vascularity of the tissues, individual tolerance, and the technique of anesthesia. The lowest dosage needed to provide effective anesthesia should be administered. Dosages should be reduced for children and for elderly and debilitated patients. The maximum dose should not exceed 4.5 mg/kg (2 mg/lb) of body weight. Although the incidence of adverse effects with Lidocaine Hydrochloride Topical Solution, 4% is quite low, caution should be exercised, particularly when employing large volumes, since the incidence of adverse effects is directly proportional to the total dose of local anesthetic agent administered.
The dosages recommended below are for normal, healthy adults:
When used as a spray, or when applied by means of cotton applicators or packs, as when instilled into a cavity, the suggested dosage of Lidocaine Hydrochloride Topical Solution, 4% is 1 to 5 mL (40 to 200 mg lidocaine HCl), ie, 0.6 to 3 mg/kg or 0.3 to 1.5 mg/lb body weight.
NOTE: The solution may be applied with a sterile swab which is discarded after a single use. When spraying, transfer the solution from the original container to an atomizer.
-
MAXIMUM RECOMMENDED DOSAGES
Normal Healthy Adults
The maximum recommended dose of Lidocaine Hydrochloride Topical Solution, 4% should be such that the dose of lidocaine HCl is kept below 300 mg and in any case should not exceed 4.5 mg/kg (2 mg/lb) body weight.
Children
It is difficult to recommend a maximum dose of any drug for children since this varies as a function of age and weight. For children of less than ten years who have a normal lean body mass and normal body development, the maximum dose may be determined by the application of one of the standard pediatric drug formulas (eg, Clark's rule). For example, in a child of five years weighing 50 lbs, the dose of lidocaine HCl should not exceed 75 to 100 mg when calculated according to Clark's rule. In any case, the maximum dose of Lidocaine Hydrochloride Topical Solution, 4% with epinephrine should not exceed 7 mg/kg (3.2 mg/lb) of body weight. When used without epinephrine, the amount of Lidocaine Hydrochloride Topical Solution, 4% administered should be such that the dose is kept below 300 mg and in any case should not exceed 4.5 mg/kg (2 mg/lb) of body weight.
-
HOW SUPPLIED
Lidocaine Hydrochloride Topical Solution USP, 4% is available in 50 mL screw cap glass bottles, individually cartoned. NOT FOR INJECTION.
Lidocaine Hydrochloride Topical Solution USP, 4% 50 mL NDC 63739-997-64
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Manufactured by:
PAI Pharma
Greenville, SC 29605Distributed by:
McKesson Corporation
dba Sky Packaging
4971 Southridge Blvd., Suite 101
Memphis, TN 38141Rev. 11/2023
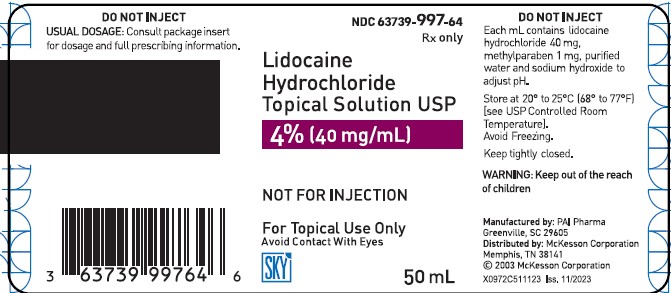
- PRINCIPAL DISPLAY PANEL - 50 mL Bottle Label
-
INGREDIENTS AND APPEARANCE
LIDOCAINE HYDROCHLORIDE
lidocaine hydrochloride solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63739-997 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LIDOCAINE HYDROCHLORIDE (UNII: V13007Z41A) (LIDOCAINE - UNII:98PI200987) LIDOCAINE HYDROCHLORIDE ANHYDROUS 40 mg in 1 mL Inactive Ingredients Ingredient Name Strength METHYLPARABEN (UNII: A2I8C7HI9T) WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) Product Characteristics Color white Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63739-997-64 1 in 1 CARTON 06/27/2024 03/31/2027 1 50 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA204494 06/27/2024 03/31/2027 Labeler - McKesson Corporation dba SKY Packaging (140529962)