AZITHROMYCIN- azithromycin tablet, film coated
Carlsbad Technology, Inc.
----------
Azithromycin Tablets
1 Indications and Usage
Azithromycin film coated tablets are a macrolide antibacterial drug indicated for the treatment of
patients with mild to moderate infections caused by susceptible strains of the designated
microorganisms in the specific conditions listed below.
1.1 Sexually Transmitted Diseases
Non-gonococcal urethritis and cervicitis due to Chlamydia trachomatis
1.2 Mycobacterial Infections
Prophylaxis of Disseminated Mycobacterium avium complex (MAC) Disease
Azithromycin film coated tablets, taken alone or in combination with rifabutin at its approved
dose, is indicated for the prevention of disseminated MAC disease in persons with advanced
HIV infection [see Dosage and Administration (2)].
Treatment of Disseminated MAC Disease
Azithromycin film coated tablets, taken in combination with ethambutol, is indicated for the
treatment of disseminated MAC infections in persons with advanced HIV infection [see Use in
Specific Populations (8.4) and Clinical Studies (14.1)].
1.3 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of
azithromycin film coated tablets and other antibacterial drugs, azithromycin film coated
tablets should be used only to treat infections that are proven or strongly suspected to be
caused by susceptible bacteria. When culture and susceptibility information are available,
they should be considered in selecting or modifying antibacterial therapy. In the absence of
such data, local epidemiology and susceptibility patterns may contribute to the empiric
selection of therapy.
2 Dosage and Administration
[see Indications and Usage (1)]
2.1 Sexually Transmitted Diseases
The recommended dose of azithromycin film coated tablets for the treatment of nongonococcal
urethritis and cervicitis due to C. trachomatis is a single 1 gram (1000 mg) dose of
azithromycin.
2.2 Mycobacterial Infections
Prevention of Disseminated MAC Infections
The recommended dose of azithromycin for the prevention of disseminated Mycobacterium
avium complex (MAC) disease is: 1,200 mg taken once weekly. This dose of azithromycin may
be combined with the approved dosage regimen of rifabutin.
Treatment of Disseminated MAC Infections
Azithromycin should be taken at a daily dose of 600 mg, in combination with ethambutol at
the recommended daily dose of 15 mg/kg. Other antimycobacterial drugs that have shown in
vitro activity against MAC may be added to the regimen of azithromycin plus ethambutol at the
discretion of the physician or health care provider.
3 Dosage Forms and Strength
Azithromycin Tablets USP, 600 mg (debossed “YSP257” on one side and plain on the reverse side)
are supplied as white to off-white film-coated tablets containing azithromycin dihydrate equivalent
to 600 mg azithromycin. These are packaged in bottles of 30 tablets.
4 Contraindications
4.1 Hypersensitivity
Azithromycin is contraindicated in patients with known hypersensitivity to azithromycin,
erythromycin, any macrolide, or ketolide drug.
4.2 Hepatic Dysfunction
Azithromycin is contraindicated in patients with a history of cholestatic jaundice/hepatic
dysfunction associated with prior use of azithromycin.
5 Warnings and Precautions
5.1 Hypersensitivity
Serious allergic reactions, including angioedema, anaphylaxis, and dermatologic reactions
including Acute Generalized Exanthematous Pustulosis (AGEP), Stevens-Johnson Syndrome,
and toxic epidermal necrolysis, have been reported rarely in patients on azithromycin therapy.
[see Contraindications (4.1)]
Fatalities have been reported. Cases of Drug Reaction with Eosinophilia and Systemic Symptoms
(DRESS) have also been reported. Despite initially successful symptomatic treatment of the
allergic symptoms, when symptomatic therapy was discontinued, the allergic symptoms
recurred soon thereafter in some patients without further azithromycin exposure. These
patients required prolonged periods of observation and symptomatic treatment. The
relationship of these episodes to the long tissue half-life of azithromycin and subsequent
prolonged exposure to antigen is presently unknown.
If an allergic reaction occurs, the drug should be discontinued and appropriate therapy should
be instituted. Physicians should be aware that allergic symptoms may reappear when
symptomatic therapy is discontinued.
5.2 Hepatotoxicity
Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure
have been reported, some of which have resulted in death. Discontinue azithromycin
immediately if signs and symptoms of hepatitis occur.
5.3 Infantile Hypertrophic Pyloric Stenosis (IHPS)
Following the use of azithromycin in neonates (treatment up to 42 days of life), IHPS has been
reported. Direct parents and caregivers to contact their physician if vomiting or irritability
with feeding occurs.
5.4 QT Prolongation
Prolonged cardiac repolarization and QT interval, imparting a risk of developing cardiac
arrhythmia and torsades de pointes, have been seen with treatment with macrolides,
including azithromycin. Cases of torsades de pointes have been spontaneously reported
during postmarketing surveillance in patients receiving azithromycin. Providers should
consider the risk of QT prolongation which can be fatal when weighing the risks and benefits
of azithromycin for at-risk groups including:
● patients with known prolongation of the QT interval, a history of torsades de pointes,
congenital long QT syndrome, bradyarrhythmias or uncompensated heart failure
● patients on drugs known to prolong the QT interval
● patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or
hypomagnesemia, clinically significant bradycardia, and in patients receiving Class IA
(quinidine, procainamide) or Class III (dofetilide, amiodarone, sotalol) antiarrhythmic
agents.
Elderly patients may be more susceptible to drug-associated effects on the QT interval.
5.5 Clostridium difficile-Associated Diarrhea (CDAD)
CDAD has been reported with use of nearly all antibacterial agents, including azithromycin,
and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial
agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD.
Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these
infections can be refractory to antibacterial therapy and may require colectomy. CDAD must
be considered in all patients who present with diarrhea following antibiotic use. Careful
medical history is necessary since CDAD has been reported to occur over two months after
the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may
need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation,
antibiotic treatment of C. difficile, and surgical evaluation should be instituted as
clinically indicated.
5.6 Exacerbation of Myasthenia Gravis
Exacerbations of symptoms of myasthenia gravis and new onset of myasthenic syndrome
have been reported in patients receiving azithromycin therapy.
5.7 Use in Sexually Transmitted Infections
Azithromycin, at the recommended dose, should not be relied upon to treat gonorrhea or
syphilis. Antibacterial agents used in high doses for short periods of time to treat nongonococcal
urethritis may mask or delay the symptoms of incubating gonorrhea or syphilis.
All patients with sexually transmitted urethritis or cervicitis should have a serologic test for
syphilis and appropriate cultures for gonorrhea performed at the time of diagnosis.
Appropriate antibacterial therapy and follow-up tests for these diseases should be initiated if
infection is confirmed.
5.8 Development of Drug-Resistant Bacteria
Prescribing azithromycin in the absence of a proven or strongly suspected bacterial infection
or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk
of the development of drug-resistant bacteria.
6 Adverse Reactions
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates
observed in the clinical trials of a drug cannot be directly compared to rates in the clinical
trials of another drug and may not reflect the rates observed in practice.
In clinical trials, most of the reported adverse reactions were mild to moderate in severity and
were reversible upon discontinuation of the drug. Approximately 0.7% of the patients from
the multiple-dose clinical trials discontinued azithromycin therapy because of treatmentrelated
adverse reactions. Serious adverse reactions included angioedema and cholestatic
jaundice. Most of the adverse reactions leading to discontinuation were related to the
gastrointestinal tract, e.g., nausea, vomiting, diarrhea, or abdominal pain. [see Clinical Studies
(14.2)]
Multiple-dose regimen
Overall, the most common adverse reactions in adult patients receiving a multiple-dose
regimen of azithromycin were related to the gastrointestinal system with diarrhea/loose
stools (5%), nausea (3%), and abdominal pain (3%) being the most frequently reported.
No other adverse reactions occurred in patients on the multiple-dose regimen of azithromycin
with a frequency greater than 1%. Adverse reactions that occurred with a frequency of 1%
or less included the following:
Cardiovascular: Palpitations and chest pain.
Gastrointestinal: Dyspepsia, flatulence, vomiting, melena, and cholestatic jaundice.
Genitourinary: Monilia, vaginitis, and nephritis.
Nervous System: Dizziness, headache, vertigo, and somnolence.
General: Fatigue.
Allergic: Rash, photosensitivity, and angioedema.
Chronic therapy with 1200 mg weekly regimen
The nature of adverse reactions seen with the 1200 mg weekly dosing regimen for the
prevention of Mycobacterium avium infection in severely immunocompromised HIV-infected
patients were similar to those seen with short-term dosing regimens. [see Clinical Studies (14)]
Chronic therapy with 600 mg daily regimen combined with ethambutol
The nature of adverse reactions seen with the 600 mg daily dosing regimen for the treatment
of Mycobacterium avium complex infection in severely immunocompromised HIV-infected
patients were similar to those seen with short term dosing regimens. Five percent of patients
experienced reversible hearing impairment in the pivotal clinical trial for the treatment of
disseminated MAC in patients with AIDS. Hearing impairment has been reported with
macrolide antibiotics, especially at higher doses. Other treatment-related adverse reactions
occurring in >5% of subjects and seen at any time during a median of 87.5 days of therapy
include: abdominal pain (14%), nausea (14%), vomiting (13%), diarrhea (12%), flatulence
(5%), headache (5%), and abnormal vision (5%). Discontinuations from treatment due to
laboratory abnormalities or adverse reactions considered related to study drug occurred in 8
of 88 (9.1%) of subjects.
Single 1 gram dose regimen
Overall, the most common adverse reactions in patients receiving a single-dose regimen of 1
gram of azithromycin were related to the gastrointestinal system and were more frequently
reported than in patients receiving the multiple-dose regimen.
Adverse reactions that occurred in patients on the single 1 gram dosing regimen of
azithromycin with a frequency of 1% or greater included diarrhea/loose stools (7%), nausea
(5%), abdominal pain (5%), vomiting (2%), dyspepsia (1%), and vaginitis (1%).
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of azithromycin.
Because these reactions are reported voluntarily from a population of uncertain size, it is not
always possible to reliably estimate their frequency or establish a causal relationship to drug
exposure.
Adverse reactions reported with azithromycin during the postmarketing period in adult and/or
pediatric patients for which a causal relationship may not be established include:
Allergic: Arthralgia, edema, urticaria, and angioedema.
Cardiovascular: Arrhythmias, including ventricular tachycardia, and hypotension. There have
been reports of QT prolongation and torsades de pointes.
Gastrointestinal: Anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea pseudomembranous
colitis, pancreatitis, oral candidiasis, pyloric stenosis, and tongue discoloration.
General: Asthenia, paresthesia, fatigue, malaise, and anaphylaxis
Genitourinary: Interstitial nephritis, acute renal failure, and vaginitis.
Hematopoietic: Thrombocytopenia.
Liver/Biliary: Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and
hepatic failure. [see Warnings and Precautions (5.2)]
Nervous System: Convulsions, dizziness/vertigo, headache, somnolence, hyperactivity,
nervousness, agitation, and syncope.
Psychiatric: Aggressive reaction and anxiety.
Skin/Appendages: Pruritus, and serious skin reactions including erythema multiforme, AGEP,
Stevens-Johnson Syndrome, toxic epidermal necrolysis, and DRESS.
Special Senses: Hearing disturbances including hearing loss, deafness, and/or tinnitus, and
reports of taste/smell perversion and/or loss.
6.3 Laboratory Abnormalities
Significant abnormalities (irrespective of drug relationship) occurring during the clinical trials
were reported as follows:
● With an incidence of 1-2%, elevated serum creatine phosphokinase, potassium, ALT (SGPT),
GGT, and AST (SGOT).
● With an incidence of less than 1%, leukopenia, neutropenia, decreased platelet count,
elevated serum alkaline phosphatase, bilirubin, BUN, creatinine, blood glucose, LDH, and
phosphate.
When follow-up was provided, changes in laboratory tests appeared to be reversible.
In multiple-dose clinical trials involving more than 3000 patients, 3 patients discontinued
therapy because of treatment-related liver enzyme abnormalities and 1 because of a renal
function abnormality.
In a phase 1 drug interaction study performed in normal volunteers, 1 of 6 subjects given the
combination of azithromycin and rifabutin, 1 of 7 given rifabutin alone, and 0 of 6 given
azithromycin alone developed a clinically significant neutropenia (<500 cells/mm3).
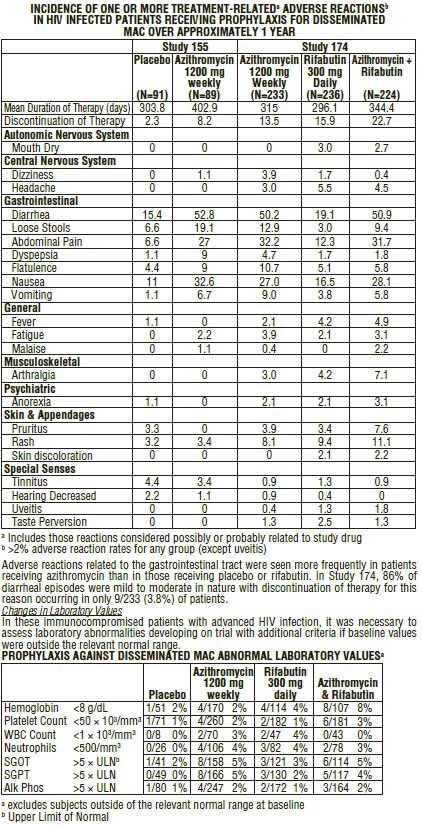
Laboratory abnormalities seen in clinical trials for the prevention of disseminated Mycobacterium
avium disease in severely immunocompromised HIV-infected patients. [see Clinical Studies (14)]
Chronic therapy (median duration: 87.5 days, range: 1-229 days) that resulted in laboratory
abnormalities in >5% of subjects with normal baseline values in the pivotal trial for treatment
of disseminated MAC in severely immunocompromised HIV-infected patients treated with
azithromycin 600 mg daily in combination with ethambutol include: a reduction in absolute
neutrophils to <50% of the lower limit of normal (10/52, 19%) and an increase to five times
the upper limit of normal in alkaline phosphatase (3/35, 9%). These findings in subjects with
normal baseline values are similar when compared to all subjects for analyses of neutrophil
reductions (22/75, 29%) and elevated alkaline phosphatase (16/80, 20%). Causality of these
laboratory abnormalities due to the use of study drug has not been established.
7 Drug Interactions
7.1 Nelfinavir
Co-administration of nelfinavir at steady-state with a single oral dose of azithromycin resulted
in increased azithromycin serum concentrations. Although a dose adjustment of azithromycin
is not recommended when administered in combination with nelfinavir, close monitoring
for known adverse reactions of azithromycin, such as liver enzyme abnormalities and hearing
impairment, is warranted. [see Adverse Reactions (6)]
7.2 Warfarin
Spontaneous postmarketing reports suggest that concomitant administration of azithromycin
may potentiate the effects of oral anticoagulants such as warfarin, although the prothrombin
time was not affected in the dedicated drug interaction study with azithromycin and
warfarin. Prothrombin times should be carefully monitored while patients are receiving
azithromycin and oral anticoagulants concomitantly.
7.3 Potential Drug-Drug Interaction with Macrolides
Interactions with digoxin, colchicine or phenytoin have not been reported in clinical trials with
azithromycin. No specific drug interaction studies have been performed to evaluate potential
drug-drug interaction. However, drug interactions have been observed with other macrolide
products. Until further data are developed regarding drug interactions when digoxin,
colchicine or phenytoin are used with azithromycin careful monitoring of patients is advised.
8 Use in Specific Populations
8.1 Pregnancy
Risk Summary
Available data from published literature and postmarketing experience over several decades
with azithromycin use in pregnant women have not identified any drug-associated risks for
major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
Developmental toxicity studies with azithromycin in rats, mice, and rabbits showed no druginduced
fetal malformations at doses up to 3, 2, and 1 times, respectively, an adult human
daily dose of 600 mg based on body surface area. Decreased viability and delayed
development were observed in the offspring of pregnant rats administered azithromycin from
day 6 of pregnancy through weaning at a dose equivalent to 3 times an adult human daily
dose of 600 mg based on body surface area (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated
populations is unknown. All pregnancies have a background risk of birth defect, loss, or other
adverse outcomes. In the U.S. general population, the estimated background risk of major
birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%,
respectively.
Data
Human Data
Available data from published observational studies, case series, and case reports over
several decades do not suggest an increased risk for major birth defects, miscarriage, or
adverse maternal or fetal outcomes with azithromycin use in pregnant women. Limitations of
these data include the lack of randomization and inability to control for confounders such as
underlying maternal disease and maternal use of concomitant medications.
Animal Data
Azithromycin administered during the period of organogenesis did not cause fetal malformations
in rats and mice at oral doses up to 200 mg/kg/day (moderately maternally toxic). Based
on body surface area, this dose is approximately 3 (rats) and 2 (mice) times an adult human
daily dose of 600 mg. In rabbits administered azithromycin at oral doses of 10, 20, and 40
mg/kg/day during organogenesis, reduced maternal body weight and food consumption were
observed in all groups; no evidence of fetotoxicity or teratogenicity was observed at these
doses, the highest of which is approximately equal to an adult human daily dose of 600 mg
based on body surface area.
In a pre- and postnatal development study, azithromycin was administered orally to pregnant
rats from day 6 of pregnancy until weaning at doses of 50 or 200 mg/kg/day. Maternal toxicity
(reduced food consumption and body weight gain; increased stress at parturition) was
observed at the higher dose. Effects in the offspring were noted at 200 mg/kg/day during the
postnatal development period (decreased viability, delayed developmental landmarks). These
effects were not observed in a pre- and postnatal rat study when up to 200 mg/kg/day of
azithromycin was given orally beginning on day 15 of pregnancy until weaning.
8.2 Lactation
Risk Summary
Azithromycin is present in human milk (see Data). Non-serious adverse reactions have been
reported in breastfed infants after maternal administration of azithromycin (see Clinical
Considerations). There are no available data on the effects of azithromycin on milk production.
The developmental and health benefits of breastfeeding should be considered along with the
mother’s clinical need for azithromycin and any potential adverse effects on the breastfed
infant from azithromycin or from the underlying maternal condition.
Clinical Considerations
Advise women to monitor the breastfed infant for diarrhea, vomiting, or rash.
Data
Azithromycin breastmilk concentrations were measured in 20 women after receiving a single
2 g oral dose of azithromycin during labor. Breastmilk samples collected on days 3 and 6
postpartum as well as 2 and 4 weeks postpartum revealed the presence of azithromycin in
breastmilk up to 4 weeks after dosing. In another study, a single dose of azithromycin 500
mg was administered intravenously to 8 women prior to incision for cesarean section.
Breastmilk (colostrum) samples obtained between 12 and 48 hours after dosing revealed that
azithromycin persisted in breastmilk up to 48 hours.
8.4 Pediatric Use
In controlled clinical studies, azithromycin has been administered to pediatric patients
ranging in age from 6 months to 12 years. For information regarding the use of azithromycin
for oral suspension in the treatment of pediatric patients, [see Indications and Usage (1) and
Dosage and Administration (2)] of the prescribing information for azithromycin for oral
suspension 100 mg/5 mL and 200 mg/5 mL bottles.
HIV-Infected Pediatric Patients: The safety and efficacy of azithromycin for the prevention or
treatment of MAC in HIV-infected children have not been established. Safety data are
available for 72 children 5 months to 18 years of age (mean 7 years) who received azithromycin
for treatment of opportunistic infections. The mean duration of therapy was 242 days
(range 3-2004 days) at doses of <1 to 52 mg/kg/day (mean 12 mg/kg/day). Adverse reactions
were similar to those observed in the adult population, most of which involved the
gastrointestinal tract. Treatment-related reversible hearing impairment in children was
observed in 4 subjects (5.6%). Two (2.8%) children prematurely discontinued treatment due
to adverse reactions: one due to back pain and one due to abdominal pain, hot and cold
flushes, dizziness, headache, and numbness. A third child discontinued due to a laboratory
abnormality (eosinophilia). The protocols upon which these data are based specified a daily
dose of 10-20 mg/kg/day (oral and/or IV) of azithromycin.
8.5 Geriatric Use
In multiple-dose clinical trials of oral azithromycin, 9% of patients were at least 65 years of
age (458/4949) and 3% of patients (144/4949) were at least 75 years of age. No overall
differences in safety or effectiveness were observed between these subjects and younger
subjects, and other reported clinical experience has not identified differences in responses
between the elderly and younger patients, but greater sensitivity of some older individuals
cannot be ruled out.
Elderly patients may be more susceptible to development of torsades de pointes arrhythmias
than younger patients. [see Warnings and Precautions (5.4)]
Azithromycin film coated tablets 600 mg contain 4.88 mg of sodium per tablet.
Geriatric Patients with Opportunistic Infections, Including (MAC) Disease: Safety data are available for
30 patients (65-94 years old) treated with azithromycin at doses >300 mg/day for a mean of
207 days. These patients were treated for a variety of opportunistic infections, including
MAC. The adverse reactions were generally similar to that seen in younger patients, except
for a higher incidence of adverse reactions relating to the gastrointestinal system and to
reversible impairment of hearing. [see Dosage and Administration (2)]
10 Overdosage
Adverse reactions experienced in higher than recommended doses were similar to those seen at
normal doses. In the event of overdosage, general symptomatic and supportive measures are
indicated as required.
11 Description
Azithromycin Tablets, USP contains the active ingredient azithromycin, a macrolide antibacterial
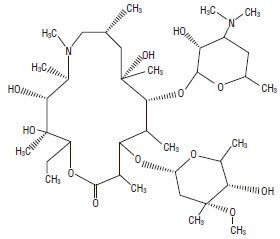
drug, for oral administration. Azithromycin has the chemical name (2R,3S,4R,5R,8R,10R,11R,12S,
13S,14R)-13-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α -L-ribo-hexopyranosyl)oxy]-2-
ethyl-3,4,10-trihydroxy-3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-
β-D-xylo-hexopyranosyl]oxy]-1-oxa-6-azacyclopentadecan-15-one. Azithromycin is derived from
erythromycin; however, it differs chemically from erythromycin in that a methyl-substituted
nitrogen atom is incorporated into the lactone ring. Its molecular formula is C38H72N2O12, and its
molecular weight is 749.0. Azithromycin has the following structural formula:
Azithromycin, as the dihydrate, is a white crystalline powder with a molecular formula of
C38H72N2O12.2H2O and a molecular weight of 785.0.
Azithromycin Tablets, USP contain azithromycin dihydrate equivalent to 600 mg azithromycin.
They also contain the following inactive ingredients: dibasic calcium phosphate dihydrate,
pregelatinized starch, croscarmellose sodium, magnesium stearate, sodium lauryl sulfate, and a
film coat consisting of polydextrose, titanium dioxide, hypromellose, triacetin, and polyethylene
glycol 8000.
12 Clinical Pharmacology
12.1 Mechanism of Action
Azithromycin is a macrolide antibacterial drug. [see Microbiology (12.4)]
12.2 Pharmacodynamics
Based on animal models of infection, the antibacterial activity of azithromycin appears to
correlate with the ratio of area under the concentration-time curve to minimum inhibitory
concentration (AUC/MIC) for certain pathogens (S. pneumoniae and S. aureus).
The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and
microbiological cure has not been elucidated in clinical trials with azithromycin.
Cardiac Electrophysiology
QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116
healthy subjects who received either chloroquine (1000 mg) alone or in combination with oral
azithromycin (500 mg, 1000 mg, and 1500 mg once daily). Co-administration of azithromycin
increased the QTc interval in a dose- and concentration- dependent manner. In comparison
to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF
were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1000 mg and
1500 mg azithromycin, respectively.
12.3 Pharmacokinetics
The pharmacokinetic parameters of azithromycin in plasma after dosing as per labeled
recommendations in healthy young adults and asymptomatic HIV-positive adults (age 18-40
years old) are portrayed in the following chart:
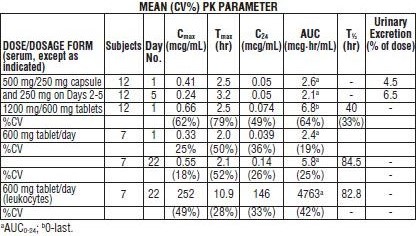
With a regimen of 500 mg on Day 1 and 250 mg/day on Days 2-5, Cmin and Cmax remained
essentially unchanged from Day 2 through Day 5 of therapy. However, without a loading
dose, azithromycin Cmin levels required 5 to 7 days to reach steady state.
In asymptomatic HIV-positive adult subjects receiving azithromycin film coated tablets 600
mg once daily for 22 days, steady state azithromycin serum levels were achieved by Day 15
of dosing.
The high values in adults for apparent steady-state volume of distribution (31.1 L/kg) and
plasma clearance (630 mL/min) suggest that the prolonged half-life is due to extensive
uptake and subsequent release of drug from tissues.
Absorption
The 1 gram single-dose packet is bioequivalent to four 250 mg azithromycin capsule.
When the oral suspension of azithromycin was administered with food, the Cmax increased by
46% and the AUC by 14%.
The absolute bioavailability of two 600 mg tablets was 34% (CV=56%). Administration of two
600 mg tablets with food increased Cmax by 31% (CV=43%) while the extent of absorption
(AUC) was unchanged (mean ratio of AUCs=1.00; CV=55%).
Distribution
The serum protein binding of azithromycin is variable in the concentration range approximating
human exposure, decreasing from 51% at 0.02 mcg/mL to 7% at 2 mcg/mL.
The antibacterial activity of azithromycin is pH related and appears to be reduced with
decreasing pH. However, the extensive distribution of drug to tissues may be relevant to
clinical activity.
Azithromycin has been shown to penetrate into tissues in humans, including skin, lung,
tonsil, and cervix. Extensive tissue distribution was confirmed by examination of additional
tissues and fluids (bone, ejaculum, prostate, ovary, uterus, salpinx, stomach, liver, and
gallbladder). As there are no data from adequate and well-controlled studies of azithromycin
treatment of infections in these additional body sites, the clinical importance of these tissue
concentration data is unknown.
Azithromycin concentrates in phagocytes and fibroblasts as demonstrated by in vitro
incubation techniques. Using such methodology, the ratio of intracellular to extracellular
concentration was >30 after one hr of incubation. In vivo studies suggest that concentration
in phagocytes may contribute to drug distribution to inflamed tissues.
Following oral administration of a single 1200 mg dose (two 600 mg tablets), the mean
maximum concentration in peripheral leukocytes was 140 mcg/mL. Concentration remained
above 32 mcg/mL, for approximately 60 hr. The mean half-lives for 6 males and 6 females
were 34 hr and 57 hr, respectively. Leukocyte-to-plasma Cmax ratios for males and females
were 258 (±77%) and 175 (±60%), respectively, and the AUC ratios were 804 (±31%) and
541 (±28%) respectively. The clinical relevance of these findings is unknown.
Following oral administration of multiple daily doses of 600 mg (1 tablet/day) to asymptomatic
HIV-positive adults, mean maximum concentration in peripheral leukocytes was 252
mcg/mL (±49%). Trough concentrations in peripheral leukocytes at steady-state averaged
146 mcg/mL (±33%). The mean leukocyte-to-serum Cmax ratio was 456 (±38%) and the mean
leukocyte to serum AUC ratio was 816 (±31%). The clinical relevance of these findings is
unknown.
Metabolism
In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed.
Elimination
Plasma concentrations of azithromycin following single 500 mg oral and IV doses declined in
a polyphasic pattern resulting in an average terminal half-life of 68 hr. Biliary excretion of
azithromycin, predominantly as unchanged drug, is a major route of elimination. Over the
course of a week, approximately 6% of the administered dose appears as unchanged drug in
urine.
Specific Populations
Patients with Renal Impairment
Azithromycin pharmacokinetics was investigated in 42 adults (21 to 85 years of age) with
varying degrees of renal impairment. Following the oral administration of a single 1.0 g dose
of azithromycin (4 × 250 mg capsules), the mean Cmax and AUC0-120 increased by 5.1% and
4.2%, respectively, in subjects with GFR 10 to 80 mL/min compared to subjects with normal
renal function (GFR >80 mL/min). The mean Cmax and AUC0-120 increased 61% and 35%,
respectively, in subjects with end-stage renal disease (GFR <10 mL/min) compared to
subjects with normal renal function (GFR >80 mL/min).
Patients with Hepatic Impairment
The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been
established.
Male and Female Patients
There are no significant differences in the disposition of azithromycin between male and
female subjects. No dosage adjustment is recommended on the basis of gender.
Geriatric Patients
Pharmacokinetic parameters in older volunteers (65 to 85 years old) were similar to those in
younger volunteers (18 to 40 years old) for the 5-day therapeutic regimen. Dosage adjustment
does not appear to be necessary for older patients with normal renal and hepatic function
receiving treatment with this dosage regimen. [see Geriatric Use (8.5)]
Pediatric Patients
For information regarding the pharmacokinetics of azithromycin for oral suspension in
pediatric patients, see the prescribing information for azithromycin for oral suspension 100
mg/5 mL and 200 mg/5 mL bottles.
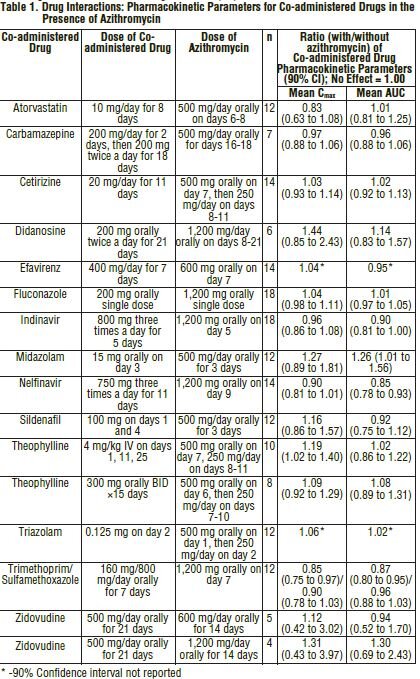
Drug Interaction Studies
Drug interaction studies were performed with azithromycin and other drugs likely to be coadministered.
The effects of co-administration of azithromycin on the pharmacokinetics of
other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of
azithromycin are shown in Table 2.
Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics
of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is
recommended when co-administered with azithromycin.
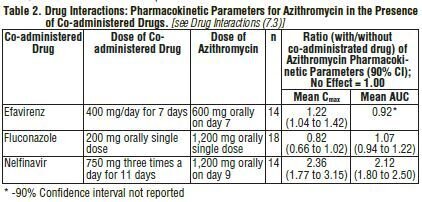
Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the
pharmacokinetics of azithromycin. Nelfinavir significantly increased the Cmax and AUC of
azithromycin. No dosage adjustment of azithromycin is recommended when administered
with drugs listed in Table 2. [see Drug Interactions (7.3)]
12.4 Microbiology
Mechanism of Action
Azithromycin acts by binding to the 23S rRNA of the 50S ribosomal subunit of susceptible
microorganisms inhibiting bacterial protein synthesis and impeding the assembly of the 50S
ribosomal subunit.
Resistance
The most frequently encountered mechanism of resistance to azithromycin is modification of
the 23S rRNA target, most often by methylation. Ribosomal modifications can determine
cross resistance to other macrolides, lincosamides, and streptogramin B (MLSB phenotype).
The mechanism of acquired mutational resistance in isolates of Mycobacterium avium complex
(i.e., 23S rRNA genemutation) is the same for both clarithromycin and azithromycin.
Antimicrobial Activity
Azithromycin has been shown to be active against the following microorganisms, both in vitro
and in clinical infections. [see Indications and Usage (1)]
Mycobacteria
Mycobacterium avium complex (MAC) consisting of:
Mycobacterium avium
Mycobacterium intracellulare
Other Microorganisms
Chlamydia trachomatis
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test
methods and quality control standards recognized by FDA for this drug, please see:
https://www.fda.gov/STIC.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate carcinogenic potential.
Azithromycin has shown no mutagenic potential in standard laboratory tests: mouse
lymphoma assay, human lymphocyte clastogenic assay, and mouse bone marrow
clastogenic assay. In fertility studies conducted in male and female rats, oral administration
of azithromycin for 64 to 66 days (males) or 15 days (females) prior to and during
cohabitation resulted in decreased pregnancy rate at 20 and 30 mg/kg/day when both males
and females were treated with azithromycin. This minimal effect on pregnancy rate
(approximately 12% reduction compared to concurrent controls) did not become more
pronounced when the dose was increased from 20 to 30 mg/kg/day (approximately 0.3 to 0.5
times the adult human daily dose of 600 mg based on body surface area) and it was not
observed when only one animal in the mated pair was treated. There were no effects on any
other reproductive parameters, and there were no effects on fertility at 10 mg/kg/day. The
relevance of these findings to patients being treated with azithromycin at the doses and
durations recommended in the prescribing information is uncertain.
13.2 Animal Toxicology
Phospholipidosis (intracellular phospholipid accumulation) has been observed in some
tissues of mice, rats, and dogs given multiple doses of azithromycin. It has been
demonstrated in numerous organ systems (e.g., eye, dorsal root ganglia, liver, gallbladder,
kidney, spleen, and/or pancreas) in dogs and rats treated with azithromycin at doses which,
expressed on the basis of body surface area, are similar to or less than the highest
recommended adult human dose. This effect has been shown to be reversible after cessation
of azithromycin treatment. Based on the pharmacokinetic data, phospholipidosis has been
seen in the rat (50 mg/kg/day dose) at the observed maximal plasma concentration of 1.3
mcg/mL (1.6 times the observed Cmax of 0.821 mcg/mL at the adult dose of 2 g.) Similarly, it
has been shown in the dog (10 mg/kg/day dose) at the observed maximal serum concentration
of 1 mcg/mL (1.2 times the observed Cmax of 0.821 mcg/mL at the adult dose of 2 g).
Phospholipidosis was also observed in neonatal rats dosed for 18 days at 30 mg/kg/day,
which is less than the pediatric dose of 60 mg/kg based on the surface area. It was not
observed in neonatal rats treated for 10 days at 40 mg/kg/day with mean maximal serum
concentrations of 1.86 mcg/mL, approximately 1.5 times the Cmax of 1.27 mcg/mL at the
pediatric dose. Phospholipidosis has been observed in neonatal dogs (10 mg/kg/day) at
maximum mean whole blood concentrations of 3.54 mcg/mL, approximately 3 times the
pediatric dose Cmax.
The significance of the finding for animals and for humans is unknown.
14 Clinical Studies
14.1 Clinical Studies in Patients with Advanced HIV Infection for the Prevention and Treatment
of Disease Due to Disseminated Mycobacterium avium Complex (MAC)
[see Indications and Usage (1)]
Prevention of Disseminated MAC Disease
Two randomized, double-blind clinical trials were performed in patients with CD4 counts
<100 cells/μL. The first trial (Study 155) compared azithromycin (1200 mg once weekly) to
placebo and enrolled 182 patients with a mean CD4 count of 35 cells/mcgL. The second trial
(Study 174) randomized 723 patients to either azithromycin (1200 mg once weekly), rifabutin
(300 mg daily), or the combination of both. The mean CD4 count was 51 cells/mcgL. The
primary endpoint in these trials was disseminated MAC disease. Other endpoints included the
incidence of clinically significant MAC disease and discontinuations from therapy for drugrelated
side effects.
MAC bacteremia
In Study 155, 85 patients randomized to receive azithromycin and 89 patients randomized to
receive placebo met the entrance criteria. Cumulative incidences at 6, 12, and 18 months of
the possible outcomes are in the following table:

Comparing the cumulative one-year incidence rates, azithromycin monotherapy is at least as
effective as rifabutin monotherapy. The difference (rifabutin–azithromycin) in the one-year
rates (7.6%) is statistically significant (p=0.022) with an adjusted 95% confidence interval
(0.9%, 14.3%). Additionally, azithromycin/rifabutin combination therapy is more effective
than rifabutin alone. The difference (rifabutin–azithromycin/rifabutin) in the cumulative oneyear
incidence rates (12.5%) is statistically significant (p<0.001) with an adjusted 95%
confidence interval of 6.6%, 18.4%. The comparable number of patients experiencing
adverse events and the fewer number of patients lost to follow-up on rifabutin should be
taken into account when interpreting the significance of this difference.
In Study 174, sensitivity testing1 was performed on all available MAC isolates from subjects
randomized to either azithromycin, rifabutin, or the combination. The distribution of MIC
values for azithromycin from susceptibility testing of the breakthrough isolates was similar
between trial arms. As the efficacy of azithromycin in the treatment of disseminated MAC has
not been established, the clinical relevance of these in vitro MICs as an indicator of
susceptibility or resistance is not known.
Clinically Significant Disseminated MAC Disease
In association with the decreased incidence of bacteremia, patients in the groups randomized
to either azithromycin alone or azithromycin in combination with rifabutin showed reductions
in the signs and symptoms of disseminated MAC disease, including fever or night sweats,
weight loss, and anemia.
Discontinuations from Therapy for Drug-Related Side Effects
In Study 155, discontinuations for drug-related toxicity occurred in 8.2% of subjects treated
with azithromycin and 2.3% of those given placebo (p=0.121). In Study 174, more subjects
discontinued from the combination of azithromycin and rifabutin (22.7%) than from
azithromycin alone (13.5%; p=0.026) or rifabutin alone (15.9%; p=0.209).
Safety
As these patients with advanced HIV disease were taking multiple concomitant medications
and experienced a variety of intercurrent illnesses, it was often difficult to attribute adverse
reactions to study medication. Overall, the nature of adverse reactions seen on the weekly
dosage regimen of azithromycin over a period of approximately one year in patients with
advanced HIV disease were similar to that previously reported for shorter course therapies.
Treatment of Disseminated MAC Disease
One randomized, double-blind clinical trial (Study 189) was performed in patients with
disseminated MAC. In this trial, 246 HIV-infected patients with disseminated MAC received
either azithromycin 250 mg daily (N=65), azithromycin 600 mg daily (N=91), or clarithromycin
500 mg twice a day (N=90), each administered with ethambutol 15 mg/kg daily, for 24
weeks. Blood cultures and clinical assessments were performed every 3 weeks through week
12 and monthly thereafter through week 24. After week 24, patients were switched to any
open-label therapy at the discretion of the investigator and followed every 3 months through
the last follow-up visit of the trial. Patients were followed from the baseline visit for a period
of up to 3.7 years (median: 9 months). MAC isolates recovered during treatment or posttreatment
were obtained whenever possible.
The primary endpoint was sterilization by week 24. Sterilization was based on data from the
central laboratory, and was defined as two consecutive observed negative blood cultures for
MAC, independent of missing culture data between the two negative observations. Analyses
were performed on all randomized patients who had a positive baseline culture for MAC.
The azithromycin 250 mg arm was discontinued after an interim analysis at 12 weeks showed
a significantly lower clearance of bacteremia compared to clarithromycin 500 mg twice a day.
Efficacy results for the azithromycin 600 mg daily and clarithromycin 500 mg twice a day
treatment regimens are described in the following table:
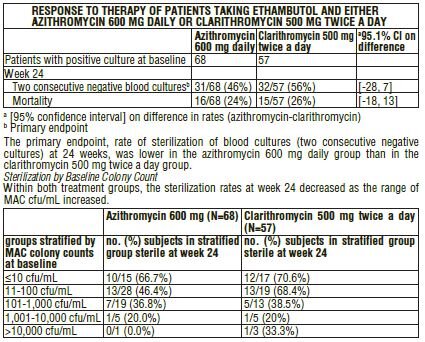
Susceptibility Pattern of MAC Isolates
Susceptibility testing was performed on MAC isolates recovered at baseline, at the time of
breakthrough on therapy or during post-therapy follow-up. The T100 radiometric broth
method was employed to determine azithromycin and clarithromycin MIC values. Azithromycin
MIC values ranged from <4 to >256 mcg/mL and clarithromycin MICs ranged from <1 to
>32 mcg/mL. The individual MAC susceptibility results demonstrated that azithromycin MIC
values could be 4 to 32-fold higher than clarithromycin MIC values.
During treatment and post-treatment follow-up for up to 3.7 years (median: 9 months) in
Study 189, a total of 6/68 (9%) and 6/57 (11%) of the patients randomized to azithromycin
600 mg daily and clarithromycin 500 mg twice a day respectively, developed MAC blood
culture isolates that had a sharp increase in MIC values. All twelve MAC isolates had
azithromycin MICs ≥256 mcg/mL and clarithromycin MICs >32 mcg/mL. These high MIC
values suggest development of drug resistance. However, at this time, specific breakpoints
for separating susceptible and resistant MAC isolates have not been established for either
macrolide.
15 References
1. Griffith DE, Aksamit T, Brown-Elliot BA, et al. An official ATS/IDSA statement: Diagnosis, treatment,
and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;
175:367-416.
16 How Supplied/Storage and Handling
Azithromycin Tablets USP, 600 mg (debossed “YSP257” on one side and plain on the reverse
side) are supplied as white to off-white film-coated tablets containing azithromycin dihydrate
equivalent to 600 mg azithromycin. These are packaged in bottles of 30 tablets.
AzithromycinTablets USP, 600 mg tablets are supplied as follows:
Bottles of 30 NDC 61442-403-30
Tablets should be stored at 20° to 25℃ (68° to 77℉) [see USP Controlled Room Temperature].
17 Patient Counseling Information
Azithromycin tablets may be taken with or without food. However, increased tolerability has been
observed when tablets are taken with food.
Patients should also be cautioned not to take aluminum- and magnesium-containing antacids and
azithromycin simultaneously.
The patient should be directed to discontinue azithromycin immediately and contact a physician if
any signs of an allergic reaction occur.
Direct parents or caregivers to contact their physician if vomiting and irritability with feeding
occurs in the infant.
Patients should be counseled that antibacterial drugs, including azithromycin, should only be
used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When
azithromycin is prescribed to treat bacterial infection, patients should be told that although it is
common to feel better early in the course of therapy, the medication should be taken exactly as
directed. Skipping doses or not completing the full course of therapy may (1) decrease the
effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop
resistance and will not be treatable by azithromycin or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibacterial which usually ends when the antibiotic is
discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery
and bloody stools (with or without stomach cramps and fever) even as late as two or more
months after having taken the last dose of the antibacterial. If this occurs, patients should contact
their physician as soon as possible.
| AZITHROMYCIN
azithromycin tablet, film coated |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| Labeler - Carlsbad Technology, Inc. (781047246) |
| Registrant - Carlsbad Technology, Inc. (781047246) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Carlsbad Technology, Inc. | 968263561 | manufacture(61442-403) | |
