ORENITRAM- treprostinil tablet, extended release
Avera McKennan Hospital
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use ORENITRAM
® safely and effectively. See Full Prescribing Information for ORENITRAM.
ORENITRAM (treprostinil) extended-release tablets, for oral use Initial U.S. Approval: 2002 INDICATIONS AND USAGEOrenitram is a prostacyclin vasodilator indicated for:
As the sole vasodilator, the effect on exercise is small. Orenitram has not been shown to add to other vasodilator therapy. ( 1.1) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSExtended-Release Tablets: 0.125 mg, 0.25 mg, 1 mg, 2.5 mg and 5 mg. ( 3) CONTRAINDICATIONS
WARNINGS AND PRECAUTIONSADVERSE REACTIONSMost common adverse reactions (incidence >5%) reported in clinical studies with Orenitram are headache, diarrhea, nausea, and flushing. ( 6.1) To report SUSPECTED ADVERSE REACTIONS, contact United Therapeutics Corp. at 1-866-458-6479 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSSee 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 3/2017 |
FULL PRESCRIBING INFORMATION
1. INDICATIONS AND USAGE
1.1 Pulmonary Arterial Hypertension
Orenitram is indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1) to improve exercise capacity.
The study that established effectiveness included predominately patients with WHO functional class II-III symptoms and etiologies of idiopathic or heritable PAH (75%) or PAH associated with connective tissue disease (19%). When used as the sole vasodilator, the effect of Orenitram on exercise is about 10% of the deficit, and the effect, if any, on a background of another vasodilator is probably less than this.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
Take Orenitram with food. Swallow Orenitram tablets whole; do not crush, split, or chew.
The recommended starting dose of Orenitram is 0.25 mg twice daily (BID) with food, taken approximately 12 hours apart or 0.125 mg three times daily (TID) with food, taken approximately 8 hours apart. Increase the dose to the highest tolerated dose. The recommended increment is 0.25 or 0.5 mg BID or 0.125 mg TID every 3-4 days. If dose increments are not tolerated consider titrating slower.
The appropriate maintenance dose is determined by tolerability.
If intolerable pharmacologic effects occur, decrease the dose in increments of 0.25 mg. Avoid abrupt discontinuation [see Warnings and Precautions (5.1)] .
2.2 Transitioning from Subcutaneous or Intravenous Routes of Administration of Treprostinil
Decrease the dose of Remodulin while simultaneously increasing the dose of Orenitram. The dose of Remodulin can be reduced up to 30 ng/kg/min per day and the dose of Orenitram simultaneously increased up to 6 mg per day (2 mg TID) if tolerated. The following equation can be used to estimate a comparable total daily dose of Orenitram in mg using a patient's dose of IV/SC treprostinil (in ng/kg/min) and weight (in kg).
Orenitram total daily dose (mg) = 0.0072 × Remodulin dose (ng/kg/min) × weight (kg)
2.3 Dose Adjustment in Patients with Hepatic Impairment
In patients with mild hepatic impairment (Child Pugh Class A) start at 0.125 mg BID with 0.125 mg BID dose increments every 3 to 4 days. Avoid use of Orenitram in patients with moderate hepatic impairment (Child Pugh Class B). Orenitram is contraindicated in patients with severe hepatic impairment (Child Pugh Class C) [see Contraindications (4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)] .
2.4 Dose Adjustment for Use with CYP2C8 Inhibitors
When co-administered with strong CYP2C8 inhibitors (e.g., gemfibrozil) the initial dose is 0.125 mg BID with 0.125 mg BID dose increments every 3 to 4 days.
2.5 Interruptions and Discontinuation
If a dose of medication is missed, the patient should take the missed dose as soon as possible, with food. If a patient misses two or more doses, restart at a lower dose and re-titrate.
In the event of a planned short-term treatment interruption for patients unable to take oral medications, consider a temporary infusion of subcutaneous or intravenous treprostinil. To calculate the total daily dose (mg) of treprostinil for the parenteral route use the following equation:
| Remodulin (ng/kg/min) = | 139 × Orenitram total daily dose (mg) | |
| weight (kg) |
When discontinuing Orenitram, reduce the dose in steps of 0.5 to 1 mg per day [see Warnings and Precautions (5.1)] .
3 DOSAGE FORMS AND STRENGTHS
Orenitram (treprostinil) extended-release tablets are available in the following five strengths:
- 0.125 mg [White tablet imprinted with UT 0.125]
- 0.25 mg [Green tablet imprinted with UT 0.25]
- 1 mg [Yellow tablet imprinted with UT 1]
- 2.5 mg [Pink tablet imprinted with UT 2.5]
- 5 mg [Red tablet imprinted with UT 5]
4 CONTRAINDICATIONS
Severe hepatic impairment (Child Pugh Class C) [see Use In Specific Populations (8.6) and Clinical Pharmacology (12.3)] .
5 WARNINGS AND PRECAUTIONS
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In a 12-week placebo-controlled monotherapy study (Study 1; WHO Group 1; functional class II-III), the most commonly reported adverse reactions that occurred in patients receiving Orenitram included: headache, diarrhea, nausea, and flushing. Table 1 lists the most common adverse reactions that occurred at a rate on Orenitram at least 5% higher than on placebo.
Orenitram patients in Table 1 for Study 1 (N = 151) had access to 0.25 mg tablets at randomization. Approximately 91% of such patients experienced an adverse reaction, but only 4% discontinued therapy for an adverse reaction (compared to 3% receiving placebo). The overall discontinuation rate for any reason was 17% for active and 14% for placebo.
| Reaction | Orenitram
N=151 | Placebo
N=77 |
|---|---|---|
| Headache | 63% | 19% |
| Diarrhea | 30% | 16% |
| Nausea | 30% | 18% |
| Flushing | 15% | 6% |
| Pain in jaw | 11% | 4% |
| Pain in extremity | 14% | 8% |
| Hypokalemia | 9% | 3% |
| Abdominal discomfort | 6% | 0% |
Orenitram was studied in a long-term, open-label extension study in which 824 patients were dosed for a mean duration of approximately 2 years. About 70% of patients continued treatment with Orenitram for at least a year. The mean dose was 4.2 mg BID at one year. The adverse reactions were similar to those observed in the placebo-controlled trials.
The safety of Orenitram was also evaluated in an open-label study transitioning patients from Remodulin. The safety profile during this study was similar to that observed in the three pivotal studies.
6.2 Post-Marketing Experience
The following adverse reactions have been identified during postapproval use of Orenitram: dizziness, dyspepsia, vomiting, myalgia, and arthralgia. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
7 DRUG INTERACTIONS
7.1 Antihypertensive Agents or Other Vasodilators
Concomitant administration of Orenitram with diuretics, antihypertensive agents or other vasodilators increases the risk of symptomatic hypotension.
7.2 Anticoagulants
Treprostinil inhibits platelet aggregation; there is increased risk of bleeding, particularly among patients receiving anticoagulants.
7.3 Effect of CYP2C8 Inhibitors
Co-administration of Orenitram and the CYP2C8 enzyme inhibitor gemfibrozil in healthy adult volunteers increases exposure to treprostinil. Reduce the starting dose of Orenitram to 0.125 mg BID and use 0.125 mg BID increments every 3 to 4 days [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)] .
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C.
Animal reproductive studies with treprostinil diolamine have shown an adverse effect on the fetus. There are no adequate and well-controlled studies in humans.
In rats, treatment with treprostinil diolamine had no effect on reproductive performance or sperm motility at doses up to 10 mg/kg/day. The exposures at this dose level are about 10- (male) to 18- (female) fold the usual human exposure at the mean dose of 3.4 mg BID.
In pregnant rats, reversible, dose-dependent decreases in body weight gain and food consumption were observed during the first four days of dosing in animals administered 10, 20 and 30 mg/kg/day treprostinil diolamine. In a dose range-finding study, there was a 17% decrease in the pregnancy rate in the animals administered 20 and 30 mg/kg/day. One dam in each of the 20 and 30 mg/kg/day had litters with no viable fetuses. In the definitive study (0, 5, 10 and 20 mg/kg/day), there were four treatment-related deaths, and a 32% decrease in the pregnancy rate for rats administered 20 mg/kg/day. There was an 8% decrease in the pregnancy rate in the animals administered 10 mg/kg/day. Across both studies, an increase in post-implantation loss was observed in animals administered 10 to 30 mg/kg/day, and a significant decrease in the mean number of live births was seen at dose levels ≥10 mg/kg/day. The no observed adverse effect level was 5 mg/kg/day (maternal, fetal viability and growth), and 20 mg/kg/day (teratogenicity), the highest dose tested in the definitive study. The exposures at 5 and 20 mg/kg/day doses represent 13 and 55 times, respectively, the human exposure.
For F 1 progeny, a decreased copulation index was observed at the 5 and 10 mg/kg/day treprostinil diolamine dose levels in rats. The no observed effect levels for physical development, reflex development, exploratory behavior, learning and memory, and sexual maturation was 10 mg/kg/day. The no observed effect level for F 1 progeny general development (based on body weight) was 10 mg/kg/day for females and ≤ 2.5 mg/kg/day for males; the no observed effect level for F 1 reproductive performance was 2.5 mg/kg/day or 6 times the human exposure.
In pregnant rabbits, the primary maternal adverse effects were gastrointestinal disturbance; dose-dependent decreases in mean body weight, body weight gain, and food consumption were observed. During the post-dose phase, the effect was reversed. In a dose range-finding study, there was a 17% decrease in the pregnancy rate for animals administered 4 mg/kg/day. A dose-dependent increase in post-implantation loss was observed. Two dams administered 4 mg/kg/day had litters with no viable fetuses; the mean fetal weight was slightly decreased in animals administered 4 mg/kg/day. In the definitive study, mean fetal weights were significantly decreased in animals administered 0.5 to 3 mg/kg/day of treprostinil diolamine. At doses of 1.5 and 3 mg/kg/day, external fetal and soft tissue malformations were observed in a few fetuses, and the total fetal skeletal malformations were significantly increased. The no observed adverse effect level was less than 0.5 mg/kg/day (maternal), 1.5 mg/kg/day (fetal viability and growth), and 0.5 mg/kg/day (teratogenicity). The 0.5 mg/kg/day dose represents about 5 times the human exposure.
8.2 Labor and Delivery
The effect of Orenitram on labor and delivery in humans is unknown. No treprostinil treatment-related effects on labor and delivery were seen in animal studies.
8.3 Nursing Mothers
It is not known whether treprostinil is excreted in human milk or absorbed systemically after ingestion. Because many drugs are excreted in human milk, choose Orenitram or breastfeeding.
8.5 Geriatric Use
Clinical studies of Orenitram did not include sufficient numbers of patients aged 65 years and over to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic or cardiac function, and of concomitant disease or other drug therapy.
8.6 Patients with Hepatic Impairment
There is a marked increase in the systemic exposure to treprostinil in hepatically impaired patients [see Dosage and Administration (2.3), Contraindications (4), and Clinical Pharmacology (12.3)] .
8.7 Patients with Renal Impairment
No dose adjustments are required in patients with renal impairment. Orenitram is not removed by dialysis [see Clinical Pharmacology (12.3)] .
10 OVERDOSAGE
Signs and symptoms of overdose with Orenitram during clinical trials reflect its dose-limiting pharmacologic effects and include severe headache, nausea, vomiting, diarrhea, and hypotension. Treat supportively.
11 DESCRIPTION
Orenitram is an extended release osmotic tablet for oral administration. Orenitram is formulated as the diolamine salt of treprostinil, a tricyclic benzindene analogue of prostacyclin. The chemical name is Acetic acid, 2-[[(1 R,2 R,3a S,9a S)-2,3,3a,4,9,9a-hexahydro-2-hydroxy-1-[(3 S)-3-hydroxyoctyl]-1 H-benz[f]inden-5-yl]oxy]-, complexed with 2,2'-iminobis[ethanol] (1:1). The molecular formula is C 23H 34O 5.C 4H 11NO 2, the molecular weight is 495.65, and it has the following structural formula:
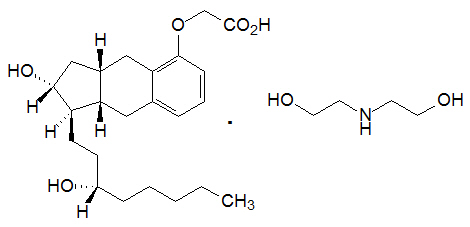
Orenitram tablets are formulated in five strengths, which contain 0.125 mg of treprostinil (equivalent to 0.159 mg treprostinil diolamine), 0.25 mg of treprostinil (equivalent to 0.317 mg treprostinil diolamine), 1 mg of treprostinil (equivalent to 1.27 mg treprostinil diolamine), 2.5 mg of treprostinil (equivalent to 3.17 mg treprostinil diolamine) or 5 mg of treprostinil (equivalent to 6.35 mg treprostinil diolamine). The formulations also contain xylitol, maltodextrin, sodium lauryl sulfate, magnesium stearate, cellulose acetate, triethyl citrate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, and talc. In addition tablets may contain colorants FD&C Blue #2, iron oxide yellow, and iron oxide red. The imprinting ink contains shellac glaze, ethanol, isopropyl alcohol USP, iron oxide black, n-butyl alcohol, and propylene glycol.
Orenitram is designed to release treprostinil at a near zero-order rate using an osmotic tablet technology. The tablet core is coated with a semi-permeable membrane and has a laser-drilled aperture through the membrane. Upon contact with water (e.g., after ingestion), the core tablet absorbs water through the semi-permeable membrane. The water dissolves the water-soluble treprostinil diolamine and the water-soluble osmotic excipients, which creates hydrostatic pressure within the membrane, eventually forcing the drug out through the tablet at a controlled rate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The major pharmacologic actions of treprostinil are direct vasodilation of pulmonary and systemic arterial vascular beds, inhibition of platelet aggregation, and inhibition of smooth muscle cell proliferation.
12.2 Pharmacodynamics
In a clinical trial of 240 healthy adult volunteers, single doses of inhaled treprostinil 54 µg (the target clinical dose) and 84 µg (supratherapeutic inhalation dose) prolonged the corrected QTc interval by approximately 10 msec. The QTc effect dissipated rapidly as the concentration of treprostinil decreased. Orenitram has not been evaluated in a thorough QTc study.
12.3 Pharmacokinetics
In patients with PAH, pharmacokinetics of treprostinil is dose-proportional for systemic exposure (AUC 0-t) over the dose range of 0.5 and 15 mg BID. Upon repeat administration with a BID regimen, the accumulation in the systemic exposures to treprostinil is minimal and results in a peak-to-trough ratio of approximately 7. However, a TID regimen will reduce the peak-to-trough fluctuations to approximately 2.5 for the same total daily dose.
Absorption
The absolute oral bioavailability of Orenitram is approximately 17%. Maximum treprostinil concentrations occur between approximately 4 and 6 hours following Orenitram administration. Time to reach steady-state concentrations for both BID and TID regimens is approximately 1 to 2 days.
The absorption of Orenitram is affected by food. The AUC inf of treprostinil was increased by 49% and the C max was increased by an average of 13% when Orenitram was administered following a high-fat, high-calorie meal compared to fasting conditions in healthy volunteers. The relative bioavailability of treprostinil following oral administration of Orenitram 1 mg is not significantly altered by meal types ranging from 250 to 500 calories in healthy volunteers.
When Orenitram 1 mg was administered with alcohol at 0.5 mg/kg or the equivalent of 3 servings (at the same time, or ± 1 hour relative to alcohol consumption), there was no significant change (10% to 20% increase) in the exposure to treprostinil compared to Orenitram administered alone.
Distribution
The treprostinil component of Orenitram is highly bound to human plasma proteins, approximately 96% over a treprostinil concentration range of 0.01-10 μg/mL.
Metabolism and Excretion
In a study conducted in healthy volunteers using [ 14C] treprostinil, treprostinil was extensively metabolized on the side chain of the molecule via oxidation, oxidative cleavage, dehydration, and glucuronic acid conjugation. Treprostinil is primarily metabolized by CYP2C8 and to a lesser extent by CYP2C9. No new metabolites are found upon oral administration compared to parenteral administration of treprostinil. Only 1.13% and 0.19% is excreted as unchanged parent drug in the feces and urine, respectively. Based on in vitro studies treprostinil does not inhibit or induce major CYP enzymes [see Drug Interactions (7.3)] .
Specific Populations
Hepatic Impairment: In subjects with mild (n=8) hepatic impairment, administration of a single 1 mg dose of Orenitram resulted in a mean C max and an AUC 0-inf that were 1.6- and 2.1-fold, respectively, values seen in healthy subjects. With moderate impairment (n=8), the corresponding ratios were 4.0- and 4.8-fold, and with severe impairment (n=6), they were 4.8- and 7.6-fold [see Dosage and Administration (2.3), Contraindications (4), and Use in Specific Populations (8.6)].
Drug Interactions
Results of drug interaction studies are shown in Figure 1. Only for the strong CYP2C8 inhibitor does the interaction affect dosing [see Dosage and Administration (2.4)] .
Figure 1: Impact of Co-Administered Drugs on the Systemic Exposure of Treprostinil 1 mg Compared to Orenitram Administered Alone
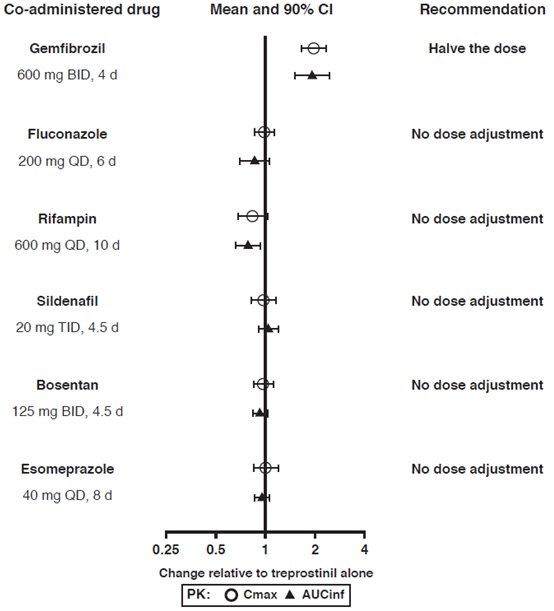
Warfarin: A drug interaction study was carried out with Remodulin co-administered with warfarin (25 mg/day) in healthy volunteers. There was no clinically significant effect of either medication on the pharmacokinetics of treprostinil. Additionally, treprostinil did not affect the pharmacokinetics or pharmacodynamics of warfarin. The pharmacokinetics of R- and S- warfarin and the international normalized ratio (INR) in healthy subjects given a single 25 mg dose of warfarin were unaffected by continuous subcutaneous infusion of treprostinil at an infusion rate of 10 ng/kg/min.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Treprostinil diolamine did not demonstrate any carcinogenic effects in mouse or rat carcinogenicity studies. Oral administration of treprostinil diolamine to Tg.rasH2 mice at 0, 5, 10 and 20 mg/kg/day in males and 0, 3, 7.5 and 15 mg/kg/day in females daily for 26 weeks did not significantly increase the incidence of tumors. The exposures obtained at the highest dose levels used in males and females are about 8- and 17-fold, respectively, the human exposure at the mean dose of 3.4 mg BID. Oral administration of treprostinil diolamine to Sprague Dawley rats at 0, 1, 3 and 10 mg/kg/day daily for 104 weeks did not significantly increase the incidence of tumors. The exposures obtained at the highest dose levels used in males and females are about 21- and 29-fold, respectively, the human exposure.
In vitro genotoxicity studies with high doses of treprostinil did not demonstrate any mutagenic or clastogenic effects. Treprostinil diolamine was tested in vivo in a rat micronucleus assay and did not induce an increased incidence of micronucleated polychromatic erythrocytes.
No adverse effect doses for fertility, fetal viability / growth, fetal development (teratogenicity), and postnatal development were determined in rats. In pregnant rabbits, external fetal and soft tissue malformations and fetal skeletal malformation occurred with the no observed adverse effect level for these adverse effects of 0.5 mg/kg/day (5 times the human exposure) [see Use in Specific Populations (8.1)] .
14 CLINICAL STUDIES
14.1 Clinical Trials in Pulmonary Arterial Hypertension (PAH)
Three multi-center, randomized, double-blind studies were conducted and compared Orenitram to placebo in a total of 349 (Study 1), 350 (Study 2), and 310 (Study 3) patients with PAH.
Study 1 (effect seen with no background vasodilator)
Study 1 was a 12-week, randomized (2:1 Orenitram to placebo), double-blind, placebo-controlled, international efficacy and safety study of Orenitram in patients with WHO Group 1 PAH not currently receiving PAH therapy. The primary efficacy endpoint was placebo-corrected change in six-minute walk distance (6MWD) from Baseline to Week 12. Study drug dose was titrated to a maximum of 12 mg BID based on clinical response and study drug tolerability. Study 1 enrolled 349 patients (overall analysis population) who were not receiving any PAH medication. At the beginning of the study, subjects were dosed with only the 1 mg tablets with 0.5 and 0.25 mg tablets introduced at sequentially later dates during the study. The primary analysis population consisted of the 228 patients who had access to the 0.25 mg tablet at the time of randomization. Patients were administered Orenitram or placebo twice daily, with the doses titrated to effect over the course of the 12-week trial. Patients were in WHO functional class II (~33%) and class III (~66%) with either idiopathic or heritable PAH (~75%), collagen vascular disease associated PAH (~19%), or PAH associated with HIV (1%) or congenital heart defect (5%) or other conditions (~6%). The patients' mean baseline 6MWD was approximately 330 meters. In the primary analysis population, 17% of patients discontinued Orenitram compared to 14% of patients on placebo.
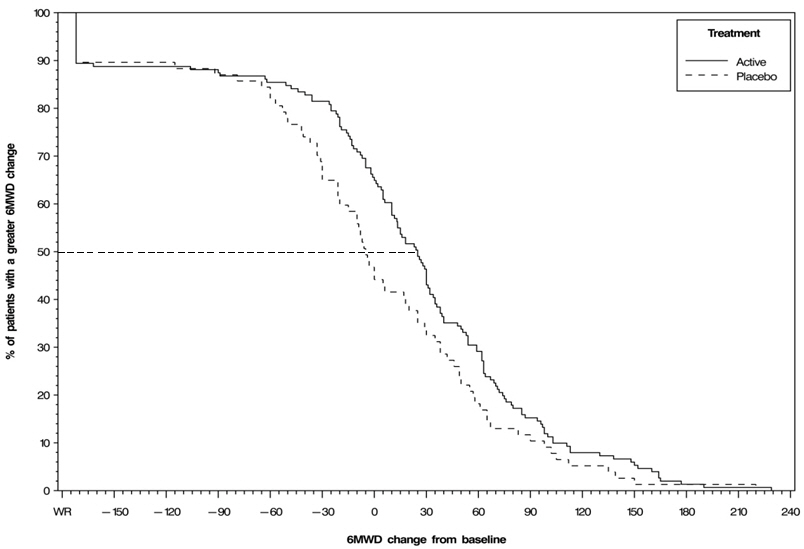
The primary efficacy endpoint of the trial was the change in 6MWD at 12 weeks for the primary analysis population. Analysis of Study 1 results demonstrated that those patients receiving Orenitram compared to patients receiving placebo improved their median 6MWD by approximately +23 meters (Hodges-Lehmann estimate; p=0.013, non-parametric analysis of covariance in accordance with the pre-specified statistical analysis plan) as compared to patients receiving placebo as demonstrated in (Figure 2). The within group median change from baseline was +25 meters for Orenitram and -5 meters for placebo at week 12 (N=228). Mean dose (±SD) in the Orenitram group was 2.3 ± 1.3, 3.2 ± 1.9, and 3.4 ± 1.9 mg BID at Weeks 4, 8, and 12, respectively, with a maximum dose of 12 mg BID. The distribution of the 6MWD change from baseline at Week 12 was also plotted across the range of observed values (Figure 3).
Figure 2: Hodges-Lehmann Estimate of Treatment Effect by Visit for the Primary Analysis Population (Study 1)
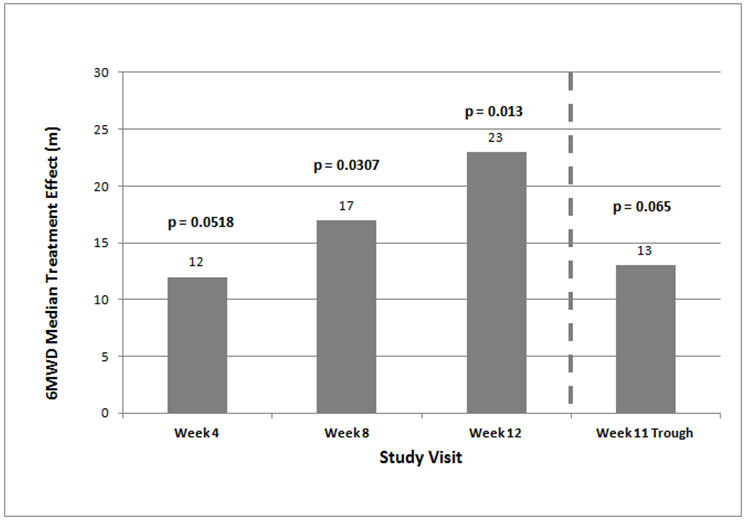
Figure 3: Plot of the Distribution of Peak 6MWD Changes at Week 12 for the Primary Analysis Population (Study 1)
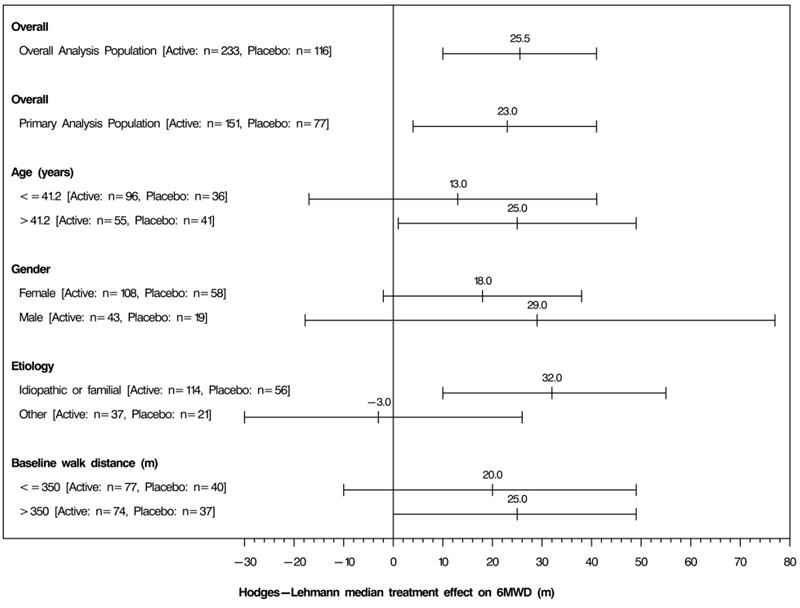
The placebo-corrected median treatment effect on 6MWD was estimated (using the Hodges Lehmann estimator) within various subpopulations defined by age, gender, disease etiology, and baseline 6MWD (Figure 4).
Figure 4: Placebo Corrected Median Treatment Effect (Hodges-Lehmann estimate with 95% CI) on 6MWD Change from Baseline at Week 12 for Various Subgroups in the Primary Analysis Population (Study 1)
Studies 2 and 3 (no effect on a background of ERA, PDE-5 inhibitor, or both)
Studies 2 (N=350) and 3 (N=310) were 16-week, randomized, double-blind, placebo-controlled, international efficacy and safety studies of Orenitram in patients with WHO Group 1 PAH. The primary efficacy endpoint was placebo-corrected change in 6MWD from Baseline to Week 16. Patients were in WHO functional class II (~23%) and class III (~77%) with either idiopathic or heritable PAH (~66%), collagen vascular disease associated PAH (~29%), or PAH associated with HIV (1%) or congenital heart defect (4%). The patients' mean baseline 6MWD was approximately 340 meters. Approximately 40% were receiving both an ERA and a PDE-5 inhibitor. The results did not demonstrate a benefit in exercise testing with median 6MWD at Week 16 (11 meters [Hodges-Lehmann estimate; p=0.072] and 10 meters [Hodges-Lehmann estimate; p=0.089], respectively).
Long-Term Treatment of Pulmonary Hypertension
Patients (N=824) from the placebo-controlled studies entered a long-term, uncontrolled, open-label extension study. The average exposure to Orenitram was approximately 2 years with a maximum exposure of approximately 6 years. The dose of Orenitram continued to increase over time with doses (mean ± SD) of 3.6 ± 2.7, 4.2 ± 3.1, and 5 ± 3.7 mg BID at 6 (n=649), 12 (n=433), and 24 months (n=238), respectively, with a maximum dose of 21 mg BID. Reasons for discontinuation from the study included adverse event (16%), progression of disease (15%), death (13%), and withdrawn consent (7%). In the 522 subjects that completed the 12-month efficacy assessment, their mean 6MWD improved by 24 meters compared to baseline (30 meters in monotherapy patients and 20 meters when Orenitram was used in combination with an ERA and/or a PDE-5 inhibitor). Of the patients that remained in the study, overall survival was 92%, 87%, and 82% at the end of 1, 2, and 3-years, respectively, with progression-free survival (progression defined as death, discontinuation or addition of a PAH therapy) of 74%, 61%, and 47%. Without a control group, these data must be interpreted cautiously.
Remodulin to Orenitram Transition Study
A 24-week, multicenter, open-label study enrolled 33 WHO Group 1 patients on stable doses of Remodulin. All patients received background therapy with a PDE-5 inhibitor and/or ERA. Patients were WHO Functional Class I or II and hemodynamically stable at baseline with a cardiac index >2.2 L/m 2, RAP<11 mmHg, and PVR<10 Woods units. The primary endpoint of the study was the safety and tolerability of the transition. Successful transition was defined as transition from Remodulin to Orenitram at Week 4 (no longer receiving Remodulin) and clinically maintained on Orenitram through Week 24 (as measured by 6MWD and hemodynamics).
All patients transitioned from Remodulin to Orenitram (median time to transition of 3 days) with thirty-one patients (94%) completing transition in 5 days (range 2 to 29 days). Two subjects discontinued Orenitram. The mean Orenitram total daily dose at the end of transition was 27 mg ± 12 mg compared to a mean Remodulin dose prior to transition of 59 ng/kg/min (25 to 111 ng/kg/min). The mean Orenitram total daily dose at Week 24 was 36 mg ± 16 mg. After 24 weeks of treatment with Orenitram, 6MWD and hemodynamics remained stable. Without a control group, these data must be interpreted cautiously.
16 HOW SUPPLIED / STORAGE AND HANDLING
16.1 How Supplied
Orenitram is an 8 mm round biconvex tablet with strength identifying color and printing and supplied as follows:
NDC 69189-0676-1 single dose pack with 1 tablet as repackaged by Avera McKennan Hospital
| Strength | Color | Printing on Tablets | NDC #
100-Count Bottle | NDC #
10-Count Bottle |
|---|---|---|---|---|
| 0.25 mg | Green | UT 0.25 | 66302-302-01 | 66302-302-10 |
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information).
Tell patients:
- Abrupt discontinuation of therapy could result in worsening of PAH symptoms.
- Take Orenitram with food.
- Swallow Orenitram tablets whole. Do not split, chew, crush, or break. Do not take a tablet that is damaged or broken.
- The biologically inert components of the tablet remain intact during gastrointestinal transit and are eliminated in the feces as an insoluble shell.
©Copyright 2017 United Therapeutics Corp. All rights reserved.
United Therapeutics Corp.
Research Triangle Park, NC 27709
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Revised: 01 2016 |
| Patient Information
Orenitram (R) (oh-REN-i-tram) (treprostinil) extended-release tablets |
|
| What is Orenitram?
Orenitram is a prescription medicine used to treat pulmonary arterial hypertension (PAH) which is high blood pressure in the arteries of your lungs. Orenitram may improve your ability to exercise. It is not known if Orenitram is safe and effective in children under 18 years of age. |
|
| Who should not take Orenitram?
Do not take Orenitram if you have severe liver problems. |
|
| What should I tell my healthcare provider before taking Orenitram?
Before you take Orenitram, tell your healthcare provider if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Orenitram and other medicines may affect each other causing side effects. Do not start any new medicine until you check with your healthcare provider. Especially tell your healthcare provider if you take another medicine that contains treprostinil, such as Remodulin ® or Tyvaso ®. Know the medicines you take. Keep a list of them to show to your healthcare provider and pharmacist when you get a new medicine. |
|
How should I take Orenitram?
|
|
| What are the possible side effects of Orenitram?
Orenitram can cause serious side effects, including an increased risk of bleeding. The most common side effects of Orenitram include:
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Orenitram. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store Orenitram?
Keep Orenitram and all medicines out of the reach of children. |
|
| General information about the safe and effective use of Orenitram.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Orenitram for a condition for which it was not prescribed. Do not give Orenitram to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about Orenitram that is written for health professionals. |
|
| What are the ingredients in Orenitram?
Active ingredient: treprostinil Inactive ingredients: xylitol, maltodextrin, sodium lauryl sulfate, magnesium stearate, cellulose acetate, triethyl citrate, polyvinyl alcohol, titanium dioxide, polyethylene glycol, and talc. In addition tablets may contain colorants FD&C Blue #2, iron oxide yellow, and iron oxide red. The imprinting ink contains shellac glaze, ethanol, isopropyl alcohol, iron oxide black, n-butyl alcohol, and propylene glycol. United Therapeutics Corp.,Research Triangle Park, NC 27709 USA
|
|
| ORENITRAM
treprostinil tablet, extended release |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| Labeler - Avera McKennan Hospital (068647668) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Avera McKennan Hospital | 068647668 | relabel(69189-0676) , repack(69189-0676) | |