Label: GLEOLAN- aminolevulinic acid hydrochloride powder, for solution
- NDC Code(s): 59137-231-01
- Packager: Medexus Pharma, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated January 10, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use GLEOLAN safely and effectively. See full prescribing information for GLEOLAN.
GLEOLAN® (aminolevulinic acid hydrochloride) for oral solution
Initial U.S. Approval: [1999]INDICATIONS AND USAGE
Gleolan is an optical imaging agent indicated in patients with glioma (suspected World Health Organization Grades III or IV on preoperative imaging) as an adjunct for the visualization of malignant tissue during surgery. ( 1)
DOSAGE AND ADMINISTRATION
- For oral use only ( 2.1)
- Recommended reconstituted oral dose of Gleolan is 20 mg/kg. ( 2.1)
- Administer Gleolan to patient orally 3 hours (range 2 to 4 hours) before anesthesia. ( 2.1)
- See Full Prescribing Information for reconstitution information. ( 2.2)
- Use appropriate visualization techniques with appropriate surgical microscopes and light source filters. ( 2.4)
DOSAGE FORMS AND STRENGTHS
For oral solution: 1,500 mg aminolevulinic acid hydrochloride lyophilized powder, equivalent to 1,170 mg aminolevulinic acid per vial. The reconstituted aminolevulinic acid hydrochloride solution contains 30 mg per mL and is clear and colorless to slightly yellowish in color. ( 3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Phototoxic reactions: Do not administer phototoxic drugs (St. John's wort, griseofulvin, thiazide diuretics, sulfonylureas, phenothiazines, sulphonamides, quinolones and tetracyclines), and topical preparations containing ALA for 24 hours during the perioperative period. Reduce exposure to sunlight or room lights for 48 hours after oral administration of Gleolan. ( 5.1, 7)
- Risk of misinterpretation: Non-fluorescing tissue in the surgical field does not rule out the presence of tumor. ( 5.2, 14)
ADVERSE REACTIONS
- Adverse reactions occurring in >1% of patients in the week following surgery were pyrexia, hypotension, nausea, and vomiting. ( 6.1)
- Adverse reactions occurring in < 1% of patients in the first 6 weeks after surgery were: chills, photosensitivity reaction, solar dermatitis, hypotension, abnormal liver function test, and diarrhea. ( 6.1)
- Neurologic events related to the surgical procedure occurred in 29% of patients and included: aphasia, hemiparesis, hemianopia, headache, seizure, hemiplegia, monoparesis, hypoesthesia, and brain edema. ( 6.1)
- Elevated liver enzymes occurred in clinical studies. There were no cases of liver failure. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact NXDC toll-free at (844) 517-5252 and adverseevents@nxdevcorp.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
2.2 Reconstitution of Gleolan
2.3 Gleolan Administration
2.4 Imaging Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Phototoxic Reaction
5.2 Risk of Misinterpretation
5.3 Hypersensitivity Reactions
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Post Marketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal Impairment
8.7 Patients with Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
11.1 Chemical Properties
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
- For oral use only
- The recommended oral dose of reconstituted Gleolan is 20 mg / kg body weight. More than 1 vial may be required.
2.2 Reconstitution of Gleolan
Gleolan powder must be reconstituted prior to administration by a healthcare provider according to the following instructions:
- Determine the total number of vials needed to achieve the intended dose for the patient according to the equation below (rounded up to the nearest whole vial):
# of vials= Patient Body Weight (kg) 75 kg / vial - Completely removethe white cap and aluminum crimp seal from each vial.
- Remove and retain the rubber stopper from the vial.
- Using an appropriate volumetric measuring device (e.g., flask, graduated cylinder, dosing syringe), measure 50 mL of drinking water and add to each vial containing 1,500 mg of Gleolan.
- Gently swirl the vial to completely dissolve the powder.
- The resulting reconstituted solution (30 mg of Gleolan per mL) is clear and colorless to slightly yellowish.
- If required, replace the stopper and store reconstituted solution for up to 24 hours at room temperature prior to administration.
2.3 Gleolan Administration
Gleolan is for ORAL USE ONLY. The reconstituted Gleolan solution is administered according to the following steps:
- Calculate the administration volume, in mL, to achieve the intended dose according to the following equation:
Administration Volume (mL) = Patient Body Weight (kg)* 20 mg/kg 30 mg/mL - Transfer the entire contents of the prepared vial(s) into an appropriate dosing container (e.g., oral medicine bottle); ensure the entire contents of the vials are transferred.
- After transfer, discard the empty vial(s).
- Using a disposable volumetric syringe, remove the administration volume of reconstituted Gleolan solution from the dosing container and transfer to a separate oral dosing container.
- Discard unneeded volume of Gleolan solution.
- Administer orally 3 hours (range 2 to 4 hours) prior to induction of anesthesia.
2.4 Imaging Instructions
- Gleolan must be used with a standard surgical operating microscope adapted with a blue light emitting light source (power density 40-80 mW/cm 2) and ancillary excitation and emission filters to visualize fluorescence excitation in the wavelength of 375 to 440 nm and for observation from 620 to 710 nm. Filters transmit porphyrin fluorescence as red-violet, as well as a fraction of backscattered blue excitation light necessary for distinguishing nonfluorescing tissue.
- Gleolan should only be used by neurosurgeons who have completed a training program on use of fluorescence in surgery. Training is provided by the distributor.
-
3 DOSAGE FORMS AND STRENGTHS
For oral solution: 1,500 mg aminolevulinic acid hydrochloride (ALA HCl) lyophilized powder, equivalent to 1,170 mg aminolevulinic acid (ALA) , in a 50 mL single-dose clear, colorless, glass vial with rubber stopper. After reconstitution with 50 mL drinking water, the solution contains 30 mg per mL of aminolevulinic acid hydrochloride (equivalent to 23.4 mg per mL of aminolevulinic acid) and is clear and colorless to slightly yellowish in color.
-
4 CONTRAINDICATIONS
- Hypersensitivity to the aminolevulinic acid (ALA) or porphyrins. [see Warnings and Precautions (5.3)]
- Acute or chronic types of porphyria, due to potential ineffectiveness of the drug in these patients.
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Phototoxic Reaction
Due to the risk of phototoxic reactions, do not administer phototoxic drugs (St. John's wort, griseofulvin, thiazide diuretics, sulfonylureas, phenothiazines, sulphonamides, quinolones and tetracyclines), and topical preparations containing ALA for 24 hours during the perioperative period [see Drug Interactions (7)] . Reduce exposure to sunlight or room lights for 48 hours after administration of Gleolan.
5.2 Risk of Misinterpretation
Errors may occur with the use of Gleolan for intraoperative visualization of malignant glioma, including false negatives and false positives. Non-fluorescing tissue in the surgical field does not rule out the presence of tumor in patients with glioma [see Clinical Studies (14)] . Fluorescence may be seen in areas of inflammation or metastases from other tumor types.
5.3 Hypersensitivity Reactions
Hypersensitivity reactions, including serious hypersensitivity reactions have occurred; these reactions include anaphylactic shock, swelling, and urticaria [see Contraindications (4), Adverse Reactions (6.2)] . Always have cardiopulmonary resuscitation personnel and equipment readily available and monitor all patients for hypersensitivity reactions.
-
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of Gleolan is supported by data from 5 open label clinical studies, which included 527 patients with glioma who received ALA HCl. Adverse reactions that occurred in > 1% of patients in the week following surgery were pyrexia, hypotension, nausea, and vomiting. Adverse reactions occurring in the first 6 weeks after surgery in < 1% of patients were: chills, photosensitivity reaction, solar dermatitis, hypotension, abnormal liver function test, and diarrhea. One patient experienced respiratory failure due to drug overdose [see Overdosage (10)] .
Neurologic Events
Nervous system disorders occurred in 29% of patients within the first week after surgery. Events occurring in > 1% of patients included aphasia (8%), hemiparesis (7.8%), hemianopsia (3.2%), headache (2.7%), seizure (1.9%), hemiplegia (1.9%), monoparesis (1.3%) and hypoesthesia (1.1%). Brain edema occurred in < 1 % of patients in the first 6 weeks after surgery. In a randomized clinical trial (Study 3), the numbers of serious neurologic adverse events in the post operative period were higher in patients randomized to ALA fluorescence arm compared to the control arm. An imbalance was notable for the adverse events aphasia, ataxia, convulsion and hemianopsia, and is likely related to the higher amount of brain resection performed in the ALA arm. At longer follow up periods, the numbers between the two arms appeared similar [see Clinical Trials (14)] .
Elevated Liver Enzymes
Worsening of ≥ 2 Common Toxicity Criteria (CTC) grades in alanine aminotransferase (ALT) and gamma-glutamyl transferase (GGT) occurred in (15.8% and 11.6%, respectively) within the first week after surgery. Absolute levels ranged from 2 times to greater than 10 times the upper limit of normal (ULN) for each parameter. At 6 weeks, ALT remained elevated in 2.9% of patients (range 2 to greater than 5 × ULN), and GGT was elevated in 7.5% of patients (range 2 to greater than 10 × ULN). No cases of liver failure occurred.
6.2 Post Marketing Experience
The following adverse reactions are among those that have been identified during post-approval use of Gleolan outside of the United States. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune Disorders: anaphylactic shock, angioedema, drug eruption, urticaria, erythema.
Metabolism and Nutrition Disorders: metabolic acidosis.
-
7 DRUG INTERACTIONS
Phototoxic Drugs
Patients exposed to a photosensitizing agent may experience a phototoxic skin reaction (severe sunburn). Due to the risk of possible phototoxic reactions, avoid administering phototoxic drugs such as St. John's wort, griseofulvin, thiazide diuretics, sulfonylureas, phenothiazines, sulphonamides, quinolones and tetracyclines, and topical preparations containing ALA for 24 hours before and after administration of Gleolan.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available human data on Gleolan in pregnant women to inform a drug associated risk of adverse developmental outcomes. In animal reproduction studies, no adverse developmental effects were observed with oral ALA HCl administration to pregnant rabbits during organogenesis at doses 3 times the maximum recommended human oral dose (see Data) .
The estimated background risk of major birth defects and miscarriage for the indicated populations are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Animal data
ALA HCl was administered to rabbits at oral doses of 15, 50 and 150 mg/kg/day [approximately 0.1, 0.6, and 3 times the maximum human recommended dose (MHRD), respectively based on AUC comparisons] from gestation days 6-18. The no-observed-adverse-effect level (NOAEL) for maternal toxicity was 50 mg/kg/day and the NOAEL for embryo-fetal developmental toxicity was 150 mg/kg/day.
8.2 Lactation
Risk summary
There are no data on the presence of ALA HCl in either human or animal milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Gleolan and any potential adverse effects on the breastfed infant from Gleolan or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of Gleolan in pediatric patients have not been established.
8.5 Geriatric Use
Of 527 subjects in clinical studies of Gleolan, 182 were 65 to < 75 years of age and 7 were ≥ 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. No dose adjustment is required in elderly patients.
8.6 Patients with Renal Impairment
Because approximately one third of the ALA dose is excreted in urine as parent drug, ALA clearance may be reduced in patients with renal impairment; it is not known if dose adjustment is needed [see Clinical Pharmacology (12.3)] .
8.7 Patients with Hepatic Impairment
The contribution of the liver to the elimination of ALA following Gleolan dosing is unknown. ALA clearance may be reduced in patients with hepatic impairment; it is not known if dose adjustment is needed [see Clinical Pharmacology (12.3)] .
- 10 OVERDOSAGE
-
11 DESCRIPTION
11.1 Chemical Properties
Gleolan (aminolevulinic acid hydrochloride) is an optical imaging agent for oral solution. The 50-mL, clear vial contains 1,500 mg of lyophilized aminolevulinic acid hydrochloride powder (equivalent to 1,170 mg aminolevulinic acid). After reconstitution, the product has a concentration of 30 mg aminolevulinic acid hydrochloride per mL (equivalent to 23.4 mg aminolevulinic acid per mL). The chemical name is 5-amino-4-oxo-pentanoic acid hydrochloride. The chemical formula for aminolevulinic acid hydrochloride is C 5H 10ClNO 3. Its molecular weight is 167.59 g/mol with the following structural formula:

-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ALA occurs endogenously as a metabolite that is formed in the mitochondria from succinyl-CoA and glycine. Exogenous administration of ALA leads to accumulation of the ALA metabolite PpIX in tumor cells. The reason for the accumulation of PpIX in neoplastic brain tissue is not known.
During glioma surgery, Gleolan is used with an operating microscope adapted with a blue emitting light source (power density 40-80 mW/cm 2) and filters for excitation light of wavelength 375 to 440 nm, and observation at wavelengths of 620 to 710 nm. This allows tumor tissue to be visualized as red fluorescence. Tissue lacking sufficient PpIX concentrations appears blue.
12.2 Pharmacodynamics
The effect of the timing of the Gleolan dosing on fluorescence intensity in brain tissue is unknown. The relationship between systemic ALA plasma concentrations at the time of visualization and fluorescence intensity in brain is also unknown. The dose of 20 mg / kg provided stronger ALA-induced fluorescence in glioma tissue by both visual and spectrophotometric assessment compared to lower doses tested.
12.3 Pharmacokinetics
In 12 healthy subjects, the mean half-life of ALA following the recommended dose of Gleolan solution was 0.9 ± 1.2 hours (mean ± std dev) with a range of 0.8 to 1.3 hours. Maximum concentrations of the PpIX metabolite (T maxfor PpIX) occurred with a median of 4 hours and a range of 1.2 to 7.8 hours. The elimination half-life of PpIX was 3.6 ± 1.8 hours (mean ± std dev) with a range of 1.2 to 7.8 hours.
Absorption
In 12 healthy subjects, the absolute bioavailability of ALA following the recommended dose of Gleolan solution was 100.0% ± 1.1 with a range of 78.5% to 131.2%. Maximum ALA plasma concentrations were reached with a median of 0.8 hour (range 0.5 – 1.0 hour).
Distribution
In in vitro experiments using ALA concentrations up to approximately 25% of the maximal concentration that occurs in plasma following the recommended dose of Gleolan solution, the mean protein binding of ALA was 12%.
Elimination
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
-
14 CLINICAL STUDIES
The efficacy of 20 mg / kg ALA HCl was evaluated in 3 clinical studies (Study 1-3) involving patients, ages 18 to 75 years old, who had a preoperative MRI compatible with high-grade glioma (WHO Grade III or IV) and were undergoing surgical resection.
Study 1 was an open-label study of 33 patients with newly diagnosed high-grade glioma and Study 2 was an open-label study of 36 patients with recurrent high-grade glioma. In Studies 1 and 2, after initial debulking was carried out under white light, biopsies were obtained under fluorescent light from fluorescent and nonfluorescent sites. Presence of fluorescence (positive/negative) was compared to tumor status (true/false) using histopathology as the reference standard. True positives and false positives among fluorescent biopsies and true negatives and false negatives among nonfluorescent biopsies are provided in Table 1.
Study 3 was a randomized, multicenter study in 415 patients with a preoperative diagnosis of high-grade glioma by MRI. Patients were randomized in 1:1 ratio to ALA fluorescence arm or to white light control arm. Biopsies were obtained from tumor-core, tumor-margin and regions just distant to the tumor margins. In 349 patients high grade glioma was confirmed by a blinded central read and histopathology. The remaining patients were diagnosed with metastatic disease, abscess, low-grade glioma or other conditions.
In patients with confirmed high-grade glioma randomized to the ALA fluorescence arm, presence of fluorescence at a biopsy level was compared to tumor status using histopathology as the reference standard (Table 1). In 4 patients with low-grade glioma (WHO Grade I or II) who received ALA HCl, 9 out of 10 biopsies were false negative.
The extent of resection among patients with confirmed high-grade glioma in the ALA fluorescence arm was compared to that among patient in the control arm, with the "completeness" of resection being determined by a central blinded read of early post-surgical MRI. Percentage of patients who had "completeness" of resection was 64% in the ALA arm and 38% in the control arm, with the difference of 26% [95% CI: (16%, 36%)].
Table 1. Presence of Fluorescence Compared to Histopathology (biopsy level) Study 1
(N=297) *Study 2
(N=370) *Study 3
(N=479) *- *
- N is Number of total (fluorescent and non-fluorescent) biopsies
Number of Fluorescent Biopsies 185 354 319 True Positive 178 342 312 False Positive 7 12 7 Number of Nonfluorescent Biopsies 112 16 160 True Negative 27 3 30 False Negative 85 13 130 - 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise patients that they may experience elevated liver enzymes (ALT and GGT) within the first week after surgery. This elevation may persist after 6 weeks.
Advise patients to reduce exposure to sunlight or room lights for 48 hours after administration of Gleolan due to risk of phototoxic reactions.
- SPL UNCLASSIFIED SECTION
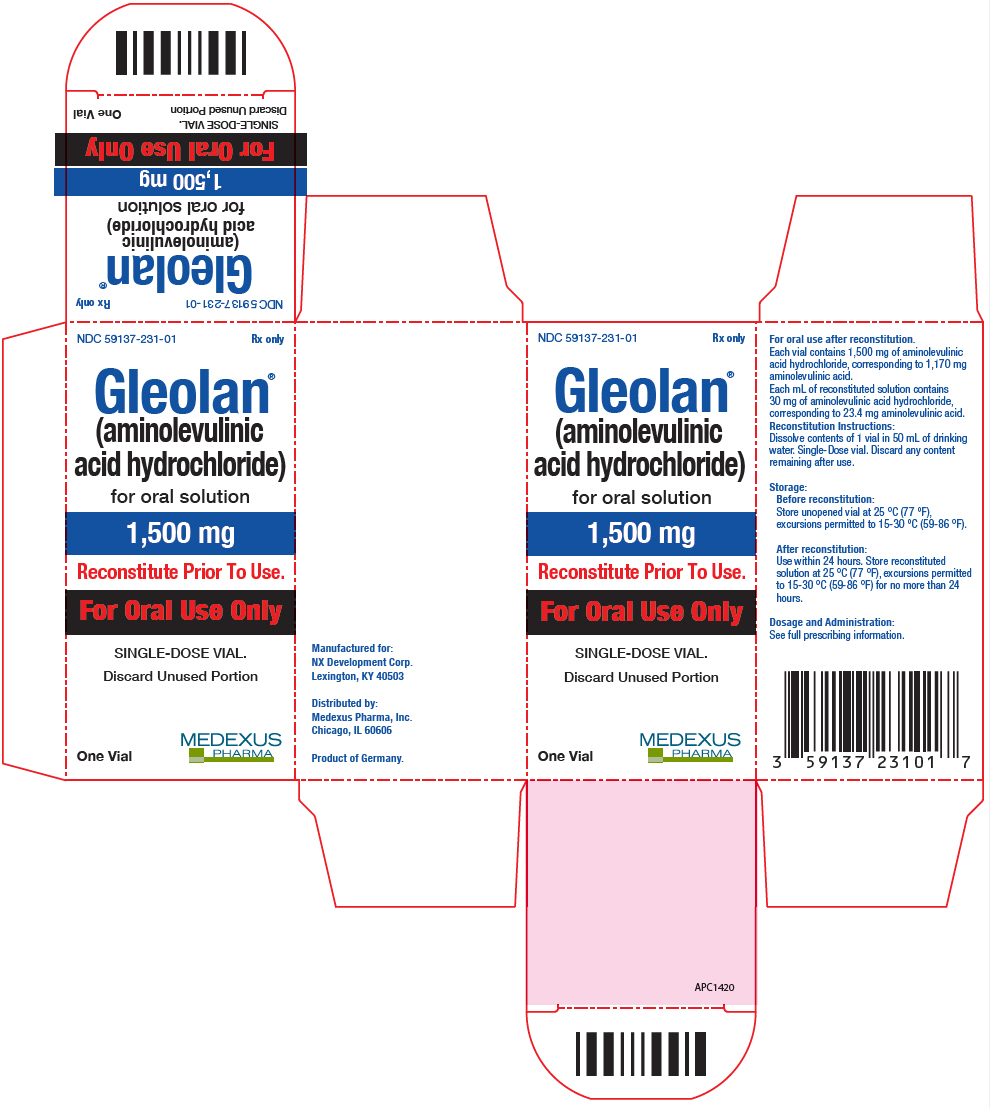
- PRINCIPAL DISPLAY PANEL - 1,500 mg Vial Carton
-
INGREDIENTS AND APPEARANCE
GLEOLAN
aminolevulinic acid hydrochloride powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:59137-231 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMINOLEVULINIC ACID HYDROCHLORIDE (UNII: V35KBM8JGR) (AMINOLEVULINIC ACID - UNII:88755TAZ87) AMINOLEVULINIC ACID HYDROCHLORIDE 1500 mg Product Characteristics Color white (CLEAR TO SLIGHTLY YELLOWISH) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:59137-231-01 1 in 1 CARTON 03/01/2022 1 1 in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA208630 04/14/2018 Labeler - Medexus Pharma, Inc. (078811131) Registrant - NX Development Corp (079994320)