CERVARIX- human papillomavirus bivalent (types 16 and 18) vaccine, recombinant injection, suspension
GlaxoSmithKline Biologicals SA
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use CERVARIX safely and effectively. See full prescribing information for CERVARIX.
CERVARIX [Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant] Suspension for Intramuscular Injection Initial U.S. Approval: 2009 INDICATIONS AND USAGECERVARIX is a vaccine indicated for the prevention of the following diseases caused by oncogenic human papillomavirus (HPV) types 16 and 18:
CERVARIX is approved for use in females 9 through 25 years of age. Limitations of Use and Effectiveness (1.2) DOSAGE AND ADMINISTRATIONThree doses (0.5-mL each) by intramuscular injection according to the following schedule: 0, 1, and 6 months. (2.2) DOSAGE FORMS AND STRENGTHSSingle-dose prefilled syringes containing a 0.5-mL suspension for injection. (3) CONTRAINDICATIONSSevere allergic reactions (e.g., anaphylaxis) to any component of CERVARIX. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov DRUG INTERACTIONSDo not mix CERVARIX with any other vaccine in the same syringe or vial. (7.1) USE IN SPECIFIC POPULATIONSSee 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 4/2016 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Indications
CERVARIX® is indicated for the prevention of the following diseases caused by oncogenic human papillomavirus (HPV) types 16 and 18 [see Clinical Studies (14)]:
- •
- cervical cancer,
- •
- cervical intraepithelial neoplasia (CIN) Grade 2 or worse and adenocarcinoma in situ, and
- •
- cervical intraepithelial neoplasia (CIN) Grade 1.
CERVARIX is approved for use in females 9 through 25 years of age.
1.2 Limitations of Use and Effectiveness
CERVARIX does not provide protection against disease due to all HPV types [see Clinical Studies (14.3)].
CERVARIX has not been demonstrated to provide protection against disease from vaccine and non-vaccine HPV types to which a woman has previously been exposed through sexual activity [see Clinical Studies (14.2)].
Females should continue to adhere to recommended cervical cancer screening procedures [see Patient Counseling Information (17)].
Vaccination with CERVARIX may not result in protection in all vaccine recipients.
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
Shake syringe well before withdrawal and use. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If either of these conditions exists, the vaccine should not be administered. With thorough agitation, CERVARIX is a homogeneous, turbid, white suspension. Do not administer if it appears otherwise.
Attach a sterile needle and administer intramuscularly.
Do not administer this product intravenously, intradermally, or subcutaneously.
3 DOSAGE FORMS AND STRENGTHS
CERVARIX is a suspension for intramuscular injection available in 0.5-mL single-dose prefilled TIP-LOK® syringes.
4 CONTRAINDICATIONS
Severe allergic reactions (e.g., anaphylaxis) to any component of CERVARIX [see Description (11)].
5 WARNINGS AND PRECAUTIONS
5.1 Syncope
Because vaccinees may develop syncope, sometimes resulting in falling with injury, observation for 15 minutes after administration is recommended. Syncope, sometimes associated with tonic-clonic movements and other seizure-like activity, has been reported following vaccination with CERVARIX. When syncope is associated with tonic-clonic movements, the activity is usually transient and typically responds to restoring cerebral perfusion by maintaining a supine or Trendelenburg position.
5.2 Latex
The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions.
5.3 Preventing and Managing Allergic Vaccine Reactions
Prior to administration, the healthcare provider should review the immunization history for possible vaccine hypersensitivity and previous vaccination‑related adverse reactions to allow an assessment of benefits and risks. Appropriate medical treatment and supervision should be readily available in case of anaphylactic reactions following administration of CERVARIX.
6 ADVERSE REACTIONS
The most common local adverse reactions (≥20% of subjects) were pain, redness, and swelling at the injection site.
The most common general adverse events (≥20% of subjects) were fatigue, headache, myalgia, gastrointestinal symptoms, and arthralgia.
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared with rates in the clinical trials of another vaccine, and may not reflect the rates observed in practice. There is the possibility that broad use of CERVARIX could reveal adverse reactions not observed in clinical trials.
Studies in Females 9 through 25 Years of Age
The safety of CERVARIX was evaluated by pooling data from controlled and uncontrolled clinical trials involving 23,952 females 9 through 25 years of age in the pre-licensure clinical development program. In these studies, 13,024 females (9 through 25 years of age) received at least one dose of CERVARIX and 10,928 females received at least one dose of a control [Hepatitis A Vaccine containing 360 EL.U. (10 through 14 years of age), Hepatitis A Vaccine containing 720 EL.U. (15 through 25 years of age), or Al(OH)3 (500 mcg, 15 through 25 years of age)].
Data on solicited local and general adverse events were collected by subjects or parents using standardized diary cards for 7 consecutive days following each vaccine dose (i.e., day of vaccination and the next 6 days). Unsolicited adverse events were recorded with diary cards for 30 days following each vaccination (day of vaccination and 29 subsequent days). Parents and/or subjects were also asked at each study visit about the occurrence of any adverse events and instructed to immediately report serious adverse events throughout the study period. These studies were conducted in North America, Latin America, Europe, Asia, and Australia. Overall, the majority of subjects were white (59.5%), followed by Asian (25.9%), Hispanic (8.5%), black (3.4%), and other racial/ethnic groups (2.7%).
Solicited Adverse Events: The reported frequencies of solicited local injection site reactions (pain, redness, and swelling) and general adverse events (fatigue, fever, gastrointestinal symptoms, headache, arthralgia, myalgia, and urticaria) within 7 days after vaccination in females 9 through 25 years of age are presented in Table 1. An analysis of solicited local injection site reactions by dose is presented in Table 2. Local reactions were reported more frequently with CERVARIX when compared with the control groups; in ≥76% of recipients of CERVARIX, these local reactions were mild to moderate in intensity. Compared with Dose 1, pain was reported less frequently after Doses 2 and 3 of CERVARIX, in contrast to redness and swelling where there was a small increased incidence. There was no increase in the frequency of general adverse events with successive doses.
|
CERVARIX (9-25 years) % |
HAV 720b (15-25 years) % |
HAV 360c (10-14 years) % |
Al(OH)3 Controld (15-25 years) % |
|
|
Local Adverse Reaction |
N = 6,669 |
N = 3,079 |
N = 1,027 |
N = 549 |
|
Pain |
91.9 |
78.0 |
64.2 |
87.2 |
|
Redness |
48.4 |
27.6 |
25.2 |
24.4 |
|
Swelling |
44.3 |
19.8 |
17.3 |
21.3 |
|
General Adverse Event |
N = 6,670 |
N = 3,079 |
N = 1,027 |
N = 549 |
|
Fatigue |
54.6 |
53.7 |
42.3 |
53.6 |
|
Headache |
53.4 |
51.3 |
45.2 |
61.4 |
|
GIe |
27.9 |
27.3 |
24.6 |
32.8 |
|
Fever (≥99.5°F) |
12.9 |
10.9 |
16.0 |
13.5 |
|
Rash |
9.5 |
8.4 |
6.7 |
10.0 |
|
N = 6,119 |
N = 3,079 |
N = 1,027 |
— |
|
|
Myalgiaf |
48.8 |
44.9 |
33.1 |
— |
|
Arthralgiaf |
20.7 |
17.9 |
19.9 |
— |
|
Urticariaf |
7.2 |
7.9 |
5.4 |
— |
aTotal vaccinated cohort included subjects with at least one documented dose (N).
bHAV 720 = Hepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
cHAV 360 = Hepatitis A Vaccine control group [360 EL.U. of antigen and 250 mcg of Al(OH)3].
dAl(OH)3 Control = Control containing 500 mcg Al(OH)3.
eGI = Gastrointestinal symptoms, including nausea, vomiting, diarrhea, and/or abdominal pain.
fAdverse events solicited in a subset of subjects.
|
CERVARIX (9-25 years) % |
HAV 720b (15-25 years) % |
HAV 360c (10-14 years) % |
Al(OH)3 Controld (15-25 years) % |
|||||||||
|
Post-dose |
Post-dose |
Post-dose |
Post-dose |
|||||||||
|
1 |
2 |
3 |
1 |
2 |
3 |
1 |
2 |
3 |
1 |
2 |
3 |
|
|
N |
6,653 |
6,428 |
6,168 |
3,070 |
2,919 |
2,758 |
1,027 |
1,021 |
1,011 |
546 |
521 |
500 |
|
Pain |
87.0 |
76.4 |
78.5 |
65.6 |
54.4 |
56.1 |
48.5 |
38.5 |
36.9 |
79.1 |
66.8 |
72.4 |
|
Pain, Grade 3e |
7.5 |
5.6 |
7.7 |
2.0 |
1.4 |
2.0 |
0.8 |
0.2 |
1.6 |
9.0 |
6.0 |
8.6 |
|
Redness |
28.4 |
30.1 |
35.7 |
16.6 |
15.2 |
16.1 |
15.6 |
13.3 |
12.1 |
11.5 |
11.5 |
15.6 |
|
Redness, >50 mm |
0.2 |
0.5 |
1.0 |
0.1 |
0.1 |
0.0 |
0.1 |
0.2 |
0.1 |
0.2 |
0.0 |
0.0 |
|
Swelling |
22.8 |
25.5 |
32.7 |
10.5 |
9.4 |
10.5 |
9.4 |
8.6 |
7.6 |
10.3 |
10.4 |
12.0 |
|
Swelling, >50 mm |
1.1 |
1.0 |
1.3 |
0.2 |
0.2 |
0.2 |
0.4 |
0.3 |
0.0 |
0.0 |
0.0 |
0.0 |
aTotal vaccinated cohort included subjects with at least one documented dose (N).
bHAV 720 = Hepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
cHAV 360 = Hepatitis A Vaccine control group [360 EL.U. of antigen and 250 mcg of Al(OH)3].
dAl(OH)3 Control = Control containing 500 mcg Al(OH)3.
eDefined as spontaneously painful or pain that prevented normal daily activities.
The pattern of solicited local adverse reactions and general adverse events following administration of CERVARIX was similar between the age cohorts (9 through 14 years and 15 through 25 years).
Unsolicited Adverse Events: The frequency of unsolicited adverse events that occurred within 30 days of vaccination (≥1% for CERVARIX and greater than any of the control groups) in females 9 through 25 years of age are presented in Table 3.
|
CERVARIX % |
HAV 720b % |
HAV 360c % |
Al(OH)3 Controld % |
|
|
N = 6,893 |
N = 3,186 |
N = 1,032 |
N = 581 |
|
|
Headache |
5.2 |
7.6 |
3.3 |
9.3 |
|
Nasopharyngitis |
3.7 |
3.4 |
5.9 |
3.3 |
|
Influenza |
3.1 |
5.6 |
1.3 |
1.9 |
|
Pharyngolaryngeal pain |
2.9 |
2.7 |
2.2 |
2.2 |
|
Dizziness |
2.2 |
2.6 |
1.5 |
3.1 |
|
Upper respiratory infection |
2.0 |
1.3 |
6.7 |
1.5 |
|
Chlamydia infection |
1.9 |
4.4 |
0.0 |
0.0 |
|
Dysmenorrhea |
1.9 |
2.3 |
1.9 |
4.0 |
|
Pharyngitis |
1.4 |
1.8 |
2.2 |
0.5 |
|
Injection site bruising |
1.4 |
1.8 |
0.7 |
1.5 |
|
Vaginal infection |
1.3 |
2.2 |
0.1 |
0.9 |
|
Injection site pruritus |
1.3 |
0.5 |
0.6 |
0.2 |
|
Back pain |
1.1 |
1.3 |
0.7 |
3.1 |
|
Urinary tract infection |
1.0 |
1.4 |
0.3 |
1.2 |
aTotal vaccinated cohort included subjects with at least one dose administered (N).
bHAV 720 = Hepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
cHAV 360 = Hepatitis A Vaccine control group [360 EL.U. of antigen and 250 mcg of Al(OH)3].
dAl(OH)3 Control = Control containing 500 mcg Al(OH)3.
New Onset Autoimmune Diseases (NOADs): The pooled safety database, which included controlled and uncontrolled trials which enrolled females 9 through 25 years of age, was searched for new medical conditions indicative of potential new onset autoimmune diseases. Overall, the incidence of potential NOADs, as well as NOADs, in the group receiving CERVARIX was 0.8% (96/12,772) and comparable to the pooled control group (0.8%, 87/10,730) during the 4.3 years of follow-up (Table 4).
In the largest randomized, controlled trial (Study 2) which enrolled females 15 through 25 years of age and which included active surveillance for potential NOADs, the incidence of potential NOADs and NOADs was 0.8% among subjects who received CERVARIX (78/9,319) and 0.8% among subjects who received Hepatitis A Vaccine [720 EL.U. of antigen and 500 mcg Al(OH)3] control (77/9,325).
|
CERVARIX N = 12,772 |
Pooled Control Groupb N = 10,730 |
|
|
n (%)c |
n (%)c |
|
|
Total Number of Subjects with at Least One Medical Condition |
96 (0.8) |
87 (0.8) |
|
Arthritisd |
9 (0.1) |
4 (0.0) |
|
Celiac disease |
2 (0.0) |
5 (0.0) |
|
Dermatomyositis |
0 (0.0) |
1 (0.0) |
|
Diabetes mellitus insulin-dependent (Type 1 or unspecified) |
5 (0.0) |
5 (0.0) |
|
Erythema nodosum |
3 (0.0) |
0 (0.0) |
|
Hyperthyroidisme |
15 (0.1) |
15 (0.1) |
|
Hypothyroidismf |
30 (0.2) |
28 (0.3) |
|
Inflammatory bowel diseaseg |
8 (0.1) |
4 (0.0) |
|
Multiple sclerosis |
4 (0.0) |
1 (0.0) |
|
Myelitis transverse |
1 (0.0) |
0 (0.0) |
|
Optic neuritis/Optic neuritis retrobulbar |
3 (0.0) |
1 (0.0) |
|
Psoriasish |
8 (0.1) |
11 (0.1) |
|
Raynaud’s phenomenon |
0 (0.0) |
1 (0.0) |
|
Rheumatoid arthritis |
4 (0.0) |
3 (0.0) |
|
Systemic lupus erythematosusi |
2 (0.0) |
3 (0.0) |
|
Thrombocytopeniaj |
1 (0.0) |
1 (0.0) |
|
Vasculitisk |
1 (0.0) |
3 (0.0) |
|
Vitiligo |
2 (0.0) |
2 (0.0) |
aTotal vaccinated cohort included subjects with at least one documented dose (N).
bPooled Control Group = Hepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3], Hepatitis A Vaccine control group [360 EL.U. of antigen and 250 mcg of Al(OH)3], and a control containing 500 mcg Al(OH)3.
cn (%): Number and percentage of subjects with medical condition.
dTerm includes reactive arthritis and arthritis.
eTerm includes Basedow's disease, goiter, and hyperthyroidism.
fTerm includes thyroiditis, autoimmune thyroiditis, and hypothyroidism.
gTerm includes colitis ulcerative, Crohn's disease, proctitis ulcerative, and inflammatory bowel disease.
hTerm includes psoriatic arthropathy, nail psoriasis, guttate psoriasis, and psoriasis.
iTerm includes systemic lupus erythematosus and cutaneous lupus erythematosus.
jTerm includes idiopathic thrombocytopenic purpura and thrombocytopenia.
kTerm includes leukocytoclastic vasculitis and vasculitis.
Serious Adverse Events
In the pooled safety database, inclusive of controlled and uncontrolled studies, which enrolled females 9 through 72 years of age, 5.3% (864/16,381) of subjects who received CERVARIX and 5.9% (814/13,811) of subjects who received control reported at least one serious adverse event, without regard to causality, during the entire follow-up period (up to 7.4 years).
Among females 9 through 25 years of age enrolled in these clinical studies, 6.3% of subjects who received CERVARIX and 7.2% of subjects who received the control reported at least one serious adverse event during the entire follow-up period (up to 7.4 years).
Deaths
In completed and ongoing studies which enrolled 57,323 females 9 through 72 years of age, 37 deaths were reported during the 7.4 years of follow-up: 20 in subjects who received CERVARIX (0.06%, 20/33,623) and 17 in subjects who received control (0.07%, 17/23,700). Causes of death among subjects were consistent with those reported in adolescent and adult female populations. The most common causes of death were motor vehicle accident (5 subjects who received CERVARIX; 5 subjects who received control) and suicide (2 subjects who received CERVARIX; 5 subjects who received control), followed by neoplasm (3 subjects who received CERVARIX; 2 subjects who received control), autoimmune disease (3 subjects who received CERVARIX; 1 subject who received control), infectious disease (3 subjects who received CERVARIX; 1 subject who received control), homicide (2 subjects who received CERVARIX; 1 subject who received control), cardiovascular disorders (2 subjects who received CERVARIX), and death of unknown cause (2 subjects who received control). Among females 10 through 25 years of age, 31 deaths were reported (0.05%, 16/29,467 of subjects who received CERVARIX and 0.07%, 15/20,192 of subjects who received control).
6.2 Postmarketing Experience
In addition to reports in clinical trials, worldwide voluntary reports of adverse events received for CERVARIX since market introduction (2007) are listed below. This list includes serious events or events that have suspected causal association to CERVARIX. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccination.
Blood and Lymphatic System Disorders
Lymphadenopathy.
Immune System Disorders
Allergic reactions (including anaphylactic and anaphylactoid reactions), angioedema, erythema multiforme.
Nervous System Disorders
Syncope or vasovagal responses to injection (sometimes accompanied by tonic-clonic movements).
7 DRUG INTERACTIONS
7.1 Concomitant Vaccine Administration
There are no data to assess the concomitant use of CERVARIX with other vaccines.
Do not mix CERVARIX with any other vaccine in the same syringe or vial.
7.2 Hormonal Contraceptives
Among 7,693 subjects 15 through 25 years of age in Study 2 (CERVARIX, N = 3,821 or Hepatitis A Vaccine 720 EL.U., N = 3,872) who used hormonal contraceptives for a mean of 2.8 years, the observed efficacy of CERVARIX was similar to that observed among subjects who did not report use of hormonal contraceptives.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
Reproduction studies have been performed in rats at a dose approximately 47 times the human dose (on a mg/kg basis) and revealed no evidence of impaired fertility or harm to the fetus due to CERVARIX. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Non-clinical Studies
An evaluation of the effect of CERVARIX on embryo-fetal, pre- and post-natal development was conducted using rats. One group of rats was administered CERVARIX 30 days prior to gestation and during the period of organogenesis (gestation Days 6, 8, 11, and 15). A second group of rats was administered saline at 30 days prior to gestation followed by CERVARIX on Days 6, 8, 11, and 15 of gestation. Two additional groups of rats received either saline or adjuvant following the same dosing regimen. CERVARIX was administered at 0.1 mL/rat/occasion (approximately 47-fold excess relative to the projected human dose on a mg/kg basis) by intramuscular injection. No adverse effects on mating, fertility, pregnancy, parturition, lactation, or embryo-fetal, pre- and post-natal development were observed. There were no vaccine-related fetal malformations or other evidence of teratogenesis.
Clinical Studies
Overall Outcomes: In pre-licensure clinical studies, pregnancy testing was performed prior to each vaccine administration and vaccination was discontinued if a subject had a positive pregnancy test. In all clinical trials, subjects were instructed to take precautions to avoid pregnancy until 2 months after the last vaccination. During pre-licensure clinical development, a total of 7,276 pregnancies were reported among 3,696 females receiving CERVARIX and 3,580 females receiving a control (Hepatitis A Vaccine 360 EL.U., Hepatitis A Vaccine 720 EL.U., or 500 mcg Al(OH)3). The overall proportions of pregnancy outcomes were similar between treatment groups. The majority of women gave birth to normal infants (62.2% and 62.6% of recipients of CERVARIX and control, respectively). Other outcomes included spontaneous abortion (11.0% and 10.8% of recipients of CERVARIX and control, respectively), elective termination (5.8% and 6.1% of recipients of CERVARIX and control, respectively), abnormal infant other than congenital anomaly (2.8% and 3.2% of recipients of CERVARIX and control, respectively), and premature birth (2.0% and 1.7% of recipients of CERVARIX and control, respectively). Other outcomes (congenital anomaly, stillbirth, ectopic pregnancy, and therapeutic abortion) were reported less frequently in 0.1% to 0.8% of pregnancies in both groups.
Outcomes around Time of Vaccination: In pre-licensure studies, sub-analyses were conducted to describe pregnancy outcomes in 761 women (N = 396 for CERVARIX and N = 365 for pooled control, HAV 360 EL.U., HAV 720 EL.U., or 500 mcg Al(OH)3) who received a dose of CERVARIX or control between 45 days prior to and 30 days after the last menstrual period (LMP) and for whom pregnancy outcome was known. The majority of women gave birth to normal infants (65.2% and 69.3% of recipients of CERVARIX and control, respectively). Spontaneous abortion was reported in a total of 11.7% of subjects (13.6% of recipients of CERVARIX and 9.6% of control recipients), and elective termination was reported in a total of 9.7% of subjects (9.9% of recipients of CERVARIX and 9.6% of control recipients). Abnormal infant other than congenital anomaly was reported in a total of 4.9% of subjects (5.1% of recipients of CERVARIX and 4.7% of control recipients), and premature birth was reported in a total of 2.5% of subjects (2.5% of both groups). Other outcomes (congenital anomaly, stillbirth, ectopic pregnancy, and therapeutic abortion) were reported in 0.3% to 1.8% of pregnancies among recipients of CERVARIX and in 0.3% to 1.4% of pregnancies among control recipients.
A post-hoc analysis was performed on a pooled database of pregnancies with known outcome among women 15 to 25 years of age enrolled in controlled clinical trials (N = 4,670 for CERVARIX and N = 4,689 for pooled control, HAV 360 EL.U., HAV 720 EL.U., or 500 mcg Al(OH)3). In an analysis of pregnancies with exposure to CERVARIX or control between 45 days prior to and 30 days after the LMP, the relative risk of spontaneous abortion was 1.54 (95% CI: 0.95, 2.54) for exposure to one dose of CERVARIX (n/N = 46/326) compared with one dose of control (n/N = 33/338) and 1.21 (95% CI: 0.27, 7.33) for exposure to 2 doses of CERVARIX (n/N = 8/71) compared with 2 doses of control (n/N = 3/38).
The association between vaccination with CERVARIX and spontaneous abortion was evaluated in a post-marketing, retrospective, observational, cohort study using primary care medical records in the United Kingdom. The study assessed the risk of spontaneous abortion during weeks 1 to 19 of gestation in two cohorts of women 15 to 25 years of age: one cohort who received one or more doses of CERVARIX between 45 days prior to and 30 days after the LMP (close exposure) and another cohort who received the last dose of CERVARIX between 18 months and 120 days prior to the LMP (remote exposure). The hazard ratio for spontaneous abortion was 1.26 (95% CI: 0.77, 2.09) for the close-exposure cohort (n/N = 23/207) compared with the remote-exposure cohort (n/N = 56/632). In sensitivity analyses for the close-exposure cohort, the hazard ratio compared with the remote-exposure cohort was 1.07 (95% CI: 0.61, 1.86) for women who received only one dose of CERVARIX (n/N = 17/178) and 2.59 (95% CI: 1.11, 6.04) for women who received 2 doses of CERVARIX (n/N = 6/29).
8.3 Nursing Mothers
In non-clinical studies in rats, serological data suggest a transfer of anti–HPV-16 and anti–HPV-18 antibodies via milk during lactation in rats. Excretion of vaccine-induced antibodies in human milk has not been studied for CERVARIX. Because many drugs are excreted in human milk, caution should be exercised when CERVARIX is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients younger than 9 years of age have not been established. The safety and effectiveness of CERVARIX have been evaluated in 1,275 subjects 9 through 14 years of age and 6,362 subjects 15 through 17 years of age. [See Adverse Reactions (6.1), Clinical Studies (14.5).]
11 DESCRIPTION
CERVARIX [Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant] is a non-infectious recombinant, AS04-adjuvanted vaccine that contains recombinant L1 protein, the major antigenic protein of the capsid, of oncogenic HPV types 16 and 18. The L1 proteins are produced in separate bioreactors using the recombinant Baculovirus expression vector system in a serum-free culture media composed of chemically-defined lipids, vitamins, amino acids, and mineral salts. Following replication of the L1 encoding recombinant Baculovirus in Trichoplusia ni insect cells, the L1 protein accumulates in the cytoplasm of the cells. The L1 proteins are released by cell disruption and purified by a series of chromatographic and filtration methods. Assembly of the L1 proteins into virus-like particles (VLPs) occurs at the end of the purification process. The purified, non-infectious VLPs are then adsorbed on to aluminum (as hydroxide salt). The adjuvant system, AS04, is composed of 3-O-desacyl-4’-monophosphoryl lipid A (MPL) adsorbed on to aluminum (as hydroxide salt).
CERVARIX is prepared by combining the adsorbed VLPs of each HPV type together with the AS04 adjuvant system in sodium chloride, sodium dihydrogen phosphate dihydrate, and Water for Injection.
CERVARIX is a sterile suspension for intramuscular injection. Each 0.5-mL dose is formulated to contain 20 mcg of HPV type 16 L1 protein, 20 mcg of HPV type 18 L1 protein, 50 mcg of the 3-O-desacyl-4’-monophosphoryl lipid A (MPL), and 0.5 mg of aluminum hydroxide. Each dose also contains 4.4 mg of sodium chloride and 0.624 mg of sodium dihydrogen phosphate dihydrate. Each dose may also contain residual amounts of insect cell and viral protein (<40 ng) and bacterial cell protein (<150 ng) from the manufacturing process. CERVARIX does not contain a preservative.
The tip caps contain natural rubber latex; the plungers are not made with natural rubber latex.
14 CLINICAL STUDIES
Cervical intraepithelial neoplasia (CIN) Grade 2 and 3 lesions or cervical adenocarcinoma in situ (AIS) are the immediate and necessary precursors of squamous cell carcinoma and adenocarcinoma of the cervix, respectively. Their detection and removal has been shown to prevent cancer. Therefore, CIN2/3 and AIS (precancerous lesions) serve as surrogate markers for the prevention of cervical cancer. In clinical studies to evaluate the efficacy of CERVARIX, the endpoints were cases of CIN2/3 and AIS associated with HPV-16, HPV-18, and other oncogenic HPV types. Persistent infection with HPV-16 and HPV-18 that lasts for 12 months was also an endpoint.
The efficacy of CERVARIX to prevent histopathologically-confirmed CIN2/3 or AIS was assessed in 2 double-blind, randomized, controlled clinical studies that enrolled a total of 19,778 females 15 through 25 years of age.
Study 1 (HPV 001) enrolled women who were negative for oncogenic HPV DNA (HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) in cervical samples, seronegative for HPV-16 and HPV-18 antibodies, and had normal cytology. This represents a population presumed “naïve” without current HPV infection at the time of vaccination and without prior exposure to either HPV-16 or HPV-18. Subjects were enrolled in an extended follow-up study (Study 1 Extension [HPV 007]) to evaluate the long-term efficacy, immunogenicity, and safety. These subjects have been followed for up to 6.4 years.
In Study 2 (HPV 008), women were vaccinated regardless of baseline HPV DNA status, serostatus, or cytology. This study reflects a population of women naïve (without current infection and without prior exposure) or non-naïve (with current infection and/or with prior exposure) to HPV. Before vaccination, cervical samples were assessed for oncogenic HPV DNA (HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) and serostatus of HPV-16 and HPV-18 antibodies.
In both studies, testing for oncogenic HPV types was conducted using SPF10-LiPA25 PCR to detect HPV DNA in archived biopsy samples.
14.1 Prophylactic Efficacy against HPV Types 16 and 18
Study 2
A randomized, double-blind, controlled clinical trial was conducted in which 18,665 healthy females 15 through 25 years of age received CERVARIX or Hepatitis A Vaccine control on a 0-, 1-, and 6-month schedule. Among subjects, 54.8% of subjects were white, 31.5% Asian, 7.1% Hispanic, 3.7% black, and 2.9% were of other racial/ethnic groups.
In this study, women were randomized and vaccinated regardless of baseline HPV DNA status, serostatus, or cytology. Women with HPV-16 or HPV-18 DNA present in baseline cervical samples (HPV DNA positive) at study entry were considered currently infected with that specific HPV type. If HPV DNA was not detected by PCR, women were considered HPV DNA negative. Additionally, cervical samples were assessed for cytologic abnormalities and serologic testing was performed for anti–HPV-16 and anti–HPV-18 serum antibodies at baseline. Women with anti-HPV serum antibodies present were considered to have prior exposure to HPV and characterized as seropositive. Women seropositive for HPV-16 or HPV-18 but DNA negative for that specific serotype were considered as having cleared a previous natural infection. Women without antibodies to HPV-16 and HPV-18 were characterized as seronegative. Before vaccination, 73.6% of subjects were naïve (without current infection [DNA negative] and without prior exposure [seronegative]) to HPV-16 and/or HPV-18.
Efficacy endpoints included histological evaluation of precancerous and dysplastic lesions (CIN Grade 1, Grade 2, or Grade 3), and AIS. Virological endpoints (HPV DNA in cervical samples detected by PCR) included 12-month persistent infection (defined as at least 2 positive specimens for the same HPV type over a minimum interval of 10 months).
The according-to-protocol (ATP) cohort for efficacy analyses for HPV-16 and/or HPV-18 included all subjects who received 3 doses of vaccine, for whom efficacy endpoint measures were available and who were HPV-16 and/or HPV-18 DNA negative and seronegative at baseline and HPV-16 and/or HPV-18 DNA negative at Month 6 for the HPV type considered in the analysis. Case counting for the ATP cohort started on Day 1 after the third dose of vaccine. This cohort included women who had normal or low-grade cytology (cytological abnormalities including atypical squamous cells of undetermined significance [ASC-US] or low-grade squamous intraepithelial lesions [LSIL]) at baseline and excluded women with high-grade cytology.
The total vaccinated cohort (TVC) for each efficacy analysis included all subjects who received at least one dose of the vaccine, for whom efficacy endpoint measures were available, irrespective of their HPV DNA status, cytology, and serostatus at baseline. This cohort included women with or without current HPV infection and/or prior exposure. Case counting for the TVC started on Day 1 after the first dose.
The TVC naïve is a subset of the TVC that had normal cytology and were HPV DNA negative for 14 oncogenic HPV types and seronegative for HPV-16 and HPV-18 at baseline.
The pre-defined final analysis was event-triggered, i.e., performed when at least 36 CIN2/3 or AIS cases associated with HPV-16 or HPV-18 were accrued in the ATP cohort. The mean follow-up after the first dose was approximately 39 months and included approximately 3,300 women who completed the Month 48 visit.
The pre-defined end-of-study analysis was performed at the end of the 4-year follow-up period (i.e., after all subjects completed the Month 48 visit) and included all subjects from the TVC. The mean follow-up after the first dose was approximately 44 months and included approximately 15,600 women who completed the Month 48 visit.
CERVARIX was efficacious in the prevention of precancerous lesions or AIS associated with HPV-16 or HPV-18 (Table 5).
|
Final Analysis |
End-of-Study Analysis |
|||||||||
|
CERVARIX |
Controlb |
% Efficacy (96.1% CI)c |
CERVARIX |
Controlb |
% Efficacy (95% CI) |
|||||
|
N |
n |
N |
n |
N |
n |
N |
n |
|||
|
CIN2/3 or AIS |
7,344 |
4 |
7,312 |
56 |
92.9 (79.9, 98.3) |
7,338 |
5 |
7,305 |
97 |
94.9 (87.7, 98.4) |
|
CIN1/2/3 or AIS |
7,344 |
8 |
7,312 |
96 |
91.7 (82.4, 96.7) |
7,338 |
12 |
7,305 |
165 |
92.8 (87.1, 96.4) |
CI = Confidence Interval; n = Number of cases.
aSubjects (including women who had normal cytology, ASC‑US, or LSIL at baseline) who received 3 doses of vaccine and were HPV DNA negative and seronegative at baseline and HPV DNA negative at Month 6 for the corresponding HPV type (N).
bHepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
cThe 96.1% confidence interval reflected in the final analysis results from statistical adjustment for the previously conducted interim analysis.
Since CIN3 or AIS represents a more immediate precursor to cervical cancer, cases of CIN3 or AIS associated with HPV-16 or HPV-18 were evaluated. In the ATP cohort, CERVARIX was efficacious in the prevention of CIN3 or AIS associated with HPV-16 or HPV-18 in the final analysis (80.0% [96.1% CI: 0.3, 98.1]); these results were confirmed in the end-of-study analysis (91.7% [95% CI: 66.6, 99.1]).
Subjects who were already infected with one vaccine HPV type (16 or 18) prior to vaccination were protected from precancerous lesions or AIS and infection caused by the other vaccine HPV type.
Efficacy of CERVARIX against 12-month persistent infection with HPV-16 or HPV-18 was also evaluated. In the ATP cohort, CERVARIX reduced the incidence of 12-month persistent infection with HPV-16 and/or HPV-18 by 91.4% (96.1% CI: 86.1, 95.0) in the final analysis; these results were confirmed in the end-of-study analysis (92.9% [95% CI: 89.4, 95.4]).
Immune response following natural infection does not reliably confer protection against future infections. Among subjects who received 3 doses of CERVARIX and who were seropositive at baseline and DNA negative for HPV-16 or HPV-18 at baseline and Month 6, CERVARIX reduced the incidence of 12-month persistent infection by 95.8% (96.1% CI: 72.4, 99.9) in the final analysis; these results were confirmed in the end-of-study analysis (94.0% [95% CI: 76.7, 99.3]). However, the number of cases of CIN2/3 or AIS was too few in these analyses to determine efficacy against histopathological endpoints in this population.
Study 1 and Study 1 Extension
In a second double-blind, randomized, controlled study (Study 1), the efficacy of CERVARIX in the prevention of HPV-16 or HPV-18 incident and persistent infections was compared with aluminum hydroxide control in 1,113 females 15 through 25 years of age. The population was naïve to current oncogenic HPV infection or prior exposure to HPV-16 and HPV-18 at the time of vaccination (total cohort). A total of 776 subjects were enrolled in the extended follow-up study (Study 1 Extension) to evaluate the long-term efficacy, immunogenicity, and safety of CERVARIX. These subjects have been followed for up to 6.4 years.
In Study 1 and Study 1 Extension, with up to 6.4 years of follow-up (mean 5.9 years), in naïve females 15 through 25 years of age, efficacy against CIN2/3 or AIS associated with HPV-16 or HPV-18 was 100% (98.67% CI: 28.4, 100). Efficacy against 12-month persistent infection with HPV-16 or HPV-18 was 100% (98.67% CI: 74.4, 100). The confidence interval reflected in this final analysis results from statistical adjustment for analyses previously conducted.
14.2 Efficacy against HPV Types 16 and 18, Regardless of Current Infection or Prior Exposure to HPV-16 or HPV-18
Study 2
The study included women regardless of HPV DNA status (current infection) and serostatus (prior exposure) to vaccine types HPV-16 or HPV-18 at baseline. Efficacy analyses included lesions arising among women regardless of baseline DNA status and serostatus, including HPV infections present at first vaccination and those from infections acquired after Dose 1. In this population, which includes naïve (without current infection and prior exposure) and non-naïve women, CERVARIX was efficacious in the prevention of precancerous lesions or AIS associated with HPV-16 or HPV-18 (Table 6).
However, among women HPV DNA positive regardless of serostatus at baseline, there was no clear evidence of efficacy against precancerous lesions or AIS associated with HPV-16 or HPV-18 (Table 6).
|
Final Analysis |
End-of-Study Analysis |
|||||||||
|
CERVARIX |
Controla |
% Efficacy (96.1% CI)b |
CERVARIX |
Controla |
% Efficacy (95% CI) |
|||||
|
N |
n |
N |
n |
N |
n |
N |
n |
|||
|
CIN1/2/3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
3 |
5,436 |
85 |
96.5 (89.0, 99.4) |
5,466 |
5 |
5,452 |
141 |
96.5 (91.6, 98.9) |
|
HPV‑16 or 18 DNA Positive at Baselined |
641 |
90 |
592 |
92 |
— |
642 |
99 |
593 |
101 |
— |
|
Regardless of Baseline Statuse |
8,667 |
107 |
8,682 |
240 |
55.5f (43.2, 65.3) |
8,694 |
121 |
8,708 |
324 |
62.9f (54.1, 70.1) |
|
CIN2/3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
1 |
5,436 |
63 |
98.4 (90.4, 100) |
5,466 |
1 |
5,452 |
97 |
99.0 (94.2, 100) |
|
HPV‑16 or 18 DNA Positive at Baselined |
641 |
74 |
592 |
73 |
— |
642 |
80 |
593 |
82 |
— |
|
Regardless of Baseline Statuse |
8,667 |
82 |
8,682 |
174 |
52.8f (37.5, 64.7) |
8,694 |
90 |
8,708 |
228 |
60.7f (49.6, 69.5) |
|
CIN3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
0 |
5,436 |
13 |
100 (64.7, 100) |
5,466 |
0 |
5,452 |
27 |
100 (85.5, 100) |
|
HPV‑16 or 18 DNA Positive at Baselined |
641 |
41 |
592 |
38 |
— |
642 |
48 |
593 |
47 |
— |
|
Regardless of Baseline Statuse |
8,667 |
43 |
8,682 |
65 |
33.6f (-1.1, 56.9) |
8,694 |
51 |
8,708 |
94 |
45.7f (22.9, 62.2) |
CI = Confidence Interval; n = Number of histopathological cases associated with HPV-16 and/or HPV-18.
Table does not include disease due to non-vaccine HPV types.
aHepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
bThe 96.1% confidence interval reflected in the final analysis results from statistical adjustment for the previously conducted interim analysis.
cTVC naïve: Includes all vaccinated subjects (who received at least one dose of vaccine) who had normal cytology, were HPV DNA negative for 14 oncogenic HPV types, and seronegative for HPV-16 and HPV-18 at baseline (N). Case counting started on Day 1 after the first dose.
dTVC subset: Includes all vaccinated subjects (who received at least one dose of vaccine) who were HPV DNA positive for HPV-16 or HPV-18 irrespective of serostatus at baseline (N). Case counting started on Day 1 after the first dose.
eTVC: Includes all vaccinated subjects (who received at least one dose of vaccine) irrespective of HPV DNA status and serostatus at baseline (N). Case counting started on Day 1 after the first dose.
fObserved vaccine efficacy includes the prophylactic efficacy of CERVARIX and the impact of CERVARIX on the course of infections present at first vaccination.
14.3 Efficacy against Cervical Disease Irrespective of HPV Type, Regardless of Current or Prior Infection with Vaccine or Non-vaccine HPV Types
Study 2
The impact of CERVARIX against the overall burden of HPV-related cervical disease results from a combination of prophylactic efficacy against, and disease contribution of, HPV-16, HPV-18, and non-vaccine HPV types.
In the population naïve to oncogenic HPV (TVC naïve), CERVARIX reduced the overall incidence of CIN1/2/3 or AIS, CIN2/3 or AIS, and CIN3 or AIS regardless of the HPV DNA type in the lesion (Table 7). In the population of women naïve and non-naïve (TVC), vaccine efficacy against CIN1/2/3 or AIS, CIN2/3 or AIS, and CIN3 or AIS was demonstrated in all women regardless of HPV DNA type in the lesion (Table 7).
|
Final Analysis |
End-of-Study Analysis |
|||||||||
|
CERVARIX |
Controla |
% Efficacy (96.1% CI)b |
CERVARIX |
Controla |
% Efficacy (95% CI) |
|||||
|
N |
n |
N |
n |
N |
n |
N |
n |
|||
|
CIN1/2/3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
106 |
5,436 |
211 |
50.1 (35.9, 61.4) |
5,466 |
174 |
5,452 |
346 |
50.3 (40.2, 58.8) |
|
Irrespective of HPV DNA at Baselined |
8,667 |
451 |
8,682 |
577 |
21.7 (10.7, 31.4) |
8,694 |
579 |
8,708 |
798 |
27.7 (19.5, 35.2) |
|
CIN2/3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
33 |
5,436 |
110 |
70.2 (54.7, 80.9) |
5,466 |
61 |
5,452 |
172 |
64.9 (52.7, 74.2) |
|
Irrespective of HPV DNA at Baselined |
8,667 |
224 |
8,682 |
322 |
30.4 (16.4, 42.1) |
8,694 |
287 |
8,708 |
428 |
33.1 (22.2, 42.6) |
|
CIN3 or AIS |
||||||||||
|
Prophylactic Efficacyc |
5,449 |
3 |
5,436 |
23 |
87.0 (54.9, 97.7) |
5,466 |
3 |
5,452 |
44 |
93.2 (78.9, 98.7) |
|
Irrespective of HPV DNA at Baselined |
8,667 |
77 |
8,682 |
116 |
33.4 (9.1, 51.5) |
8,694 |
86 |
8,708 |
158 |
45.6 (28.8, 58.7) |
CI = Confidence Interval; n = Number of cases.
aHepatitis A Vaccine control group [720 EL.U. of antigen and 500 mcg Al(OH)3].
bThe 96.1% confidence interval reflected in the final analysis results from statistical adjustment for the previously conducted interim analysis.
cTVC naïve: Includes all vaccinated subjects (who received at least one dose of vaccine) who had normal cytology, were HPV DNA negative for 14 oncogenic HPV types (including HPV-16 and HPV-18), and seronegative for HPV-16 and HPV-18 at baseline (N). Case counting started on Day 1 after the first dose.
dTVC: Includes all vaccinated subjects (who received at least one dose of vaccine) irrespective of HPV DNA status and serostatus at baseline (N). Case counting started on Day 1 after the first dose.
In exploratory end-of-study analyses, CERVARIX reduced definitive cervical therapy procedures (includes loop electrosurgical excision procedure [LEEP], cold-knife Cone, and laser procedures) by 33.2% (95% CI: 20.8, 43.7) in the TVC and by 70.2% (95% CI: 57.8, 79.3) in the TVC naïve.
To assess reductions in disease caused by non-vaccine HPV types, analyses were conducted combining 12 non‑vaccine oncogenic HPV types, including and excluding lesions in which HPV-16 or HPV-18 were also detected. Among females who received 3 doses of CERVARIX and were DNA negative for the specific HPV type at baseline and Month 6, CERVARIX reduced the incidence of CIN2/3 or AIS in the final analysis by 54.0% (96.1% CI: 34.0, 68.4) and 37.4% (96.1% CI: 7.4, 58.2), respectively. In the end-of-study analysis, CERVARIX reduced the incidence of CIN2/3 or AIS by 46.8% (95% CI: 30.7, 59.4) and 24.1% (95% CI: -1.5, 43.5), respectively.
End-of-study analyses were conducted to assess the impact of CERVARIX on CIN2/3 or AIS due to specific non-vaccine HPV types. The ATP cohort for these analyses included all subjects irrespective of serostatus who received 3 doses of CERVARIX and were DNA negative for the specific HPV type at baseline and Month 6. These analyses were also conducted in the TVC-naïve population.
In analyses including lesions in which HPV-16 or HPV-18 were also detected, vaccine efficacy in prevention of CIN2/3 or AIS associated with HPV-31 was 87.5% (95% CI: 68.3, 96.1) and 89.4% (95% CI: 65.5, 97.9), respectively. In analyses excluding lesions in which HPV-16 or HPV-18 were detected, vaccine efficacy in prevention of CIN2/3 or AIS associated with HPV-31 was 84.3% (95% CI: 59.5, 95.2) and 83.4% (95% CI: 43.3, 96.9), respectively.
14.4 Immunogenicity
The minimum anti-HPV titer that confers protective efficacy has not been determined.
The antibody response to HPV-16 and HPV-18 was measured using a type-specific binding ELISA (developed by GlaxoSmithKline) and a pseudovirion-based neutralization assay (PBNA). In a subset of subjects tested for HPV-16 and HPV-18, the ELISA has been shown to correlate with the PBNA. The scales for these assays are unique to each HPV type and each assay, thus, comparison between HPV types or assays is not appropriate.
Duration of Immune Response
The duration of immunity following a complete schedule of immunization with CERVARIX has not been established. In Study 1 and Study 1 Extension, the immune response against HPV-16 and HPV-18 was evaluated for up to 76 months post-Dose 1, in females 15 through 25 years of age. Vaccine-induced geometric mean titers (GMTs) for both HPV-16 and HPV-18 peaked at Month 7 and thereafter reached a plateau that was sustained from Month 18 up to Month 76. At all timepoints, >98% of subjects were seropositive for both HPV-16 (≥8 EL.U./mL, the limit of detection) and HPV-18 (≥7 EL.U./mL, the limit of detection) by ELISA.
In Study 2, immunogenicity was measured by seropositivity rates and GMTs for ELISA and PBNA (Table 8). The ATP cohort for immunogenicity included all evaluable subjects for whom data concerning immunogenicity endpoint measures were available. These included subjects for whom assay results were available for antibodies against at least one vaccine type. Subjects who acquired either HPV-16 or HPV-18 infection during the trial were excluded.
|
Time Point |
N |
% Seropositive (95% CI) |
GMT (95% CI) |
|
Anti–HPV-16 ELISAb (EL.U./mL) |
|||
|
Month 7 |
816 |
99.5 |
9,120.0 (8,504.9, 9,779.7) |
|
Month 12 |
793 |
99.7 |
3,266.3 (3,043.3, 3,505.6) |
|
Month 24 |
755 |
99.9 |
1,587.7 (1,484.8, 1,697.7) |
|
Month 36 |
759 |
100 |
1,281.7 (1,198.3, 1,370.9) |
|
Month 48 |
746 |
100 |
1,174.3 (1,096.1, 1,258.0) |
|
Anti–HPV-18 ELISAb (EL.U./mL) |
|||
|
Month 7 |
879 |
99.4 |
4,682.9 (4,388.8, 4,996.7) |
|
Month 12 |
853 |
100 |
1,514.7 (1,422.3, 1,613.0) |
|
Month 24 |
810 |
99.9 |
702.2 (655.2, 752.6) |
|
Month 36 |
817 |
100 |
538.1 (502.0, 576.8) |
|
Month 48 |
806 |
99.8 |
476.2 (443.2, 511.6) |
|
Anti–HPV-16 PBNAc (ED50) |
|||
|
Month 7 |
46 |
100 |
26,457.0 (19,167.5, 36,518.6) |
|
Month 12 |
45 |
100 |
7,885.5 (5,500.4, 11,304.8) |
|
Month 24 |
46 |
100 |
3,396.4 (2,388.0, 4,830.6) |
|
Month 36 |
41 |
100 |
2,245.1 (1,616.6, 3,117.9) |
|
Month 48 |
41 |
97.6 |
1,931.1 (1,294.4, 2,880.8) |
|
Anti–HPV-18 PBNAc (ED50) |
|||
|
Month 7 |
46 |
100 |
8,413.9 (6,394.7, 11,070.7) |
|
Month 12 |
45 |
97.8 |
1,748.2 (1,223.6, 2,497.7) |
|
Month 24 |
46 |
100 |
1,552.5 (1,112.9, 2,165.5) |
|
Month 36 |
41 |
100 |
1,326.9 (948.0, 1,857.3) |
|
Month 48 |
41 |
95.1 |
1,078.1 (714.9, 1,625.6) |
aSubjects who received 3 doses of vaccine for whom assay results were available for at least one post-vaccination antibody measurement (N). Subjects who acquired either HPV‑16 or HPV‑18 infection during the study were excluded.
bEnzyme linked immunosorbent assay (assay cut-off 8 EL.U./mL for anti–HPV‑16 antibody and 7 EL.U./mL for anti–HPV‑18 antibody).
cPseudovirion-based neutralization assay (assay cut-off 40 ED50 for both anti–HPV‑16 antibody and anti–HPV‑18 antibody).
14.5 Bridging of Efficacy from Women to Adolescent Girls
The immunogenicity of CERVARIX was evaluated in 3 clinical studies involving 1,275 girls 9 through 14 years of age who received at least one dose of CERVARIX.
Study 3 (HPV 013) was a double-blind, randomized, controlled study in which 1,035 subjects received CERVARIX and 1,032 subjects received a Hepatitis A Vaccine 360 EL.U. as the control vaccine with a subset of subjects evaluated for immunogenicity. All initially seronegative subjects in the group who received CERVARIX were seropositive after vaccination, i.e., had levels of antibody greater than the limit of detection of the assay to both HPV-16 (≥8 EL.U./mL) and HPV-18 (≥7 EL.U./mL) antigens. The GMTs for anti–HPV-16 and anti–HPV-18 antibodies in initially seronegative subjects are presented in Table 9.
|
Age Group |
Anti–HPV-16 Antibodies GMT EL.U./mL (95% CI) |
Anti–HPV-18 Antibodies GMT EL.U./mL (95% CI) |
||||
|
N |
Month 7 |
Month 18 |
N |
Month 7 |
Month 18 |
|
|
10-14 years of age |
556-619 |
19,882.0 (18,626.7, 21,221.9) |
3,888.8 (3,605.0, 4,195.0) |
562-628 |
8,262.0 (7,725.0, 8,836.2) |
1,539.4 (1,418.8, 1,670.3) |
aSubjects who received 3 doses of vaccine for whom assay results were available for at least one post-vaccination antibody measurement (N).
In Study 4 (HPV 012), the immunogenicity of CERVARIX administered to girls 10 through 14 years of age was compared with that in females 15 through 25 years of age. The immune response in girls 10 through 14 years of age measured one month post-Dose 3 was non-inferior to that seen in females 15 through 25 years of age for both HPV-16 and HPV-18 antigens (Table 10).
|
Antibody Assay |
10-14 Years of Age |
15-25 Years of Age |
||||
|
N |
GMTb EL.U./mL (95% CI) |
SeropositivityRatec % |
N |
GMTb EL.U./mL (95% CI) |
SeropositivityRatec % |
|
|
Anti–HPV-16 |
143 |
17,272.5 (15,117.9, 19,734.1) |
100 |
118 |
7,438.9 (6,324.6, 8,749.6) |
100 |
|
Anti–HPV-18 |
141 |
6,863.8 (5,976.3, 7,883.0) |
100 |
116 |
3,070.1 (2,600.0, 3,625.4) |
100 |
aSubjects who received 3 doses of vaccine for whom assay results were available for at least one post-vaccination antibody measurement (N).
bNon-inferiority based on the upper limit of the 2-sided 95% CI for the GMT ratio (15 through 25 year olds/10 through 14 year olds) was <2.
cNon-inferiority based on the upper limit of the 2-sided 95% CI for the difference between the seropositivity rates for 10 through 14 year olds and 15 through 25 year olds was <10%.
In Study 5, a post-hoc analysis compared the immunogenicity of CERVARIX administered to girls 9 through 14 years of age (n = 68) with that in females 15 through 25 years of age (n = 114). In these initially seronegative subjects, the immune response in girls 9 through 14 years of age measured one month post-Dose 3 was non-inferior to that observed in females 15 through 25 years of age for both HPV-16 and HPV-18 antigens [lower limit of the 2-sided 95% CI for the GMT ratio (9 through 14 year olds/15 through 25 year olds) was >0.5]. The GMTs for anti–HPV-16 and anti–HPV-18 antibodies at Month 7 were 22,261.3 EL.U./mL and 7,398.8 EL.U./mL, respectively, in girls 9 through 14 years of age and 10,322.0 EL.U./mL and 4,261.5 EL.U./mL, respectively, in females 15 through 25 years of age.
Based on these immunogenicity data, the efficacy of CERVARIX is inferred in girls 9 through 14 years of age.
16 HOW SUPPLIED/STORAGE AND HANDLING
CERVARIX is available in 0.5-mL single-dose disposable prefilled TIP-LOK syringes (packaged without needles):
NDC 58160-830-05 Syringe in Package of 1: NDC 58160-830-34
NDC 58160-830-43 Syringe in Package of 10: NDC 58160-830-52
Store refrigerated between 2º and 8ºC (36º and 46ºF). Do not freeze. Discard if the vaccine has been frozen. Upon storage, a fine, white deposit with a clear, colorless supernatant may be observed. This does not constitute a sign of deterioration.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information). Patient labeling is provided as a tear-off leaflet at the end of this Full Prescribing Information.
Provide the Vaccine Information Statements prior to immunization. These are required by the National Childhood Vaccine Injury Act of 1986 and are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
Inform the patient, parent, or guardian:
- •
- Vaccination does not substitute for routine cervical cancer screening. Women who receive CERVARIX should continue to undergo cervical cancer screening per standard of care.
- •
- CERVARIX does not protect against disease from HPV types to which a woman has previously been exposed through sexual activity.
- •
- Since syncope has been reported following vaccination in young females, sometimes resulting in falling with injury, observation for 15 minutes after administration is recommended.
- •
- Safety has not been established in pregnant women.
CERVARIX and TIP-LOK are registered trademarks of the GSK group of companies.
Manufactured by GlaxoSmithKline Biologicals
Rixensart, Belgium, US License 1617
Distributed by GlaxoSmithKline
Research Triangle Park, NC 27709
©2016 the GSK group of companies. All rights reserved.
CRX:12PI
-------------------------------------------------------------------------------------------------------------
PATIENT INFORMATION
CERVARIX® (SERV-ah-rix)
[Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant]
Read this Patient Information carefully before getting CERVARIX. You (the person getting CERVARIX) will need 3 doses of the vaccine. Read this information before each dose of CERVARIX. This information does not take the place of talking with your healthcare provider about CERVARIX.
What is CERVARIX?
CERVARIX is a vaccine given by injection (shot) to girls and women 9 through 25 years of age.
- •
- CERVARIX helps protect against cervical cancer and precancers caused by human papillomavirus (HPV) types 16 and 18.
- •
- There are many types of HPV but only certain types cause cervical cancer. HPV types 16 and 18 are the 2 most common types of HPV that lead to cervical cancer and precancers.
- •
- Abnormal Pap smear results can indicate the presence of precancers. Some precancers can lead to cervical cancer.
- •
- CERVARIX is not a treatment for HPV.
- •
- You can not get HPV diseases from CERVARIX.
What important information should I know about CERVARIX?
- •
- You should continue to get routine cervical cancer screening (such as a Pap smear).
- •
- CERVARIX may not fully protect everyone who gets the vaccine.
- •
- Not all cervical cancers are caused by the HPV types CERVARIX protects against. CERVARIX will not protect against diseases from all HPV types.
- •
- CERVARIX will not protect against HPV types that you already have.
Who should not get CERVARIX?
You should not get CERVARIX if you have or have had:
- •
- an allergic reaction to a previous dose of CERVARIX.
- •
- an allergy to any of the ingredients in CERVARIX (listed below).
What should I tell my healthcare provider before getting CERVARIX?
Tell your healthcare provider about all your health conditions, including if you:
- •
- have had an allergic reaction after a previous dose of CERVARIX.
- •
- have an allergy to latex.
- •
- have a weakened immune system.
- •
- are taking any other medicine or have recently gotten any other vaccine.
- •
- have a fever over 100°F (37.8°C).
- •
- are pregnant or are planning to get pregnant during the time period of the 3 shots. CERVARIX is not recommended for use in pregnant women.
Your healthcare provider will decide if you should get CERVARIX.
How is CERVARIX given?
CERVARIX is given as an injection (shot) in a muscle in your arm.
You will need a total of 3 shots as follows:
- •
- First dose: given at a time decided by you and your healthcare provider
- •
- Second dose: given 1 month after the first dose
- •
- Third dose: given 6 months after the first dose
Fainting may occur, sometimes resulting in falling with injury, especially in young females. Your healthcare provider may ask you to sit or lie down for 15 minutes after you get CERVARIX. Some people who faint may shake or become stiff. If this happens, it may require evaluation or treatment by your healthcare provider.
Make sure you get all 3 doses on time for the best protection. If you miss a scheduled dose, talk to your healthcare provider.
What are the possible side effects of CERVARIX?
The most common side effects of CERVARIX are:
- •
- pain, redness, and swelling where you got the shot
- •
- feeling tired
- •
- headache
- •
- muscle aches
- •
- nausea, vomiting, diarrhea, and stomach pain
- •
- joint aches
Other possible side effects include:
- •
- swollen glands (neck, armpit, or groin).
Call your healthcare provider or seek medical treatment immediately if you develop hives, difficulty breathing, or swelling of the throat, because these may be signs of a severe allergic reaction.
Tell your healthcare provider about these or any other side effects that concern you. For a more complete list of side effects, ask your healthcare provider.
What are the ingredients in CERVARIX?
CERVARIX contains proteins of HPV types 16 and 18. The vaccine also contains 3-O-desacyl-4’-monophosphoryl lipid A (MPL), aluminum hydroxide, sodium chloride, and sodium dihydrogen phosphate dehydrate.
CERVARIX contains no preservatives.
This is a summary of information about CERVARIX. If you would like more information, please talk with your healthcare provider or visit www.cervarix.com.
CERVARIX is a registered trademark of the GSK group of companies.
Manufactured by GlaxoSmithKline Biologicals
Rixensart, Belgium, US License 1617
Distributed by GlaxoSmithKline
Research Triangle Park, NC 27709
©2016 the GSK group of companies. All rights reserved.
April 2016
CRX:6PIL
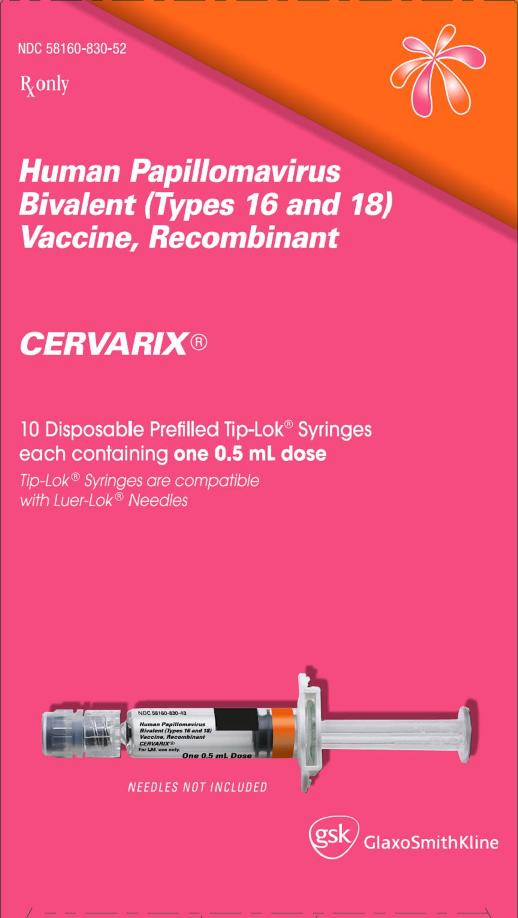
PRINCIPAL DISPLAY PANEL
NDC 58160-830-52
CERVARIX®
Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant
Rx only
10 Disposable Prefilled Tip-Lok® Syringes each containing one 0.5 mL dose
Tip-Lok® Syringes are compatible with Luer-Lok® Needles
NEEDLES NOT INCLUDED
Made in Belgium
©2015, the GSK group of companies
Rev. 2/15
474537
| CERVARIX
human papillomavirus bivalent (types 16 and 18) vaccine, recombinant injection, suspension |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - GlaxoSmithKline Biologicals SA (372748392) |