RELISTOR- methylnaltrexone bromide
RELISTOR- methylnaltrexone bromide injection, solution
Wyeth Pharmaceuticals Inc., a subsidiary of Pfizer Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use RELISTOR safely and effectively. See full prescribing information for RELISTOR. RELISTOR (methylnaltrexone bromide) Subcutaneous Injection Initial U.S. Approval: 2008 RECENT MAJOR CHANGESINDICATIONS AND USAGERELISTOR is indicated for the treatment of opioid-induced constipation in patients with advanced illness who are receiving palliative care, when response to laxative therapy has not been sufficient. Use of RELISTOR beyond four months has not been studied. (1) DOSAGE AND ADMINISTRATIONRELISTOR is administered as a subcutaneous injection. The usual schedule is one dose every other day, as needed, but no more frequently than one dose in a 24-hour period. (2.2) The recommended dose of RELISTOR is 8 mg for patients weighing 38 to less than 62 kg (84 to less than 136 lb) or 12 mg for patients weighing 62 to 114 kg (136 to 251 lb). Patients whose weights fall outside of these ranges should be dosed at 0.15 mg/kg. See the table below to determine the correct injection volume. (2.2)
Only patients requiring an 8 mg or 12 mg dose should be prescribed pre-filled syringes (2.2, 3). In patients with severe renal impairment (creatinine clearance less than 30 mL/min), dose reductions of RELISTOR by one half is recommended. (8.6) DOSAGE FORMS AND STRENGTHSRELISTOR is available in the following dosage forms: (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe most common (> 5%) adverse reactions reported with RELISTOR are abdominal pain, flatulence, nausea, dizziness, diarrhea and hyperhidrosis. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Wyeth Pharmaceuticals Inc. at 1-800-934-5556 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONSIn an in vitro study, methylnaltrexone bromide was a weak inhibitor of cytochrome P450 (CYP) isozyme CYP2D6 activity, but in an in vivo study it did not significantly affect the metabolism of the CYP2D6 substrate, dextromethorphan (7.1) USE IN SPECIFIC POPULATIONSPediatric Use: Safety and efficacy of RELISTOR have not been established in pediatric patients. (8.4) See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling See 17 for FDA-approved patient labeling and FDA-approved patient labeling. Revised: 1/2011 |
|||||||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
RELISTOR® is indicated for the treatment of opioid-induced constipation in patients with advanced illness who are receiving palliative care, when response to laxative therapy has not been sufficient. Use of RELISTOR beyond four months has not been studied.
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
FOR SUBCUTANEOUS INJECTION ONLY
RELISTOR should be injected in the upper arm, abdomen or thigh.
2.2 Dosing
RELISTOR is administered as a subcutaneous injection. The usual schedule is one dose every other day, as needed, but no more frequently than one dose in a 24-hour period [see Clinical Studies (14)].
The recommended dose of RELISTOR is 8 mg for patients weighing 38 to less than 62 kg (84 to less than 136 lb) or 12 mg for patients weighing 62 to 114 kg (136 to 251 lb). Patients whose weight falls outside of these ranges should be dosed at 0.15 mg/kg. See the table below to determine the correct injection volume. The pre-filled syringe is designed to deliver a fixed dose; therefore, patients requiring dosing calculated on a mg/kg basis should not be prescribed pre-filled syringes.
| Patient Weight | Injection Volume | Dose | |
| Pounds | Kilograms | ||
| Less than 84 | Less than 38 | See below* | 0.15 mg/kg |
| 84 to less than 136 | 38 to less than 62 | 0.4 mL | 8 mg |
| 136 to 251 | 62 to 114 | 0.6 mL | 12 mg |
| More than 251 | More than 114 | See below* | 0.15 mg/kg |
| *The injection volume for these patients should be calculated using one of the following: | |||
- Multiply the patient weight in pounds by 0.0034 and round up the volume to the nearest 0.1 mL.
- Multiply the patient weight in kilograms by 0.0075 and round up the volume to the nearest 0.1 mL.
Use in Patients with Severe Renal Impairment
In patients with severe renal impairment (creatinine clearance less than 30 mL/min), dose reduction of RELISTOR by one-half is recommended [see Use in Specific Populations (8.6)].
The pre-filled syringe is designed to deliver a fixed dose; therefore, patients with severe renal impairment should not be prescribed pre-filled syringes unless their body weight calculated dose is 8 mg or 12 mg.
2.3 Preparation for Injection
RELISTOR is a sterile, clear, and colorless to pale yellow aqueous solution. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If any of these are present, the vial should not be used.
Preparation of RELISTOR Using the Single-use Vial
Once drawn into the syringe, if immediate administration is not possible, store at ambient room temperature and administer within 24 hours [see Patient Counseling Information (17)].
3 DOSAGE FORMS AND STRENGTHS
RELISTOR is available in the following dosage forms and strengths. Only patients requiring an 8 mg or 12 mg dose should be prescribed pre-filled syringes.
- Single-use vial containing 12 mg/0.6 mL solution for subcutaneous injection [see Dosage and Administration (2.2)].
- Single-use pre-filled syringe containing 8 mg/0.4 mL solution for subcutaneous injection, with a 29-gauge x ½-inch fixed needle and a needle guard [see Dosage and Administration (2.2)].
- Single-use pre-filled syringe containing 12 mg/0.6 mL solution for subcutaneous injection, with a 29-gauge x ½-inch fixed needle and a needle guard [see Dosage and Administration (2.2)].
4 CONTRAINDICATIONS
RELISTOR is contraindicated in patients with known or suspected mechanical gastrointestinal obstruction.
5 WARNINGS AND PRECAUTIONS
5.1 Severe or Persistent Diarrhea
If severe or persistent diarrhea occurs during treatment, advise patients to discontinue therapy with RELISTOR and consult their physician.
5.2 Intestinal Perforation
Rare cases of gastrointestinal (GI) perforation have been reported in advanced illness patients with conditions that may be associated with localized or diffuse reduction of structural integrity in the wall of the GI tract (i.e., cancer, peptic ulcer, Ogilvie's syndrome). Perforations have involved varying regions of the GI tract: (e.g., stomach, duodenum, colon).
Use RELISTOR with caution in patients with known or suspected lesions of the GI tract. Advise patients to discontinue therapy with RELISTOR and promptly notify their physician if they develop severe, persistent, and/or worsening abdominal symptoms.
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under varying conditions, adverse reaction rates observed in the clinical trials of a drug may not reflect the rates observed in practice.
The safety of RELISTOR was evaluated in two, double-blind, placebo-controlled trials in patients with advanced illness receiving palliative care: Study 1 included a single-dose, double-blind, placebo-controlled period, whereas Study 2 included a 14-day multiple dose, double-blind, placebo-controlled period [see Clinical Studies (14)]. In both studies, patients had advanced illness with a life expectancy of less than 6 months and received care to control their symptoms. The majority of patients had a primary diagnosis of incurable cancer; other primary diagnoses included end-stage COPD/emphysema, cardiovascular disease/heart failure, Alzheimer's disease/dementia, HIV/AIDS, or other advanced illnesses. Patients were receiving opioid therapy (median daily baseline oral morphine equivalent dose = 172 mg), and had opioid-induced constipation (either <3 bowel movements in the preceding week or no bowel movement for 2 days). Both the methylnaltrexone bromide and placebo patients were on a stable laxative regimen for at least 3 days prior to study entry and continued on their regimen throughout the study.
The adverse reactions in patients receiving RELISTOR are shown in table below.
| Adverse Reactions from all Doses in Double-Blind, Placebo-Controlled Clinical Studies of RELISTOR* | ||
|---|---|---|
| Adverse Reaction | RELISTOR
N = 165 | Placebo
N = 123 |
| * Doses: 0.075, 0.15, and 0.30 mg/kg/dose | ||
| Abdominal Pain | 47 (28.5%) | 12 (9.8%) |
| Flatulence | 22 (13.3%) | 7 (5.7%) |
| Nausea | 19 (11.5%) | 6 (4.9%) |
| Dizziness | 12 (7.3%) | 3 (2.4%) |
| Diarrhea | 9 (5.5%) | 3 (2.4%) |
| Hyperhidrosis | 11 (6.7%) | 8 (6.5%) |
6.2 Postmarketing Experience
Rare cases of gastrointestinal (GI) perforation have been reported in advanced illness patients with conditions that may be associated with localized or diffuse reduction of structural integrity in the wall of the GI tract (i.e., cancer, peptic ulcer, Ogilvie's syndrome). Perforations have involved varying regions of the GI tract: (e.g., stomach, duodenum, colon). Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
7 DRUG INTERACTIONS
7.1 Drugs Metabolized by Cytochrome P450 Isozymes
In in vitro drug metabolism studies methylnaltrexone bromide did not significantly inhibit the activity of cytochrome P450 (CYP) isozymes CYP1A2, CYP2A6, CYP2C9, CYP2C19 or CYP3A4, while it is a weak inhibitor of CYP2D6. In a clinical drug interaction study in healthy adult male subjects, a subcutaneous dose of 0.30 mg/kg of methylnaltrexone bromide did not significantly affect the metabolism of dextromethorphan, a CYP2D6 substrate.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
Reproduction studies have been performed in pregnant rats at intravenous doses up to about 14 times the recommended maximum human subcutaneous dose of 0.3 mg/kg based on the body surface area and in pregnant rabbits at intravenous doses up to about 17 times the recommended maximum human subcutaneous dose based on the body surface area and have revealed no evidence of impaired fertility or harm to the fetus due to methylnaltrexone bromide. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, methylnaltrexone bromide should be used during pregnancy only if clearly needed.
8.2 Labor and Delivery
Effects of RELISTOR on mother, fetus, duration of labor, and delivery are unknown. There were no effects on the mother, labor, delivery, or on offspring survival and growth in rats following subcutaneous injection of methylnaltrexone bromide at dosages up to 25 mg/kg/day.
8.3 Nursing Mothers
Results from an animal study using [3H]-labeled methylnaltrexone bromide indicate that methylnaltrexone bromide is excreted via the milk of lactating rats. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when RELISTOR is administered to a nursing woman.
8.5 Geriatric Use
In the phase 2 and 3 double-blind studies, a total of 77 (24%) patients aged 65-74 years (54 methylnaltrexone bromide, 23 placebo) and a total of 100 (31.2%) patients aged 75 years or older (61 methylnaltrexone bromide, 39 placebo) were enrolled. There was no difference in the efficacy or safety profile of these elderly patients when compared to younger patients. Therefore, no dose adjustment is recommended based on age.
8.6 Renal Impairment
No dose adjustment is required in patients with mild or moderate renal impairment. Dose-reduction by one half is recommended in patients with severe renal impairment (creatinine clearance less than 30 mL/min).
In a study of volunteers with varying degrees of renal impairment receiving a single dose of 0.30 mg/kg methylnaltrexone bromide, renal impairment had a marked effect on the renal excretion of methylnaltrexone bromide. Severe renal impairment decreased the renal clearance of methylnaltrexone bromide by 8- to 9-fold and resulted in a 2-fold increase in total methylnaltrexone bromide exposure (AUC). Cmax was not significantly changed. No studies were performed in patients with end-stage renal impairment requiring dialysis.
8.7 Hepatic Impairment
No dose adjustment is required for patients with mild or moderate hepatic impairment. The effect of mild and moderate hepatic impairment on the systemic exposure to methylnaltrexone bromide has been studied in 8 subjects each, with Child-Pugh Class A and B, compared to healthy subjects. Results showed no meaningful effect of hepatic impairment on the AUC or Cmax of methylnaltrexone bromide. The effect of severe hepatic impairment on the pharmacokinetics of methylnaltrexone bromide has not been studied.
9 DRUG ABUSE AND DEPENDENCE
10 OVERDOSAGE
10.1 Human Experience
During clinical trials of RELISTOR administered subcutaneously, no cases of methylnaltrexone bromide overdose were reported. In a study of healthy volunteers (n = 41), a single dose of 0.50 mg/kg administered as a subcutaneous injection was well-tolerated. A study of healthy volunteers noted orthostatic hypotension associated with a dose of 0.64 mg/kg administered as an IV bolus.
10.2 Management of Overdosage
No specific information is available on the treatment of overdose with RELISTOR. In the event of overdose, employ the usual supportive measures, e.g., clinical monitoring and supportive therapy as dictated by the patient's clinical status. Signs or symptoms of orthostatic hypotension should be monitored, and treatment should be initiated, as appropriate.
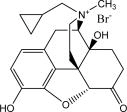
11 DESCRIPTION
RELISTOR (methylnaltrexone bromide) Subcutaneous Injection, a peripherally-acting mu-opioid receptor antagonist, is a sterile, clear and colorless to pale yellow aqueous solution. The chemical name for methylnaltrexone bromide is (R)-N-(cyclopropylmethyl) noroxymorphone methobromide. The molecular formula is C21H26NO4Br, and the molecular weight is 436.36.
Each 3 mL vial contains 12 mg of methylnaltrexone bromide in 0.6 mL of water. The excipients are 3.9 mg sodium chloride USP, 0.24 mg edetate calcium disodium USP, and 0.18 mg glycine hydrochloride. During manufacture, the pH may have been adjusted with hydrochloric acid and/or sodium hydroxide.
Each 8 mg/0.4 mL pre-filled syringe (1 mL syringe) contains 8 mg of methylnaltrexone bromide in 0.4 mL of water. The excipients are 2.6 mg sodium chloride USP, 0.16 mg edetate calcium disodium USP, and 0.12 mg glycine hydrochloride.
Each 12 mg/0.6 mL pre-filled syringe (1 mL syringe) contains 12 mg of methylnaltrexone bromide in 0.6 mL of water. The excipients are 3.9 mg sodium chloride USP, 0.24 mg edetate calcium disodium USP, and 0.18 mg glycine hydrochloride.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Methylnaltrexone bromide is a selective antagonist of opioid binding at the mu-opioid receptor. As a quaternary amine, the ability of methylnaltrexone bromide to cross the blood-brain barrier is restricted. This allows methylnaltrexone bromide to function as a peripherally-acting mu‑opioid receptor antagonist in tissues such as the gastrointestinal tract, thereby decreasing the constipating effects of opioids without impacting opioid-mediated analgesic effects on the central nervous system.
12.2 Pharmacodynamics
Use of opioids induces slowing of gastrointestinal motility and transit. Antagonism of gastrointestinal mu-opioid receptors by methylnaltrexone bromide inhibits opioid-induced delay of gastrointestinal transit time in a dose-dependent manner in rats. The effects of methylnaltrexone bromide on central mu-opioid receptors were evaluated in a pharmacodynamic study in which subjects received a dose of remifentanil, sufficient to produce pupiliary constriction, followed by placebo, naloxone, or methylnaltrexone. Following remifentanil administration, the methylnaltrexone and placebo groups showed no change in pupiliary constriction while the naloxone group showed a marked change over the time interval tested.
12.3 Pharmacokinetics
Absorption
Following subcutaneous administration, methylnaltrexone bromide is absorbed rapidly, with peak concentrations (Cmax) achieved at approximately 0.5 hours. Across the range of doses evaluated peak plasma concentration and area under the plasma concentration-time curve (AUC) increase in a dose-proportional manner, as shown in the table below.
| PHARMACOKINETIC PARAMETERS OF METHYLNALTREXONE BROMIDE FOLLOWING SINGLE SUBCUTANEOUS DOSES | |||
|---|---|---|---|
| a Expressed as mean (SD). | |||
| Parameter | 0.15 mg/kg | 0.30 mg/kg | 0.50 mg/kg |
| Cmax (ng/mL)a | 117 (32.7) | 239 (62.2) | 392 (147.9) |
| tmax (hr)b | 0.5 (0.25-0.75) | 0.5 (0.25-0.75) | 0.5 (0.25-0.75) |
| AUC24 (ng∙hr/mL)a | 175 (36.6) | 362 (63.8) | 582 (111.2) |
Distribution
Methylnaltrexone bromide undergoes moderate tissue distribution. The steady-state volume of distribution (Vss) is approximately 1.1 L/kg. The fraction of methylnaltrexone bromide bound to human plasma proteins is 11.0% to 15.3%, as determined by equilibrium dialysis.
Metabolism
In a mass balance study, approximately 60% of the administered radioactivity recovered with 5 distinct metabolites and none of the detected metabolites was in amounts over 6% of administered radioactivity. Conversion to methyl-6-naltrexol isomers (5% of total) and methylnaltrexone sulfate (1.3% of total) appear to be the primary pathways of metabolism. N‑demethylation of methylnaltrexone to produce naltrexone is not significant.
12.4 Effect on Cardiac Repolarization
In a randomized, double blind placebo- and (open-label) moxifloxacin-controlled 4-period crossover study, 56 healthy subjects were administered methylnaltrexone bromide 0.3 mg/kg and methylnaltrexone bromide 0.64 mg/kg by IV infusion over 20 minutes, placebo, and a single oral dose of moxifloxacin. At both the 0.3 mg/kg and 0.64 mg/kg methylnaltrexone bromide doses, no significant effect on the QTc interval was detected.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of methylnaltrexone bromide.
13.2 Animal Toxicology and/or Pharmacology
A single subcutaneous dose of 500 mg/kg of methylnaltrexone bromide was not lethal to rats.
Reproduction studies have been performed in pregnant rats at intravenous doses up to 25 mg/kg/day (about 14 times the recommended maximum human subcutaneous dose of 0.3 mg/kg based on the body surface area) and in pregnant rabbits at intravenous doses up to 16 mg/kg/day (about 17 times the recommended maximum human subcutaneous dose based on the body surface area) and have revealed no evidence of impaired fertility or harm to the fetus due to methylnaltrexone bromide.
In an in vitro human cardiac potassium ion channel (hERG) assay, methylnaltrexone bromide caused concentration-dependent inhibition of hERG current (1%, 12%, 13% and 40% inhibition at 30, 100, 300 and 1000 μM concentrations, respectively). Methylnaltrexone bromide had a hERG IC50 of > 1000 μM. In isolated dog Purkinje fibers, methylnaltrexone bromide caused prolongations in action potential duration (APD). The highest tested concentration (10 μM) in the dog Purkinje fiber study was about 18 and 37 times the Cmax at human subcutaneous (SC) doses of 0.3 and 0.15 mg/kg, respectively. In isolated rabbit Purkinje fibers, methylnaltrexone bromide (up to 100 μM) did not have an effect on APD, compared to vehicle control. The highest methylnaltrexone bromide concentration (100 μM) tested was about 186 and 373 times the human Cmax at SC doses of 0.3 and 0.15 mg/kg, respectively. In anesthetized dogs, methylnaltrexone bromide caused decreases in blood pressure, heart rate, cardiac output, left ventricular pressure, left ventricular end diastolic pressure, and +dP/dt at ≥ 1 mg/kg. In conscious dogs, methylnaltrexone bromide caused a dose-related increase in QTc interval. After a single IV dosage of 20 mg/kg to beagle dogs, predicted Cmax and AUC values were approximately 482 and 144 times, respectively, the exposure at human SC dose of 0.15 mg/kg and 241 times and 66 times, respectively, the exposure at a human SC dose of 0.3 mg/kg. In conscious guinea pigs, methylnaltrexone caused mild prolongation of QTc (4% over baseline) at 20 mg/kg, IV. A thorough QTc assessment was conducted in humans [see Pharmacokinetics (12.4)].
In juvenile rats administered intravenous methylnaltrexone bromide for 13 weeks, adverse clinical signs such as convulsions, tremors and labored breathing occurred at dosages of 3 and 10 mg/kg/day (about 3.2 and 11 times, respectively, the recommended human dose of 0.15 mg/kg based on the body surface area). Similar adverse clinical signs were seen in adult rats at 20 mg/kg/day (about 22 times the recommended human dose of 0.15 mg/kg based on the body surface area). Juvenile rats were found to be more sensitive to the toxicity of RELISTOR when compared to adults. The no observed adverse effect levels (NOAELs) in juvenile and adult rats were 1 and 5 mg/kg/day, respectively (about 1.1 and 5.4 times respectively, the recommended human dose of 0.15 mg/kg based on the body surface area).
In juvenile dogs administered intravenous methylnaltrexone bromide for 13 weeks, juvenile dogs had a toxicity profile similar to adult dogs. Following IV administration of methylnaltrexone bromide for 13 weeks, decreased heart rate (13.2 % reduction compared to pre-dose) in juvenile dogs and prolonged QTc interval in juvenile (9.6% compared to control) and adult (up to 15% compared to control) dogs occurred at 20 mg/kg/day (about 72 times the recommended human subcutaneous doses of 0.15 mg/kg based on the body surface area). Clinical signs consistent with effects on the CNS (including tremors and decreased activity) occurred in both juvenile and adult dogs. The NOAELs in juvenile and adult dogs were 5 mg/kg/day (about 18 times the recommended human subcutaneous doses of 0.15 mg/kg based on the body surface area).
14 CLINICAL STUDIES
The efficacy and safety of RELISTOR in the treatment of opioid-induced constipation in advanced illness patients receiving palliative care was demonstrated in two randomized, double-blind, placebo-controlled studies. In these studies, the median age was 68 years (range 21-100); 51% were females. In both studies, patients had advanced illness with a life expectancy of less than 6 months and received care to control their symptoms. The majority of patients had a primary diagnosis of incurable cancer; other primary diagnoses included end-stage COPD/emphysema, cardiovascular disease/heart failure, Alzheimer's disease/dementia, HIV/AIDS, or other advanced illnesses. Prior to screening, patients had been receiving palliative opioid therapy (median daily baseline oral morphine equivalent dose = 172 mg), and had opioid-induced constipation (either <3 bowel movements in the preceding week or no bowel movement for >2 days). Patients were on a stable opioid regimen ≥ 3 days prior to randomization (not including PRN or rescue pain medication) and received their opioid medication during the study as clinically needed. Patients maintained their regular laxative regimen for at least 3 days prior to study entry, and throughout the study. Rescue laxatives were prohibited from 4 hours before to 4 hours after taking an injection of study medication.
Study 1 compared a single, double-blind, subcutaneous dose of RELISTOR 0.15 mg/kg, or RELISTOR 0.3 mg/kg versus placebo. The double-blind dose was followed by an open-label 4‑week dosing period, where RELISTOR could be used as needed, no more frequently than 1 dose in a 24 hour period. Throughout both study periods, patients maintained their regular laxative regimen. A total of 154 patients (47 RELISTOR 0.15 mg/kg, 55 RELISTOR 0.3 mg/kg, 52 placebo) were enrolled and treated in the double-blind period. The primary endpoint was the proportion of patients with a rescue-free laxation within 4 hours of the double-blind dose of study medication. RELISTOR-treated patients had a significantly higher rate of laxation within 4 hours of the double-blind dose (62% for 0.15 mg/kg and 58% for 0.3 mg/kg) than did placebo-treated patients (14%); p < 0.0001 for each dose versus placebo (Figure 1).
Study 2 compared double-blind, subcutaneous doses of RELISTOR given every other day for 2 weeks versus placebo. Patients received opioid medication ≥ 2 weeks prior to receiving study medication. During the first week (days 1, 3, 5, 7) patients received either 0.15 mg/kg RELISTOR or placebo. In the second week the patient's assigned dose could be increased to 0.30 mg/kg if the patient had 2 or fewer rescue-free laxations up to day 8. At any time, the patient's assigned dose could be reduced based on tolerability. Data from 133 (62 RELISTOR, 71 placebo) patients were analyzed. There were 2 primary endpoints: proportion of patients with a rescue-free laxation within 4 hours of the first dose of study medication and proportion of patients with a rescue-free laxation within 4 hours after at least 2 of the first 4 doses of study medication. RELISTOR-treated patients had a higher rate of laxation within 4 hours of the first dose (48%) than placebo-treated patients (16%); p < 0.0001 (Figure 1). RELISTOR-treated patients also had significantly higher rates of laxation within 4 hours after at least 2 of the first 4 doses (52%) than did placebo-treated patients (9%); p < 0.0001. In both studies, in approximately 30% of patients, laxation was reported within 30 minutes of a dose of RELISTOR.
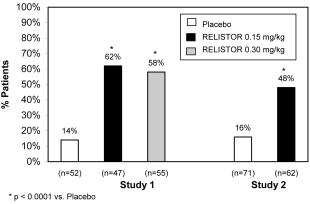
Figure 1. Laxation Response Within 4 Hours of the First Dose
In both studies, there was no evidence of differential effects of age or gender on safety or efficacy. No meaningful subgroup analysis could be conducted on race because the study population was predominantly Caucasian (88%). The rates of discontinuation due to adverse events during the double blind placebo controlled clinical trials (Study 1 and Study 2) were comparable between RELISTOR (1.2%) and placebo (2.4%).
Durability of response was demonstrated in Study 2, in which the laxation response rate was consistent from dose 1 through dose 7 over the course of the 2-week, double-blind period.
The efficacy and safety of methylnaltrexone bromide was also demonstrated in open-label treatment administered from Day 2 through Week 4 in Study 1, and in two open-label extension studies (Study 1EXT and Study 2EXT) in which RELISTOR was given as needed for up to 4 months. During open-label treatment, patients maintained their regular laxative regimen. A total of 136, 21, and 82 patients received at least 1 open-label dose in studies 1, 1EXT, and 2EXT, respectively. Laxation response rates observed during double-blind treatment with RELISTOR were maintained over the course of 3 to 4 months of open-label treatment.
There was no relationship between baseline opioid dose and laxation response in methylnaltrexone bromide-treated patients in these studies. In addition, median daily opioid dose did not vary meaningfully from baseline in either RELISTOR-treated patients or in placebo-treated patients. There were no clinically relevant changes in pain scores from baseline in either the methylnaltrexone bromide or placebo-treated patients.
16 HOW SUPPLIED/STORAGE AND HANDLING
| NDC NUMBER | PACK SIZE | CONTENTS |
| 0008-1218-01 | 1 vial per carton | one 12 mg/0.6 mL single-use vial |
| 0008-2513-02 | 7 trays per kit | Each tray contains: one 12 mg/0.6 mL single-use vial, one 1 cc (mL) syringe with retractable (27-gauge x ½-inch) needle (VanishPoint®), two alcohol swabs |
| 0008-1225-10 | 7 pre-filled syringes per carton | seven 8 mg/0.4 mL single-use pre-filled syringes with needle guard system |
| 0008-1218-10 | 7 pre-filled syringes per carton | seven 12 mg/0.6 mL single-use pre-filled syringes with needle guard system |
17 PATIENT COUNSELING INFORMATION
[See FDA-Approved Patient Labeling]
Instruct patients that the usual schedule is one dose every other day, as needed, but no more frequently than one dose in a 24-hour period.
In approximately 30% of patients in clinical trials, laxation was reported within 30 minutes of a dose of RELISTOR; therefore, advise patients to be within close proximity to toilet facilities once the drug is administered.
Instruct patients not to continue taking RELISTOR if they experience severe or persistent diarrhea. Instruct patients that common side effects of RELISTOR include transient abdominal pain, nausea and vomiting.
Instruct patients not to continue taking RELISTOR and to promptly notify their physician if they experience severe, persistent, and/or worsening abdominal symptoms because these could be symptoms of intestinal perforation [see Warnings and Precautions (5.2)].
Instruct patients to discontinue RELISTOR if they stop taking their opioid pain medication.
Read the Patient Information that comes with RELISTOR before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or your treatment.
RELISTOR is a prescription medicine used to treat constipation that is caused by prescription pain medicines, called opioids, in patients receiving supportive care for their advanced illness, when other medicines for constipation, called laxatives, have not worked well enough.
Do not take RELISTOR if you have or may have a blockage in your intestines called a mechanical bowel obstruction. Symptoms of this blockage are vomiting, stomach pain, and swelling of your abdomen. Talk to your healthcare provider if you have any of these symptoms before taking RELISTOR.
Tell your healthcare provider about all of your medical conditions, including if you:
- are pregnant or plan to become pregnant. It is not known if RELISTOR can harm your unborn baby. If you become pregnant while using RELISTOR, tell your healthcare provider right away.
- are breast-feeding or plan to breast-feed. It is not known if RELISTOR passes into your breast milk.
- have kidney problems.
Tell your healthcare provider about all medicines you take. Continue taking your other medicines for constipation unless your healthcare provider tells you to stop taking them.
- Take RELISTOR exactly as your healthcare provider tells you.
- Take RELISTOR by an injection under the skin (subcutaneous injection) of the upper arm, abdomen, or thigh.
- Do not take more than one dose in a 24-hour period.
- Most patients have a bowel movement within a few minutes to a few hours after taking a dose of RELISTOR.
- If you stop taking your prescription pain medicine, check with your healthcare provider before continuing to take RELISTOR.
- If you take more RELISTOR than prescribed, talk to your healthcare provider right away.
See the detailed Patient Instructions for Use at the end of this Patient Information leaflet for information about how to prepare and inject RELISTOR.
Common side effects of RELISTOR include:
- abdominal (stomach) pain
- gas
- nausea
- dizziness
- diarrhea
- sweating
- If you get diarrhea that is severe or does not stop while taking RELISTOR, stop taking RELISTOR and call your healthcare provider.
- If you get abdominal pain that is severe or will not go away, or nausea or vomiting that is new or worse, stop taking RELISTOR and call your healthcare provider.
These are not all of the possible side effects of RELISTOR. Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1‑800‑FDA‑1088.
- Store RELISTOR vials or pre-filled syringes at 68 to 77°F (20 to 25°C).
- Do not freeze RELISTOR.
- Keep RELISTOR away from light until you are ready to use it.
- If RELISTOR has been drawn into a syringe and you are unable to use the medicine right away, keep the syringe at room temperature for up to 24 hours. The syringe does not need to be kept away from light during the 24-hour period.
Keep RELISTOR and all medicines, needles and syringes out of the reach of children.
General information about RELISTOR
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use RELISTOR for a condition for which it was not prescribed. Do not give RELISTOR to other people, even if they have the same symptoms that you have. It may harm them.
This leaflet summarizes the most important information about RELISTOR. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about RELISTOR that is written for healthcare providers. For more information, go to WWW.RELISTOR.COM or call 1-800-934-5556.
What are the ingredients in RELISTOR?
Active ingredient: methylnaltrexone bromide
Inactive ingredients: sodium chloride, edetate calcium disodium USP, glycine hydrochloride. During manufacture, the pH may have been adjusted with hydrochloric acid and/or sodium hydroxide.


Patient Instructions for Use of RELISTOR® PRE-FILLED SYRINGE
The following instructions explain how to prepare and give an injection of RELISTOR the right way, when using a pre-filled syringe of RELISTOR.
The Patient Instructions for Use includes the following steps:
Step 1: Choosing and preparing an injection site
Step 2: Preparing the injection for pre-filled syringe
Before starting, read and make sure that you understand the Patient Instructions for Use. If you have any questions, talk to your healthcare provider.
Gather the supplies you will need for your injection. These include:
- RELISTOR pre-filled syringe
- Alcohol swab
- Cotton ball or gauze
- Adhesive bandage
- Do not use a RELISTOR pre-filled syringe more than one time, even if there is medicine left in the syringe.
- Store RELISTOR pre-filled syringes at 68°F to 77°F (20°C to 25°C). Do not freeze RELISTOR. Keep RELISTOR away from light until you are ready to use it. For more information about how to store RELISTOR, see the section called "How should I store RELISTOR?" in the FDA-Approved Patient Labeling.
- Safely throw away RELISTOR pre-filled syringes after use (see Step 4 below).
- To avoid needle-stick injuries, do not recap used needles.
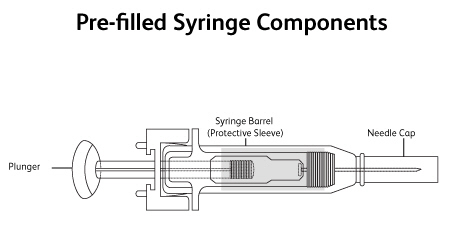
- Avoid touching the trigger fingers of the RELISTOR pre-filled syringe to keep from activating the safety device too soon. The safety device (needle guard) is activated by pressure from the plunger on the trigger fingers (Figure 1).
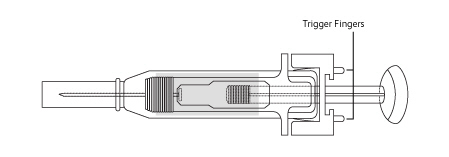
Figure 1
Step 1: Choosing and preparing an injection site
- Choose an injection site - abdomen, thighs, or upper arms. See shaded areas in Figures 2 and 3 below. Do not inject at the exact same spot each time (rotate injection sites). Do not inject into areas where the skin is tender, bruised, red or hard. Avoid areas with scars or stretch marks.
Figure 2. Abdomen or thigh – use these sites when injecting yourself or another person.
Figure 3. Upper arm – use this site only when injecting another person.

Figure 2 Figure 3
- Clean the injection site with an alcohol swab and let it air-dry. Do not touch this area again before giving the injection (Figure 4).

Figure 4
Step 2: Preparing the injection for pre-filled syringe
- Find a quiet place. Choose a flat, clean, well-lit working surface.
- Wash your hands with soap and warm water before preparing for the injection.
- Look at the pre-filled syringe of RELISTOR (Figure 5). Make sure that the dose prescribed by your healthcare provider matches the dose on the pre-filled syringe label. Look at the plunger rod of the syringe. If the dose prescribed by your healthcare provider is 8 mg, the plunger rod will be yellow; if the prescribed dose is 12 mg, the plunger rod of the syringe will be purple (Figure 5).
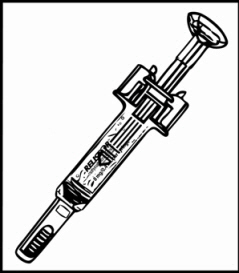
Figure 5
- The liquid in the pre-filled syringe should be clear and colorless to pale yellow, and should not have any particles in it. If not, do not use the pre-filled syringe, and call your healthcare provider.
- Firmly hold the barrel of the pre-filled syringe and pull the needle cap straight off (Figure 6). Do not touch the needle or allow it to touch any surface.
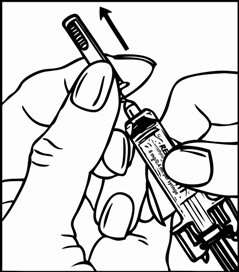
Figure 6
- Pinch the skin around the injection site (Figure 7).

Figure 7
- Insert the full length of the needle into the skin at a 45-degree angle with a quick "dart-like" motion (Figure 8).
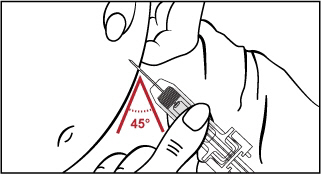
Figure 8
Let go of skin and slowly push down on the plunger with your thumb until the pre-filled syringe is empty (Figure 9). This will release the needle safety device.

Figure 9
- Continue to hold pressure on the plunger with your thumb and quickly pull the needle out of the skin. Be careful to keep the needle at the same angle as it was inserted. Then remove your thumb from the plunger to allow the protective sleeve to cover the needle (Figure 10). There may be a little bleeding at the injection site.

Figure 10
- Hold a cotton ball or gauze over the injection site (Figure 11). Do not rub the injection site. Apply an adhesive bandage to the injection site if needed.

Figure 11
- Do not re-use the pre-filled syringe or recap the needle. Place used pre-filled syringe in a closeable, puncture-resistant container. You may use a sharps container (such as a red biohazard container), a hard plastic container (such as a detergent bottle), or metal container (such as an empty coffee can). Ask your healthcare provider for instructions on the right way to throw away (dispose of) the container. There may be state and local laws about how you should throw away used needles and syringes.
- If you have any questions, talk to your healthcare provider or pharmacist.
Patient Instructions for Use of RELISTOR® VIAL AND STANDARD SYRINGE AND NEEDLE
The following instructions explain how to prepare and give an injection of RELISTOR the right way, when using a vial of RELISTOR, and a standard syringe.
The Patient Instructions for Use includes the following steps:
Step 1: Choosing and preparing an injection site
Step 2: Preparing the injection
Step 3: Preparing the syringe
Before starting, read and make sure that you understand the Patient Instructions for Use. If you have any questions, talk to your healthcare provider.
Gather the supplies you will need for your injection. These include:
- RELISTOR vial
- 1 mL syringe with a 27-gauge needle for subcutaneous use
- 2 alcohol swabs
- Cotton ball or gauze
- Adhesive bandage
Important Notes:
- Use the syringes and needles prescribed by your healthcare provider.
- Do not use a RELISTOR vial more than one time, even if there is medicine left in the vial.
- If RELISTOR has been drawn into a syringe and you are unable to use the medicine right away, keep the syringe at room temperature for up to 24 hours. The syringe does not need to be kept away from light during the 24-hour period. For more information about how to store RELISTOR, see the section called "How should I store RELISTOR?" in the FDA-Approved Patient Labeling.
- Safely throw away RELISTOR vials after use.
- Do not re-use syringes or needles.
- To avoid needle stick injuries, do not recap used needles.
Step 1: Choosing and preparing an injection site
- Choose an injection site — abdomen, thighs, or upper arms. See shaded areas in Figures 1 and 2 below. Do not inject at the exact same spot each time (rotate injection sites). Do not inject into areas where the skin is tender, bruised, red or hard. Avoid areas with scars or stretch marks.
Figure 1. Abdomen or thigh – use these sites when injecting yourself or another person.
Figure 2. Upper arm – use this site only when injecting another person.

Figure 1 Figure 2
- Clean the injection site with an alcohol swab and let it air dry. Do not touch this area again before giving the injection (Figure 3).

Figure 3
Step 2: Preparing the injection
- Find a quiet place. Choose a flat, clean, well-lit working surface.
- Wash your hands with soap and warm water before preparing for the injection.
- Look at the vial of RELISTOR (Figure 1). The liquid in the vial should be clear and colorless to pale yellow, and should not have any particles in it. If not, do not use the vial, and call your healthcare provider.
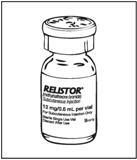
Figure 1
Step 3: Preparing the syringe
- Remove the cap from the RELISTOR vial (Figure 2).

Figure 2
- Wipe the rubber stopper with an alcohol swab (Figure 3).

Figure 3
- Firmly hold the barrel of the syringe and pull the needle cap straight off (Figure 4). Do not touch the needle or allow it to touch any surface.

Figure 4
- Carefully pull back the plunger to the line that matches the dose prescribed by your healthcare provider (Figure 5). For most patients, this will be the 0.4 ml mark which is an 8 mg dose or the 0.6 ml mark which is a 12 mg dose.

Figure 5
- Insert the needle straight down into the rubber top of the vial (Figure 6). Do not insert it at an angle. This may cause the needle to bend or break. You will feel some resistance as the needle passes through the rubber top.
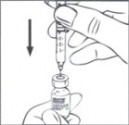
Figure 6
- Gently push down the plunger until all of the air is out of the syringe and has gone into the vial (Figure 7).

Figure 7
- With the needle still in the vial, turn the vial and syringe upside down. Hold the syringe at eye level. Make sure the tip of the needle is in the fluid. Slowly pull back on the plunger (Figure 8) to the mark that matches your prescribed dose. For most patients, this will be the 0.4 ml mark which is an 8 mg dose or the 0.6 ml mark which is a 12 mg dose.

Figure 8
- With the needle still in the vial, gently tap the side of the syringe to make any air bubbles rise to the top (Figure 9).

Figure 9
- Slowly push the plunger up until all air bubbles are out of the syringe (Figure 10).
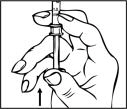
Figure 10
- Make sure the tip of the needle is in the fluid. Slowly pull back the plunger to draw the right amount of liquid back into the syringe (Figure 11).

Figure 11
Check to be sure that you have the right dose of RELISTOR in the syringe.
- Slowly withdraw the needle from the vial. Do not touch the needle or allow it to touch any surface. Safely throw away the unused medicine in the vial. See Step 5.
Step 4: Injecting RELISTOR
- Pinch the skin around the injection site (Figure 12).

Figure 12
- Insert the full length of the needle into the skin at a 45-degree angle with a quick "dart-like" motion (Figure 13).
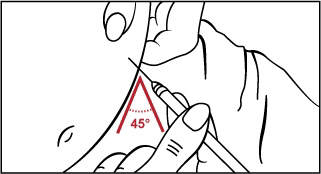
Figure 13
- Let go of skin and slowly push down on the plunger until the syringe is empty (Figure 14).

Figure 14
- When the syringe is empty, quickly pull the needle out of the skin, being careful to keep it at the same angle as it was inserted. There may be a little bleeding at the injection site.
- Hold a cotton ball or gauze over the injection site (Figure 15). Do not rub the injection site. Apply an adhesive bandage to the injection site if needed.

Figure 15
Step 5: Disposing of supplies
- Do not re-use a syringe or needle.
- Do not recap a used needle.
- Place used needle, syringes, and vials in a closeable, puncture-resistant container. You may use a sharps container (such as a red biohazard container), a hard plastic container (such as a detergent bottle), or metal container (such as an empty coffee can). Ask your healthcare provider for instructions on the right way to throw away (dispose of) the container. There may be state and local laws about how you should throw away used needles and syringes.
Patient Instructions for Use of RELISTOR®
VIAL AND SYRINGE WITH RETRACTABLE NEEDLE IN TRAY
The following instructions explain how to prepare and give an injection of RELISTOR the right way, when using a RELISTOR tray containing a syringe with a retractable needle. A retractable needle is one that is pulled back so that it is covered after use, to prevent needle stick injury.
The Patient Instructions for Use includes the following steps:
Step 1: Choosing and preparing an injection site
Step 2: Preparing the injection
Step 3: Preparing the syringe
Before starting, read and make sure that you understand the Patient Instructions for Use. Familiarize yourself with the RELISTOR tray, which contains the supplies you need for an injection. If you have any questions, talk to your healthcare provider. Your tray should include the following:
- RELISTOR vial
- 1 mL syringe with retractable needle (VanishPoint®)
- 2 alcohol swabs
- Prescribing Information - information about RELISTOR that is written for healthcare professionals
- Patient Instructions for Use of RELISTOR - instructions about RELISTOR that are written for patients
In addition, you will need a cotton ball or gauze, and you may need an adhesive bandage.
Important Notes:
- Do not use a RELISTOR vial more than one time, even if there is medicine left in the vial.
- If RELISTOR has been drawn into a syringe and you are unable to use the medicine right away, keep the syringe at room temperature for up to 24 hours. The syringe does not need to be kept away from light during the 24-hour period. For more information about how to store RELISTOR, see the section called "How should I store RELISTOR?" in the FDA-Approved Patient Labeling.
- Safely throw away RELISTOR vials after use.
- Do not reuse syringes and needles.
- To avoid needle stick injuries, do not recap used needles.
Step 1: Choosing and preparing an injection site
- Choose an injection site — abdomen, thighs, or upper arms. See shaded areas in Figures 1 and 2 below. Do not inject at the exact same spot each time (rotate injection sites). Do not inject into areas where the skin is tender, bruised, red, or hard. Avoid areas with scars or stretch marks.
Figure 1. Abdomen or thigh – use these sites when injecting yourself or another person.
Figure 2. Upper arm – use this site only when injecting another person.

Figure 1 Figure 2
- Clean the injection site with an alcohol swab and let it air dry. Do not touch this area again before giving the injection (Figure 3).

Figure 3
Step 2: Preparing the injection
- Find a quiet place. Choose a flat, clean, well-lit working surface.
- Wash your hands with soap and warm water before preparing for the injection.
- Look at the vial of RELISTOR (Figure 4). The liquid in the vial should be clear and colorless to pale yellow, and should not have any particles in it. If not, do not use the vial and call your healthcare provider.
Figure 4
Step 3: Preparing the syringe
- Remove the cap from the vial containing RELISTOR (Figure 5).

Figure 5
- Wipe the rubber stopper with an alcohol swab (Figure 6).

Figure 6
- Firmly hold the barrel of the syringe and remove the needle cap straight off (Figure 7). Do not touch the needle or allow it to touch any surface.

Figure 7
- Carefully pull back on the plunger to the line that matches the dose prescribed by your healthcare provider (Figure 8). For most patients, this will be the 0.4 mL mark which is an 8 mg dose or the 0.6 mL mark which is a 12 mg dose.

Figure 8
- Insert the needle straight down into the rubber top of the RELISTOR vial (Figure 9). Do not insert it at an angle. This may cause the needle to bend or break. You will feel some resistance as the needle passes through the rubber top.
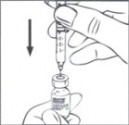
Figure 9
- Gently push down the plunger until you feel resistance, and most of the air has gone out of the syringe and into the vial (Figure 10). Do not push past the resistance point. Doing this will make the needle retract (pull back) into the syringe barrel.
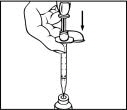
Figure 10
- With the needle still in the vial, turn the vial and syringe upside down. Hold the syringe at eye level. Make sure the tip of the needle is in the fluid. Slowly pull back on the plunger (Figure 11) to the mark that matches your prescribed dose (usually the 0.4 mL mark which is an 8 mg dose or the 0.6 mL mark which is a 12 mg dose).

Figure 11
You may see some fluid or bubbles inside the vial when the syringe is filled. This is normal.
- With the needle still in the vial, gently tap the syringe to make any air bubbles rise to the top (Figure 12).

Figure 12
- Slowly push the plunger up until all air bubbles are out of the syringe (Figure 13).
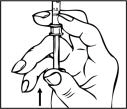
Figure 13
- Make sure the tip of the needle is in the fluid. Slowly pull back the plunger to draw the right amount of liquid back into the syringe (Figure 14).

Figure 14
Check to be sure that you have the right dose of RELISTOR in the syringe.
Note: A small air bubble may stay in the syringe. This is okay and it will not affect the dose of medicine in the syringe.
- Slowly withdraw the needle from the vial (do not touch the needle or allow the needle to touch any surface). Safely throw away the unused medicine in the vial. See Step 5.
Step 4: Injecting RELISTOR
- Pinch the skin around the injection site as you were instructed (Figure 15).

Figure 15
- Insert the full length of the needle into the skin at 45-degree angle with a "quick dart-like" motion (Figure 16).
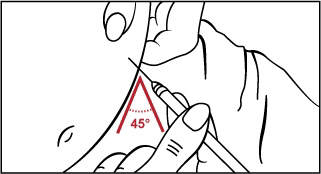
Figure 16
- Let go of the skin and slowly push down on the plunger past the resistance point, until the syringe is empty and you hear a click (Figure 17).

Figure 17
- The click sound means that the needle (Figure 18) has been retracted (pulled back) into the syringe barrel (Figure 19).

Figure 18 Figure 19
- Hold a cotton ball or gauze over the injection site (Figure 20). Do not rub the injection site. Apply an adhesive bandage to the injection site if needed.

Figure 20
Step 5: Disposing of supplies
- Do not re-use a syringe or needle.
- Do not recap a used needle.
- Place used needles, syringes and vials in a closeable, puncture-resistant container. You may use a sharps container (such as a red biohazard container), a hard plastic container (such as a detergent bottle), or a metal container (such as an empty coffee can). Ask your healthcare provider for instructions on the right way to throw away (dispose of) the container. There may be state and local laws about how you should throw away used needles and syringes.
- If you have any questions, talk to your healthcare provider or pharmacist.


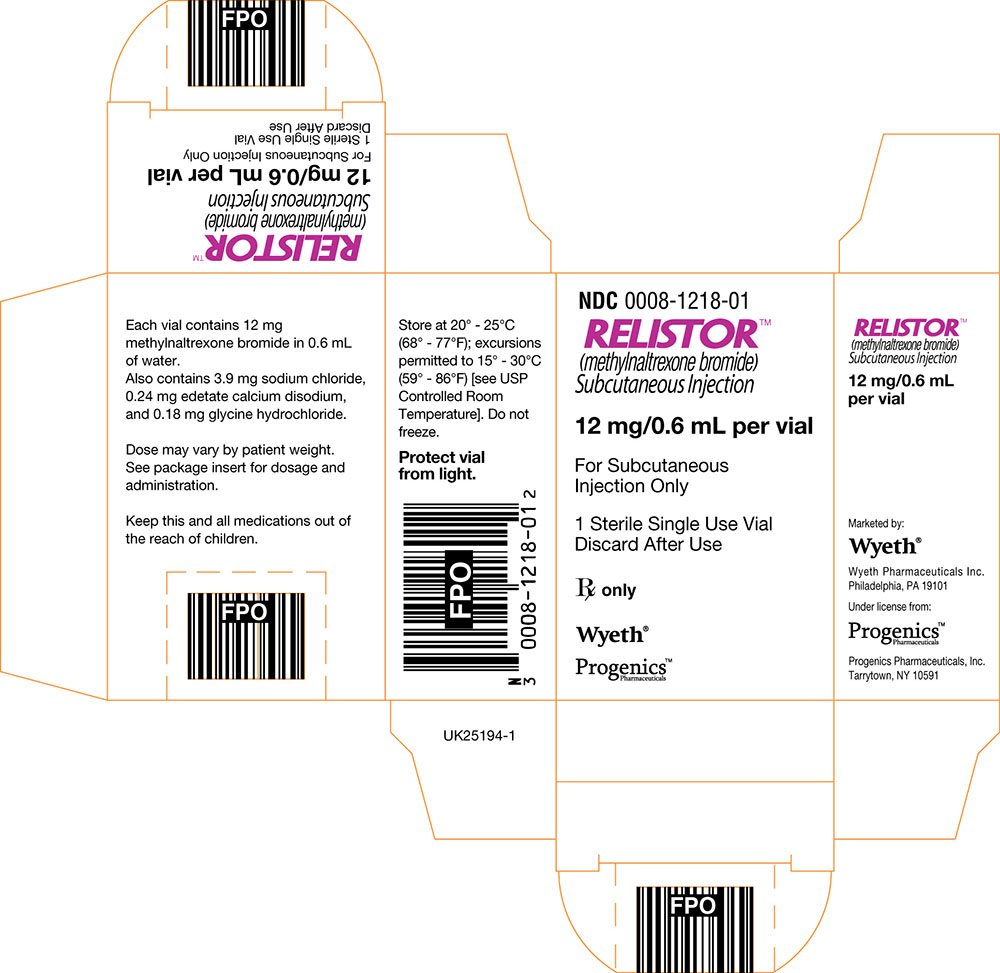
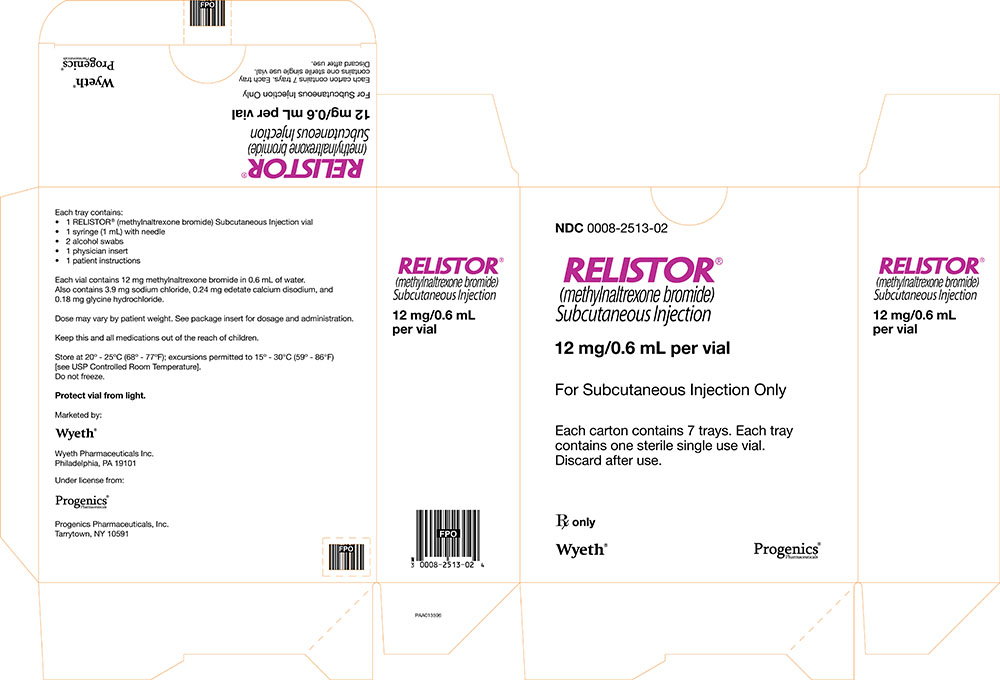
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - TRAY
For Subcutaneous Injection Only
Contains one sterile single use vial

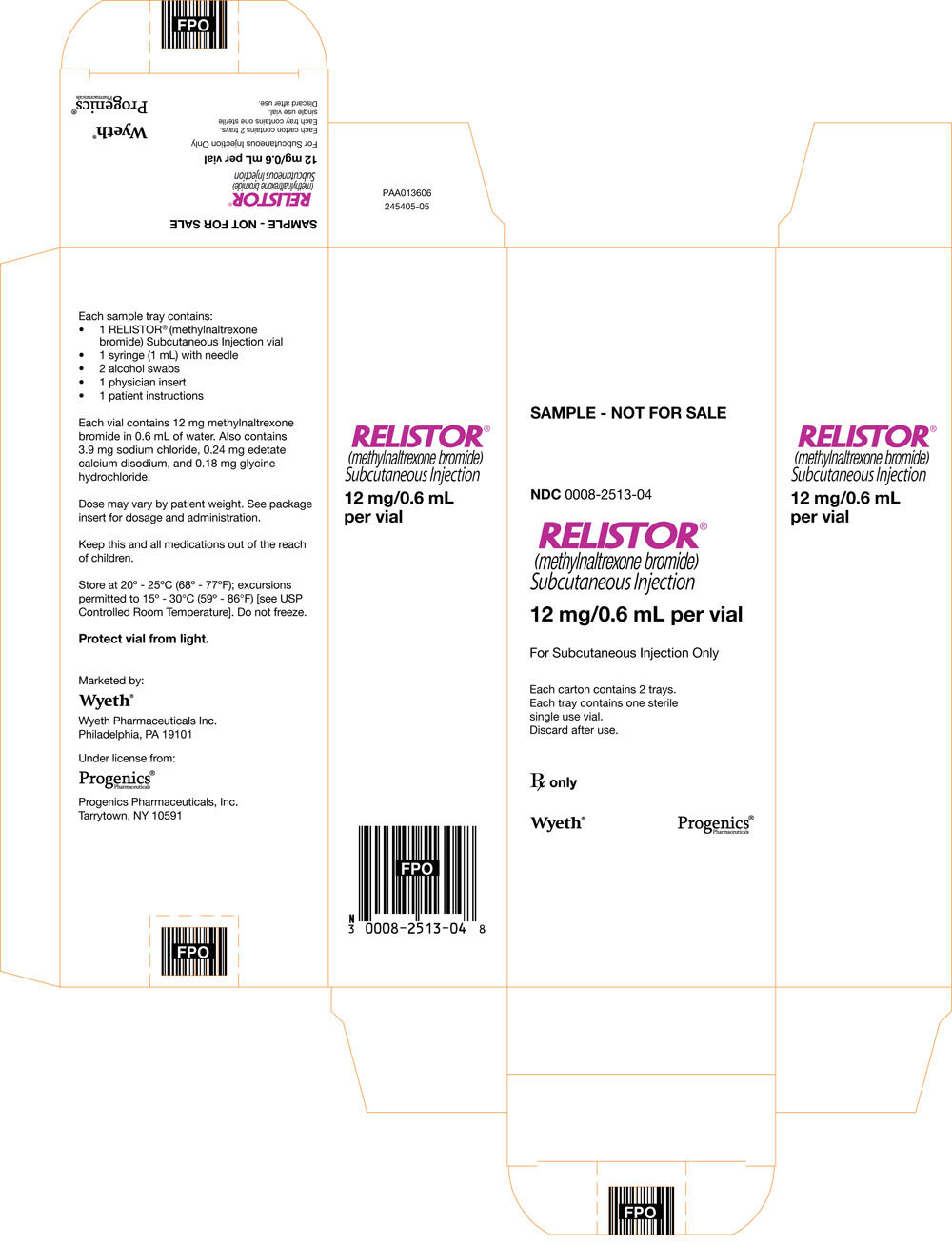
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - CARTON
For Subcutaneous Injection Only
Each carton contains 7 trays. Each tray contains one sterile single use vial.
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - VIAL SAMPLE
For Subcutaneous Injection Only
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - TRAY SAMPLE
For Subcutaneous Injection Only
Contains one sterile single use vial
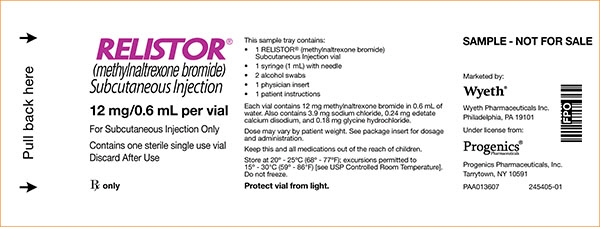
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - CARTON SAMPLE
For Subcutaneous Injection Only
Each tray contains one sterile single use vial.
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 8 mg/0.4 mL - SYRINGE LABEL
For Subcutaneous Injection Only
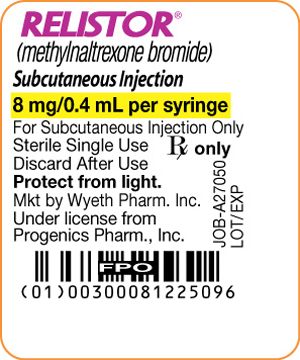
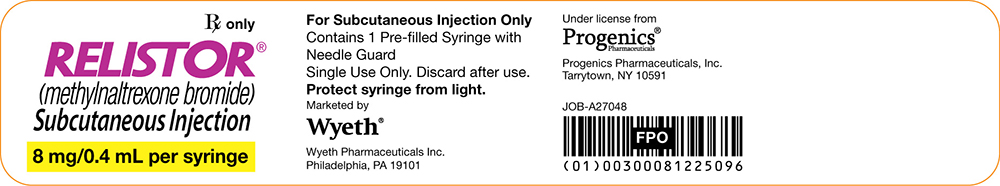
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 8 mg/0.4 mL - SYRINGE LIDDING
For Subcutaneous Injection Only
Contains 1 Pre-filled Syringe with Needle Guard
Single Use Only. Discard after use.
Under license from Progenics Pharmaceuticals
Progenics Pharmaceuticals, Inc.
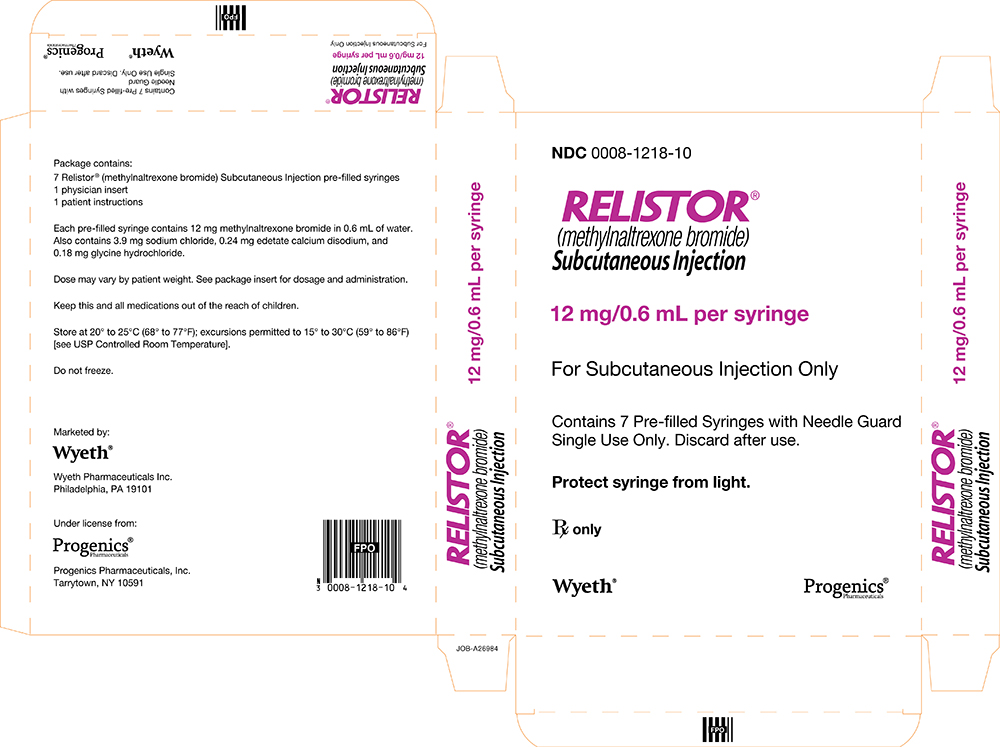
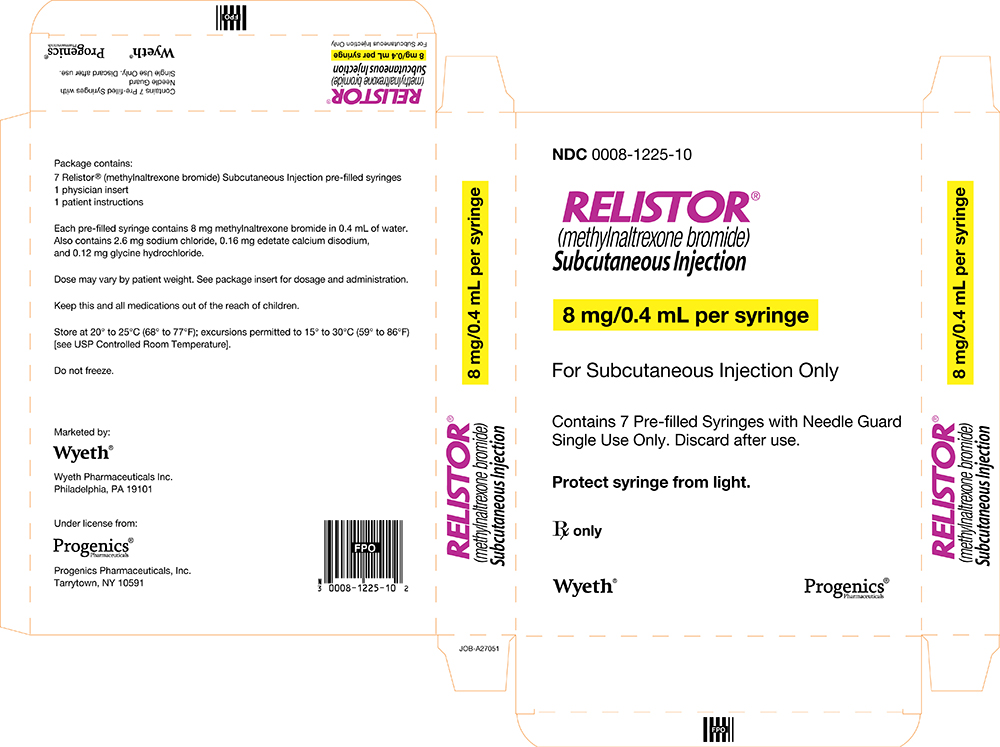
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 8 mg/0.4 mL - CARTON
For Subcutaneous Injection Only
Contains 7 Pre-filled Syringes with Needle Guard
Single Use Only. Discard after use.
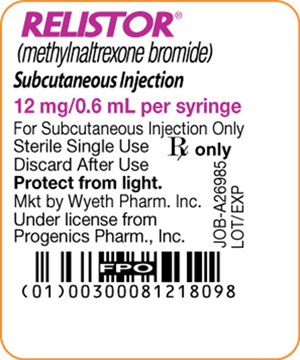
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - SYRINGE LABEL
For Subcutaneous Injection Only
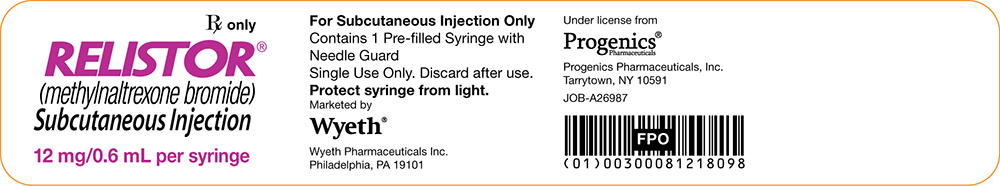
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 12 mg/0.6 mL - SYRINGE LIDDING
For Subcutaneous Injection Only
Contains 1 Pre-filled Syringe with Needle Guard
Single Use Only. Discard after use.
Under license from Progenics Pharmaceuticals
Progenics Pharmaceuticals, Inc.
| RELISTOR
methylnaltrexone bromide kit |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| RELISTOR
methylnaltrexone bromide injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RELISTOR
methylnaltrexone bromide injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Wyeth Pharmaceuticals Inc., a subsidiary of Pfizer Inc. (828831441) |
| Registrant - Progenics Pharmaceuticals Inc. (195551247) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Triad Isotopes, Inc. | 196172063 | MANUFACTURE(0008-1225, 0008-1218, 0008-2513) | |