FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
XALATAN is indicated for the reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension.
2 DOSAGE AND ADMINISTRATION
The recommended dosage is one drop in the affected eye(s) once daily in the evening. If one dose is missed, treatment should continue with the next dose as normal.
The dosage of XALATAN should not exceed once daily; the combined use of two or more prostaglandins, or prostaglandin analogs including XALATAN is not recommended. It has been shown that administration of these prostaglandin drug products more than once daily may decrease the IOP lowering effect or cause paradoxical elevations in IOP.
Reduction of the IOP starts approximately 3 to 4 hours after administration and the maximum effect is reached after 8 to 12 hours.
XALATAN may be used concomitantly with other topical ophthalmic drug products to lower IOP. In vitro studies have shown that precipitation occurs when eye drops containing thimerosal are mixed with XALATAN. If more than one topical ophthalmic drug is being used, the drugs should be administered at least five (5) minutes apart. Contact lenses should be removed prior to the administration of XALATAN, and may be reinserted 15 minutes after administration.
4 CONTRAINDICATIONS
Known hypersensitivity to latanoprost, benzalkonium chloride, or any other ingredients in this product.
5 WARNINGS AND PRECAUTIONS
5.1 Pigmentation
XALATAN has been reported to cause changes to pigmented tissues. The most frequently reported changes have been increased pigmentation of the iris, periorbital tissue (eyelid), and eyelashes. Pigmentation is expected to increase as long as latanoprost is administered.
The pigmentation change is due to increased melanin content in the melanocytes rather than to an increase in the number of melanocytes. After discontinuation of latanoprost, pigmentation of the iris is likely to be permanent, while pigmentation of the periorbital tissue and eyelash changes have been reported to be reversible in some patients. Patients who receive treatment should be informed of the possibility of increased pigmentation. Beyond 5 years the effects of increased pigmentation are not known [see Clinical Studies (14.2)].
Iris color change may not be noticeable for several months to years. Typically, the brown pigmentation around the pupil spreads concentrically towards the periphery of the iris and the entire iris or parts of the iris become more brownish. Neither nevi nor freckles of the iris appear to be affected by treatment. While treatment with XALATAN can be continued in patients who develop noticeably increased iris pigmentation, these patients should be examined regularly.
5.2 Eyelash Changes
XALATAN may gradually change eyelashes and vellus hair in the treated eye; these changes include increased length, thickness, pigmentation, the number of lashes or hairs, and misdirected growth of eyelashes. Eyelash changes are usually reversible upon discontinuation of treatment.
5.3 Intraocular Inflammation
XALATAN should be used with caution in patients with a history of intraocular inflammation (iritis/uveitis) and should generally not be used in patients with active intraocular inflammation because inflammation may be exacerbated.
5.4 Macular Edema
Macular edema, including cystoid macular edema, has been reported during treatment with XALATAN. XALATAN should be used with caution in aphakic patients, in pseudophakic patients with a torn posterior lens capsule, or in patients with known risk factors for macular edema.
5.5 Herpetic Keratitis
Reactivation of herpes simplex keratitis has been reported during treatment with XALATAN. XALATAN should be used with caution in patients with a history of herpetic keratitis. XALATAN should be avoided in cases of active herpes simplex keratitis because inflammation may be exacerbated.
5.6 Bacterial Keratitis
There have been reports of bacterial keratitis associated with the use of multiple-dose containers of topical ophthalmic products. These containers had been inadvertently contaminated by patients who, in most cases, had a concurrent corneal disease or a disruption of the ocular epithelial surface.
6 ADVERSE REACTIONS
The following adverse reactions were reported in postmarketing experience and are discussed in greater detail in other sections of the label:
- •
- Iris pigmentation changes [see Warnings and Precautions (5.1)]
- •
- Eyelid skin darkening [see Warnings and Precautions (5.1)]
- •
- Eyelash changes (increased length, thickness, pigmentation, and number of lashes) [see Warnings and Precautions (5.2)]
- •
- Intraocular inflammation (iritis/uveitis) [see Warnings and Precautions (5.3)]
- •
- Macular edema, including cystoid macular edema [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
XALATAN was studied in three multicenter, randomized, controlled clinical trials. Patients received 50 mcg/mL XALATAN once daily or 5 mg/mL active-comparator (timolol) twice daily. The patient population studied had a mean age of 65±10 years. Seven percent of patients withdrew before the 6-month endpoint.
|
Symptom/Finding |
Adverse Reactions (incidence (%)) |
|
|
Latanoprost (n=460) |
Timolol (n=369) |
|
|
Foreign body sensation |
13 |
8 |
|
Punctate keratitis |
10 |
9 |
|
Stinging |
9 |
12 |
|
Conjunctival hyperemia |
8 |
3 |
|
Blurred vision |
8 |
8 |
|
Itching |
8 |
8 |
|
Burning |
7 |
8 |
|
Increased pigmentation of the Iris |
7 |
0 |
Less than 1% of the patients treated with XALATAN required discontinuation of therapy because of intolerance to conjunctival hyperemia.
|
Adverse Reactions (incidence (%)) |
||
|
Latanoprost (n=460) |
Timolol (n=369) |
|
|
Ocular Events/Signs and Symptoms | ||
|
Excessive tearing |
4 |
6 |
|
Eyelid discomfort/pain |
4 |
2 |
|
Dry eye |
3 |
3 |
|
Eye pain |
3 |
3 |
|
Eyelid margin crusting |
3 |
3 |
|
Erythema of the eyelid |
3 |
2 |
|
Photophobia |
2 |
1 |
|
Eyelid edema |
1 |
3 |
|
Blepharitis |
1 |
3 |
|
Systemic Events | ||
|
Upper respiratory tract infection/nasopharyngitis/influenza |
3 |
3 |
|
Myalgia/arthralgia/back pain |
1 |
0.5 |
|
Rash/allergic skin reaction |
1 |
0.3 |
6.2 Postmarketing Experience
The following reactions have been identified during postmarketing use of XALATAN in clinical practice. Because they are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The reactions, which have been chosen for inclusion due to either their seriousness, frequency of reporting, possible causal connection to XALATAN, or a combination of these factors, include:
Nervous System Disorders: Dizziness; headache; toxic epidermal necrolysis
Eye Disorders: Eyelash and vellus hair changes of the eyelid (increased length, thickness, pigmentation, and number of eyelashes); keratitis; corneal edema and erosions; intraocular inflammation (iritis/uveitis); macular edema, including cystoid macular edema; trichiasis; periorbital and lid changes resulting in deepening of the eyelid sulcus; iris cyst; eyelid skin darkening; localized skin reaction on the eyelids; conjunctivitis; pseudopemphigoid of the ocular conjunctiva.
Respiratory, Thoracic and Mediastinal Disorders: Asthma and exacerbation of asthma; dyspnea
Gastrointestinal Disorders: Nausea; vomiting
Skin and Subcutaneous Tissue Disorders: Pruritis
Infections and Infestations: Herpes keratitis
Cardiac Disorders: Angina; palpitations; angina unstable
General Disorders and Administration Site Conditions: Chest pain
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate and well-controlled studies of XALATAN administration in pregnant women.to inform drug-associated risks.
In animal reproduction studies, intravenous (IV) administration of latanoprost to pregnant rabbits and rats throughout the period of organogenesis produced malformations, embryofetal lethality and spontaneous abortion at clinically relevant doses [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. However, the background risk in the U.S. general population of major birth defects is 2 to 4%, and of miscarriage is 15 to 20% of clinically recognized pregnancies.
Data
Animal Data
Embryofetal studies were conducted in pregnant rabbits administered latanoprost daily by IV injection on gestation days 6 through 18, to target the period of organogenesis. A no observed adverse effect level (NOAEL) was not established for rabbit developmental toxicity. Post-implantation loss due to late resorption was shown as doses ≥0.2 mcg/kg/day (equivalent to 1.3 times the maximum recommended human ophthalmic dose [RHOD], on a mg/m2 basis, assuming 100% absorption). Spina bifida and abortion occurred at 5 mcg/kg/day (equivalent to 32 times the maximum RHOD). Total litter loss due to early resorption was observed at doses ≥50 mcg/kg/day (324 times the maximum RHOD). Transient signs of maternal toxicity were observed after IV dosing (increased breathing, muscle tremors, slight motor incoordination) at 300 mcg/kg/day (1946 times the maximum RHOD). No maternal toxicity was observed at doses up to 50 mcg/kg/day.
Embryofetal studies were conducted in pregnant rats administered latanoprost daily by IV injection on gestation days 6 through 15, to target the period of organogenesis. A NOAEL for rat developmental toxicity was not established. Cleft palate was observed at 1 mcg/kg (equivalent to 3.2 times the maximum RHOD, on a mg/m2 basis, assuming 100% absorption). Brain porencephalic cyst(s) were observed ≥50 mcg/kg (162 times the maximum RHOD). Skeletal anomalies were observed at 250 mcg/kg (811 times the maximum RHOD). No maternal toxicity was detectable at 250 mcg/kg/day.
Prenatal and postnatal development was assessed in rats. Pregnant rats were administered latanoprost daily by IV injection from gestation day 15, through delivery, until weaning (lactation Day 21). No adverse effects on rat offspring were observed at doses up to 10 mcg/kg/day (32 times the maximum RHOD, on a mg/m2 basis, assuming 100% absorption). At 100 mcg/kg/day (324 times the maximum RHOD), maternal deaths and pup mortality occurred.
8.2 Lactation
Risk Summary
It is not known whether this drug or its metabolites are excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when XALATAN is administered to a nursing woman.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for XALATAN and any potential adverse effects on the breastfed child from XALATAN.
10 OVERDOSAGE
IV infusion of up to 3 mcg/kg of latanoprost in healthy volunteers produced mean plasma concentrations 200 times higher than during clinical treatment with XALATAN and no adverse reactions were observed. IV dosages of 5.5 to 10 mcg/kg caused abdominal pain, dizziness, fatigue, hot flushes, nausea, and sweating.
If overdosage with XALATAN occurs, treatment should be symptomatic.
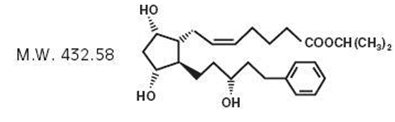
11 DESCRIPTION
Latanoprost is a prostaglandin F2α analogue. Its chemical name is isopropyl-(Z)-7[(1R,2R,3R,5S)3,5-dihydroxy-2-[(3R)-3-hydroxy-5-phenylpentyl]cyclopentyl]-5-heptenoate. Its molecular formula is C26H40O5 and its chemical structure is:
Latanoprost is a colorless to slightly yellow oil that is very soluble in acetonitrile and freely soluble in acetone, ethanol, ethyl acetate, isopropanol, methanol, and octanol. It is practically insoluble in water.
XALATAN (latanoprost ophthalmic solution) 0.005% is supplied as a sterile, isotonic, buffered aqueous solution of latanoprost with a pH of approximately 6.7 and an osmolality of approximately 267 mOsmol/kg. Each mL of XALATAN contains 50 mcg of latanoprost. Benzalkonium chloride, 0.02% is added as a preservative. The inactive ingredients are: sodium chloride, sodium dihydrogen phosphate monohydrate, disodium hydrogen phosphate anhydrous, and water for injection. One drop contains approximately 1.5 mcg of latanoprost.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Latanoprost is a prostaglandin F2α analogue that is believed to reduce the IOP by increasing the outflow of aqueous humor. Studies in animals and man suggest that the main mechanism of action is increased uveoscleral outflow. Elevated IOP represents a major risk factor for glaucomatous field loss. The higher the level of IOP, the greater the likelihood of optic nerve damage and visual field loss.
12.2 Pharmacodynamics
Reduction of the IOP in man starts about 3-4 hours after administration and maximum effect is reached after 8-12 hours. IOP reduction is present for at least 24 hours.
12.3 Pharmacokinetics
Absorption
Latanoprost is absorbed through the cornea where the isopropyl ester prodrug is hydrolyzed to the acid form to become biologically active.
Distribution
The distribution volume in humans is 0.16 ± 0.02 L/kg. The acid of latanoprost can be measured in aqueous humor during the first 4 hours, and in plasma only during the first hour after local administration. Studies in man indicate that the peak concentration in the aqueous humor is reached about two hours after topical administration.
Elimination
Metabolism
Latanoprost, an isopropyl ester prodrug, is hydrolyzed by esterases in the cornea to the biologically active acid. The active acid of latanoprost reaching the systemic circulation is primarily metabolized by the liver to the 1,2-dinor and 1,2,3,4-tetranor metabolites via fatty acid β-oxidation.
Excretion
The elimination of the acid of latanoprost from human plasma is rapid (t1/2 = 17 min) after both IV and topical administration. Systemic clearance is approximately 7 mL/min/kg. Following hepatic β-oxidation, the metabolites are mainly eliminated via the kidneys. Approximately 88% and 98% of the administered dose are recovered in the urine after topical and IV dosing, respectively.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Latanoprost was not carcinogenic in either mice or rats when administered by oral gavage at doses of up to 170 mcg/kg/day (approximately 2800 times the recommended maximum human dose) for up to 20 and 24 months, respectively.
Mutagenesis
Latanoprost was not mutagenic in bacteria, in mouse lymphoma, or in mouse micronucleus tests. Chromosome aberrations were observed in vitro with human lymphocytes. Additional in vitro and in vivo studies on unscheduled DNA synthesis in rats were negative.
Impairment of Fertility
Latanoprost has not been found to have any effect on male or female fertility in rat studies at IV doses up to 250 mcg/kg/day (811 times the maximum RHOD, on a mg/m2 basis, assuming 100% absorption).
14 CLINICAL STUDIES
14.1 Elevated Baseline IOP
Patients with mean baseline IOP of 24 – 25 mmHg who were treated for 6 months in multi-center, randomized, controlled trials demonstrated 6 – 8 mmHg reductions in IOP. This IOP reduction with XALATAN 0.005% dosed once daily was equivalent to the effect of timolol 0.5% dosed twice daily.
14.2 Progression of Increased Iris Pigmentation
A 3-year open-label, prospective safety study with a 2-year extension phase was conducted to evaluate the progression of increased iris pigmentation with continuous use of XALATAN once-daily as adjunctive therapy in 519 patients with open-angle glaucoma. The analysis was based on observed-cases population of the 380 patients who continued in the extension phase.
Results showed that the onset of noticeable increased iris pigmentation occurred within the first year of treatment for the majority of the patients who developed noticeable increased iris pigmentation. Patients continued to show signs of increasing iris pigmentation throughout the 5 years of the study. Observation of increased iris pigmentation did not affect the incidence, nature, or severity of adverse events (other than increased iris pigmentation) recorded in the study. IOP reduction was similar regardless of the development of increased iris pigmentation during the study.
16 HOW SUPPLIED/STORAGE AND HANDLING
XALATAN is a clear, isotonic, buffered, preserved colorless solution of latanoprost 50 mcg/mL (0.005%). It is supplied as a 2.5 mL solution in a 5 mL clear low density polyethylene bottle with a clear polyethylene dropper tip, a turquoise high density polyethylene screw cap, and a tamper-evident clear low density polyethylene overcap.
2.5 mL fill, 50 mcg/mL (0.005%): Package of 1 bottle: NDC 0013-8303-04
Storage: Protect from light. Store unopened bottle(s) under refrigeration at 2°C to 8°C (36°F to 46°F). During shipment to the patient, the bottle may be maintained at temperatures up to 40°C (104°F) for a period not exceeding 8 days. Once a bottle is opened for use, it may be stored at room temperature up to 25°C (77°F) for 6 weeks.
17 PATIENT COUNSELING INFORMATION
Potential for Pigmentation
Advise patients about the potential for increased brown pigmentation of the iris, which may be permanent. Inform patients about the possibility of eyelid skin darkening, which may be reversible after discontinuation of XALATAN [see Warnings and Precautions (5.1)].
Potential for Eyelash Changes
Inform patients of the possibility of eyelash and vellus hair changes in the treated eye during treatment with XALATAN. These changes may result in a disparity between eyes in length, thickness, pigmentation, number of eyelashes or vellus hairs, and/or direction of eyelash growth. Eyelash changes are usually reversible upon discontinuation of treatment.
Handling the Container
Instruct patients to avoid allowing the tip of the dispensing container to contact the eye or surrounding structures because this could cause the tip to become contaminated by common bacteria known to cause ocular infections. Serious damage to the eye and subsequent loss of vision may result from using contaminated solutions [see Warnings and Precautions (5.6)].
When to Seek Physician Advice
Advise patients that if they develop an intercurrent ocular condition (e.g., trauma or infection) or have ocular surgery, or develop any ocular reactions, particularly conjunctivitis and eyelid reactions, they should immediately seek their physician’s advice concerning the continued use of the multiple-dose container.
Contact Lens Use
Advise patients that XALATAN contains benzalkonium chloride, which may be absorbed by contact lenses. Contact lenses should be removed prior to administration of the solution. Lenses may be reinserted 15 minutes following administration of XALATAN.
Use with Other Ophthalmic Drugs
Advise patients that if more than one topical ophthalmic drug is being used, the drugs should be administered at least five (5) minutes apart.
If a Dose is Missed
Advise patients that if one dose is missed, treatment should continue with the next dose as normal.
This product’s labeling may have been updated. For the most recent prescribing information, please visit www.pfizer.com.
Pfizer Manufacturing Belgium NV
Puurs, Belgium
LAB-0135-14.1
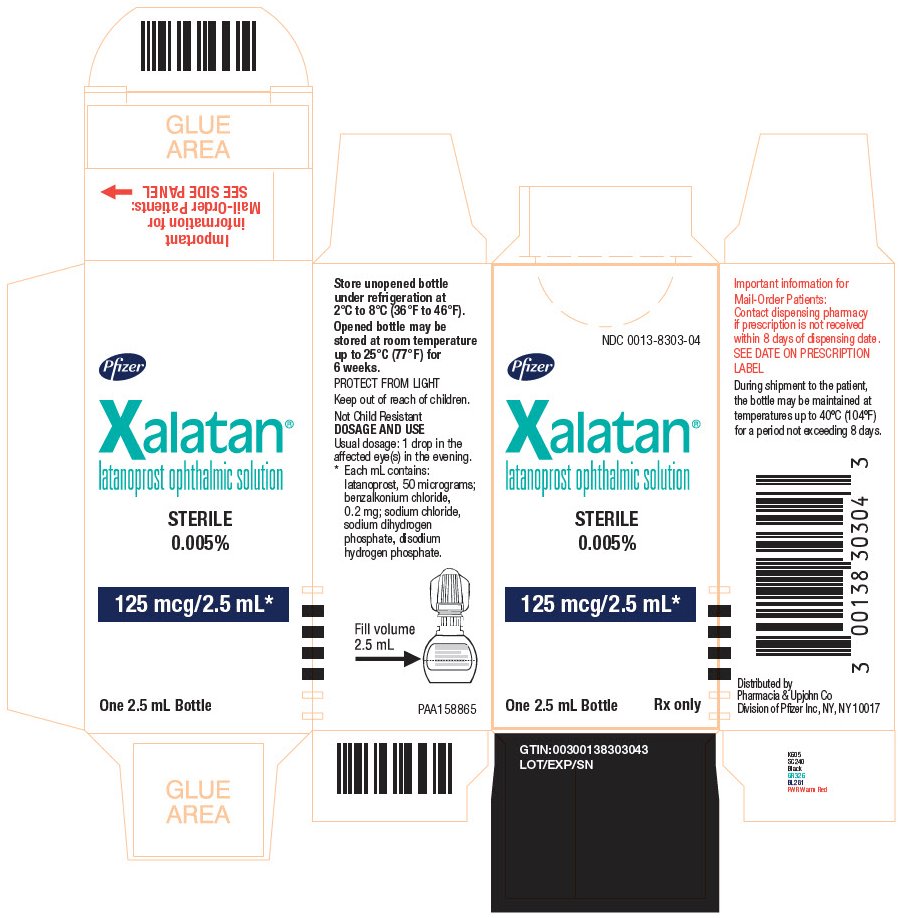
PRINCIPAL DISPLAY PANEL - 2.5 mL
NDC 0013-8303-04
Pfizer
Xalatan®
latanoprost ophthalmic solution
STERILE
0.005%
125 mcg/2.5 mL*
One 2.5 mL Bottle Rx only
Store unopened bottle
under refrigeration at
2°C to 8°C (36°F to 45°F).
Opened bottle may be
stored at room temperature
up to 25°C (77°F) for
6 weeks.
PROTECT FROM LIGHT
Keep out of reach of children.
Not Child Resistant
DOSAGE AND USE
Usual doeage: 1 drop in the
affected eye(s) in the evening.
* Each mL contains:
latanoprost, 50 micorgrams:
benzalkonium chloride,
0.2 mg; sodium chloride,
sodium dihydrogen
phosphate, disodium
hydrogen phosphate.
Important information for
Mail-Order Patients:
Contact dispensing pharmacy
if prescription is not received
within 8 days of dispensing date.
SEE DATE ON PRESCRIPTION
LABEL
During shipment to the patient,
the bottle may be maintained at
temperatures up to 40°C (104°F)
for a period not exceeding 8 days.
Distributed by
Pharmacia & Upjohn Co
Division of Pfizer Inc, NY, NY 10017