FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Prevention of Chemotherapy Induced Nausea and Vomiting (CINV)
EMEND1, in combination with other antiemetic agents, is indicated for the:
- prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy (HEC) including high-dose cisplatin
- prevention of nausea and vomiting associated with initial and repeat courses of moderately emetogenic cancer chemotherapy (MEC) [see Dosage and Administration (2.1)].
- 1
-
Registered trademark of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
Copyright © 2003, 2005, 2006 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All Rights Reserved
1.2 Prevention of Postoperative Nausea and Vomiting (PONV)
EMEND is indicated for the prevention of postoperative nausea and vomiting [see Dosage and Administration (2.2)].
1.3 Limitations of Use
EMEND has not been studied for the treatment of established nausea and vomiting.
Chronic continuous administration is not recommended [see Warnings and Precautions (5.5)].
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Chemotherapy Induced Nausea and Vomiting (CINV)
Capsules of EMEND (aprepitant) are given for 3 days as part of a regimen that includes a corticosteroid and a 5-HT3 antagonist. The recommended dose of EMEND is 125 mg orally 1 hour prior to chemotherapy treatment (Day 1) and 80 mg orally once daily in the morning on Days 2 and 3.
EMEND may be taken with or without food.
EMEND (fosaprepitant dimeglumine) for Injection (115 mg) is a prodrug of aprepitant and may be substituted for oral EMEND (125 mg), 30 minutes prior to chemotherapy, on Day 1 only of the CINV regimen as an intravenous infusion administered over 15 minutes.
In clinical studies with EMEND, the following regimen was used for the prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy:
| Day 1 | Day 2 | Day 3 | Day 4 | |
|
||||
| EMEND* | 125 mg orally | 80 mg orally | 80 mg orally | none |
| Dexamethasone† | 12 mg orally | 8 mg orally | 8 mg orally | 8 mg orally |
| Ondansetron‡ | 32 mg I.V. | none | none | none |
In a clinical study with EMEND, the following regimen was used for the prevention of nausea and vomiting associated with moderately emetogenic cancer chemotherapy:
| Day 1 | Day 2 | Day 3 | |
|
|||
| EMEND* | 125 mg orally | 80 mg orally | 80 mg orally |
| Dexamethasone† | 12 mg orally | none | none |
| Ondansetron‡ | 2 x 8 mg orally | none | none |
2.2 Prevention of Postoperative Nausea and Vomiting (PONV)
The recommended oral dosage of EMEND is 40 mg within 3 hours prior to induction of anesthesia.
EMEND may be taken with or without food.
2.4 Patients with Renal Impairment
No dosage adjustment is necessary for patients with renal impairment or for patients with end stage renal disease (ESRD) undergoing hemodialysis.
2.5 Patients with Hepatic Impairment
No dosage adjustment is necessary for patients with mild to moderate hepatic impairment (Child-Pugh score 5 to 9). There are no clinical data in patients with severe hepatic impairment (Child-Pugh score >9).
2.6 Coadministration with Other Drugs
For additional information on dose adjustment for corticosteroids when coadministered with EMEND, see Drug Interactions (7.1).
Refer to the full prescribing information for coadministered antiemetic agents.
3 DOSAGE FORMS AND STRENGTHS
- Capsules EMEND 40 mg are opaque, hard, gelatin capsules, with white body and mustard yellow cap with “464” and “40 mg” printed radially in black ink on the body.
- Capsules EMEND 80 mg are white, opaque, hard, gelatin capsules, with “461” and “80 mg” printed radially in black ink on the body.
- Capsules EMEND 125 mg are opaque, hard, gelatin capsules, with white body and pink cap with “462” and “125 mg” printed radially in black ink on the body.
4 CONTRAINDICATIONS
EMEND is contraindicated in patients who are hypersensitive to any component of the product.
EMEND is a dose-dependent inhibitor of cytochrome P450 isoenzyme 3A4 (CYP3A4). EMEND should not be used concurrently with pimozide, terfenadine, astemizole, or cisapride. Inhibition of CYP3A4 by aprepitant could result in elevated plasma concentrations of these drugs, potentially causing serious or life-threatening reactions [see Drug Interactions (7.1)].
5 WARNINGS AND PRECAUTIONS
5.1 CYP3A4 Interactions
EMEND (aprepitant), a dose-dependent inhibitor of CYP3A4, should be used with caution in patients receiving concomitant medications that are primarily metabolized through CYP3A4. Moderate inhibition of CYP3A4 by aprepitant, 125 mg/80 mg regimen, could result in elevated plasma concentrations of these concomitant medications.
Weak inhibition of CYP3A4 by a single 40 mg dose of aprepitant is not expected to alter the plasma concentrations of concomitant medications that are primarily metabolized through CYP3A4 to a clinically significant degree.
When aprepitant is used concomitantly with another CYP3A4 inhibitor, aprepitant plasma concentrations could be elevated. When EMEND is used concomitantly with medications that induce CYP3A4 activity, aprepitant plasma concentrations could be reduced and this may result in decreased efficacy of EMEND [see Drug Interactions (7.1)].
Chemotherapy agents that are known to be metabolized by CYP3A4 include docetaxel, paclitaxel, etoposide, irinotecan, ifosfamide, imatinib, vinorelbine, vinblastine and vincristine. In clinical studies, EMEND (125 mg/80 mg regimen) was administered commonly with etoposide, vinorelbine, or paclitaxel. The doses of these agents were not adjusted to account for potential drug interactions.
In separate pharmacokinetic studies no clinically significant change in docetaxel or vinorelbine pharmacokinetics was observed when EMEND (125 mg/80 mg regimen) was co-administered.
Due to the small number of patients in clinical studies who received the CYP3A4 substrates vinblastine, vincristine, or ifosfamide, particular caution and careful monitoring are advised in patients receiving these agents or other chemotherapy agents metabolized primarily by CYP3A4 that were not studied [see Drug Interactions (7.1)].
5.2 Coadministration with Warfarin (a CYP2C9 substrate)
Coadministration of EMEND with warfarin may result in a clinically significant decrease in International Normalized Ratio (INR) of prothrombin time. In patients on chronic warfarin therapy, the INR should be closely monitored in the 2-week period, particularly at 7 to 10 days, following initiation of the 3-day regimen of EMEND with each chemotherapy cycle, or following administration of a single 40 mg dose of EMEND for the prevention of postoperative nausea and vomiting [see Drug Interactions (7.1)].
5.3 Coadministration with Hormonal Contraceptives
Upon coadministration with EMEND, the efficacy of hormonal contraceptives during and for 28 days following the last dose of EMEND may be reduced. Alternative or back-up methods of contraception should be used during treatment with EMEND and for 1 month following the last dose of EMEND [see Drug Interactions (7.1)].
5.4 Patients with Severe Hepatic Impairment
There are no clinical or pharmacokinetic data in patients with severe hepatic impairment (Child-Pugh score >9). Therefore, caution should be exercised when EMEND is administered in these patients [see Clinical Pharmacology (12.3) and Dosage and Administration (2.5)].
6 ADVERSE REACTIONS
The overall safety of aprepitant was evaluated in approximately 5300 individuals.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
6.1 Clinical Trials Experience
Chemotherapy Induced Nausea and Vomiting
Highly Emetogenic Chemotherapy
In 2 well-controlled clinical trials in patients receiving highly emetogenic cancer chemotherapy, 544 patients were treated with aprepitant during Cycle 1 of chemotherapy and 413 of these patients continued into the Multiple-Cycle extension for up to 6 cycles of chemotherapy. EMEND was given in combination with ondansetron and dexamethasone.
In Cycle 1, clinical adverse experiences were reported in approximately 69% of patients treated with the aprepitant regimen compared with approximately 68% of patients treated with standard therapy. Table 1 shows the percent of patients with clinical adverse experiences reported at an incidence ≥3%.
| Aprepitant Regimen (N = 544) | Standard Therapy (N = 550) |
|
| Body as a Whole/Site Unspecified | ||
|
Asthenia/Fatigue Dizziness Dehydration Abdominal Pain Fever Mucous Membrane Disorder |
17.8 6.6 5.9 4.6 2.9 2.6 |
11.8 4.4 5.1 3.3 3.5 3.1 |
| Digestive System | ||
|
Nausea Constipation Diarrhea Vomiting Heartburn Gastritis Epigastric Discomfort |
12.7 10.3 10.3 7.5 5.3 4.2 4.0 |
11.8 12.2 7.5 7.6 4.9 3.1 3.1 |
| Eyes, Ears, Nose, and Throat | ||
|
Tinnitus |
3.7 |
3.8 |
| Hemic and Lymphatic System | ||
|
Neutropenia |
3.1 |
2.9 |
| Metabolism and Nutrition | ||
|
Anorexia |
10.1 |
9.5 |
| Nervous System | ||
|
Headache Insomnia |
8.5 2.9 |
8.7 3.1 |
| Respiratory System | ||
|
Hiccups |
10.8 |
5.6 |
In addition, isolated cases of serious adverse experiences, regardless of causality, of bradycardia, disorientation, and perforating duodenal ulcer were reported in highly emetogenic CINV clinical studies.
Moderately Emetogenic Chemotherapy
During Cycle 1 of 2 moderately emetogenic chemotherapy studies, 868 patients were treated with the aprepitant regimen and 686 of these patients continued into extensions for up to 4 cycles of chemotherapy. In the combined analysis of Cycle 1 data for these 2 studies, adverse experiences were reported in approximately 69% of patients treated with the aprepitant regimen compared with approximately 72% of patients treated with standard therapy.
In the combined analysis of Cycle 1 data for these 2 studies, the adverse experience profile in both moderately emetogenic chemotherapy studies was generally comparable to the highly emetogenic chemotherapy studies. Table 2 shows the percent of patients with clinical adverse experiences reported at an incidence ≥3%.
| Aprepitant Regimen (N = 868) | Standard Therapy (N = 846) |
|
| Blood and Lymphatic System Disorders | ||
|
Neutropenia |
5.8 |
5.6 |
| Metabolism and Nutrition Disorders | ||
|
Anorexia |
6.2 |
7.2 |
| Psychiatric Disorders | ||
|
Insomnia |
2.6 |
3.7 |
| Nervous System Disorders | ||
|
Headache Dizziness |
13.2 2.8 |
14.3 3.4 |
| Gastrointestinal Disorders | ||
|
Constipation Diarrhea Dyspepsia Nausea Stomatitis |
10.3 7.6 5.8 5.8 3.1 |
15.5 8.7 3.8 5.1 2.7 |
| Skin and Subcutaneous Tissue Disorders | ||
|
Alopecia |
12.4 |
11.9 |
| General Disorders and General Administration Site Conditions | ||
|
Fatigue Asthenia |
15.4 4.7 |
15.6 4.6 |
In a combined analysis of these two studies, isolated cases of serious adverse experiences were similar in the two treatment groups.
Highly and Moderately Emetogenic Chemotherapy
The following additional clinical adverse experiences (incidence >0.5% and greater than standard therapy), regardless of causality, were reported in patients treated with aprepitant regimen in either HEC or MEC studies:
Infections and infestations: candidiasis, herpes simplex, lower respiratory infection, oral candidiasis, pharyngitis, septic shock, upper respiratory infection, urinary tract infection.
Neoplasms benign, malignant and unspecified (including cysts and polyps): malignant neoplasm, non-small cell lung carcinoma.
Blood and lymphatic system disorders: anemia, febrile neutropenia, thrombocytopenia.
Metabolism and nutrition disorders: appetite decreased, diabetes mellitus, hypokalemia.
Psychiatric disorders: anxiety disorder, confusion, depression.
Nervous system: peripheral neuropathy, sensory neuropathy, taste disturbance, tremor.
Eye disorders: conjunctivitis.
Cardiac disorders: myocardial infarction, palpitations, tachycardia.
Vascular disorders: deep venous thrombosis, flushing, hot flush, hypertension, hypotension.
Respiratory, thoracic and mediastinal disorders: cough, dyspnea, nasal secretion, pharyngolaryngeal pain, pneumonitis, pulmonary embolism, respiratory insufficiency, vocal disturbance.
Gastrointestinal disorders: abdominal pain upper, acid reflux, deglutition disorder, dry mouth, dysgeusia, dysphagia, eructation, flatulence, obstipation, salivation increased.
Skin and subcutaneous tissue disorders: acne, diaphoresis, pruritus, rash.
Musculoskeletal and connective tissue disorders: arthralgia, back pain, muscular weakness, musculoskeletal pain, myalgia.
Renal and urinary disorders: dysuria, renal insufficiency.
Reproductive system and breast disorders: pelvic pain.
General disorders and administrative site conditions: edema, malaise, pain, rigors.
Investigations: weight loss.
Stevens-Johnson syndrome was reported as a serious adverse experience in a patient receiving aprepitant with cancer chemotherapy in another CINV study.
Laboratory Adverse Experiences
Table 3 shows the percent of patients with laboratory adverse experiences reported at an incidence ≥3% in patients receiving highly emetogenic chemotherapy.
| Aprepitant Regimen (N = 544) | Standard Therapy (N = 550) |
|
|
Proteinuria ALT Increased Blood Urea Nitrogen Increased Serum Creatinine Increased AST Increased |
6.8 6.0 4.7 3.7 3.0 |
5.3 4.3 3.5 4.3 1.3 |
The following additional laboratory adverse experiences (incidence >0.5% and greater than standard therapy), regardless of causality, were reported in patients treated with aprepitant regimen: alkaline phosphatase increased, hyperglycemia, hyponatremia, leukocytes increased, erythrocyturia, leukocyturia.
The adverse experience profiles in the Multiple-Cycle extensions of HEC and MEC studies for up to 6 cycles of chemotherapy were generally similar to that observed in Cycle 1.
Postoperative Nausea and Vomiting
In well-controlled clinical studies in patients receiving general anesthesia, 564 patients were administered 40 mg aprepitant orally and 538 patients were administered 4 mg ondansetron IV.
Clinical adverse experiences were reported in approximately 60% of patients treated with 40 mg aprepitant compared with approximately 64% of patients treated with 4 mg ondansetron IV. Table 4 shows the percent of patients with clinical adverse experiences reported at an incidence ≥3% of the combined studies.
| Aprepitant 40 mg (N = 564) | Ondansetron (N = 538) |
|
| Infections and Infestations | ||
|
Urinary Tract Infection | 2.3 | 3.2 |
| Blood and Lymphatic System Disorders | ||
|
Anemia | 3.0 | 4.3 |
| Psychiatric Disorders | ||
|
Insomnia | 2.1 | 3.3 |
| Nervous System Disorders | ||
|
Headache | 5.0 | 6.5 |
| Cardiac Disorders | ||
|
Bradycardia | 4.4 | 3.9 |
| Vascular Disorders | ||
|
Hypotension Hypertension |
5.7 2.1 |
4.6 3.2 |
| Gastrointestinal Disorders | ||
|
Nausea Constipation Flatulence Vomiting |
8.5 8.5 4.1 2.5 |
8.6 7.6 5.8 3.9 |
| Skin and Subcutaneous Tissue Disorders | ||
|
Pruritus | 7.6 | 8.4 |
| General Disorders and General Administration Site Conditions | ||
|
Pyrexia | 5.9 | 10.6 |
The following additional clinical adverse experiences (incidence >0.5% and greater than ondansetron), regardless of causality, were reported in patients treated with aprepitant:
Infections and infestations: postoperative infection
Metabolism and nutrition disorders: hypokalemia, hypovolemia.
Nervous system disorders: dizziness, hypoesthesia, syncope.
Vascular disorders: hematoma
Respiratory, thoracic and mediastinal disorders: dyspnea, hypoxia, respiratory depression.
Gastrointestinal disorders: abdominal pain, abdominal pain upper, dry mouth, dyspepsia.
Skin and subcutaneous tissue disorders: urticaria
General disorders and administrative site conditions: hypothermia, pain.
Investigations: blood pressure decreased
Injury, poisoning and procedural complications: operative hemorrhage, wound dehiscence.
Other adverse experiences (incidence ≤0.5%) reported in patients treated with aprepitant 40 mg for postoperative nausea and vomiting included:
Nervous system disorders: dysarthria, sensory disturbance.
Eye disorders: miosis, visual acuity reduced.
Respiratory, thoracic and mediastinal disorders: wheezing
Gastrointestinal disorders: bowel sounds abnormal, stomach discomfort.
There were no serious adverse drug-related experiences reported in the postoperative nausea and vomiting clinical studies in patients taking 40 mg aprepitant.
Laboratory Adverse Experiences
One laboratory adverse experience, hemoglobin decreased (40 mg aprepitant 3.8%, ondansetron 4.2%), was reported at an incidence ≥3% in a patient receiving general anesthesia.
The following additional laboratory adverse experiences (incidence >0.5% and greater than ondansetron), regardless of causality, were reported in patients treated with aprepitant 40 mg: blood albumin decreased, blood bilirubin increased, blood glucose increased, blood potassium decreased, glucose urine present.
The adverse experience of ALT increased occurred with similar incidence in patients treated with aprepitant 40 mg (1.1%) as in patients treated with ondansetron 4 mg (1.0%).
Other Studies
In addition, two serious adverse experiences were reported in postoperative nausea and vomiting (PONV) clinical studies in patients taking a higher dose of aprepitant: one case of constipation, and one case of sub-ileus.
Angioedema and urticaria were reported as serious adverse experiences in a patient receiving aprepitant in a non-CINV/non-PONV study.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postmarketing use of aprepitant. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to the drug.
Skin and subcutaneous tissue disorders: pruritus, rash, urticaria, rarely Stevens-Johnson syndrome/toxic epidermal necrolysis.
Immune system disorders: hypersensitivity reactions including anaphylactic reactions.
7 DRUG INTERACTIONS
Aprepitant is a substrate, a weak-to-moderate (dose-dependent) inhibitor, and an inducer of CYP3A4. Aprepitant is also an inducer of CYP2C9.
7.1 Effect of Aprepitant on the Pharmacokinetics of Other Agents
CYP3A4 Substrates:
Weak inhibition of CYP3A4 by a single 40 mg dose of aprepitant is not expected to alter the plasma concentrations of concomitant medications that are primarily metabolized through CYP3A4 to a clinically significant degree. However, higher aprepitant doses or repeated dosing at any aprepitant dose may have a clinically significant effect.
As a moderate inhibitor of CYP3A4 at a dose of 125 mg/80 mg, aprepitant can increase plasma concentrations of concomitantly administered oral medications that are metabolized through CYP3A4 [see Contraindications (4)]. The use of fosaprepitant may increase CYP3A4 substrate plasma concentrations to a lesser degree than the use of oral aprepitant (125 mg).
5-HT3 antagonists: In clinical drug interaction studies, aprepitant did not have clinically important effects on the pharmacokinetics of ondansetron, granisetron, or hydrodolasetron (the active metabolite of dolasetron).
Corticosteroids:
Dexamethasone: EMEND, when given as a regimen of 125 mg with dexamethasone coadministered orally as 20 mg on Day 1, and EMEND when given as 80 mg/day with dexamethasone coadministered orally as 8 mg on Days 2 through 5, increased the AUC of dexamethasone, a CYP3A4 substrate, by 2.2-fold on Days 1 and 5. The oral dexamethasone doses should be reduced by approximately 50% when coadministered with EMEND (125 mg/80 mg regimen), to achieve exposures of dexamethasone similar to those obtained when it is given without EMEND. The daily dose of dexamethasone administered in clinical chemotherapy induced nausea and vomiting studies with EMEND reflects an approximate 50% reduction of the dose of dexamethasone [see Dosage and Administration (2.1)]. A single dose of EMEND (40 mg) when coadministered with a single oral dose of dexamethasone 20 mg, increased the AUC of dexamethasone by 1.45-fold. Therefore, no dose adjustment is recommended.
Methylprednisolone: EMEND, when given as a regimen of 125 mg on Day 1 and 80 mg/day on Days 2 and 3, increased the AUC of methylprednisolone, a CYP3A4 substrate, by 1.34-fold on Day 1 and by 2.5-fold on Day 3, when methylprednisolone was coadministered intravenously as 125 mg on Day 1 and orally as 40 mg on Days 2 and 3. The IV methylprednisolone dose should be reduced by approximately 25%, and the oral methylprednisolone dose should be reduced by approximately 50% when coadministered with EMEND (125 mg/80 mg regimen) to achieve exposures of methylprednisolone similar to those obtained when it is given without EMEND. Although the concomitant administration of methylprednisolone with the single 40 mg dose of aprepitant has not been studied, a single 40 mg dose of EMEND produces a weak inhibition of CYP3A4 (based on midazolam interaction study) and it is not expected to alter the plasma concentrations of methylprednisolone to a clinically significant degree. Therefore, no dose adjustment is recommended.
Chemotherapeutic agents: [see Warnings and Precautions (5.1)]
Docetaxel: In a pharmacokinetic study, EMEND (125 mg/80 mg regimen) did not influence the pharmacokinetics of docetaxel.
Vinorelbine: In a pharmacokinetic study, EMEND (125 mg/80 mg regimen) did not influence the pharmacokinetics of vinorelbine to a clinically significant degree.
CYP2C9 Substrates (Warfarin, Tolbutamide):
Aprepitant has been shown to induce the metabolism of S(-) warfarin and tolbutamide, which are metabolized through CYP2C9. Coadministration of EMEND with these drugs or other drugs that are known to be metabolized by CYP2C9, such as phenytoin, may result in lower plasma concentrations of these drugs.
Warfarin: A single 125-mg dose of EMEND was administered on Day 1 and 80 mg/day on Days 2 and 3 to healthy subjects who were stabilized on chronic warfarin therapy. Although there was no effect of EMEND on the plasma AUC of R(+) or S(-) warfarin determined on Day 3, there was a 34% decrease in S(-) warfarin (a CYP2C9 substrate) trough concentration accompanied by a 14% decrease in the prothrombin time (reported as International Normalized Ratio or INR) 5 days after completion of dosing with EMEND. In patients on chronic warfarin therapy, the prothrombin time (INR) should be closely monitored in the 2-week period, particularly at 7 to 10 days, following initiation of the 3-day regimen of EMEND with each chemotherapy cycle, or following administration of a single 40 mg dose of EMEND for the prevention of postoperative nausea and vomiting.
Tolbutamide: EMEND, when given as 125 mg on Day 1 and 80 mg/day on Days 2 and 3, decreased the AUC of tolbutamide (a CYP2C9 substrate) by 23% on Day 4, 28% on Day 8, and 15% on Day 15, when a single dose of tolbutamide 500 mg was administered orally prior to the administration of the 3-day regimen of EMEND and on Days 4, 8, and 15.
EMEND, when given as a 40-mg single oral dose on Day 1, decreased the AUC of tolbutamide (a CYP2C9 substrate) by 8% on Day 2, 16% on Day 4, 15% on Day 8, and 10% on Day 15, when a single dose of tolbutamide 500 mg was administered orally prior to the administration of EMEND 40 mg and on Days 2, 4, 8, and 15. This effect was not considered clinically important.
Oral contraceptives: Aprepitant, when given once daily for 14 days as a 100-mg capsule with an oral contraceptive containing 35 mcg of ethinyl estradiol and 1 mg of norethindrone, decreased the AUC of ethinyl estradiol by 43%, and decreased the AUC of norethindrone by 8%.
In another study, a daily dose of an oral contraceptive containing ethinyl estradiol and norethindrone was administered on Days 1 through 21, and EMEND was given as a 3-day regimen of 125 mg on Day 8 and 80 mg/day on Days 9 and 10 with ondansetron 32 mg IV on Day 8 and oral dexamethasone given as 12 mg on Day 8 and 8 mg/day on Days 9, 10, and 11. In the study, the AUC of ethinyl estradiol decreased by 19% on Day 10 and there was as much as a 64% decrease in ethinyl estradiol trough concentrations during Days 9 through 21. While there was no effect of EMEND on the AUC of norethindrone on Day 10, there was as much as a 60% decrease in norethindrone trough concentrations during Days 9 through 21.
In another study, a daily dose of an oral contraceptive containing ethinyl estradiol and norgestimate (which is converted to norelgestromin) was administered on Days 1 through 21, and EMEND 40 mg was given on Day 8. In the study, the AUC of ethinyl estradiol decreased by 4% and 29% on Day 8 and Day 12, respectively, while the AUC of norelgestromin increased by 18% on Day 8 and decreased by 10% on Day 12. In addition, the trough concentrations of ethinyl estradiol and norelgestromin on Days 8 through 21 were generally lower following coadministration of the oral contraceptive with EMEND 40 mg on Day 8 compared to the trough levels following administration of the oral contraceptive alone.
The coadministration of EMEND may reduce the efficacy of hormonal contraceptives (these can include birth control pills, skin patches, implants, and certain IUDs) during and for 28 days after administration of the last dose of EMEND. Alternative or back-up methods of contraception should be used during treatment with EMEND and for 1 month following the last dose of EMEND.
Midazolam: EMEND increased the AUC of midazolam, a sensitive CYP3A4 substrate, by 2.3-fold on Day 1 and 3.3-fold on Day 5, when a single oral dose of midazolam 2 mg was coadministered on Day 1 and Day 5 of a regimen of EMEND 125 mg on Day 1 and 80 mg/day on Days 2 through 5. The potential effects of increased plasma concentrations of midazolam or other benzodiazepines metabolized via CYP3A4 (alprazolam, triazolam) should be considered when coadministering these agents with EMEND (125 mg/80 mg). A single dose of EMEND (40 mg) increased the AUC of midazolam by 1.2-fold on Day 1, when a single oral dose of midazolam 2 mg was coadministered on Day 1 with EMEND 40 mg; this effect was not considered clinically important.
In another study with intravenous administration of midazolam, EMEND was given as 125 mg on Day 1 and 80 mg/day on Days 2 and 3, and midazolam 2 mg IV was given prior to the administration of the 3-day regimen of EMEND and on Days 4, 8, and 15. EMEND increased the AUC of midazolam by 25% on Day 4 and decreased the AUC of midazolam by 19% on Day 8 relative to the dosing of EMEND on Days 1 through 3. These effects were not considered clinically important. The AUC of midazolam on Day 15 was similar to that observed at baseline.
An additional study was completed with intravenous administration of midazolam and EMEND. Intravenous midazolam 2 mg was given 1 hour after oral administration of a single dose of EMEND 125 mg. The plasma AUC of midazolam was increased by 1.5-fold. Depending on clinical situations (e.g., elderly patients) and degree of monitoring available, dosage adjustment for intravenous midazolam may be necessary when it is coadministered with EMEND for the chemotherapy induced nausea and vomiting indication (125 mg on Day 1 followed by 80 mg on Days 2 and 3).
7.2 Effect of Other Agents on the Pharmacokinetics of Aprepitant
Aprepitant is a substrate for CYP3A4; therefore, coadministration of EMEND with drugs that inhibit CYP3A4 activity may result in increased plasma concentrations of aprepitant. Consequently, concomitant administration of EMEND with strong CYP3A4 inhibitors (e.g., ketoconazole, itraconazole, nefazodone, troleandomycin, clarithromycin, ritonavir, nelfinavir) should be approached with caution. Because moderate CYP3A4 inhibitors (e.g., diltiazem) result in a 2-fold increase in plasma concentrations of aprepitant, concomitant administration should also be approached with caution.
Aprepitant is a substrate for CYP3A4; therefore, coadministration of EMEND with drugs that strongly induce CYP3A4 activity (e.g., rifampin, carbamazepine, phenytoin) may result in reduced plasma concentrations of aprepitant that may result in decreased efficacy of EMEND.
Ketoconazole: When a single 125-mg dose of EMEND was administered on Day 5 of a 10-day regimen of 400 mg/day of ketoconazole, a strong CYP3A4 inhibitor, the AUC of aprepitant increased approximately 5-fold and the mean terminal half-life of aprepitant increased approximately 3-fold. Concomitant administration of EMEND with strong CYP3A4 inhibitors should be approached cautiously.
Rifampin: When a single 375-mg dose of EMEND was administered on Day 9 of a 14-day regimen of 600 mg/day of rifampin, a strong CYP3A4 inducer, the AUC of aprepitant decreased approximately 11-fold and the mean terminal half-life decreased approximately 3-fold.
Coadministration of EMEND with drugs that induce CYP3A4 activity may result in reduced plasma concentrations and decreased efficacy of EMEND.
7.3 Additional Interactions
EMEND is unlikely to interact with drugs that are substrates for the P-glycoprotein transporter, as demonstrated by the lack of interaction of EMEND with digoxin in a clinical drug interaction study.
Diltiazem: In patients with mild to moderate hypertension, administration of aprepitant once daily, as a tablet formulation comparable to 230 mg of the capsule formulation, with diltiazem 120 mg 3 times daily for 5 days, resulted in a 2-fold increase of aprepitant AUC and a simultaneous 1.7-fold increase of diltiazem AUC. These pharmacokinetic effects did not result in clinically meaningful changes in ECG, heart rate or blood pressure beyond those changes induced by diltiazem alone.
Paroxetine: Coadministration of once daily doses of aprepitant, as a tablet formulation comparable to 85 mg or 170 mg of the capsule formulation, with paroxetine 20 mg once daily, resulted in a decrease in AUC by approximately 25% and Cmax by approximately 20% of both aprepitant and paroxetine.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic effects
Pregnancy Category B: Reproduction studies have been performed in rats at oral doses up to 1000 mg/kg twice daily (plasma AUC0‑24hr of 31.3 mcg•hr/mL, about 1.6 times the human exposure at the recommended dose) and in rabbits at oral doses up to 25 mg/kg/day (plasma AUC0‑24hr of 26.9 mcg•hr/mL, about 1.4 times the human exposure at the recommended dose) and have revealed no evidence of impaired fertility or harm to the fetus due to aprepitant. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Aprepitant is excreted in the milk of rats. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for possible serious adverse reactions in nursing infants from aprepitant and because of the potential for tumorigenicity shown for aprepitant in rodent carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness of EMEND in pediatric patients have not been established.
8.5 Geriatric Use
In 2 well-controlled chemotherapy-induced nausea and vomiting clinical studies, of the total number of patients (N=544) treated with EMEND, 31% were 65 and over, while 5% were 75 and over. In well-controlled postoperative nausea and vomiting clinical studies, of the total number of patients (N=1120) treated with EMEND, 7% were 65 and over, while 2% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Greater sensitivity of some older individuals cannot be ruled out. Dosage adjustment in the elderly is not necessary.
10 OVERDOSAGE
No specific information is available on the treatment of overdosage.
Drowsiness and headache were reported in one patient who ingested 1440 mg of aprepitant.
In the event of overdose, EMEND should be discontinued and general supportive treatment and monitoring should be provided. Because of the antiemetic activity of aprepitant, drug-induced emesis may not be effective.
Aprepitant cannot be removed by hemodialysis.
11 DESCRIPTION
EMEND (aprepitant) is a substance P/neurokinin 1 (NK1) receptor antagonist, chemically described as 5-[[(2R,3S)-2-[(1R)-1-[3,5-bis(trifluoromethyl)phenyl]ethoxy]-3-(4-fluorophenyl)-4-morpholinyl]methyl]-1,2-dihydro-3H-1,2,4-triazol-3-one.
Its empirical formula is C23H21F7N4O3, and its structural formula is:
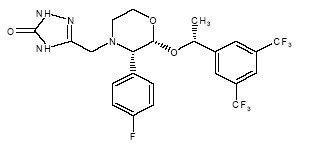
Aprepitant is a white to off-white crystalline solid, with a molecular weight of 534.43. It is practically insoluble in water. Aprepitant is sparingly soluble in ethanol and isopropyl acetate and slightly soluble in acetonitrile.
Each capsule of EMEND for oral administration contains either 40 mg, 80 mg, or 125 mg of aprepitant and the following inactive ingredients: sucrose, microcrystalline cellulose, hydroxypropyl cellulose and sodium lauryl sulfate. The capsule shell excipients are gelatin, titanium dioxide, and may contain sodium lauryl sulfate and silicon dioxide. The 40‑mg capsule shell also contains yellow ferric oxide, and the 125‑mg capsule also contains red ferric oxide and yellow ferric oxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Aprepitant is a selective high-affinity antagonist of human substance P/neurokinin 1 (NK1) receptors. Aprepitant has little or no affinity for serotonin (5-HT3), dopamine, and corticosteroid receptors, the targets of existing therapies for chemotherapy-induced nausea and vomiting (CINV) and postoperative nausea and vomiting (PONV).
Aprepitant has been shown in animal models to inhibit emesis induced by cytotoxic chemotherapeutic agents, such as cisplatin, via central actions. Animal and human Positron Emission Tomography (PET) studies with aprepitant have shown that it crosses the blood brain barrier and occupies brain NK1 receptors. Animal and human studies show that aprepitant augments the antiemetic activity of the 5-HT3-receptor antagonist ondansetron and the corticosteroid dexamethasone and inhibits both the acute and delayed phases of cisplatin-induced emesis.
12.2 Pharmacodynamics
NK1 Receptor Occupancy
In two single-blind, multiple-dose, randomized, and placebo control studies, healthy young men received oral aprepitant doses of 10 mg (N=2), 30 mg (N=3), 100 mg (N=3) or 300 mg (N=5) once daily for 14 days with 2 or 3 subjects on placebo. Both plasma aprepitant concentration and NK1 receptor occupancy in the corpus striatum by positron emission tomography were evaluated, at predose and 24 hours after the last dose. At aprepitant plasma concentrations of ~10 ng/mL and ~100 ng/mL, the NK1 receptor occupancies were ~50% and ~90%, respectively. The oral aprepitant regimen for CINV produces mean trough plasma aprepitant concentrations >500 ng/mL, which would be expected to, based on the fitted curve with the Hill equation, result in >95% brain NK1 receptor occupancy. However, the receptor occupancy for either CINV or PONV dosing regimen has not been determined. In addition, the relationship between NK1 receptor occupancy and the clinical efficacy of aprepitant has not been established.
Cardiac Electrophysiology
In a randomized, double-blind, positive-controlled, thorough QTc study, a single 200-mg dose of fosaprepitant had no effect on the QTc interval. QT prolongation with the oral dosing regimens for CINV and PONV are not expected.
12.3 Pharmacokinetics
Absorption
Following oral administration of a single 40 mg dose of EMEND in the fasted state, mean area under the plasma concentration-time curve (AUC0‑∞) was 7.8 mcg•hr/mL and mean peak plasma concentration (Cmax) was 0.7 mcg/mL, occurring at approximately 3 hours postdose (Tmax). The absolute bioavailability at the 40‑mg dose has not been determined.
Following oral administration of a single 125-mg dose of EMEND on Day 1 and 80 mg once daily on Days 2 and 3, the AUC0-24hr was approximately 19.6 mcg•hr/mL and 21.2 mcg•hr/mL on Day 1 and Day 3, respectively. The Cmax of 1.6 mcg/mL and 1.4 mcg/mL were reached in approximately 4 hours (Tmax) on Day 1 and Day 3, respectively. At the dose range of 80-125 mg, the mean absolute oral bioavailability of aprepitant is approximately 60 to 65%. Oral administration of the capsule with a standard high-fat breakfast had no clinically meaningful effect on the bioavailability of aprepitant.
The pharmacokinetics of aprepitant are non-linear across the clinical dose range. In healthy young adults, the increase in AUC0‑∞ was 26% greater than dose proportional between 80‑mg and 125‑mg single doses administered in the fed state.
Distribution
Aprepitant is greater than 95% bound to plasma proteins. The mean apparent volume of distribution at steady state (Vdss) is approximately 70 L in humans.
Aprepitant crosses the placenta in rats and rabbits and crosses the blood brain barrier in humans [see Clinical Pharmacology (12.1)].
Metabolism
Aprepitant undergoes extensive metabolism. In vitro studies using human liver microsomes indicate that aprepitant is metabolized primarily by CYP3A4 with minor metabolism by CYP1A2 and CYP2C19. Metabolism is largely via oxidation at the morpholine ring and its side chains. No metabolism by CYP2D6, CYP2C9, or CYP2E1 was detected. In healthy young adults, aprepitant accounts for approximately 24% of the radioactivity in plasma over 72 hours following a single oral 300-mg dose of [14C]-aprepitant, indicating a substantial presence of metabolites in the plasma. Seven metabolites of aprepitant, which are only weakly active, have been identified in human plasma.
Excretion
Following administration of a single IV 100-mg dose of [14C]-aprepitant prodrug to healthy subjects, 57% of the radioactivity was recovered in urine and 45% in feces. A study was not conducted with radiolabeled capsule formulation. The results after oral administration may differ.
Aprepitant is eliminated primarily by metabolism; aprepitant is not renally excreted. The apparent plasma clearance of aprepitant ranged from approximately 62 to 90 mL/min. The apparent terminal half-life ranged from approximately 9 to 13 hours.
Special Populations
Gender
Following oral administration of a single 125-mg dose of EMEND, no difference in AUC0‑24hr was observed between males and females. The Cmax for aprepitant is 16% higher in females as compared with males. The half-life of aprepitant is 25% lower in females as compared with males and Tmax occurs at approximately the same time. These differences are not considered clinically meaningful. No dosage adjustment for EMEND is necessary based on gender.
Geriatric
Following oral administration of a single 125-mg dose of EMEND on Day 1 and 80 mg once daily on Days 2 through 5, the AUC0‑24hr of aprepitant was 21% higher on Day 1 and 36% higher on Day 5 in elderly (≥65 years) relative to younger adults. The Cmax was 10% higher on Day 1 and 24% higher on Day 5 in elderly relative to younger adults. These differences are not considered clinically meaningful. No dosage adjustment for EMEND is necessary in elderly patients.
Pediatric
EMEND has not been evaluated in patients below 18 years of age.
Race
Following oral administration of a single 125-mg dose of EMEND, the AUC0-24hr is approximately 25% and 29% higher in Hispanics as compared with Whites and Blacks, respectively. The Cmax is 22% and 31% higher in Hispanics as compared with Whites and Blacks, respectively. These differences are not considered clinically meaningful. There was no difference in AUC0-24hr or Cmax between Whites and Blacks. No dosage adjustment for EMEND is necessary based on race.
Hepatic Insufficiency
Following administration of a single 125‑mg dose of EMEND on Day 1 and 80 mg once daily on Days 2 and 3 to patients with mild hepatic impairment (Child-Pugh score 5 to 6), the AUC0-24hr of aprepitant was 11% lower on Day 1 and 36% lower on Day 3, as compared with healthy subjects given the same regimen. In patients with moderate hepatic impairment (Child-Pugh score 7 to 9), the AUC0-24hr of aprepitant was 10% higher on Day 1 and 18% higher on Day 3, as compared with healthy subjects given the same regimen. These differences in AUC0‑24hr are not considered clinically meaningful; therefore, no dosage adjustment for EMEND is necessary in patients with mild to moderate hepatic impairment.
There are no clinical or pharmacokinetic data in patients with severe hepatic impairment (Child-Pugh score >9) [see Warnings and Precautions (5.4)].
Renal Insufficiency
A single 240-mg dose of EMEND was administered to patients with severe renal impairment (CrCl<30 mL/min) and to patients with end stage renal disease (ESRD) requiring hemodialysis.
In patients with severe renal impairment, the AUC0-∞ of total aprepitant (unbound and protein bound) decreased by 21% and Cmax decreased by 32%, relative to healthy subjects. In patients with ESRD undergoing hemodialysis, the AUC0‑∞ of total aprepitant decreased by 42% and Cmax decreased by 32%. Due to modest decreases in protein binding of aprepitant in patients with renal disease, the AUC of pharmacologically active unbound drug was not significantly affected in patients with renal impairment compared with healthy subjects. Hemodialysis conducted 4 or 48 hours after dosing had no significant effect on the pharmacokinetics of aprepitant; less than 0.2% of the dose was recovered in the dialysate.
No dosage adjustment for EMEND is necessary for patients with renal impairment or for patients with ESRD undergoing hemodialysis.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies were conducted in Sprague-Dawley rats and in CD-1 mice for 2 years. In the rat carcinogenicity studies, animals were treated with oral doses ranging from 0.05 to 1000 mg/kg twice daily. The highest dose produced a systemic exposure to aprepitant (plasma AUC0‑24hr) of 0.7 to 1.6 times the human exposure (AUC0‑24hr = 19.6 mcg•hr/mL) at the recommended dose of 125 mg/day. Treatment with aprepitant at doses of 5 to 1000 mg/kg twice daily caused an increase in the incidences of thyroid follicular cell adenomas and carcinomas in male rats. In female rats, it produced hepatocellular adenomas at 5 to 1000 mg/kg twice daily and hepatocellular carcinomas and thyroid follicular cell adenomas at 125 to 1000 mg/kg twice daily. In the mouse carcinogenicity studies, the animals were treated with oral doses ranging from 2.5 to 2000 mg/kg/day. The highest dose produced a systemic exposure of about 2.8 to 3.6 times the human exposure at the recommended dose. Treatment with aprepitant produced skin fibrosarcomas at 125 and 500 mg/kg/day doses in male mice.
Aprepitant was not genotoxic in the Ames test, the human lymphoblastoid cell (TK6) mutagenesis test, the rat hepatocyte DNA strand break test, the Chinese hamster ovary (CHO) cell chromosome aberration test and the mouse micronucleus test.
Aprepitant did not affect the fertility or general reproductive performance of male or female rats at doses up to the maximum feasible dose of 1000 mg/kg twice daily (providing exposure in male rats lower than the exposure at the recommended human dose and exposure in female rats at about 1.6 times the human exposure).
14 CLINICAL STUDIES
14.1 Prevention of Chemotherapy Induced Nausea and Vomiting (CINV)
Oral administration of EMEND in combination with ondansetron and dexamethasone (aprepitant regimen) has been shown to prevent acute and delayed nausea and vomiting associated with highly emetogenic chemotherapy including high-dose cisplatin, and nausea and vomiting associated with moderately emetogenic chemotherapy.
Highly Emetogenic Chemotherapy (HEC)
In 2 multicenter, randomized, parallel, double-blind, controlled clinical studies, the aprepitant regimen (see Table 6) was compared with standard therapy in patients receiving a chemotherapy regimen that included cisplatin >50 mg/m2 (mean cisplatin dose = 80.2 mg/m2). Of the 550 patients who were randomized to receive the aprepitant regimen, 42% were women, 58% men, 59% White, 3% Asian, 5% Black, 12% Hispanic American, and 21% Multi-Racial. The aprepitant-treated patients in these clinical studies ranged from 14 to 84 years of age, with a mean age of 56 years. 170 patients were 65 years or older, with 29 patients being 75 years or older.
Patients (N = 1105) were randomized to either the aprepitant regimen (N = 550) or standard therapy (N = 555). The treatment regimens are defined in Table 5.
| Aprepitant placebo and dexamethasone placebo were used to maintain blinding. | ||
| Treatment Regimen | Day 1 | Days 2 to 4 |
| Aprepitant | Aprepitant 125 mg PO Dexamethasone 12 mg PO Ondansetron 32 mg I.V. | Aprepitant 80 mg PO Daily (Days 2 and 3 only) Dexamethasone 8 mg PO Daily (morning) |
| Standard Therapy | Dexamethasone 20 mg PO Ondansetron 32 mg I.V. | Dexamethasone 8 mg PO Daily (morning) Dexamethasone 8 mg PO Daily (evening) |
During these studies 95% of the patients in the aprepitant group received a concomitant chemotherapeutic agent in addition to protocol-mandated cisplatin. The most common chemotherapeutic agents and the number of aprepitant patients exposed follows: etoposide (106), fluorouracil (100), gemcitabine (89), vinorelbine (82), paclitaxel (52), cyclophosphamide (50), doxorubicin (38), docetaxel (11).
The antiemetic activity of EMEND was evaluated during the acute phase (0 to 24 hours post-cisplatin treatment), the delayed phase (25 to 120 hours post-cisplatin treatment) and overall (0 to 120 hours post-cisplatin treatment) in Cycle 1. Efficacy was based on evaluation of the following endpoints:
Primary endpoint:
- complete response (defined as no emetic episodes and no use of rescue therapy)
Other prespecified endpoints:
- complete protection (defined as no emetic episodes, no use of rescue therapy, and a maximum nausea visual analogue scale [VAS] score <25 mm on a 0 to 100 mm scale)
- no emesis (defined as no emetic episodes regardless of use of rescue therapy)
- no nausea (maximum VAS <5 mm on a 0 to 100 mm scale)
- no significant nausea (maximum VAS <25 mm on a 0 to 100 mm scale)
A summary of the key study results from each individual study analysis is shown in Table 6 and in Table 7.
| ENDPOINTS | Aprepitant Regimen (N = 260)* % | Standard Therapy (N = 261)* % | p-Value |
| Visual analogue scale (VAS) score range: 0 mm = no nausea; 100 mm = nausea as bad as it could be. | |||
|
|||
| PRIMARY ENDPOINT | |||
| Complete Response | |||
| Overall† | 73 | 52 | <0.001 |
| OTHER PRESPECIFIED ENDPOINTS | |||
| Complete Response | |||
| Acute phase‡
Delayed phase§ | 89 75 | 78 56 | <0.001 <0.001 |
| Complete Protection | |||
| Overall Acute phase Delayed phase | 63 85 66 | 49 75 52 | 0.001 NS¶ <0.001 |
| No Emesis | |||
| Overall Acute phase Delayed phase | 78 90 81 | 55 79 59 | <0.001 0.001 <0.001 |
| No Nausea | |||
| Overall Delayed phase | 48 51 | 44 48 | NS#
NS# |
| No Significant Nausea | |||
| Overall Delayed phase | 73 75 | 66 69 | NS#
NS# |
| Visual analogue scale (VAS) score range: 0 mm = no nausea; 100 mm = nausea as bad as it could be. | |||
|
|||
| ENDPOINTS | Aprepitant Regimen (N = 261)* % | Standard Therapy (N = 263)* % | p-Value |
| PRIMARY ENDPOINT | |||
| Complete Response | |||
| Overall† | 63 | 43 | <0.001 |
| OTHER PRESPECIFIED ENDPOINTS | |||
| Complete Response | |||
| Acute phase‡
Delayed phase§ | 83 68 | 68 47 | <0.001 <0.001 |
| Complete Protection | |||
| Overall Acute phase Delayed phase | 56 80 61 | 41 65 44 | <0.001 <0.001 <0.001 |
| No Emesis | |||
| Overall Acute phase Delayed phase | 66 84 72 | 44 69 48 | <0.001 <0.001 <0.001 |
| No Nausea | |||
| Overall Delayed phase | 49 53 | 39 40 | NS¶
NS¶ |
| No Significant Nausea | |||
| Overall Delayed phase | 71 73 | 64 65 | NS#
NS# |
In both studies, a statistically significantly higher proportion of patients receiving the aprepitant regimen in Cycle 1 had a complete response in the overall phase (primary endpoint), compared with patients receiving standard therapy. A statistically significant difference in complete response in favor of the aprepitant regimen was also observed when the acute phase and the delayed phase were analyzed separately.
In both studies, the estimated time to first emesis after initiation of cisplatin treatment was longer with the aprepitant regimen, and the incidence of first emesis was reduced in the aprepitant regimen group compared with standard therapy group as depicted in the Kaplan-Meier curves in Figure 1.
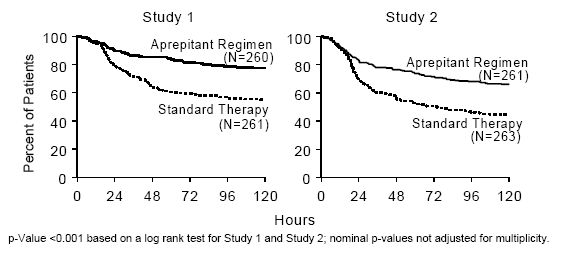
Figure 1: Percent of Patients Receiving Highly Emetogenic Chemotherapy Who Remain Emesis Free Over Time — Cycle 1
Patient-Reported Outcomes: The impact of nausea and vomiting on patients’ daily lives was assessed in Cycle 1 of both Phase III studies using the Functional Living Index–Emesis (FLIE), a validated nausea- and vomiting-specific patient-reported outcome measure. Minimal or no impact of nausea and vomiting on patients’ daily lives is defined as a FLIE total score >108. In each of the 2 studies, a higher proportion of patients receiving the aprepitant regimen reported minimal or no impact of nausea and vomiting on daily life (Study 1: 74% versus 64%; Study 2: 75% versus 64%).
Multiple-Cycle Extension: In the same 2 clinical studies, patients continued into the Multiple-Cycle extension for up to 5 additional cycles of chemotherapy. The proportion of patients with no emesis and no significant nausea by treatment group at each cycle is depicted in Figure 2. Antiemetic effectiveness for the patients receiving the aprepitant regimen is maintained throughout repeat cycles for those patients continuing in each of the multiple cycles.
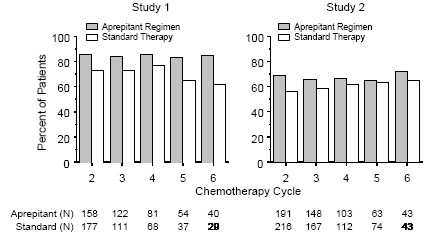
Figure 2: Proportion of Patients Receiving Highly Emetogenic Chemotherapy with No Emesis and No Significant Nausea by Treatment Group and Cycle
Moderately Emetogenic Chemotherapy (MEC)
In a multicenter, randomized, double-blind, parallel-group, clinical study in breast cancer patients, the aprepitant regimen (see Table 9) was compared with a standard of care therapy in patients receiving a moderately emetogenic chemotherapy regimen that included cyclophosphamide 750-1500 mg/m2; or cyclophosphamide 500-1500 mg/m2 and doxorubicin (≤60 mg/m2) or epirubicin (≤100 mg/m2).
In this study, the most common combinations were cyclophosphamide + doxorubicin (60.6%); and cyclophosphamide + epirubicin + fluorouracil (21.6%).
Of the 438 patients who were randomized to receive the aprepitant regimen, 99.5% were women. Of these, approximately 80% were White, 8% Black, 8% Asian, 4% Hispanic, and <1% Other. The aprepitant-treated patients in this clinical study ranged from 25 to 78 years of age, with a mean age of 53 years; 70 patients were 65 years or older, with 12 patients being over 74 years.
Patients (N = 866) were randomized to either the aprepitant regimen (N = 438) or standard therapy (N = 428). The treatment regimens are defined in Table 8.
| Aprepitant placebo and dexamethasone placebo were used to maintain blinding. | ||
| Treatment Regimen | Day 1 | Days 2 to 3 |
| Aprepitant | Aprepitant 125 mg PO*
Dexamethasone 12 mg PO† Ondansetron 8 mg PO x 2 doses‡ | Aprepitant 80 mg PO Daily |
| Standard Therapy | Dexamethasone 20 mg PO Ondansetron 8 mg PO x 2 doses | Ondansetron 8 mg PO Daily (every 12 hours) |
The antiemetic activity of EMEND was evaluated based on the following endpoints:
Primary endpoint:
Complete response (defined as no emetic episodes and no use of rescue therapy) in the overall phase (0 to 120 hours post-chemotherapy)
Other prespecified endpoints:
- no emesis (defined as no emetic episodes regardless of use of rescue therapy)
- no nausea (maximum VAS <5 mm on a 0 to 100 mm scale)
- no significant nausea (maximum VAS <25 mm on a 0 to 100 mm scale)
- complete protection (defined as no emetic episodes, no use of rescue therapy, and a maximum nausea visual analogue scale [VAS] score <25 mm on a 0 to 100 mm scale)
- complete response during the acute and delayed phases.
A summary of the key results from this study is shown in Table 9.
| ENDPOINTS | Aprepitant Regimen (N = 433)* % | Standard Therapy (N = 424)* % | p-Value |
| PRIMARY ENDPOINT† | |||
| Complete Response | 51 | 42 | 0.015 |
| OTHER PRESPECIFIED ENDPOINTS† | |||
| No Emesis | 76 | 59 | NS‡ |
| No Nausea | 33 | 33 | NS |
| No Significant Nausea | 61 | 56 | NS |
| No Rescue Therapy | 59 | 56 | NS |
| Complete Protection | 43 | 37 | NS |
In this study, a statistically significantly (p=0.015) higher proportion of patients receiving the aprepitant regimen (51%) in Cycle 1 had a complete response (primary endpoint) during the overall phase compared with patients receiving standard therapy (42%). The difference between treatment groups was primarily driven by the “No Emesis Endpoint”, a principal component of this composite primary endpoint. In addition, a higher proportion of patients receiving the aprepitant regimen in Cycle 1 had a complete response during the acute (0-24 hours) and delayed (25-120 hours) phases compared with patients receiving standard therapy; however, the treatment group differences failed to reach statistical significance, after multiplicity adjustments.
Patient-Reported Outcomes: In a phase III study in patients receiving moderately emetogenic chemotherapy, the impact of nausea and vomiting on patients’ daily lives was assessed in Cycle 1 using the FLIE. A higher proportion of patients receiving the aprepitant regimen reported minimal or no impact on daily life (64% versus 56%). This difference between treatment groups was primarily driven by the “No Vomiting Domain” of this composite endpoint.
Multiple-Cycle Extension: Patients receiving moderately emetogenic chemotherapy were permitted to continue into the Multiple-Cycle extension of the study for up to 3 additional cycles of chemotherapy. Antiemetic effect for patients receiving the aprepitant regimen is maintained during all cycles.
Postmarketing Trial: In a postmarketing, multicenter, randomized, double-blind, parallel-group, clinical study in 848 cancer patients, the aprepitant regimen (N = 430) was compared with a standard of care therapy (N = 418) in patients receiving a moderately emetogenic chemotherapy regimen that included any IV dose of oxaliplatin, carboplatin, epirubicin, idarubicin, ifosfamide, irinotecan, daunorubicin, doxorubicin; cyclophosphamide IV (<1500 mg/m2); or cytarabine IV (>1 g/m2).
Of the 430 patients who were randomized to receive the aprepitant regimen, approximately 76% were women and 24% were men. The distribution by race was 67% White, 6% Black or African American, 11% Asian, and 12% multiracial. Classified by ethnicity, 36% were Hispanic and 64% were non-Hispanic. The aprepitant-treated patients in this clinical study ranged from 22 to 85 years of age, with a mean age of 57 years; approximately 59% of the patients were 55 years or older with 32 patients being over 74 years. Patients receiving the aprepitant regimen were receiving chemotherapy for a variety of tumor types including 50% with breast cancer, 21% with gastrointestinal cancers including colorectal cancer, 13% with lung cancer and 6% with gynecological cancers.
The antiemetic activity of EMEND was evaluated based on no vomiting (with or without rescue therapy) in the overall period (0 to 120 hours post-chemotherapy) and complete response (defined as no vomiting and no use of rescue therapy) in the overall period.
A summary of the key results from this study is shown in Table 10.
|
|||
|
ENDPOINTS |
Aprepitant Regimen (N = 430)* % |
Standard Therapy (N = 418)* % |
p-Value |
| No Vomiting Overall | 76 | 62 | <0.0001 |
| Complete Response Overall | 69 | 56 | 0.0003 |
In this study, a statistically significantly higher proportion of patients receiving the aprepitant regimen (76%) in Cycle 1 had no vomiting during the overall phase compared with patients receiving standard therapy (62%). In addition, a higher proportion of patients receiving the aprepitant regimen (69%) in Cycle 1 had a complete response in the overall phase (0-120 hours) compared with patients receiving standard therapy (56%). In the acute phase (0 to 24 hours following initiation of chemotherapy), a higher proportion of patients receiving aprepitant compared to patients receiving standard therapy were observed to have no vomiting (92% and 84%, respectively) and complete response (89% and 80%, respectively). In the delayed phase (25 to 120 hours following initiation of chemotherapy), a higher proportion of patients receiving aprepitant compared to patients receiving standard therapy were observed to have no vomiting (78% and 67%, respectively) and complete response (71% and 61%, respectively).
In a subgroup analysis by tumor type, a numerically higher proportion of patients receiving aprepitant were observed to have no vomiting and complete response compared to patients receiving standard therapy. For gender, the difference in complete response rates between the aprepitant and standard regimen groups was 14% in females (64.5% and 50.3%, respectively) and 4% in males (82.2% and 78.2%, respectively) during the overall phase. A similar difference for gender was observed for the no vomiting endpoint.
14.2 Prevention of Postoperative Nausea and Vomiting (PONV)
In two multicenter, randomized, double-blind, active comparator-controlled, parallel-group clinical studies (PONV Studies 1 and 2), aprepitant was compared with ondansetron for the prevention of postoperative nausea and vomiting in 1658 patients undergoing open abdominal surgery. Patients were randomized to receive 40 mg aprepitant, 125 mg aprepitant, or 4 mg ondansetron. Aprepitant was given orally with 50 mL of water 1 to 3 hours before anesthesia. Ondansetron was given intravenously immediately before induction of anesthesia. A comparison between the 125 mg dose and the 40 mg dose did not demonstrate any additional clinical benefit. The remainder of this section will focus on the results in the 40 mg aprepitant dose recommended for PONV.
Of the 564 patients who received 40 mg aprepitant, 92% were women and 8% were men; of these, 58% were White, 13% Hispanic American, 7% Multi-Racial, 14% Black, 6% Asian, and 2% Other. The age of patients treated with 40 mg aprepitant ranged from 19 to 84 years, with a mean age of 46.1 years. 46 patients were 65 years or older, with 13 patients being 75 years or older.
The antiemetic activity of EMEND was evaluated during the 0 to 48 hour period following the end of surgery. The two pivotal studies were of similar design; however, they differed in terms of study hypothesis, efficacy analyses and geographic location. PONV Study 1 was a multinational study including the U.S., whereas, PONV Study 2 was conducted entirely in the U.S.
Efficacy measures in PONV Study 1 included:
- no emesis (defined as no emetic episodes regardless of use of rescue therapy) in the 0 to 24 hours following the end of surgery (primary)
- complete response (defined as no emetic episodes and no use of rescue therapy) in the 0 to 24 hours following the end of surgery (primary)
- no emesis (defined as no emetic episodes regardless of use of rescue therapy) in the 0 to 48 hours following the end of surgery (secondary)
- time to first use of rescue medication in the 0 to 24 hours following the end of surgery (exploratory)
- time to first emesis in the 0 to 48 hours following the end of surgery (exploratory).
A closed testing procedure was applied to control the type I error for the primary endpoints.
The results of the primary and secondary endpoints for 40 mg aprepitant and 4 mg ondansetron are described in Table 11:
| n/m = Number of responders/number of patients in analysis. Δ Difference (%): Aprepitant 40 mg minus Ondansetron. |
||||
|
||||
| Treatment | n/m (%) | Aprepitant
vs Ondansetron |
||
| Δ | Odds
ratio* | Analysis | ||
| Primary Endpoints | ||||
| No Vomiting 0 to 24 hours (Superiority) (no emetic episodes) |
||||
| Aprepitant 40 mg | 246/293 (84.0) | 12.6% | 2.1 | P<0.001† |
| Ondansetron | 200/280 (71.4) | |||
| Complete Response (Non-inferiority: If LB‡ >0.65) (no emesis and no rescue therapy, 0 to 24 hours) |
||||
| Aprepitant 40 mg | 187/293 (63.8) | 8.8% | 1.4 | LB=1.02 |
| Ondansetron | 154/280 (55.0) | |||
| Complete Response (Superiority: If LB >1.0) (no emesis and no rescue therapy, 0 to 24 hours) |
||||
| Aprepitant 40 mg | 187/293 (63.8) | 8.8% | 1.4 | LB=1.02§ |
| Ondansetron | 154/280 (55.0) | |||
| Secondary Endpoint | ||||
| No Vomiting 0 to 48 (Superiority) (no emetic episodes) |
||||
| Aprepitant 40 mg | 238/292 (81.5) | 15.2% | 2.3 | P<0.001† |
| Ondansetron | 185/279 (66.3) | |||
The use of aprepitant did not affect the time to first use of rescue medication when compared to ondansetron. However, compared to the ondansetron group, use of aprepitant delayed the time to first vomiting, as depicted in Figure 3.
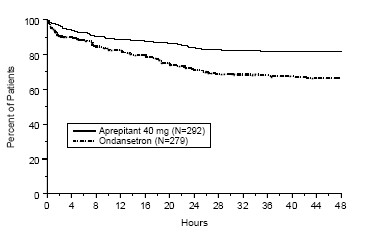
Figure 3: Percent of Patients Who Remain Emesis Free During the 48 Hours Following End of Surgery
Efficacy measures in PONV Study 2 included:
- complete response (defined as no emetic episodes and no use of rescue therapy) in the 0 to 24 hours following the end of surgery (primary)
- no emesis (defined as no emetic episodes regardless of use of rescue therapy) in the 0 to 24 hours following the end of surgery (secondary)
- no use of rescue therapy in the 0 to 24 hours following the end of surgery (secondary)
- no emesis (defined as no emetic episodes regardless of use of rescue therapy) in the 0 to 48 hours following the end of surgery (secondary).
PONV Study 2 failed to satisfy its primary hypothesis that aprepitant is superior to ondansetron in the prevention of PONV as measured by the proportion of patients with complete response in the 24 hours following end of surgery.
The study demonstrated that both dose levels of aprepitant had a clinically meaningful effect with respect to the secondary endpoint “no vomiting” during the first 24 hours after surgery and showed that the use of 40 mg aprepitant was associated with a 16% improvement over ondansetron for the no vomiting endpoint.
| n/m = Number of responders/number of patients in analysis. Δ Difference (%): Aprepitant 40 mg minus Ondansetron. |
||||
| Treatment | n/m(%) | Aprepitant vs Ondansetron |
||
| Δ | Odds ratio* | p-Value | ||
| Primary Endpoint | ||||
| Complete Response
(no emesis and no rescue therapy, 0 to 24 hours) |
||||
| Aprepitant 40 mg | 111/248 (44.8) | 2.5% | 1.1 | 0.61 |
| Ondansetron | 104/246 (42.3) | |||
| Secondary Endpoints | ||||
| No Vomiting
(no emetic episodes, 0 to 24 hours) |
||||
| Aprepitant 40 mg | 223/248 (89.9) | 16.3% | 3.2 | <0.001† |
| Ondansetron | 181/246 (73.6) | |||
| No Use of Rescue Medication
(for established emesis or nausea, 0 to 24 hours) |
||||
| Aprepitant 40 mg | 112/248 (45.2) | -0.7% | 1.0 | 0.83 |
| Ondansetron | 113/246 (45.9) | |||
| No Vomiting 0 to 48 (Superiority) (no emetic episodes, 0 to 48 hours) |
||||
| Aprepitant 40 mg | 209/247 (84.6) | 17.7% | 2.7 | <0.001† |
| Ondansetron | 164/245 (66.9) | |||
16 HOW SUPPLIED/STORAGE AND HANDLING
No. 6741 — 40 mg capsules: Opaque, hard gelatin capsule with white body and mustard yellow cap with “464” and “40 mg” printed radially in black ink on the body. They are supplied as follows:
NDC 42254-160-01 unit-of-use package of 1
Storage
Store at 20-25°C (68-77°F) [see USP Controlled Room Temperature].
Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USA
9988902
U.S. Patent Nos.: 5,145,684; 5,719,147; 6,048,859; 6,096,742; 6,235,735
17 PATIENT COUNSELING INFORMATION
[See FDA-Approved Patient Labeling.]
17.1 Instructions
Physicians should instruct their patients to read the patient package insert before starting therapy with EMEND and to reread it each time the prescription is renewed.
Patients should be instructed to take EMEND only as prescribed. For the prevention of chemotherapy induced nausea and vomiting (CINV), patients should be advised to take their first dose (125 mg) of EMEND 1 hour prior to chemotherapy treatment. For the prevention of postoperative nausea and vomiting (PONV), patients should receive their medication (40 mg capsule of EMEND) within 3 hours prior to induction of anesthesia.
Allergic reactions, which may be serious, and may include hives, rash and itching and cause difficulty in breathing or swallowing, have been reported in general use with EMEND. Physicians should instruct their patients to stop taking EMEND and call their doctor right away if they experience an allergic reaction. In addition, severe skin reactions may occur rarely.
EMEND may interact with some drugs including chemotherapy; therefore, patients should be advised to report to their doctor the use of any other prescription, non-prescription medication or herbal products.
Patients on chronic warfarin therapy should be instructed to have their clotting status closely monitored in the 2-week period, particularly at 7 to 10 days, following initiation of the 3-day regimen of EMEND 125 mg/80 mg with each chemotherapy cycle, or following administration of a single 40 mg dose of EMEND for the prevention of postoperative nausea and vomiting.
Administration of EMEND may reduce the efficacy of hormonal contraceptives. Patients should be advised to use alternative or back-up methods of contraception during treatment with EMEND and for 1 month following the last dose of EMEND.
FDA-Approved Patient Labeling
Patient Information
EMEND® (EE mend)
(aprepitant)
Capsules
Read the Patient Information that comes with EMEND before you start taking it and each time you refill your prescription. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or treatment.
What is EMEND?
EMEND is a prescription medicine used in adults to prevent nausea and vomiting:
- caused by certain anti-cancer (chemotherapy) medicines. When used for this purpose, EMEND is always used with other medicines.
- after surgery.
EMEND is not used to treat nausea and vomiting that you already have.
EMEND should not be used continuously for a long time (chronic use).
It is not known if EMEND is safe and effective in children.
Who should not take EMEND?
Do not take EMEND if you:
- are taking any of the following medicines:
- ORAP® (pimozide)
- SELDANE® (terfenadine)
- HISMANAL® (astemizole)
- PROPULSID® (cisapride)
Taking EMEND with any of these medicines could cause serious or life-threatening problems.
- are allergic to any of the ingredients in EMEND. See the end of this leaflet for a list of all the ingredients in EMEND.
What should I tell my doctor before and during treatment with EMEND?
Before you take EMEND, tell your doctor if you:
- have liver problems
- are pregnant or plan to become pregnant. It is not known if EMEND can harm your unborn baby.
Women who use birth control medicines containing hormones to prevent pregnancy (birth control pills, skin patches, implants, and certain IUDs) should also use a back-up method of birth control during treatment with EMEND and for up to 1 month after using EMEND to prevent pregnancy.
- are breast-feeding. It is not known if EMEND passes into your milk and if it can harm your baby.
Tell your doctor about all the medicines you are taking or plan to take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
EMEND may cause serious life-threatening reactions if used with certain medicines. See the section “Who should not take EMEND?"
EMEND may affect how other medicines work, and other medicines may affect how EMEND works. Ask your doctor or pharmacist before you take any new medicine. They can tell you if it is safe to take the medicine with EMEND.
Know the medicines you take. Keep a list of them to show your doctor or pharmacist when you get a new medicine.
How should I take EMEND?
- Take EMEND exactly as prescribed.
- If you take too much EMEND, call your doctor, local emergency department or poison control center right away.
- If you are receiving cancer chemotherapy, EMEND is taken as 3 doses over 3 days - starting on the day you have chemotherapy, and the two days after chemotherapy. There are two ways that your doctor may prescribe EMEND for you:
- Capsules of EMEND by mouth for all 3 doses:
- You should get a package that has three capsules of EMEND.
- Day 1 (Day of chemotherapy): Take one 125-mg capsule of EMEND (white and pink) by mouth 1 hour before you start your chemotherapy treatment.
- Day 2 and Day 3 (the two days after chemotherapy): Take one 80-mg capsule of EMEND (white) by mouth, each morning for the 2 days after your chemotherapy treatment.
Or
- Intravenous (IV) injection into a vein the first day, then capsules by mouth on the two days after chemotherapy:
- Day 1 (Day of chemotherapy): EMEND will be given to you by intravenous (IV) injection in your vein 30 minutes before you start your chemotherapy treatment.
- You should get a package that has two capsules of EMEND.
- Day 2 and Day 3 (the two days after chemotherapy): Take one 80-mg capsule of EMEND (white) by mouth, each morning for the 2 days after your chemotherapy treatment.
- If you are receiving chemotherapy, EMEND may be taken with or without food.
- If you are having surgery:
- Your doctor will prescribe a 40-mg capsule of EMEND for you before surgery. You take EMEND within three hours before surgery.
- Follow your doctor’s instructions about restrictions on eating and drinking before surgery.
- If you take the blood thinner medicine warfarin sodium (COUMADIN®, JANTOVEN®), your doctor may do blood tests after you take EMEND to check your blood clotting.
What are the possible side effects of EMEND?
EMEND may cause serious side effects, including:
-
Serious allergic reactions. Allergic reactions can happen with EMEND and may be serious. Stop taking EMEND and call your doctor right away if you have any of these signs or symptoms of an allergic reaction:
- hives
- rash
- itching
- trouble breathing or swallowing.
- Severe skin reactions may occur rarely.
In people taking EMEND to prevent nausea and vomiting caused by chemotherapy, the most common side effects of EMEND include:
- tiredness
- nausea
- hiccups
- constipation
- diarrhea
- loss of appetite
- headache
- hair loss
In people taking EMEND to prevent nausea and vomiting after surgery, the most common side effects are:
- constipation
- nausea
- itch
- fever
- low blood pressure
- headache
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of EMEND. For more information ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store EMEND?
- Store EMEND at room temperature, between 68°F and 77°F (20°C and 25°C).
- Keep EMEND and all medicines out of the reach of children.
General information about EMEND
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use EMEND for a condition for which it was not prescribed. Do not give EMEND to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about EMEND. If you would like to know more information, talk with your doctor. You can ask your doctor or pharmacist for information about EMEND that is written for health professionals. For more information about EMEND call 1-800-622-4477 or go to www.emend.com.
What are the ingredients in EMEND?
Active ingredient: aprepitant
Inactive ingredients: sucrose, microcrystalline cellulose, hydroxypropyl cellulose and sodium lauryl sulfate. The capsule shell excipients are gelatin, titanium dioxide, and may contain sodium lauryl sulfate and silicon dioxide. The 125-mg capsule shell also contains red ferric oxide and yellow ferric oxide. The 40-mg capsule shell also contains yellow ferric oxide.
U.S. Patent Nos.: 5,145,684; 5,719,147; 6,048,859; 6,096,742; 6,235,735
The brands listed in the above sections “Who should not take EMEND?” and “What should I tell my doctor before and during treatment with EMEND?” are the registered trademarks of their respective owners and are not trademarks of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
EMEND® is a registered trademark of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
Copyright © 2003, 2005, 2006 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved
Issued March 2011
Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
Whitehouse Station, NJ 08889, USA
9988902
Repackaged by:
Rebel Distributors Corp
Thousand Oaks, CA 91320