INDICATIONS & USAGE SECTION
- 1.1 Short-Term Treatment of Active Duodenal Ulcer
Lansoprazole delayed-release capsules are indicated for short-term treatment (for 4 weeks) for healing and symptom relief of active duodenal ulcer. [See Clinical Studies (14)]
1.2 H. pylori Eradication to Reduce the Risk of Duodenal Ulcer RecurrenceTriple Therapy: Lansoprazole delayed-release capsules /amoxicillin /clarithromycin
Lansoprazole delayed-release capsules in combination with amoxicillin plus clarithromycin as triple therapy is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or one-year history of a duodenal ulcer) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence. [See Clinical Studies (14)]
Please refer to the full prescribing information for amoxicillin and clarithromycin.
Dual Therapy: Lansoprazole delayed-release capsules /amoxicillin
Dual Therapy: Lansoprazole delayed-release capsules /amoxicillinLansoprazole delayed-release capsules in combination with amoxicillin as dual therapy is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or one-year history of a duodenal ulcer) who are either allergic or intolerant to clarithromycin or in whom resistance to clarithromycin is known or suspected (see the clarithromycin package insert, MICROBIOLOGY section). Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence. [See Clinical Studies (14)]
Please refer to the full prescribing information for amoxicillin.
1.3 Maintenance of Healed Duodenal UlcersLansoprazole delayed-release capsules are indicated to maintain healing of duodenal ulcers. Controlled studies do not extend beyond 12 months. [See Clinical Studies (14)]
1.4 Short-Term Treatment of Active Benign Gastric UlcerLansoprazole delayed-release capsules are indicated for short-term treatment (up to 8 weeks) for healing and symptom relief of active benign gastric ulcer. [See Clinical Studies (14)]
1.5 Healing of NSAID-Associated Gastric UlcerLansoprazole delayed-release capsules are indicated for the treatment of NSAID-associated gastric ulcer in patients who continue NSAID use. Controlled studies did not extend beyond 8 weeks. [See Clinical Studies (14)]
1.6 Risk Reduction of NSAID-Associated Gastric UlcerLansoprazole delayed-release capsules are indicated for reducing the risk of NSAID-associated gastric ulcers in patients with a history of a documented gastric ulcer who require the use of an NSAID. Controlled studies did not extend beyond 12 weeks. [See Clinical Studies (14)]
1.7 Gastroesophageal Reflux Disease (GERD)Short-Term Treatment of Symptomatic GERD
Lansoprazole delayed-release capsules is indicated for the treatment of heartburn and other symptoms associated with GERD for upto 8 weeks. [See Clinical Studies (14)]
Short-Term Treatment of Erosive Esophagitis
Lansoprazole delayed-release capsules is indicated for short-term treatment (up to 8 weeks) for healing and symptom relief of all grades of erosive esophagitis.
For patients who do not heal with lansoprazole delayed-release capsules for 8 weeks (5 to10%), it may be helpful to give an additional 8 weeks of treatment. If there is a recurrence of erosive esophagitis an additional 8-week course of lansoprazole delayed-release capsules may be considered. [See Clinical Studies (14)]
1.8 Maintenance of Healing of Erosive Esophagitis (EE)Lansoprazole delayed-release capsules are indicated to maintain healing of erosive esophagitis. Controlled studies did not extend beyond 12 months. [See Clinical Studies (14)]
1.9 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome (ZES)Lansoprazole delayed-release capsules are indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison syndrome. [See Clinical Studies (14)]
DOSAGE & ADMINISTRATION SECTION
-
Lansoprazole is available as a capsule, and is available in 15 mg and 30 mg strengths. Directions for use specific to the route and available methods of administration is presented below. Lansoprazole delayed-release capsules should be taken before eating. Lansoprazole delayed-release capsule products SHOULD NOT BE CRUSHED OR CHEWED. In the clinical trials, antacids were used concomitantly with lansoprazole delayed-release capsules.
2.1 Recommended DoseIndication Recommended Dose Frequency *† Duodenal Ulcers Short-Term Treatment 15 mg Once daily for 4 weeks Maintenance of Healed 15 mg Once daily H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence* Triple Therapy: Lansoprazole delayed-release capsules 30 mg Twice daily (q12h) for 10 or 14 days Amoxicillin 1 gram Twice daily (q12h) for 10 or 14 days Clarithromycin 500 mg Twice daily (q12h) for 10 or 14 days Dual Therapy: Lansoprazole delayed-release capsules 30 mg Three times daily (q8h) for 14 days Amoxicillin 1 gram Three times daily (q8h) for 14 days Benign Gastric Ulcer Short-Term Treatment 30 mg Once daily for up to 8 weeks NSAID-associated Gastric Ulcer Healing 30 mg Once daily for 8 weeks† * Risk Reduction 15 mg Once daily for up to 12 weeks† Gastroesophageal Reflux Disease (GERD) Short-Term Treatment of Symptomatic GERD 15 mg Once daily for up to 8 weeks Short -Term Treatment of Erosive Esophagitis 30 mg Once daily for up to 8 weeks‡ Pediatric (1 to 11 years of age)
Short-Term Treatment of Symptomatic GERD and Short-Term Treatment of Erosive Esophagitis≤ 30 kg 15 mg Once daily for up to 12 weeks †§ > 30 kg 30 mg Once daily for up to 12 weeks§ (12 to 17 years of age)
Short-Term Treatment of Symptomatic GERDNonerosive GERD 15 mg Once daily for up to 8 weeks Erosive Esophagitis 30 mg Once daily for up to 8 weeks Maintenance of Healing of Erosive Esophagitis 15 mg Once daily# Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome 60 mg Once daily¶ * Please refer to amoxicillin and clarithromycin full prescribing information for CONTRAINDICATIONS and WARNINGS, and for information regarding dosing in elderly and renally-impaired patients.
† Controlled studies did not extend beyond indicated duration.
‡ For patients who do not heal with lansoprazole delayed-release capsules for 8 weeks (5 to 10%), it may be helpful to give an additional 8 weeks of treatment. If there is a recurrence of erosive esophagitis, an additional 8 week course of lansoprazole delayed-release capsules may be considered.
§The lansoprazole delayed-release capsules dose was increased (up to 30 mg twice daily) in some pediatric patients after 2 or more weeks of treatment if they remained symptomatic. For pediatric patients unable to swallow an intact capsule please see Administration Options.
¶ Varies with individual patient. Recommended adult starting dose is 60 mg once daily. Doses should be adjusted to individual patient needs and should continue for as long as clinically indicated. Dosages up to 90 mg twice daily have been administered. Daily dose of greater than 120 mg should be administered in divided doses. Some patients with Zollinger-Ellison Syndrome have been treated continuously with lansoprazole delayed-release capsules for more than 4 years.
# Controlled studies did not extend beyond 12 months
Patients should be instructed that if a dose is missed, it should be taken as soon as possible. However, if the next scheduled dose is due, the patient should not take the missed dose, and should be instructed to take the next dose on time. Patients should be instructed not to take 2 doses at one time to make up for a missed dose.
2.2 Special PopulationsRenal impairment patients and geriatric patients do not require dosage adjustment. However, consider dose adjustment in patients with severe liver impairment. [See Use in Specific Populations (8.5, 8.6 and 8.7]
2.3 Important Administration InformationAdministration Options
Lansoprazole Delayed-Release Capsules - Oral Administration
- Lansoprazole delayed-release capsules should be swallowed whole.
- Alternatively, for patients who have difficulty swallowing capsules, lansoprazole delayed-release capsules can be opened and administered as follows:
- Open capsule.
- Sprinkle intact granules on one tablespoon of either applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
- Swallow immediately.
- Lansoprazole Delayed-Release Capsules may also be emptied into a small volume of either apple juice, orange juice or tomato juice and administered as follows:
- Open capsule.
- Sprinkle intact granules into a small volume of either apple juice, orange juice or tomato juice (60 mL – approximately 2 ounces).
- Mix briefly.
- Swallow immediately.
- To ensure complete delivery of the dose, the glass should be rinsed with two or more volumes of juice and the contents swallowed immediately.
Lansoprazole Delayed-Release Capsules - Nasogastric Tube (≥ 16 French) Administration
- For patients who have a nasogastric tube in place, lansoprazole delayed-release capsules can be administered as follows:
- Open capsule.
- Mix intact granules into 40 mL of apple juice. DO NOT USE OTHER LIQUIDS.
- Inject through the nasogastric tube into the stomach.
- Flush with additional apple juice to clear the tube.
USE IN OTHER FOODS AND LIQUIDS HAS NOT BEEN STUDIED CLINICALLY AND IS THEREFORE NOT RECOMMENDED.
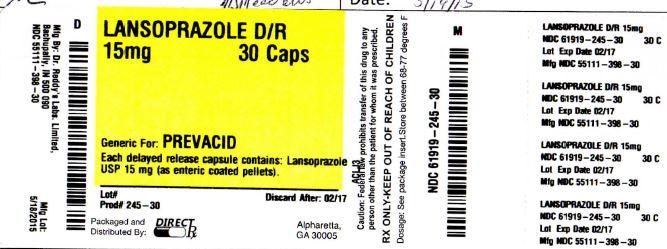
DOSAGE FORMS & STRENGTHS SECTION
Lansoprazole delayed release capsules USP, 15 mg are white to pale yellow colored enteric coated pellets filled in size ‘3’ hard gelatin capsules with opaque pink colored cap and opaque green colored body, imprinted ‘RDY’ on cap and ‘LAN’ on body with white ink.
Lansoprazole delayed release capsules USP, 30 mg are white to pale yellow colored enteric coated pellets filled in size ‘1’ hard gelatin capsules with opaque pink colored cap and opaque black colored body, imprinted ‘RDY’ on cap and ‘399’ on body with white ink.
CONTRAINDICATIONS SECTION
Lansoprazole delayed-release capsules are contraindicated in patients with known severe hypersensitivity to any component of the formulation of lansoprazole delayed-release capsules. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute interstitial nephritis, and urticaria [see Adverse Reactions (6)].
WARNINGS AND PRECAUTIONS SECTION
- 5.1 Gastric Malignancy
Symptomatic response to therapy with lansoprazole does not preclude the presence of gastric malignancy.
5.2 Acute Interstitial NephritisAcute interstitial nephritis has been observed in patients taking PPIs including lansoprazole. Acute interstitial nephritis may occur at any point during PPI therapy and is generally attributed to an idiopathic hypersensitivity reaction. Discontinue lansoprazole delayed-release capsules if acute interstitial nephritis develops [see Contraindications ( 4)].
5.3 Cyanocobalamin (vitamin B12) DeficiencyDaily treatment with any acid-suppressing medications over a long period of time (e.g., longer than 3 years) may lead to malabsorption of cyanocobalamin (vitamin B12) caused by hypo- or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed.
5.4 Clostridium difficile Associated DiarrheaPublished observational studies suggest that proton pump inhibitor (PPI) therapy like lansoprazole delayed-release capsules may be associated with an increased risk of Clostridium difficile associated diarrhea (CDAD), especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2)].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
CDAD has been reported with use of nearly all antibacterial agents. For more information specific to antibacterial agents (clarithromycin and amoxicillin) indicated for use in combination with lansoprazole delayed release capsules, refer to WARNINGS and PRECAUTIONS sections of those package inserts.
5.5 Bone FractureSeveral published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2) and Adverse Reactions (6.2)].
5.6 HypomagnesemiaHypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].
5.7 Concomitant use of lansoprazole delayed-release capsules with MethotrexateLiterature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions ( 7.6) and Clinical Pharmacology ( 12.3)].
ADVERSE REACTIONS SECTION
6.1 Clinical
Worldwide, over 10,000 patients have been treated with lansoprazole delayed-release capsules in Phase 2 or Phase 3 clinical trials involving various dosages and durations of treatment. In general, lansoprazole delayed-release capsules treatment has been well-tolerated in both short-term and long-term trials.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The following adverse reactions were reported by the treating physician to have a possible or probable relationship to drug in 1% or more of lansoprazole delayed-release capsules-treated patients and occurred at a greater rate in lansoprazole delayed-release capsules-treated patients than placebo-treated patients in Table 1.
Table 1: Incidence of Possibly or Probably Treatment-Related Adverse Reactions in Short-Term, Placebo-Controlled lansoprazole delayed-release capsules Studies
Body System/Adverse Event
lansoprazole delayed-release capsules
(N= 2768)
%
Placebo
(N= 1023)
%
Body as a Whole
Abdominal Pain 2.1 1.2
Digestive System
Constipation 1 0.4
Diarrhea 3.8 2.3
Nausea 1.3 1.2
Headache was also seen at greater than 1% incidence but was more common on placebo. The incidence of diarrhea was similar between patients who received placebo and patients who received 15 mg and 30 mg of lansoprazole delayed-release capsules, but higher in the patients who received 60 mg of lansoprazole delayed-release capsules (2.9%, 1.4%, 4.2%, and 7.4%, respectively).
The most commonly reported possibly or probably treatment-related adverse event during maintenance therapy was diarrhea.
In the risk reduction study of lansoprazole delayed-release capsules for NSAID-associated gastric ulcers, the incidence of diarrhea for patients treated with lansoprazole delayed-release capsules, misoprostol, and placebo was 5%, 22%, and 3%, respectively.
Another study for the same indication, where patients took either a COX-2 inhibitor or lansoprazole and naproxen, demonstrated that the safety profile was similar to the prior study. Additional reactions from this study not previously observed in other clinical trials with lansoprazole delayed-release capsules included contusion, duodenitis, epigastric discomfort, esophageal disorder, fatigue, hunger, hiatal hernia, hoarseness, impaired gastric emptying, metaplasia, and renal impairment.
Additional adverse experiences occurring in less than 1% of patients or subjects who received lansoprazole delayed-release capsules in domestic trials are shown below:
Body as a Whole – abdomen enlarged, allergic reaction, asthenia, back pain, candidiasis, carcinoma, chest pain (not otherwise specified), chills, edema, fever, flu syndrome, halitosis, infection (not otherwise specified), malaise, neck pain, neck rigidity, pain, pelvic pain
Cardiovascular System - angina, arrhythmia, bradycardia, cerebrovascular accident/cerebral infarction, hypertension/hypotension, migraine, myocardial infarction, palpitations, shock (circulatory failure), syncope, tachycardia, vasodilation
Digestive System – abnormal stools, anorexia, bezoar, cardiospasm, cholelithiasis, colitis, dry mouth, dyspepsia, dysphagia, enteritis, eructation, esophageal stenosis, esophageal ulcer, esophagitis, fecal discoloration, flatulence, gastric nodules/fundic gland polyps, gastritis, gastroenteritis, gastrointestinal anomaly, gastrointestinal disorder, gastrointestinal hemorrhage, glossitis, gum hemorrhage, hematemesis, increased appetite, increased salivation, melena, mouth ulceration, nausea and vomiting, nausea and vomiting and diarrhea, gastrointestinal moniliasis, rectal disorder, rectal hemorrhage, stomatitis, tenesmus, thirst, tongue disorder, ulcerative colitis, ulcerative stomatitis
Endocrine System - diabetes mellitus, goiter, hypothyroidism
Hemic and Lymphatic System - anemia, hemolysis, lymphadenopathy
Metabolism and Nutritional Disorders - avitaminosis, gout, dehydration, hyperglycemia/hypoglycemia, peripheral edema, weight gain/loss
Musculoskeletal System - arthralgia, arthritis, bone disorder, joint disorder, leg cramps, musculoskeletal pain, myalgia, myasthenia, ptosis, synovitis
Nervous System – abnormal dreams, agitation, amnesia, anxiety, apathy, confusion, convulsion, dementia, depersonalization, depression, diplopia, dizziness, emotional lability, hallucinations, hemiplegia, hostility aggravated, hyperkinesia, hypertonia, hypesthesia, insomnia, libido decreased/increased, nervousness, neurosis, paresthesia, sleep disorder, somnolence, thinking abnormality, tremor, vertigo
Respiratory System - asthma, bronchitis, cough increased, dyspnea, epistaxis, hemoptysis, hiccup, laryngeal neoplasia, lung fibrosis, pharyngitis, pleural disorder, pneumonia, respiratory disorder, upper respiratory inflammation/infection, rhinitis, sinusitis, stridor
Skin and Appendages - acne, alopecia, contact dermatitis, dry skin, fixed eruption, hair disorder, maculopapular rash, nail disorder, pruritus, rash, skin carcinoma, skin disorder, sweating, urticaria
Special Senses – abnormal vision, amblyopia, blepharitis, blurred vision, cataract, conjunctivitis, deafness, dry eyes, ear/eye disorder, eye pain, glaucoma, otitis media, parosmia, photophobia, retinal degeneration/disorder, taste loss, taste perversion, tinnitus, visual field defect
Urogenital System - abnormal menses, breast enlargement, breast pain, breast tenderness, dysmenorrhea, dysuria, gynecomastia, impotence, kidney calculus, kidney pain, leukorrhea, menorrhagia, menstrual disorder, penis disorder, polyuria, testis disorder, urethral pain, urinary frequency, urinary retention, urinary tract infection, urinary urgency, urination impaired, vaginitis.
6.2 Postmarketing Experience
Additional adverse experiences have been reported since lansoprazole delayed-release capsules has been marketed. The majority of these cases are foreign-sourced and a relationship to lansoprazole delayed-release capsules has not been established. Because these reactions were reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events are listed below by COSTART body system.
Body as a Whole – anaphylactic/anaphylactoid reactions; Digestive System - hepatotoxicity, pancreatitis, vomiting; Hemic and Lymphatic System - agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, thrombocytopenia, and thrombotic thrombocytopenic purpura; Infections and Infestations – Clostridium difficile associated diarrhea; Metabolism and Nutritional Disorders – hypomagnesemia; Musculoskeletal System - bone fracture,myositis; Skin and Appendages – severe dermatologic reactions including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal); Special Senses - speech disorder; Urogenital System – interstitial nephritis, urinary retention.
6.3 Combination Therapy with Amoxicillin and Clarithromycin
In clinical trials using combination therapy with lansoprazole delayed-release capsules plus amoxicillin and clarithromycin, and lansoprazole delayed-release capsules plus amoxicillin, no adverse reactions peculiar to these drug combinations were observed. Adverse reactions that have occurred have been limited to those that had been previously reported with lansoprazole delayed-release capsules, amoxicillin, or clarithromycin.
Triple Therapy: Lansoprazole delayed-release capsules /amoxicillin/clarithromycin
The most frequently reported adverse reactions for patients who received triple therapy for 14 days were diarrhea (7%), headache (6%), and taste perversion (5%). There were no statistically significant differences in the frequency of reported adverse reactions between the 10 and 14 day triple therapy regimens. No treatment-emergent adverse reactions were observed at significantly higher rates with triple therapy than with any dual therapy regimen.
Dual Therapy: Lansoprazole delayed-release capsules /amoxicillin
The most frequently reported adverse reactions for patients who received lansoprazole delayed-release capsules three times daily plus amoxicillin three times daily dual therapy were diarrhea (8%) and headache (7%). No treatment-emergent adverse reactions were observed at significantly higher rates with lansoprazole delayed-release capsules three times daily plus amoxicillin three times daily dual therapy than with lansoprazole delayed-release capsules alone.
For information about adverse reactions with antibacterial agents (amoxicillin and clarithromycin) indicated in combination with lansoprazole delayed-release capsules, refer to the ADVERSE REACTIONS section of their package inserts.
6.4 Laboratory Values
The following changes in laboratory parameters in patients who received lansoprazole delayed-release capsules were reported as adverse reactions:
Abnormal liver function tests, increased SGOT (AST), increased SGPT (ALT), increased creatinine, increased alkaline phosphatase, increased globulins, increased GGTP, increased/decreased/abnormal WBC, abnormal AG ratio, abnormal RBC, bilirubinemia, blood potassium increased, blood urea increased, crystal urine present, eosinophilia, hemoglobin decreased, hyperlipemia, increased/decreased electrolytes, increased/decreased cholesterol, increased glucocorticoids, increased LDH, increased/decreased/abnormal platelets, increased gastrin levels and positive fecal occult blood. Urine abnormalities such as albuminuria, glycosuria, and hematuria were also reported. Additional isolated laboratory abnormalities were reported.
In the placebo controlled studies, when SGOT (AST) and SGPT (ALT) were evaluated, 0.4% (4/978) and 0.4% (11/2677) patients, who received placebo and lansoprazole delayed-release capsules, respectively, had enzyme elevations greater than three times the upper limit of normal range at the final treatment visit. None of these patients who received lansoprazole delayed-release capsules reported jaundice at any time during the study.
In clinical trials using combination therapy with lansoprazole delayed-release capsules plus amoxicillin and clarithromycin, and lansoprazole delayed-release capsules plus amoxicillin, no increased laboratory abnormalities particular to these drug combinations were observed.
For information about laboratory value changes with antibacterial agents (amoxicillin and clarithromycin) indicated in combination with lansoprazole delayed-release capsules, refer to the ADVERSE REACTIONS section of their package inserts.
DRUG INTERACTIONS SECTION
- 7.1 Drugs with pH-Dependent Absorption Kinetics
Due to its effects on gastric acid secretion, lansoprazole can reduce the absorption of drugs where gastric pH is an important determinant of their bioavailability. Like with other drugs that decrease the intragastric acidity, the absorption of drugs such as ampicillin esters, ketoconazole, atazanavir, iron salts, erlotinib, and mycophenolate mofetil (MMF) can decrease, while the absorption of drugs such as digoxin can increase during treatment with lansoprazole delayed-release capsules [see Clinical Pharmacology ( 12.3)].
Lansoprazole delayed-release capsules are likely to substantially decrease the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, lansoprazole delayed-release capsules should not be co-administered with atazanavir [see Clinical Pharmacology ( 12.3)].
Co-administration of PPIs in healthy subjects and in transplant patients receiving MMF has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in MMF solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving PPIs and MMF. Use lansoprazole delayed-release capsules with caution in transplant patients receiving MMF.
7.2 WarfarinIn a study of healthy subjects, co-administration of single or multiple 60 mg doses of lansoprazole delayed-release capsules and warfarin did not affect the pharmacokinetics of warfarin nor prothrombin time (see Clinical Pharmacology (12.3). However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with PPIs and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time. [See Clinical Pharmacology (12.3)]
7.3 TacrolimusConcomitant administration of lansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.
7.4 TheophyllineA minor increase (10%) in the clearance of theophylline was observed following the administration of lansoprazole delayed-release capsules concomitantly with theophylline. Although the magnitude of the effect on theophylline clearance is small, individual patients may require additional titration of their theophylline dosage when lansoprazole delayed-release capsules is started or stopped to ensure clinically effective blood levels. [See Clinical Pharmacology (12.3)]
7.5 ClopidogrelConcomitant administration of lansoprazole and clopidogrel in healthy subjects had no clinically important effect on exposure to the active metabolite of clopidogrel or clopidogrel-induced platelet inhibition [see Clinical Pharmacology (12.3)]. No dose adjustment of clopidogrel is necessary when administered with an approved dose of lansoprazole delayed-release capsules.
7.6 MethotrexateCase reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of high dose methotrexate with PPIs have been conducted [see Warnings and Precautions ( 5.7)].
In a study of rheumatoid arthritis patients receiving low-dose methotrexate, lansoprazole delayed-release capsules and naproxen, no effect on pharmacokinetics of methotrexate was observed [see Clinical Pharmacology ( 12.3)].
7.7 Combination Therapy with ClarithromycinConcomitant administration of clarithromycin with other drugs can lead to serious adverse reactions due to drug interactions [see Warnings and Precautions in prescribing information for clarithromycin]. Because of these drug interactions, clarithromycin is contraindicated for co-administration with certain drugs [see Contraindications in prescribing information for clarithromycin].
For information on drug interactions for amoxicillin or clarithromycin, refer to their full prescribing information, DRUG INTERACTIONS section
USE IN SPECIFIC POPULATIONS SECTION
8.1 Pregnancy
Teratogenic effects
Pregnancy Category B. Reproduction studies have been performed in pregnant rats at oral doses up to 40 times the recommended human dose and in pregnant rabbits at oral doses up to 16 times the recommended human dose and have revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole. There are, however, no adequate or well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed [See Nonclinical Toxicology (13.2)].
See full prescribing information for clarithromycin before using in pregnant women.
8.3 Nursing Mothers
Lansoprazole or its metabolites are excreted in the milk of rats. It is not known whether lansoprazole is excreted in human milk. Because many drugs are excreted in human milk, because of the potential for serious adverse reactions in nursing infants from lansoprazole, and because of the potential for tumorigenicity shown for lansoprazole in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue lansoprazole, taking into account the importance of lansoprazole to the mother.
8.4 Pediatric Use
The safety and effectiveness of lansoprazole delayed-release capsules have been established in pediatric patients 1 to 17 years of age for short-term treatment of symptomatic GERD and erosive esophagitis.
Neonate to less than 1 year of age
The pharmacokinetics of lansoprazole were studied in pediatric patients with GERD aged less than 28 days and 1 to 11 months. Compared to healthy adults receiving 30 mg, neonates had higher exposure (mean weight-based normalized AUC values 2.04-and 1.88-fold higher at doses of 0.5 mg/kg/day and 1 mg/kg/day, respectively). Infants aged ≤10 weeks had clearance and exposure values that were similar to neonates. Infants aged greater than 10 weeks who received 1 mg/kg/day had mean AUC values that were similar to adults who received a 30 mg dose.
Lansoprazole was not found to be effective in a U.S. and Polish 4 week multicenter, double-blind, placebo-controlled, parallel-group study of 162 patients between one month and less than 12 months of age with symptomatic GERD based on a medical history of crying/fussing/irritability associated with feedings who had not responded to conservative GERD management (i.e., non-pharmacologic intervention) for 7 to 14 days. Patients received lansoprazole as a suspension daily (0.2 to 0.3 mg/kg/day in infants ≤10 weeks of age or 1 to 1.5 mg/kg/day in infants greater than 10 weeks or placebo) for up to 4 weeks of double-blind treatment.
The primary efficacy endpoint was assessed by greater than 50% reduction from baseline in either the percent of feedings with a crying/fussing/irritability episode or the duration (minutes) of a crying/fussing/irritability episode within one hour after feeding.
There was no difference in the percentage of responders between the lansoprazole pediatric suspension group and placebo group (54% in both groups). There were no adverse events reported in pediatric clinical studies (1 month to less than 12 months of age) that were not previously observed in adults. Based on the results of the Phase 3 efficacy study, lansoprazole was not shown to be effective. Therefore, these results do not support the use of lansoprazole in treating symptomatic GERD in infants.
One to 11 years of age
In an uncontrolled, open-label, U.S. multicenter study, 66 pediatric patients (1 to 11 years of age) with GERD were assigned, based on body weight, to receive an initial dose of either lansoprazole delayed-release capsules 15 mg daily if ≤ 30 kg or lansoprazole delayed-release capsules 30 mg daily if greater than 30 kg administered for 8 to 12 weeks. The lansoprazole delayed-release capsules dose was increased (up to 30 mg twice daily) in 24 of 66 pediatric patients after 2 or more weeks of treatment if they remained symptomatic. At baseline 85% of patients had mild to moderate overall GERD symptoms (assessed by investigator interview), 58% had non-erosive GERD and 42% had erosive esophagitis (assessed by endoscopy).
After 8 to 12 weeks of lansoprazole delayed-release capsules treatment, the intent-to-treat analysis demonstrated an approximate 50% reduction in frequency and severity of GERD symptoms.
Twenty-one of 27 erosive esophagitis patients were healed at 8 weeks and 100% of patients were healed at 12 weeks by endoscopy (Table 2).
Table 2: GERD symptom improvement and Erosive Esophagitis healing rates in pediatric patients age 1 to 11
GERD
Final Visit* % (n/N)
* At Week 8 or Week 12 † Symptoms assessed by patients diary kept by caregiver. ‡ No data were available for 4 pediatric patients.
Symptomatic GERD
Improvement in Overall GERD Symptoms†
76% (47/62 ‡)
Erosive Esophagitis
Improvement in Overall GERD Symptoms†
Healing Rate
81% (22/27)
100% (27/27)
In a study of 66 pediatric patients in the age group 1 year to 11 years old after treatment with lansoprazole delayed-release capsules given orally in doses of 15 mg daily to 30 mg twice daily, increases in serum gastrin levels were similar to those observed in adult studies. Median fasting serum gastrin levels increased 89% from
51 pg/ mL at baseline to 97 pg/mL [interquartile range (25th to 75th percentile) of 71 to 130 pg/ mL] at the final visit.
The pediatric safety of lansoprazole delayed-release capsules has been assessed in 66 pediatric patients aged 1 to 11 years of age. Of the 66 patients with GERD 85% (56/66) took lansoprazole delayed-release capsules for 8 weeks and 15% (10/66) took it for 12 weeks.
The most frequently reported (2 or more patients) treatment-related adverse reactions in patients 1 to 11 years of age (N=66) were constipation (5%) and headache (3%).
Twelve to 17 years of age
In an uncontrolled, open-label, U.S. multicenter study, 87 adolescent patients (12 to 17 years of age) with symptomatic GERD were treated with lansoprazole delayed-release capsules for 8 to 12 weeks. Baseline upper endoscopies classified these patients into two groups: 64 (74%) nonerosive GERD and 23 (26%) erosive esophagitis (EE). The nonerosive GERD patients received lansoprazole delayed-release capsules 15 mg daily for 8 weeks and the EE patients received lansoprazole delayed-release capsules 30 mg daily for 8 to 12 weeks. At baseline, 89% of these patients had mild to moderate overall GERD symptoms (assessed by investigator interviews). During 8 weeks of lansoprazole delayed-release capsules treatment, adolescent patients experienced a 63% reduction in frequency and a 69% reduction in severity of GERD symptoms based on diary results.
Twenty-one of 22 (95.5%) adolescent erosive esophagitis patients were healed after 8 weeks of lansoprazole delayed-release capsules treatment. One patient remained unhealed after 12 weeks of treatment (Table 3).
Table 3: GERD symptom improvement and Erosive Esophagitis healing rates in pediatric patients age 12 to 17
GERD
Final Visit % (n/N)
* Symptoms assessed by patient diary (parents/caregivers as necessary). † No data available for 5 patients. ‡ Data from one healed patient was excluded from this analysis due to timing of final endoscopy.
Symptomatic GERD (All Patients)
Improvement in Overall GERD Symptoms* 73.2% (60/82)†
Nonerosive GERD
Improvement in Overall GERD Symptoms* 71.2% (42/59)†
Erosive Esophagitis
Improvement in Overall GERD Symptoms* 78.3% (18/23)
Healing Rate ‡ 95.5% (21/22)‡
In these 87 adolescent patients, increases in serum gastrin levels were similar to those observed in adult studies, median fasting serum gastrin levels increased 42% from 45 pg/mL at baseline to 64 pg/mL [interquartile range (25th to 75th percentile) of 44 to 88 pg/mL] at the final visit. (Normal serum gastrin levels are 25 to 111 pg/mL).
The safety of lansoprazole delayed-release capsules has been assessed in these 87 adolescent patients. Of the 87 adolescent patients with GERD, 6% (5/87) took lansoprazole delayed-release capsules for less than 6 weeks, 93% (81/87) for 6 to 10 weeks, and 1% (1/87) for greater than 10 weeks.
The most frequently reported (at least 3%) treatment-related adverse reactions in these patients were headache (7%), abdominal pain (5%), nausea (3%) and dizziness (3%). Treatment-related dizziness, reported in this package insert as occurring in less than 1% of adult patients, was reported in this study by 3 adolescent patients with nonerosive GERD, who had dizziness concurrently with other reactions (such as migraine, dyspnea, and vomiting).
8.5 Geriatric Use
No dosage adjustment of lansoprazole delayed-release capsules is necessary in geriatric patients. The incidence rates of lansoprazole delayed-release capsules-associated adverse reactions and laboratory test abnormalities are similar to those seen in younger patients. [See Clinical Pharmacology (12.3)]
8.6 Renal Impairment
No dosage adjustment of lansoprazole delayed-release capsules is necessary in patients with renal impairment. The pharmacokinetics of lansoprazole in patients with various degrees of renal impairment were not substantially different compared to those in subjects with normal renal function. [See Clinical Pharmacology (12.3)]
8.7 Hepatic Impairment
In patients with various degrees of chronic hepatic impairment, an increase in the mean AUC of up to 500% was observed at steady state compared to healthy subjects. Consider dose reduction in patients with severe hepatic impairment. [See Clinical Pharmacology (12.3)]
8.8 Gender
Over 4,000 women were treated with lansoprazole delayed-release capsules. Ulcer healing rates in females were similar to those in males. The incidence rates of adverse reactions in females were similar to those seen in males. [See Clinical Pharmacology (12.3)]
8.9 Race
The pooled mean pharmacokinetic parameters of lansoprazole delayed-release capsules from twelve U.S. Phase 1 studies (N=513) were compared to the mean pharmacokinetic parameters from two Asian studies (N=20). The mean AUCs of lansoprazole delayed-release capsules in Asian subjects were approximately twice those seen in pooled U.S. data; however, the inter-individual variability was high. The Cmax values were comparable.
OVERDOSAGE SECTION
Lansoprazole delayed-release capsules are not removed from the circulation by hemodialysis. In one reported overdose, a patient consumed 600 mg of lansoprazole delayed-release capsules with no adverse reaction. Oral lansoprazole delayed-release capsules doses up to 5000 mg/kg in rats [approximately 1300 times the 30 mg human dose based on body surface area BSA)] and in mice (about 675.7 times the 30 mg human dose based on (BSA) did not produce deaths or any clinical signs.
DESCRIPTION SECTION
The active ingredient in lansoprazole delayed-release capsules USP is lansoprazole USP, a substituted benzimidazole, 2-[[[3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridyl] methyl] sulfinyl] benzimidazole, a compound that inhibits gastric acid secretion. Its empirical formula is C16H14F3N3O2S with a molecular weight of 369.37. Lansoprazole USP has the following structure:
Lansoprazole USP is a white to brownish-white powder which melts with decomposition at approximately 166°C. Lansoprazole USP is freely soluble in dimethylformamideand practically insoluble in water.
Lansoprazole USP is stable when exposed to light for up to two months. The rate of degradation of the compound in aqueous solution increases with decreasing pH. The degradation half-life of the drug substance in aqueous solution at 25°C is approximately 0.5 hour at pH 5.0 and approximately 18 hours at pH 7.0.
Lansoprazole USP is supplied as delayed-release capsules.
The delayed-release capsules are available in two dosage strengths: 15 mg and 30 mg of lansoprazole USP per capsule. Each delayed-release capsule contains enteric-coated granules consisting of 15 mg or 30 mg of lansoprazole USP (active ingredient) and the following inactive ingredients: ammonium hydroxide, hydroxypropyl cellulose, low substituted hydroxypropyl cellulose, magnesium carbonate, methacrylic acid copolymer, polyethylene glycol, polysorbate 80, propylene glycol, shellac, simethicone, starch, sucrose, sugar spheres, talc, and titanium dioxide.
Components of the gelatin capsule include gelatin, iron oxide red, iron oxide yellow, FD&C Blue 2, sodium lauryl sulphate and titanium dioxide for 15 mg capsules and gelatin, iron oxide black, iron oxide red, iron oxide yellow, sodium lauryl sulphate and titanium dioxide for 30 mg capsules.
CLINICAL PHARMACOLOGY SECTION
- 12.1 Mechanism of Action
Lansoprazole belongs to a class of antisecretory compounds, the substituted benzimidazoles, that suppress gastric acid secretion by specific inhibition of the (H+, K+)-ATPase enzyme system at the secretory surface of the gastric parietal cell. Because this enzyme system is regarded as the acid (proton) pump within the parietal cell, lansoprazole has been characterized as a gastric acid-pump inhibitor, in that it blocks the final step of acid production. This effect is dose-related and leads to inhibition of both basal and stimulated gastric acid secretion irrespective of the stimulus. Lansoprazole does not exhibit anticholinergic or histamine type-2 antagonist activity.
12.2 PharmacodynamicsAntisecretory Activity: After oral administration, lansoprazole was shown to significantly decrease the basal acid output and significantly increase the mean gastric pH and percent of time the gastric pH was greater than 3 and greater than 4. Lansoprazole also significantly reduced meal-stimulated gastric acid output and secretion volume, as well as pentagastrin-stimulated acid output. In patients with hypersecretion of acid, lansoprazole significantly reduced basal and pentagastrin-stimulated gastric acid secretion. Lansoprazole inhibited the normal increases in secretion volume, acidity and acid output induced by insulin.
The intragastric pH results of a five-day, pharmacodynamic, crossover study of 15 mg and 30 mg of once daily lansoprazole are presented in Table 4:
Table 4: Mean Antisecretory Effects After Single and Multiple Daily Lansoprazole Dosing Lansoprazole Parameter Baseline Value 15 mg 30 mg Day 1 Day 5 Day 1 Day 5 NOTE: An intragastric pH of greater than 4 reflects a reduction in gastric acid by 99%. *(p<0.05) versus baseline only. †(p<0.05) versus baseline and lansoprazole 15 mg. Mean 24-Hour pH 2.1 2.7 * 4.0 * 3.6 † 4.9 † Mean Nighttime pH 1.9 2.4 3.0 * 2.6 3.8 † % Time Gastric pH>3 18 33 * 59 * 51 † 72 † % Time Gastric pH>4 12 22 * 49 * 41 † 66 † After the initial dose in this study, increased gastric pH was seen within 1 to 2 hours with 30 mg of lansoprazole and 2 to 3 hours with 15 mg of lansoprazole. After multiple daily dosing, increased gastric pH was seen within the first hour post-dosing with 30 mg of lansoprazole and within 1 to 2 hours post-dosing with 15 mg of lansoprazole.
Acid suppression may enhance the effect of antimicrobials in eradicating Helicobacter pylori (H. pylori). The percentage of time gastric pH was elevated above 5 and 6 was evaluated in a crossover study of lansoprazole delayed-release capsules given daily, twice daily and three times daily (Table 5).
Table 5: Mean Antisecretory Effects After 5 Days of twice daily and three times daily Dosing Lansoprazole Parameter 30 mg daily 15 mg twice daily 30 mg twice daily 30 mg three times daily *(p<0.05) versus lansoprazole 30 mg daily †(p<0.05) versus lansoprazole 30 mg daily, 15 mg twice daily and 30 mg twice daily. % Time Gastric pH>5 43 47 59 * 77 † % Time Gastric pH>6 20 23 28 45 † The inhibition of gastric acid secretion as measured by intragastric pH gradually returned to normal over two to four days after multiple doses. There was no indication of rebound gastric acidity.
Enterochromaffin-like (ECL) Cell Effects
During lifetime exposure of rats with up to 150 mg/kg/day of lansoprazole dosed seven days per week, marked hypergastrinemia was observed followed by ECL cell proliferation and formation of carcinoid tumors, especially in female rats. Gastric biopsy specimens from the body of the stomach from approximately 150 patients treated continuously with lansoprazole for at least one year did not show evidence of ECL cell effects similar to those seen in rat studies. Longer term data are needed to rule out the possibility of an increased risk of the development of gastric tumors in patients receiving long-term therapy with lansoprazole. [See Nonclinical Toxicology (13.1)]
Other Gastric Effects in Humans
Lansoprazole did not significantly affect mucosal blood flow in the fundus of the stomach. Due to the normal physiologic effect caused by the inhibition of gastric acid secretion, a decrease of about 17% in blood flow in the antrum, pylorus, and duodenal bulb was seen. Lansoprazole significantly slowed the gastric emptying of digestible solids. Lansoprazole increased serum pepsinogen levels and decreased pepsin activity under basal conditions and in response to meal stimulation or insulin injection. As with other agents that elevate intragastric pH, increases in gastric pH were associated with increases in nitrate-reducing bacteria and elevation of nitrite concentration in gastric juice in patients with gastric ulcer. No significant increase in nitrosamine concentrations was observed.
Serum Gastrin Effects
In over 2100 patients, median fasting serum gastrin levels increased 50% to 100% from baseline but remained within normal range after treatment with 15 to 60 mg of oral lansoprazole. These elevations reached a plateau within two months of therapy and returned to pretreatment levels within four weeks after discontinuation of therapy.
Endocrine Effects
Human studies for up to one year have not detected any clinically significant effects on the endocrine system. Hormones studied include testosterone, luteinizing hormone (LH), follicle stimulating hormone (FSH), sex hormone binding globulin (SHBG), dehydroepiandrosterone sulfate (DHEA-S), prolactin, cortisol, estradiol, insulin, aldosterone, parathormone, glucagon, thyroid stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), and somatotropic hormone (STH). Lansoprazole in oral doses of 15 to 60 mg for up to one year had no clinically significant effect on sexual function. In addition, lansoprazole in oral doses of 15 to 60 mg for two to eight weeks had no clinically significant effect on thyroid function. In 24-month carcinogenicity studies in Sprague-Dawley rats with daily lansoprazole dosages up to 150 mg/kg, proliferative changes in the Leydig cells of the testes, including benign neoplasm, were increased compared to control rats.
Other Effects
No systemic effects of lansoprazole on the central nervous system, lymphoid, hematopoietic, renal, hepatic, cardiovascular, or respiratory systems have been found in humans. Among 56 patients who had extensive baseline eye evaluations, no visual toxicity was observed after lansoprazole treatment (up to 180 mg/day) for up to 58 months. After lifetime lansoprazole exposure in rats, focal pancreatic atrophy, diffuse lymphoid hyperplasia in the thymus, and spontaneous retinal atrophy were seen.
Microbiology
Lansoprazole, clarithromycin and/or amoxicillin have been shown to be active against most strains of Helicobacter pylori in vitro and in clinical infections as described in the INDICATIONS AND USAGE section. [See Indications and Usage (1.2)]
Helicobacter pylori Pretreatment Resistance
Clarithromycin pretreatment resistance (≥2.0 mcg/mL) was 9.5% (91/960) by E-test and 11.3% (12/106) by agar dilution in the dual and triple therapy clinical trials (M93-125, M93-130, M93-131, M95-392, and M95-399).
Amoxicillin pretreatment susceptible isolates (≤0.25 mcg/mL) occurred in 97.8% (936/957) and 98 % (98/100) of the patients in the dual and triple therapy clinical trials by E-test and agar dilution, respectively. Twenty-one of 957 patients (2.2%) by E-test and 2 of 100 patients (2%) by agar dilution had amoxicillin pretreatment MICs of greater than 0.25 mcg/mL. One patient on the 14-day triple therapy regimen had an unconfirmed pretreatment amoxicillin minimum inhibitory concentration (MIC) of greater than 256 mcg/mL by E-test and the patient was eradicated of H. pylori (Table 6).
Table 6: Clarithromycin Susceptibility Test Results andClinical/Bacteriological Outcomes* ClarithromycinPretreatment Results Clarithtromycin Post-treatment Results H. pylorinegative-eradicated H. pylori positive – noteradicatedPost-treatment susceptibilityresults S† I† R† No MIC Triple Therapy 14-day (lansoprazole 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily) (M95-399, M93-131, M95-392) Susceptible† 112 105 7 Intermediate† 3 3 Resistant† 17 6 7 4 Triple Therapy 10-Day (lansoprazole 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily) (M95-399) Susceptible† 42 40 1 1 Intermediate† Resistant† 4 1 3 *Includes only patients with pretreatment clarithromycin susceptibility test results
†Susceptible (S) MIC ≤ 0.25 mcg/mL, Intermediate (I) MIC 0.5 -1 mcg/mL, Resistant (R) MIC ≥2 mcg/mL
Patients not eradicated of H. pylori following lansoprazole/amoxicillin/clarithromycin triple therapy will likely have clarithromycin resistant H. pylori. Therefore, for those patients who fail therapy, clarithromycin susceptibility testing should be done when possible. Patients with clarithromycin resistant H. pylori should not be treated withlansoprazole/amoxicillin/clarithromycin triple therapy or with regimens which include clarithromycin as the sole antimicrobial agent.
Amoxicillin Susceptibility Test Results and Clinical/Bacteriological Outcomes: In the dual and triple therapy clinical trials, 82.6% (195/236) of the patients that had pretreatment amoxicillin susceptible MICs (≤0.25 mcg/mL) were eradicated of H. pylori. Of those with pretreatment amoxicillin MICs of greater than 0.25 mcg/mL, three of six had the H. pylori eradicated. A total of 30% (21/70) of the patients failed lansoprazole 30 mg three times daily /amoxicillin 1 g three times daily dual therapy and a total of 12.8% (22/172) of the patients failed the 10 and 14 day triple therapy regimens. Post-treatment susceptibility results were not obtained on 11 of the patients who failed therapy. Nine of the 11 patients with amoxicillin post-treatment MICs that failed the triple therapy regimen also had clarithromycin resistant H. pylori isolates.
Susceptibility Test for Helicobacter pylori: For susceptibility testing information about Helicobacter pylori, see Microbiology section in prescribing information for clarithromycin and amoxicillin.
12.3 PharmacokineticsLansoprazole delayed-release capsules contain an enteric-coated granule formulation of lansoprazole. Absorption of lansoprazole begins only after the granules leave the stomach. Absorption is rapid, with mean peak plasma levels of lansoprazole occurring after approximately 1.7 hours. After a single-dose administration of 15 mg to 60 mg of oral lansoprazole, the peak plasma concentrations (Cmax) of lansoprazole and the area under the plasma concentration curves (AUCs) of lansoprazole were approximately proportional to the administered dose. Lansoprazole does not accumulate and its pharmacokinetics are unaltered by multiple dosing.
Absorption: The absorption of lansoprazole is rapid, with the mean Cmax occurring approximately 1.7 hours after oral dosing, and the absolute bioavailability is over 80%. In healthy subjects, the mean (±SD) plasma half-life was 1.5 (±1) hours. Both the Cmax and AUC are diminished by about 50% to 70% if lansoprazole is given 30 minutes after food, compared to the fasting condition. There is no significant food effect if lansoprazole is given before meals.
Distribution: Lansoprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 0.05 to 5 mcg/mL.
Metabolism: Lansoprazole is extensively metabolized in the liver. Two metabolites have been identified in measurable quantities in plasma (the hydroxylated sulfinyl and sulfone derivatives of lansoprazole). These metabolites have very little or no antisecretory activity. Lansoprazole is thought to be transformed into two active species which inhibit acid secretion by blocking the proton pump [(H+, K+)-ATPase enzyme system] at the secretory surface of the gastric parietal cell. The two active species are not present in the systemic circulation. The plasma elimination half-life of lansoprazole is less than 2 hours while the acid inhibitory effect lasts more than 24 hours. Therefore, the plasma elimination half-life of lansoprazole does not reflect its duration of suppression of gastric acid secretion.
Elimination: Following single-dose oral administration of lansoprazole delayed-release capsules, virtually no unchanged lansoprazole was excreted in the urine. In one study, after a single oral dose of 14C-lansoprazole, approximately one-third of the administered radiation was excreted in the urine and two-thirds was recovered in the feces. This implies a significant biliary excretion of the lansoprazole metabolites.
Specific Populations
Pediatric Use:
One to 17 years of age
The pharmacokinetics of lansoprazole were studied in pediatric patients with GERD aged 1 to 11 years and 12 to 17 years in two separate clinical studies. In children aged 1 to 11 years, lansoprazole was dosed 15 mg daily for subjects weighing ≤ 30 kg and 30 mg daily for subjects weighing greater than 30 kg. Mean Cmax and AUC values observed on Day 5 of dosing were similar between the two dose groups and were not affected by weight or age within each weight-adjusted dose group used in the study. In adolescent subjects aged 12 to 17 years, subjects were randomized to receive lansoprazole at 15 mg or 30 mg daily. Mean Cmax and AUC values of lansoprazole were not affected by body weight or age; and nearly dose-proportional increases in mean Cmax and AUC values were observed between the two dose groups in the study. Overall, lansoprazole pharmacokinetics in pediatric patients aged 1 to 17 years were similar to those observed in healthy adult subjects.
Geriatric Use: The clearance of lansoprazole is decreased in the elderly, with elimination half-life increased approximately 50% to 100%. Because the mean half-life in the elderly remains between 1.9 to 2.9 hours, repeated once daily dosing does not result in accumulation of lansoprazole. Peak plasma levels were not increased in the elderly. No dosage adjustment is necessary in the elderly [See Use in Specific Populations (8.5)].
Renal Impairment: In patients with severe renal impairment, plasma protein binding decreased by 1% to 1.5% after administration of 60 mg of lansoprazole. Patients with renal impairment had a shortened elimination half-life and decreased total AUC (free and bound). The AUC for free lansoprazole in plasma, however, was not related to the degree of renal impairment; and the Cmax and tmax (time to reach the maximum concentration) were not different than the Cmax and tmax from subjects with normal renal function. No dosage adjustment is necessary in patients with renal impairment [See Use in Specific Populations (8.6]).
Hepatic Impairment: In patients with various degrees of chronic hepatic impairment, the mean plasma half-life of lansoprazole was prolonged from 1.5 hours to 3.2 to 7.2 hours. An increase in the mean AUC of up to 500% was observed at steady state in hepatically-impaired patients compared to healthy subjects. Consider dose reduction in patients with severe hepatic impairment [See Use in Specific Populations (8.7)].
Gender: In a study comparing 12 male and 6 female human subjects who received lansoprazole, no gender differences were found in pharmacokinetics and intragastric pH results [See Use in Specific Populations (8.8)].
Drug-Drug Interactions
Lansoprazole may interfere with the absorption of other drugs where gastric pH is an important determinant of bioavailability (e.g., ketoconazole, ampicillin esters, iron salts, digoxin).
Lansoprazole is metabolized through the cytochrome P450 system, specifically through the CYP3A and CYP2C19 isozymes. Studies have shown that lansoprazole does not have clinically significant interactions with other drugs metabolized by the cytochrome P450 system, such as warfarin, antipyrine, indomethacin, ibuprofen, phenytoin, propranolol, prednisone, diazepam, or clarithromycin in healthy subjects. These compounds are metabolized through various cytochrome P450 isozymes including CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A.
Atazanavir: Lansoprazole delayed-release capsules causes long-lasting inhibition of gastric acid secretion. lansoprazole delayed-release capsules substantially decreases the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, lansoprazole delayed-release capsules, or other proton pump inhibitors, should not be co-administered with atazanavir.
Theophylline: When lansoprazole delayed-release capsules were administered concomitantly with theophylline (CYP1A2, CYP3A), a minor increase (10%) in the clearance of theophylline was seen. Because of the small magnitude and the direction of the effect on theophylline clearance, this interaction is unlikely to be of clinical concern. Nonetheless, individual patients may require additional titration of their theophylline dosage when lansoprazole delayed-release capsules is started or stopped to ensure clinically effective blood levels.
Warfarin: In a study of healthy subjects neither the pharmacokinetics of warfarin enantiomers nor prothrombin time were affected following single or multiple 60 mg doses of lansoprazole. However, there have been reports of increased International Normalized Ratio (INR) and prothrombin time in patients receiving proton pump inhibitors, including lansoprazole delayed-release capsules, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Methotrexate and 7-hydromethotrexate: In an open-label, single-arm, eight-day, pharmacokinetic study of 28 adult rheumatoid arthritis patients (who required the chronic use of 7.5 to 15 mg of methotrexate given weekly), administration of 7 days of naproxen 500 mg twice daily and lansoprazole delayed-release capsules 30 mg daily had no effect on the pharmacokinetics of methotrexate and 7-hydroxymethotrexate. While this study was not designed to assess the safety of this combination of drugs, no major adverse reactions were noted. However, this study was conducted with low doses of methotrexate. A drug interaction study with high doses of methotrexate has not been conducted.
Amoxicillin: Lansoprazole delayed-release capsules has also been shown to have no clinically significant interaction with amoxicillin.
Sucralfate: In a single-dose crossover study examining lansoprazole delayed-release capsules 30 mg and omeprazole 20 mg each administered alone and concomitantly with sucralfate 1 gram, absorption of the proton pump inhibitors was delayed and their bioavailability was reduced by 17% and 16%, respectively, when administered concomitantly with sucralfate. Therefore, proton pump inhibitors should be taken at least 30 minutes prior to sucralfate. In clinical trials, antacids were administered concomitantly with lansoprazole delayed-release capsules and there was no evidence of a change in the efficacy of lansoprazole delayed-release capsules.
Clopidogrel: Clopidogrel is metabolized to its active metabolite in part by CYP2C19. A study of healthy subjects who were CYP2C19 extensive metabolizers, receiving once daily administration of clopidogrel 75 mg alone or concomitantly with lansoprazole delayed-release capsules 30 mg (n=40), for 9 days was conducted. The mean AUC of the active metabolite of clopidogrel was reduced by approximately 14% (mean AUC ratio was 86%, with 90% CI of 80 to 92%) when lansoprazole delayed-release capsules was coadministered compared to administration of clopidogrel alone. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation (induced by 5 mcM ADP) was related to the change in the exposure to clopidogrel active metabolite. The clinical significance of this finding is not clear.
NONCLINICAL TOXICOLOGY SECTION
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In two 24-month carcinogenicity studies, Sprague-Dawley rats were treated with oral lansoprazole doses of 5 to 150 mg/kg/day –about 1 to 40 times the exposure on a body surface (mg/m2) basis of a 50 kg person of average height [1.46 m2 body surface area (BSA)] given the recommended human dose of 30 mg/day. Lansoprazole produced dose-related gastric enterochromaffin-like (ECL) cell hyperplasia and ECL cell carcinoids in both male and female rats. It also increased the incidence of intestinal metaplasia of the gastric epithelium in both sexes. In male rats, lansoprazole produced a dose-related increase of testicular interstitial cell adenomas. The incidence of these adenomas in rats receiving doses of 15 to 150 mg/kg/day (4 to 40 times the recommended human dose based on BSA) exceeded the low background incidence (range = 1.4 to 10%) for this strain of rat.
In a 24-month carcinogenicity study, CD-1 mice were treated with oral lansoprazole doses of 15 to 600 mg/kg/day, 2 to 80 times the recommended human dose based on BSA. Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. It also produced an increased incidence of liver tumors (hepatocellular adenoma plus carcinoma). The tumor incidences in male mice treated with 300 and 600 mg/kg/day (40 to 80 times the recommended human dose based on BSA) and female mice treated with 150 to 600 mg/kg/day (20 to 80 times the recommended human dose based on BSA) exceeded the ranges of background incidences in historical controls for this strain of mice. Lansoprazole treatment produced adenoma of rete testis in male mice receiving 75 to 600 mg/kg/day (10 to 80 times the recommended human dose based on BSA).
A 26-week p53 (+/-) transgenic mouse carcinogenicity study was not positive.
Lansoprazole was positive in the Ames test and the in vitro human lymphocyte chromosomal aberration assay.Lansoprazole was not genotoxic in the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test, or the rat bone marrow cell chromosomal aberration test.
Lansoprazole at oral doses up to 150 mg/kg/day (40 times the recommended human dose based on BSA) was found to have no effect on fertility and reproductive performance of male and female rats.
13.2 Animal Toxicology and/or Pharmacology
Reproductive Toxicology Studies
Reproduction studies have been performed in pregnant rats at oral lansoprazole doses up to 150 mg/kg/day [40 times the recommended human dose (30 mg/day) based on body surface area (BSA)] and pregnant rabbits at oral lansoprazole doses up to 30 mg/kg/day (16 times the recommended human dose based on BSA) and have revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole.
CLINICAL STUDIES SECTION
-
Duodenal Ulcer
In a U.S. multicenter, double-blind, placebo-controlled, dose-response (15, 30, and 60 mg of lansoprazole delayed-release capsules once daily) study of 284 patients with endoscopically documented duodenal ulcer, the percentage of patients healed after two and four weeks was significantly higher with all doses of lansoprazole delayed-release capsules than with placebo. There was no evidence of a greater or earlier response with the two higher doses compared with lansoprazole delayed-release capsules 15 mg. Based on this study and the second study described below, the recommended dose of lansoprazole delayed-release capsules in duodenal ulcer is 15 mg per day (Table 7).
Table 7: Duodenal Ulcer Healing Rates Lansoprazole Placebo Week 15 mg daily 30 mg daily 60 mg daily (N=68) (N=74) (N=70) (N=72) *(p≤0.001) versus placebo. 2 42.4% * 35.6% * 39.1% * 11.3% 4 89.4% * 91.7% * 89.9% * 46.1% Lansoprazole delayed-release capsules 15 mg was significantly more effective than placebo in relieving day and nighttime abdominal pain and in decreasing the amount of antacid taken per day.
In a second U.S. multicenter study, also double-blind, placebo-controlled, dose-comparison (15 and 30 mg of lansoprazole delayed-release capsules once daily), and including a comparison with ranitidine, in 280 patients with endoscopically documented duodenal ulcer, the percentage of patients healed after four weeks was significantly higher with both doses of lansoprazole delayed-release capsules than with placebo. There was no evidence of a greater or earlier response with the higher dose of lansoprazole delayed-release capsules. Although the 15 mg dose of lansoprazole delayed-release capsules was superior to ranitidine at 4 weeks, the lack of significant difference at 2 weeks and the absence of a difference between 30 mg of lansoprazole delayed-release capsules and ranitidine leaves the comparative effectiveness of the two agents undetermined (Table 8). [See Indications and Usage (1.1)]
Table 8: Duodenal Ulcer Healing Rates Lansoprazole Ranitidine Placebo Week 15 mg daily 30 mg daily 300 mg h.s. (N=80) (N=77) (N=82) (N=41) *(p≤0.05) versus placebo and ranitidine. †(p≤0.05) versus placebo. 2 35% 44.2% 30.5% 34.2% 4 92.3% * 80.3% † 70.5% † 47.5% H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Randomized, double-blind clinical studies performed in the U.S. in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) evaluated the efficacy of lansoprazole delayed-release capsules in combination with amoxicillin capsules and clarithromycin tablets as triple 14 day therapy or in combination with amoxicillin capsules as dual 14 day therapy for the eradication of H. pylori. Based on the results of these studies, the safety and efficacy of two different eradication regimens were established:
Triple therapy: Lansoprazole delayed-release capsules 30 mg twice daily / amoxicillin 1 gm twice daily / clarithromycin 500 mg twice daily
Dual therapy: Lansoprazole delayed-release capsules 30 mg three times daily / amoxicillin 1 gm three times daily
All treatments were for 14 days. H. pylori eradication was defined as two negative tests (culture and histology) at 4 to 6 weeks following the end of treatment. Triple therapy was shown to be more effective than all possible dual therapy combinations. Dual therapy was shown to be more effective than both monotherapies. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence. A randomized, double-blind clinical study performed in the U.S. in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) compared the efficacy of lansoprazole triple therapy for 10 and 14 days. This study established that the 10-day triple therapy was equivalent to the 14-day triple therapy in eradicating H. pylori (Tables 9 and 10). [See Indications and Usage (1.2)]
Table 9 H. pylori Eradication Rates – Triple Therapy (Lansoprazole/ amoxicillin/clarithromycin) Percent of Patients Cured
[95% Confidence Interval]
(Number of patients)
Study Duration Triple Therapy Evaluable Analysis* Triple Therapy Intent-to-Treat Analysis# M93-131 14 days 92† [80-97.7] (N=48) 86† [73.3-93.5] (N=55) M95-392 14 days 86‡ [75.7-93.6] (N=66) 83‡ [72-90.8] (N=70) M95-399+ 14 days 85 [77-91] (N=113) 82 [73.9-88.1] (N=126) 10 days 84 [76-89.8] (N=123) 81 [73.9-87.6] (N=135) *Based on evaluable patients with confirmed duodenal ulcer (active or within one year) and H. pylori infection at baseline defined as at least two of three positive endoscopic tests from CLOtest, histology and/or culture. Patients were included in the analysis if they completed the study. Additionally, if patients dropped out of the study due to an adverse event related to the study drug, they were included in the evaluable analysis as failures of therapy.
#Patients were included in the analysis if they had documented H. pylori infection at baseline as defined above and had a confirmed duodenal ulcer (active or within one year). All dropouts were included as failures of therapy.
†(p<0.05) versus lansoprazole /amoxicillin and lansoprazole /clarithromycin dual therapy.
‡(p<0.05) versus clarithromycin/amoxicillin dual therapy.
+The 95% confidence interval for the difference in eradication rates, 10-day minus 14-day is (-10.5, 8.1) in the evaluable analysis and (-9.7, 9.1) in the intent-to-treat analysis.
Table 10 H. pylori Eradication Rates – 14-Day Dual Therapy (lansoprazole /amoxicillin) Percent of Patients Cured
[95% Confidence Interval]
(Number of patients)
Study Dual Therapy Evaluable Analysis* Dual Therapy Intent-to-Treat Analysis# M93-131 77† [62.5-87.2] (N=51) 70† [56.8-81.2] (N=60) M93-125 66‡ [51.9-77.5] (N=58) 61‡ [48.5-72.9] (N=67) * Based on evaluable patients with confirmed duodenal ulcer (active or within one year) and H. pylori infection at baseline defined as at least two of three positive endoscopic tests from CLOtest, histology and/or culture. Patients were included in the analysis if they completed the study. Additionally, if patients dropped out of the study due to an adverse event related to the study drug, they were included in the analysis as failures of therapy.
# Patients were included in the analysis if they had documented H. pylori infection at baseline as defined above and had a confirmed duodenal ulcer (active or within one year). All dropouts were included as failures of therapy.
† (p<0.05) versus lansoprazole alone.
‡ (p<0.05) versus lansoprazole alone or amoxicillin alone.
Long-Term Maintenance Treatment of Duodenal Ulcers
lansoprazole delayed-release capsules has been shown to prevent the recurrence of duodenal ulcers. Two independent, double-blind, multicenter, controlled trials were conducted in patients with endoscopically confirmed healed duodenal ulcers. Patients remained healed significantly longer and the number of recurrences of duodenal ulcers was significantly less in patients treated with lansoprazole delayed-release capsules than in patients treated with placebo over a 12-month period (Table 11). [See Indications and Usage (1.3)]
Table 11: Endoscopic Remission Rates Trial Drug No. of Pts. Percent in Endoscopic Remission 0-3 mo. 0-6 mo. 0-12 mo. %=Life Table Estimate *(p≤0.001) versus placebo. #1 lansoprazole delayed-release capsules 15 mg daily 86 90% * 87% * 84% * Placebo 83 49% 41% 39% #2 lansoprazole delayed-release capsules 30 mg daily 18 94% * 94% * 85% * lansoprazole delayed-release capsules 15 mg daily 15 87% * 79% * 70% * Placebo 15 33% 0% 0% In trial #2, no significant difference was noted between lansoprazole delayed-release capsules 15 mg and 30 mg in maintaining remission.
Gastric Ulcer
In a U.S. multicenter, double-blind, placebo-controlled study of 253 patients with endoscopically documented gastric ulcer, the percentage of patients healed at four and eight weeks was significantly higher with lansoprazole delayed-release capsules 15 mg and 30 mg once a day than with placebo (Table 12). [See Indications and Usage (1.4)]
Table 12: Gastric Ulcer Healing Rates Lansoprazole Placebo Week 15 mg daily 30 mg daily 60 mg daily (N=65) (N=63) (N=61) (N=64) *(p≤0.05) versus placebo. 4 64.6% * 58.1% * 53.3% * 37.5% 8 92.2% * 96.8% * 93.2% * 76.7% Patients treated with any lansoprazole delayed-release capsules dose reported significantly less day and night abdominal pain along with fewer days of antacid use and fewer antacid tablets used per day than the placebo group.
Independent substantiation of the effectiveness of lansoprazole delayed-release capsules 30 mg was provided by a meta-analysis of published and unpublished data.
Healing of NSAID-Associated Gastric Ulcer
In two U.S. and Canadian multicenter, double-blind, active-controlled studies in patients with endoscopically confirmed NSAID-associated gastric ulcer who continued their NSAID use, the percentage of patients healed after 8 weeks was statistically significantly higher with 30 mg of lansoprazole delayed-release capsules than with the active control. A total of 711 patients were enrolled in the study, and 701 patients were treated. Patients ranged in age from 18 to 88 years (median age 59 years), with 67% female patients and 33% male patients. Race was distributed as follows: 87% Caucasian, 8% Black, 5% Other. There was no statistically significant difference between lansoprazole delayed-release capsules 30 mg daily and the active control on symptom relief (i.e., abdominal pain) (Table 13). [See Indications and Usage (1.5)]
Table 13: NSAID-Associated Gastric Ulcer Healing Rates * *Actual observed ulcer(s) healed at time points + 2 days †Dose for healing of gastric ulcer ‡(p≤0.05) versus the active control Study #1 Lansoprazole Active Control † 30 mg daily Week 4 60% (53/88) ‡ 28% (23/83) Week 8 79% (62/79) ‡ 55% (41/74) Study #2 Lansoprazole Active Control † 30 mg daily Week 4 53% (40/75) 38% (31/82) Week 8 77% (47/61) ‡ 50% (33/66) Risk Reduction of NSAID-Associated Gastric Ulcer
In one large U.S., multicenter, double-blind, placebo- and misoprostol-controlled (misoprostol blinded only to the endoscopist) study in patients who required chronic use of an NSAID and who had a history of an endoscopically documented gastric ulcer, the proportion of patients remaining free from gastric ulcer at 4, 8, and 12 weeks was significantly higher with 15 or 30 mg of lansoprazole than placebo. A total of 537 patients were enrolled in the study, and 535 patients were treated. Patients ranged in age from 23 to 89 years (median age 60 years), with 65% female patients and 35% male patients. Race was distributed as follows: 90% Caucasian, 6% Black, 4% other. The 30 mg dose of lansoprazole demonstrated no additional benefit in risk reduction of the NSAID-associated gastric ulcer than the 15 mg dose (Table 14). [See Indications and Usage (1.6)]
Table 14: Proportion of Patients Remaining Free of Gastric Ulcers * Lansoprazole Lansoprazole Misoprostol Placebo 15 mg daily 30 mg daily 200 mcg four times daily Week (N=121) (N=116) (N=106) (N=112) (p<0.001) Lansoprazole 15 mg daily versus placebo;Lansoprazole 30 mg daily versus placebo; and misoprostol 200 mcg four times daily versus placebo.
(p<0.05) Misoprostol 200 mcg four times daily versus Lansoprazole 15 mg daily; and misoprostol 200 mcg four times daily versus Lansoprazole 30 mg daily.*% = Life Table Estimate 4 90% 92% 96% 66% 8 86% 88% 95% 60% 12 80% 82% 93% 51% Gastroesophageal Reflux Disease (GERD)
Symptomatic GERD: In a U.S. multicenter, double-blind, placebo-controlled study of 214 patients with frequent GERD symptoms, but no esophageal erosions by endoscopy, significantly greater relief of heartburn associated with GERD was observed with the administration of lansoprazole 15 mg once daily up to 8 weeks than with placebo. No significant additional benefit from lansoprazole 30 mg once daily was observed.
The intent-to-treat analyses demonstrated significant reduction in frequency and severity of day and night heartburn. Data for frequency and severity for the 8-week treatment period are presented in Table 15 and in Figures 1 and 2:
Table 15: Frequency of Heartburn Variable Placebo
(n=43)Lansoprazole 15 mg
(n=80)Lansoprazole 30 mg
(n=86)Median *(p<0.01) versus placebo. % of Days without Heartburn Week 1 0% 71% * 46% * Week 4 11% 81% * 76% * Week 8 13% 84% * 82% * % of Nights without Heartburn Week 1 17% 86% * 57% * Week 4 25% 89% * 73% * Week 8 36% 92% * 80% * Figure 1 Figure 2 In two U.S., multicenter double-blind, ranitidine-controlled studies of 925 total patients with frequent GERD symptoms, but no esophageal erosions by endoscopy, lansoprazole 15 mg was superior to ranitidine 150 mg (twice daily) in decreasing the frequency and severity of day and night heartburn associated with GERD for the 8-week treatment period. No significant additional benefit from lansoprazole 30 mg once daily was observed. [See Indications and Usage (1.7)]
Erosive Esophagitis
In a U.S. multicenter, double-blind, placebo-controlled study of 269 patients entering with an endoscopic diagnosis of esophagitis with mucosal grading of 2 or more and grades 3 and 4 signifying erosive disease, the percentages of patients with healing are presented in Table 16:
Table 16: Erosive Esophagitis Healing Rates Lansoprazole Placebo 15 mg daily 30 mg daily 60 mg daily Week (N=69) (N=65) (N=72) (N=63) *(p≤0.001) versus placebo. †(p≤0.05) versus lansoprazole 15 mg. 4 67.6% * 81.3% *† 80.6% *† 32.8% 6 87.7% * 95.4% * 94.3% * 52.5% 8 90.9% * 95.4% * 94.4% * 52.5% In this study, all lansoprazole groups reported significantly greater relief of heartburn and less day and night abdominal pain along with fewer days of antacid use and fewer antacid tablets taken per day than the placebo group.
Although all doses were effective, the earlier healing in the higher two doses suggests 30 mg daily as the recommended dose.
Lansoprazole was also compared in a U.S. multicenter, double-blind study to a low dose of ranitidine in 242 patients with erosive reflux esophagitis.Lansoprazoles at a dose of 30 mg was significantly more effective than ranitidine 150 mg twice daily as shown below (Table 17).
Table 17: Erosive Esophagitis Healing Rates Week Lansoprazole
30 mg daily
(N=115)Ranitidine
150 mg twice daily
(N=127)*(p≤0.001) versus ranitidine. 2 66.7% * 38.7% 4 82.5% * 52% 6 93% * 67.8% 8 92.1% * 69.9% In addition, patients treated with lansoprazole reported less day and nighttime heartburn and took less antacid tablets for fewer days than patients taking ranitidine 150 mg twice daily.
Although this study demonstrates effectiveness of lansoprazole in healing erosive esophagitis, it does not represent an adequate comparison with ranitidine because the recommended ranitidine dose for esophagitis is 150 mg four times daily, twice the dose used in this study.
In the two trials described and in several smaller studies involving patients with moderate to severe erosive esophagitis, lansoprazole produced healing rates similar to those shown above.
In a U.S. multicenter, double-blind, active-controlled study, 30 mg of lansoprazole was compared with ranitidine 150 mg twice daily in 151 patients with erosive reflux esophagitis that was poorly responsive to a minimum of 12 weeks of treatment with at least one H2-receptor antagonist given at the dose indicated for symptom relief or greater, namely, cimetidine 800 mg/day, ranitidine 300 mg/day, famotidine 40 mg/day or nizatidine 300 mg/day. Lansoprazole 30 mg was more effective than ranitidine 150 mg twice daily in healing reflux esophagitis, and the percentage of patients with healing were as follows. This study does not constitute a comparison of the effectiveness of histamine H2-receptor antagonists with lansoprazole , as all patients had demonstrated unresponsiveness to the histamine H2-receptor antagonist mode of treatment. It does indicate, however, that lansoprazole may be useful in patients failing on a histamine H2-receptor antagonist (Table 18). [See Indications and Usage (1.7)]
Table 18: Reflux Esophagitis Healing Rates in Patients Poorly Responsive to Histamine H2-Receptor Antagonist Therapy Week Lansoprazole
30 mg daily
(N=100)Ranitidine
150 mg twice daily
(N=51)*(p≤0.001) versus ranitidine. 4 74.7% * 42.6% 8 83.7% * 32% Long-Term Maintenance Treatment of Erosive Esophagitis
Two independent, double-blind, multicenter, controlled trials were conducted in patients with endoscopically confirmed healed esophagitis. Patients remained in remission significantly longer and the number of recurrences of erosive esophagitis was significantly less in patients treated with lansoprazole than in patients treated with placebo over a 12-month period (Table 19).
Table 19: Endoscopic Remission Rates Percent in Endoscopic Remission Trial Drug No. of Pts. 0-3 mo. 0-6 mo. 0-12 mo. %=Life Table Estimate *(p≤0.001) versus placebo. #1 Lansoprazole 15 mg daily 59 83% * 81% * 79% * Lansoprazole 30 mg daily 56 93% * 93% * 90% * Placebo 55 31% 27% 24% #2 Lansoprazole 15 mg daily 50 74% * 72% * 67% * Lansoprazole 30 mg daily 49 75% * 72% * 55% * Placebo 47 16% 13% 13% Regardless of initial grade of erosive esophagitis, lansoprazole 15 mg and 30 mg were similar in maintaining remission.
In a U.S., randomized, double-blind, study, lansoprazole 15 mg daily (n = 100) was compared with ranitidine 150 mg twice daily (n = 106), at the recommended dosage, in patients with endoscopically-proven healed erosive esophagitis over a 12-month period. Treatment with lansoprazoles resulted in patients remaining healed (Grade 0 lesions) of erosive esophagitis for significantly longer periods of time than those treated with ranitidine (p<0.001). In addition, lansoprazoles was significantly more effective than ranitidine in providing complete relief of both daytime and nighttime heartburn. Patients treated with lansoprazoles remained asymptomatic for a significantly longer period of time than patients treated with ranitidine. [See Indications and Usage (1.8)]
Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
In open studies of 57 patients with pathological hypersecretory conditions, such as Zollinger-Ellison syndrome (ZES) with or without multiple endocrine adenomas, lansoprazole significantly inhibited gastric acid secretion and controlled associated symptoms of diarrhea, anorexia and pain. Doses ranging from 15 mg every other day to 180 mg per day maintained basal acid secretion below 10 mEq/hr in patients without prior gastric surgery and below 5 mEq/hr in patients with prior gastric surgery.
Initial doses were titrated to the individual patient need, and adjustments were necessary with time in some patients. [See Dosage and Administration (2.1)] lansoprazole was well tolerated at these high dose levels for prolonged periods (greater than four years in some patients). In most ZES patients, serum gastrin levels were not modified by lansoprazole. However, in some patients, serum gastrin increased to levels greater than those present prior to initiation of lansoprazole therapy. [See Indications and Usage (1.9)]
REFERENCES SECTION
0.1 National Committee for Clinical Laboratory Standards. Summary Minutes, Subcommittee on Antimicrobial Susceptibility Testing, Tampa, FL, January 11-13, 1998.
HOW SUPPLIED SECTION
Lansoprazole delayed release capsules USP, 15 mg are white to pale yellow colored enteric coated pellets filled in size ‘3’ hard gelatin capsules with opaque pink colored cap and opaque green colored body, imprinted ‘RDY’ on cap and ‘LAN’ on body with white ink. They are supplied in bottles of 30’s, 60’s, 90's,100’s, 500’s and unit dose package of 10 (1 x 10).
Bottles of 30 NDC 55111-398-30
Bottles of 60 NDC 55111-398-60
Bottles of 90 NDC 55111-398-90
Bottles of 100 NDC 55111-398-01
Bottles of 500 NDC 55111-398-05
Unit Dosage Package of 10 (1x10) NDC 55111-398-79
Lansoprazole delayed release capsules USP, 30 mg are white to pale yellow colored enteric coated pellets filled in size ‘1’ hard gelatin capsules with opaque pink colored cap and opaque black colored body, imprinted ‘RDY’ on cap and ‘399’ on body with white ink. They are supplied in bottles of 30’s, 60’s, 90's, 100’s, 500’s and unit dose package of 10 (1 x 10).
Bottles of 30 NDC 55111-399-30
Bottles of 60 NDC 55111-399-60
Bottles of 90 NDC 55111-399-90
Bottles of 100 NDC 55111-399-01
Bottles of 500 NDC 55111-399-05
Unit Dosage Package of 10 (1x10) NDC 55111-399-79
Store at 20°–25° C (68°–77° F); [See USP Controlled Room Temperature].
INFORMATION FOR PATIENTS SECTION
[See FDA-Approved Medication Guide and Patient Instructions for Use]
Patient should be informed of the following:
Advise patients to immediately report and seek care for diarrhea that does not improve. This may be a sign of Clostridium difficile associated diarrhea [see Warnings and Precautions (5.2)].
Advise patients to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia [see Warnings and Precautions (5.4)].
Information for Patients
Lansoprazole is available as a capsule and is available in 15 mg and 30 mg strengths. Directions for use specific to the route and available methods of administration is presented below. [See Dosage and Administration (2.3)]
Lansoprazole should be taken before eating.
Lansoprazole products SHOULD NOT BE CRUSHED OR CHEWED.
Administration Options
1 Lansoprazole Delayed-Release Capsules
Lansoprazole delayed-release capsules should be swallowed whole.
Alternatively, for patients who have difficulty swallowing capsules, lansoprazole delayed-release capsules can be opened and administered as follows:
o Open capsule.
o Sprinkle intact granules on one tablespoon of either applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
o Swallow immediately.
Lansoprazole
o Open capsule.
o Sprinkle intact granules into a small volume of either apple juice, orange juice or tomato juice (60 mL – approximately 2 ounces).
o Mix briefly.
o Swallow immediately.
o To ensure complete delivery of the dose, the glass should be rinsed with two or more volumes of juice and the contents swallowed immediately.
Lansoprazole delayed-release capsules – Nasogastric Tube (≥16 French) Administration
For patients who have a nasogastric tube in place, lansoprazole delayed-release capsules can be administered as follows:
o Open capsule.
o Mix intact granules into 40 mL of apple juice. DO NOT USE OTHER LIQUIDS.
o Inject through the nasogastric tube into the stomach.
o Flush with additional apple juice to clear the tube.
USE IN OTHER FOODS AND LIQUIDS HAS NOT BEEN STUDIED CLINICALLY AND IS THEREFORE NOT RECOMMENDED.
SPL MEDGUIDE SECTION
-
MEDICATION GUIDE
Lansoprazole Delayed-Release Capsules, USP
Read this Medication Guide before you start taking lansoprazole delayed-release capsules and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment.
What is the most important information that I should know about lansoprazole delayed-release capsules?
Lansoprazole delayed-release capsules may help your acid-related symptoms, but you could still have serious stomach problems. Talk with your doctor.
Lansoprazole delayed-release capsules can cause serious side effects, including:
- Diarrhea. Lansoprazole delayed-release capsules may increase your risk of getting severe diarrhea. This diarrhea may be caused by an infection (Clostridium difficile) in your intestines. Call your doctor right away if you have watery stool, stomach pain, and fever that does not go away.
- Bone fractures. People who take multiple daily doses of proton pump inhibitor medicines for a long period of time (a year or longer) may have an increased risk of fractures of the hip, wrist or spine. You should take lansoprazole delayed-release capsules exactly as prescribed, at the lowest dose possible for your treatment and for the shortest time needed. Talk to your doctor about your risk of bone fracture if you take lansoprazole delayed-release capsules.
Lansoprazole delayed-release capsules can have other serious side effects. See “What are the possible side effects of lansoprazole delayed-release capsules?”
What are lansoprazole delayed-release capsules?
Lansoprazole delayed-release capsules are prescription medicine called a proton pump inhibitor (PPI). Lansoprazole delayed-release capsules reduces the amount of acid in your stomach.
Lansoprazole delayed-release capsules are used in adults:
- for 4 weeks for the healing and symptom relief of duodenal ulcers. The duodenal area is the area where food passes when it leaves the stomach.
- with certain antibiotics to treat an infection called H. pylori. Sometimes H. pylori bacteria can cause duodenal ulcers. The infection needs to be treated to prevent ulcers from coming back.
- for continued healing of duodenal ulcers. for up to 8 weeks to heal stomach ulcers.
- for up to 8 weeks to heal stomach ulcers in some people taking pain medicines called non-steroidal anti-inflammatory drugs (NSAIDs).
- for reducing the risk of stomach ulcers in some people taking NSAIDs.
- for up to 8 weeks for the relief of heartburn and other symptoms of gastroesophageal reflux disease (GERD).
- GERD happens when acid in your stomach backs up into the tube (esophagus) that connects your mouth to your stomach. This may cause a burning feeling in your chest or throat, sour taste or burping.
- for 8 weeks to heal the acid-related damage to the lining of the esophagus (called erosive esophagitis) and to relieve symptoms. If needed, your doctor may prescribe another 8 weeks of lansoprazole delayed-release capsules.
- for continued healing of erosive esophagitis.
- for the long-term treatment of conditions where your stomach makes too much acid. This includes a condition called Zollinger-Ellison syndrome.
Lansoprazole delayed-release capsules are used in children and adolescents (ages 1 to 17):
- for up to 12 weeks to treat GERD and erosive esophagitis in children 1 to 11 years old.
- for up to 8 weeks to treat GERD and erosive esophagitis in adolescents 12 to 17 years old.
Lansoprazole delayed-release capsules are not effective for symptoms of GERD in children under the age of 1 year.
Who should not take lansoprazole delayed-release capsules?
- Do not take lansoprazole delayed-release capsules if you are allergic to lansoprazole or any of the other ingredients in lansoprazole delayed-release capsules. See the end of this Medication Guide for a complete list of ingredients in lansoprazole delayed-release capsules.
What should I tell my doctor before taking lansoprazole delayed-release capsules?
Before you take lansoprazole delayed-release capsules, tell your doctor if you:
- have been told that you have low magnesium levels in your blood.
- have liver problems
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if lansoprazole delayed-release capsules will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if lansoprazole delayed-release capsules passes into your breast milk. You and your doctor should decide if you will take lansoprazole delayed-release capsules or breastfeed. You should not do both. Talk to your doctor about the best way to feed your baby if you take lansoprazole delayed-release capsules.
Tell your doctor about all the medicines you take, including prescription and non-prescription drugs, vitamins, and herbal supplements. Lansoprazole delayed-release capsules may affect how other medicines work, and other medicines may affect how lansoprazole delayed-release capsules works.
Especially tell your doctor if you take:
- atazanavir (Reyataz)
- erlotinib (Tarceva)
- digoxin (Lanoxin)
- a product that contains iron
- ketoconazole (Nizoral)
- warfarin (Coumadin, Jantoven)
- tacrolimus (Prograf)
- theophylline (Theo-24, Elixophyllin, Theochron, Theolair)
- an antibiotic that contains ampicillin or clarithromycin
- methotrexate
- mycophenolate mofetil (Cellcept)
Ask your doctor or pharmacist for a list of these medicines if you are not sure.
Know the medicines that you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take lansoprazole delayed-release capsules?
- Take lansoprazole delayed-release capsules exactly as prescribed by your doctor.
- Do not change your dose or stop taking lansoprazole delayed-release capsules without talking to your doctor.
- You should take lansoprazole delayed-release capsules before eating.
- Lansoprazole Delayed-Release Capsules:
- You should swallow lansoprazole delayed-release capsules whole.
- Do not crush or chew lansoprazole delayed-release capsules.
- If you have trouble swallowing a whole capsule, you can open the capsule and take the contents with certain foods or juices. See the “Instructions for Use” at the end of this Medication Guide for instructions on how to take lansoprazole delayed-release capsules with certain foods and juices.
- See the “Instructions for Use” at the end of this Medication Guide for instructions on how to mix and give lansoprazole delayed-release capsules through a nasogastric tube.
- If you miss a dose, take it as soon as you remember. If it is almost time for your next dose, skip the missed dose. Just take the next dose at your regular time. Do not take 2 doses at the same time.
- If you take too much lansoprazole delayed-release capsules, call your doctor right away.
What are the possible side effects of lansoprazole delayed-release capsules?
Lansoprazole delayed-release capsules can cause serious side effects, including:
See “What is the most important information that I should know about lansoprazole delayed-release capsules?”
- Vitamin B12 deficiency. Lansoprazole delayed-release capsules reduces the amount of acid in your stomach. Stomach acid is needed to absorb vitamin B12 properly. Talk with your doctor about the possibility of vitamin B12 deficiency if you have been on lansoprazole delayed-release capsules for a long time (more than 3 years).
- Low magnesium levels in your body. This problem can be serious. Low magnesium can happen in some people who take a proton pump inhibitor medicine for at least 3 months. If low magnesium levels happen, it is usually after a year of treatment. You may or may not have symptoms of low magnesium.
Tell your doctor right away if you develop any of these symptoms:
- seizures
- dizziness
- abnormal or fast heartbeat
- jitteriness
- jerking movements or shaking (tremors)
- muscle weakness
- spasms of the hands and feet
- cramps or muscle aches
- spasm of the voice box
Your doctor may check the level of magnesium in your body before you start taking lansoprazole delayed-release capsules, or during treatment; if you will be taking lansoprazole delayed-release capsules for a long period of time.
The most common side effects of lansoprazole delayed-release capsules in adults and children include:
- diarrhea
- stomach pain
- nausea
- constipation
- headache
Other side effects:
- Serious allergic reactions. Tell your doctor if you get any of the following symptoms with lansoprazole delayed-release capsules.
- rash face swelling throat tightness difficulty breathing
Your doctor may stop lansoprazole delayed-release capsules if these symptoms happen.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of lansoprazole delayed-release capsules. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store lansoprazole delayed-release capsules?
- Store lansoprazole delayed-release capsules at room temperature between 20° to 25° C (68° to 77° F)
Keep lansoprazole delayed-release capsules and all medicines out of the reach of children.
General information about lansoprazole delayed-release capsules
Medicines are sometimes prescribed for conditions other than those listed in a Medication Guide. Do not use lansoprazole delayed-release capsules for conditions for which it was not prescribed. Do not give lansoprazole delayed-release capsules to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about lansoprazole delayed-release capsules. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about lansoprazole delayed-release capsules that is written for healthcare professionals.
For more information, call 1-888-375-3784.
What are the ingredients in lansoprazole delayed-release capsules?
Active ingredient: lansoprazole.
Inactive ingredients in lansoprazole delayed-release capsules:
Ammonium hydroxide, hydroxypropyl cellulose, low substituted hydroxypropyl cellulose, magnesium carbonate, methacrylic acid copolymer, polyethylene glycol, polysorbate 80, propylene glycol, shellac, simethicone, starch, sucrose, sugar spheres, talc, and titanium dioxide.
Components of the gelatin capsule include gelatin, iron oxide red, iron oxide yellow, FD&C Blue 2, sodium lauryl sulphate and titanium dioxide for 15 mg capsules and gelatin, iron oxide black, iron oxide red, iron oxide yellow, sodium lauryl sulphate and titanium dioxide for 30 mg capsules.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Patient Instructions for Use
Lansoprazole Delayed-Release Capsules USP
Lansoprazole Delayed-Release Capsules
- Swallow lansoprazole delayed-release capsules whole. Do not crush or chew them.
- You should take lansoprazole delayed-release capsules before eating.
- Lansoprazole Delayed-Release Capsule with certain food:
You can only use applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
1. Open the capsule.
2. Sprinkle the granules on 1 tablespoon of either applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
3. Swallow right away.
- Lansoprazole Delayed-Release Capsule with certain juices:
You can only use apple juice, orange juice or tomato juice.
1 Open the capsule.
2 Sprinkle the granules into 60 mL (about ¼ cup) of either apple juice, orange juice or tomato juice.
3 Stir.
4 Swallow right away.
5 To make sure that the entire dose is taken, rinse the glass with 1/2 cup or more of juice to get out any leftover granules. Swallow the juice right away.
- Lansoprazole Delayed-Release Capsules through a nasogastric tube (NG tube) 16 French or larger, as prescribed by your doctor:
You can only use apple juice.
1 Open the capsule and empty the granules into a syringe.
2 Do not break or crush the granules.
3 Mix with 40 mL of apple juice. Do not use other liquids.
4 Attach the syringe to the NG tube and give the medicine in the syringe through the NG tube into the stomach.
5 After giving the granules, flush the NG tube with more apple juice to clear the tube.
Lansoprazole delayed-release capsules should not be used in foods or liquids not listed above.
How should I store lansoprazole delayed-release capsules?
- Store lansoprazole delayed-release capsules at room temperature between 20° to 25° C (68° to 77° F)
Keep lansoprazole delayed-release capsules and all medicines out of the reach of children.
This instruction for Use has been approved by the U.S. Food and Drug Administration.
To reorder additional Medication Guides, please contact Dr. Reddy's Customer Service at 1-866-733-3952.
All trademark names are the property of their respective owners.
Rx Only
Manufactured by:
Dr. Reddy’s Laboratories Limited
Bachupally – 500 090 INDIA
Revised: 0115