FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions for Using the Glucagon Emergency Kit for Low Blood Sugar to Treat Severe Hypoglycemia
Glucagon for Injection is for subcutaneous, intramuscular, or intravenous injection. Administer intravenously ONLY under medical supervision.
Instruct patients and their caregivers on the signs and symptoms of severe hypoglycemia. Because severe hypoglycemia requires the help of others to recover, instruct the patient to inform those around them about Glucagon for Injection and its Instructions for Use. Administer Glucagon for Injection as soon as possible when severe hypoglycemia is recognized.
Instruct the patient or caregiver to read the Instructions for Use at the time they receive a prescription for Glucagon for Injection. Emphasize the following instructions to the patient or caregiver:
- Using the supplied prefilled syringe, carefully insert the needle through the rubber stopper of the vial containing Glucagon for Injection powder and inject all the liquid from the syringe into the vial.
- Shake the vial gently until the powder is completely dissolved and no particles remain in the fluid. The reconstituted solution should be clear and colorless. Inspect visually for particulate matter and discoloration. If the resulting solution is cloudy or contains particulate matter do not use.
- The reconstituted solution is 1 mg per mL glucagon.
- Immediately after reconstitution, inject the solution subcutaneously or intramuscularly in the upper arm, thigh, or buttocks. In addition, healthcare providers may administer intravenously.
- Call for emergency assistance immediately after administering the dose.
- When the patient has responded to the treatment and is able to swallow, give oral carbohydrates to restore the liver glycogen and prevent recurrence of hypoglycemia.
- Discard any unused portion.
2.2 Dosage in Adults and Pediatric Patients for Using the Glucagon Emergency Kit for Low Blood Sugar to Treat Severe Hypoglycemia
Adults and Pediatric Patients Weighing More Than 25 kg or for Pediatric Patients with Unknown Weight 6 Years and Older
- The recommended dosage is 1 mg (1 mL) injected subcutaneously or intramuscularly into the upper arm, thigh, or buttocks, or intravenously.
- If there has been no response after 15 minutes, an additional 1 mg dose (1 mL) of Glucagon for Injection may be administered using a new kit while waiting for emergency assistance.
Pediatric Patients Weighing Less Than 25 kg or for Pediatric Patients with Unknown Weight Less Than 6 Years of Age
- The recommended dosage is 0.5 mg (0.5 mL) injected subcutaneously or intramuscularly into the upper arm, thigh, or buttocks, or intravenously.
- If there has been no response after 15 minutes, an additional 0.5 mg dose (0.5 mL) of Glucagon for Injection may be administered using a new kit while waiting for emergency assistance.
2.3 Important Administration Instruction for Using Glucagon for Injection Diagnostic Kit and Glucagon for Injection Single-Dose Vial as a Diagnostic Aid
- Reconstitute Glucagon for Injection with 1 mL of Sterile Water for Injection. Using a syringe, withdraw all of the Sterile Water for Injection (if supplied) or 1 mL Sterile Water for Injection and inject into the Glucagon for Injection vial.
- Shake the vial gently until the powder is completely dissolved and no particles remain in the fluid. The reconstituted fluid should be clear and colorless. Inspect visually for particulate matter and discoloration. If the resulting solution is cloudy or contains particulate matter do not use.
- The reconstituted solution is 1 mg per mL glucagon.
- Immediately after reconstitution, inject the solution intravenously or intramuscularly into upper arm, thigh, or buttocks.
- Discard any unused portion.
- After the end of the diagnostic procedure, give oral carbohydrates to patients who have been fasting, if this is compatible with the diagnostic procedure.
2.4 Dosage in Adults for Using Glucagon for Injection Diagnostic Kit and Glucagon for Injection Single-Dose Vial as a Diagnostic Aid
- The recommended diagnostic dose for relaxation of the stomach, duodenal bulb, duodenum, and small bowel is 0.2 mg to 0.5 mg administered intravenously or 1 mg administered intramuscularly; the recommended dose to relax the colon is 0.5 mg to 0.75 mg administered intravenously or 1 mg to 2 mg administered intramuscularly [see Clinical Pharmacology (12.2)].
- The onset of action after an injection will depend on the organ under examination and route of administration [see Clinical Pharmacology (12.2)].
3 DOSAGE FORMS AND STRENGTHS
Glucagon for Injection is a white lyophilized powder supplied as follows:
Treatment of Severe Hypoglycemia
- 1 mg single-dose vial of Glucagon for Injection with a 1 mL single-dose syringe of Sterile Water for Injection, USP (Glucagon Emergency Kit for Low Blood Sugar)
Use as a Diagnostic Aid
- 1 mg single-dose vial of Glucagon for Injection
- 1 mg single-dose vial of Glucagon for Injection with a 1 mL single-dose vial of Sterile Water for Injection, USP (Diagnostic Kit)
4 CONTRAINDICATIONS
Glucagon for Injection is contraindicated in patients with:
- Pheochromocytoma [see Warnings and Precautions (5.1)]
- Insulinoma [see Warnings and Precautions (5.2)] because of the risk of hypoglycemia
- Known hypersensitivity to glucagon or any of the excipients in Glucagon for Injection. Allergic reactions have been reported with glucagon and include anaphylactic shock with breathing difficulties and hypotension [see Warnings and Precautions (5.3)]
- Glucagonoma [see Warnings and Precautions (5.8)] because of risk of hypoglycemia when used as a diagnostic aid
5 WARNINGS AND PRECAUTIONS
5.1 Catecholamine Release in Patients with Pheochromocytoma
Glucagon for Injection is contraindicated in patients with pheochromocytoma because glucagon may stimulate the release of catecholamines from the tumor [see Contraindications (4)]. If the patient develops a dramatic increase in blood pressure and a previously undiagnosed pheochromocytoma is suspected, 5 to 10 mg of phentolamine mesylate, administered intravenously, has been shown to be effective in lowering blood pressure.
5.2 Hypoglycemia in Patients with Insulinoma
In patients with insulinoma, administration of glucagon may produce an initial increase in blood glucose; however, Glucagon for Injection administration may directly or indirectly (through an initial rise in blood glucose) stimulate exaggerated insulin release from an insulinoma and cause hypoglycemia. Glucagon for Injection is contraindicated in patients with insulinoma [see Contraindications (4)]. If a patient develops symptoms of hypoglycemia after a dose of Glucagon for Injection, give glucose orally or intravenously.
5.3 Hypersensitivity and Allergic Reactions
Allergic reactions have been reported with glucagon, these include generalized rash, and in some cases anaphylactic shock with breathing difficulties and hypotension. Glucagon for Injection is contraindicated in patients with a prior hypersensitivity reaction [see Contraindications (4)].
5.4 Lack of Efficacy in Patients with Decreased Hepatic Glycogen
Glucagon for Injection is effective in treating hypoglycemia only if sufficient hepatic glycogen is present. Patients in states of starvation, with adrenal insufficiency or chronic hypoglycemia may not have adequate levels of hepatic glycogen for Glucagon for Injection administration to be effective. Patients with these conditions should be treated with glucose.
5.5 Necrolytic Migratory Erythema
Necrolytic migratory erythema (NME), a skin rash commonly associated with glucagonomas (glucagon-producing tumors) and characterized by scaly, pruritic erythematous plaques, bullae, and erosions, has been reported postmarketing following continuous glucagon infusion. NME lesions may affect the face, groin, perineum and legs or be more widespread. In the reported cases NME resolved with discontinuation of the glucagon, and treatment with corticosteroids was not effective. Should NME occur, consider whether the benefits of continuous glucagon infusion outweigh the risks.
5.6 Hyperglycemia in Patients with Diabetes Mellitus when Used as a Diagnostic Aid
Treatment with Glucagon for Injection in patients with diabetes mellitus may cause hyperglycemia. Monitor diabetic patients for changes in blood glucose levels during treatment and treat if indicated.
5.7 Blood Pressure and Heart Rate Increase in Patients with Cardiac Disease when Used as a Diagnostic Aid
Glucagon for Injection may increase myocardial oxygen demand, blood pressure, and pulse rate which may be life-threatening in patients with cardiac disease. Cardiac monitoring is recommended in patients with cardiac disease during use of Glucagon for Injection as a diagnostic aid, and an increase in blood pressure and pulse rate may require therapy.
5.8 Hypoglycemia in Patients with Glucagonoma
Glucagon administered to patients with glucagonoma may cause secondary hypoglycemia. Glucagon for Injection is contraindicated in patients with glucagonoma when used as a diagnostic aid [see Contraindications (4)]. Test patients suspected of having glucagonoma for blood levels of glucagon prior to treatment, and monitor for changes in blood glucose levels during treatment. If a patient develops symptoms of hypoglycemia after a dose of Glucagon for Injection, give glucose orally or intravenously.
6 ADVERSE REACTIONS
The following important adverse reactions are described below and elsewhere in the labeling:
- Hypersensitivity and Allergic Reactions [see Warnings and Precautions (5.3)]
- Necrolytic Migratory Erythema [see Warnings and Precautions (5.5)]
- Hyperglycemia in Patients with Diabetes Mellitus when Used as a Diagnostic Aid [see Warnings and Precautions (5.6)]
- Blood Pressure and Heart Rate Increase in Patients with Cardiac Disease when Used as a Diagnostic Aid [see Warnings and Precautions (5.7)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in clinical trials of another drug and may not reflect the rates observed in practice.
In a randomized single-blind clinical study of Glucagon for Injection, 29 healthy subjects received a single dose of 1 mg Glucagon for Injection intramuscularly. Table 1 shows the most common adverse reactions that were not present at baseline and occurred in at least 5% of patients.
| Glucagon for Injection (N=29) % of Patients |
|
| Nausea | 17 |
| Vomiting | 7 |
In a randomized, single-blind clinical study of Glucagon for Injection, 31 healthy subjects received a single dose of 1 mg Glucagon for Injection subcutaneously. Table 2 shows the most common adverse reactions that were not present at baseline and occurred in at least 5% of patients. (2.1)].
| Glucagon for Injection (N=31) % of Patients |
|
| Injection site swelling | 58 |
| Injection site erythema | 55 |
| Vomiting | 36 |
| Nausea | 32 |
| Decreased blood pressure | 23 |
| Asthenia | 23 |
| Headache | 13 |
| Dizziness | 10 |
| Pallor | 10 |
| Diarrhea | 7 |
| Somnolence | 7 |
6.2 Postmarketing Experience
Additional adverse reactions have been identified during post-approval use of glucagon. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- hypoglycemia and hypoglycemic coma. Patients taking indomethacin may be more likely to experience hypoglycemia following glucagon administration [see Drug Interactions (7)].
- Necrolytic migratory erythema (NME) cases have been reported postmarketing in patients receiving continuous infusion of glucagon.
7 DRUG INTERACTIONS
7.1
| Beta-Blockers | |
| Clinical Impact: | Patients taking beta-blockers may have a transient increase in pulse and blood pressure when given Glucagon for Injection. |
| Intervention: | The increase in blood pressure and heart rate may require therapy in patients with coronary artery disease. |
| Indomethacin | |
| Clinical Impact: | In patients taking indomethacin, Glucagon for Injection may lose its ability to raise blood glucose or may even produce hypoglycemia. |
| Intervention: | Monitor blood glucose levels during glucagon treatment of patients taking indomethacin. |
| Anticholinergic Drugs | |
| Clinical Impact: | The concomitant use of anticholinergic drugs and Glucagon for Injection increases the risk of gastrointestinal adverse reactions due to additive effects on inhibition of gastrointestinal motility. |
| Intervention: | Concomitant use of anticholinergic drugs with Glucagon for Injection for use as a diagnostic aid is not recommended. |
| Warfarin | |
| Clinical Impact: | Glucagon for Injection may increase the anticoagulant effect of warfarin. |
| Intervention: | Monitor patients for unusual bruising or bleeding, as adjustments in warfarin dosage may be required. |
| Insulin | |
| Clinical Impact: | Insulin acts antagonistically to glucagon. |
| Intervention: | Monitor blood glucose when Glucagon for Injection is used as a diagnostic aid in patients receiving insulin. |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from case reports and a small number of observational studies with glucagon use in pregnant women over decades of use have not identified a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Multiple small studies have demonstrated a lack of transfer of pancreatic glucagon across the human placental barrier during early gestation. In rat and rabbit reproduction studies, no embryofetal toxicity was observed with glucagon administered by injection during the period of organogenesis at doses representing up to 100 and 200 times the human dose, respectively, based on body surface area (mg/m2) (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
8.2 Lactation
Risk Summary
There is no information available on the presence of glucagon in human or animal milk, the effects of glucagon on the breastfed child or the effects of glucagon on milk production. However, glucagon is a peptide and would be expected to be broken down to its constituent amino acids in the infant's digestive tract and is therefore, unlikely to cause harm to an exposed infant.
8.4 Pediatric Use
The safety and effectiveness of Glucagon for Injection for the treatment of severe hypoglycemia in pediatric patients with diabetes have been established.
Safety and effectiveness for use as a diagnostic aid during radiologic examinations to temporarily inhibit movement of the gastrointestinal tract in pediatric patients have not been established.
10 OVERDOSAGE
If overdosage occurs, the patient may experience nausea, vomiting, inhibition of GI tract motility, increase in blood pressure and pulse rate. In case of suspected overdosing, the serum potassium may decrease and should be monitored and corrected if needed. If the patient develops a dramatic increase in blood pressure, phentolamine mesylate has been shown to be effective in lowering blood pressure for the short time that control would be needed.
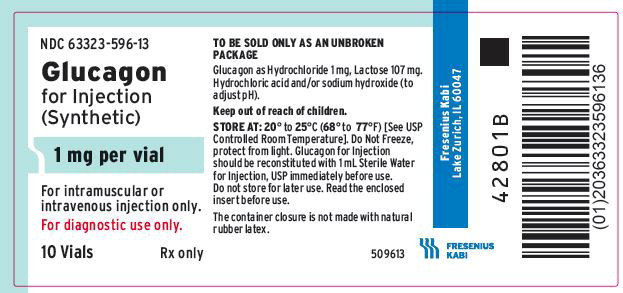
11 DESCRIPTION
Glucagon is an antihypoglycemic agent and a gastrointestinal motility inhibitor. It is produced by solid phase peptide synthesis. The chemical structure of the glucagon is identical to human glucagon. Glucagon is a single-chain polypeptide containing 29 amino acid residues. The structure of glucagon is:
 |
|
| Molecular Formula = C153H225N43O49S | Molecular Weight = 3483 |
Glucagon for Injection is a sterile, lyophilized white powder in a 3 mL vial for subcutaneous, intramuscular or intravenous use. The reconstituted solution contains glucagon as hydrochloride 1 mg per mL and lactose monohydrate (107 mg). Glucagon for Injection is supplied at pH 2.5 to 3.5 and is soluble in water.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Glucagon increases blood glucose concentration by activating hepatic glucagon receptors, thereby stimulating glycogen breakdown and release of glucose from the liver. Hepatic stores of glycogen are necessary for glucagon to produce an antihypoglycemic effect. Extrahepatic effects of glucagon include relaxation of the smooth muscle of the stomach, duodenum, small bowel, and colon.
12.2 Pharmacodynamics
Treatment of Severe Hypoglycemia
Blood glucose concentration rises within 10 minutes of injection and maximal concentrations are attained at approximately 30 minutes after injection (see Figure 1). The duration of hyperglycemic action after intravenous or intramuscular injection is 60 to 90 minutes.
Figure 1. Recovery from Insulin Induced Hypoglycemia (mean blood glucose) After Intramuscular Injection of 1 mg of Another Glucagon for Injection Product in Type I Diabetic Men
Diagnostic Aid
|
aDose is determined based on the length of the procedure. |
||||
| Route of Administration | Dosea | Time of Maximal
Glucose Concentration | Time of Onset of
Action for GI Smooth Muscle Relaxation | Duration of
Smooth Muscle Relaxation |
| Intravenous | 0.25 to 0.5 mg | 5 to 20 minutes | 45 seconds | 9 to 17 minutes |
|
aDose is determined based on the length of the procedure. |
||||
| Route of Administration | Dosea | Time of Maximal
Glucose Concentration | Time of Onset of
Action for GI Smooth Muscle Relaxation | Duration of
Smooth Muscle Relaxation |
| Intramuscular | 1 mg | 30 minutes | 8 to 10 minutes | 12 to 27 minutes |
| 2 mg | 30 minutes | 4 to 7 minutes | 21 to 32 minutes | |
In a study in healthy subjects, a subcutaneous dose of 1 mg Glucagon for Injection resulted on average a peak blood glucose concentration of 79.3 mg/dL with a median time of 50 minutes after injection.
12.3 Pharmacokinetics
Absorption
Following subcutaneous administration of Glucagon for Injection, the median time to reach the maximum baseline uncorrected plasma glucagon concentrations of 3533 pg/mL was approximately 10 to 13 minutes after dosing Following intramuscular administration of 1 mg dose, the maximum baseline uncorrected plasma glucagon concentrations of 3391 pg/mL were attained approximately 10 minutes after dosing.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long term studies in animals to evaluate carcinogenic potential have not been performed.
Mutagenesis
Synthetic glucagon was negative in the bacterial reverse mutation assay (Ames test). The clastogenic potential of synthetic glucagon in the Chinese Hamster Ovary (CHO) assay was positive in the absence of metabolic activation. Doses of 100 and 200 mg/kg of glucagon of both pancreatic and recombinant origins gave slightly higher incidences of micronucleus formation in male mice but there was no effect in females. The weight of evidence indicates that synthetic and recombinant glucagon are not different and do not pose a genotoxic risk to humans.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Glucagon for Injection is supplied as a sterile, lyophilized white powder available as follows:
| Presentation | NDC | Strength | Description |
| Treatment of Severe Hypoglycemia | |||
| Glucagon Emergency Kit for Low Blood Sugar | 63323-582-82 | 1 mg per vial | 1 mL single-dose vial of Glucagon for Injection with 1 mL single-dose syringe of Sterile Water for Injection, USP for reconstitution |
| Use as a Diagnostic Aid | |||
| 10 Single-dose vials | 63323-596-13 | 1 mg per vial | 1 mL single-dose vial of Glucagon for Injection (NDC 63323-596-11) |
| Diagnostic Kit | 63323-593-03 | 1 mg per vial | 1 mL single-dose vial of Glucagon for Injection (NDC 63323-596-03) with 1 mL single-dose vial of Sterile Water for Injection, USP for reconstitution (NDC 63323-185-03) |
16.2 Recommended Storage
Before Reconstitution
The package containing Glucagon for Injection vials may be stored up to 24 months at 20° to 25° C (68° to 77° F) [see USP Controlled Room Temperature] prior to reconstitution. Do not freeze. Keep in the original package to protect from light.
After Reconstitution
Use reconstituted glucagon solution immediately. Discard any unused portion [see Dosage and Administration (2.3)].
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Recognition of Severe Hypoglycemia
Inform patient and family members or caregivers on how to recognize the signs and symptoms of severe hypoglycemia and the risks of prolonged hypoglycemia.
Administration
Review the Patient Information and Instructions for Use with the patient and family members or caregivers.
Serious Hypersensitivity
Inform patients that allergic reactions can occur with Glucagon for Injection. Advise patients to seek immediate medical attention if they experience any symptoms of serious hypersensitivity reactions [see Warnings and Precautions (5.3)].
|
This Patient Information has been approved by the U.S. Food and Drug Administration |
Approved: 09/2019 |
||
| PATIENT INFORMATION
Glucagon (GLOO-ka-gon) for injection, for subcutaneous, intramuscular or intravenous use |
|||
| What is Glucagon?
Glucagon is a prescription medicine used:
|
|||
| Who should not use Glucagon?
Do not use Glucagon if:
|
|||
| What should I tell my doctor before using Glucagon?
Before using Glucagon, tell your doctor about all of your medical conditions, including if you:
|
|||
| Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. Glucagon may affect the way other medicines work, and other medicines may affect how Glucagon works. Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine. | |||
How should I use Glucagon?
|
|||
| What are the possible side effects of Glucagon?
Glucagon may cause serious side effects, including:
|
|||
| The most common side effects of Glucagon include: | |||
|
|
|
|
| Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Glucagon. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |||
| How should I store Glucagon?
Before you mix the Glucagon powder and liquid:
|
|||
After you mix the Glucagon powder and liquid:
|
|||
| Keep Glucagon and all medicines out of the reach of children. | |||
| General information about the safe and effective use of Glucagon:
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Glucagon for a condition for which it was not prescribed. Do not give Glucagon to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about Glucagon that is written for health professionals. |
|||
| What are the ingredients in the Glucagon?
Active Ingredient: Glucagon Inactive ingredients: lactose monohydrate and sterile water for reconstitution For more information, go to www.fresenius-kabi.com/us or call 1-800-551-7176. |
|||
Instructions for Use
Glucagon (GLOO-ka-gon)
for injection, for subcutaneous, intramuscular or intravenous use
Read this Instructions for Use before you start using Glucagon and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or treatment. Talk to your doctor or pharmacist if you have any questions about how to use Glucagon.
Important:
- Read and become familiar with this Instructions for Use before an emergency happens.
- Show your family members and others where you keep your Glucagon Emergency Kit for Low Blood Sugar and how to use it the right way.
- Call for emergency medical help right after you use Glucagon.
- Do not share your Glucagon syringes or needles with another person. You may give other people a serious infection or other people may get a serious infection from you.
- The prefilled syringe that comes with your Glucagon Emergency Kit for Low Blood Sugar is meant for use with Glucagon only. Do not use Glucagon syringes to inject other medicines.
How should I store Glucagon?
Before you mix the Glucagon powder and liquid:
- Store Glucagon at room temperature between 68° to 77°F (20° to 25°C). Check the expiration date on your vial of Glucagon. Do not use Glucagon if the expiration date has passed.
- Do not freeze Glucagon.
- Keep Glucagon in its original package and Glucagon out of light.
After you mix the Glucagon powder and liquid:
- Use Glucagon right away.
- Throw away any unused Glucagon.
- Glucagon should be clear and colorless. Do not use Glucagon if it is cloudy or if you see particles in the solution.
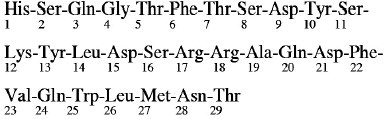
Supplies you will need for your Glucagon injection (See Figure A):
- 1 Glucagon Emergency Kit for Low Blood Sugar that contains:
- 1 vial that contains 1 mg of Glucagon for injection and 1 prefilled glass syringe with attached needle that contains 1 mL of Sterile Water for Injection.
 |
| Figure A |
- 1 puncture resistant container for throwing away used needles and syringes. See “How should I dispose of (throw away) used Glucagon prefilled syringes” at the end of these instructions.
- Cotton ball or gauze pad (not included in kit)
- Preparing the Glucagon dose:
- The Glucagon medicine comes as a dry powder. Before you use Glucagon, you must mix the dry powder with the syringe of sterile water that comes in the Glucagon Emergency Kit for Low Blood Sugar. Do not use any other liquid to mix the medicine.
- Check that the orange plastic cap on your vial of Glucagon is firmly attached. Do not use the vial of Glucagon if the orange plastic cap is loose or missing.
| Step 1. Using your thumb, flip the orange plastic cap off the Glucagon vial (See Figure B). | Figure B
| 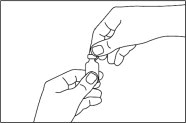 |
Step 2. Pick up the prefilled syringe containing sterile water. Hold the syringe with 1 hand and with your other hand pull the needle cover off the syringe (See Figure C).
| Figure C | 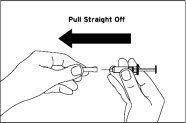 |
| Step 3. Pick up the Glucagon vial. Hold the vial of dry powder with 1 hand and with your other hand push the needle of the prefilled syringe through the center of the rubber stopper (See Figure D). | Figure D | 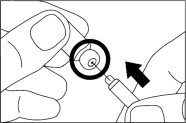 |
Step 4. Hold the vial and syringe together, with the needle still inserted into the vial. Carefully turn the vial and syringe together right side up. Slowly push the plunger down until the syringe is empty (See Figure E).
| Figure E | 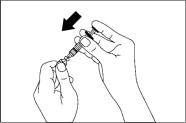 |
Step 5. Hold the entire unit (the vial and syringe) in 1 hand and gently shake the vial until the powder is completely dissolved (See Figure F).
| Figure F |  |
Step 6. Firmly hold the vial and syringe together, with the needle still inserted into the vial. Carefully turn the vial and syringe together upside down. Gently pull down on the plunger and slowly withdraw all of the liquid into the syringe (See Figure G).
| Figure G | 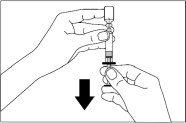 |
| Step 7. Keep the needle inside the vial. Check the syringe for air bubbles. If you see bubbles, tap the syringe until the bubbles rise to the top of the syringe (See Figure H). Gently push on the plunger to move only the air bubbles back into the vial. | Figure H | 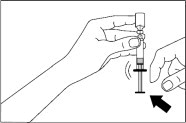 |
| Step 8. Hold the vial and syringe as shown (See Figure I) | Figure I |  |
| Giving the Glucagon for Injection: | ||
| Step 9. Choose the injection site (See Figure J). Common injection sites for Glucagon are upper arms, thighs, or buttocks. Patient does not need to be laying down to administer the medication as long as the common injection sites can be easily accessed. | Figure J | 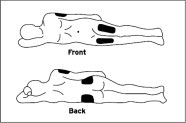 |
| Step 10. With 1 hand gently pinch the skin at the injection site. With your other hand insert the needle into the skin and push the syringe plunger down until the syringe is empty (See Figure K). | Figure K |  |
| After Giving the Glucagon injection: | ||
| Step 11. Pull the needle out of the skin and press on the injection site (See Figure L). Use a gauze pad or cotton ball (not included in the kit) if needed to press the injection site to make sure there is no direct contact with the skin. | Figure L | 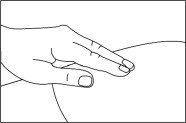 |
Throw away your used syringe with the needle attached and any Glucagon you did not use. See “How should I dispose of (throw away) used Glucagon prefilled syringes” at the end of these instructions.
Step 12. Turn the person on their side. When an unconscious person awakens, they may vomit. Turning the person on their side will lessen the chance of choking.
Step 13. Call for emergency medical help right away. If the person does not respond after 15 minutes,
another dose may be given, if available.
Step 14. Feed the person as soon as they are awake and able to swallow.
Give the person a fast acting source of sugar (such as a regular soft drink or fruit juice) and a long acting source of sugar (such as crackers and cheese or a meat sandwich).
Step 15. Even if the Glucagon for Injection treatment wakes the person, tell their doctor right away. The doctor should be told whenever a severe drop in blood sugar (hypoglycemia reaction) happens. The person's dose of diabetes medicine may need to be changed.
Hypoglycemia may happen again after receiving Glucagon for Injection treatment. Early symptoms of hypoglycemia may include:
|
|
If not treated early, hypoglycemia may worsen and the person may have severe hypoglycemia. Signs of severe hypoglycemia include:
|
|
How should I dispose of (throw away) Glucagon pre-filled syringes?
- Put used syringes in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles and syringes in your household trash.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
Keep Glucagon and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Approved: 09/2019
The brand names mentioned in this document are the trademarks of their respective owners.
www.fresenius-kabi.com/us
451081D
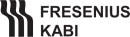
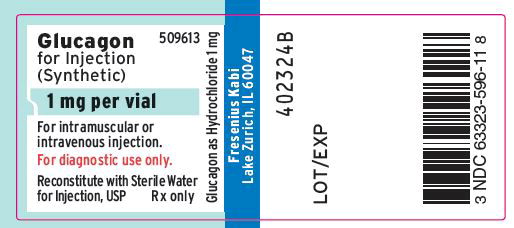
PACKAGE LABEL - PRINCIPAL DISPLAY - Glucagon Kit 1 mg Vial Label
Glucagon 509603
for Injection
(Synthetic)
1 mg per vial
For intramuscular or intravenous injection.
For diagnostic use only.
Reconstitute with Sterile Water for Injection, USP Rx only
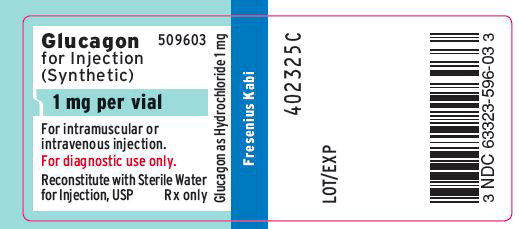
PACKAGE LABEL - PRINCIPAL DISPLAY - Glucagon Kit 1 mL Diluent Vial Label
Sterile Water for Injection, USP
1 mL per vial
FOR DRUG DILUENT USE ONLY
Contains no antimicrobial or other added substance. Do not
give intravenously unless rendered nearly Isotonic.
Discard unused portion.
1 mL Single Dose Vial Rx only
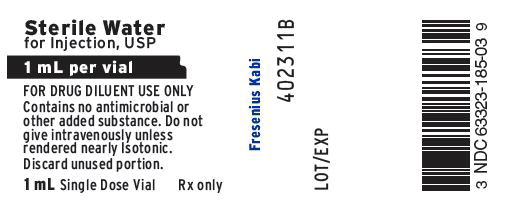
PACKAGE LABEL - PRINCIPAL DISPLAY - Glucagon Kit 1 mg Vial Carton Panel
Glucagon 509603
for Injection
(Synthetic)
1 mg per vial
For intramuscular or intravenous injection only.
FOR DIAGNOSTIC USE ONLY.
Reconstitute with Sterile Water for Injection, USP immediately before use.
Each kit contains:
- One single dose vial with 1 mg of Glucagon for Injection
- One single dose vial with 1 mL of Sterile Water for Injection, USP
Single Dose Vials
Rx only